A National Portrait of Public Attitudes toward Opioid Use in the US: A Latent Class Analysis
Abstract
:1. Introduction
2. Theoretical Framework: Stigma
Structural Stigma: How Policies Reflect Societal Stigmas and How They Can Negatively Affect Individual Health Outcomes
3. Methods
3.1. Study Sample
3.2. Measures: Latent Class Indicators Measuring Public Attitudes toward Opioid Use Disorder
3.3. Covariates
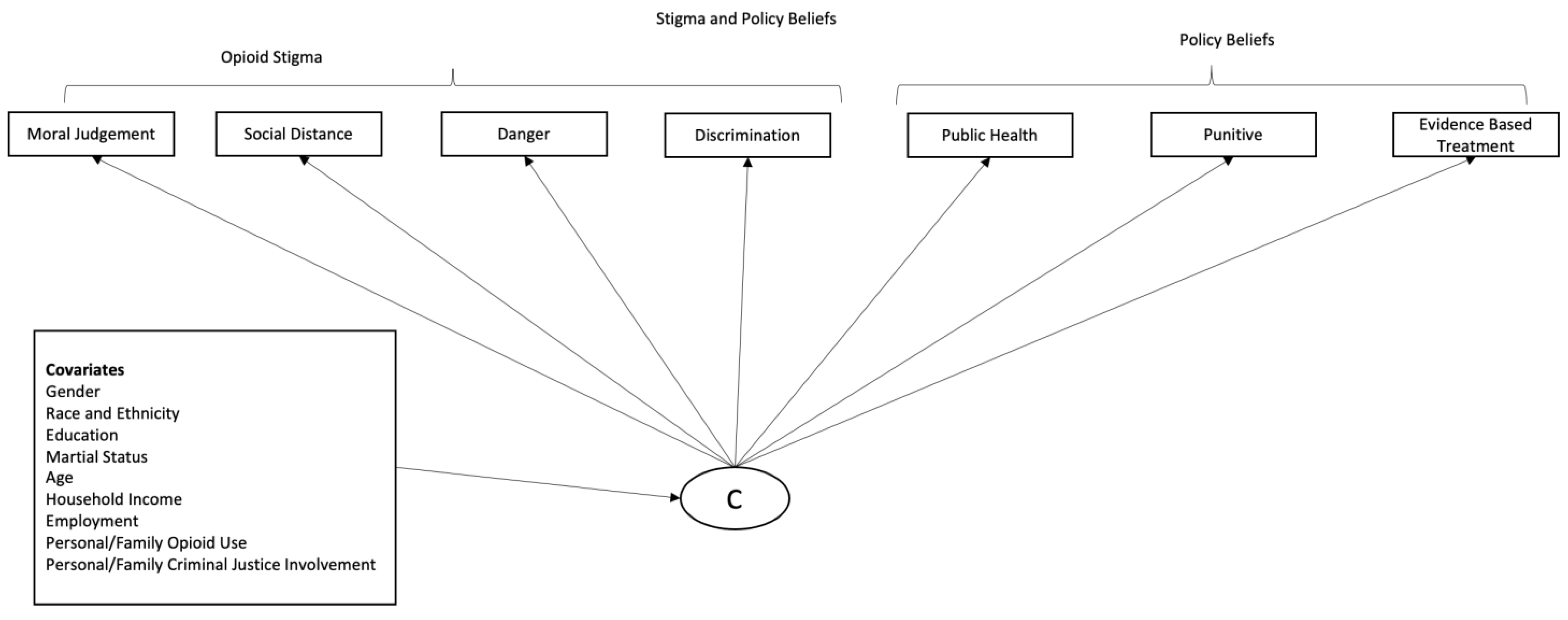
3.4. Analytical Model
4. Results
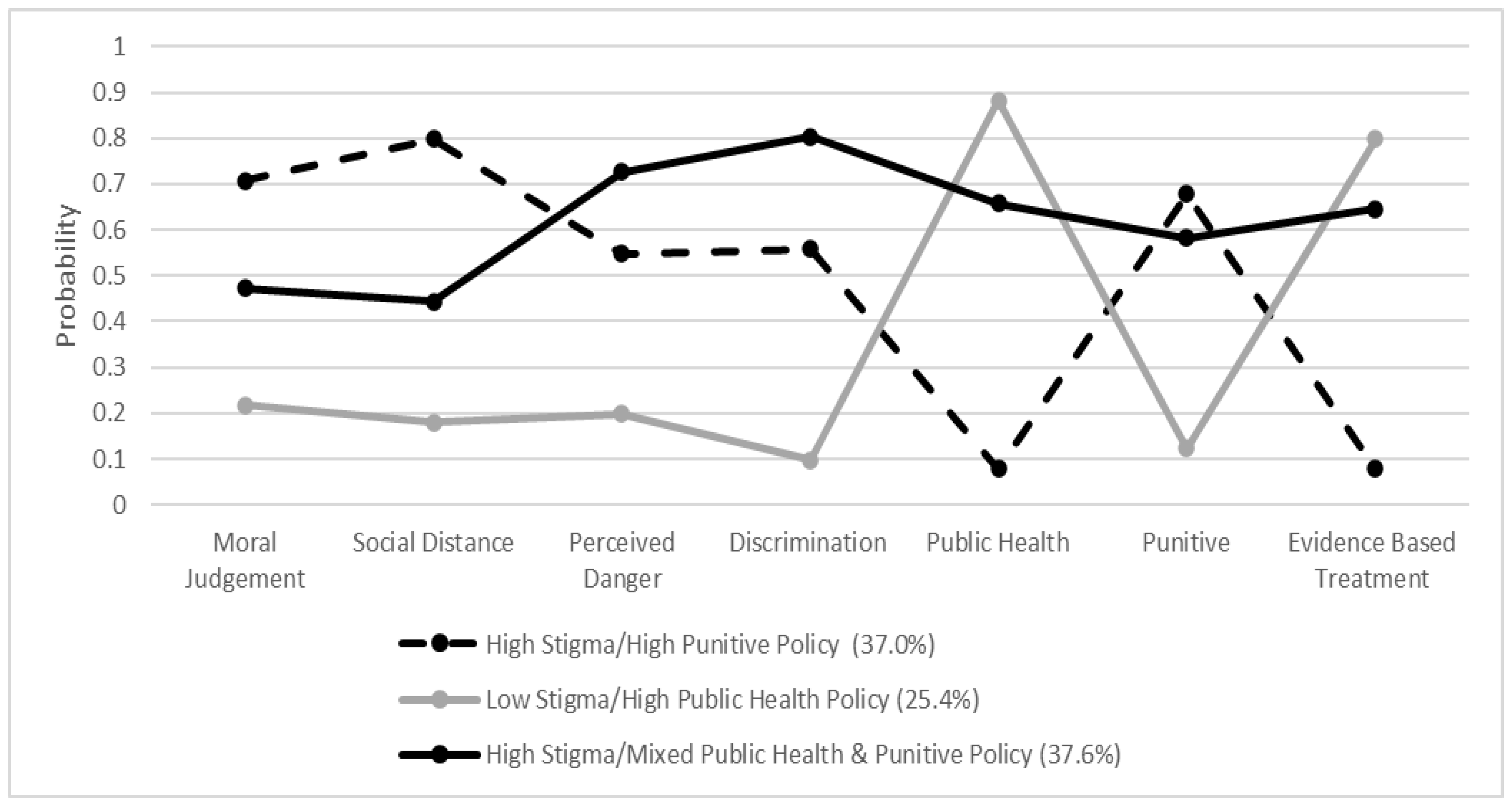
4.1. Latent Classes of Opioid Stigma and Policy Beliefs
4.2. Associations between Individual Characteristics and Class Membership
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Centers for Disease Control and Prevention. Vital signs: Overdoses of prescription opioid pain relievers—United States, 1999–2008. MMWR Morb. Mortal. Wkly. Rep. 2011, 60, 1487–1492. [Google Scholar]
- Rudd, R.A.; Seth, P.; David, F.; Scholl, L. Increases in drug and opioid-involved overdose deaths—United States, 2010–2015. Morb. Mortal. Wkly. Rep. 2016, 65, 1445–1452. [Google Scholar] [CrossRef] [Green Version]
- O’Donnell, J.K.; Gladden, R.M.; Seth, P. Trends in Deaths Involving Heroin and Synthetic Opioids Excluding Methadone, and Law Enforcement Drug Product Reports, by Census Region—United States, 2006–2015. MMWR Morb. Mortal. Wkly. Rep. 2017, 66, 897–903. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ciccarone, D. The rise of illicit fentanyls, stimulants and the fourth wave of the opioid overdose crisis. Curr. Opin. Psychiatry 2021, 34, 344. [Google Scholar] [CrossRef] [PubMed]
- New York City Department of Health and Mental Hygeine. Consistent With Nationwide Trends, Overdose Deaths Rise in New York City in First Quarter of 2020; New York City Department of Health and Mental Hygiene: New York, NY, USA, 2020.
