Applying Machine Learning to Construct a Model of Risk of Depression in Patients Following Cardiac Surgery with the Use of the SF-12 Survey
Abstract
:1. Introduction
2. Methods
2.1. Participants
2.2. Measures
2.3. Assessment of Risk of Depression Based on SF-12
2.4. Ethical Approval and Statement of Informed Consent
2.5. Statistical Analysis
3. Results
3.1. Baseline Characteristics of the Study Population
3.2. Short Form Health Survey (SF-12) Results
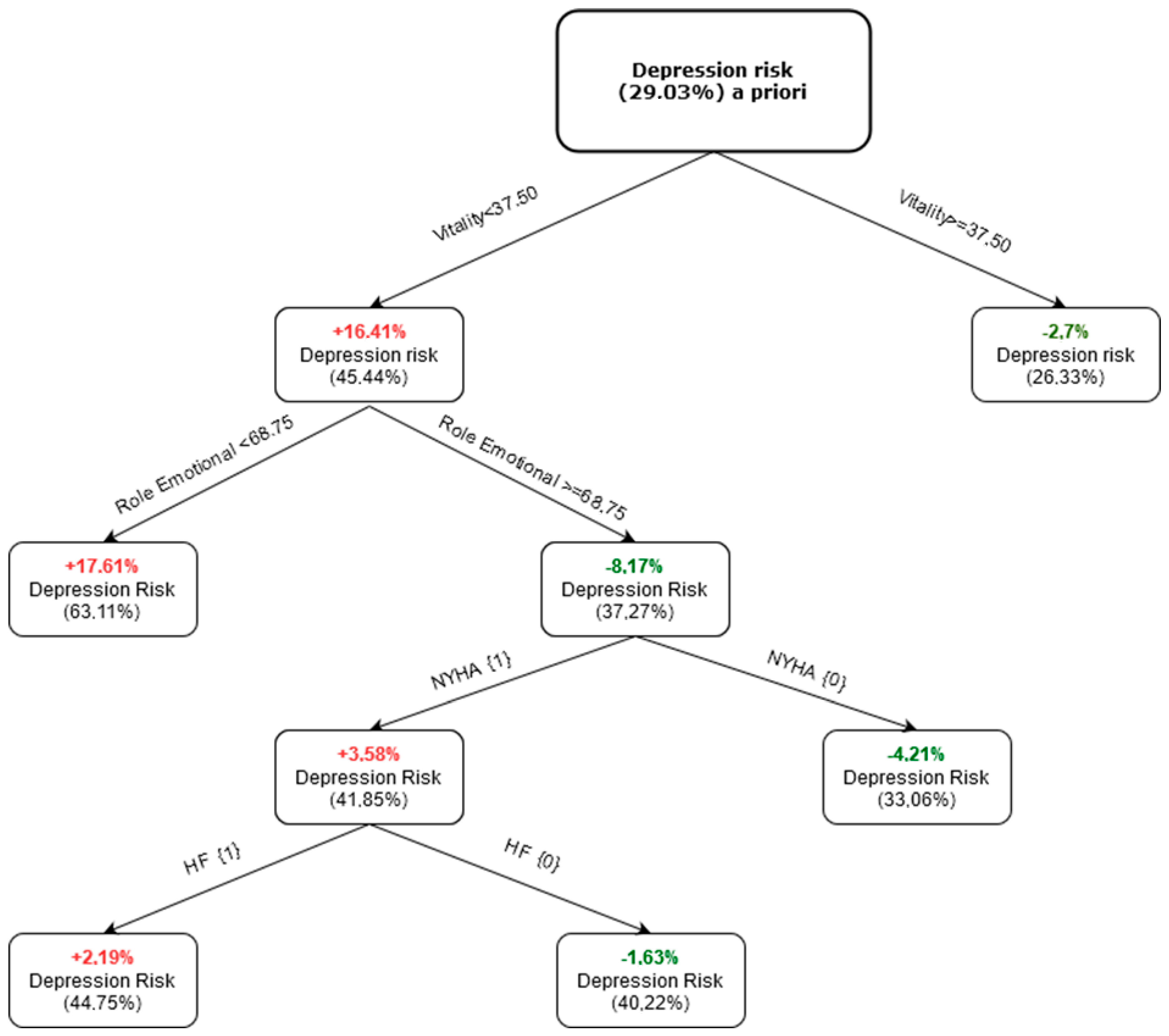
3.3. Model of Risk of Depression
4. Discussion
5. Study Strengths and Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wang, J.; Wu, X.; Lai, W.; Long, E.; Zhang, X.; Li, W.; Zhu, Y.; Chen, C.; Zhong, X.; Liu, Z.; et al. Prevalence of depression and depressive symptoms among outpatients: A systematic review and meta-analysis. BMJ Open 2017, 7, e017173. [Google Scholar] [CrossRef] [Green Version]
- Stanicki, P.; Szarpak, J.; Wieteska, M.; Kaczyńska, A.; Milanowska, J. Postoperative depression in patients after coronary artery bypass grafting (CABG)—A review of the literature. Pol. Prz. Chir. 2020, 92, 32–38. [Google Scholar] [CrossRef]
- Correa-Rodríguez, M.; Abu Ejheisheh, M.; Suleiman-Martos, N.; Membrive-Jiménez, M.J.; Velando-Soriano, A.; Schmidt-RioValle, J.; Gómez-Urquiza, J.L. Prevalence of depression in coronary artery bypass surgery: A Systematic Review and Meta-Analysis. J. Clin. Med. 2020, 9, 909. [Google Scholar] [CrossRef] [Green Version]
- Ravven, S.; Bader, C.; Azar, A.; Rudolph, J.L. Depressive symptoms after CABG surgery: A meta-analysis. Harv. Rev. Psychiatry 2013, 21, 59–69. [Google Scholar] [CrossRef] [Green Version]
- Takagi, H.; Ando, T.; Umemoto, T. Perioperative depression or anxiety and postoperative mortality in cardiac surgery: A systematic review and meta-analysis. Heart Vessels 2017, 32, 1458–1468. [Google Scholar] [CrossRef]
- Kemp, D.; Malhotra, S.; Franco, K.; Tesar, G.; Bronson, D. Perioperative depression or anxiety and postoperative mortality in cardiac surgery: A systematic review and meta-analysis. Heart disease and depression: Don’t ignore the relationship. Clevel. Clin. J. Med. 2003, 70, 745–761. [Google Scholar] [CrossRef]
- Lichtman, J.H.; Bigger, J.T., Jr.; Blumenthal, J.A.; Frasure-Smith, N.; Kaufmann, P.G.; Lespérance, F.; Mark, D.B.; Sheps, D.S.; Taylor, C.B.; Froelicher, E.S. Depression and coronary heart disease: Recommendations for screening, referral, and treatment: A science advisory from the American Heart Association Prevention Committee of the Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Interdisciplinary Council on Quality of Care and Outcomes Research: Endorsed by the American Psychiatric Association. Circulation 2008, 118, 1768–1775. [Google Scholar] [CrossRef] [Green Version]
