Auditing the Audits: A Systematic Review on Different Procedures in Telemedicine
Abstract
1. Introduction
- Teleconsultation: This term can refer to two distinct processes.
- Remote counselling between health professionals from different areas of intervention. Consultation often occurs because of the absence of a medical specialist and concerns a patient’s diagnosis or treatment [5].
- Remote real-time medical examination in which one or more physicians assess a patient’s state of health using information technologies. Currently, there are two main options to deliver this kind of visit: purchasing a solution from a vendor and installing the study premises or buying video conferencing as a service from a vendor [6]. The first option allows easier management and better security control of devices, but the second option (the most popular one) involves:
- 2.
- Remote cooperation: In emergencies or critical scenarios, one physician helps and cooperates with another online through real-time video and audio communication. These scenarios could include both the recent COVID-19 pandemic [7] and operating room surgery [8,9]. In this latter case, the surgical team operates on the patient, while the remote participants can collaboratively work thanks to high-quality video-audio streams.
- 3.
- Telemonitoring: The periodic biomedical remote monitoring of the patients from a tablet, smartphone, or computer web browser is connected with low-cost and basic medical devices such as blood pressure cuffs, thermometers, and digital scales [10].
- Economic-managerial audit: aims to assess the appropriateness and efficiency of planning, the management of resources, and expenditure.
- Organizational audit: evaluates organizational processes (e.g., information system, workload assessment, organisational procedures aimed at the acquisition and support of technologies). System audit: examines the main organisational aspects, practices, procedures, and controls that support the efficiency of an entire organisation, a hospital, or a department. Clinical audit: is an intervention aimed at collecting and comparing clinical data with reference standards [21,22]. It is fundamental to improving clinical practice and equity in different settings.
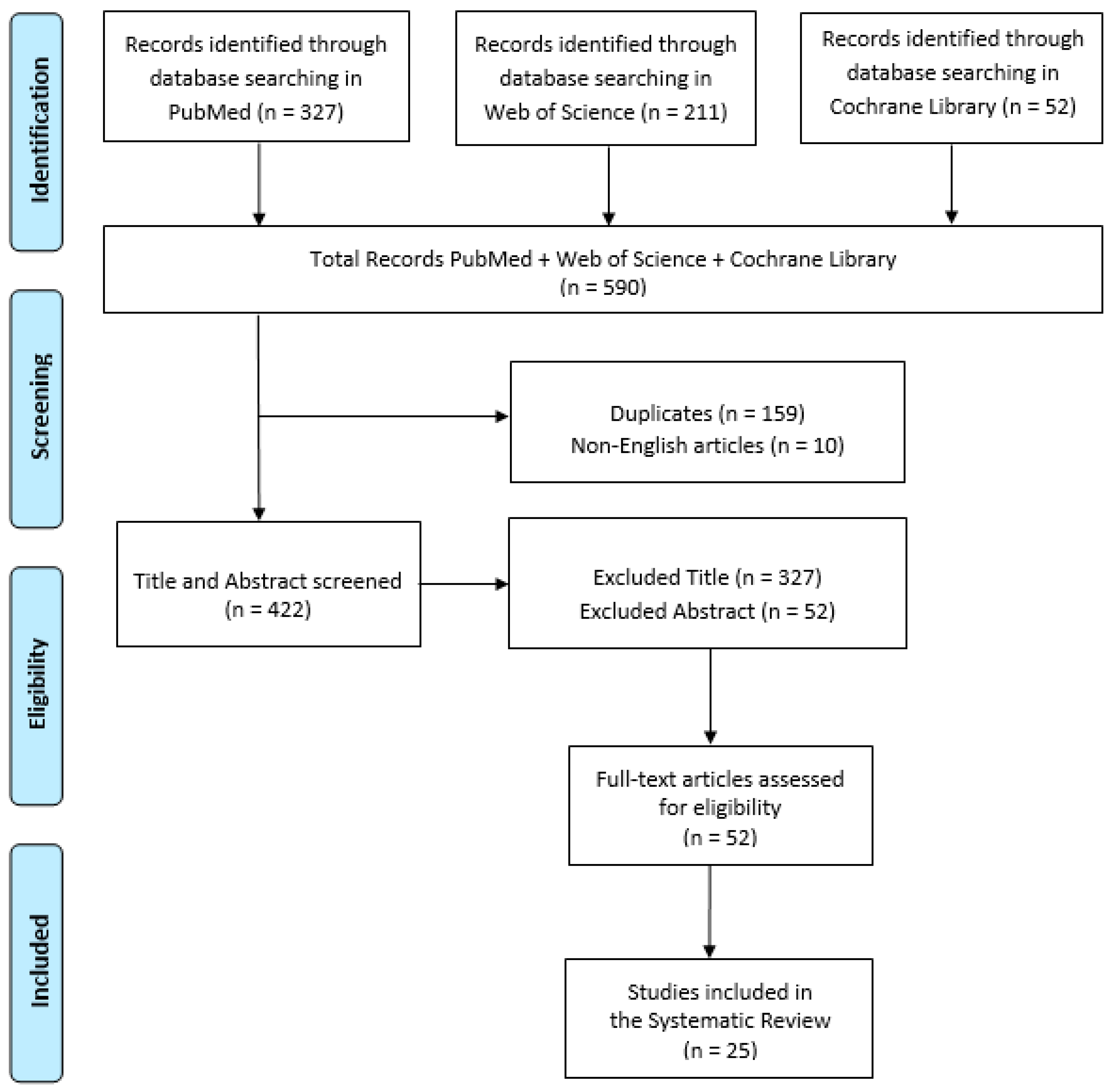
2. Materials and Methods
3. Results
3.1. Telemedicine Service
3.2. Studies Data
3.3. Satisfaction
- –
- –
- –
- Very helpful, especially in the peripheries, to cut on travelling and waiting time, thus saving money [41].