- Stephenson, J. Drug Overdose Deaths Head Toward Record Number in 2020, CDC Warns. JAMA Health Forum 2020, 1, e201318. [Google Scholar]
- Lundgren, L.M.; Curtis, M.A.; Oettinger, C. Postincarceration Policies for those with Criminal Drug Convictions: A National Policy Review. Fam. Soc. J. Contemp. Soc. Serv. 2010, 91, 31–38. [Google Scholar] [CrossRef]
- Tsai, A.C.; Kiang, M.V.; Barnett, M.L.; Beletsky, L.; Keyes, K.M.; McGinty, E.E.; Smith, L.R.; Strathdee, S.A.; Wakeman, S.E.; Venkataramani, A.S. Stigma as a fundamental hindrance to the United States opioid overdose crisis response. PLoS Med. 2019, 16, e1002969. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Walters, S.M.; Frank, D.; Van Ham, B.; Jaiswal, J.; Muncan, B.; Earnshaw, V.; Schneider, J.; Friedman, S.R.; Ompad, D.C. PrEP Care Continuum Engagement Among Persons Who Inject Drugs: Rural and Urban Differences in Stigma and Social Infrastructure. AIDS Behav. 2021, 26, 1308–1320. [Google Scholar] [CrossRef] [PubMed]
- Walters, S.M.; Kral, A.H.; Lamb, S.; Goldshear, J.L.; Wenger, L.; Bluthenthal, R.N. Correlates of Transactional Sex and Violent Victimization among Men Who Inject Drugs in Los Angeles and San Francisco, California. J. Urban Health 2021, 98, 70–82. [Google Scholar] [CrossRef]
- Western, B. Punishment and Inequality in America; Russell Sage Foundation: New York, NY, USA, 2006. [Google Scholar]
- Alexander, M. The New Jim Crow: Mass Incarceration in the Age of Colorblindness; The New Press: New York, NY, USA, 2020. [Google Scholar]
- Kerr, J.; Jackson, T. Stigma, sexual risks, and the war on drugs: Examining drug policy and HIV/AIDS inequities among African Americans using the Drug War HIV/AIDS Inequities Model. Int. J. Drug Policy 2016, 37, 31–41. [Google Scholar] [CrossRef] [PubMed]
- Massoglia, M.; Pridemore, W.A. Incarceration and health. Annu. Rev. Sociol. 2015, 41, 291–310. [Google Scholar] [CrossRef] [PubMed]
- Weidner, R.R.; Schultz, J. Examining the relationship between U.S. incarceration rates and population health at the county level. SSM Popul. Health 2019, 9, 100466. [Google Scholar] [CrossRef] [PubMed]
- Mital, S.; Wolff, J.; Carroll, J.J. The relationship between incarceration history and overdose in North America: A scoping review of the evidence. Drug Alcohol Depend. 2020, 213, 108088. [Google Scholar] [CrossRef] [PubMed]
- Walters, S.M.; Frank, D.; Felsher, M.; Jaiswal, J.; Fletcher, S.; Bennett, A.S.; Friedman, S.R.; Ouellet, L.J.; Ompad, D.C.; Jenkins, W. How the rural risk environment underpins hepatitis C risk: Qualitative findings from rural southern Illinois, United States. Int. J. Drug Policy 2023, 112, 103930. [Google Scholar] [CrossRef] [PubMed]
- Walters, S.M.; Bolinski, R.S.; Almirol, E.; Grundy, S.; Fletcher, S.; Schneider, J.; Friedman, S.R.; Ouellet, L.J.; Ompad, D.C.; Jenkins, W.; et al. Structural and community changes during COVID-19 and their effects on overdose precursors among rural people who use drugs: A mixed-methods analysis. Addict. Sci. Clin. Pract. 2022, 17, 24. [Google Scholar] [CrossRef] [PubMed]
- Sordo, L.; Barrio, G.; Bravo, M.J.; Indave, B.I.; Degenhardt, L.; Wiessing, L.; Ferri, M.; Pastor-Barriuso, R. Mortality risk during and after opioid substitution treatment: Systematic review and meta-analysis of cohort studies. BMJ 2017, 357, j1550. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Albers, E. Harm reduction: Contribution to a critical appraisal from the perspective of people who use drugs. In Harm Reduction in Substance Use and High Risk Behaviour: International Policy and Practice; Wiley Blackwell: Hoboken, NJ, USA, 2012; pp. 124–131. Available online: https://www.researchgate.net/publication/265580861 (accessed on 5 January 2023).
