The Effect of Environmental Factors on Immunological Pathways of Asthma in Children of the Polish Mother and Child Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Study Design
2.3. Child Sociodemographic, Exposure, and Health Assessment
2.4. Allergen Sensitization
2.5. Lung Function Assessment
2.6. Immunological Assessment
2.7. Statistical Analysis
3. Results
3.1. Univariate Logistic Regression
3.1.1. Environmental Factors and Asthma Risk
3.1.2. Family History and Asthma Risk
3.1.3. Immunological Parameters and Asthma Risk
3.1.4. Lung Function Test Results and Asthma Risk
3.2. Multivariate Logistic Regression
3.3. FOXP3 Level Depending on Selected Environmental Factors
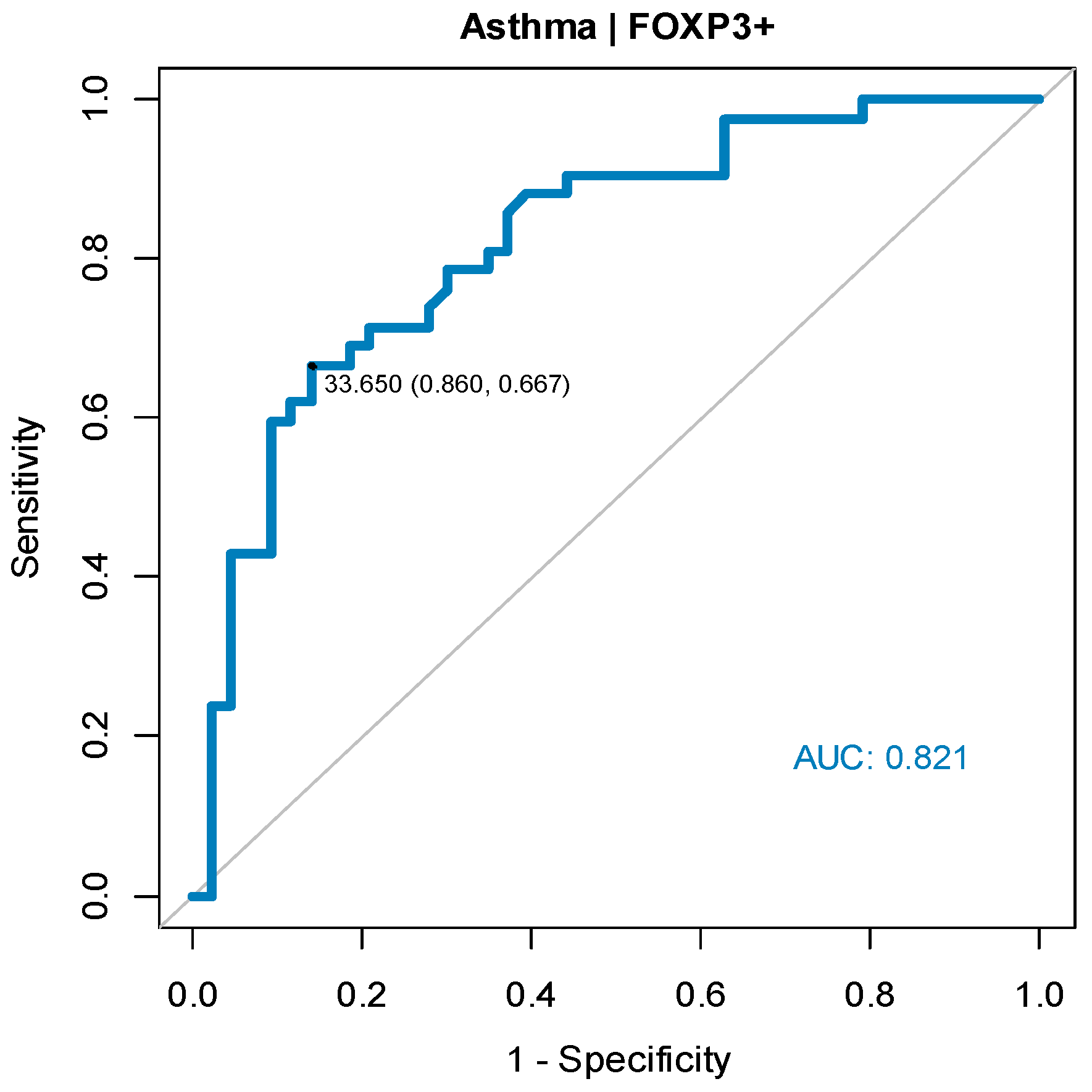
3.4. ROC Curve
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Federico, M.J.; McFarlane, A.E., 2nd; Szefler, S.J.; Abrams, E.M. The Impact of Social Determinants of Health on Children with Asthma. J. Allergy Clin. Immunol. Pract. 2020, 8, 1808–1814. [Google Scholar] [CrossRef]
- Haahtela, T. A biodiversity hypothesis. Allergy 2019, 74, 1445–1456. [Google Scholar] [CrossRef] [PubMed]
- Hufnagl, K.; Pali-Schöll, I.; Roth-Walter, F.; Jensen-Jarolim, E. Dysbiosis of the gut and lung microbiome has a role in asthma. Semin Immunopathol. 2020, 42, 75–93. [Google Scholar] [CrossRef] [PubMed]
- Zhao, S.T.; Wang, C.Z. Regulatory T cells and asthma. J. Zhejiang Univ.-SCIENCE B 2018, 19, 663–673. [Google Scholar] [CrossRef]
- Khan, M.A. Regulatory T cells mediated immunomodulation during asthma: A therapeutic standpoint. J. Transl. Med. 2020, 18, 456. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.; Hou, X.; Ni, Y.; Du, W.; Han, H.; Yu, Y.; Shi, G. The Imbalance of FOXP3/GATA3 in Regulatory T Cells from the Peripheral Blood of Asthmatic Patients. J. Immunol. Res. 2018, 2018, 3096183. [Google Scholar] [CrossRef] [PubMed]
- Ohkura, N.; Sakaguchi, S. Transcriptional and epigenetic basis of Treg cell development and function: Its genetic anomalies or variations in autoimmune diseases. Cell Res. 2020, 30, 465–474. [Google Scholar] [CrossRef] [PubMed]
- Xu, C.J.; Söderhäll, C.; Bustamante, M.; Baïz, N.; Gruzieva, O.; Gehring, U.; Mason, D.; Chatzi, L.; Basterrechea, M.; Llop, S.; et al. DNA methylation in childhood asthma: An epigenome-wide meta-analysis. Lancet Respir. Med. 2018, 6, 379–388. [Google Scholar] [CrossRef]
