Over the Counter Pain Medications Used by Adults: A Need for Pharmacist Intervention
Abstract
1. Introduction
2. Material and Methods
2.1. Data Source
2.2. Patients Group
2.3. Statistical Analysis
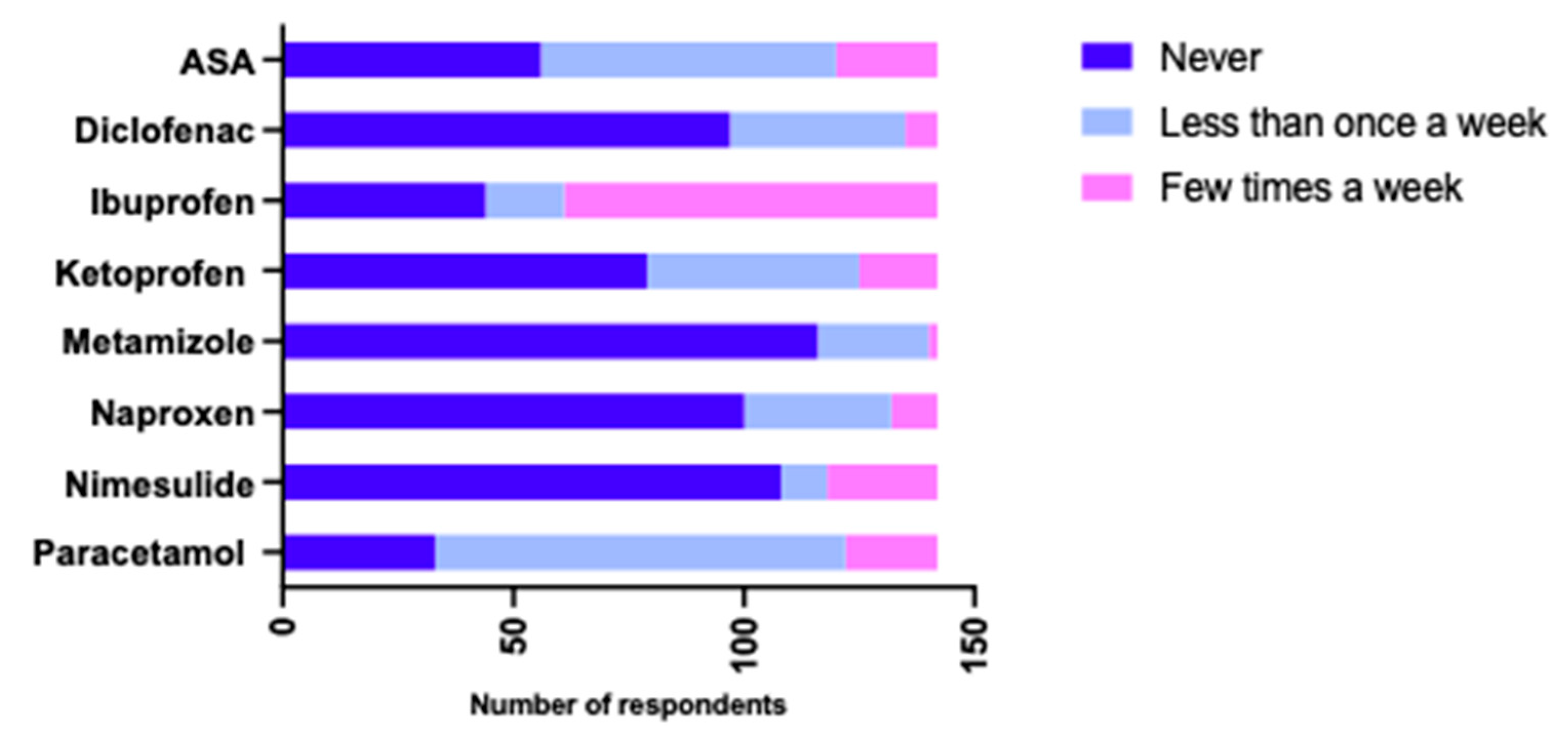
3. Results
3.1. Analysis of the Safety of Paracetamol Therapy
3.2. Analysis of the Safety of Ibuprofen Therapy
3.3. Analysis of the Safety of Acetylsalicylic Acid (ASA) Therapy
3.4. Analysis of the Safety of Ketoprofen Therapy
3.5. Analysis of the Safety of Diclofenac Therapy
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hamidi, M.; Joseph, B. Changing Epidemiology of the American Population. Clin. Geriatr. Med. 2019, 35, 1–12. [Google Scholar] [CrossRef]
- Andres, T.M.; McGrane, T.; McEvoy, M.D.; Allen, B.F.S. Geriatric Pharmacology: An Update. Anesthesiol. Clin. 2019, 37, 475–492. [Google Scholar] [CrossRef]
- Główny Urząd Statystyczny/Obszary Tematyczne/Osoby Starsze/Osoby Starsze/Sytuacja Osób Starszych w Polsce w 2020 Roku. Available online: https://stat.gov.pl/obszary-tematyczne/osoby-starsze/osoby-starsze/sytuacja-osob-starszych-w-polsce-w-2020-roku,2,3.html (accessed on 16 January 2023).