- National Harm Reduction Coalition. Principles of Harm Reduction; National Harm Reduction Coalition: New York, NY, USA, 2020. [Google Scholar]
- Friedman, S.R.; de Jong, W.; Rossi, D.; Touzé, G.; Rockwell, R.; Des Jarlais, D.C.; Elovich, R. Harm reduction theory: Users’ culture, micro-social indigenous harm reduction, and the self-organization and outside-organizing of users’ groups. Int. J. Drug Policy 2007, 18, 107–117. [Google Scholar] [CrossRef] [Green Version]
- Harris, M.; Rhodes, T. Methadone diversion as a protective strategy: The harm reduction potential of ‘generous constraints’. Int. J. Drug Policy 2013, 24, e43–e50. [Google Scholar] [CrossRef]
- Langendam, M.W.; van Brussel, G.H.; Coutinho, R.A.; Van Ameijden, E. The impact of harm-reduction-based methadone treatment on mortality among heroin users. Am. J. Public Health 2001, 91, 774. [Google Scholar]
- Marlatt, G.A. Harm reduction: Come as you are. Addict. Behav. 1996, 21, 779–788. [Google Scholar] [CrossRef]
- Parkin, S.; Neale, J.; Brown, C.; Campbell, A.N.; Castillo, F.; Jones, J.D.; Strang, J.; Comer, S.D. Opioid overdose reversals using naloxone in New York City by people who use opioids: Implications for public health and overdose harm reduction approaches from a qualitative study. Int. J. Drug Policy 2020, 79, 102751. [Google Scholar] [CrossRef]
- Vakharia, S.P.; Little, J. Starting where the client is: Harm reduction guidelines for clinical social work practice. Clin. Soc. Work J. 2017, 45, 65–76. [Google Scholar] [CrossRef]
- Kravitz-Wirtz, N.; Davis, C.S.; Ponicki, W.R.; Rivera-Aguirre, A.; Marshall, B.D.L.; Martins, S.S.; Cerdá, M. Association of Medicaid Expansion With Opioid Overdose Mortality in the United States. JAMA Netw. Open 2020, 3, e1919066. [Google Scholar] [CrossRef] [PubMed]
- Meinhofer, A.; Witman, A.E. The role of health insurance on treatment for opioid use disorders: Evidence from the Affordable Care Act Medicaid expansion. J. Health Econ. 2018, 60, 177–197. [Google Scholar] [CrossRef] [PubMed]
- Malta, M.; Varatharajan, T.; Russell, C.; Pang, M.; Bonato, S.; Fischer, B. Opioid-related treatment, interventions, and outcomes among incarcerated persons: A systematic review. PLoS Med. 2019, 16, e1003002. [Google Scholar] [CrossRef] [Green Version]
- Smart, R.; Pardo, B.; Davis, C.S. Systematic review of the emerging literature on the effectiveness of naloxone access laws in the United States. Addiction 2021, 116, 6–17. [Google Scholar] [CrossRef] [PubMed]
- Goffman, E. Stigma: Notes on the Management of Spoiled Identity; Simon and Schuster: New York, NY, USA, 2009. [Google Scholar]
- Link, B.G.; Phelan, J.C. Conceptualizing stigma. Annu. Rev. Sociol. 2001, 27, 363–385. [Google Scholar] [CrossRef]
- Pescosolido, B.A.; Martin, J.K. The stigma complex. Annu. Rev. Sociol. 2015, 41, 87–116. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hatzenbuehler, M.L.; Link, B.G. Introduction to the special issue on structural stigma and health. Soc. Sci. Med. 2014, 103, 1–6. [Google Scholar] [CrossRef]
- Hatzenbuehler, M.L. Structural stigma: Research evidence and implications for psychological science. Am. Psychol. 2016, 71, 742. [Google Scholar] [CrossRef]
- Hatzenbuehler, M.L. The influence of state laws on the mental health of sexual minority youth. JAMA Pediatr. 2017, 171, 322–324. [Google Scholar] [CrossRef] [PubMed]
- Corrigan, P.W.; Markowitz, F.E.; Watson, A.C. Structural Levels of Mental Illness Stigma and Discrimination. Schizophr. Bull. 2004, 30, 481–491. [Google Scholar] [CrossRef] [Green Version]
- Corrigan, P.W.; Watson, A.C.; Heyrman, M.L.; Warpinski, A.; Gracia, G.; Slopen, N.; Hall, L.L. Structural Stigma in State Legislation. Psychiatr. Serv. 2005, 56, 557–563. [Google Scholar] [CrossRef] [Green Version]
- Hoppe, T. Punishing Disease: HIV and the Criminalization of Sickness; University of California Press: Oakland, CA, USA, 2017. [Google Scholar]
- Paterson, B.; Hirsch, G.; Andres, K. Structural factors that promote stigmatization of drug users with hepatitis C in hospital emergency departments. Int. J. Drug Policy 2013, 24, 471–478. [Google Scholar] [CrossRef]
- Musto, D.F. The American Disease: Origins of Narcotic Control (Expanded Edition); Oxford University Press: Oxford, NY, USA, 1987. [Google Scholar]
