Abstract
This study aims to investigate the relationship between social determinants of health (SDH), incidence, and mortality to verify which sociodemographic factors, symptoms, and comorbidities predict clinical management; second, this study aims to conduct a survival analysis of individuals with COVID-19 in the Xingu Health Region. Consequently, this study adopted an ecological framework, employing secondary data of COVID-19-positive individuals from the Xingu Health Region, Pará State, Brazil. The data were obtained through the database of the State of Pará Public Health Secretary (SESPA) for the period from March 2020 to March 2021. The incidence and mortality were higher in Vitória do Xingu and Altamira. Municipalities with a higher percentage of citizens with health insurance and higher public health expenditure showed a higher incidence and mortality. A higher gross domestic product was associated with a higher incidence. Females were found to be associated with better clinical management. To live in Altamira was a risk factor for intensive care unit admission. The symptoms and comorbidities that predicted worse clinical management were dyspnea, fever, emesis, chills, diabetes, cardiac and renal diseases, obesity, and neurological diseases. There were higher incidence, mortality, and lower survival rates among the elderly. Thus, it can be concluded that SDH indicators, symptomatology, and comorbidities have implications for the incidence, mortality, and clinical management of COVID-19 in the Xingu Health Region of eastern Amazonia, Brazil.
1. Introduction
Coronavirus disease 2019 (COVID-19) is a highly contagious infectious disease caused by a new betacoronavirus belonging to the large viral family of Coronaviridae. The first cases of COVID-19 were reported in December 2019 in Wuhan, China [1,2]. Initially, the outbreak of severe acute respiratory syndrome by type 2 coronavirus (SARS-CoV-2) was confirmed in the province of Hubei; however, this virus spread rapidly to several countries, causing a pandemic in 2020 [3,4,5].
Regarding symptoms, the clinical manifestation of COVID-19 virus can range from asymptomatic to severe [6]. The main clinical symptoms of COVID-19 patients include fever, cough, myalgia or fatigue, and dyspnea [7,8]. Additionally, olfactory and gustatory dysfunctions are common clinical findings in these patients [9]. Minor symptoms include sputum production, headache, haemoptysis [8], dizziness, diarrhea, nausea, vomiting [6], and skin lesions [10,11]. The fatality rate is approximately 5% (95% CI (0.01–0.11)) [12]. The prevalence of comorbidities is considered a risk factor for severe patients. However, the symptoms of infected patients are nonspecific [6], and there is a need to know the characteristics of each population and its implications for clinical evolution.
Since the start of the pandemic till the present, the literature on possible treatments for COVID-19 disease is increasing; however, vitamin supplements, anti-inflammatory agents, and antimicrobial therapy have shown a lack of efficacy in the treatment of patients; the best care strategy throughout the course of the disease remains unknown [13,14].
SARS-CoV-2 has negative effects on clinical practice. Regarding health workers, they are at higher risk of infection due to their efforts to protect the community; consequently, they are exposed to psychological distress, fatigue, and stigma [15]. Furthermore, in the initial phase of the COVID-19 pandemic, the mental health and well-being of the general population were affected, with increasing rates of suicidal thoughts among the population [16]. In addition to host factors, environmental or social factors contribute to the high infection risk, especially factors such as poor living conditions, nutrition, ventilation, sanitation, and overcrowding [17]. Although specific population groups may have higher risk factors, the differences in social-epidemiological patterns, and differences by age and gender have been little studied. Social inequalities due to different living and working conditions and socioeconomic status should be taken into account when assessing the risk to different population groups [18].
The Brazilian Amazon represents approximately 58.9% of Brazil’s national territory, hosts a complex biodiversity which includes diverse cultures, ecosystem services, and human settlements, with various degrees of urbanization and rurality ranging from metropolitan regions such as Belém and Manaus to traditional riverside, indigenous, and quilombola communities [19]. In the eastern Brazilian Amazonia, nine municipalities along the Transamazonian highway comprise the microregion of the middle Xingu. The Xingu River, one of the main right-bank tributaries of the Amazon Basin and the largest fluvial system in the world, runs alongside these municipalities [20]. The population of the state of Pará exceeds 370,000. Altamira is the most populous city in the region, with a population of 116,000 individuals. The other eight municipalities of the state include Anapú, Medicilândia, Vitória do Xingu, Brasil Novo, Senador José Porfírio, Porto de Moz, Pacajá, and Uruará (with populations between 10,000 and 50,000 inhabitants) [21].
The Xingu Health Region is one of the more than 400 health regions in Brazil established by states in collaboration with municipalities under the provisions of Decree No. 7508 of 2011 [22]. A health region is a geographic area composed of neighboring municipalities delimited by common characteristics, such as cultural, economic, and social aspects; additionally, in a health region, there is an integration of infrastructure and transportation to conduct health-related actions and deliver services in an integrated and equitable manner [22,23].
The Belo Monte Hydroelectric Power Plant, the largest of its kind in Brazil, is located in this region. This hydroelectric dam was constructed between 2010 and 2017 through the Growth Acceleration Program funding, which led to a transformation in the social and demographic profile of all municipalities in the area, including a population increase, as well as financial and commercial movements, resulting in numerous investments [20,24]. However, simultaneously, there has also been an increase in socioeconomic problems such as violence, exacerbation of agrarian conflicts, relocation of traditional populations, prostitution, and deficiency in educational and health services [25]. Thus, the multiplicity and territorial and cultural complexities of the Xingu region result in a scenario of great social vulnerability, which potentially has a significant influence on the transmission, morbidity, and mortality rates of COVID-19 [26,27].
As humanity’s coexistence with the pandemic evolves, there is a need to understand its legacy across different social organizations and populations affected by the health, environmental, and economic crises it has brought about globally, taking into account the local and regional aspects [28,29].
In this sense, the Brazilian health policy works to improve the living conditions and environment of the population by adopting a technical, operational, and organizational approach to the management of health interventions and services. This approach is based on the conceptual model of the social determinants of health (SDH) theory [30], which suggests that health and disease processes are influenced by factors arranged at different levels, from micro factors such as hereditary factors, age, gender, and lifestyle, to macro factors related to environmental, cultural, and socioeconomic issues [27,31,32].
Additionally, in a pre-vaccination context, understanding the clinical symptoms and comorbidities in each population and their implications for COVID-19 incidence and mortality can contribute to the construction of a more effective and integrated health surveillance model [33,34]. Moreover, the identification of symptoms and comorbidities that are predictors of severe illness and intensive care unit (ICU) admission in these populations can help in the risk stratification of each patient in health services and facilitate more effective planning and mobilization of resources [35,36,37].
This study has the following objectives: (1) to investigate the relationship between SDH, incidence, and mortality; (2) to verify which sociodemographic factors, symptoms, and comorbidities predict clinical management; and (3) to analyze which sociodemographic and clinical factors are associated with lower survival of individuals with COVID-19 in the Xingu Health Region in the eastern Brazilian Amazon. This study hypothesized that poorer indicators of SDH are related to higher rates of incidence and mortality and that variables including advanced age, the female sex, living in cities with poorer social development, and specific symptoms and comorbidities serve as predictors of more severe clinical management, such as medical ward and intensive care, and lower survival in individuals with COVID-19 in the health region of Xingu in the eastern Brazilian Amazon.
2. Materials and Methods
2.1. Study Design
An observational study design employing an ecological approach with descriptive and inferential analyses was adopted.
2.2. Study Population and Period
This study examined the secondary data of individuals diagnosed with COVID-19 between March 2020 and March 2021 in a pre-vaccination scenario in the Xingu Health Region, Pará State, Brazil.
2.3. Inclusion and Exclusion Criteria
Diagnosis of SARS-CoV-2 by a reverse transcription-polymerase chain reaction (RT-PCR) or a serological test (rapid test) was defined as the study inclusion criterion. Therefore, only cases that were RT-PCR- or rapid test-positive were included in the study. Cases with missing data (i.e., sociodemographic information) were excluded.
