Changes in Community-Dwelling Elderly’s Activity and Participation Affecting Depression during COVID-19 Pandemic: A Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Procedure and Outcome Measures
2.4. Data Analysis
2.5. Ethical Considerations
3. Results
3.1. Participant Characteristics and Activity Implementation Status
3.2. Changes in the Number of Activities Compared to Pre-Pandemic Status
3.3. Effect of Activity Retention and the Number of Social Networks on Depression in the COVID-19 Pandemic
4. Discussion
4.1. Participant Characteristics and Activity Implementation Status
4.2. Comparison of Activity Retention Rates before and during the Pandemic
4.3. Factors Associating Depression in the Community-Dwelling Elderly during the COVID-19 Pandemic
4.4. Practical Implications and Future Research
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| IADL | Mean (SD) | L-Leisure | Mean (SD) | H-Leisure | Mean (SD) | Sociocultural Activity | Mean (SD) |
|---|---|---|---|---|---|---|---|
| Putting the rubbish/recycling out | 0.98 (0.09) | Reading a newspaper | 0.98 (0.13) | Gardening/growing flowers | 0.93 (0.20) | Voting | 0.96 (0.17) |
| Keeping household accounts | 0.97 (0.12) | Taking a rest | 0.96 (0.14) | Ground golf | 0.87 (0.35) | Cleaning/maintaining family Buddhist altar | 0.95 (0.15) |
| Washing up | 0.96 (0.14) | Watching television | 0.93 (0.20) | Growing vegetables | 0.85 (0.29) | Being with spouse/partner | 0.92 (0.24) |
| Caring for own health at home | 0.95 (0.18) | Sitting and thinking | 0.93 (0.18) | Radio gymnastic/yoga/Pilates | 0.84 (0.29) | Giving seasonal gift | 0.84 (0.29) |
| Preparing a hot drink | 0.95 (0.15) | Using a computer | 0.91 (0.23) | Walking | 0.78 (0.30) | Visiting graves | 0.74 (0.33) |
| Doing the laundry | 0.92 (0.21) | Listening to the radio | 0.91 (0.19) | Shopping for recreation | 0.71 (0.29) | Writing letters | 0.72 (0.31) |
| Cleaning the room | 0.92 (0.21) | Using mobile phone | 0.91 (0.19) | Going to garden/park | 0.68 (0.35) | Studying for personal advancement | 0.68 (0.43) |
| Working in paid employment | 0.92 (0.20) | Reading a book/magazine | 0.89 (0.24) | Going to spa | 0.40 (0.40) | Attending a community/senior group | 0.68 (0.34) |
| Cooking meal | 0.91 (0.24) | Watching video/DVD | 0.86 (0.28) | Traveling | 0.30 (0.36) | Volunteering (nonpaid work) | 0.65 (0.36) |
| Payment | 0.90 (0.25) | Doing crosswords/Sudoku | 0.85 (0.26) | Taking a day trip | 0.30 (0.34) | Going to coffee shop with family or friends | 0.60 (0.32) |
| Driving | 0.90 (0.23) | Arranging room | 0.85 (0.23) | mean (SD) | 0.67 (0.32) | Eating out | 0.58 (0.30) |
| Keeping a diary | 0.89 (0.28) | Cooking/baking as a hobby | 0.84 (0.30) | Going to places of worship | 0.57 (0.40) | ||
| Talking on the telephone | 0.89 (0.21) | Listening to music | 0.83 (0.29) | Visiting family/friends who are ill | 0.55 (0.39) | ||
| Using ATM | 0.89 (0.21) | Looking at photo albums/home videos | 0.70 (0.37) | Doing activities with children/grandchildren | 0.54 (0.44) | ||
| Taking care of others | 0.87 (0.27) | Taking photographs | 0.68 (0.40) | Going to the library | 0.45 (0.49) | ||
| Hanging out Futon | 0.86 (0.25) | Handcraft/knitting | 0.66 (0.39) | Visiting friends/acquaintances | 0.45 (0.38) | ||
| Going to the doctor/dentist | 0.86 (0.24) | Coloring books/collage of pieces of colored paper | 0.63 (0.48) | Gathering with family/relatives | 0.39 (0.42) | ||
| Taking care of pets | 0.85 (0.29) | Karaoke | 0.45 (0.43) | Going to alumni | 0.28 (0.40) | ||
| Sewing/repairing clothes | 0.84 (0.29) | mean (SD) | 0.82 (0.27) | mean (SD) | 0.64 (0.34) | ||
| Cleaning around house | 0.84 (0.28) | ||||||
| Going to the hairdresser/barber | 0.83 (0.24) | ||||||
| Food/grocery shopping | 0.79 (0.25) | ||||||
| Riding a bicycle | 0.75 (0.38) | ||||||
| Heavy household chores | 0.73 (0.34) | ||||||
| Shopping for clothes/shoes | 0.66 (0.33) | ||||||
| Using public transport | 0.61 (0.33) | ||||||
| mean (SD) | 0.86 (0.24) |
References
- Shimokihara, S.; Maruta, M.; Akasaki, Y.; Ikeda, Y.; Han, G.; Kamasaki, T.; Tokuda, K.; Hidaka, Y.; Akasaki, Y.; Tabira, T. Association between Frequency of Going Out and Psychological Condition among Community-Dwelling Older Adults after the COVID-19 Pandemic in Japan. Healthcare 2022, 10, 439. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health. Labour and Welfare (in Japan) Preventing COVID-19 and Stopping Its Spread. Available online: https://www.c19.mhlw.go.jp/covid-19-en.html (accessed on 19 November 2022).
