Analysis of the Mental and Physical Health Symptomatology Scale in a Sample of Emerging and Migrant Adults in Chile
Abstract
1. Introduction
1.1. Vulnerable Groups: Emerging Adults and Migrants
1.2. Instruments to Assess the State of Mental and Physical Health
2. Study 1
2.1. Participants
2.2. Measures
2.3. Procedures
2.4. Analysis
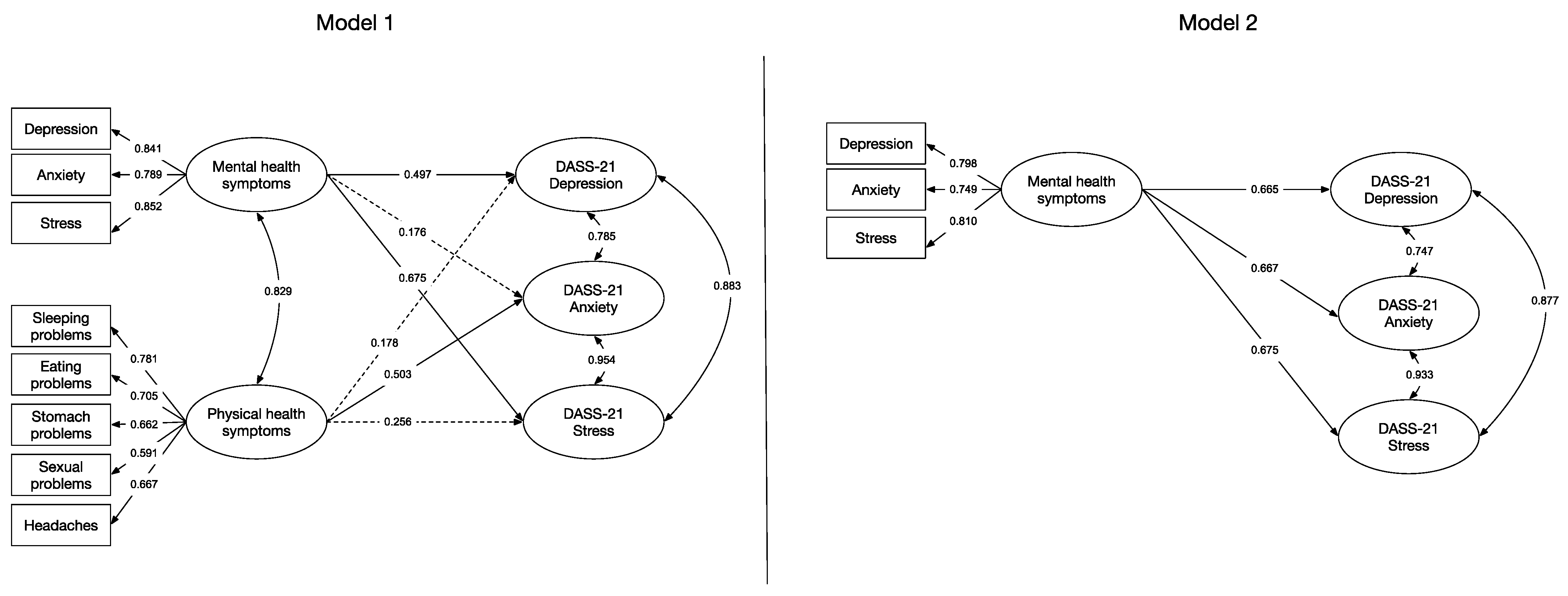
2.5. Results
3. Study 2
3.1. Participants
3.2. Instruments
3.3. Procedures
3.4. Analysis
3.5. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Gobernanza. In Constitución. Available online: https://www.who.int/es/about/governance/constitution (accessed on 5 January 2023).
- Morrison, V.; Bennett, P. Psicología de la Salud, 1st ed.; Pearson: Madrid, España, 2008. [Google Scholar]
- Manríquez-Robles, D. Los desafíos en la salud mental de los trabajadores de la salud durante y post pandemia SARS-CoV-2. Rev. Chil. Salud Pública 2022, 26, 112–113. [Google Scholar] [CrossRef]
- Pan American Health Organization. The Burden of Mental Disorders in the Region of the Americas; Pan American Health Organization Press: Washington, DC, USA, 2018; Available online: https://iris.paho.org/handle/10665.2/49578 (accessed on 26 January 2023).
