Operationalising a Recovery-Oriented Support and Information Programme Online: The EOLAS Programme
Abstract
1. Introduction
1.1. The EOLAS Programmes
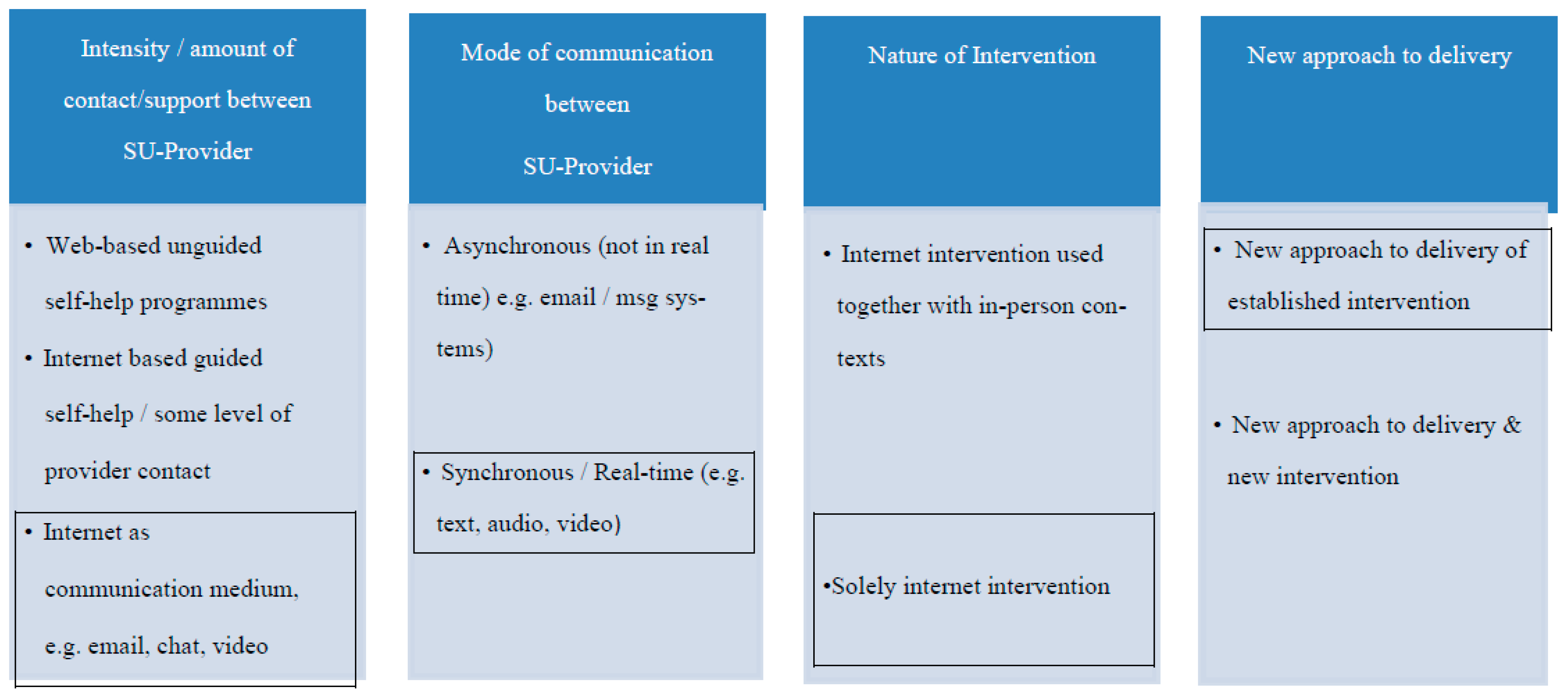
1.2. Virtual Interventions
2. Methods
2.1. Aim of the Study
2.2. Design
2.3. Data Collection Tools
2.4. Setting
2.5. Recruitment to the Evaluation
2.6. Data Analysis
2.7. Ethics
3. Results
3.1. Participant Profile
3.2. Impact of the Programme
“I made myself [goals]. For me it was… to get up early in the morning… Now obviously being off work and stuff I just fell into a rut, so it was just managing my time better in the morning. Getting up at seven and getting lunches prepared and stuff. And to get me back exercising. And since then, I have been [doing these]. Yeah, yeah, I feel like I’ve taken back a bit of control over myself.”(8003, SU)
“And just in general… talk…, be able to talk to somebody, a peer, about your condition which was very helpful, yeah. Well, it allowed me as the weeks went on to be more open about my own condition and how it affected me. And yeah, by the last couple of weeks I was talking clearly and able to share my stories.”(8004, SU)
“So, it was nice to be able to say that yeah people in all, like people in all walks of life have it [mental illness] and that we can still function and have a good job as well because of it.”(3001, SU)
“You learn how some people are coping, what challenges they have, how they are managing them and… you know, it gives you a bit of insight into what [services] is out there.”(4001, FM)
“While I was new to experiencing a family member suffering psychosis, I felt that the other participants’ family members had severe and long-term psychotic mental illness. From this I was left feeling isolated and a little hopeless at the prospect of recovery. But that did not mean I didn’t take good information from the sessions.”(FM, survey comments)
3.3. Use of Technology and Technology Support
“You wouldn’t be as into it [in comparison to in-person communication]. …there was just, ‘Am I talking or am I not talking or am I being heard, or can you see me?’ There was a bit of that going on.”(9001, FM)
“The challenges were mainly the people who didn’t show their face online. It was hard to interact with those people.”(8004, SU)
“No. I didn’t have an issue with it [non-camera use]. I don’t think anyone did really … for the people were still talking and sharing experiences. …there was no negative impact in any way….”(8002, SU)