- Günster, C.; Klose, J.; Schmacke, N. Versorgungs-Report 2012; Schattauer: Stuttgart, Germany, 2012. [Google Scholar]
- Wieczorowska-Tobis, K.; Rajska-Neumann, A.; Grześkowiak, E. Metody unikania jatropatogenii na przykładzie leków stosowanych w chorobach układu sercowo-naczyniowego How to avoid iatrogenic syndromes in subjects treated with cardiovascular drugs? GERIATRIA 2009, 3, 92–96. [Google Scholar]
- Morin, L.; Johnell, K.; Laroche, M.L.; Fastbom, J.; Wastesson, J.W. The epidemiology of polypharmacy in older adults: Register-based prospective cohort study. Clin. Epidemiol. 2018, 10, 289–298. [Google Scholar] [CrossRef]
- Doan, J.; Zakrzewski-Jakubiak, H.; Roy, J.; Turgeon, J.; Tannenbaum, C. Prevalence and risk of potential cytochrome P450-mediated drug-drug interactions in older hospitalized patients with polypharmacy. Ann. Pharmacother. 2013, 47, 324–332. [Google Scholar] [CrossRef]
- Maher, R.L.; Hanlon, J.; Hajjar, E.R. Clinical Consequences of Polypharmacy in Elderly. Expert Opin. Drug Saf. 2014, 13, 57–65. [Google Scholar] [CrossRef]
- Charlesworth, C.J.; Smit, E.; Lee, D.S.H.; Alramadhan, F.; Odden, M.C. Polypharmacy among Adults Aged 65 Years and Older in the United States: 1988–2010. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2015, 70, 989–995. [Google Scholar] [CrossRef]
- O’Donoghue, A.C.; Johnson, M.; Sullivan, H.W.; Parvanta, S.; Ray, S.; Southwell, B.G. Aging and Direct-to-Consumer Prescription Drug Television Ads: The Effects of Individual Differences and Risk Presentation. J. Health Commun. 2019, 24, 368–376. [Google Scholar] [CrossRef]
- Wójta-Kempa, M.; Krzyzanowski, D.M. Correlates of Abusing and Misusing Over-the-Counter Pain Relievers among Adult Population of Wrocław (Poland). Adv. Clin. Exp. Med. 2016, 25, 349–360. [Google Scholar] [CrossRef]
- Majnarić, L.T.; Wittlinger, T.; Stolnik, D.; Babič, F.; Bosnić, Z.; Rudan, S. Prescribing Analgesics to Older People: A Challenge for GPs. Int. J. Environ. Res. Public Health 2020, 17, 4017. [Google Scholar] [CrossRef]
- Marttinen, M.K.; Kautiainen, H.; Haanpää, M.; Pohjankoski, H.; Hintikka, J.; Kauppi, M.J. Analgesic purchases among older adults—A population-based study. BMC Public Health 2021, 21, 256. [Google Scholar] [CrossRef]
- Prostran, M.; Vujović, K.S.; Vučković, S.; Medić, B.; Srebro, D.; Divac, N.; Stojanović, R.; Vujović, A.; Jovanović, L.; Jotić, A.; et al. Pharmacotherapy of pain in the older population: The place of opioids. Front. Aging Neurosci. 2016, 8, 144. [Google Scholar] [CrossRef]
- Ingrasciotta, Y.; Sultana, J.; Giorgianni, F.; Menditto, E.; Scuteri, A.; Tari, M.; Tari, D.U.; Basile, G.; Trifiro’, G. Analgesic drug use in elderly persons: A population-based study in Southern Italy. PLoS ONE 2019, 14, e0222836. [Google Scholar] [CrossRef]
- Wongrakpanich, S.; Wongrakpanich, A.; Melhado, K.; Rangaswami, J. A Comprehensive Review of Non-Steroidal Anti-Inflammatory Drug Use in the Elderly. Aging Dis. 2018, 9, 143–150. [Google Scholar] [CrossRef]
- Pilotto, A.; Franceschi, M.; Leandro, G.; Di Mario, F. NSAID and aspirin use by the elderly in general practice: Effect on gastrointestinal symptoms and therapies. Drugs Aging 2003, 20, 701–710. [Google Scholar] [CrossRef]
- Vandraas, K.F.; Spigset, O.; Mahic, M.; Slørdal, L. Non-steroidal anti-inflammatory drugs: Use and co-treatment with potentially interacting medications in the elderly. Eur. J. Clin. Pharmacol. 2010, 66, 823–829. [Google Scholar] [CrossRef]