- Yamada, M.; Kimura, Y.; Ishiyama, D.; Otobe, Y.; Suzuki, M.; Koyama, S.; Kikuchi, T.; Kusumi, H.; Arai, H. Effect of the COVID-19 epidemic on physical activity in community-dwelling older adults in Japan: A cross-sectional online survey. J. Nutr. Health Aging 2020, 24, 948–950. [Google Scholar] [CrossRef] [PubMed]
- Sepúlveda-Loyola, W.; Rodríguez-Sánchez, I.; Pérez-Rodríguez, P.; Ganz, F.; Torralba, R.; Oliveira, D.V.; Rodríguez-Mañas, L. Impact of social isolation due to COVID-19 on health in older people: Mental and physical effects and recommendations. J. Nutr. Health Aging 2020, 24, 938–947. [Google Scholar] [CrossRef] [PubMed]
- Callow, D.D.; Arnold-Nedimala, N.A.; Jordan, L.S.; Pena, G.S.; Won, J.; Woodard, J.L.; Smith, J.C. The mental health benefits of physical activity in older adults survive the COVID-19 pandemic. Am. J. Geriatr. Psychiatry 2020, 28, 1046–1057. [Google Scholar] [CrossRef] [PubMed]
- Wolf, S.; Seiffer, B.; Zeibig, J.M.; Welkerling, J.; Brokmeier, L.; Atrott, B. Is physical activity associated with less depression and anxiety during the COVID-19 pandemic? a rapid systematic review. Sports Med. 2021, 51, 1771–1783. [Google Scholar] [CrossRef]
- Currier, D.; Lindner, R.; Spittal, M.J.; Cvetkovski, S.; Pirkis, J.; English, D.R. Physical activity and depression in men: Increased activity duration and intensity associated with lower likelihood of current depression. J. Affect. Disord. 2020, 260, 426–431. [Google Scholar] [CrossRef] [PubMed]
- Giuli, C.; Papa, R.; Mocchegiani, E.; Marcellini, F. Predictors of participation in physical activity for community-dwelling elderly Italians. Arch. Gerontol Geriatr. 2012, 54, 50–54. [Google Scholar] [CrossRef]
- Jeong, E.H.; Park, J.H. The relationship among leisure activities, depression and quality of life in community-dwelling elderly Koreans. Gerontol. Geriatr. Med. 2020, 6, 2333721420923449. [Google Scholar] [CrossRef]
- Chang, C.-F.; Lin, M.-H.; Wang, J.; Fan, J.-Y.; Chou, L.-N.; Chen, M.-Y. The relationship between geriatric depression and health-promoting behaviors among community-dwelling seniors. J. Nurs. Res. 2013, 21, 75–82. [Google Scholar] [CrossRef]
- Choi, E.; Han, K.-M.; Chang, J.; Lee, Y.J.; Choi, K.W.; Han, C.; Ham, B.-J. Social participation and depressive symptoms in community-dwelling older adults: Emotional social support as a mediator. J. Psychiatr. Res. 2021, 137, 589–596. [Google Scholar] [CrossRef]
- Park, M.J.; Park, N.S.; Chiriboga, D.A. A latent class analysis of social activities and health among community-dwelling older adults in Korea. Aging Ment. Health 2018, 22, 625–630. [Google Scholar] [CrossRef]
- Caroppo, E.; Mazza, M.; Sannella, A.; Marano, G.; Avallone, C.; Claro, A.E.; Janiri, D.; Moccia, L.; Janiri, L.; Sani, G. Will nothing be the same again?: Changes in lifestyle during COVID-19 pandemic and consequences on mental health. Int. J. Environ. Res. Public Health 2021, 18, 8433. [Google Scholar] [CrossRef] [PubMed]
- Uemura, J.I.; Tanikaga, M.; Tanaka, M.; Shimose, M.; Hoshino, A.; Igarashi, G. Selection of activity items for development of the activity card sort–Japan version. OTJR (Thorofare N. J.) 2019, 39, 23–31. [Google Scholar] [CrossRef]
- Packer, T.L.; Boshoff, K.; Dejonge, D. Development of the activity card sort–Australia. Aust. Occup. Ther. J. 2008, 55, 199–206. [Google Scholar] [CrossRef]
- Alegre-Muelas, C.; Alegre-Ayala, J.; Huertas-Hoyas, E.; Martínez-Piédrola, M.; Pérez-Corrales, J.; Máximo-Bocanegra, N.; Sánchez-Camarero, C.; Pérez-de-Heredia-Torres, M. Spanish transcultural adaptation of the activity card sort. Occup. Ther. Int. 2019, 2019, 4175184. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Laver-Fawcett, A.J.; Mallinson, S.H. Development of the activity card sort–United Kingdom version (ACS-UK). OTJR (Thorofare N. J.) 2013, 33, 134–145. [Google Scholar] [CrossRef]