- Bae, D.J.; Jun, J.A.; Chang, H.S.; Park, J.S.; Park, C.S. Epigenetic Changes in Asthma: Role of DNA CpG Methylation. Tuberc. Respir. Dis. 2020, 83, 1–13. [Google Scholar] [CrossRef]
- Stern, D.A.; Morgan, W.J.; Halonen, M.; Wright, A.L.; Martinez, F.D. Wheezing and bronchial hyper-responsiveness in early childhood as predictors of newly diagnosed asthma in early adulthood: A longitudinal birth-cohort study. Lancet 2008, 372, 1058–1064. [Google Scholar] [CrossRef]
- Ponka, P.; Lok, C.N. The transferrin receptor: Role in health and disease. Int. J. Biochem. Cell Biol. 1999, 31, 1111–1137. [Google Scholar] [CrossRef] [PubMed]
- Brzozowska, A.; Woicka-Kolejwa, K.; Jerzynska, J.; Majak, P.; Stelmach, I. Allergic Rhinitis and House Dust Mite Sensitization Determine Persistence of Asthma in Children. Indian J. Pediatr. 2022, 89, 673–681. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.; Tibbitt, C.A.; Feng, X.; Stark, J.M.; Rohrbeck, L.; Rausch, L.; Sedimbi, S.K.; Karlsson, M.C.I.; Lambrecht, B.N.; Coquet, J.M.; et al. PPAR-γ promotes type 2 immune responses in allergy and nematode infection. Sci. Immunol. 2017, 2, eaal5196. [Google Scholar] [CrossRef] [PubMed]
- Williams, J.J.; Munro, K.M.; Palmer, T.M. Role of ubiquitylation in controlling suppressor of cytokine signalling 3 (SOCS3) function and expression. Cells 2014, 3, 546–562. [Google Scholar] [CrossRef]
- Zafra, M.P.; Cañas, J.A.; Mazzeo, C.; Gámez, C.; Sanz, V.; Fernández-Nieto, M.; Quirce, S.; Barranco, P.; Ruiz-Hornillos, J.; Sastre, J.; et al. SOCS3 silencing attenuates eosinophil functions in asthma patients. Int. J. Mol. Sci. 2015, 16, 5434–5451. [Google Scholar] [CrossRef] [PubMed]
- Meyer-Martin, H.; Hahn, S.A.; Beckert, H.; Belz, C.; Heinz, A.; Jonuleit, H.; Becker, C.; Taube, C.; Korn, S.; Tuettenberg, A.; et al. GARP inhibits allergic airway inflammation in a humanized mouse model. Allergy 2016, 71, 1274–1283. [Google Scholar] [CrossRef]
- Zimmer, N.; Trzeciak, E.R.; Graefen, B.; Satoh, K.; Tuettenberg, A. GARP as a Therapeutic Target for the Modulation of Regulatory T Cells in Cancer and Autoimmunity. Front. Immunol. 2022, 13, 928450. [Google Scholar] [CrossRef]
- Stelmach, I.; Grzelewski, T.; Bobrowska-Korzeniowska, M.; Kopka, M.; Majak, P.; Jerzynska, J.; Stelmach, W.; Polańska, K.; Sobala, W.; Gromadzińska, J.; et al. The role of zinc, copper, plasma glutathione peroxidase enzyme, and vitamins in the development of allergic diseases in early childhood: The Polish mother and child cohort study. Allergy Asthma Proc. 2014, 35, 227–232. [Google Scholar] [CrossRef]