2.4. Setting
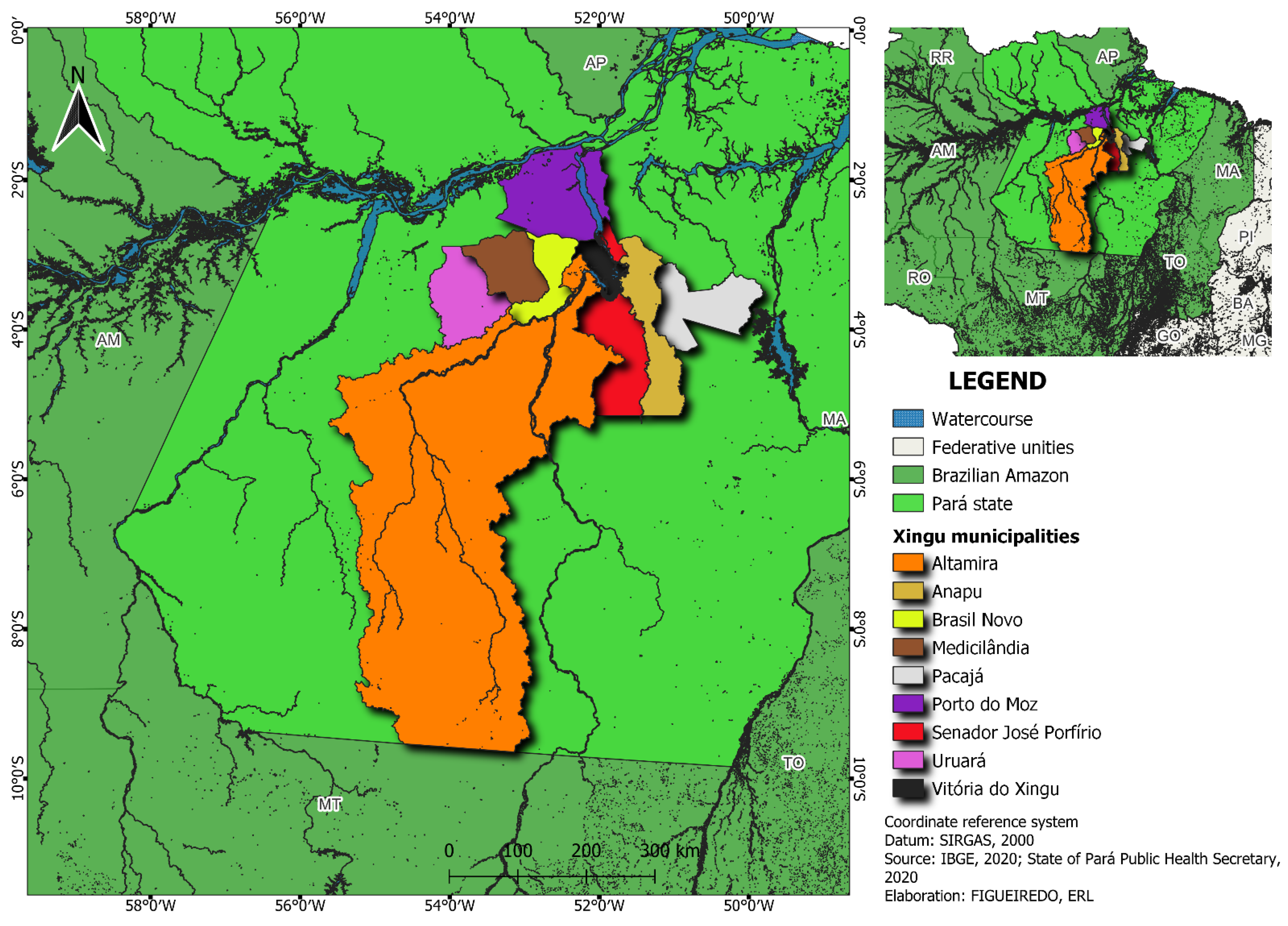
The data obtained from the nine municipalities of the Xingu Health Region, Pará State, Brazil (Figure 1), were analyzed. To visualize these cities, a map was constructed using QGIS Desktop 3.26.
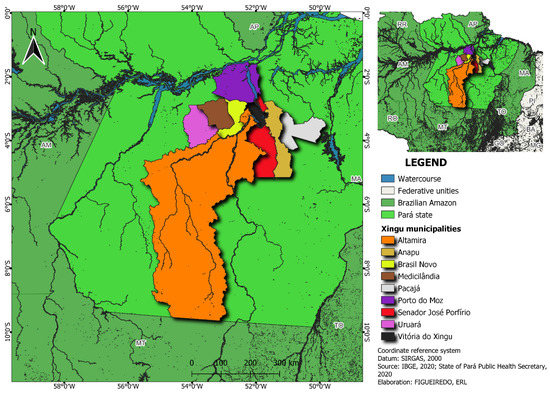
Figure 1.
Map of the Xingu Health Region.
2.5. Assessments
The databases of SESPA, the Brazilian Institute of Geography and Statistics (IBGE), e-Gestor AB, and the National Institute for Space Research (INPE) were utilized. The open-access database maintained by SESPA includes information regarding cases identified as COVID-19-positive, reported daily by municipal health departments and health services as part of the COVID-19 surveillance system in the state of Pará. These data are published daily between 5:00 and 7:00 p.m. on the www.covid-19.pa.gov.br portal; this portal comprises all the data on the COVID-19 pandemic in Pará [36]. The IBGE database includes data on Brazil, its states, and its municipalities; it includes infographics, maps, and other information on topics such as education, labor, the economy, population, health, and territory [21,37]. The e-Gestor AB database [38,39] is a platform that provides access to primary healthcare (PHC) information systems for the management of PHC data by managers and health professionals, facilitating access to data that can be useful in the organization and planning of health services. The INPE database includes environmental information on activities conducted by top research institutes in the country following minimum quality standards to facilitate the understanding and reuse of information [40].
The sociodemographic factors analyzed included age, sex, and municipality of residence. The clinical symptoms evaluated included fever, cough, dyspnea, nausea, headache, runny nose, nasal congestion, sore throat, diarrhea, chills, conjunctivitis, odynophagia, anosmia, ageusia, adynamia, myalgia, and arthralgia. The comorbidities considered included obesity; asthma; diabetes; immunodeficiency diseases; heart disease; pneumopathy; and neurological, renal, hematological, and hepatic diseases. The clinical management analysis included home care and the need for hospitalization, separating those who needed a medical ward from those who were hospitalized in intensive care units (ICUs). The time to symptom onset, date of death, and mortality of individuals were recorded. These data were obtained from the database provided by SESPA [36]. The incidence and mortality rates were calculated subsequently. IBGE [21,37] data were used to estimate the number of individuals in the Brazilian population (2020) in terms of the calculation of incidence and mortality rates, overall and according to sex, per 1000 inhabitants.
The SDH indicators used in the analysis of the Xingu Health Region are provided in Table 1. The SDH indicators analyzed included sociodemographic and habitation factors (population density [21,37]; percentage of elderly in the population [21,37]; percentage of the vulnerable households with an older adult in the population [21,37]; percentage of people in households with walls not made of masonry or wood [21,37]), economic and environmental factors (Gini index [21,37]; gross domestic product (GDP) [21,37]; Human Development Index [21,37]; percentage urbanization of public roads [41]; hotspot concentration [40]), health and resources (percentage of primary health care coverage [38,39]; percentage of people with health insurance [38,39]; number of physicians per 1000 individuals [38,39]; public health expenditure in the municipality, in BRL/inhabitant, per capita), and education and work (schooling sub-index [21,39]; illiteracy rate at age 15 and above [21,37]; unemployment rate at 10 years or older [21,37]). Classification of the indicators was based on the social gradients in health as theorized by Dalgreen and Whitehead [42] with respect to SDH [30].

Table 1.
Exploratory analysis of SDH indicators in the study of incidence and mortality by COVID-19 in the Xingu Health Region.
2.6. Statistical Analysis
Descriptive statistical analysis was conducted to compute frequencies (absolute and relative), means, and standard deviations (parametric) or medians with interquartile range (IQR, non-parametric) for each group. The incidence and mortality rates for every 1000 individuals were also calculated. For the spatial representation of incidence and mortality in the Xingu Health Region, the values of the four classes were constructed based on the equal interval technique, which is based on the amplitude of the data.
Bivariate correlation coefficients, Pearson’s r (parametric), and Spearman’s rs (nonparametric), were used to verify the level of correlation between variables. Binary logistic regression analysis was used to establish the determining factors for clinical management and mortality. Initially, univariate analysis was performed considering a p-value of <0.25. To verify multicollinearity, the variance inflation factor (VIF) was calculated, and variables that presented a VIF value above 10 were removed from the final model. Statistical significance was set at p < 0.05. An odds ratio (OR) with a 95% confidence interval (95% CI) was used to quantify the degree of association.