- Stenman, M.; Holzmann, M.; Sartipy, U. Association between preoperative depression and long-term survival following coronary artery bypass surgery—A systematic review and meta-analysis. Int. J. Cardiol. 2016, 222, 462–466. [Google Scholar] [CrossRef]
- Protogerou, C.; Fleeman, N.; Dwan, K.; Richardson, M.; Dundar, Y.; Hagger, M.S. Moderators of the effect of psychological interventions on depression and anxiety in cardiac surgery patients: A systematic review and meta-analysis. Behav. Res. Ther. 2015, 73, 151–164. [Google Scholar] [CrossRef] [Green Version]
- Rahul, C.D. Machine Learning in Medicine. Circulation 2015, 132, 1920–1930. [Google Scholar] [CrossRef] [Green Version]
- Topolski, M. The Modified Principal Component Analysis Feature Extraction Method for the Task of Diagnosing Chronic Lymphocytic Leukemia Type B-CLL. J. Univers. Comput. Sci. 2020, 26, 734–746. [Google Scholar] [CrossRef]
- Lee, Y.; Ragguett, R.-M.; Mansur, R.B.; Boutilier, J.J.; Rosenblat, J.D.; Trevizol, A.; Brietzke, E.; Lin, K.; Pan, Z.; Subramaniapillai, M.; et al. Applications of machine learning algorithms to predict therapeutic outcomes in depression: A meta-analysis and systematic review. J. Affect. Disord. 2018, 241, 519–532. [Google Scholar] [CrossRef]
- Shin, D.; Lee, K.J.; Adeluwa, T.; Hur, J. Machine Learning-Based Predictive Modeling of Postpartum Depression. J. Clin. Med. 2020, 9, 2899. [Google Scholar] [CrossRef]
- Aleem, S.; Huda, N.U.; Amin, R.; Khalid, S.; Alshamrani, S.S.; Alshehri, A. Machine Learning Algorithms for Depression: Diagnosis, Insights, and Research Directions. Electronics 2022, 11, 1111. [Google Scholar] [CrossRef]
- Zulfiker, S.; Nasrin Kabir, N.; Biswas, A.A.; Nazneen, T.; Uddin, M.S. An in-depth analysis of machine learning approaches to predict depression. Curr. Res. Behav. Sci. 2021, 2, 100044. [Google Scholar] [CrossRef]
- Bhakta, I.; Sau, A. Prediction of depression among senior citizens using machine learning classifiers. Int. J. Comput. Appl. 2016, 144, 11–16. [Google Scholar] [CrossRef]
- Takousi, M.G.; Schmeer, S.; Manaras, I.; Olympios, C.D.; Makos, G.; Troop, N.A. Health-Related Quality of Life after Coronary Revascularization: A systematic review with meta-analysis. Hell. J. Cardiol. 2016, 23, 223–237. [Google Scholar] [CrossRef] [Green Version]
- Maruish, M.E. (Ed.) User’s Manual for the SF-12v2 Health Survey, 3rd ed.; QualityMetric Incorporated: Lincoln, RI, USA, 2012. [Google Scholar]
- Ringnér, M. What is principal component analysis? Nat. Biotechnol. 2008, 26, 303. [Google Scholar] [CrossRef]
- Schölkopf, B. The kernel trick for distances. Adv. Neural Inf. Process. Syst. 2001, 13, 301–307. [Google Scholar]
- Topolski, M. Algorithm of multidimensional analysis of main features of PCA with blurry observation of facility features detection of carcinoma cells multiple myeloma. In Progress in Computer Recognition Systems. CORES 2019. Advances in Intelligent Systems and Computing; Burduk, R., Kurzynski, M., Wozniak, M., Eds.; Springer: Cham, Switzerland, 2020. [Google Scholar] [CrossRef]