3.4. Experiences of Attending EOLAS-Online
“Just when they said about recording, I hadn’t thought of it before. Only when [the co-facilitators] said it I kind of thought, ‘Oh yeah, people could record that now and put it somewhere else’, you know.”(3002, SU)
“I was just afraid I’d know someone on the course that would tell people [e.g., work colleagues] like that I’m bipolar. So, you know yeah, yeah it’s always kind of in the back of your mind.”(3001, SU)
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Higgins, A.; Kilkku, N.; Kristofersson, K.G. Perspectives and Frameworks Underpinning the Practice of Advanced Mental Health Nursing. In Advanced Practice in Mental Health Nursing: A European Perspective; Higgins, A., Kilkku, N., Kristofersson, K.G., Eds.; Springer: Berlin/Heidelberg, Germany, 2022. [Google Scholar]
- World Health Organization. Guidance on Community Mental Health Services: Promoting Person-Centred and Rights-Based Approaches. 2021. Available online: https://www.who.int/publications/i/item/9789240025707 (accessed on 15 December 2021).
- Beresford, P. From ‘Recovery’ to Reclaiming Madness. Clin. Psychol. Forum 2015, 268, 16–20. [Google Scholar] [CrossRef]
- Kaiser, B.N.; Varma, S.; Carpenter-Song, E.; Sareff, R.; Rai, S.; Kohrt, B.A. Eliciting recovery narratives in global mental health: Benefits and potential harms in service user participation. Psychiatr. Rehabil. J. 2020, 43, 111–120. [Google Scholar] [CrossRef] [PubMed]
- Clarke, M. Co-production in mental health care. Ment. Health Rev. J. 2015, 20, 213–219. [Google Scholar] [CrossRef]
- Gheduzzi, E.; Masella, C.; Segato, F. Implementing co-production in mental health organisations. J. Ment. Health Train. Educ. Pract. 2019, 14, 480–492. [Google Scholar] [CrossRef]
- Grim, K.; Tistad, M.; Schön, U.-K.; Rosenberg, D. The Legitimacy of User Knowledge in Decision-Making Processes in Mental health Care: An Analysis of Epistemic Injustice. J. Psychol. Rehabil. Ment. Health 2019, 6, 157–173. [Google Scholar] [CrossRef]
- Health Service Executive. Early Intervention in Psychosis Model of Care. 2019. Available online: https://www.hse.ie/eng/about/who/cspd/ncps/mental-health/psychosis/resources/hse-early-intervention-in-psychosis-model-of-care-june-2019.pdf (accessed on 16 September 2021).
- NICE, National Institute for Health and Care Excellence. Psychosis and Schizophrenia in Adults: Prevention and Management. 2014. Available online: https://www.nice.org.uk/guidance/cg178 (accessed on 14 September 2021).