- –
- –
3.4. Feedback
- –
- It increases the skills of healthcare workers through the proper communication of errors made.
- –
- It increases awareness of the implications of making mistakes.
- –
- It allows the development of critical thinking and improved decision-making process.
- –
- In addition, it has emerged that it is not only important to communicate the error but also the timing and manner in which this occurs.
3.5. Organizational Aspects
3.6. Models
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Wilson, L.S.; Maeder, A.J. Recent Directions in Telemedicine: Review of Trends in Research and Practice. Healthc. Inform. Res. 2015, 21, 213–222. [Google Scholar] [CrossRef] [PubMed]
- Nesbitt, T.S. The Evolution of Telehealth: Where Have We Been and Where Are We Going; National Academies Press: Washington, DC, USA, 2012. [Google Scholar]
- Blackburn, H. Translation of The Telecardiogram, article by W. Einthoven. Am. Heart J. 1957, 53, 602–615. [Google Scholar]
- Zanaboni, P.; Wootton, R. Adoption of telemedicine: From pilot stage to routine delivery. BMC Med. Inform. Decis. Mak. 2012, 12, 1. [Google Scholar] [CrossRef] [PubMed]
- Lai, F. Robotic telepresence for collaborative clinical outreach. Stud. Health Technol. Inform. 2008, 132, 233–235. [Google Scholar] [PubMed]
- Baker, J.; Stanley, A. Telemedicine Technology: A Review of Services, Equipment, and Other Aspects. Curr. Allergy Asthma Rep. 2018, 18, 60. [Google Scholar] [CrossRef]
- Witowska-Zimny, M.; Nieradko-Iwanicka, B. Telemedicine in Emergency Medicine in the COVID-19 Pandemic-Experiences and Prospects—A Narrative Review. Int. J. Environ. Res. Public Health 2022, 19, 8216. [Google Scholar] [CrossRef]
- Bao, X.; Guo, S.; Xiao, N.; Li, Y.; Yang, C.; Shen, R.; Cui, J.; Jiang, Y.; Liu, X.; Liu, K. Operation evaluation in-human of a novel remote-controlled vascular interventional robot. Biomed. Microdevices 2018, 20, 34. [Google Scholar] [CrossRef]
- Marescaux, J.; Leroy, J.; Rubino, F.; Smith, M.; Vix, M.; Simone, M.; Mutter, D. Transcontinental Robot-Assisted Remote Telesurgery: Feasibility and Potential Applications. Ann. Surg. 2002, 235, 487–492. [Google Scholar] [CrossRef]
- Barrett, M.; Combs, V.; Su, J.G.; Henderson, K.; Tuffli, M. AIR Louisville: Addressing asthma with technology, crowdsourcing, cross-sector collaboration, and policy. Health Aff. (Millwood) 2018, 37, 525–534. [Google Scholar] [CrossRef]
- Finkelstein, S.M.; Speedie, S.M.; Potthoff, S. Home Telehealth Improves Clinical Outcomes at Lower Cost for Home Healthcare. Telemed. e-Health 2006, 12, 128–136. [Google Scholar] [CrossRef]
- Coulter, A. Patient Engagement—What Works? J. Ambul. Care Manag. 2012, 35, 80–89. [Google Scholar] [CrossRef]
- Weinstein, R.S.; Lopez, A.M.; Joseph, B.A.; Erps, K.A.; Holcomb, M.; Barker, G.P.; Krupinski, E.A. Telemedicine, Telehealth, and Mobile Health Applications That Work: Opportunities and Barriers. Am. J. Med. 2013, 127, 183–187. [Google Scholar] [CrossRef] [PubMed]
- Planinc, I.; Milicic, D.; Cikes, M. Telemonitoring in Heart Failure Management. Card. Fail. Rev. 2020, 6, e06. [Google Scholar] [CrossRef] [PubMed]
- Rojas, S.V.; Gagnon, M.P. A systematic review of the key indicators for assessing telehomecare cost-effectiveness. Telemed. J. E Health 2008, 14, 896–904. [Google Scholar] [CrossRef] [PubMed]
- Armfield, N.R.; Edirippulige, S.K.; Bradford, N.; Smith, A. Telemedicine—Is the cart being put before the horse? Med. J. Aust. 2014, 200, 530–533. [Google Scholar] [CrossRef] [PubMed]
- Elwyn, G.; Hardisty, A.R.; Peirce, S.C.; May, C.; Evans, R.; Robinson, D.K.R.; Bolton, C.E.; Yousef, Z.; Conley, E.C.; Rana, O.F.; et al. Detecting deterioration in patients with chronic disease using telemonitoring: Navigating the ‘trough of disillusionment’. J. Eval. Clin. Pract. 2011, 18, 896–903. [Google Scholar] [CrossRef]
- Wootton, R.; Geissbuhler, A.; Jethwani, K.; Kovarik, C.; Person, D.A.; Vladzymyrskyy, A.; Zanaboni, P.; Zolfo, M. Long-running telemedicine networks delivering humanitarian services: Experience, performance and scientific output. Bull. World Health Organ. 2012, 90, 341–347. [Google Scholar] [CrossRef]
- May, C.R.; Finch, T.L.; Cornford, J.; Exley, C.; Gately, C.; Kirk, S.; Jenkings, K.N.; Osbourne, J.; Robinson, A.L.; Rogers, A.; et al. Integrating telecare for chronic disease management in the community: What needs to be done? BMC Health Serv. Res. 2011, 11, 131. [Google Scholar] [CrossRef]
- Francesconi, P.; Bellini, B.; Furlan, F. Audit & Feedback: Un esempio di utilizzo per migliorare l’aderenza alle terapie. Recent. Prog. Med. 2021, 112, 574–578. [Google Scholar]
- Cardile, D.; Ielo, A.; Corallo, F.; Cappadona, I.; D’Aleo, G.; De Cola, M.C.; Bramanti, P.; Ciurleo, R. Communication Training: Significance and Effects of a Preliminary Psychological Intervention upon an Audit Team. Int. J. Environ. Res. Public Health 2023, 20, 4173. [Google Scholar] [CrossRef]