- Topolski, M.; Topolska, K. Algorithm for Constructing a Classifier Team Using a Modified PCA (Principal Component Analysis) in the Task of Diagnosis of Acute Lymphocytic Leukaemia Type B-CLL. In Hybrid Artificial Intelligent Systems. HAIS 2019. Lecture Notes in Computer Science; Pérez García, H., Sánchez González, L., Castejón Limas, M., Quintián Pardo, H., Corchado Rodríguez, E., Eds.; Springer: Cham, Switzerland, 2019; Volume 11734. [Google Scholar] [CrossRef]
- Topolski, M. Application of the Stochastic Gradient Method in the construction of the main components of PCA in the task diagnosis of multiple sclerosis in children. Comput. Sci. ICCS 2020, 12140, 35–44. [Google Scholar] [CrossRef]
- Auensen, A.; Hussain, A.I.; Garratt, A.M.; Gullestad, L.L.; Pettersen, K.I. Patient-reported outcomes after referral for possible valve replacement in patients with severe aortic stenosis. Eur. J. Cardio-Thorac. Surg. 2018, 53, 129–135. [Google Scholar] [CrossRef] [Green Version]
- Curtis, L.H.; Phelps, C.E.; McDermott, M.P.; Rubin, H.R. The value of patient-reported health status in predicting short-term outcomes after coronary artery bypass graft surgery. Med. Care 2002, 40, 1090–1100. [Google Scholar] [CrossRef]
- Batika, P.C.; Zairis, M.N.; Patsourakos, N.G.; Meletiadou, M.E.; Georgilas, A.T.; Foussas, S.G.; Tousoulis, D. Effect of depression on long-term prognosis after successful coronary stenting. Hell. J. Cardiol. 2018, 59, 43–45. [Google Scholar] [CrossRef]
- Richter, D. Men are from Mars, women are from Venus: Female hearts break easier than male from sadness. Hell. J. Cardiol. 2021, 62, 368–369. [Google Scholar] [CrossRef]
- Doering, L.V.; Moser, D.K.; Riegel, B.; McKinley, S.; Davidson, P.; Baker, H.; Meischke, H.; Dracup, K. Persistent comorbid symptoms of depression and anxiety predict mortality in heart disease. Int. J. Cardiol. 2010, 145, 188–192. [Google Scholar] [CrossRef] [Green Version]
- Pietrzyk, E.; Gorczyca-Michta, I.; Michta, K.; Nowakowska, M.; Wożakowska-Kapłon, B. Depression in patients after coronary artery bypass grafting. Psychiatr. Pol. 2014, 48, 987–996. [Google Scholar] [CrossRef]
- Gjeilo, K.H.; Stenseth, R.; Wahba, A.; Lydersen, S.; Klepstad, P. Long-term health-related quality of life and survival after cardiac surgery: A prospective study. J. Thorac. Cardiovasc. Surg. 2018, 156, 2183–2190.e2. [Google Scholar] [CrossRef]
- Ussia, G.P.; Mulè, M.; Barbanti, M.; Cammalleri, V.; Scarabelli, M.; Immè, S.; Capodanno, D.; Ciriminna, S.; Tamburino, C. Quality of life assessment after percutaneous aortic valve implantation. Eur. Heart J. 2009, 30, 1790–1796. [Google Scholar] [CrossRef] [Green Version]