- Druss, B.G.; Zhao, L.; von Esenwein, S.A.; Bona, J.R.; Fricks, L.; Jenkins-Tucker, S.; Sterling, E.; Diclemente, R.J.; Lorig, K. The Health and Recovery Peer (HARP) Program: A peer-led intervention to improve medical self-management for persons with serious mental illness. Schizophr. Res. 2010, 118, 264–270. [Google Scholar] [CrossRef]
- Pickett, S.A.; Diehl, S.; Steigman, P.J.; Prater, J.D.; Fox, A.; Cook, J.A. Early outcomes and lessons learned from a study of the Building Recovery of Individual Dreams and Goals through Education and Support (BRIDGES) program in Tennessee. Psychiatr. Rehabil. J. 2010, 34, 96–103. [Google Scholar] [CrossRef]
- Salcedo, S.; Gold, A.K.; Sheikh, S.; Marcus, P.H.; Nierenberg, A.A.; Deckersbach, T.; Sylvia, L.G. Empirically supported psychosocial interventions for bipolar disorder: Current state of the research. J. Affect. Disord. 2016, 201, 203–214. [Google Scholar] [CrossRef]
- Xia, J.; Merinder, L.B.; Belgamwar, M.R. Psychoeducation for schizophrenia. Cochrane Database Syst. Rev. 2011, 2011, CD002831. [Google Scholar] [CrossRef]
- Harvey, C. Family psychoeducation for people living with schizophrenia and their families. BJPsych Adv. 2018, 24, 9–19. [Google Scholar] [CrossRef]
- McFarlane, W.R. Family Interventions for Schizophrenia and the Psychoses: A Review. Fam. Process 2016, 55, 460–482. [Google Scholar] [CrossRef] [PubMed]
- Sin, J.; Gillard, S.; Spain, D.; Cornelius, V.; Chen, T.; Henderson, C. Effectiveness of psychoeducational interventions for family carers of people with psychosis: A systematic review and meta-analysis. Clin. Psychol. Rev. 2017, 56, 13–24. [Google Scholar] [CrossRef] [PubMed]
- Sin, J.; Norman, I. Psychoeducational interventions for family members of people with schizophrenia: A mixed-method systematic review. J. Clin. Psychiatry 2013, 74, e1145–e1162. [Google Scholar] [CrossRef] [PubMed]
- Jormfeldt, H.; Rask, M.; Brunt, D.; Bengtsson, A.; Svedberg, P. Experiences of a person-centred health education group intervention: A qualitative study among people with a persistant mental illness. Issues Ment. Health Nurs. 2010, 33, 209–216. [Google Scholar] [CrossRef] [PubMed]
- Lefley, H.P. A psychoeducation support group for serious mental illness. J. Spec. Group Work 2009, 34, 369–381. [Google Scholar] [CrossRef]
- Barry, J.; Monahan, C.; Ferguson, S.; Lee, K.; Kelly, R.; Monahan, M.; Murphy, R.; Ferguson, S.; Lee, K.; Bennett, A.; et al. “I came, I saw, I conquered”: Reflections on participating in a PhotoVoice project. J. Ment. Health Train. Educ. Pract. 2021, 16, 257–268. [Google Scholar] [CrossRef]
- Higgins, A.; Downes, C.; Monahan, M.; Hevey, D.; Boyd, F.; Cusack, N.; Gibbons, P. Evaluation of a co-facilitated information and learning programme for service users: The EOLAS programme. Ir. J. Psychol. Med. 2019, 37, 89–98. [Google Scholar] [CrossRef]
- Higgins, A.; Downes, C.; Monahan, M.; Hevey, D.; Boyd, F.; Cusack, N.; Gibbons, P. Family members’ perspectives on the acceptability and impact of a co-facilitated information programme: The EOLAS mental health programme. Ir. J. Psychol. Med. 2019, 39, 64–73. [Google Scholar] [CrossRef]
- Higgins, A.; Hevey, D.; Gibbons, P.; O’Connor, C.; Boyd, F.; McBennett, P.; Monaghan, M. Impact of co-facilitated information programmes on outcomes for service users and family members: The EOLAS programmes (paper 2). Ir. J. Psychol. Med. 2016, 34, 29–37. [Google Scholar] [CrossRef]
- Health Service Executive, Patient Safety First, Department of Health. eHealth Strategy for Ireland. 2013. Available online: https://assets.gov.ie/16174/092e7c62f97b472b83cdb6dfdcdfd5c7.pdf (accessed on 19 October 2021).