- Ciurleo, R.; De Cola, M.C.; Agabiti, N.; Di Martino, M.; Bramanti, P.; Corallo, F. Audit and feedback in cardio- and cerebrovascular setting: Toward a path of high reliability in Italian healthcare. Front. Public Health 2022, 10, 907201. [Google Scholar] [CrossRef]
- Morris, C.; Scott, R.E.; Mars, M. An Audit and Survey of Informal Use of Instant Messaging for Dermatology in District Hospitals in KwaZulu-Natal, South Africa. Int. J. Environ. Res. Public Health 2022, 19, 7462. [Google Scholar] [CrossRef] [PubMed]
- Biscak, T.M.; Manoharan, S.; Eley, R.; Sinnott, M.; Soyer, H.P. Audit of a State-wide store and forward teledermatology service in Australia. J. Telemed. Telecare 2013, 19, 362–366. [Google Scholar] [CrossRef] [PubMed]
- Miller, B.J.; Finnane, A.; Vun, Y.; Halloran, S.; Stapelberg, A.; Soyer, H.P.; Caffery, L. Real-time teledermatology clinics in a tertiary public hospital: A clinical audit. Australas. J. Dermatol. 2020, 61, e383–e387. [Google Scholar] [CrossRef]
- McWilliams, T.; Hendricks, J.; Twigg, D.; Wood, F.; Giles, M. Telehealth for paediatric burn patients in rural areas: A retrospective audit of activity and cost savings. Burns 2016, 42, 1487–1493. [Google Scholar] [CrossRef]
- Biggs, K.; Lowe, P.; Walsh, J.; Lagios, K. Audit of a sexual health website email link for general practitioners. Int. J. STD AIDS 2010, 21, 60–62. [Google Scholar] [CrossRef] [PubMed]
- Ng, L.; Narayanan, N.; Diamond, D.; Pitigala, N. Audit of acute psychiatric presentations during New Zealand’s first COVID-19 national lockdown. Australas. Psychiatry 2021, 30, 223–228. [Google Scholar] [CrossRef] [PubMed]
- Harvey, R.; Roques, P.K.; Fox, N.C.; Rossor, M.N. CANDID--Counselling and Diagnosis in Dementia: A national telemedicine service supporting the care of younger patients with dementia. Int. J. Geriatr. Psychiatry 1998, 13, 381–388. [Google Scholar] [CrossRef]
- Handschu, R.; Scibor, M.; Wacker, A.; Stark, D.R.; Köhrmann, M.; Erbguth, F.; Oschmann, P.; Schwab, S.; Marquardt, L. Feasibility of Certified Quality Management in a Comprehensive Stroke Care Network Using Telemedicine: STENO Project. Int. J. Stroke 2014, 9, 1011–1016. [Google Scholar] [CrossRef]
- Haydon, H.M.; Caffery, L.J.; Snoswell, C.L.; E Thomas, E.; Taylor, M.; Budge, M.; Probert, J.; Smith, A.C. Optimising specialist geriatric medicine services by telehealth. J. Telemed. Telecare 2021, 27, 674–679. [Google Scholar] [CrossRef]
- Kennedy, C.; Bowman, R.; Fariza, N.; Ackuaku, E.; Ntim-Amponsah, C.; Murdoch, I. Audit of Web-based telemedicine in ophthalmology. J. Telemed. Telecare 2006, 12, 88–91. [Google Scholar] [CrossRef] [PubMed]
- Patel, A.; Fothergill, A.S.; Barnard, K.E.C.; Dunbar, H.; Crossland, M.D. Lockdown low vision assessment: An audit of 500 telephone-based modified low vision consultations. Ophthalmic Physiol. Opt. 2021, 41, 295–300. [Google Scholar] [CrossRef]
- O’Day, R.; Smith, C.; Muir, J.; Turner, A. Optometric use of a teleophthalmology service in rural Western Australia: Comparison of two prospective audits. Clin. Exp. Optom. 2016, 99, 163–167. [Google Scholar] [CrossRef] [PubMed]
- Bartnik, S.E.; Copeland, S.P.; Aicken, A.J.; Turner, A.W. Optometry-facilitated teleophthalmology: An audit of the first year in Western Australia. Clin. Exp. Optom. 2018, 101, 700–703. [Google Scholar] [CrossRef] [PubMed]
- Owen, P.J.; Keating, S.E.; Askew, C.D.; Clanchy, K.M.; Jansons, P.; Maddison, R.; Maiorana, A.; McVicar, J.; Robinson, S.; Mundell, N.L. Impact of the COVID-19 Pandemic on Exercise Physiology Services in Australia: A Retrospective Audit. Sports Med. Open 2022, 8, 94. [Google Scholar] [CrossRef]
- Navein, J.; Hagmann, J.; Ellis, J. Telemedicine in Support of Peacekeeping Operations Overseas: An Audit. Telemed. J. 1997, 3, 207–214. [Google Scholar] [CrossRef]
- Dunkerley, S.; Kurar, L.; Butler, K.; James, M.; Lowdon, I. The success of virtual clinics during COVID-19: A closed loop audit of the British orthopaedic association (BOAST) guidelines of outpatient orthopaedic fracture management. Injury 2020, 51, 2822–2826. [Google Scholar] [CrossRef]
- Beard, M.; Orlando, J.; Kumar, S. Overcoming the tyranny of distance: An audit of process and outcomes from a pilot telehealth spinal assessment clinic. J. Telemed. Telecare 2016, 23, 733–739. [Google Scholar] [CrossRef]
- Vitacca, M.; Bazza, A.; Bianchi, L.; Gilè, S.; Assoni, G.; Porta, R.; Bertella, E.; Fiorenza, D.; Barbano, L.; Comini, L.; et al. Tele-assistance in chronic respiratory failure: Patients’ characterization and staff workload of 5-year activity. Telemed. J. e-Health Off. J. Am. Telemed. Assoc. 2010, 16, 299–305. [Google Scholar] [CrossRef]
- Williams, M. Using telehealth for rural paediatric diabetics: Does it deliver good care? J. Paediatr. Child Health 2020, 57, 109–113. [Google Scholar] [CrossRef]