- Bobrowska-Korzeniowska, M.; Jerzyńska, J.; Polańska, K.; Gromadzińska, J.; Hanke, W.; Wasowicz, W.; Stelmach, I. The role of antioxidants and 25-hydroxyvitamin D during pregnancy in the development of allergic diseases in early school-age children Polish Mother and Child Cohort Study. Allergy Asthma Proc. 2020, 41, e19–e25. [Google Scholar] [CrossRef]
- Bobrowska-Korzeniowska, M.; Kapszewicz, K.; Jerzynska, J.; Stelmach, W.; Polanska, K.; Gromadzinska, J.; Mikolajewska, K.; Hanke, W.; Stelmach, I. Early life environmental exposure in relation to new onset and remission of allergic diseases in school children: Polish Mother and Child Cohort Study. Allergy Asthma Proc. 2019, 40, 329–337. [Google Scholar] [CrossRef]
- Polańska, K.; Hanke, W.; Gromadzińska, J.; Ligocka, D.; Gulczyńska, E.; Sobala, W.; Wąsowicz, W. Polish mother and child cohort study—Defining the problem, the aim of the study and methodological assumptions. Int. Occup. Med. Environ. Health. 2009, 22, 383–391. [Google Scholar] [CrossRef] [PubMed]
- Polańska, K.; Hanke, W.; Król, A.; Potocka, A.; Waszkowska, M.; Jacukowicz, A.; Gromadzińska, J.; Wąsowicz, W.; Jerzyńska, J.; Stelmach, W.; et al. Polish Mother and Child Cohort Study (REPRO_PL)—Methodology of the follow-up of the children at the age of 7. Int. J. Occup. Med. Environ. Health 2016, 29, 883–893. [Google Scholar] [CrossRef] [PubMed]
- Bobrowska-Korzeniowska, M.; Brzozowska, A.; Jerzyńska, J.; Stelmach, W.; Stelmach, I. Usefulness of sRtot and Rint in bronchodilator testing in the diagnosis of asthma in children. Adv. Dermatol. Allergol. 2020, 37, 685–689. [Google Scholar] [CrossRef] [PubMed]
- Gromadzinska, J.; Polanska, K.; Kozlowska, L.; Mikolajewska, K.; Stelmach, I.; Jerzynska, J.; Stelmach, W.; Grzesiak, M.; Hanke, W.; Wasowicz, W. Vitamins A and E during Pregnancy and Allergy Symptoms in an Early Childhood-Lack of Association with Tobacco Smoke Exposure. Int. J. Environ. Res. Public Health 2018, 15, 1245. [Google Scholar] [CrossRef]
- Global Strategy for Asthma Management and Prevention. Available online: https://ginasthma.org/wp-content/uploads/2022/07/GINA-Main-Report-2022-FINAL-22-07-01-WMS.pdf (accessed on 31 December 2022).