- Chan, V.W.K.; Chung, J.C.C.; Packer, T.L. Validity and reliability of the activity card sort–Hong Kong version. OTJR Occup. Particip. Health 2006, 26, 152–158. [Google Scholar] [CrossRef]
- Orellano, E.M.; Ito, M.; Dorne, R.; Irizarry, D.; Dávila, R. Occupational participation of older adults: Reliability and validity of the Activity Card Sort–Puerto Rican version. OTJR Occup. Particip. Health 2012, 32, 266–272. [Google Scholar] [CrossRef]
- Seaton, L.; Brown, T. The relationship between body function and structure factors and the activity-participation of healthy community-dwelling older adults. Phys. Occup. Ther. Geriatr. 2018, 36, 121–135. [Google Scholar] [CrossRef]
- Plagg, B.; Engl, A.; Piccoliori, G.; Eisendle, K. Prolonged social isolation of the elderly during COVID-19: Between benefit and damage. Arch. Gerontol. Geriatr. 2020, 89, 104086. [Google Scholar] [CrossRef]
- Cotterell, N.; Buffel, T.; Phillipson, C. Preventing social isolation in older people. Maturitas 2018, 113, 80–84. [Google Scholar] [CrossRef] [Green Version]
- Courtin, E.; Knapp, M. Social isolation, loneliness and health in old age: A scoping review. Health Soc. Care Community 2017, 25, 799–812. [Google Scholar] [CrossRef]
- Fulbright, S.A. Rates of depression and participation in senior centre activities in community-dwelling older persons. J. Psychiatr. Ment. Health Nurs. 2010, 17, 385–391. [Google Scholar] [CrossRef] [PubMed]
- Gorenko, J.A.; Moran, C.; Flynn, M.; Dobson, K.; Konnert, C. Social isolation and psychological distress among older adults related to COVID-19: A narrative review of remotely delivered interventions and recommendations. J. Appl. Gerontol. 2021, 40, 3–13. [Google Scholar] [CrossRef]
- Cornwell, E.Y.; Waite, L.J. Measuring social isolation among older adults using multiple indicators from the NSHAP study. J. Gerontol. B Psychol. Sci. Soc. Sci. 2009, 64, i38–i46. [Google Scholar] [CrossRef] [Green Version]
- Robins, L.M.; Hill, K.D.; Finch, C.F.; Clemson, L.; Haines, T. The association between physical activity and social isolation in community-dwelling older adults. Aging Ment. Health 2018, 22, 175–182. [Google Scholar] [CrossRef]
- Gyasi, R.M.; Adu-Gyamfi, S.; Obeng, B.; Asamoah, E.; Kisiangani, I.; Ochieng, V.; Appiah, K. Association between physical activity participation and perceived social isolation at older ages: Do social participation, age and sex differences matter? Arch. Gerontol. Geriatr. 2021, 96, 104441. [Google Scholar] [CrossRef]
- Toepoel, V. Ageing, leisure, and social connectedness: How could leisure help reduce social isolation of older people? Soc. Indic. Res. 2013, 113, 355–372. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. STROBE Checklist: Cross-Sectional Studies. Available online: https://www.strobe-statement.org/ (accessed on 19 November 2022).
- Status of Kozoji New Town (Population), Aging Rate (Ishiodai, Kasugai, Japan, as of October 2020). Available online: https://www.city.kasugai.lg.jp/_res/projects/default_project/_page_/001/008/950/zinkou202010.pdf (accessed on 19 November 2022).
- Baum, C.M.; Edwards, D.F. Activity Card Sort (ACS): Test Manual, 2nd ed.; AOTA Press: Bethesda, MD, USA, 2008. [Google Scholar]
- Spitzer, J.; Tse, T.; Baum, C.M.; Carey, L.M. Mild impairment of cognition impacts on activity participation after stroke in a community-dwelling Australian cohort. OTJR (Thorofare N. J.) 2011, 31, S8–S15. [Google Scholar] [CrossRef] [PubMed]