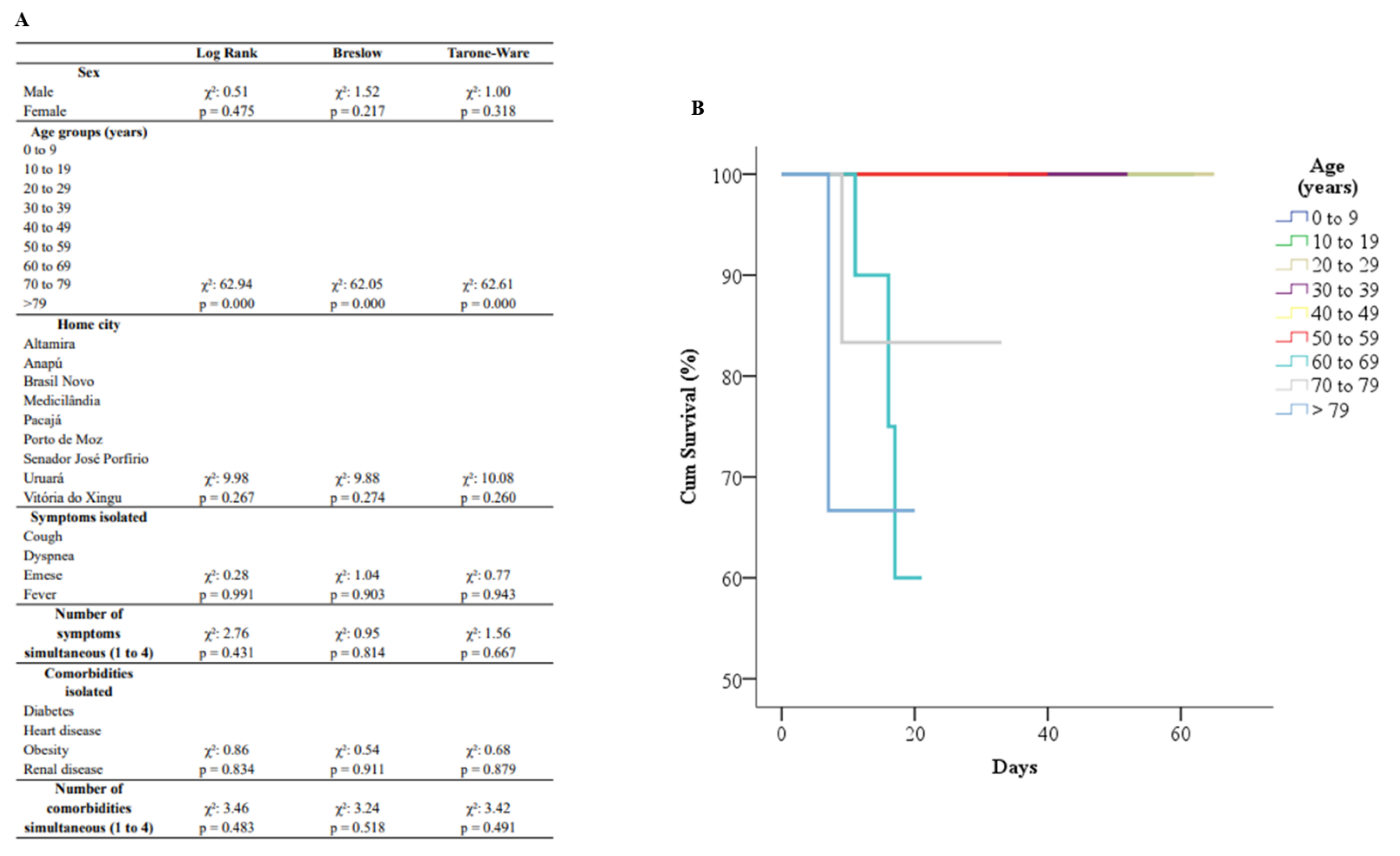
Survival curves were obtained by using the Kaplan–Meier estimator; additionally, log-rank (initial), Breslow (intermediary), and Tarone–Ware (final) tests were used to identify statistically significant differences in the different periods [42].
SPSS Version 26.0 (IBM Corp. Released 2019. IBM SPSS Statistics for Windows, Version 26.0. IBM Corp., Armonk, NY, USA) was used for the statistical analyses.
2.7. Ethical Issues
The open-access database used in this study is maintained by the State of Pará Public Health Secretary (SESPA), a state government agency, and contains consolidated information pertaining to individuals who have sought healthcare services owing to COVID-19-related symptoms. The individuals covered in this database are not identified; hence, according to National Health Council (CNS) Resolution No. 510 of 7 April 2016, evaluation by the relevant research ethics committee was not required [43].
3. Results
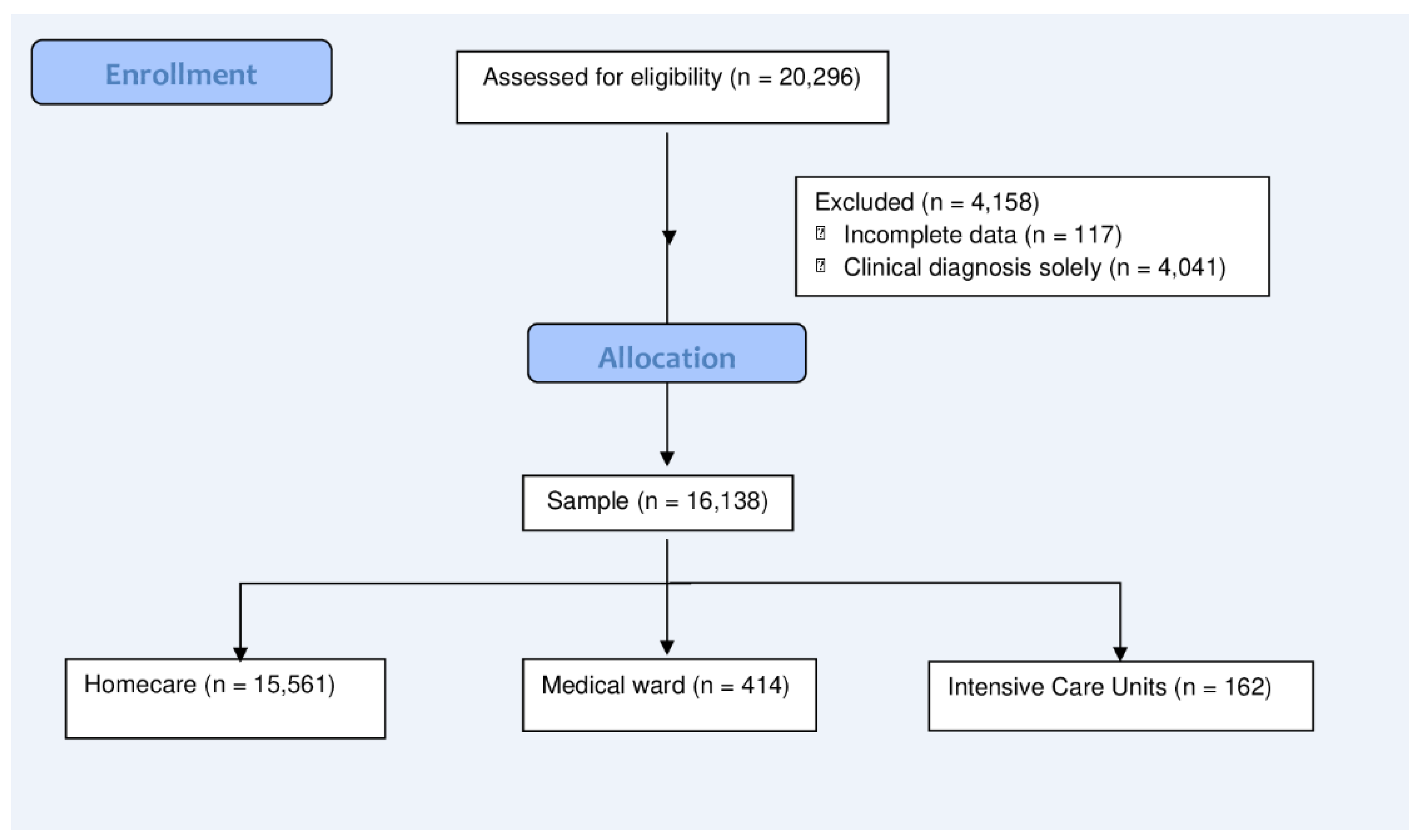
Overall, 20,296 COVID-19 cases were identified during the study period. However, 117 cases were excluded due to the incomplete sociodemographic information of these patients. Furthermore, 4041 cases were excluded since no other information except the clinical diagnosis was available. The final sample included 16,138 patients (Figure 2).
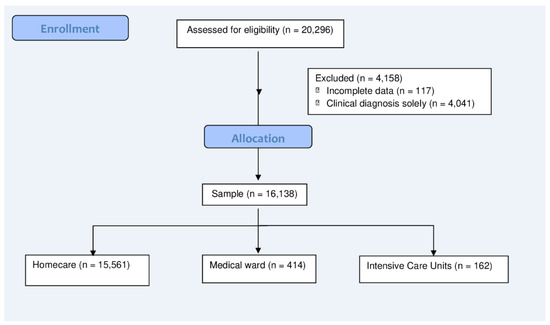
Figure 2.
Flow diagram of the selection and distribution of individuals in the groups.