- Webster, K.; Fraser, S.; Mair, F.; Ferguson, J. Provision of telehealth to the Scottish Police College. J. Telemed. Telecare 2008, 14, 160–162. [Google Scholar] [CrossRef] [PubMed]
- Alkmim, M.B.M.; Marcolino, M.S.; Maia, J.X.; Pessoa, C.G.; Machado, E.; Sousa, L. Clinical Quality Control of a Large-Scale Teleconsultation Service. Stud. Health Technol. Inform. 2015, 216, 988. [Google Scholar] [CrossRef] [PubMed]
- Keyworth, C.; Hart, J.; Thoong, H.; Ferguson, J.; Tully, M.; Murray, J. A Technological Innovation to Reduce Prescribing Errors Based on Implementation Intentions: The Acceptability and Feasibility of My Prescribe. JMIR Hum. Factors 2017, 4, e17. [Google Scholar] [CrossRef] [PubMed]
- Morozov, S.; Guseva, E.; Ledikhova, N.; Vladzymyrskyy, A.; Safronov, D. Telemedicine-based system for quality management and peer review in radiology. Insights Imaging 2018, 9, 337–341. [Google Scholar] [CrossRef]
- Orchard, J.; Li, J.; Freedman, B.; Webster, R.; Salkeld, G.; Hespe, C.; Gallagher, R.; Patel, A.; Kamel, B.; Neubeck, L.; et al. Atrial Fibrillation Screen, Management, and Guideline-Recommended Therapy in the Rural Primary Care Setting: A Cross-Sectional Study and Cost-Effectiveness Analysis of eHealth Tools to Support All Stages of Screening. J. Am. Heart Assoc. 2020, 9, e017080. [Google Scholar] [CrossRef]
- Jury, S.C.; Kornberg, A.J. Integrating telehealth in to ‘business as usual’: Is it really possible? J. Telemed. Telecare 2016, 22, 499–503. [Google Scholar] [CrossRef]
- Glasgow, R.E.; Vogt, T.M.; Boles, S.M. Evaluating the public health impact of health promotion interventions: The RE-AIM framework. Am. J. Public Health 1999, 89, 1322–1327. [Google Scholar] [CrossRef]
- Kidholm, K.; Jensen, L.K.; Kjølhede, T.; Nielsen, E.; Horup, M.B. Validity of the Model for Assessment of Telemedicine: A Delphi study. J. Telemed. Telecare 2016, 24, 118–125. [Google Scholar] [CrossRef]
- Kidholm, K.; Clemensen, J.; Caffery, L.; Smith, A. The Model for Assessment of Telemedicine (MAST): A scoping review of empirical studies. J. Telemed. Telecare 2017, 23, 803–813. [Google Scholar] [CrossRef]
- Kidholm, K.; Ekeland, A.G.; Jensen, L.K.; Rasmussen, J.; Pedersen, C.D.; Bowes, A.; Flottorp, S.; Bech, M. A Model for Assessment of Telemedicine Applications: Mast. Int. J. Technol. Assess. Health Care 2012, 28, 44–51. [Google Scholar] [CrossRef]
- Kapoor, L.; Basnet, R.; Chand, R.D.; Singh, S.; Mishra, S.K. An Audit of Problems in Implementation of Telemedicine Programme. In Proceedings of the 2007 9th International Conference on e-Health Networking, Application and Services, Taipei, Taiwan, 19–22 June 2007; pp. 87–89. [Google Scholar] [CrossRef]
- Ndoro, S. Effective multidisciplinary working: The key to high-quality care. Br. J. Nurs. 2014, 23, 724–727. [Google Scholar] [CrossRef] [PubMed]
- Keers, R.N.; Williams, S.D.; Cooke, J.; Ashcroft, D.M. Causes of Medication Administration Errors in Hospitals: A Systematic Review of Quantitative and Qualitative Evidence. Drug Saf. 2013, 36, 1045–1067. [Google Scholar] [CrossRef]
- Chan, J.C.; Gupta, A.K.; Stewart, S.; Babidge, W.; McCulloch, G.; Worthington, M.G.; Maddern, G.J. “Nobody told me”: Communication Issues Affecting Australian Cardiothoracic Surgery Patients. Ann. Thorac. Surg. 2019, 108, 1801–1806. [Google Scholar] [CrossRef] [PubMed]
- Moore, K. Improving communication between emergency department staff. Emerg. Nurse 2014, 22, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Whitten, P.S.; Allen, A. Analysis of Telemedicine from an Organizational Perspective. Telemed. J. 1995, 1, 203–213. [Google Scholar] [CrossRef] [PubMed]
- Hargie, O.D.W.; Tourish, D. Assessing the Effectiveness of Communication in Organisations: The Communication Audit Approach. Health Serv. Manag. Res. 1993, 6, 276–285. [Google Scholar] [CrossRef] [PubMed]
- Goldhaber, G.; Rogers, D. Auditing Organisational Communication Systems; Kendall/Hunt: Dubuque, Iowa, 1979. [Google Scholar]
- Downs, C. Communication Audits; Scott/Foresman: Location, UK, 1988. [Google Scholar]
| Study | Type | Aim | Disease | Telemedicine System | Population | Duration |
|---|---|---|---|---|---|---|
| Morris C., Scott E., Mars M., 2022 [23] | Retrospective | Auditing the informal use of instant messaging for dermatology by:
| Dermatology | Telecounselling | Service Users Medical Specialist (Dermatologists) Referring doctors | 4 years and 3 months |
| Biscak T.M. et al., 2013 [24] | Retrospective | To assess the use of the teledermatology service, including the characteristics of clinicians using the service and their perceptions of it. | Dermatology | Telecounselling | Consultations Referring doctors | 1 year |
| Miller B.J. et al., 2020 [25] | Retrospective | Evaluate a telemedicine system that provides a real-time videoconference teledermatology clinic to enable patients in rural and remote Queensland to access a specialist for dermatology care. | Dermatology | Telecounselling | Consultations | 2 years |