- Carpenter, B.D.; Edwards, D.F.; Pickard, J.G.; Palmer, J.L.; Stark, S.; Neufeld, P.S.; Morrow-Howell, N.; Perkinson, M.A.; Morris, J.C. Anticipating relocation: Concerns about moving among NORC residents. J Gerontol. Soc. Work 2007, 49, 165–184. [Google Scholar] [CrossRef] [PubMed]
- Foster, E.R.; Golden, L.; Duncan, R.P.; Earhart, G.M. Community-based argentine tango dance program is associated with increased activity participation among individuals with Parkinson’s disease. Arch. Phys. Med. Rehabil. 2013, 94, 240–249. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lubben, J.; Blozik, E.; Gillmann, G.; Iliffe, S.; von Renteln Kruse, W.; Beck, J.C.; Stuck, A.E. Performance of an abbreviated version of the Lubben Social Network Scale among three European Community-dwelling older adult populations. Gerontologist 2006, 46, 503–513. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kurimoto, A.; Awata, S.; Ohkubo, T.; Tsubota-Utsugi, M.; Asayama, K.; Takahashi, K.; Suenaga, K.; Satoh, H.; Imai, Y. Reliability and validity of the Japanese version of the abbreviated Lubben Social Network Scale. Nihon Ronen Igakkai Zasshi 2011, 48, 149–157. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Imamura, K.; Kamide, N.; Sakamoto, M.; Sato, H.; Shiba, Y.; Matsunaga, A. Association between social network and physical function in community-dwelling older adults in Japan. Phys. Ther. Res. 2020, 23, 153–159. [Google Scholar] [CrossRef]
- Iwasa, H.; Yoshida, Y. Personality and health literacy among community-dwelling older adults living in Japan. Psychogeriatrics 2020, 20, 824–832. [Google Scholar] [CrossRef]
- Sheikh, J.I.; Yesavage, J.A. Geriatric Depression Scale (GDS) recent evidence and development of a shorter version. Clin. Gerontol. 1986, 5, 165–173. [Google Scholar] [CrossRef]
- Sugishita, K.; Sugishita, M.; Hemmi, I.; Asada, T.; Tanigawa, T. A validity and reliability study of the Japanese version of the Geriatric Depression Scale 15 (GDS-15-J). Clin. Gerontol. 2017, 40, 233–240. [Google Scholar] [CrossRef]
- Nishida, T.; Nakao, R.; Nishihara, M.; Kawasaki, R.; Honda, A.; Honda, S. The relationship between mindfulness and depression in community-dwelling frail elderly. Int. J. Gerontol. 2019, 13, 273–277. [Google Scholar] [CrossRef]
- Kume, Y.; Kodama, A.; Takahashi, T.; Lee, S.; Makizako, H.; Ono, T.; Shimada, H.; Ota, H. Social frailty is independently associated with geriatric depression among older adults living in northern Japan: A cross-sectional study of ORANGE registry. Geriatr. Gerontol. Int. 2022, 22, 145–151. [Google Scholar] [CrossRef]
- Iwasa, H.; Masui, Y.; Inagaki, H.; Yoshida, Y.; Shimada, H.; Otsuka, R.; Kikuchi, K.; Nonaka, K.; Yoshida, H.; Yoshida, H.; et al. Development of the Japan Science and Technology agency index of competence to assess functional capacity in older adults: Conceptual definitions and preliminary items. Gerontol. Geriatr. Med. 2015, 1, 2333721415609490. [Google Scholar] [CrossRef] [Green Version]
- Iwasa, H.; Masui, Y.; Inagaki, H.; Yoshida, Y.; Shimada, H.; Otsuka, R.; Kikuchi, K.; Nonaka, K.; Yoshida, H.; Yoshida, H.; et al. Assessing competence at a higher level among older adults: Development of the Japan Science and Technology agency index of competence (JST-IC). Aging Clin. Exp. Res. 2018, 30, 383–393. [Google Scholar] [CrossRef] [PubMed]
- Iwasa, H.; Yoshida, Y.; Inagaki, H.; Masui, Y.; Shimada, H.; Kikuchi, K.; Ootsuka, R.; Nonaka, K.; Yoshida, H.; Suzuki, T. Development of a new index of daily functioning for the elderly in the community: Measurement invariance and standard values of the JST IC. J. Health Welf Stat. 2018, 65, 1–7. (In Japanese) [Google Scholar]