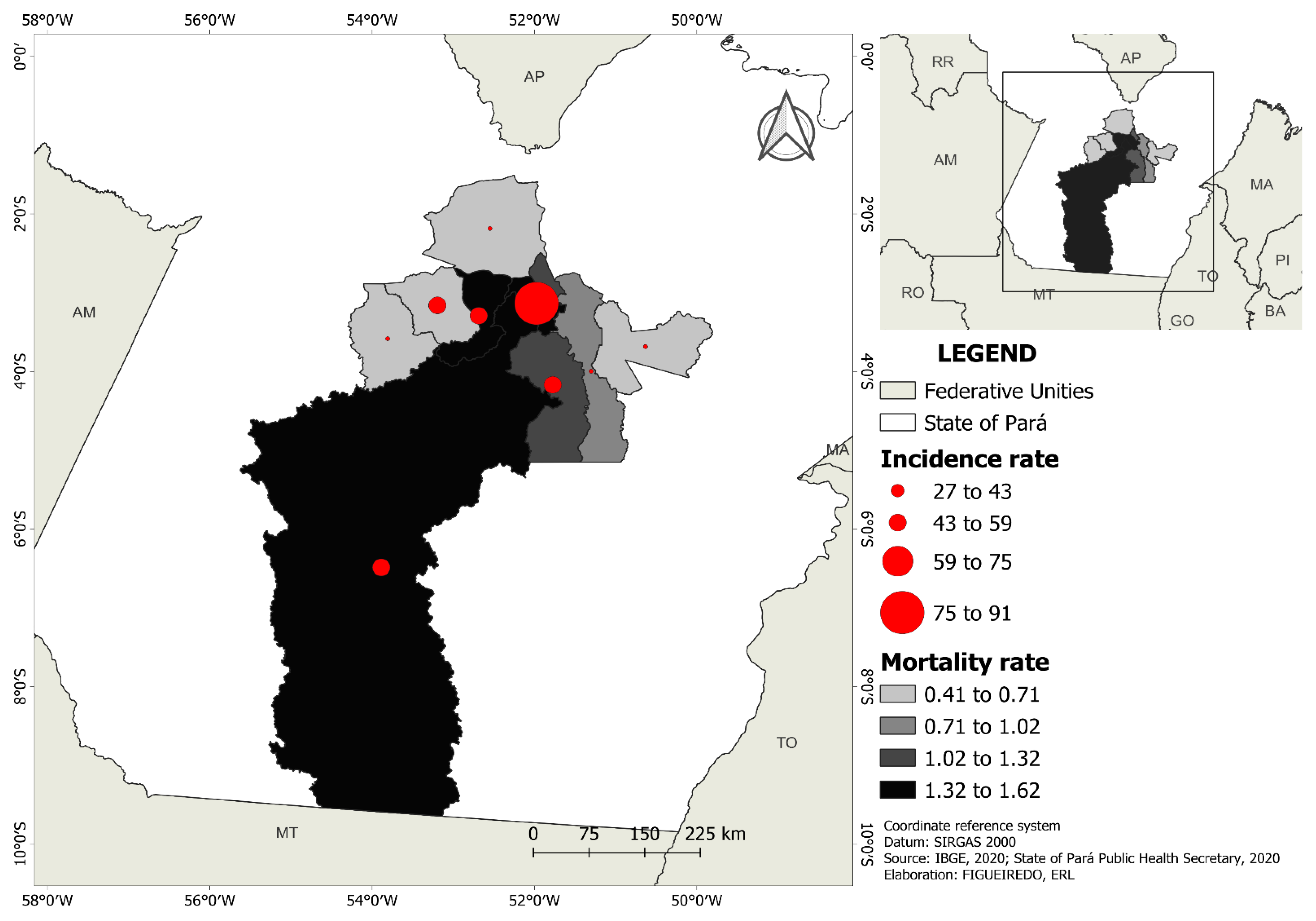
The incidence rate of COVID-19 per 1000 inhabitants in the Xingu Health Region was 45.59 and the mortality rate was 1.01. In descending order, the highest incidence rate was observed in Vitória do Xingu (90.84), followed by Altamira (56.83), Senador José Porfírio (56.62), Brasil Novo (54.19), Medicilândia (48.07), Anapu (39.75), Pacajá (33.07), Porto de Moz (28.66), and Uruará (26.94). However, most cases were reported in Altamira (41%), Pacajá (9.9%), and Medicilândia (9.5%). It was observed that 359 individuals did not survive being infected with COVID-19. In descending order, Altamira (1.62) showed the highest mortality rate, followed by Brasil Novo (1.47), Vitória do Xingu (1.44), Senador José Porfírio (1.31), Anapú (0.87), Porto de Moz (0.67), Medicilândia (0.63), Uruará (0.42), and Pacajá (0.41). Deaths were concentrated in Altamira (52%), Porto de Moz (7.8%), and Anapú (7%) (Figure 3).
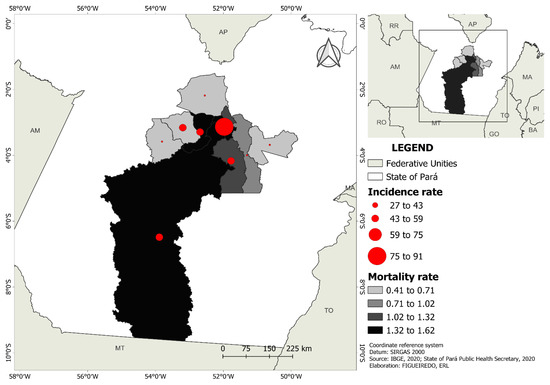
Figure 3.
Incidence and mortality rate distribution per 1000 inhabitants of municipalities in the Xingu Health Region.
3.1. Relationship among the SDH Indicators, Incidence, and Mortality
The incidence and mortality rates according to sex and SDH indicators in all municipalities in the Xingu Health Region are presented in Table 1.
When assessing the correlation of incidence and SDH indicators, correlations with the following variables were observed: GDP (rs = 0.8000, p = 0.013), percentage of people with health insurance (rs = 0.8000, p = 0.013), public health expenditure in the municipality (rs = 0.7667, p = 0.021), and percentage of the population residing in households with walls not made of masonry or wood (r = −0.6764, p = 0.040).
When assessing the correlation of mortality and SDH indicators, correlations with the following variables were observed: percentage of people with health insurance (rs = 0.8333, p = 0.008), public health expenditure in the municipality (rs = 0.7333, p = 0.030), and percentage of the population residing in households with walls not made of masonry or wood (r = −0.6812, p = 0.040). The other SDH indicators were not significant for incidence or mortality.
3.2. Sociodemographic Factors, Symptoms and Comorbidities as Predictors of Clinical Management
The sociodemographic factors associated with admission to a medical ward included age and residing in Brasil Novo. However, the female sex, residing in Uruará and Vitória do Xingu, and being locally diagnosed were associated with a lower chance of being admitted to a medical ward. Regarding symptoms, fever, cough, emesis, and dyspnea were associated with admission to a medical ward. Individuals with a headache, sore throat, myalgia, and arthralgia were less likely to be admitted to a medical ward. The predictive comorbidities for admission to a medical ward included diabetes, heart disease, neurological diseases, kidney diseases, and obesity (Table 2).

Table 2.
Sociodemographic factors, symptoms and comorbidities as predictors of admission to a medical ward in relation to home care.
The sociodemographic factors including advanced age and having an imported case were associated with admission to an ICU. However, the female sex and residing in the municipalities of Brasil Novo, Pacajá, and Vitória do Xingu, compared with Altamira, were protective factors for ICU admission (Table 3).

Table 3.
Sociodemographic factors, symptoms, and comorbidities as predictors of admission to intensive care units (ICU) compared with home care.
Emesis, chills, and dyspnea were predictors of ICU admission. However, patients with a headache and sore throat were less likely to be hospitalized. The comorbidities of diabetes, heart disease, and obesity were identified as risk factors for ICU admission (Table 3).
The predictors for admission to ICU were having an imported case, chills, dyspnea, and diabetes. The female sex and residing in the municipalities of Brasil Novo, Medicilândia, Pacajá, and Vitória do Xingu, in comparison with Altamira, were considered protective factors for ICU admission (Table 4).

Table 4.
Sociodemographic factors, symptoms, and comorbidities as predictors of admission to intensive care units (ICU) in relation to admission to a medical ward.
3.3. Sociodemographic Factors, Symptoms and Comorbidities as Predictors of Mortality
A total of 359 individuals (2.2 %) died due to being infected with COVID-19 during the study period. The sociodemographic factors predicting higher mortality included advanced age and residing in the municipality of Anapu. Having an imported case and residing in Pacajá were correlated with lower mortality rates. Individuals with dyspnea and fever had a higher risk of death. However, individuals with a sore throat and anosmia showed less association. Regarding comorbidities, heart disease was correlated with a higher chance of death. According to clinical management, patients admitted to ICU were most likely to die, followed by those admitted to a medical ward. Other variables did not present significant differences (Table 5).