- Parsons, J.P.; Hallstrand, T.S.; Mastronarde, J.G.; Kaminsky, D.A.; Rundell, K.W.; Hull, J.H.; Storms, W.W.; Weiler, J.M.; Cheek, F.M.; Wilson, K.C.; et al. American Thoracic Society Subcommittee on Exercise-induced Bronchoconstriction. An official American Thoracic Society clinical practice guideline: Exercise-induced bronchoconstriction. Am. J. Respir. Crit. Care Med. 2013, 187, 1016–1027. [Google Scholar] [CrossRef]
- Santacroce, L.; Charitos, I.A.; Ballini, A.; Inchingolo, F.; Luperto, P.; De Nitto, E.; Topi, S. The Human Respiratory System and its Microbiome at a Glimpse. Biology 2020, 9, 318. [Google Scholar] [CrossRef]
- Rajani, P.S.; Seppo, A.E.; Järvinen, K.M. Immunologically Active Components in Human Milk and Development of Atopic Disease, With Emphasis on Food Allergy, in the Pediatric Population. Front. Pediatr. 2018, 6, 218. [Google Scholar] [CrossRef]
- Kumar, P.H.; Devgan, A. The Association of Breastfeeding with Childhood Asthma: A Case-Control Study from India. Cureus 2021, 13, e19810. [Google Scholar] [CrossRef]
- Zhu, X.; Chen, Q.; Liu, Z.; Luo, D.; Li, L.; Zhong, Y. Low expression and hypermethylation of FOXP3 in regulatory T cells are associated with asthma in children. Exp. Ther. Med. 2020, 19, 2045–2052. [Google Scholar] [CrossRef]
- Solarz, K.; Obuchowicz, A.; Asman, M.; Nowak, W.; Witecka, J.; Pietrzak, J.; Marek, M.; Łonak, A.; Stadnicka, I.; Hajduga-Staśko, B. Abundance of domestic mites in dwellings of children and adolescents with asthma in relation to environmental factors and allergy symptoms. Sci. Rep. 2021, 11, 18453. [Google Scholar] [CrossRef]
- Böhm, L.; Maxeiner, J.; Meyer-Martin, H.; Reuter, S.; Finotto, S.; Klein, M.; Schild, H.; Schmitt, E.; Bopp, T.; Taube, C. IL-10 and regulatory T cells cooperate in allergen-specific immunotherapy to ameliorate allergic asthma. J. Immunol. 2015, 194, 887–897. [Google Scholar] [CrossRef] [PubMed]
- Prunicki, M.; Stell, L.; Dinakarpandian, D.; de Planell-Saguer, M.; Lucas, R.W.; Hammond, S.K.; Balmes, J.R.; Zhou, X.; Paglino, T.; Nadeau, K.C.; et al. Exposure to NO2, CO, and PM2.5 is linked to regional DNA methylation differences in asthma. Clin. Epigenetics 2018, 10, 2. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Peng, B.; Wu, S.; Xu, N. Epigenetic Regulation of Regulatory T Cells in Kidney Disease and Transplantation. Curr. Gene. Ther. 2017, 17, 461–468. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Wang, J.; Wang, H.; Li, Y.; Jia, Y.; Yi, M.; Chen, O. Association of infant antibiotic exposure and risk of childhood asthma: A meta-analysis. World Allergy Organ J. 2021, 14, 100607. [Google Scholar] [CrossRef]