- Manríquez-Robles, D. El derecho a la salud mental en la nueva constitución. Una discusión inmediata. In Una Nueva Constitución. Una Propuesta Desde La Araucanía; Carrasco, C., Quiroz, C., Eds.; Ediciones UC Temuco: Temuco, Chile, 2021; pp. 237–245. Available online: https://ediciones.uct.cl/una-nueva-constitucion/ (accessed on 26 January 2023).
- World Health Organization. Notas descriptivas. In Trastornos Mentales. Available online: https://www.who.int/es/news-room/fact-sheets/detail/mental-disorders (accessed on 15 November 2022).
- Ministerio de Salud de Chile. Plan Nacional de Salud Mental 2017–2025, 1st ed.; Ministerio de Salud de Chile: Santiago, Chile, 2017. [Google Scholar]
- Manríquez-Robles, D. Los desafíos en la cobertura, acceso y calidad de la atención en salud mental durante la pandemia por SARS-CoV-2. Rev. Chil. Salud Pública 2022, 25, 257–258. [Google Scholar] [CrossRef]
- Cortés-Gabaudan, F. Dicciomed: Diccionario Médico-Biológico, Histórico Y Etimológico. Available online: https://dicciomed.usal.es/palabra/ascitis (accessed on 25 January 2023).
- González, M.; Landero, R.; García-Campayo, J. Relación entre la depresión, La ansiedad y los síntomas psicosomáticos en una muestra de estudiantes universitarios del norte de México. Rev. Panam. Salud Publica 2009, 25, 141–145. Available online: https://iris.paho.org/handle/10665.2/9873 (accessed on 26 January 2023). [CrossRef]
- Ministerio de Salud de Chile. Encuesta Nacional De Salud 2016–2017. In Segunda Entrega de Resultados, 1st ed.; Ministerio de Salud de Chile: Santiago, Chile, 2018. [Google Scholar]
- Abuín, M.R.; Rivera, L. La medición de síntomas psicológicos y psicosomáticos: El Listado de Síntomas Breve (LSB-50). Clin. Salud 2014, 25, 131–141. [Google Scholar] [CrossRef]
- Jones, G. Psychosocial vulnerability and early life adversity as risk factors for central sensitivity syndromes. Curr. Rheumatol. Rev. 2016, 12, 140–153. [Google Scholar] [CrossRef] [PubMed]
- Instituto Nacional de la Juventud. X Encuesta nacional de Juventudes 2022. In Gobierno de Chile, 1st ed.; Ministerio de Desarrollo Social y Familia de Chile: Santiago, Chile, 2022. [Google Scholar]
- Arnett, J.J. The Oxford Handbook of Emerging Adulthood, 1st ed.; Oxford University Press: Oxford, UK, 2015. [Google Scholar]
- Arnett, J.J. Adolescencia Y Adultez Emergente: Un Enfoque Cultural, 3rd ed.; Pearson Educación: London, UK, 2008. [Google Scholar]
- Barrera-Herrera, A.; Vinet, E.V. Adultez emergente y características culturales de la etapa en universitarios chilenos. Ter. Psicol. 2017, 35, 47–56. [Google Scholar] [CrossRef]
- Arnett, J.J. Emerging adulthood: A theory of development from the late teens through the twenties. Am. Psychol. 2000, 55, 469–480. Available online: https://psycnet.apa.org/doi/10.1037/0003-066X.55.5.469 (accessed on 26 January 2023). [CrossRef]
- Barrera-Hererra, A.; San Martín, Y. Prevalencia de sintomatología de salud mental y hábitos de salud en una muestra de universitarios chilenos. Psykhe (Santiago) 2021, 30, 1–16. [Google Scholar] [CrossRef]