- Abdu, N.; Mosazghi, A.; Teweldemedhin, S.; Asfaha, L.; Teshale, M.; Kibreab, M.; Anand, I.S.; Tesfamariam, E.H.; Russom, M. Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): Usage and co-prescription with other potentially interacting drugs in elderly: A cross-sectional study. PLoS ONE 2020, 15, e0238868. [Google Scholar] [CrossRef]
- Guo, J.; Huang, X.; Dou, L.; Yan, M.; Shen, T.; Tang, W.; Li, J. Aging and aging-related diseases: From molecular mechanisms to interventions and treatments. Signal Transduct. Target. Ther. 2022, 7, 391. [Google Scholar] [CrossRef]
- Sanford, A.M.; Morley, J.E.; Berg-Weger, M.; Lundy, J.; Little, M.O.; Leonard, K.; Malmstrom, T.K. High prevalence of geriatric syndromes in older adults. PLoS ONE 2020, 15, e0233857. [Google Scholar] [CrossRef]
- Doos, L.; Roberts, E.O.; Corp, N.; Kadam, U.T. Multi-drug therapy in chronic condition multimorbidity: A systematic review. Fam. Pract. 2014, 31, 654–663. [Google Scholar] [CrossRef]
- Cybulski, M.; Cybulski, L.; Krajewska-Kulak, E.; Orzechowska, M.; Cwalina, U. Preferences and attitudes of older adults of Bialystok, Poland toward the use of over-the-counter drugs. Clin. Interv. Aging 2018, 13, 623–632. [Google Scholar] [CrossRef]
- Weiner, M.; Tokarska-Rodak, M.; Bida, A. Using analgesics in different age groups, including intergenerational relations. Rozpr. Społeczne 2019, 13, 72–79. [Google Scholar] [CrossRef]
- Reguła, J.; Gastroenterologii, K.; Wocial, T.; Kraszewska, E.; Butruk, E. Stosowanie niesteroidowych leków przeciwzapalnych w Polsce—Badanie ankietowe u 38 tysięcy chorych. Gastroenterol. Klin. Postępy I Stand. 2011, 3, 72–78. Available online: https://journals.viamedica.pl/gastroenterologia_kliniczna/article/view/29278 (accessed on 16 January 2023).
- Fialová, D.; Příhodová, V.; Brkič, J.; Kummer, I.; Grešáková, S.; Lukačišinová, A.; Topinková, E. Evaluation of geriatric drug -disease interactions in seniors in log-term care in the Czech Republic. Klin. Farmakol. A Farm. 2020, 34, 99–107. [Google Scholar] [CrossRef]
- Midão, L.; Giardini, A.; Menditto, E.; Kardas, P.; Costa, E. Polypharmacy prevalence among older adults based on the survey of health, ageing and retirement in Europe. Arch. Gerontol. Geriatr. 2018, 78, 213–220. [Google Scholar] [CrossRef]
- Gnjidic, D.; Husband, A.; Todd, A. Challenges and innovations of delivering medicines to older adults. Adv. Drug Deliv. Rev. 2018, 135, 97–105. [Google Scholar] [CrossRef]
- Mangoni, A.A.; Jackson, S.H.D. Age-related changes in pharmacokinetics and pharmacodynamics: Basic principles and practical applications. Br. J. Clin. Pharmacol. 2004, 57, 6–14. [Google Scholar] [CrossRef]
- Benlidayi, I.C.; Kutsal, Y.G. Antirheumatic drugs in older adults and polypharmacy issues. Z. Gerontol. Geriatr. 2022, 55, 507–512. [Google Scholar] [CrossRef]
- Mullan, J.; Weston, K.M.; Bonney, A.; Burns, P.; Mullan, J.; Rudd, R. Consumer knowledge about over-the-counter NSAIDs: They don’t know what they don’t know. Aust. N. Z. J. Public Health 2017, 41, 210–214. [Google Scholar] [CrossRef]
- Vega-Morales, D.; Pérez-Luna, I.R.M.; Aguirre-García, V.A.; Vázquez-Fuentes, B.R. Non-Steroidal Anti-Inflammatory Drugs in the Elderly. Agreement with Safe Prescription Recommendations According to Cardiovascular and Gastrointestinal Risks. Reumatol. Clin. 2020, 17, 499–503. [Google Scholar] [CrossRef]