- Momen, N.C.; Liu, X. Maternal antibiotic use during pregnancy and asthma in children: Population-based cohort study and sibling design. Eur. Respir. J. 2021, 57, 2000937. [Google Scholar] [CrossRef]
- Turi, K.N.; Gebretsadik, T.; Ding, T.; Abreo, A.; Stone, C.; Hartert, T.V.; Wu, P. Dose, Timing, and Spectrum of Prenatal Antibiotic Exposure and Risk of Childhood Asthma. Clin. Infect. Dis. 2021, 72, 455–462. [Google Scholar] [CrossRef]
- Loewen, K.; Monchka, B.; Mahmud, S.M.; Jong, G.T.; Azad, M.B. Prenatal antibiotic exposure and childhood asthma: A population-based study. Eur. Respir. J. 2018, 52, 1702070. [Google Scholar] [CrossRef]

| Variable | Total (N = 85) | Asthma (N = 42) | No Asthma (N = 43) |
|---|---|---|---|
| Gender, n (%) | |||
| Female | 42 (49.4) | 20 (47.6) | 22 (51.2) |
| Male | 43 (50.6) | 22 (52.4) | 21 (48.8) |
| Age, n (%) | |||
| 9 years | 21 (24.7) | 5 (11.9) | 16 (37.2) |
| 10 years | 20 (23.5) | 6 (14.3) | 14 (32.6) |
| 11 years | 22 (25.9) | 14 (33.3) | 8 (18.6) |
| 12 years | 22 (25.9) | 17 (40.5) | 5 (11.6) |
| BMI, kg/m2, median (Q1; Q3) | 19.00 (17.00; 20.00) | 19.00 (17.00; 21.00) | 19.00 (18.00; 19.00) |
| Birth weight, g, mean ± SD | 3324.88 ± 332.05 | 3357.50 ± 316.37 | 3293.02 ± 347.43 |
| Mother’s age, years, mean ± SD | 28.37 ± 3.86 | 29.20 ± 3.73 | 27.58 ± 3.86 |
| Delivery type, n (%) | |||
| Natural spontaneous | 56 (66.7) | 23 (54.8) | 33 (78.6) |
| Natural induced | 9 (10.7) | 5 (11.9) | 4 (9.5) |
| Forceps or vacuum | 14 (16.7) | 12 (28.6) | 2 (4.8) |
| Cesarean section | 5 (6.0) | 2 (4.8) | 3 (7.1) |
| Breastfeeding *, n (%) | 68 (80.0) | 26 (61.9) | 42 (97.7) |
| Mother’s education, n (%) | |||
| Secondary | 16 (18.8) | 6 (14.3) | 10 (23.3) |
| Higher | 69 (81.2) | 36 (85.7) | 33 (76.7) |
| Place of residence | |||
| City, n (%) | 66 (78.6) | 39 (92.9) | 27 (64.3) |
| Village, n (%) | 19 (22.4) | 3 (7.1) | 16 (37.2) |
| Allergy in family, n (%) | 56 (67.5) | 37 (92.5) | 19 (44.2) |
| Atopic dermatitis, n (%) | 16 (18.8) | 11 (26.2) | 5 (11.6) |
| Food allergy, n (%) | 15 (17.6) | 10 (23.8) | 5 (11.6) |
| AR/conjunctivitis, n (%) | 44 (51.8) | 37 (88.1) | 7 (16.3) |