- Arnett, J.J.; Žukauskienė, R.; Sugimura, K. The new life stage of emerging adulthood at ages 18–29 years: Implications for mental health. Lancet Psychiatry 2014, 1, 569–576. [Google Scholar] [CrossRef]
- Micin, S.; Bagladi, V. Salud Mental En estudiantes universitarios: Incidencia de psicopatología y antecedentes de conducta suicida en población que acude a un servicio de salud estudiantil. Ter. Psicol. 2011, 29, 53–64. [Google Scholar] [CrossRef]
- Baader, T.; Rojas, C.; Molina, J.; Gotelli, M.; Alamo, C.; Fierro, C.; Venezian, S.; Dittus, P. Diagnóstico de la prevalencia de trastornos de la salud mental en estudiantes universitarios y los factores de riesgo emocionales asociados. Rev. Chil. Neuropsiquiatr. 2014, 52, 167–176. [Google Scholar] [CrossRef]
- Stallman, H.M.; Shochet, I. Prevalence of mental health problems in australian university health services. Aust. Psychol. 2009, 44, 122–127. [Google Scholar] [CrossRef]
- Arrieta-Vergara, K.M.; Díaz-Cárdenas, S.; González-Martínez, F. Síntomas de depresión y ansiedad en jóvenes universitarios: Prevalencia y factores relacionados. Rev. Clin. Med. Fam. 2014, 7, 14–22. [Google Scholar] [CrossRef]
- World Health Organization. Notas descriptivas. In Salud del Adolescente y el Joven Adulto. Available online: https://www.who.int/es/news-room/fact-sheets/detail/adolescents-health-risks-and-solutions (accessed on 25 January 2022).
- United Nations Department of Economic and Social Affairs. International Migrant Stock. Available online: https://www.un.org/development/desa/pd/content/international-migrant-stock (accessed on 25 January 2022).
- Avaria, A.; Cabieses, B.; Obach, A. Salud y Migraciones. Relevancia, Consideraciones Generales y Desafíos Para el Chile de Hoy, 1st ed.; RIL Editores: Santiago, Chile, 2021. [Google Scholar]
- Charlson, F.; van Ommeren, M.; Flaxman, A.; Cornett, J.; Whiteford, H.; Saxena, S. New WHO prevalence estimates of mental disorders in conflict settings: A systematic review and meta-analysis. Lancet 2019, 394, 240–248. [Google Scholar] [CrossRef]
- International Organization for Migration. World Migration Report 2022; International Organization for Migration Press: Geneva, Switzerland, 2021; Available online: https://publications.iom.int/books/world-migration-report-2022 (accessed on 26 January 2023).
- Baeza-Rivera, M.J.; Salinas-Oñate, N.; Salazar-Fernández, C.; Larenas-Said, J.; Araneda-Leal, L. Inmigración en La Araucanía, ¿Cómo viven este proceso haitianos, colombianos y venezolanos? Rev. Psicol. 2022, 31, 42–53. [Google Scholar] [CrossRef]
- Baeza-Rivera, M.J.; Salazar-Fernández, C.; Manríquez-Robles, D.; Salinas-Oñate, N.; Smith-Castro, V. Acculturative stress, perceived social support, and mental health: The mediating effect of negative emotions associated with discrimination. Int. J. Environ. Res. Public Health 2022, 19, 16522. [Google Scholar] [CrossRef]
- Urzúa, A.; Heredia, O.; Caqueo-Urízar, A. Mental health and stress by acculturation in immigrants from South America in northern Chile. Rev. Med. Chil. 2016, 144, 563–570. [Google Scholar] [CrossRef]