| McWilliams T. et al., 2016 [26]. | Retrospective | To conduct a retrospective audit of avoided transfers and bed days as a result of the use of the paediatric Burns Telehealth Service and to estimate their cost savings in 2012/13. | Pediatric burn | Telecounselling Monitoring | Caregivers of patients | 8 years |
| Biggs K. et al., 2010 [27] | Retrospective | Evaluate an “Email a Clinician” link on a medically reviewed sexual health website which allows general practitioners to communicate remotely with sexual health clinic specialists. | Sexual Health | Telecounselling | General Pratictioners Health care Workers | 1 year |
| NG L., Narayanan N., Diamond D., Pitigala N., 2022 [28] | N.A. | To identify service user demographic and clinical characteristics of an acute mental health service in South Auckland during the first New Zealand coronavirus. | Psychiatry | Telecounselling | Service Users | 1 Month (comparison) |
| Harvey R. et al., 1998 [29] | Retrospective | To audit and evaluate the introduction of a novel support service for younger people with dementia, their families, and the professionals caring for them. | Neurology | Telecounselling | Service Users | 2 year |
| Handschu et al., 2014 [30] | N.A. | The implementation and certification of a single quality management system for stroke care in all participating hospitals of the network, including stroke centers and local hospitals. | Neurology (Stroke) | Telecounselling | Consulting PhysiciansPhysicians in local hospitals Patients | 4 years |
| Haydon H.M. et al. 2021 [31] | N.A. | Investigate the growth and reach of Geri-Connect: a service established in 2017 to support people living in residential aged care facilities in regional Victoria, Australia. | Geriatry | Telecounselling Telemonitoring | Clinicians | 3 years |
| Kennedy C. et al., 2006 [32] | N.A. | To audit a web-based telemedicine service in ophthalmology. | Ophthalmology | Telecounselling | Service Users | 1 year |
| Patel A. et al., 2020 [33] | N.A. | Assess the efficacy of the telephone service offered by the Moorfields Eye Hospital NHS Foundation Trust (London) during the COVID-19 pandemic. | Ophthalmology | Telecounselling | Consultations Service Users | // |
| O’Day et al., 2016 [34] | Prospectivee | Comparing two five-month prospective audits of a teleophthalmology service (Lions Outback Vision) in rural Western Australia. | Ophthalmology | Telecounselling | Consultations | 2 years (comparison) |
| Bartnik et al., 2018 [35] | Retrospective | Audit the lion’s outback vision and provide practical insights for others looking to embed a telemedicine program as part of delivering outreach clinical services. | Ophthalmology | Telecounselling | Consultations | 1 year |
| Owen J. et al., 2022 [36] | Retrospective | To examine the impact of the COVID-19 pandemic on the reach, efficacy, adoption, and implementation of telehealth delivery for the exercise of physiology services. | Physiology | Telecounselling | Physiology clinicians | 5 months |
| Navein J., Hagmann J., Ellis J. 1997 [37] | Retrospective | Evaluate a satellite-based telemedicine system deployed in support of remote primary-care physicians in the U.S. military. | Orthopedics | Telecounselling Monitoring | Referring/Consulting clinicians Patients | 1 year and 3 months |
| Dunkerley S. et al., 2020 [38] | Prospective | Assess how the initial changes implemented within the department had affected outpatient fracture management and evaluate if the structure was meeting the new standards set by BOAST (the British Orthopedic Association). | Fracture | Telecounselling Monitoring | Referring/Consulting clinicians Patients | 1 month |
| Beard M., Orlando J.F., Kumar S. 2017 [39] | Prospective | Determine the feasibility, appropriateness, and access to a telehealth clinic by auditing the process and outcomes by a pilot telehealth spinal assessment clinic. | Spinal disorders | Telecounselling | Consultations | 5 months |
| Vitacca et al., 2010 [40] | Retrospective | Evaluate patients’ characterization and staff workload on a teleassistance service for patients with chronic respiratory failure. | Respiratory failure | Monitoring | Patients | 5 years |
| Williams M. 2020 [41] | Retrospective | To evaluate rural paediatric diabetic telehealth clinics, including whether they meet clinical standards and provide equivalent care to central clinics: families were satisfied, and difficulties were encountered. | Pediatric diabetic | Telecounselling Monitoring | Referring/Consulting clinicians Patients | 1 year |
| Webster et al., 2008 [42] | N.A. | Evaluate a telemedicine service established for the Scottish Police College with medical advice provided from the Aberdeen Royal Infirmary, | Injury/illness | Telecounselling | Consultations Service Users | 1 year and 4 months |