- Wozney, L.; Newton, A.S.; Gehring, N.D.; Bennett, K.; Huguet, A.; Hartling, L.; Dyson, M.P.; McGrath, P. Implementation of eMental Health care: Viewpoints from key informants from organizations and agencies with eHealth mandates. BMC Med. Inform. Decis. Mak. 2017, 17, 78. [Google Scholar] [CrossRef]
- Department of Health. Sharing the Vision. A Mental Health Policy for Everyone; The Stationary Office: Dublin, Ireland, 2020.
- Berger, T. The therapeutic alliance in internet interventions: A narrative review and suggestions for future research. Psychother. Res. 2017, 27, 511–524. [Google Scholar] [CrossRef] [PubMed]
- Poole, R.; Simpson, S.A.; Smith, D.J. Internet-based psychoeducation for bipolar disorder: A qualitative analysis of feasibility, acceptability and impact. BMC Psychiatry 2012, 12, 139. [Google Scholar] [CrossRef] [PubMed]
- Proudfoot, J.; Parker, G.; Manicavasagar, V.; Hadzi-Pavlovic, D.; Whitton, A.; Nicholas, J.; Smith, M.; Burckhardt, R. Effects of adjunctive peer support on perceptions of illness control and understanding in an online psychoeducation program for bipolar disorder: A randomised controlled trial. J. Affect. Disord. 2012, 142, 98–105. [Google Scholar] [CrossRef] [PubMed]
- Todd, N.J.; Jones, S.H.; Hart, A.; Lobban, F.A. A web-based self-management intervention for Bipolar Disorder ‘living with bipolar’: A feasibility randomised controlled trial. J. Affect. Disord. 2014, 169, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Glynn, S.M.; Randolph, E.T.; Garrick, T.; Lui, A. A proof of concept trial of an online psychoeducational program for relatives of both veterans and civilians living with schizophrenia. Psychiatr. Rehabil. J. 2010, 33, 278–287. [Google Scholar] [CrossRef]
- Kaplan, K.; Solomon, P.; Salzer, M.S.; Brusilovskiy, E. Assessing an Internet-based parenting intervention for mothers with a serious mental illness: A randomized controlled trial. Psychiatr. Rehabil. J. 2014, 37, 222–231. [Google Scholar] [CrossRef] [PubMed]
- Rotondi, A.J.; Anderson, C.M.; Haas, G.L.; Eack, S.M.; Spring, M.B.; Ganguli, R.; Newhill, C.; Rosenstock, J. Web-Based Psychoeducation Intervention for Persons with Schizophrenia and Their Supporters: One-Year Outcomes. Psychiatr. Serv. 2010, 61, 1099–1105. [Google Scholar] [CrossRef]
- Rotondi, A.J.; Haas, G.L.; Anderson, C.M.; Newhill, C.E.; Spring, M.B.; Ganguli, R.; Gardner, W.B.; Rosenstock, J.B. A Clinical Trial to Test the Feasibility of a Telehealth Psychoeducational Intervention for Persons with Schizophrenia and Their Families: Intervention and 3-Month Findings. Rehabil. Psychol. 2005, 50, 325–336. [Google Scholar] [CrossRef]
- Alvarez-Jimenez, M.; Bendall, S.; Lederman, R.; Wadley, G.; Chinnery, G.; Vargas, S.; Larkin, M.; Killackey, E.; Gorry, P.D.; Gleeson, J.F. On the HORYZON: Moderated online social therapy for long-term recovery in first episode psychosis. Schizophr. Res. 2013, 143, 143–149. [Google Scholar] [CrossRef]
- Ben-Zeev, D.; Brian, R.M.; Jonathan, G.; Razzano, L.; Pashka, N.; Carpenter-Song, E.; Drake, R.E.; Scherer, E.A. Mobile Health (mHealth) Versus Clinic-Based Group Intervention for People with Serious Mental Illness: A Randomized Controlled Trial. Psychiatr. Serv. 2018, 69, 978–985. [Google Scholar] [CrossRef]
- Batchelor, R.; Gulshan, S.; Shritharan, H.; Williams, E.; Henderson, C.; Gillard, S.; Woodham, L.A.; Cornelius, V.; Elkes, J.; Sin, J. Perceived Acceptability and Experiences of a Digital Psychoeducation and Peer Support Intervention (COPe-support): Interview Study with Carers Supporting Individuals with Psychosis. J. Med. Internet Res. 2022, 24, e27781. [Google Scholar] [CrossRef] [PubMed]