- Urzúa, A.; Basabe, N.; Pizarro, J.; Ferrer, R. Afrontamiento del estrés por aculturación: Inmigrantes latinos en Chile. Univ. Psychol. 2018, 16, 1–13. [Google Scholar] [CrossRef]
- Urzúa, A.; Leiva-Gutiérrez, J.; Caqueo-Urízar, A.; Vera-Villarroel, P. Rooting mediates the effect of stress by acculturation on the psychological well-being of immigrants living in Chile. PLoS ONE 2019, 14, e0219485. [Google Scholar] [CrossRef]
- Urzúa, A.; Henríquez, D.; Caqueo-Urízar, A.; Smith-Castro, V. Validation of the brief scale for the evaluation of acculturation stress in migrant population (EBEA). Psicol-Reflex Crit. 2021, 34, 3. [Google Scholar] [CrossRef]
- Urzúa, A.; Ferrer, R.; Canales-Gaete, V.; Núñez-Aragón, D.; Ravanal-Labraña, I.; Tabilo-Poblete, B. The influence of acculturation strategies in quality of life by immigrants in northern Chile. Qual. Life Res. 2017, 26, 717–726. [Google Scholar] [CrossRef] [PubMed]
- Rojas, G.; Fritsch, R.; Castro, A.; Guajardo, V.; Torres, P.; Díaz, B. Trastornos mentales comunes y uso de servicios de salud en población inmigrante. Rev. Med. Chil. 2011, 139, 1298–1304. [Google Scholar] [CrossRef] [PubMed]
- Fajardo, M.; Patiño, M.; Patiño, C. Estudios actuales sobre aculturación y salud mental en inmigrantes: Revisión y perspectivas. Rev. Iberoam. Psicol. Cienc. Tecnol. 2008, 1, 39–50. [Google Scholar]
- Sánchez, G.; López, M. Ansiedad y modos de aculturación en la población inmigrante. Apunt. Psicol. 2008, 26, 399–410. Available online: http://hdl.handle.net/11441/59345 (accessed on 26 January 2023).
- Bekteshi, V.; van Hook, M. Contextual approach to acculturative stress among latina immigrants in the U.S. J. Immigr. Minor. Health 2015, 17, 1401–1411. [Google Scholar] [CrossRef]
- Antúnez, Z.; Vinet, E.V. Escalas de Depresión, Ansiedad y Estrés (DASS-21): Validación de la versión abreviada en estudiantes universitarios chilenos. Ter. Psicol. 2012, 30, 49–55. [Google Scholar] [CrossRef]
- Baader, T.; Molina, J.; Venezian, S.; Rojas, C.; Farías, R.; Fierro-Freixenet, C.; Backenstrass, M.; Mundt, C. Validación y utilidad de la encuesta PHQ-9 (Patient Health Questionnaire) en el diagnóstico de depresión en pacientes usuarios de atención primaria en Chile. Rev. Chil. Neuropsiquiatr. 2012, 50, 10–22. [Google Scholar] [CrossRef]
- Pérez-Villalobos, C.; Bonnefoy-Dibarrat, C.; Cabrera-Flores, A.; Peine-Grandón, S.; Abarca, K.M.; Baqueano-Rodríguez, M.; Jiménez-Espinoza, J. Problemas de salud mental en alumnos universitarios de primer año de Concepción, Chile. An. Psicol. 2012, 28, 797–804. [Google Scholar] [CrossRef]
- Antúnez, Z.; Vinet, E.V. Problemas de salud mental en estudiantes de una universidad regional chilena. Rev. Med. Chil. 2013, 141, 209–216. [Google Scholar] [CrossRef]
- Fritsch, R.; Escanilla, X.; Goldsack, V.; Grinberg, A.; Navarrete, A.; Pérez, A.; Rivera, C.; Gonzalez, I.; Sepúlveda, R.; Rojas, G. Diferencias de género en el malestar psíquico de estudiantes universitarios. Rev. Psiquiatr. Clín. 2016, 43, 22–30. Available online: https://pesquisa.bvsalud.org/portal/resource/pt/lil-444128 (accessed on 26 January 2023).