| Alkmim M.B.M et al., 2015 [43] | N.A. | To describe the audit of the teleconsultation responses performed by the Telehealth Network of Minas Gervais (TNMG). | Mixed | Telecounselling | Service Users | 1 month |
| Jury S.C., Kornberg J.A. 2016 [47] | N.A. | Evaluate the possibility of integrating telehealth into “business as usual”. | N.S. | Telecounselling | Clinicians | 1 month |
| Study | Type | Aim | Disease | Telemedicine System | Population | Duration |
|---|---|---|---|---|---|---|
| Keyworth C. et al., 2017 [44] | N.S. | Evaluate the acceptability and feasibility of providing feedback via MyPrescribe: a mobile-compatible website. Analyze and discuss the findings in the context of the COM-B model. Outline a series of practical implications and recommendations for using MyPrescribe. | Mixed (heart care, renal transplant/renal, gastroenterology | Tele monitoring | Pharmacists Junior doctors | 4 months |
| Morozov S. et al., 2018 [45] | N.S. | Evaluation of a telemedicine-based peer review of computed tomography and magnetic resonance imaging to enhance quality management in radiology. | Radiology Mixed | Tele monitoring | Patients | 12 Months |
| Orchard J. et al., 2020 [46] | N.S. | Cost-effective Analysis of eHealth Tools to Support All Stages of Screening. | Atrial fibrillation | Tele monitoring | Patients | 11 months |
| Study | Procedure | Recipients | N | Collected Data |
|---|---|---|---|---|
| Morris C., Scott E., Mars M., 2022 [23] | An audit was performed to assess the nature and content of the information sent to dermatologists by referring doctors. A 43 item questionnaire was administered to collect information related to the service. | Service Users Medical Specialist (Dermatologists) Referring doctors | 1034 messages sent. 830 answers received. 81 responses to questionnaires | Demographics, technical issues response times, satisfaction, consultations, consent and guidelines, data security. |
| Biscak T.M. et al., 2013 [24] | An audit was conducted to evaluate all teledermatology consultations. A retrospective questionnaire was administered to obtain feedback from the clinicians who used the service during the audit period. | Consultations Referring doctors | 685 emails analysed 34 responses to questionnaire | Consultation diagnosis satisfaction |
| Miller B.J. et al., 2020 [25] | An audit of the tele dermatology clinic was performed via a retrospective chart review of all referrals to the clinic for a two-year period (September 2015 to October 2017). | Consultations | 483 consultations for 178 patients. | Demographics, service activity and wait times, urgency category assigned to videoconferencing patients, diagnoses |
| McWilliams T. et al., 2016 [26] | A retrospective chart audit identified activity, avoided unnecessary acute and scar review patient transfers, inpatient bed days, and their associated avoided costs to the tertiary burn unit and patient travel funding. | Caregivers of patients | 904 patients | Avoided unnecessary acute and scar review, patient transfers, inpatient bed days and their associated avoided costs to the tertiary burn unit. |
| Biggs K. et al., 2010 [27] | Every email sent to the web-linked email account was identified and analyzed to determinate its content and sender classification. | General Practitioners Health care workers | 324 emails analysed. | Email nature and information requested by the sender |
| NG L., Narayanan N.,Diamond D., Pitigala N., 2022 [28] | A clinical audit was conducted on data from electronic psychiatric clinical assessment forms, to compare two randomly selected group (2020 vs. 2019 group) | Service Users | 413 service users during 2020. 785 service users during 2019. | First group: Demographics, Technology Diagnoses, psychological issues, follow-up. Second group: Same 1st group variables plus psychological COVID-19 related issues. |
| Harvey R. et al., 1998 [29] | General information was collected on every caller. Calls were divided into two main groups: a “registered” group and a “generic” one. Only the first group received specific clinical advice via a letter to their GP. | Service Users | 1121 calls received | Demographics, relationship between caller and patient, consultation |
| Handschu et al., 2014 [30] | Data recording by teleconsultations and all thrombolysis cases, as well as technical data and service complaints within the network, was implemented. | Consulting Physicians Physicians in local hospitals Patients | 2049 stroke teleconsultation in 2009 2324 patients in 2011 4517 patients seen in all local hospital. | Demographics, Consultation, Thrombolysis procedure informations. Deviations/key notes for improvement in internal audits from 2009 to 2011. |