Table 5.
Sociodemographic factors, symptoms and comorbidities as predictors of mortality.
3.4. Survival Analysis
Only the variable age group showed an association with COVID-19 survival, and individuals aged 60 years or older exhibited the lowest survival rate. The results of the Kaplan–Meier survival analysis conducted for COVID-19, according to sex, age group, home city, symptom, and commodity, are presented in Figure 4.
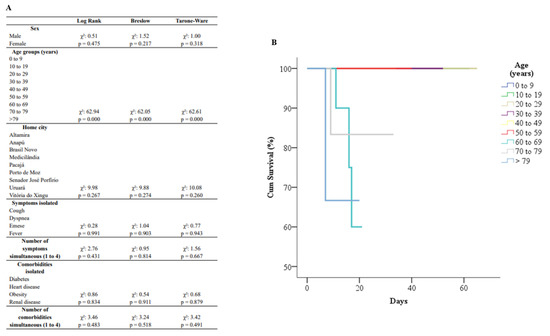
Figure 4.
Kaplan–Meier survival analysis for COVID-19 by sex, age groups, home city, symptoms and comorbidities (A); representation graphic for age groups (B).
4. Discussion
Amazonian communities continue to face particular challenges in relation to the COVID-19 pandemic, owing to the fact that each community has a different type of organizational structure and a different type of social and cultural behavior [44]. Moreover, in Brazil, the denialist administration of the federal government, which has operated without a unified policy to combat and control the COVID-19 disease, has reinforced historical structural inequalities and regional vulnerabilities [45]. This has adversely affected vulnerable populations in rural and remote areas as well as traditional peoples (indigenous peoples, forest peoples, quilombolas, and riverine peoples) who reside in the Brazilian Amazon [46]. Additionally, it must be noted that socioeconomic inequalities and limited access to health services can contribute to increased incidence and mortality [47].
The COVID-19 incidence rate distribution per 1000 inhabitants varied in each municipality of the Xingu Health Region, with the highest incidence rate in Vitória do Xingu (90.84) and the lowest incidence rate in Uruará (26.94). Vitória do Xingu is a port city, through which a significant number of individuals move to other municipalities of the Xingu region due to its connection with the Transamazonian region, as well as with the Amazon River, which differs from Uruará. This may explain the high incidence in this city. Port areas are common epicenters of disease transmission, as demonstrated by the outbreak of the Spanish influenza epidemic in the city of Recife, in northeast Brazil, in the early 20th century; the influenza virus in this case was transmitted via a British ship docked in the city port [48].
Regarding COVID-19 mortality, our study showed that 40.8% of the confirmed COVID-19 cases and 52% of deaths were reported in Altamira, in addition to residence in Altamira being a risk factor for ICU admission. Thus, the confirmed cases were distributed more between cities than mortality. The dependency illustrated the relationship between some Brazilian northern municipalities and highlighted how the virus spread intensely in a local city due to the influence of two other bigger cities [49]. Altamira is the urban center and most populous city of the Xingu Health Region, where the majority of healthcare professionals and specialized services are concentrated. Therefore, it can be supposed that for moderate or severe cases (more likely to evolve to death), these individuals sought healthcare in Altamira. Furthermore, these findings indicate that patients did not stay isolated in their houses but continued to travel between municipalities, especially due to the region’s economic characteristics, of which the export production chain occupies a significant percentage.
Vitória do Xingu and Altamira were the cities with the highest number of foreign cases and highest incidence rates. Similar findings were obtained for mortality, with the highest rates observed in Altamira, Brasil Novo, and Vitória do Xingu. The geography of the Xingu region could explain these findings. As can be seen in Figure 1, both cities are located on the Xingu River, and the existing ports in these cities simultaneously ship a variety of products and people. Despite this economic infrastructure and connection between these cities, wealth is not well distributed [50], and the COVID-19 pandemic started in cities with better socioeconomic conditions and subsequently migrated to more vulnerable local communities [51,52].
Confirming these results, positive correlations between incidence and GDP, the percentage of people with health insurance, and public health expenditure in the municipality were observed in this study. Additionally, a negative correlation was observed between incidence and the percentage of the population residing in households with walls not made of masonry or wood. A positive correlation was observed between the percentage of people with health insurance and public health spending in the municipality. Further, a negative correlation was observed between mortality and the percentage of the population residing in households with walls not made of masonry or wood. Healthcare workers, ICU beds, and mechanical ventilators, which are frequently needed in COVID-19 severe cases, are unequally distributed in Brazil [53,54]. Considering the above, it can be assumed that the spread of COVID-19 and its associated mortality were influenced by high SDH indicators in the economic, health, and resource sectors, as well as by interdependence between cities. Additionally, political and socioeconomic factors were critical to the spatial and temporal dynamics of COVID-19 outcomes in Brazil, especially in the first wave, in which the largest municipalities with a higher socioeconomic profile were the most affected [53]. It was also observed that the municipalities with better coverage indicators and health resources had higher incidence and mortality rates, suggesting misuse of these resources [54].
Considering sociodemographic characteristics, sex-disaggregated mortality and morbidity surveillance data should be a priority in COVID-19 research [55]. Sex differences in viral transmission and disease progression deserve explicit attention due to different levels of exposure between men and women; as comorbidities are usually more prevalent in men, this can be linked with evidence indicating that males are more associated with severely affected with COVID-19 and death [56]. It has also been suggested that the exposure of women to the COVID-19 virus may be higher than that of men, since frontline providers are generally women, comprising 70% of the global health and social care workforce [57]. This study’s results show that females formed the highest proportion in the group that stayed in home care and recovered, were less associated with the need for hospitalization, and were less likely to die. It is not yet well investigated whether biological differences [57] and lifestyle habits, or a combination of these, are the main factors associated with death due to COVID-19 among males.
We also found that older age was associated with the need for hospitalization and death. This can be attributed to the fact that the aging process leads to several changes that increase COVID-19 susceptibility, such as immunosenescence, changes in T-cell diversity, inflammation, a dysregulated renin-angiotensin system, changes in the glycome, advanced biological age, and epigenetic changes [58], that impair the autoimmunity of the individual in addition to the presence of comorbidities [59].
Despite the variety of symptoms investigated, fever, cough, and dyspnea were the most prevalent among patients who required hospitalization; this result is similar to other studies that evaluated symptomatic patients [60,61,62]. We observed that individuals with these symptoms and emesis were more likely to be hospitalized in a medical ward (moderate cases). Regarding ICU admission (severe cases), emesis, dyspnea, and chills remained as risk factors. Systematic and non-systematic reviews have reported that fever, dyspnea, chills, and gastrointestinal symptoms were associated with severe COVID-19 infection and ICU admission [63,64,65,66].
Additionally, headache, sore throat, and myalgia/arthralgia were less associated with the need for hospitalization and were consequently related to a better prognosis. In a systematic review and meta-analysis that investigated predictors and outcomes, an association between headache, myalgia/arthralgia, and COVID-19 severity was not observed [67], even though these were prevalent in many studies. This study shows that these symptoms were more prevalent in homecare cases and did not vary between those that needed hospitalization; therefore, it can be supposed that despite being cited in many studies, these symptoms did not present a risk factor in relation to illness severity.
Diabetes, heart disease, and obesity were consistently associated with the need for hospitalization, either in a medical ward or ICU. The existing literature provides sufficient evidence to support the role of each comorbidity as a risk factor for severe diseases [12,65,66,67,68]. Low-grade chronic inflammation, a compromised immune response, and prothrombotic status are the complications associated with diabetes and obesity [59]. In relation to heart disease, one of the phases of viral action is the inhibition of the Angiotensin 2-Converter enzyme (ECA-2), which could deregulate the renin-angiotensin-aldosterone system, causing local and systemic tissue lesions [68]. Additionally, kidney and neurological diseases were associated with the need for hospitalization in a medical ward. However, there have been limited studies on the association between preexisting kidney diseases and COVID-19, and most studies in the literature have shown that kidney-related conditions are associated with the risk of mortality [60,62,63,66,67,68]. In relation to neurological diseases, a systematic review has pointed out that mental and neurological disorders were associated with COVID-19 disease severity and further with mortality [69].
The literature provides differing evidence with respect to symptoms as predictors of death. However, this study found that individuals with fever or dyspnea were more likely to die. This finding is in line with that of a Nigerian retrospective cohort study [70]. However, systematic reviews have not observed any symptoms to be a factor associated with COVID-19 mortality [63,68]. Regarding baseline characteristics, such as age and the presence of comorbidities, this study found that older individuals with heart disease were more likely to die, and this is well-evidenced in the existing scientific literature [59,68].