- Kennedy-Hendricks, A.; Barry, C.L.; Gollust, S.E.; Ensminger, M.E.; Chisolm, M.S.; McGinty, E.E. Social stigma toward persons with prescription opioid use disorder: Associations with public support for punitive and public health–oriented policies. Psychiatr. Serv. 2017, 68, 462–469. [Google Scholar] [CrossRef] [Green Version]
- Burstein, P. The impact of public opinion on public policy: A review and an agenda. Political Res. Q. 2003, 56, 29–40. [Google Scholar] [CrossRef]
- Ledford, V.; Lim, J.R.; Namkoong, K.; Chen, J.; Qin, Y. The Influence of Stigmatizing Messages on Danger Appraisal: Examining the Model of Stigma Communication for Opioid-Related Stigma, Policy Support, and Related Outcomes. Health Commun. 2021, 37, 1765–1777. [Google Scholar] [CrossRef]
- Adams, Z.W.; Taylor, B.G.; Flanagan, E.; Kwon, E.; Johnson-Kwochka, A.V.; Elkington, K.S.; Becan, J.E.; Aalsma, M.C. Opioid use disorder stigma, discrimination, and policy attitudes in a national sample of US young adults. J. Adolesc. Health 2021, 69, 321–328. [Google Scholar] [CrossRef] [PubMed]
- Sylvester, S.M.; Haeder, S.F.; Callaghan, T. Just say no? Public attitudes about supportive and punitive policies to combat the opioid epidemic. J. Public Policy 2022, 42, 270–297. [Google Scholar] [CrossRef]
- Taylor, B.G.; Lamuda, P.A.; Flanagan, E.; Watts, E.; Pollack, H.; Schneider, J. Social Stigma toward Persons with Opioid Use Disorder: Results from a Nationally Representative Survey of US Adults. Subst. Use Misuse 2021, 56, 1752–1764. [Google Scholar] [CrossRef] [PubMed]
- Dennis, J. Technical Overview of the AmeriSpeak Panel NORC’s Probability-Based Household Panel; NORC at the University of Chicago: Chicago, IL, USA, 2019. [Google Scholar]
- Fontes, A.; Chew, K.; Layrakas, P. Boosting probability-based web survey response rates via nonresponse follow-up. In Proceedings of the Conference of the American Association of Public Opinion Research, Hollywood, FL, USA, 14–17 May 2015. [Google Scholar]
- Dennis, J.M. AmeriSpeak Omnibus Field Report; NORC at the University of Chicago: Chicago, IL, USA, 2019. [Google Scholar]
- Barry, C.L.; McGinty, E.E.; Pescosolido, B.A.; Goldman, H.H. Stigma, discrimination, treatment effectiveness, and policy: Public views about drug addiction and mental illness. Psychiatr. Serv. 2014, 65, 1269–1272. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, L.H.; Grivel, M.M.; Anderson, B.; Bailey, G.L.; Opler, M.; Wong, L.Y.; Stein, M.D. A new brief opioid stigma scale to assess perceived public attitudes and internalized stigma: Evidence for construct validity. J. Subst. Abus. Treat. 2019, 99, 44–51. [Google Scholar] [CrossRef] [PubMed]
- National Institute on Drug Abuse. Opioid Factor for Teens Some Things to Think about. 2018. Available online: https://www.drugabuse.gov/publications/opioid-facts-teens/some-things-to-think-about (accessed on 5 January 2023).
- Mumford, E.A.; Liu, W.; Taylor, B.G. Youth and young adult dating relationship dynamics and subsequent abusive outcomes. J. Adolesc. 2019, 72, 112–123. [Google Scholar] [CrossRef] [PubMed]
- Mumford, E.A.; Liu, W.; Taylor, B.G. Parenting profiles and adolescent dating relationship abuse: Attitudes and experiences. J. Youth Adolesc. 2016, 45, 959–972. [Google Scholar] [CrossRef] [PubMed]
- Muthén, B.O. Latent variable mixture modeling. In New Developments and Techniques in Structural Equation Modeling; Psychology Press: London, UK, 2001; pp. 21–54. [Google Scholar]
- Ferguson, S.L.; Moore, E.W.G.; Hull, D.M. Finding latent groups in observed data: A primer on latent profile analysis in Mplus for applied researchers. Int. J. Behav. Dev. 2019, 44, 458–468. [Google Scholar] [CrossRef]
- Nylund, K.L.; Asparouhov, T.; Muthén, B.O. Deciding on the Number of Classes in Latent Class Analysis and Growth Mixture Modeling: A Monte Carlo Simulation Study. Struct. Equ. Model. A Multidiscip. J. 2007, 14, 535–569. [Google Scholar] [CrossRef]
- Lo, Y.; Mendell, N.R.; Rubin, D.B. Testing the number of components in a normal mixture. Biometrika 2001, 88, 767–778. [Google Scholar] [CrossRef]
- Ramaswamy, V.; Desarbo, W.S.; Reibstein, D.J.; Robinson, W.T. An empirical pooling approach for estimating marketing mix elasticities with PIMS data. Mark. Sci. 1993, 12, 103–124. [Google Scholar] [CrossRef]