| Haydon H.M. et al., 2021 [31] | Geri-Connect service activity data (2017–2020) were analysed to investigate the growth and reach of the service. The Model for the Assessment of Telemedicine (MAST, with these domains: Health problem and characteristics, clinical effectiveness, economic, organisational, scalability and generalisability). Semi-structured interviews with key stakeholders provided staff perspectives on the utility and barriers. | Clinicians | Data resulting for each of the 5 MAST domain. 10 phone interviews | Health problem and characteristic, clinical effectiveness, staff perception of patients, organizational aspects, scalability, generalizability. |
| Kennedy C. et al., 2006 [32] | Telemedicine website activity was monitored by a site supervisor. On this site referring doctors could upload brief case histories, problems, and treatment to seek the advice of a specialist. | Service Users | 132 cases posted to the website | Number, types of cases and additional information were analysed. |
| Patel A. et al., 2020 [33] | An audit of 500 consecutive telephone low vision appointments was performed. The successful completion of the assessment and clinical outcomes (low vision aids prescribed, onward referral) were recorded. | Consultations Service Users | 364 completed telephone low vision assessment | Participants diagnosis, Consultations. Patient lifestyle information. Social situation, employment and education. |
| O’Day et al., 2016 [34] | Two five-month audits were conducted. The first was conducted prior to the implementation of the intervention (2012), while the second was conducted during the period of intervention (2014). | Consultations | Number of video-consultations performed between the 2 audit periods | Differences between the 2 audits in: demographics, diagnosis, consultation, follow-up plan and technology |
| Bartnik et al., 2018 [35] | A retrospective audit was performed through the use of a data extraction tool to record information from all tele ophthalmology consultations performed in the time period (2015–2016). | Consultations | 709 patients referring to the service. 683 teleconsultations. | Diagnosis, consultations, cataract surgery rate, remoteness area of patients referred and imaging accompanying the referral. |
| Owen J. et al., 2022 [36] | A retrospective audit of exercise physiology services was conducted comparing Australian practises before (prior to 25 January 2020) and during the COVID-19 pandemic (after 25 January 2020). Relevant dimensions of the RE-AIM (reach, effectiveness, adoption and implementation) framework were adopted. | Physiology clinicians | 80 online survey completed | Clinicians and patients demographics, usual practise (prior to 25 January 2020) and changes to practise (after 25 January 2020), Consultations, Technology. |
| Navein J., Hagmann J., Ellis J. 1997 [37] | Data were collected using evaluation forms that were completed by referring and consulting physicians at the time of the consult and through structured interviews with referring physicians. | Referring/Consulting clinicians Patients | 53 consults 47 patients by seven GMOs/PAs | Demographics, technology and questions about: change in diagnosis/treatment and change in evacuation status resulting from the consult, improvement in the referring physician’s confidence, improvement in the military effectiveness of the unit. |
| Dunkerley S. et al., 2020 [38] | After the individuation of the four most relevant BOAST standards: an audit was designed around fracture immobilisation, the type of initial fracture clinic assessment, the default virtual follow-up clinic, and late imaging. Interventions were implemented and re-audited. | Referring/Consulting clinicians Patients | 223 patients | Emprovement in BOAST standards |
| Beard M., Orlando J.F., Kumar S. 2017 [39] | Data were recorded from all consultations managed using a videoconferencing technology between the Royal Adelaide Hospital and Port Augusta Community Health Service, South Australia between September 2013 and January 2014. Data were compared to a previous SAC clinic between August and December 2012. | Consultations | 41 participants in the SAC-T and 22 consultations in the SAC-O. | Analysis of process, service activity, clinical actions, safety and costs, demographics, clinical details. |
| Vitacca et al., 2010 [40] | Administrative and medical records from the TA service were retrospectively reviewed. Patients’ records were taken from the electronic database of the ‘‘Salvatore Maugeri Foundation’’ TA Service in Lumezzane (Brescia). Administrative and medical records from the TA service were retrospectively reviewed. | Patients | 396 consecutive CRF patients were analyzed. | Demographics, call characteristics, time of staff activity, salary cost evaluation, cost of the service. |