- Koenig, H.G.; George, L.K.; Peterson, B.L.; Pieper, C.F. Depression in medically ill hospitalized older adults: Prevalence, characteristics, and course of symptoms according to six diagnostic schemes. Am. J. Psychiatry 1997, 154, 1376–1383. [Google Scholar] [CrossRef] [Green Version]
- Buss, T.; Kruk, A.; Wiśniewski, P.; Modlińska, A.; Janiszewska, J.; Lichodziejewska-Niemierko, M. Psychometric properties of the Polish version of the Multidimensional Fatigue Inventory-20 in Cancer Patients. J. Pain Symptom Manag. 2014, 48, 730–737. [Google Scholar] [CrossRef] [PubMed]
- Arnold, L.M. Understanding fatigue in major depressive disorder and other medical disorders. Psychosomatics 2008, 49, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Bjorner, J.B.; Wallenstein, G.V.; Martin, M.C.; Lin, P.; Blaisdell-Gross, B.; Piech, C.T.; Mody, S.H. Interpreting score differences in the SF-36 Vitality scale: Using clinical conditions and functional outcomes to define the minimally important difference. Curr. Med. Res. Opin. 2007, 23, 731–739. [Google Scholar] [CrossRef] [PubMed]
- Tully, P.J.; Baker, R.A.; Turnbull, D.A.; Winefield, H.R.; Knight, J.L. Negative emotions and quality of life six months after cardiac surgery: The dominant role of depression not anxiety symptoms. J. Behav. Med. 2009, 32, 510–522. [Google Scholar] [CrossRef] [PubMed]
- Appels, A. Exhaustion and coronary heart disease: The history of a scientific quest. Patient Educ. Couns. 2004, 55, 223–229. [Google Scholar] [CrossRef] [PubMed]
- Grant, S.W.; Ouzounian, M. Closing the gender gap in cardiac surgery outcomes: More work to be done. Eur. J. Cardio-Thorac. Surg. 2022, 61, 703–704. [Google Scholar] [CrossRef] [PubMed]
- Targum, S.D.; Fava, M. Fatigue as a residual symptom of depression. Innov. Clin. Neurosci. 2011, 8, 40–43. [Google Scholar]
- Contrada, R.J.; Boulifard, D.A.; Idler, E.L.; Krause, T.J.; Labouvie, E.W. Course of depressive symptoms in patients undergoing heart surgery: Confirmatory analysis of the factor pattern and latent mean structure of the Center for Epidemiologic Studies Depression Scale. Psychosom. Med. 2006, 68, 922–930. [Google Scholar] [CrossRef]

| N (%) a | |
|---|---|
| Age; mean (SD) | 65.14 (9.47) |
| Sex | |
| Women | 75 (34.6) |
| Men | 142 (65.4) |
| History of myocardial infarction | 86 (39.6) |
| Hypertension | 155 (71.4) |
| Diabetes mellitus | 62 (28.6) |
| Recent myocardial infarction | 50 (23.0) |
| History of percutaneous coronary intervention | 54 (24.9) |
| Atrial fibrillation/flutter | 27 (12.4) |
| Heart failure | 59 (27.2) |
| Weight of the operation | |
| Isolated OPCABG b/CABG c | 123 (56.7) |
| Single non-CABG | 44 (20.3) |
| Combined 2 or 3 procedures | 50 (23.0) |
| Extracorporeal circulation | 97 (44.7) |
| Mode of operation | |
| Elective | 133 (61.3) |