- Concepcion, T.; Barbosa, C.; Vélez, J.C.; Pepper, M.; Andrade, A.; Gelaye, B.; Yanez, D.; Williams, M.A. Daytime sleepiness, poor sleep quality, eveningness chronotype, and common mental disorders among chilean college students. J. Am. Coll. Health 2014, 62, 441–448. [Google Scholar] [CrossRef] [PubMed]
- Cova, S.F.; Melipillán, A.R.; Valdivia, P.M.; Bravo, G.E.; Valenzuela, Z.B. Sintomatología depresiva y ansiosa en estudiantes de enseñanza media. Rev. Chil. Pediatr. 2007, 78, 151–159. [Google Scholar] [CrossRef]
- Cova, F.; Alvial, W.; Aro, M.; Bonifetti, A.; Hernández, M.; Rodríguez, C. Problemas de salud mental en estudiantes de la Universidad de Concepción. Ter. Psicol. 2007, 25, 105–112. [Google Scholar] [CrossRef]
- Muñoz-Carreño, N.; Robledo-Robledo, V. Síndromes y trastornos clínicos diagnosticados en un centro universitario de atención psicológica 2013–2016. Rev. Acad. UC Maule 2017, 52, 9–24. [Google Scholar] [CrossRef]
- Villacura, L.; Irarrázabal, N.; Dörr, A.; Zamorano, C.; Manosalva, J.; Cánovas, C.; Zamorano, M.; Barra, N. Mental Disorders of Students at the University of Chile. Ment. Health Prev. 2015, 3, 21–25. [Google Scholar] [CrossRef]
- Yáñez, S.; Cárdenas, M. Acculturation strategies, indicators of mental health and psychological well-being in a group of south american immigrants in Chile. Salud Soc. 2010, 1, 51–70. [Google Scholar] [CrossRef]
- Urzúa, A.; Vega, M.; Jara, A.; Trujillo, S.; Muñoz, R.; Caqueo-Urízar, A. Calidad de vida percibida en inmigrantes sudamericanos en el norte de Chile. Ter. Psicol. 2015, 33, 139–156. [Google Scholar] [CrossRef]
- Gómez, S.; Astete, V.; Infante, B.; Muñoz, C.; Florenzano, R. Aplicación de la entrevista de formulación cultural del DSM 5. Rev. GPU 2016, 12, 359–364. [Google Scholar]
- Arancibia, H. Validation of the Positive and Negative Affect Scale in the chilean population and its application on migrant people. Medwave 2019, 19, e7579. [Google Scholar] [CrossRef]
- Oei, T.P.S.; Sawang, S.; Goh, Y.W.; Mukhtar, F. Using the Depression Anxiety Stress Scale 21 (DASS-21) across cultures. Int. J. Psychol. 2013, 48, 1018–1029. [Google Scholar] [CrossRef]
- García, J.; Sanz, C. Salud mental en inmigrantes: El nuevo desafío. Med. Clin. 2002, 118, 187–191. [Google Scholar] [CrossRef] [PubMed]
- Soper, D. A-Priori Sample Size Calculator for Structural Equation Models. Available online: https://www.danielsoper.com/statcalc/calculator.aspx?id=89 (accessed on 1 March 2023).
- Flora, D.B.; Curran, P.J. An empirical evaluation of alternative methods of estimation for confirmatory factor analysis with ordinal data. Psychol. Methods 2004, 9, 466. [Google Scholar] [CrossRef] [PubMed]
- Hair, J.F.; Black, W.C.; Babin, B.J.; Anderson, R.E. Multivariate Data Analysis, 7th ed.; Pearson: New York, NY, USA, 2010. [Google Scholar]
- Schmitt, N. Uses and abuses of coefficient alpha. Psychol. Assess. 1996, 8, 350–353. [Google Scholar] [CrossRef]
- Fornell, C.; Larcker, D.F. Structural equation models with unobservable variables and measurement error: Algebra and statistics. J. Mark. Res. 1981, 18, 382–388. [Google Scholar] [CrossRef]
- Baeza-Rivera, M.J.; Salazar-Fernández, C.; Manríquez-Robles, D. Aculturación y salud mental en población migrante de la región de La Araucanía, el rol de los mediadores y moderadores. Resultados Preliminares Proyecto FONDECyT Iniciación 11181020. Reporte Técnico 2; Laboratorio de Interacciones, Cultura y Salud: Temuco, Chile, 2022. [Google Scholar] [CrossRef]