- Wada, A.; Makizako, H.; Nakai, Y.; Tomioka, K.; Taniguchi, Y.; Sato, N.; Kiuchi, Y.; Kiyama, R.; Kubozono, T.; Takenaka, T.; et al. Association between cognitive frailty and higher-level competence among community-dwelling older adults. Arch. Gerontol. Geriatr. 2022, 99, 104589. [Google Scholar] [CrossRef]
- Maruta, M.; Makizako, H.; Ikeda, Y.; Han, G.; Shimokihara, S.; Miyata, H.; Nakamura, A.; Tokuda, K.; Kubozono, T.; Ohishi, M.; et al. Characteristics of meaningful activities in community-dwelling Japanese older adults with pre-frailty and frailty. Arch. Gerontol. Geriatr. 2022, 99, 104616. [Google Scholar] [CrossRef]
- Uemura, J.I.; Uno, K.; Hoshino, A.; Tanikaga, M.; Tanaka, M.; Chishima, M. Identification of Subgroups of Activity Participation in Group of Community-Dwelling Older Adults. OTJR Occup. Ther. J. Res. 2023. [Google Scholar] [CrossRef]
- Luppa, M.; Sikorski, C.; Luck, T.; Ehreke, L.; Konnopka, A.; Wiese, B.; Weyerer, S.; König, H.H.; Riedel-Heller, S.G. Age- and gender-specific prevalence of depression in latest-life—Systematic review and meta-analysis. J. Affect. Disord. 2012, 136, 212–221. [Google Scholar] [CrossRef]
- Imaoka, M.; Nakao, H.; Nakamura, M.; Tazaki, F.; Hida, M.; Omizu, T.; Imai, R.; Takeda, M. Associations between depressive symptoms and geriatric syndromes in community-dwelling older adults in Japan: A cross-sectional study. Prev. Med. Rep. 2021, 22, 101353. [Google Scholar] [CrossRef]
- Röhr, S.; Wittmann, F.; Engel, C.; Enzenbach, C.; Witte, A.V.; Villringer, A.; Löffler, M.; Riedel-Heller, S.G. Social factors and the prevalence of social isolation in a population-based adult cohort. Soc. Psychiatry Psychiatr. Epidemiol. 2022, 57, 1959–1968. [Google Scholar] [CrossRef]
- Ibrahim, R.; Abolfathi Momtaz, Y.; Hamid, T.A. Social isolation in older Malaysians: Prevalence and risk factors. Psychogeriatrics 2013, 13, 71–79. [Google Scholar] [CrossRef]
- Shimada, K.; Yamazaki, S.; Nakano, K.; Ngoma, A.M.; Takahashi, R.; Yasumura, S. Prevalence of social isolation in community-dwelling elderly by differences in household composition and related factors: From a social network perspective in urban Japan. J. Aging Health 2014, 26, 807–823. [Google Scholar] [CrossRef] [Green Version]
- Noguchi, T.; Kubo, Y.; Hayashi, T.; Tomiyama, N.; Ochi, A.; Hayashi, H. Social isolation and self-reported cognitive decline among older adults in Japan: A longitudinal study in the COVID-19 pandemic. J. Am. Med. Dir. Assoc. 2021, 22, 1352–1356.e2. [Google Scholar] [CrossRef]
- Parlapani, E.; Holeva, V.; Nikopoulou, V.A.; Kaprinis, S.; Nouskas, I.; Diakogiannis, I. A review on the COVID-19-related psychological impact on older adults: Vulnerable or not? Aging Clin. Exp. Res. 2021, 33, 1729–1743. [Google Scholar] [CrossRef]
- Sheehan, C.M.; Tucker-Drob, E.M. Gendered expectations distort male–female differences in instrumental activities of daily living in later adulthood. J. Gerontol. B Psychol. Sci. Soc. Sci. 2019, 74, 715–723. [Google Scholar] [CrossRef] [PubMed]
- Kivi, M.; Hansson, I.; Bjälkebring, P. Up and About: Older Adults’ Well-being During the COVID-19 Pandemic in a Swedish Longitudinal Study. J. Gerontol. B Psychol. Sci. Soc. Sci. 2021, 76, e4–e9. [Google Scholar] [CrossRef]
- Morse, K.F.; Fine, P.A.; Friedlander, K.J. Creativity and leisure during COVID-19: Examining the relationship between leisure activities, motivations, and psychological well-being. Front. Psychol. 2021, 12, 609967. [Google Scholar] [CrossRef] [PubMed]
- Berkman, L.F.; Melchior, M.; Chastang, J.F.; Niedhammer, I.; Leclerc, A.; Goldberg, M. Social integration and mortality: A prospective study of French employees of electricity of France-Gas of France: The GAZEL cohort. Am. J. Epidemiol. 2004, 159, 167–174. [Google Scholar] [CrossRef] [Green Version]