| Williams M. 2020 [41] | An audit of a telehealth service for children and adolescents with type 1 diabetes mellitus at four rural sites. A feedback survey was administered to satisfaction with the telehealth service, with preference for in-person or telehealth consultation, and any concerns regarding deficits in care and suggestions for improvements. | Referring/Consulting clinicians Patients | 19 children and adolescents aged 2–17 years were seen in the rural telehealth clinics. | Growth, information, and requirements of telehealth. Satisfaction, preference for in-person or telehealth consultation, deficit in care and suggestions for improvements. |
| Webster et al., 2008 [42] | Data collection forms were constructed and used at the Police College and in Aberdeen from November 2004 to February 2006. Problems were classified as either illness or injury, based on the main presenting complaint. In addition, the Police College conducted an informal interview with people who had used the service. | Consultations Service Users | 192 patients, 97 teleconsultations. 66 satisfaction interviews for students and staff | Date of presentation, date of injury, problem type, management, treatment, follow-up and referral for physiotherapy. Satisfaction. |
| Alkmim M.B.M et al., 2015 [43] | A random sample was selected from medical and non-medical teleconsultations performed by the specialists from the TNMG. All responses were scored according to their impact on the quality of the teleconsultation. | Service Users | 640 teleconsultation responses (medical:76% non-medical: 24%) | Objectivity, quality, ethics, courtesy |
| Jury S.C., Kornberg J.A. 2016 [47] | A one-month audit of booked telehealth was completed, looking for anything that impacted on the delivery or billing of telehealth. Each clinician was also asked for feedback on the day of their consultation. | Clinicians | 125 clinician feedback | Clinician feedback on telehealth appointments, Billing, Scheduling, and requesting telehealth. |
| Study | Procedure | Recipients | N | Collected Data |
|---|---|---|---|---|
| Keyworth C. et al., 2017 [44] | Pharmacists were invited to collect prescribing error data for junior doctors. They were invited to take part in semi-structured interviews exploring the perceptions of the acceptability and feasibility of MyPrescribe as a training tool aimed at improving prescribing practices. | Pharmacists (n = 11) junior doctors (n = 52) | 200 prescribing errors Interviews | Demographics, medical specialty. Change in COM-B model (capability, opportunity, motivation, behavior). Opinions on telemedicine service. |
| Morozov S. et al., 2018 [45] | A group of experts, two or three for each record, performed a distant peer review. If one of the experts considered that the discrepancy was significant, the system sent the study to another expert. If even the second disagrees, the study is redirected for the final evaluation of the third expert. | Patients | 23.199 studies | Quality control focuses on: Technical performance and detection of pathology. Scoring of the degree of discrepancy between clinical opinion |
| Orchard J. et al., 2020 [46] | GPs and/or practice nurses offered screening for AF with smartphone handheld single-lead ECGs (iECGs) (KardiaMobile) to eligible patients. To support the screening eHealth tools information was extracted from patients’ electronic medical records and guideline recommendations were made regarding treatment. | Patients | 3103 patients screened | Demographics, iECG screening, medication, and diagnostic information from the practices’ electronic patient records, treatment, cost- effectiveness. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cardile, D.; Corallo, F.; Cappadona, I.; Ielo, A.; Bramanti, P.; Lo Buono, V.; Ciurleo, R.; De Cola, M.C. Auditing the Audits: A Systematic Review on Different Procedures in Telemedicine. Int. J. Environ. Res. Public Health 2023, 20, 4484. https://doi.org/10.3390/ijerph20054484
Cardile D, Corallo F, Cappadona I, Ielo A, Bramanti P, Lo Buono V, Ciurleo R, De Cola MC. Auditing the Audits: A Systematic Review on Different Procedures in Telemedicine. International Journal of Environmental Research and Public Health. 2023; 20(5):4484. https://doi.org/10.3390/ijerph20054484
Chicago/Turabian StyleCardile, Davide, Francesco Corallo, Irene Cappadona, Augusto Ielo, Placido Bramanti, Viviana Lo Buono, Rosella Ciurleo, and Maria Cristina De Cola. 2023. "Auditing the Audits: A Systematic Review on Different Procedures in Telemedicine" International Journal of Environmental Research and Public Health 20, no. 5: 4484. https://doi.org/10.3390/ijerph20054484
APA StyleCardile, D., Corallo, F., Cappadona, I., Ielo, A., Bramanti, P., Lo Buono, V., Ciurleo, R., & De Cola, M. C. (2023). Auditing the Audits: A Systematic Review on Different Procedures in Telemedicine. International Journal of Environmental Research and Public Health, 20(5), 4484. https://doi.org/10.3390/ijerph20054484