By identifying the symptoms and comorbidities that are predictive of serious illness and ICU admission, risk stratification within health services becomes possible. This can lead to management changes and improvements in resource allocation efficiency for patients at a higher risk of serious infection from COVID-19. Such identification would also facilitate more informed discussions regarding the predicted clinical trajectory, allowing for more accurate and timely advanced care planning. Similarly, it would assist the public health response mechanism in controlling the spread of the disease since knowledge about the different prevalence and risks of various conditions can help to focus and adapt public health efforts [71].
The limitations of the present study include the limitations that accompany the process of conducting an ecological study: errors may arise in the filling out of patient data; the underreporting of cases in terms of race or ethnicity, which was not reported in the SESPA database; and a large amount of unknown or unreported data, which affects the reliability of the analysis. Nonetheless, despite these issues, the situation has improved in recent years in Brazil [72]. Another limitation of the ecological design is the acquisition of data on SDH indicators since these data are collected from different sources and different periods [21,36,37,38,39,40]. Although ecological research makes causal inferences about individuals based on group observations, this study can contribute to the evaluation of public health policies in the communities of the Xingu Health Region, especially in the area of clinical management and surveillance of COVID-19, and provide avenues for future studies using other methodological approaches.
5. Conclusions
Incidence and mortality were higher in the cities of Vitória do Xingu and Altamira. Additionally, it was found that a higher percentage of people with health insurance and higher public health expenditure in the municipality was associated with higher incidence and mortality. A higher GDP was associated with a higher incidence. The female sex was associated with better clinical management. Residence in Altamira was a risk factor for ICU admission. Symptoms and comorbidities that predicted worse clinical management included dyspnea, fever, emesis, chills, diabetes, cardiac and renal diseases, obesity, and neurological diseases. Headache, anosmia, sore throat, myalgia, and arthralgia were protective factors. With advancing age, patients with COVID-19 face a higher incidence, mortality, and lower survival rates.
Therefore, it can be concluded that SDH indicators, symptomatology, and comorbidities have direct implications for the incidence, mortality, and clinical management of COVID-19 in the Xingu Health Region in eastern Amazonia, Brazil.
Author Contributions
Conceptualization, E.R.L.F., M.V.d.G.A. and J.S.d.M.-N.; data curation, E.R.L.F., M.V.d.G.A. and J.S.d.M.-N.; formal analysis, R.J.J., F.d.C.G., M.C.F.d.S. and A.F.d.S.-J.; project administration, A.F.d.S.-J. and J.S.d.M.-N.; supervision, N.V.G., C.d.S.C.M. and J.S.d.M.-N.; validation, J.S.d.M.-N.; writing—original draft, E.R.L.F.; writing—review and editing, E.R.L.F. and J.S.d.M.-N. All authors have read and agreed to the published version of the manuscript.
Funding
This study received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study since the database used in this research contains only consolidated information, without identifying individuals.
Informed Consent Statement
This study analyzes secondary data from retrospective medical charts from the database of SESPA that followed ethical and approval guidelines established nationwide. Thus, the requirement of patient consent was waived for this study.
Data Availability Statement
All data were made available by the https://www.covid-19.pa.gov.br/#/ (accessed on 31 August 2022).
Conflicts of Interest
The authors declare no conflict of interest.
References
- Wuhan Municipal Health Commission Report of Clustering Pneumonia of Unknown Etiology in Wuhan City. Available online: http://wjw.wuhan.gov.cn/front/web/showDetail/2019123108989 (accessed on 28 November 2022).
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y.; et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China. JAMA 2020, 323, 1061–1069. [Google Scholar] [CrossRef] [PubMed]
- New-Type Coronavirus Causes Pneumonia in Wuhan: Expert. Available online: http://www.xinhuanet.com/english/2020-01/09/c_138690570.htm (accessed on 28 November 2022).
- Martellucci, C.A.; Flacco, M.E.; Cappadona, R.; Bravi, F.; Mantovani, L.; Manzoli, L. SARS-CoV-2 Pandemic: An Overview. Adv. Biol. Regul. 2020, 77, 100736. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Coronavirus Disease 2019 (COVID-19): Situation Report, 191. 2020. Available online: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200729-covid-19-sitrep-191.pdf?%20sfvrsn=2c327e9e2 (accessed on 28 November 2022).
- Sheleme, T.; Bekele, F.; Ayela, T. Clinical Presentation of Patients Infected with Coronavirus Disease 19: A Systematic Review. Infect. Dis. 2020, 13, 1178633720952076. [Google Scholar] [CrossRef] [PubMed]
- De Vito, A.; Geremia, N.; Fiore, V.; Princic, E.; Babudieri, S.; Madeddu, G. Clinical Features, Laboratory Findings and Predictors of Death in Hospitalized Patients with COVID-19 in Sardinia, Italy. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 7861–7868. [Google Scholar] [CrossRef]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical Features of Patients Infected with 2019 Novel Coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef]
- Vaira, L.A.; Deiana, G.; Fois, A.G.; Pirina, P.; Madeddu, G.; De Vito, A.; Babudieri, S.; Petrocelli, M.; Serra, A.; Bussu, F.; et al. Objective Evaluation of Anosmia and Ageusia in COVID-19 Patients: Single-Center Experience on 72 Cases. Head Neck 2020, 42, 1252–1258. [Google Scholar] [CrossRef]
- Guarneri, C.; Rullo, E.V.; Pavone, P.; Berretta, M.; Ceccarelli, M.; Natale, A.; Nunnari, G. Silent COVID-19: What Your Skin Can Reveal. Lancet Infect. Dis. 2021, 21, 24–25. [Google Scholar] [CrossRef]
- Guarneri, C.; Venanzi Rullo, E.; Gallizzi, R.; Ceccarelli, M.; Cannavò, S.P.; Nunnari, G. Diversity of Clinical Appearance of Cutaneous Manifestations in the Course of COVID-19. J. Eur. Acad. Dermatol. Venereol. 2020, 34, e449–e450. [Google Scholar] [CrossRef]
- Li, L.; Huang, T.; Wang, Y.; Wang, Z.; Liang, Y.; Huang, T.; Zhang, H.; Sun, W.; Wang, Y. COVID-19 Patients’ Clinical Characteristics, Discharge Rate, and Fatality Rate of Meta-analysis. J. Med. Virol. 2020, 92, 577. [Google Scholar] [CrossRef]
- Fiore, V.; De Vito, A.; Bagella, P.; Princic, E.; Mariani, A.A.; Denti, L.; Fois, A.G.; Madeddu, G.; Babudieri, S.; Maida, I. Effectiveness of Vitamin D Supplements among Patients Hospitalized for COVID-19: Results from a Monocentric Matched-Cohort Study. Healthcare 2022, 10, 956. [Google Scholar] [CrossRef]
- Rodriguez-Guerra, M.; Jadhav, P.; Vittorio, T.J. Current Treatment in COVID-19 Disease: A Rapid Review. Drugs Context 2021, 10. [Google Scholar] [CrossRef]
- World Health Organization. Coronavirus Disease (COVID-19) Pandemic. 2020. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019?adgroupsurvey={adgroupsurvey}&gclid%20CJWKCAIAJS2BBHACEIWALTBWZVX8ZRICAJ1U0HR6YIFNDW7HNHMCSKU__HKYOUNI79JUDSVMYFBSNROCZVIDOQUEQUENO101S101S10 (accessed on 28 November 2022).
- O’Connor, R.C.; Wetherall, K.; Cleare, S.; McClelland, H.; Melson, A.J.; Niedzwiedz, C.L.; O’Carroll, R.E.; O’Connor, D.B.; Platt, S.; Scowcroft, E.; et al. Mental Health and Well-Being during the COVID-19 Pandemic: Longitudinal Analyses of Adults in the UK COVID-19 Mental Health & Wellbeing Study. Br. J. Psychiatry 2021, 218, 326–333. [Google Scholar] [CrossRef]
- Lekamwasam, R.; Lekamwasam, S. Effects of COVID-19 Pandemic on Health and Wellbeing of Older People: A Comprehensive Review. Ann. Geriatr. Med. Res. 2020, 24, 166–172. [Google Scholar] [CrossRef]
- Wachtler, B.; Hoebel, J. Soziale Ungleichheit und COVID-19: Sozialepidemiologische Perspektiven auf die Pandemie. Gesundheitswesen 2020, 82, 670–675. [Google Scholar] [CrossRef]
- Codeço, C.T.; Dal’Asta, A.P.; Rorato, A.C.; Lana, R.M.; Neves, T.C.; Andreazzi, C.S.; Barbosa, M.; Escada, M.I.S.; Fernandes, D.A.; Rodrigues, D.L.; et al. Epidemiology, Biodiversity, and Technological Trajectories in the Brazilian Amazon: From Malaria to COVID-19. Front. Public Health 2021, 9, 945. [Google Scholar] [CrossRef]
- Rodrigues-Filho, J.L.; Abe, D.S.; Gatti-Junior, P.; Medeiros, G.R.; Degani, R.M.; Blanco, F.P.; Faria, C.R.L.; Campanelli, L.; Soares, F.S.; Sidagis-Galli, C.V.; et al. Spatial Patterns of Water Quality in Xingu River Basin (Amazonia) Prior to the Belo Monte Dam Impoundment. Braz. J. Biol. 2015, 75, 34–46. [Google Scholar] [CrossRef]
- IBGE. Cidades e Estados. 2022. Available online: https://www.ibge.gov.br/cidades-e-estados/ (accessed on 25 July 2022).