- Lee, J.H.; Luchetti, M.; Aschwanden, D.; Sesker, A.A.; Strickhouser, J.E.; Terracciano, A.; Sutin, A.R. Perceived changes in social contact during COVID-19 pandemic in the United States. Pers. Relatsh 2022, 29, 59–76. [Google Scholar] [CrossRef]
- Cugmas, M.; Ferligoj, A.; Kogovšek, T.; Batagelj, Z. The social support networks of elderly people in Slovenia during the COVID-19 pandemic. PLoS ONE 2021, 16, e0247993. [Google Scholar] [CrossRef] [PubMed]
- Desha, L.N.; Ziviani, J.M. Use of time in childhood and adolescence: A literature review on the nature of activity participation and depression. Aust. Occup. Ther. J. 2007, 54, 4–10. [Google Scholar] [CrossRef]
- Heo, J.; Ryu, J.; Yang, H.; Kim, K.M. Serious leisure and depression in older adults: A study of pickleball players. Leis. Stud. 2018, 37, 561–573. [Google Scholar] [CrossRef]
- Kiyoshige, E.; Kabayama, M.; Gondo, Y.; Masui, Y.; Inagaki, H.; Ogawa, M.; Nakagawa, T.; Yasumoto, S.; Akasaka, H.; Sugimoto, K.; et al. Age group differences in association between IADL decline and depressive symptoms in community-dwelling elderly. BMC Geriatr. 2019, 19, 309. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sun, Z.; Yang, B.; Zhang, R.; Cheng, X. Influencing factors of understanding COVID-19 risks and coping behaviors among the elderly population. Int. J. Environ. Res. Public Health 2020, 17, 5889. [Google Scholar] [CrossRef] [PubMed]
- Yang, Q.; Wang, Y.; Tian, C.; Chen, Y.; Mao, J. The experiences of community-dwelling older adults during the COVID-19 lockdown in wuhan: A qualitative study. J. Adv. Nurs. 2021, 77, 4805–4814. [Google Scholar] [CrossRef] [PubMed]
- Mahapatra, P.; Sahoo, K.C.; Desaraju, S.; Pati, S. Coping with COVID-19 pandemic: Reflections of older couples living alone in urban Odisha, India. Prim. Health Care Res. Dev. 2021, 22, e64. [Google Scholar] [CrossRef] [PubMed]
- Chemen, S.; Gopalla, Y.N. Lived experiences of older adults living in the community during the COVID-19 lockdown—The case of mauritius. J. Aging Stud. 2021, 57, 100932. [Google Scholar] [CrossRef]
- Daly, J.R.; Depp, C.; Graham, S.A.; Jeste, D.V.; Kim, H.-C.; Lee, E.E.; Nebeker, C. Health impacts of the stay-at-home order on community-dwelling older adults and how technologies may help: Focus group study. JMIR Aging 2021, 4, e25779. [Google Scholar] [CrossRef]
- Huber, M.; Knottnerus, J.A.; Green, L.; van der Horst, H.; Jadad, A.R.; Kromhout, D.; Leonard, B.; Lorig, K.; Loureiro, M.I.; van der Meer, J.W.; et al. How should we define health? BMJ 2011, 343, d4163. [Google Scholar] [CrossRef] [Green Version]
- Lee, C.-T.; Yeh, C.-J.; Lee, M.-C.; Lin, H.-S.; Chen, V.C.-H.; Hsieh, M.-H.; Yen, C.-H.; Lai, T.-J. Leisure activity, mobility limitation and stress as modifiable risk factors for depressive symptoms in the elderly: Results of a national longitudinal study. Arch. Gerontol. Geriatr. 2012, 54, e221–e229. [Google Scholar] [CrossRef]
- Liang, Y.; Li, X.; Yang, T.; Li, M.; Ruan, Y.; Yang, Y.; Huang, Y.; Jiang, Y.; Wang, Y. Patterns of physical activity and their relationship with depression among community-dwelling older adults in Shanghai, China: A latent class approach. BMC Geriatr. 2021, 21, 587. [Google Scholar] [CrossRef]
- Kulmala, J.; Tiilikainen, E.; Lisko, I.; Ngandu, T.; Kivipelto, M.; Solomon, A. Personal social networks of community-dwelling oldest old during the COVID-19 pandemic-A qualitative study. Front. Public Health 2021, 9, 770965. [Google Scholar] [CrossRef]