| Atopy, n (%) | 47 (55.3) | 40 (95.2) | 7 (16.3) |
| Type of allergy | |||
| HDM, n (%) | 25 (29.4) | 22 (52.4) | 3 (7.0) |
| molds, n (%) | 11 (12.9) | 9 (21.4) | 2 (4.7) |
| grass/trees pollen, n (%) | 37 (43.5) | 32 (76.2) | 5 (11.6) |
| dog/cat, n (%) | 10 (11.9) | 6 (14.3) | 4 (9.5) |
| Household exposure | |||
| Nicotine exposure, n (%) | 14 (16.5) | 6 (14.3) | 8 (18.6) |
| Domestic animals, n (%) | 38 (44.7) | 20 (47.6) | 18 (41.9) |
| Dampness, n (%) | 26 (30.6) | 15 (35.7) | 11 (25.6) |
| Carpet surface, n (%) | 64 (75.3) | 38 (90.5) | 26 (60.5) |
| Cleaning, n (%) | |||
| Less than once a week | 1 (1.2) | 0 (0.0) | 1 (2.3) |
| Once a week | 20 (23.5) | 11 (26.2) | 9 (20.9) |
| Twice a week | 42 (49.4) | 25 (59.5) | 17 (39.5) |
| More than twice a week | 22 (25.9) | 6 (14.3) | 16 (37.2) |
| Use of antibiotics up to the age of 2, n (%) | 47 (56.0) | 33 (78.6) | 14 (33.3) |
| Use of antibiotics more than 2 per year in childhood, n (%) | 46 (54.8) | 32 (76.2) | 14 (33.3) |
| Immunological markers | |||
| PPARG+/11c+, median (Q1; Q3) | 12.50 (5.80; 21.80) | 14.55 (8.20; 21.87) | 10.10 (4.25; 19.35) |
| 25+/4+, median (Q1; Q3) | 4.50 (2.10; 10.40) | 7.50 (2.97; 12.45) | 3.50 (1.80; 6.40) |
| FOXP3+, median (Q1; Q3) | 43.40 (22.40; 68.40) | 24.75 (14.95; 43.93) | 60.80 (41.20; 90.55) |
| GARP+ (I), median (Q1; Q3) | 45.20 (22.20; 87.40) | 43.85 (16.90; 91.10) | 52.40 (34.50; 81.60) |
| 25+/71+ (I), median (Q1; Q3) | 4.10 (2.60; 6.70) | 3.95 (2.80; 6.20) | 4.20 (2.25; 7.25) |
| SOCS+, median (Q1; Q3) | 18.10 (7.30; 36.10) | 26.60 (14.75; 42.55) | 11.30 (5.80; 28.10) |
| 25+/71+ (II), median (Q1; Q3) | 4.30 (2.30; 7.40) | 4.35 (3.20; 6.57) | 3.70 (2.00; 10.10) |
| GARP+ (II), median (Q1; Q3) | 15.20 (8.00; 28.50) | 14.10 (8.83; 24.82) | 16.00 (7.55; 36.20) |
| FEV1, L, median (Q1; Q3) | 1.90 (1.60; 2.54) | 2.29 (1.68; 3.00) | 1.76 (1.58; 2.02) |
| FEV1, %, median (Q1; Q3) | 89.00 (84.00; 96.00) | 87.00 (81.50; 90.00) | 92.00 (88.50; 98.00) |
| FEV1/FVC, %, mean ± SD | 0.91 ± 0.11 | 0.88 ± 0.10 | 0.95 ± 0.10 |
| FeNO, ppb, median (Q1; Q3) | 28.00 (17.40; 35.40) | 32.40 (22.35; 43.65) | 16.25 (13.83; 24.68) |
| Variable | OR | 95% CI | p |
|---|---|---|---|
| Gender, female | 0.87 | 0.37–2.03 | 0.744 |
| Age, years | 1.31 | 1.14–1.57 | 0.001 |
| BMI, kg/m2 | 1.08 | 0.97–1.24 | 0.189 |
| Birth weight, g | 1.00 | 1.00–1.00 | 0.370 |
| Mother’s age, years | 1.12 | 1.00–1.27 | 0.060 |