- Raynor, D.K.; Blenkinsopp, A.; Knapp, P.R.; Grime, J.; Nicolson, D.J.; Pollock, K.; Dorer, G.; Gilbody, S.M.; Dickinson, D.; Maule, A.J.; et al. A systematic review of quantitative and qualitative research on the role and effectiveness of written information available to patients about individual medicines. Health Technol. Assess. 2007, 11, 1–177. [Google Scholar] [CrossRef]
- Chlebowska, A.; Polakowska, D.; Miszewska, J.; Kowalska, S.; Dobbek, O.; Wrzosek, N.; Zimmermann, A. Examination of the need for additional pharmaceutical services and selected elements of pharmaceutical care in Poland—A pilot study. Farm. Pol. 2021, 77, 271–280. [Google Scholar] [CrossRef]
- Merks, P.; Religioni, U.; Waszyk-Nowaczyk, M.; Kaźmierczak, J.; Białoszewski, A.; Blicharska, E.; Kowalczuk, A.; Neumann-Podczaska, A. Assessment of Pharmacists’ Willingness to Conduct Medication Use Reviews in Poland. Int. J. Environ. Res. Public Health 2022, 19, 1867. [Google Scholar] [CrossRef]
- Blouin, R.A.; Adams, M.L. The Role of the Pharmacist in Health Care: Expanding and Evolving. N. C. Med. J. 2017, 78, 165–167. [Google Scholar] [CrossRef]
- Cortejoso, L.; Dietz, R.A.; Hofmann, G.; Gosch, M.; Sattler, A. Impact of pharmacist interventions in older patients: A prospective study in a tertiary hospital in Germany. Clin. Interv. Aging 2016, 11, 1343–1350. [Google Scholar] [CrossRef]
- Bell, J.; Dziekan, G.; Pollack, C.; Mahachai, V. Self-Care in the Twenty First Century: A Vital Role for the Pharmacist. Adv. Ther. 2016, 33, 1691–1703. [Google Scholar] [CrossRef]


| Condition | Female Respondents (%) | Male Respondents (%) | χ2 | p |
|---|---|---|---|---|
| Cardiovascular diseases | 21.6 | 20.4 | 0.030 | 0.863 |
| Hypertension | 34.1 | 50.0 | 3.525 | 0.060 |
| Diabetes | 19.3 | 37.0 | 5.453 | 0.020 |
| Kidney failure | 8.0 | 11.0 | 0.401 | 0.527 |
| Depression, neurosis | 26.1 | 7.4 | 7.623 | 0.006 |
| Condition | 50–60 Years (%) | 61–75 Years (%) | Over 75 Years Old (%) | χ2 | p |
|---|---|---|---|---|---|
| Cardiovascular diseases | 14.5 | 21.2 | 57.1 | 12.917 | 0.002 |
| Hypertension | 32.9 | 42.3 | 71.4 | 7.466 | 0.024 |
| Diabetes | 15.8 | 36.5 | 42.9 | 9.174 | 0.010 |
| Kidney failure | 6.6 | 5.8 | 35.7 | 13.197 | 0.001 |
| Depression, neurosis | 18.4 | 21.2 | 14.3 | 0.375 | 0.829 |
| Obesity | 7.9 | 25.0 | 21.4 | 7.318 | 0.026 |
| Neoplasms | 6.6 | 11.5 | 14.3 | 1.405 | 0.495 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Karłowicz-Bodalska, K.; Sauer, N.; Jonderko, L.; Wiela-Hojeńska, A. Over the Counter Pain Medications Used by Adults: A Need for Pharmacist Intervention. Int. J. Environ. Res. Public Health 2023, 20, 4505. https://doi.org/10.3390/ijerph20054505
Karłowicz-Bodalska K, Sauer N, Jonderko L, Wiela-Hojeńska A. Over the Counter Pain Medications Used by Adults: A Need for Pharmacist Intervention. International Journal of Environmental Research and Public Health. 2023; 20(5):4505. https://doi.org/10.3390/ijerph20054505
Chicago/Turabian StyleKarłowicz-Bodalska, Katarzyna, Natalia Sauer, Laura Jonderko, and Anna Wiela-Hojeńska. 2023. "Over the Counter Pain Medications Used by Adults: A Need for Pharmacist Intervention" International Journal of Environmental Research and Public Health 20, no. 5: 4505. https://doi.org/10.3390/ijerph20054505
APA StyleKarłowicz-Bodalska, K., Sauer, N., Jonderko, L., & Wiela-Hojeńska, A. (2023). Over the Counter Pain Medications Used by Adults: A Need for Pharmacist Intervention. International Journal of Environmental Research and Public Health, 20(5), 4505. https://doi.org/10.3390/ijerph20054505