- Benoit-Dubé, L.; Jean, E.K.; Aguilar, M.A.; Zuniga, A.M.; Bier, N.; Couture, M.; Lussier, M.; Lajoie, X.; Belchior, P. What facilitates the acceptance of technology to promote social participation in later life? A systematic review. Disabil. Rehabil. Assist. Technol. 2020, 6, 1–11. [Google Scholar] [CrossRef]
- Skałacka, K.; Pajestka, G. Digital or In-Person: The relationship between mode of interpersonal communication during the COVID-19 pandemic and mental health in older adults from 27 countries. J. Fam. Nurs. 2021, 27, 275–284. [Google Scholar] [CrossRef] [PubMed]
- Carri, H.; Jessica, R.; George, W.; Patricia, I.; Gabe, M.; Deborah, S. Understanding social isolation among urban aging adults: Informing occupation-based approaches. OTJR Occup. Particip. Health 2017, 37, 188–198. [Google Scholar] [CrossRef]
- Turcotte, P.L.; Carrier, A.; Roy, V.; Levasseur, M. Occupational therapists’ contributions to fostering older adults’ social participation: A scoping review. Br. J. Occup. Ther. 2018, 81, 427–449. [Google Scholar] [CrossRef]
- Papageorgiou, N.; Marquis, R.; Dare, J. Identifying the enablers and barriers to community participation amongst older adults. Br. J. Occup. Ther. 2016, 79, 742–751. [Google Scholar] [CrossRef] [Green Version]
- Hyett, N.; McKinstry, C.E.; Kenny, A.; Dickson-Swift, V. Community-centred practice: Occupational therapists improving the health and wellbeing of populations. Aust. Occup. Ther. J. 2016, 63, 5–8. [Google Scholar] [CrossRef]
- Park, S.; Choi, B.; Choi, C.; Kang, J.M.; Lee, J.Y. Relationship between education, leisure activities, and cognitive functions in older adults. Aging Ment. Health 2019, 23, 1651–1660. [Google Scholar] [CrossRef]
- World Health Organization. Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health: Final Report of the Commission on Social Determinants of Health. Available online: https://apps.who.int/iris/bitstream/handle/10665/43943/9789241563703_eng.pdf (accessed on 19 November 2022).
| n (%) | Mean (SD) | Median | IQR 1 | Minimum | Max | Normality 2 | |
| Age (years) | - | 78.6 (5.64) | 78.00 | 7.00 | 68.00 | 95.00 | 0.068 |
| 65–74 | 17 (23.0) | - | - | - | - | - | - |
| 75–84 | 46 (62.2) | - | - | - | - | - | - |
| 85 and above | 11 (14.9) | - | - | - | - | - | - |
| Sex (numbers) | |||||||
| Male | 40 (54.1) | - | - | - | - | - | - |
| Female | 34 (45.9) | - | - | - | - | - | - |
| Living arrangement (numbers) | |||||||
| Living alone | 20 (27.0) | - | - | - | - | - | - |
| Living with spouse | 36 (48.6) | - | - | - | - | - | - |
| Living with other family units | 18 (24.3) | - | - | - | - | - | - |
| JST-IC (points) 3 | 11.41 (3.17) | 12.00 | 5.00 | 5.00 | 16.00 | 0.001 | |
| GDS-15-J (points) 4 | - | 3.14 (3.12) | 2.50 | 4.00 | 0.00 | 12.00 | 0.000 |
| LSNS-6 (points) 5 | - | 17.2 (5.70) | 18.00 | 8.25 | 3.00 | 29.00 | 0.337 |
| ACS-JPN 6 | |||||||
| State of implementation (items) | |||||||
| IADL (26 items) | - | 14.95 (4.91) | 16.50 | 7.38 | 2.00 | 23.00 | 0.017 |
| Male | - | 13.60 (4.85) | 13.00 | 8.38 | 5.00 | 22.00 | 0.117 |
| Female | - | 16.54 (4.56) | 17.00 | 4.25 | 2.00 | 23.00 | 0.006 |
| L-Leisure (18 items) | - | 8.70 (3.17) | 8.50 | 5.13 | 3.00 | 16.00 | 0.088 |
| H-Leisure (10 items) | - | 3.70 (1.87) | 3.50 | 2.50 | 0.00 | 9.00 | 0.207 |
| Sociocultural activity (18 items) | - | 7.29 (3.00) | 7.00 | 3.75 | 1.50 | 15.00 | 0.292 |
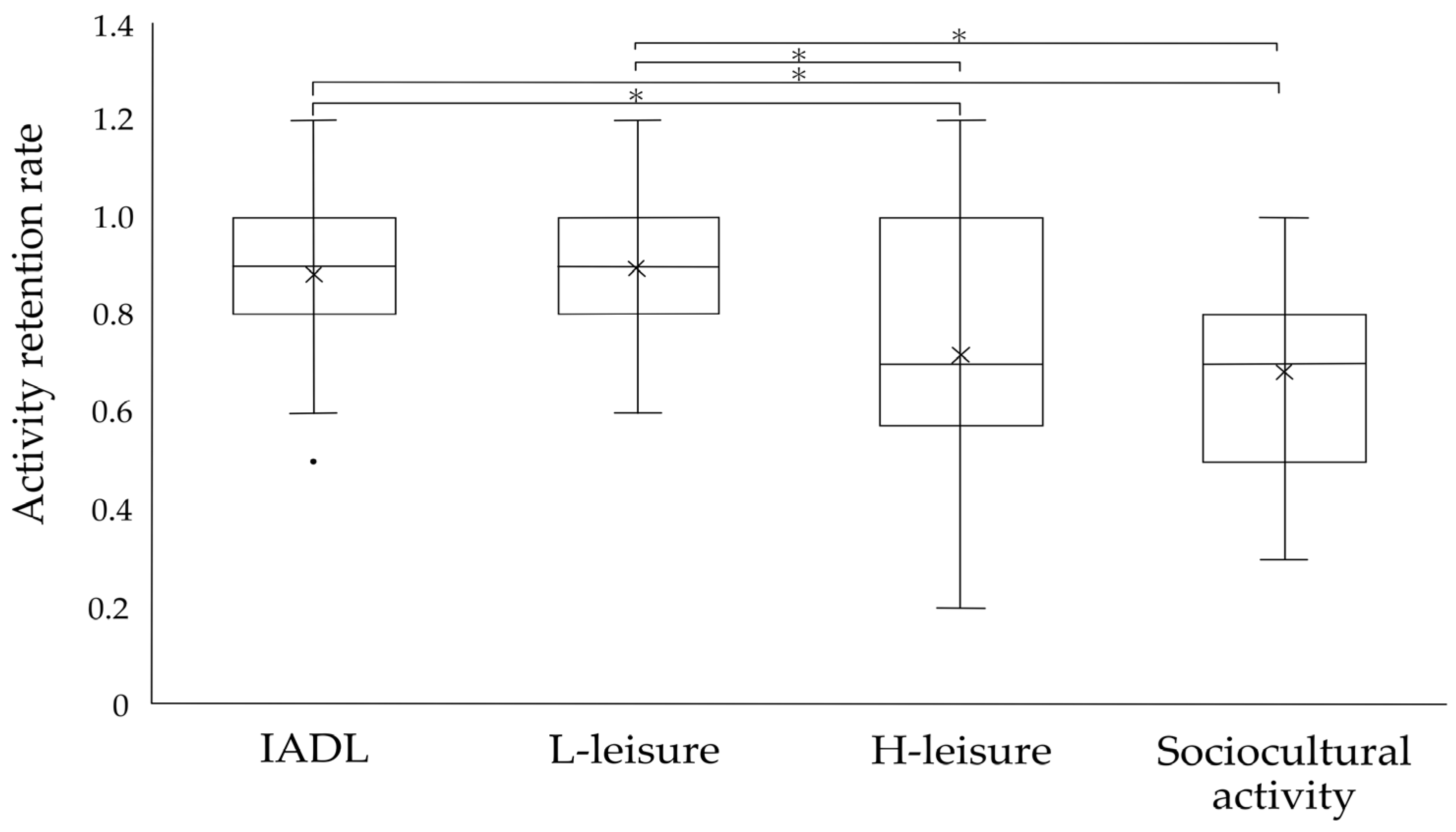
| Retention rate | |||||||
| IADL | - | 0.86 (0.24) | 0.90 | 0.20 | 0.50 | 1.20 | 0.000 |
| L-Leisure | - | 0.82 (0.27) | 0.90 | 0.20 | 0.50 | 1.20 | 0.000 |
| H-Leisure | - | 0.67 (0.32) | 0.70 | 0.43 | 0.20 | 1.20 | 0.002 |
| Sociocultural activity | - | 0.64 (0.34) | 0.70 | 0.30 | 0.30 | 1.00 | 0.000 |
| Age | Sex | Living Arrangement | ||||||
|---|---|---|---|---|---|---|---|---|