- Lovibond, P.F.; Lovibond, S.H. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995, 33, 335–343. [Google Scholar] [CrossRef] [PubMed]
- Mella, F.R.; Vinet, E.V.; Muñoz, A.M.A. Escalas de Depresión, Ansiedad y Estrés (DASS-21): Adaptación y propiedades psicométricas en estudiantes secundarios de Temuco. Rev. Argent. Clin. Psicol. 2014, 23, 179–190. [Google Scholar]
- Valencia, P. Las Escalas de Depresión, Ansiedad y Estrés (DASS-21): ¿miden Algo Más Que Un Factor General? Av. Psicol. 2019, 27, 177–189. [Google Scholar] [CrossRef]
- Solà-Sales, S.; Pérez-González, N.; van Hoey, J.; Iborra-Marmolejo, I.; Beneyto-Arrojo, M.J.; Moret-Tatay, C. The role of resilience for migrants and refugees’ mental health in times of COVID-19. Healthcare 2021, 9, 1131. [Google Scholar] [CrossRef]
- Adebayo, B.; Nichols, P.; Albrecht, M.A.; Brijnath, B.; Heslop, K. Investigating the impacts of acculturation stress on migrant care workers in australian residential aged care facilities. J. Transcult. Nurs. 2021, 32, 389–398. [Google Scholar] [CrossRef]
- Camacho, Á.; Cordero, E.D.; Perkins, T. Psychometric properties of the DASS-21 among latina/o college students by the US-Mexico border. J. Immigr. Minor. Health 2016, 18, 1017–1023. [Google Scholar] [CrossRef]
- Becerra, D.; Hernández, G.; Porchas, F.; Castillo, J.; Nguyen, V.; Perez González, R. Immigration policies and mental health: Examining the relationship between immigration enforcement and depression, anxiety, and stress among latino immigrants. J. Ethn. Cult. Divers. Soc. Work 2020, 29, 43–59. [Google Scholar] [CrossRef]
- Álamo, C.; Bejer, T.; Bagladi, V.; Cárcamo, N.; San Martín, D.; Fischer, M. Perfil integrativo de pacientes de salud mental atendidos en el centro de salud universitario de la Universidad Austral de Chile. Actual. Psicoter. Integr. 2017, 9, 9–20. [Google Scholar]
- Salinas-Oñate, N.; Baeza-Rivera, M.J.; Ortiz, M.; Betancourt, H. Development and validation of a scale for measuring cultural beliefs about psychotherapy patients in southern Chile. Psicol. Reflex. Crít. 2020, 33, 2. [Google Scholar] [CrossRef] [PubMed]
- Baeza-Rivera, M.J.; Salinas-Oñate, N.; Larenas, J. Y verás cómo quieren en Chile al amigo cuando es forastero: El caso de los colombianos en Temuco, Chile. In Desplazamiento: Perspectivas y Estrategias de Intervención Desde el Caribe Colombiano; Bustos, V., Mayor, D., Eds.; Editorial Universidad del Norte: Barranquilla, Colombia, 2022; pp. 225–249. [Google Scholar]
- Fennelly, K. The “healthy migrant” effect. Minn. Med. 2007, 90, 51–53. [Google Scholar]
- Tenorio-Corro, Y.; Arredondo, A. Utilización de los servicios de salud en la población migrante de Estados Unidos. Horiz. Sanit. 2018, 17, 89–94. [Google Scholar] [CrossRef]
- Razum, O.; Zeeb, H.; Rohrmann, S. The ‘healthy migrant effect’–not merely a fallacy of inaccurate denominator figures. Int. J. Epidemiol. 2000, 29, 191–192. [Google Scholar] [CrossRef]
- Cabieses, B.; Tunstall, H.; Pickett, K. Testing the latino paradox in Latin America: A population-based study of intra-regional immigrants in Chile. Rev. Med. Chil. 2013, 141, 1255–1265. [Google Scholar] [CrossRef]
- Cabieses, B.; Tunstall, H.; Pickett, K. Understanding the socioeconomic status of international immigrants in Chile through hierarchical cluster analysis: A population-based study. Int. Migr. 2015, 53, 303–320. [Google Scholar] [CrossRef]