- Brasil. Decreto Nº 7508, de 28 de Junho de 2011, Regulamenta a Lei no 8.080, de 19 de Setembro de 1990, Para Dispor Sobre a Organização do Sistema Único de Saúde—SUS, o Planejamento da Saúde, a Assistência à Saúde e a Articulação Interfederativa, e dá Outras Providências. 2011; Diário Oficial da República Federativa do Brasil. Brasília, DF, 29/06/2011; p. 1. Available online: https://planalto.gov.br/ccivil_03/_ato2011-2014/2011/decreto/d7508. (accessed on 25 July 2022).
- Santos, L. Região de saúde e suas redes de atenção: Modelo organizativo-sistêmico do SUS. Ciênc. Saúde Coletiva 2017, 22, 1281–1289. [Google Scholar] [CrossRef]
- da Silva Junior, O.M.; dos Santos, M.A.; Szlafsztein, C.F.; Gomez, J.M.A.; Pereira, J.P. Protected Areas as Strategies for Preserving Vegetation Cover in the Vicinity of Hydroelectric Projects in the Brazilian Amazon. Energ. Sustain. Soc. 2018, 8, 33. [Google Scholar] [CrossRef]
- Lucena, M.D.L.D.; Pereira, T.D.S.; Gonçalves, A.P.; Silva, K.D.; Sousa, L.M.D. Diversity of Loricariidae (Actinopterygii: Siluriformes) Assemblages in Two Conservation Areas of the Middle Xingu River, Brazilian Amazon, and Their Suitability for Sustainable Ornamental Fisheries. Neotrop. Ichthyol. 2021, 19. [Google Scholar] [CrossRef]
- Floss, M.; Franco, C.M.; Malvezzi, C.; Silva, K.V.; Costa, B.D.R.; Silva, V.X.D.L.; Werreria, N.S.; Duarte, D.R. A Pandemia de COVID-19 Em Territórios Rurais e Remotos: Perspectiva de Médicas e Médicos de Família e Comunidade Sobre a Atenção Primária à Saúde. Cad. Saúde Pública 2020, 36, 9–13. [Google Scholar] [CrossRef]
- Bambra, C.; Riordan, R.; Ford, J.; Matthews, F. The COVID-19 Pandemic and Health Inequalities. J. Epidemiol. Community Health 2020, 74, 964–968. [Google Scholar] [CrossRef] [PubMed]
- Caron, R.M.; Adegboye, A.R.A. COVID-19: A Syndemic Requiring an Integrated Approach for Marginalized Populations. Front. Public Health 2021, 9, 515. [Google Scholar] [CrossRef] [PubMed]
- Piroth, L.; Cottenet, J.; Mariet, A.-S.; Bonniaud, P.; Blot, M.; Tubert-Bitter, P.; Quantin, C. Comparison of the Characteristics, Morbidity, and Mortality of COVID-19 and Seasonal Influenza: A Nationwide, Population-Based Retrospective Cohort Study. Lancet Respir. Med. 2021, 9, 251–259. [Google Scholar] [CrossRef] [PubMed]
- Eslava-Castañeda, J.C. Pensando la determinación social del proceso salud-enfermedad. Rev. Salud Pública 2017, 9, 396–403. [Google Scholar] [CrossRef] [PubMed]
- Mena, G.E.; Martinez, P.P.; Mahmud, A.S.; Marquet, P.A.; Buckee, C.O.; Santillana, M. Socioeconomic Status Determines COVID-19 Incidence and Related Mortality in Santiago, Chile. Science 2021, 372, eabg5298. [Google Scholar] [CrossRef]
- Khanijahani, A.; Iezadi, S.; Gholipour, K.; Azami-Aghdash, S.; Naghibi, D. A Systematic Review of Racial/Ethnic and Socioeconomic Disparities in COVID-19. Int. J. Equity Health 2021, 20, 248. [Google Scholar] [CrossRef]
- Meyerowitz, E.A.; Richterman, A.; Gandhi, R.T.; Sax, P.E. Transmission of SARS-CoV-2: A Review of Viral, Host, and Environmental Factors. Ann. Intern. Med. 2021, 174, 69–79. [Google Scholar] [CrossRef]
- Quesada, J.A.; López-Pineda, A.; Gil-Guillén, V.F.; Arriero-Marín, J.M.; Gutiérrez, F.; Carratala-Munuera, C. Incubation Period of COVID-19: A Systematic Review and Meta-Analysis. Rev. Clínica Española 2021, 221, 109–117. [Google Scholar] [CrossRef]
- Lim, J.; Lee, J. Current Laboratory Diagnosis of Coronavirus Disease 2019. Korean J. Intern. Med. 2020, 35, 741. [Google Scholar] [CrossRef]
- SESPA. Available online: https://www.covid-19.pa.gov.br. (accessed on 31 August 2022).
- IBGE. Cidades e Estados. 2022. Available online: https://cidades.ibge.gov.br/brasil/pa/ (accessed on 28 July 2022).
- Ministério da Saúde. Cobertura da Atenção Básica (e-Gestor). 2022. Available online: https://egestorab.saude.gov.br/paginas/acessoPublico/relatorios/relHistoricoCoberturaACS.xhtml (accessed on 28 July 2022).
- Ministério da Saúde. Cobertura de Agentes Comunitários de Saúde (e-Gestor). 2022. Available online: https://egestorab.saude.gov.br/paginas/acessoPublico/relatorios/relHistoricoCoberturaACS.xhtml. (accessed on 28 July 2022).
- INPE. Open Data. 2022. Available online: https://www.gov.br/inpe/pt-br/acesso-a-info. (accessed on 31 July 2022).
- Tonin, F.S.; Araujo, A.G.; Fachi, M.M.; Ferreira, V.L.; Pontarolo, R.; Fernandez-Llimos, F. Lag Times in the Publication of Network Meta-Analyses: A Survey. BMJ Open 2021, 11, e048581. [Google Scholar] [CrossRef]
- Whitehead, M.; Dahlgren, G. Concepts and Principles for Tackling Social Inequities in Health: Levelling up Part 1. World Health Organ. Stud. Soc. Econ. Determ. Popul. Health 2006, 2, 460–474. [Google Scholar]
- Conselho Nacional de Saúde. Resolução 510, de 7 de Abril de 2016. Diário Oficial da União. 2016. Available online: https://bvsms.saude.gov.br/bvs/saudelegis/cns/2016/res0510_07_04_2016.html (accessed on 21 July 2022).
- Vallinoto, A.C.R.; da Silva Torres, M.K.; Vallinoto, M.C.; Cayres Vallinoto, I.M.V. The Challenges of COVID-19 in the Brazilian Amazonian Communities and the Importance of Seroepidemiological Surveillance Studies. Int. J. Equity Health 2020, 19, 140. [Google Scholar] [CrossRef]
- Ferrante, L.; Steinmetz, W.A.; Almeida, A.C.L.; Leão, J.; Vassão, R.C.; Tupinambás, U.; Fearnside, P.M.; Duczmal, L.H. Brazil’s Policies Condemn Amazonia to a Second Wave of COVID-19. Nat. Med. 2020, 26, 1315. [Google Scholar] [CrossRef]
- Ortega, F.; Orsini, M. Governing COVID-19 without Government in Brazil: Ignorance, Neoliberal Authoritarianism, and the Collapse of Public Health Leadership. Glob. Public Health 2020, 15, 1257–1277. [Google Scholar] [CrossRef]
- Lima, E.E.C.D.; Gayawan, E.; Baptista, E.A.; Queiroz, B.L. Spatial Pattern of COVID-19 Deaths and Infections in Small Areas of Brazil. PLoS ONE 2021, 16, e0246808. [Google Scholar] [CrossRef]
- Bertolli Filho, C. A Gripe Espanhola em São Paulo, 1918: Epidemia e Sociedade; Paz e Terra, Santa Ifigênia: São Paulo, Brazil, 2003; p. 393. Available online: https://pesquisa.bvsalud.org/portal/resource/pt/lil-384570.