- Chan, S.K.; Tse, S.; Sit, H.L.; Hui, C.L.; Lee, E.H.; Chang, W.C.; Chen, E.Y. Web-Based Psychoeducation Program for Caregivers of First-Episode of Psychosis: An Experience of Chinese Population in Hong Kong. Front. Psychol. 2016, 7, 2006. [Google Scholar] [CrossRef] [PubMed]
- Sin, J.; Woodham, L.A.; Henderson, C.; Williams, E.; Sese Hernandez, A.; Gillard, S. Usability evaluation of an eHealth intervention for family carers of individuals affected by psychosis: A mixed-method study. Digit. Health 2019, 5, 2055207619871148. [Google Scholar] [CrossRef] [PubMed]
- Sin, J.; Henderson, C.; Norman, I. Usability of online psychoeducation for siblings of people with psychosis. Int. J. Technol. Assess. Health Care 2014, 30, 374–380. [Google Scholar] [CrossRef]
- Simon, G.E. An Online Recovery Plan Program: Can Peer Coaching Increase Participation? Psychiatr. Serv. 2011, 62, 666–669. [Google Scholar] [CrossRef]
- Carpenter-Song, E.; Jonathan, G.; Brian, R.; Ben-Zeev, D. Perspectives on Mobile Health Versus Clinic-Based Group Interventions for People with Serious Mental Illnesses: A Qualitative Study. Psychiatr. Serv. 2020, 71, 49–56. [Google Scholar] [CrossRef]
- Smith, D.J.; Griffiths, E.; Poole, R.; di Florio, A.; Barnes, E.; Kelly, M.J.; Craddock, N.; Hood, K.; Simpson, S. Beating Bipolar: Exploratory trial of a novel Internet-based psychoeducational treatment for bipolar disorder. Bipolar Disord. 2011, 13, 571–577. [Google Scholar] [CrossRef]
- Alvarez-Jimenez, M.; Alcazar-Corcoles, M.A.; Gonzalez-Blanch, C.; Bendall, S.; McGorry, P.D.; Gleeson, J.F. Online, social media and mobile technologies for psychosis treatment: A systematic review on novel user-led interventions. Schizophr. Res. 2014, 156, 96–106. [Google Scholar] [CrossRef]
- Gaebel, W.; Grossimlinghaus, I.; Kerst, A.; Cohen, Y.; Hinsche-Bockenholt, A.; Johnson, B.; Mucic, D.; Petrea, I.; Rossler, W.; Thornicroft, G.; et al. European Psychiatric Association (EPA) guidance on the quality of eMental health interventions in the treatment of psychotic disorders. Eur. Arch. Psychiatry Clin. Neurosci. 2016, 266, 125–137. [Google Scholar] [CrossRef]
- Naslund, J.A.; Marsch, L.A.; McHugo, G.J.; Bartels, S.J. Emerging mHealth and eHealth interventions for serious mental illness: A review of the literature. J. Ment. Health 2015, 24, 321–332. [Google Scholar] [CrossRef]
- Barbeito, S.; Sanchez-Gutierrez, T.; Becerra-Garcia, J.A.; Gonzalez Pinto, A.; Caletti, E.; Calvo, A. A systematic review of online interventions for families of patients with severe mental disorders. J. Affect. Disord. 2020, 263, 147–154. [Google Scholar] [CrossRef] [PubMed]
- Onwumere, J.; Amaral, F.; Valmaggia, L.R. Digital Technology for Caregivers of People with Psychosis: Systematic Review. JMIR Ment. Health 2018, 5, e55. [Google Scholar] [CrossRef] [PubMed]
- Santesteban-Echarri, O.; Piskulic, D.; Nyman, R.K.; Addington, J. Telehealth interventions for schizophrenia-spectrum disorders and clinical high-risk for psychosis individuals: A scoping review. J. Telemed. Telecare 2018, 26, 14–20. [Google Scholar] [CrossRef] [PubMed]
- Sharp, R.; Kobak, K.A.; Osman, D.A. The use of videoconferencing with patients with psychosis: A review of the literature. Ann. Gen. Psychiatry 2011, 10, 14. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Reflecting on reflexive thematic analysis. Qual. Res. Sport Exerc. Health 2019, 11, 589–597. [Google Scholar] [CrossRef]