- Asparouhov, T.; Muthén, B. Auxiliary variables in mixture modeling: Three-step approaches using M plus. Struct. Equ. Model. Multidiscip. J. 2014, 21, 329–341. [Google Scholar] [CrossRef]
- Vermunt, J.K. Latent class modeling with covariates: Two improved three-step approaches. Political Anal. 2010, 18, 450–469. [Google Scholar] [CrossRef] [Green Version]
- Arbuckle, J.L. Full information estimation in the presence of incomplete data. In Advanced Structural Equation Modeling; Marcoulides, G.A., Schumacker, R.E., Eds.; Lawrence Erlbaum Associates, Inc.: Mahwah, NJ, USA, 1996; pp. 243–277. [Google Scholar]
- Schafer, J.L.; Graham, J.W. Missing data: Our view of the state of the art. Psychol. Methods 2002, 7, 147–177. [Google Scholar] [CrossRef]
- Muthén, B.; Asparouhov, T. Latent variable analysis with categorical outcomes: Multiple-group and growth modeling in Mplus. Mplus Web Notes 2002, 4, 1–22. [Google Scholar]
- Dyregrov, K.; Selseng, L.B. “Nothing to mourn, He was just a drug addict”—Stigma towards people bereaved by drug-related death. Addict. Res. Theory 2022, 30, 5–15. [Google Scholar] [CrossRef]
- Friedman, S.R.; Pouget, E.R.; Sandoval, M.; Rossi, D.; Mateu-Gelabert, P.; Nikolopoulos, G.K.; Schneider, J.A.; Smyrnov, P.; Stall, R.D. Interpersonal Attacks on the Dignity of Members of HIV Key Populations: A Descriptive and Exploratory Study. AIDS Behav. 2017, 21, 2561–2578. [Google Scholar] [CrossRef] [PubMed]
- Klin, A.; Lemish, D. Mental Disorders Stigma in the Media: Review of Studies on Production, Content, and Influences. J. Health Commun. 2008, 13, 434–449. [Google Scholar] [CrossRef] [PubMed]
- Hansen, H.; Parker, C.; Netherland, J. Race as a Ghost Variable in (White) Opioid Research. Sci. Technol. Hum. Values 2020, 45, 848–876. [Google Scholar] [CrossRef]
- Hari, J. Chasing the Scream: The First and Last Days of the War on Drugs; Bloomsbury Publishing USA: New York, NY, USA, 2015. [Google Scholar]
- McCubbins, A. American Drug Story How Racialized Media Depictions of Drug Crises Shape Policy Agendas; Arizona State University: New York, NY, USA, 2020. [Google Scholar]
- Netherland, J.; Hansen, H.B. The War on Drugs That Wasn’t: Wasted Whiteness, “Dirty Doctors”, and Race in Media Coverage of Prescription Opioid Misuse. Cult. Med. Psychiatry 2016, 40, 664–686. [Google Scholar] [CrossRef] [Green Version]
- Lindsay, S.L.; Vuolo, M. Criminalized or Medicalized? Examining the Role of Race in Responses to Drug Use. Soc. Probl. 2021, 68, 942–963. [Google Scholar] [CrossRef]
- Pyra, M.; Taylor, B.; Flanagan, E.; Hotton, A.; Lamuda, P.; Schneider, J.; Pollack, H.A. Support for evidence-informed opioid policies and interventions: The role of racial attitudes, political affiliation, and opioid stigma. Prev. Med. 2022, 158, 107034. [Google Scholar] [CrossRef]
- Galvin, M.A.; Ulmer, J.T. Expanding our understanding of focal concerns: Alternative sentences, race, and “salvageability”. Justice Q. 2021, 39, 1332–1353. [Google Scholar] [CrossRef]
- Nicosia, N.; MacDonald, J.M.; Pacula, R.L. Does mandatory diversion to drug treatment eliminate racial disparities in the incarceration of drug offenders? An examination of California’s Proposition 36. J. Quant. Criminol. 2017, 33, 179–205. [Google Scholar] [CrossRef] [Green Version]
- Friedman, S.R.; Williams, L.D.; Guarino, H.; Mateu-Gelabert, P.; Krawczyk, N.; Hamilton, L.; Walters, S.M.; Ezell, J.M.; Khan, M.; Di Iorio, J. The stigma system: How sociopolitical domination, scapegoating, and stigma shape public health. J. Community Psychol. 2021, 50, 385–408. [Google Scholar] [CrossRef] [PubMed]
- Friedman, S.R.; Williams, L.D.; Jordan, A.E.; Walters, S.; Perlman, D.C.; Mateu-Gelabert, P.; Nikolopoulos, G.K.; Khan, M.R.; Peprah, E.; Ezell, J. Toward a Theory of the Underpinnings and Vulnerabilities of Structural Racism: Looking Upstream from Disease Inequities among People Who Use Drugs. Int. J. Environ. Res. Public Health 2022, 19, 7453. [Google Scholar] [CrossRef] [PubMed]
- Ashford, R.D.; Brown, A.M.; Curtis, B. Substance use, recovery, and linguistics: The impact of word choice on explicit and implicit bias. Drug Alcohol Depend. 2018, 189, 131–138. [Google Scholar] [CrossRef] [PubMed]