| rs | p-Value | F | Z | p-Value | F | H | p-Value | |
| GDS-15 | −0.10 | 0.390 2 | - | −0.81 | 0.417 4 | - | 1.31 | 0.519 6 |
| LSNS-6 | 0.13 | 0.264 1 | 4.11 | - | 0.050 3 | 0.68 | - | 0.509 5 |
| ACS-JPN | ||||||||
| State of implementation | ||||||||
| IADL | −0.02 | 0.901 2 | - | −2.52 | 0.012 4* | - | 2.77 | 0.250 6 |
| L-Leisure | −0.14 | 0.220 1 | 1.73 | - | 0.193 3 | 2.33 | - | 0.105 5 |
| H-Leisure | −0.09 | 0.447 1 | 0.09 | - | 0.767 3 | 2.06 | - | 0.136 5 |
| Sociocultural activity | −0.09 | 0.443 1 | 0.04 | - | 0.839 3 | 0.60 | - | 0.555 5 |
| Retention rate | ||||||||
| IADL | 0.07 | 0.580 2 | - | −0.06 | 0.950 4 | - | 1.58 | 0.453 6 |
| L-Leisure | −0.04 | 0.764 2 | - | −0.41 | 0.683 4 | - | 0.73 | 0.694 6 |
| H-Leisure | 0.10 | 0.384 2 | - | −0.78 | 0.435 4 | - | 5.32 | 0.070 6 |
| Sociocultural activity | 0.12 | 0.292 2 | - | −1.14 | 0.253 4 | - | 2.86 | 0.239 6 |
| Crude Model | Model 1 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| B | 95% CI | Wald χ2 | p-Value | B | 95% CI | Wald χ2 | p-Value | |||
| ACS-JPN retention rate | ||||||||||
| IADL | −0.43 | −1.48 | 0.61 | 0.66 | 0.42 | −0.39 | −1.43 | 0.65 | 0.53 | 0.47 |
| L-Leisure | −1.41 | −2.33 | −0.49 | 9.08 | 0.00 * | −1.60 | −2.56 | −0.64 | 10.57 | 0.00 * |
| H-Leisure | −0.85 | −0.79 | 0.63 | 0.06 | 0.82 | −0.07 | −0.77 | 0.64 | 0.03 | 0.86 |
| Sociocultural activity | −0.46 | −1.22 | 0.29 | 1.44 | 0.23 | −0.38 | −1.15 | 0.39 | 0.94 | 0.33 |
| LSNS-6 | −0.05 | −0.07 | −0.02 | 16.17 | 0.00 * | −0.05 | −0.07 | −0.02 | 15.42 | 0.00 * |
| Age | - | - | - | - | - | −0.02 | −0.04 | 0.01 | 1.62 | 0.20 |
| Sex | - | - | - | - | - | - | - | - | - | - |
| Living arrangement | - | - | - | - | - | - | - | - | - | - |
| AIC | 365.41 | 365.77 | ||||||||
| BIC | 379.07 | 381.71 | ||||||||
| Model 2 | Model 3 | |||||||||
| B | 95% CI | Waldχ2 | p-Value | B | 95% CI | Waldχ2 | p-Value | |||
| ACS-JPN retention rate | ||||||||||
| IADL | −0.40 | −1.44 | 0.64 | 0.56 | 0.45 | −0.48 | −1.57 | 0.61 | 0.73 | 0.39 |
| L-Leisure | −1.60 | −2.56 | −0.64 | 10.57 | 0.00 * | −1.60 | −2.57 | −0.63 | 10.50 | 0.00 * |
| H-Leisure | −0.05 | −0.77 | 0.66 | 0.02 | 0.88 | −0.01 | −0.75 | 0.73 | 0.00 | 0.98 |
| Sociocultural activity | −0.40 | −1.20 | 0.39 | 1.00 | 0.32 | −0.41 | −1.20 | 0.38 | 1.02 | 0.31 |
| LSNS-6 | −0.05 | −0.07 | −0.02 | 14.34 | 0.00 * | −0.05 | −0.07 | −0.02 | 14.49 | 0.00 * |
| Age | −0.02 | −0.04 | 0.01 | 1.41 | 0.24 | −0.02 | −0.04 | 0.01 | 1.43 | 0.23 |
| Sex | 0.04 | −0.25 | 0.32 | 0.07 | 0.80 | 0.02 | −0.27 | 0.32 | 0.02 | 0.89 |
| Living arrangement | - | - | - | - | - | −0.08 | −0.43 | 0.26 | 0.22 | 0.64 |
| AIC | 367.71 | 369.49 | ||||||||
| BIC | 385.92 | 389.98 | ||||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tanikaga, M.; Uemura, J.-i.; Hori, F.; Hamada, T.; Tanaka, M. Changes in Community-Dwelling Elderly’s Activity and Participation Affecting Depression during COVID-19 Pandemic: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2023, 20, 4228. https://doi.org/10.3390/ijerph20054228
Tanikaga M, Uemura J-i, Hori F, Hamada T, Tanaka M. Changes in Community-Dwelling Elderly’s Activity and Participation Affecting Depression during COVID-19 Pandemic: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2023; 20(5):4228. https://doi.org/10.3390/ijerph20054228
Chicago/Turabian StyleTanikaga, Miki, Jun-ichi Uemura, Fumiko Hori, Tomomi Hamada, and Masahiro Tanaka. 2023. "Changes in Community-Dwelling Elderly’s Activity and Participation Affecting Depression during COVID-19 Pandemic: A Cross-Sectional Study" International Journal of Environmental Research and Public Health 20, no. 5: 4228. https://doi.org/10.3390/ijerph20054228