- Leamy, M.; Bird, V.; Le Boutillier, C.; Williams, J.; Slade, M. Conceptual framework for personal recovery in mental health: Systematic review and narrative synthesis. Br. J. Psychiatry 2011, 199, 445–452. [Google Scholar] [CrossRef]
- Strand, M.; Eng, L.S.; Gammon, D. Combining online and offline peer support groups in community mental health care settings: A qualitative study of service users’ experiences. Int. J. Ment. Health Syst. 2020, 14, 39. [Google Scholar] [CrossRef]
- Bond, K.; Anderson, I.M. Psychoeducation for relapse prevention in bipolar disorder: A systematic review of efficacy in randomised controlled trials. Bipolar Disord. 2015, 17, 349–362. [Google Scholar] [CrossRef]
- Eassom, E.; Giacco, D.; Dirik, A.; Priebe, S. Implementing family involvement in the treatment of patients with psychosis: A systematic review of facilitating and hindering factors. BMJ Open 2014, 4, e006108. [Google Scholar] [CrossRef]
- Department of the Environment, Climate and Communications. National Broadband Plan. 2020. Available online: https://www.gov.ie/en/publication/c1b0c9-national-broadband-plan/#national-broadband-ireland-nbi (accessed on 8 March 2022).
- McMorrow, C. Broadband Plan Connections to Be Available in 13 Countries by End of Year, but Just 3300 Made So Far. RTE.ie News. 2021. Available online: https://www.rte.ie/news/primetime/2021/1202/1264507-national-broadband-plan-slow-rollout/ (accessed on 24 March 2022).
- Russell, C. These Are the Areas in Ireland with the Slowest and Fastest Broadband Speeds. thejournal.ie. 2016. Available online: https://www.thejournal.ie/broadband-speeds-ireland-3082026-Nov2016/ (accessed on 24 March 2022).
- Watson, A.; Mellotte, H.; Hardy, A.; Peters, E.; Keen, N.; Kane, F. The digital divide: Factors impacting on uptake of remote therapy in a South London psychological therapy service for people with psychosis. J. Ment. Health 2021, 31, 825–832. [Google Scholar] [CrossRef]
- Berry, N.; Lobban, F.; Bucci, S. A qualitative exploration of service user views about using digital health interventions for self-management in severe mental health problems. BMC Psychiatry 2019, 19, 35. [Google Scholar] [CrossRef] [PubMed]
| Survey Participants (n = 15) | Interview Participants (n = 8) | |
|---|---|---|
| Role | n, (%) | n, (%) |
| Service user | 8 (53.3%) | 6 (75%) |
| Family/Supporter | 5 (33.3%) | 2 (25%) |
| Both | 1 (6.6%) | - |
| Missing | 1 (6.6%) | - |
| Gender | ||
| Female | 10 (66.6%) | 6 (75%) |
| Male | 4 (26.6%) | 2 (25%) |
| Missing | 1 (6.7%) | - |
| (a) Motivations for Attending EOLAS-OL * | n | % |
| Learn more about coping strategies | 15 | 100% |
| Meet other people with similar experiences | 15 | 100% |
| Increase my knowledge of mental health | 14 | 93.3% |
| Share experiences to help others | 12 | 80% |
| Learn more about self-care | 10 | 66.7% |
| Get support for my mental health | 10 | 66.7% |
| The online programme was more convenient as did not have to travel so saved time | 10 | 66.7% |
| Increase my social network | 6 | 40% |
| (b) Reasons for Missing Sessions * | No | Yes |
| Time conflicted with other things | 1 | 8 |
| Session was not relevant to my needs | 9 | 0 |
| Didn’t feel my voice was being heard | 9 | 0 |
| Found other people’s stories too upsetting | 9 | 0 |
| Found the technology too difficult to navigate | 9 | 0 |
| Internet connection was poor | 9 | 0 |
| I had concerns about the privacy and confidentiality of the online forum | 9 | 0 |