| Delivery type: | |||
| Natural spontaneous | RC | - | - |
| Natural induced | 1.79 | 0.43–7.94 | 0.420 |
| Forceps or vacuum | 8.61 | 2.09–58.79 | 0.008 |
| Caesarean section | 0.96 | 0.12–6.21 | 0.963 |
| Breastfeeding * | 0.04 | 0.00–0.21 | 0.002 |
| Mother’s tertiary education | 1.82 | 0.61–5.86 | 0.294 |
| City residence | 7.22 | 2.13–33.40 | 0.004 |
| Village residence | 0.13 | 0.03–0.44 | 0.003 |
| Allergy in family | 15.58 | 4.71–71.65 | <0.001 |
| Atopic dermatitis | 2.70 | 0.88–9.33 | 0.093 |
| Food allergy | 2.37 | 0.76–8.29 | 0.148 |
| AR/conjunctivitis | 38.06 | 12.02–146.10 | <0.001 |
| Atopy | 102.86 | 24.43–733.27 | <0.001 |
| Type of allergy | |||
| HDM | 14.67 | 4.43–67.36 | <0.001 |
| Molds | 5.59 | 1.33–38.36 | 0.035 |
| grass/trees pollen | 24.32 | 8.11–87.00 | <0.001 |
| dog/cat | 1.58 | 0.42–6.63 | 0.503 |
| Nicotine exposure | 0.73 | 0.22–2.31 | 0.592 |
| Domestic animals | 1.26 | 0.54–2.99 | 0.594 |
| Dampness | 1.62 | 0.64–4.18 | 0.312 |
| Carpet surface | 6.21 | 2.03–23.52 | 0.003 |
| Cleaning: | |||
| Less than once a week | 0.00 | - | 0.991 |
| Once a week | RC | - | - |
| Twice a week | 1.20 | 0.40–3.54 | 0.736 |
| More than twice a week | 0.31 | 0.08–1.08 | 0.072 |
| Use of antibiotics up to the age of 2 | 7.33 | 2.85–20.40 | <0.001 |
| Use of more than 2 antibiotics/year in childhood | 6.40 | 2.53–17.35 | <0.001 |
| Immunological markers | |||
| PPARG+/11c+ | 1.01 | 0.97–1.05 | 0.593 |
| 25+/4+ | 1.04 | 0.98–1.12 | 0.197 |
| FOXP3+ | 0.95 | 0.93–0.97 | <0.001 |
| GARP+ (I) | 1.00 | 0.98–1.01 | 0.599 |
| 25+/71+ (I) | 0.96 | 0.89–1.02 | 0.270 |
| SOCS+ | 1.01 | 0.99–1.03 | 0.190 |
| 25+/71+ (II) | 0.97 | 0.91–1.01 | 0.232 |
| GARP+ (II) | 0.99 | 0.96–1.01 | 0.227 |
| FEV1, L | 3.51 | 1.61–9.10 | 0.004 |
| FEV1, % | 0.92 | 0.86–0.97 | 0.006 |
| FEV1/FVC, % | 0.001 | 0.000–0.131 | 0.009 |
| FeNO, ppb | 1.12 | 1.04–1.23 | 0.010 |
| Variable | OR | 95% CI | p |
|---|---|---|---|
| Breastfeeding * | 0.21 | 0.01–1.73 | 0.204 |
| City residence | 3.23 | 0.42–31.82 | 0.274 |
| Other allergic disease ** | 41.12 | 5.77–896.52 | 0.002 |
| Use of antibiotics up to the age of 2 | 7.14 | 1.49–43.90 | 0.019 |
| FOXP3+ | 0.94 | 0.91–0.97 | 0.001 |
| Variable | n | Me (Q1; Q3) | MD (95% CI) | p |
|---|---|---|---|---|
| Breastfeeding * | ||||
| Yes | 68 | 49.60 (30.07; 75.17) | 28.10 (8.30; 37.60) | 0.001 |