- Barrera-Herrera, A.; Baeza-Rivera, M.J.; Escandón-Nagel, N.; Constanzo, J.; Escobar, B. Crisis social chilena y salud mental: Una mirada desde el ciclo vital. Rev. Psicol. 2022, 40, 241–263. [Google Scholar] [CrossRef]

| Name | No. Items | Response Format | Factors | Population | Country | Reliability | Validity |
|---|---|---|---|---|---|---|---|
| Brief scale for the evaluation of acculturation stress in the migrant population (EBEA) [35] | 14 | Likert from 1 (nothing stressful) to 5 (very stressful). | (1) Preparation and departure from the country of origin, (2) socioeconomic concerns and (3) adaptation to the receiving society. | 1309 adults between 18 and 60 years of age, from Colombia and Peru. | Chile | A ω between 0.83 and 0.92 for the subscales. | Concurrent (convergent, discriminant) and construct validity. |
| Adaptation of the clinical symptomatology inventory SCL-90 [51] | 50 | Likert from 0 (nothing at all) until 4 (much or very much). | (1) Somatisation, (2) interpersonal awareness, (3) depression, (4) anxiety and (5) hostility. | 109 adults between 18 and 76 years of age, from Bolivia, Colombia and Peru. | Chile | Cronbach’s alpha of 0.95. | - |
| WHOQoL-Bref questionnaire [52] | 26 | Likert from 1 to 5. | (1) General quality of life, (2) health satisfaction, (3) physical domain, (4) psychological domain, (5) psychological domain and (6) social domain. | 431 adults from Colombia and Peru. | Chile | - | - |
| OQ questionnaire [32] | 35 | Likert from 0 (never) to 4 (almost always). | (1) Interpersonal relationships, (2) social role and (3) symptoms. | 431 adults between 18 and 76 years of age, from Colombia and Peru. | Chile | An α of 0.91 for the scale, with an α between 0.65 and 0.88 for the subscales. | - |
| Cultural formulation interview (DSM 5) [53] | - | - | - | - | - | - | - |
| Positive and negative affect scale [54] | 12 | Likert from 1 (never) to 6 (always). | (1) Positive affect, (2) negative affect. | 517 adults between 18 and 76 years of age, from Chile, Colombia, Peru and Venezuela. | Chile | An α of 0.89 for the scale, with an α between 0.75 and 0.92 for the subscales. | Construct and concurrent validity. |
| Depression, anxiety and stress scale, DASS-[21,41] | 21 | Likert format, from 0 (does not describe anything that happened to me or how I felt during the week) to 3 (yes, this happened to me a lot or almost always). | (1) Depression, (2) anxiety and (3) stress. | 484 undergraduate students, between 18 and 28 years of age. | Chile | Cronbach’s alpha of 0.91, and between 0.73 to 0.85 for the subscales. | Construct, concurrent and divergent validity. |
| Patient health questionnaire (PHQ-9) [42] | 9 | Likert format from 0 (never) to 3 (almost every day). | Depression. | 1327 adults from the south of Chile. | Chile | Cronbach’s alpha of 0.83. | Construct and concurrent validity. |
| Inventario de Depresión de Beck (BDI-II) [43,44] | 21 | Likert scale from 0 to 3. | Depression. | 484 undergraduate students, between 18 and 28 years of age. | Chile | Cronbach’s alpha of 0.91. | Discriminant validity. |
| Goldberg health questionnaire (GHQ-12) [45,46] | 12 | Likert format from 0 (better than usual) to 3 (much less than usual). | 1 to 3 factors, depending on the study. | 963 undergraduate students. | Chile | Cronbach’s alpha of 0.86. | Construct validity. |
| Beck anxiety inventory (BAI) [44,47,48] | 21 | Likert scale from 0 to 3. | Anxiety. | 484 undergraduate students, between 18 and 28 years of age. | Chile | Cronbach’s alpha of 0.91. | Discriminant validity. |