| I didn’t have access to a private computer at the time the session was on | 9 | 0 |
| (a) Impact (n = 15) | ||
| Please rate your level of agreement with the following statements about the impact of EOLAS? (n = 15) | Mean | Std. Deviation |
| EOLAS increased my knowledge of mental health | 4.60 | 1.06 |
| I know more about where to get support for my mental health | 4.47 | 1.06 |
| It was beneficial to share experiences to help others | 4.27 | 1.16 |
| I learnt more about coping strategies | 4.40 | 1.12 |
| It was good to meet other people with similar experiences | 4.47 | 1.13 |
| I learnt more about self-care | 4.20 | 1.15 |
| I have increased my social network | 3.40 | 1.18 |
| (b) Overall Measures | ||
| Usefulness (n = 15) | 4.47 | 0.74 |
| Satisfaction (n = 15) | 4.20 | 1.2 |
| (a) Please Rate Your Level of Agreement with the Following Statements about Using Technology to Do EOLAS Online? (n = 15) | Mean | Std. Deviation | (b) Please Rate Your Level of Agreement with the Following Statements about Your Experience of Doing EOLAS Online? (n = 15) | Mean | Std. Deviation |
|---|---|---|---|---|---|
| I had confidence in the safety of the platform being used | 4.67 | 1.05 | I was comfortable speaking online | 4.47 | 1.13 |
| I found the technology easy to use | 4.60 | 1.10 | The handbook complemented the session content | 4.40 | 1.12 |
| I found it easy to join the session | 4.60 | 1.06 | I always had access to a private space/room | 4.40 | 1.30 |
| I have a good/stable internet connection where I live | 4.40 | 1.12 | The facilitator provided sufficient encouragement/opportunity for me to engage | 4.40 | 1.40 |
| My computer enabled me to fully engage in the session | 4.27 | 1.16 | The content of the material met my needs | 4.27 | 1.39 |
| I was able to share my video | 4.13 | 1.25 | I was comfortable sharing my video feed | 4.00 | 1.51 |
| I found it difficult to hear what people were saying | 2.07 | 1.28 | I found the online platform was not conducive to sharing personal experiences | 1.87 | 1.30 |
| I found it difficult to see people and read their nonverbal cues | 2.27 | 1.28 | I don’t trust online platforms | 1.20 | 0.41 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
O’Sullivan, K.; Downes, C.; Monahan, M.; Morrissey, J.; Byrne, G.; Farrell, G.; Gibbons, P.; Higgins, A. Operationalising a Recovery-Oriented Support and Information Programme Online: The EOLAS Programme. Int. J. Environ. Res. Public Health 2023, 20, 4417. https://doi.org/10.3390/ijerph20054417
O’Sullivan K, Downes C, Monahan M, Morrissey J, Byrne G, Farrell G, Gibbons P, Higgins A. Operationalising a Recovery-Oriented Support and Information Programme Online: The EOLAS Programme. International Journal of Environmental Research and Public Health. 2023; 20(5):4417. https://doi.org/10.3390/ijerph20054417
Chicago/Turabian StyleO’Sullivan, Karin, Carmel Downes, Mark Monahan, Jean Morrissey, Gobnait Byrne, Gerard Farrell, Patrick Gibbons, and Agnes Higgins. 2023. "Operationalising a Recovery-Oriented Support and Information Programme Online: The EOLAS Programme" International Journal of Environmental Research and Public Health 20, no. 5: 4417. https://doi.org/10.3390/ijerph20054417
APA StyleO’Sullivan, K., Downes, C., Monahan, M., Morrissey, J., Byrne, G., Farrell, G., Gibbons, P., & Higgins, A. (2023). Operationalising a Recovery-Oriented Support and Information Programme Online: The EOLAS Programme. International Journal of Environmental Research and Public Health, 20(5), 4417. https://doi.org/10.3390/ijerph20054417