- Pacífico Filho, M.; Borges, T.P.; Iwamoto, H.M.; Cançado, A.C. COVID-19 in the legal Amazon. Mercator 2021, 20. [Google Scholar] [CrossRef]
- Castro, F.d.; Lopes, G.R.; Brondizio, E.S. The Brazilian Amazon in Times of COVID-19: From Crisis to Transformation? Ambient. Soc. 2020, 23, 1–11. [Google Scholar] [CrossRef]
- Figueiredo, A.M.D.; Figueiredo, D.C.M.M.D.; Gomes, L.B.; Massuda, A.; Gil-García, E.; Vianna, R.P.D.T.; Daponte, A. Social Determinants of Health and COVID-19 Infection in Brazil: An Analysis of the Pandemic. Rev. Bras. Enferm. 2020, 73. [Google Scholar] [CrossRef]
- Borges, G.M.; Crespo, C.D. Demographic and Socioeconomic Characteristics of Brazilian Adults and COVID-19: A Risk Group Analysis Based on the Brazilian National Health Survey, 2013. Cad. Saúde Pública 2020, 36. [Google Scholar] [CrossRef]
- Xavier, D.R.; Lima e Silva, E.; Lara, F.A.; e Silva, G.R.R.; Oliveira, M.F.; Gurgel, H.; Barcellos, C. Involvement of Political and Socio-Economic Factors in the Spatial and Temporal Dynamics of COVID-19 Outcomes in Brazil: A Population-Based Study. Lancet Reg. Health Am. 2022, 10, 100221. [Google Scholar] [CrossRef]
- Funcia, F.; Bresciani, L.P.; Benevides, R.; Ocké-Reis, C.O. Análise do financiamento federal do Sistema Único de Saúde para o enfrentamento da Covid-19. Saúde Debate 2022, 46, 263–276. [Google Scholar] [CrossRef]
- Hall, K.S.; Samari, G.; Garbers, S.; Casey, S.E.; Diallo, D.D.; Orcutt, M.; Moresky, R.T.; Martinez, M.E.; McGovern, T. Centring Sexual and Reproductive Health and Justice in the Global COVID-19 Response. Lancet 2020, 395, 1175–1177. [Google Scholar] [CrossRef] [PubMed]
- Galbadage, T.; Peterson, B.M.; Awada, J.; Buck, A.S.; Ramirez, D.A.; Wilson, J.; Gunasekera, R.S. Systematic Review and Meta-Analysis of Sex-Specific COVID-19 Clinical Outcomes. Front. Med. 2020, 7, 348. [Google Scholar] [CrossRef] [PubMed]
- Wehbe, Z.; Hammoud, S.H.; Yassine, H.M.; Fardoun, M.; El-Yazbi, A.F.; Eid, A.H. Molecular and Biological Mechanisms Underlying Gender Differences in COVID-19 Severity and Mortality. Front. Immunol. 2021, 12, 1603. [Google Scholar] [CrossRef] [PubMed]
- Mueller, A.L.; McNamara, M.S.; Sinclair, D.A. Why Does COVID-19 Disproportionately Affect Older People? Aging 2020, 12, 9959. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Ding, M.; Dong, X.; Zhang, J.; Kursat Azkur, A.; Azkur, D.; Gan, H.; Sun, Y.; Fu, W.; Li, W.; et al. Risk Factors for Severe and Critically Ill COVID-19 Patients: A Review. Allergy 2021, 76, 428–455. [Google Scholar] [CrossRef]
- Li, H.; Burm, S.W.; Hong, S.H.; Ghayda, R.A.; Kronbichler, A.; Smith, L.; Koyanagi, A.; Jacob, L.; Lee, K.H.; Shin, J.I. A Comprehensive Review of Coronavirus Disease 2019: Epidemiology, Transmission, Risk Factors, and International Responses. Yonsei Med. J. 2021, 62, 1–11. [Google Scholar] [CrossRef]
- Jain, V.; Yuan, J.-M. Predictive Symptoms and Comorbidities for Severe COVID-19 and Intensive Care Unit Admission: A Systematic Review and Meta-Analysis. Int. J. Public Health 2020, 65, 533–546. [Google Scholar] [CrossRef]
- Nasir, N.; Habib, K.; Khanum, I.; Khan, N.; Muhammad, Z.A.; Mahmood, S.F. Clinical Characteristics and Outcomes of COVID-19: Experience at a Major Tertiary Care Center in Pakistan. J. Infect. Dev. Ctries. 2021, 15, 480–489. [Google Scholar] [CrossRef]
- Setiati, S.; Harimurti, K.; Safitri, E.D.; Ranakusuma, R.W.; Saldi, S.R.F.; Azwar, M.K.; Marsigit, J.; Pitoyo, Y.; Widyaningsih, W. Risk Factors and Laboratory Test Results Associated with Severe Illness and Mortality in COVID-19 Patients: A Systematic Review. Acta Med. Indones 2020, 52, 227–245. [Google Scholar]
- Yang, J.; Zheng, Y.; Gou, X.; Pu, K.; Chen, Z.; Guo, Q.; Ji, R.; Wang, H.; Wang, Y.; Zhou, Y. Prevalence of Comorbidities and Its Effects in Patients Infected with SARS-CoV-2: A Systematic Review and Meta-Analysis. Int. J. Infect. Dis. 2020, 94, 91–95. [Google Scholar] [CrossRef]
- Kipourou, D.-K.; Leyrat, C.; Alsheridah, N.; Almazeedi, S.; Al-Youha, S.; Jamal, M.H.; Al-Haddad, M.; Al-Sabah, S.; Rachet, B.; Belot, A. Probabilities of ICU Admission and Hospital Discharge According to Patient Characteristics in the Designated COVID-19 Hospital of Kuwait. BMC Public Health 2021, 21, 799. [Google Scholar] [CrossRef]
- Fang, X.; Li, S.; Yu, H.; Wang, P.; Zhang, Y.; Chen, Z.; Li, Y.; Cheng, L.; Li, W.; Jia, H.; et al. Epidemiological, Comorbidity Factors with Severity and Prognosis of COVID-19: A Systematic Review and Meta-Analysis. Aging 2020, 12, 12493. [Google Scholar] [CrossRef]
- Bonow, R.O.; O’Gara, P.T.; Yancy, C.W. Cardiology and COVID-19. JAMA 2020, 324, 1131–1132. [Google Scholar] [CrossRef]
- Li, J.; Huang, D.Q.; Zou, B.; Yang, H.; Hui, W.Z.; Rui, F.; Yee, N.T.S.; Liu, C.; Nerurkar, S.N.; Kai, J.C.Y.; et al. Epidemiology of COVID-19: A Systematic Review and Meta-Analysis of Clinical Characteristics, Risk Factors, and Outcomes. J. Med. Virol. 2021, 93, 1449–1458. [Google Scholar] [CrossRef]
- Liu, L.; Ni, S.-Y.; Yan, W.; Lu, Q.-D.; Zhao, Y.-M.; Xu, Y.-Y.; Mei, H.; Shi, L.; Yuan, K.; Han, Y.; et al. Mental and Neurological Disorders and Risk of COVID-19 Susceptibility, Illness Severity and Mortality: A Systematic Review, Meta-Analysis and Call for Action. EClinicalMedicine 2021, 40, 101111. [Google Scholar] [CrossRef]
- Elimian, K.O.; Ochu, C.L.; Ebhodaghe, B.; Myles, P.; Crawford, E.E.; Igumbor, E.; Ukponu, W.; Olayinka, A.; Aruna, O.; Dan-Nwafor, C.; et al. Patient Characteristics Associated with COVID-19 Positivity and Fatality in Nigeria: Retrospective Cohort Study. BMJ Open 2020, 10, e044079. [Google Scholar] [CrossRef]
- Talic, S.; Shah, S.; Wild, H.; Gasevic, D.; Maharaj, A.; Ademi, Z.; Li, X.; Xu, W.; Mesa-Eguiagaray, I.; Rostron, J.; et al. Effectiveness of Public Health Measures in Reducing the Incidence of Covid-19, SARS-CoV-2 Transmission, and Covid-19 Mortality: Systematic Review and Meta-Analysis. BMJ 2021, 375, e068302. [Google Scholar] [CrossRef]
- Affonso, M.V.D.G.; Souza, I.G.; Rocha, E.S.d.; Goloni-Bertollo, E.M.; Gomes, F.D.C.; Nascimento, L.S.d.; Melo-Neto, J.S.d. Association between Sociodemographic Factors, Coverage and Offer of Health Services with Mortality Due to Oral and Oropharyngeal Cancer in Brazil: A 20-Year Analysis. Int. J. Environ. Res. Public Health 2022, 19, 13208. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).