| Urgent | 68 (31.3) |
| Emergent | 16 (7.4) |
| Salvage | 0 (0) |
| NYHA Class d | |
| 0–I | 61 (28.1) |
| II–IV | 156 (71.9) |
| CCS Class e | |
| 0–I | 44 (20.3) |
| II–IV | 173 (79.7) |
| EUROscore f, mean (SD); median (min-max) | 1.86 (1.31); 1.49 (0.5–8.26) |
| Hospital stay, mean (SD), median (min-max) | 7.96 (2.68); 7 (5–25) |
| SF-12 Domain | Mean (SD) |
|---|---|
| Physical Functioning (PF) | 49.54 (30.80) |
| Role-Physical (RP) | 48.67 (22.60) |
| Bodily Pain (BP) | 60.48 (27.15) |
| General Health (GH) | 47.86 (19.92) |
| Vitality (VT) | 50.92 (25.78) |
| Social Functioning (SF) | 64.19 (26.95) |
| Role-Emotional (RE) | 65.44 (26.39) |
| Mental Health (MH) | 64.98 (20.74) |
| PCS a | 40.94 (7.86) |
| MCS b | 47.87 (10.0) |
| Depression risk c | 63 (29.03) |
| Method a | % of Total Variance Explained |
|---|---|
| PCA | 79.33 |
| KPCA | 80.66 |
| GPCA | 81.73 |
| CCPCA | 82.53 |
| LDA | 77.72 |
| NO | Centroid Class Principal Component AnalysisNumber of Principal Components | ||||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | ||
| Regg a | 0.678 | - | - | - | - | - | - |
| k-NN b | 0.713 | 0.717 | 0.711 | 0.721 | 0.712 | 0.718 | 0.711 |
| SVM c | 0.711 | 0.723 | 0.761 | 0.767 | 0.732 | 0.723 | 0.702 |
| MLP d | 0.732 | 0.739 | 0.745 | 0.782 | 0.803 | 0.766 | 0.743 |
| CART e | 0.712 | 0.730 | 0.742 | 0.780 | 0.819 | 0.767 | 0.723 |
| GNB f | 0.705 | 0.712 | 0.719 | 0.741 | 0.719 | 0.661 | 0.652 |
| Component | Eigenvalue | % of Total Variance | Cumulative Eigenvalue | Cumulative % |
|---|---|---|---|---|
| 1 | 3.73 | 31.55 | 3.73 | 31.55 |
| 2 | 2.33 | 27.55 | 6.06 | 59.10 |
| 3 | 2.19 | 15.33 | 8.25 | 74.43 |
| 4 | 1.44 | 7.43 | 9.69 | 81.86 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nowicka-Sauer, K.; Jarmoszewicz, K.; Molisz, A.; Sobczak, K.; Sauer, M.; Topolski, M. Applying Machine Learning to Construct a Model of Risk of Depression in Patients Following Cardiac Surgery with the Use of the SF-12 Survey. Int. J. Environ. Res. Public Health 2023, 20, 4876. https://doi.org/10.3390/ijerph20064876
Nowicka-Sauer K, Jarmoszewicz K, Molisz A, Sobczak K, Sauer M, Topolski M. Applying Machine Learning to Construct a Model of Risk of Depression in Patients Following Cardiac Surgery with the Use of the SF-12 Survey. International Journal of Environmental Research and Public Health. 2023; 20(6):4876. https://doi.org/10.3390/ijerph20064876
Chicago/Turabian StyleNowicka-Sauer, Katarzyna, Krzysztof Jarmoszewicz, Andrzej Molisz, Krzysztof Sobczak, Marta Sauer, and Mariusz Topolski. 2023. "Applying Machine Learning to Construct a Model of Risk of Depression in Patients Following Cardiac Surgery with the Use of the SF-12 Survey" International Journal of Environmental Research and Public Health 20, no. 6: 4876. https://doi.org/10.3390/ijerph20064876