| Study 1 | Study 2 | |
|---|---|---|
| n (Percentage/Mean (DS)) | n (Percentage/Mean (DS)) | |
| Age | 21.0 (2.39) | 34.5 (9.53) |
| Country of origin | ||
| Colombia | - | 36 (13%) |
| Venezuela | - | 235 (83%) |
| Haiti | - | 12 (4%) |
| Chile | 652 (100%) | - |
| Marital status | ||
| Single | 646 (99.2%) | 135 (47%) |
| Married | 2 (0.3%) | 69 (24%) |
| Divorced | - | 7 (2%) |
| Separated | - | 8 (3%) |
| Cohabiting | 4 (0.5%) | 64 (23%) |
| Sex | ||
| Female | 424 (65.3%) | 189 (67%) |
| Male | 215 (32.3%) | 94 (33%) |
| Non-binary | 13 (2.3%) | - |
| Socioeconomic status | ||
| Low, very low | 196 (30%) | 158 (55%) |
| Medium | 378 (58%) | 120 (42%) |
| High, very high | 78 (12%) | 5 (3%) |
| Educational level | ||
| High school completed or lower | - | 84 (30%) |
| University completed or incomplete | 652 (100%) | 177 (62%) |
| Postgraduate | - | 22 (8%) |
| Time living in Chile (months) | - | 32.12 (22.4) |
| Item | Mean | Standard Deviation | Midpoint Comparison = 4 |
|---|---|---|---|
| 1. Anxiety | 4.96 | 1.67 | t(647) = 14.54, p < 0.05 |
| 2. Stress | 5.00 | 1.57 | t(647) = 16.19, p < 0.05 |
| 3. Depression | 3.36 | 1.96 | t(647) = −8.33, p < 0.05 |
| 4. Sleeping problems | 3.97 | 2.01 | t(647) = −0.33, p = 0.37 |
| 5. Eating problems | 3.09 | 2.00 | t(647) = −10.15, p < 0.05 |
| 6. Stomach problems | 3.20 | 2.05 | t(647) = −8.30, p < 0.05 |
| 7. Sexual problems | 1.96 | 1.62 | t(647) = −32.00, p < 0.05 |
| 8. Headaches | 3.73 | 1.96 | t(647) = −3.46, p < 0.05 |
| Item | Mean | Standard Deviation | Midpoint Comparison = 4 |
|---|---|---|---|
| 1. Anxiety | 4.01 | 1.98 | t(282) = 0.120, p = 0.91 |
| 2. Stress | 4.59 | 1.90 | t(282) = 5.22, p < 0.05 |
| 3. Depression | 3.48 | 2.07 | t(282) = −4.20, p < 0.05 |
| 4. Sleeping problems | 3.87 | 2.13 | t(282) = −1.03, p = 0.30 |
| 5. Eating problems | 2.59 | 1.72 | t(282) = −13.84, p < 0.05 |
| 6. Stomach problems | 2.85 | 1.96 | t(282) = −9.86, p < 0.05 |
| 7. Sexual problems | 2.52 | 1.99 | t(282) = −12.57, p < 0.05 |
| 8. Headaches | 3.63 | 2.07 | t(282) = −3.01, p < 0.05 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barrera-Herrera, A.; Rivera Baeza, M.J.; Salazar-Fernández, C.; Manríquez-Robles, D. Analysis of the Mental and Physical Health Symptomatology Scale in a Sample of Emerging and Migrant Adults in Chile. Int. J. Environ. Res. Public Health 2023, 20, 4684. https://doi.org/10.3390/ijerph20064684
Barrera-Herrera A, Rivera Baeza MJ, Salazar-Fernández C, Manríquez-Robles D. Analysis of the Mental and Physical Health Symptomatology Scale in a Sample of Emerging and Migrant Adults in Chile. International Journal of Environmental Research and Public Health. 2023; 20(6):4684. https://doi.org/10.3390/ijerph20064684
Chicago/Turabian StyleBarrera-Herrera, Ana, María José Rivera Baeza, Camila Salazar-Fernández, and Diego Manríquez-Robles. 2023. "Analysis of the Mental and Physical Health Symptomatology Scale in a Sample of Emerging and Migrant Adults in Chile" International Journal of Environmental Research and Public Health 20, no. 6: 4684. https://doi.org/10.3390/ijerph20064684
APA StyleBarrera-Herrera, A., Rivera Baeza, M. J., Salazar-Fernández, C., & Manríquez-Robles, D. (2023). Analysis of the Mental and Physical Health Symptomatology Scale in a Sample of Emerging and Migrant Adults in Chile. International Journal of Environmental Research and Public Health, 20(6), 4684. https://doi.org/10.3390/ijerph20064684