- Werder, K.; Curtis, A.; Reynolds, S.; Satterfield, J. Addressing Bias and Stigma in the Language We Use with Persons with Opioid Use Disorder: A Narrative Review. J. Am. Psychiatr. Nurses Assoc. 2022, 28, 9–22. [Google Scholar] [CrossRef]
- Corrigan, P.W.; Nieweglowski, K. Stigma and the public health agenda for the opioid crisis in America. Int. J. Drug Policy 2018, 59, 44–49. [Google Scholar] [CrossRef]
- Judd, H.; Meier, C.L.; Yaugher, A.C.; Campbell, E.; Atismé-Bevins, K. Opioid Use Disorder Stigma Reduction Through Story Telling Narrative and Sharing: A Qualitative Review and Lessons Learned. Int. J. Ment. Health Addict. 2021, 21, 468–483. [Google Scholar] [CrossRef]
- McGinty, E.E.; Stone, E.M.; Kennedy-Hendricks, A.; Barry, C.L. Stigmatizing language in news media coverage of the opioid epidemic: Implications for public health. Prev. Med. 2019, 124, 110–114. [Google Scholar] [CrossRef]
- Kelly, J.F.; Greene, M.C.; Abry, A. A US national randomized study to guide how best to reduce stigma when describing drug-related impairment in practice and policy. Addiction 2021, 116, 1757–1767. [Google Scholar] [CrossRef]
- Perry, B.L.; Pescosolido, B.A.; Krendl, A.C. The unique nature of public stigma toward non-medical prescription opioid use and dependence: A national study. Addiction 2020, 115, 2317–2326. [Google Scholar] [CrossRef]
- Faherty, L.J.; Kranz, A.M.; Russell-Fritch, J.; Patrick, S.W.; Cantor, J.; Stein, B.D. Association of Punitive and Reporting State Policies Related to Substance Use in Pregnancy With Rates of Neonatal Abstinence Syndrome. JAMA Netw. Open 2019, 2, e1914078. [Google Scholar] [CrossRef] [Green Version]
- Metzl, J.M. Dying of Whiteness: How the Politics of Racial Resentment Is Killing America’s Heartland; Hachette: London, UK, 2019. [Google Scholar]
- Phelan, J.C.; Link, B.G.; Dovidio, J.F. Stigma and prejudice: One animal or two? Soc. Sci. Med. 2008, 67, 358–367. [Google Scholar] [CrossRef] [Green Version]
- Lagisetty, P.A.; Ross, R.; Bohnert, A.; Clay, M.; Maust, D.T. Buprenorphine Treatment Divide by Race/Ethnicity and Payment. JAMA Psychiatry 2019, 76, 979. [Google Scholar] [CrossRef] [PubMed]
- Brezel, E.R.; Powell, T.; Fox, A.D. An ethical analysis of medication treatment for opioid use disorder (MOUD) for persons who are incarcerated. Subst. Abus. 2020, 41, 150–154. [Google Scholar] [CrossRef] [PubMed]
- Frank, D.; Mateu-Gelabert, P.; Perlman, D.C.; Walters, S.M.; Curran, L.; Guarino, H. “It’s like ‘liquid handcuffs”: The effects of take-home dosing policies on Methadone Maintenance Treatment (MMT) patients’ lives. Harm Reduct. J. 2021, 18, 88. [Google Scholar] [CrossRef] [PubMed]
- Hansen, H.B.; Siegel, C.E.; Case, B.G.; Bertollo, D.N.; Dirocco, D.; Galanter, M. Variation in Use of Buprenorphine and Methadone Treatment by Racial, Ethnic, and Income Characteristics of Residential Social Areas in New York City. J. Behav. Health Serv. Res. 2013, 40, 367–377. [Google Scholar] [CrossRef]
- Bonhomme, J.; Shim, R.S.; Gooden, R.; Tysu, D.; Rust, G. Opioid Addiction and Abuse in Primary Care Practice: A Comparison of Methadone and Buprenorphine as Treatment Options. J. Natl. Med. Assoc. 2012, 104, 342–350. [Google Scholar] [CrossRef] [Green Version]
- Allen, B.; Nolan, M.L.; Paone, D. Underutilization of medications to treat opioid use disorder: What role does stigma play? Subst. Abus. 2019, 40, 459–465. [Google Scholar] [CrossRef]
- Andraka-Christou, B. Addressing Racial And Ethnic Disparities In The Use Of Medications For Opioid Use Disorder: Study examines racial and ethnic disparities in the use of medications for opioid use disorder. Health Aff. 2021, 40, 920–927. [Google Scholar] [CrossRef]
- Dowling-Guyer, S.; Johnson, M.E.; Fisher, D.G.; Needle, R.; Watters, J.; Andersen, M.; Williams, M.; Kotranski, L.; Booth, R.; Rhodes, F. Reliability of drug users’ self-reported HIV risk behaviors and validity of self-reported recent drug use. Assessment 1994, 1, 383–392. [Google Scholar] [CrossRef]
- Thornberry, T.P.; Krohn, M.D. Delinquency and Crime. In Criminal Justice 2000: Measurement and Analysis of Crime and Justice; US Department of Justice: Washington, DC, USA, 2000; p. 4. [Google Scholar]