| No | 17 | 21.50 (12.00; 33.60) | ||
| Residence | ||||
| City | 66 | 36.55 (21.85; 61.10) | −22.15 (−31.50; 1.00) | 0.067 |
| Village | 19 | 58.70 (37.95; 89.00) | ||
| Use of antibiotics up to the age of 2 ** | ||||
| Yes | 47 | 35.10 (21.70; 57.20) | −14.90 (−23.50; 3.00) | 0.141 |
| No | 37 | 50.00 (31.60; 75.00) | ||
| Use of antibiotics more than 2 per year in childhood ** | ||||
| Yes | 46 | 39.25 (21.65; 75.60) | −4.05 (−13.20; 12.80) | 0.822 |
| No | 38 | 43.30 (26.65; 60.80) | ||
| Other allergic disease *** | ||||
| Yes | 57 | 32.70 (18.90; 59.00) | −25.90 (−34.90; −9.00) | 0.001 |
| No | 28 | 58.60 (39.88; 91.38) | ||
| Cleaning | ||||
| Once a week or less frequently **** | 21 | 43.40 (22.00; 85.50) | - | 0.043 |
| Twice a week | 42 | 34.90 (21.52; 56.10) a | ||
| More than twice a week | 22 | 57.70 (34.48; 89.70) a |
| Cut-Off Point | AUC (95% CI) | Sensitivity | Specificity | Accuracy | PPV | NPV | p |
|---|---|---|---|---|---|---|---|
| 33.65 | 0.821 (0.731;0.911) | 0.67 | 0.86 | 0.76 | 0.82 | 0.73 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sara, Ż.-S.; Joanna, J.; Daniela, P.; Kinga, P.; Agnieszka, B. The Effect of Environmental Factors on Immunological Pathways of Asthma in Children of the Polish Mother and Child Cohort Study. Int. J. Environ. Res. Public Health 2023, 20, 4774. https://doi.org/10.3390/ijerph20064774
Sara Ż-S, Joanna J, Daniela P, Kinga P, Agnieszka B. The Effect of Environmental Factors on Immunological Pathways of Asthma in Children of the Polish Mother and Child Cohort Study. International Journal of Environmental Research and Public Health. 2023; 20(6):4774. https://doi.org/10.3390/ijerph20064774
Chicago/Turabian StyleSara, Żywiołowska-Smuga, Jerzyńska Joanna, Podlecka Daniela, Polańska Kinga, and Brzozowska Agnieszka. 2023. "The Effect of Environmental Factors on Immunological Pathways of Asthma in Children of the Polish Mother and Child Cohort Study" International Journal of Environmental Research and Public Health 20, no. 6: 4774. https://doi.org/10.3390/ijerph20064774
APA StyleSara, Ż.-S., Joanna, J., Daniela, P., Kinga, P., & Agnieszka, B. (2023). The Effect of Environmental Factors on Immunological Pathways of Asthma in Children of the Polish Mother and Child Cohort Study. International Journal of Environmental Research and Public Health, 20(6), 4774. https://doi.org/10.3390/ijerph20064774