- Walters, S.M.; Perlman, D.C.; Guarino, H.; Mateu-Gelabert, P.; Frank, D. Lessons from the First Wave of COVID-19 for Improved Medications for Opioid Use Disorder (MOUD) Treatment: Benefits of Easier Access, Extended Take Homes, and New Delivery Modalities. Subst. Use Misuse 2022, 57, 1144–1153. [Google Scholar] [CrossRef]
- Ho, J. Anti-Asian racism, Black Lives Matter, and COVID-19. Jpn. Forum 2021, 33, 148–159. [Google Scholar] [CrossRef]
| Frequency/Mean (Std. Dev) | |
|---|---|
| Class Indicators | |
| Moral judgement of opioid use * | 49.5% |
| Social distance from individuals who use opioids * | 50.7% |
| Perceive individuals who use opioids as dangerous * | 52.6% |
| Discrimination against individuals who use opioids (housing and employment) * | 53.4% |
| Support public policies to cover OUD treatment and protect individuals who use opioids (i.e., public health) * | 50.0% |
| Support public policies that criminalize opioid use (i.e., punitive) * | 50.1% |
| Support for evidence-based treatment * | 47.4% |
| Covariates | |
| Gender | |
| Male | 48.3% |
| Female | 51.7% |
| Race/Ethnicity | |
| White | 63.8% |
| Hispanic | 15.9% |
| Black | 11.9% |
| Other | 8.4% |
| Education | |
| No college | 38.6% |
| Some college or more | 61.4% |
| Marital Status | |
| Married or living together | 58.3% |
| Single | 41.7% |
| Age | 48.1 (17.9) |
| Household Income | |
| Above state median | 40.1% |
| Below state median | 59.9% |
| Employed | 54.5% |
| Experiences with Opioid Use and/or Overdose | |
| Personal opioid use or overdose | 13.2% |
| Family opioid use or overdose | 40.2% |
| Criminal Legal Involvement | |
| Personal criminal legal involvement | 40.2% |
| Family criminal legal involvement | 44.2% |
| Model | LL a | No. of Parameters | BIC b | VLMR-LRT c |
|---|---|---|---|---|
| 1 class | −4879.70 | 7 | 9807.81 | N/A |
| 2 class | −4585.84 | 15 | 9275.41 | <0.01 |
| 3 class d | −4512.05 | 23 | 9183.14 | 0.09 |
| 4 class | −4469.95 | 31 | 9154.25 | 0.35 |
| 5 class | −4429.38 | 39 | 9128.43 | 0.26 |
| 6 class | −4414.94 | 47 | 9154.86 | 0.52 |
| “High Stigma/High Punitive Policy” | “High Stigma/Mixed Public Health and Punitive Policy” | |||
|---|---|---|---|---|
| AOR | p-Value | AOR | p-Value | |
| Gender | ||||
| Male | 1.11 | 0.74 | 0.76 | 0.41 |
| Female | Ref | Ref | ||
| Race/Ethnicity | ||||
| Black | 1.82 | 0.16 | 1.01 | 0.98 |
| Hispanic | 1.49 | 0.39 | 0.94 | 0.92 |
| Other | 0.92 | 0.90 | 2.59 | 0.11 |
| White | Ref | Ref | ||
| Age | 1.00 | 0.83 | 1.02 | 0.13 |
| Marital Status | ||||
| Married or living together | 0.87 | 0.67 | 1.21 | 0.62 |
| Single | Ref | Ref | ||
| Employed | ||||
| Yes | 1.39 | 0.34 | 1.00 | 0.99 |
| No | Ref | Ref | ||
| Education | ||||
| Some college or more | 0.35 | 0.01 | 0.48 | 0.06 |
| No college | Ref | Ref | ||
| Household income | ||||
| Below state median | 0.65 | 0.17 | 0.99 | 0.99 |
| Above state median | Ref | Ref | ||
| Personal opioid use | ||||
| Yes | 0.36 | 0.10 | 0.55 | 0.37 |
| No | Ref | Ref | ||
| Family opioid use | ||||
| Yes | 1.01 | 0.98 | 1.86 | 0.12 |
| No | Ref | Ref | ||
| Personal criminal legal involvement | ||||
| Yes | 0.80 | 0.74 | 1.91 | 0.35 |
| No | Ref | Ref | ||
| Family criminal legal involvement | ||||
| Yes | 0.70 | 0.27 | 0.67 | 0.26 |
| No | Ref | Ref | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Walters, S.M.; Liu, W.; Lamuda, P.; Huh, J.; Brewer, R.; Johnson, O.; Bluthenthal, R.N.; Taylor, B.; Schneider, J.A. A National Portrait of Public Attitudes toward Opioid Use in the US: A Latent Class Analysis. Int. J. Environ. Res. Public Health 2023, 20, 4455. https://doi.org/10.3390/ijerph20054455
Walters SM, Liu W, Lamuda P, Huh J, Brewer R, Johnson O, Bluthenthal RN, Taylor B, Schneider JA. A National Portrait of Public Attitudes toward Opioid Use in the US: A Latent Class Analysis. International Journal of Environmental Research and Public Health. 2023; 20(5):4455. https://doi.org/10.3390/ijerph20054455
Chicago/Turabian StyleWalters, Suzan M., Weiwei Liu, Phoebe Lamuda, Jimi Huh, Russell Brewer, O’Dell Johnson, Ricky N. Bluthenthal, Bruce Taylor, and John A. Schneider. 2023. "A National Portrait of Public Attitudes toward Opioid Use in the US: A Latent Class Analysis" International Journal of Environmental Research and Public Health 20, no. 5: 4455. https://doi.org/10.3390/ijerph20054455







