Needs and Attitudes of Older Chronic Back Pain Patients towards a Wearable for Ultrasound Biofeedback during Stabilization Exercises: A Qualitative Analysis
Abstract
1. Introduction
1.1. Conceptual Framework
1.2. Research Questions
- What are the attitudes of older CBPPs towards using a mobile ultrasound device to obtain biofeedback when performing SSE?
- What needs do older CBPPs have for using a mobile ultrasound device to obtain biofeedback when performing SSE?
- How do older CBPPs evaluate the usefulness of a mobile ultrasound device for obtaining biofeedback during the performance of SSE?
- What are the requirements of CBPPs regarding the usage scenario of a mobile ultrasound device for biofeedback during the performance of SSE?
2. Materials and Methods
2.1. Study Design
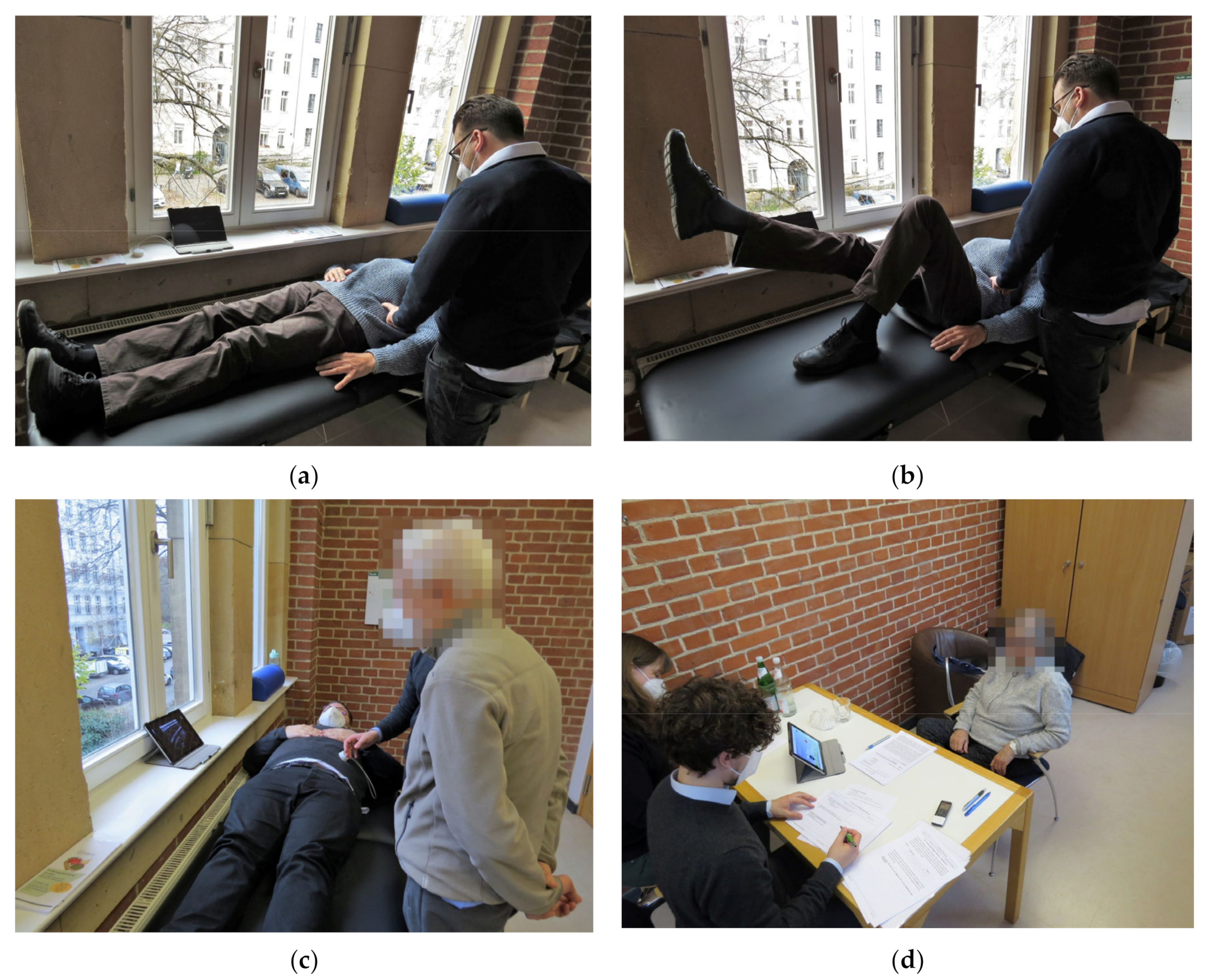
2.2. Procedure
2.2.1. Screening
- Chronic back pain lasting longer than 6 months;
- 65 years of age or older;
- Independent mobility (mobility without help of others).
- Cognitive impairment;
- Sensory and/or motor deficits;
- Inability to actively perform exercises (especially while lying on the back);
- Malignant diseases and tumors of the spine, or fibromyalgia.
2.2.2. Pilot Test
2.2.3. Study Procedure
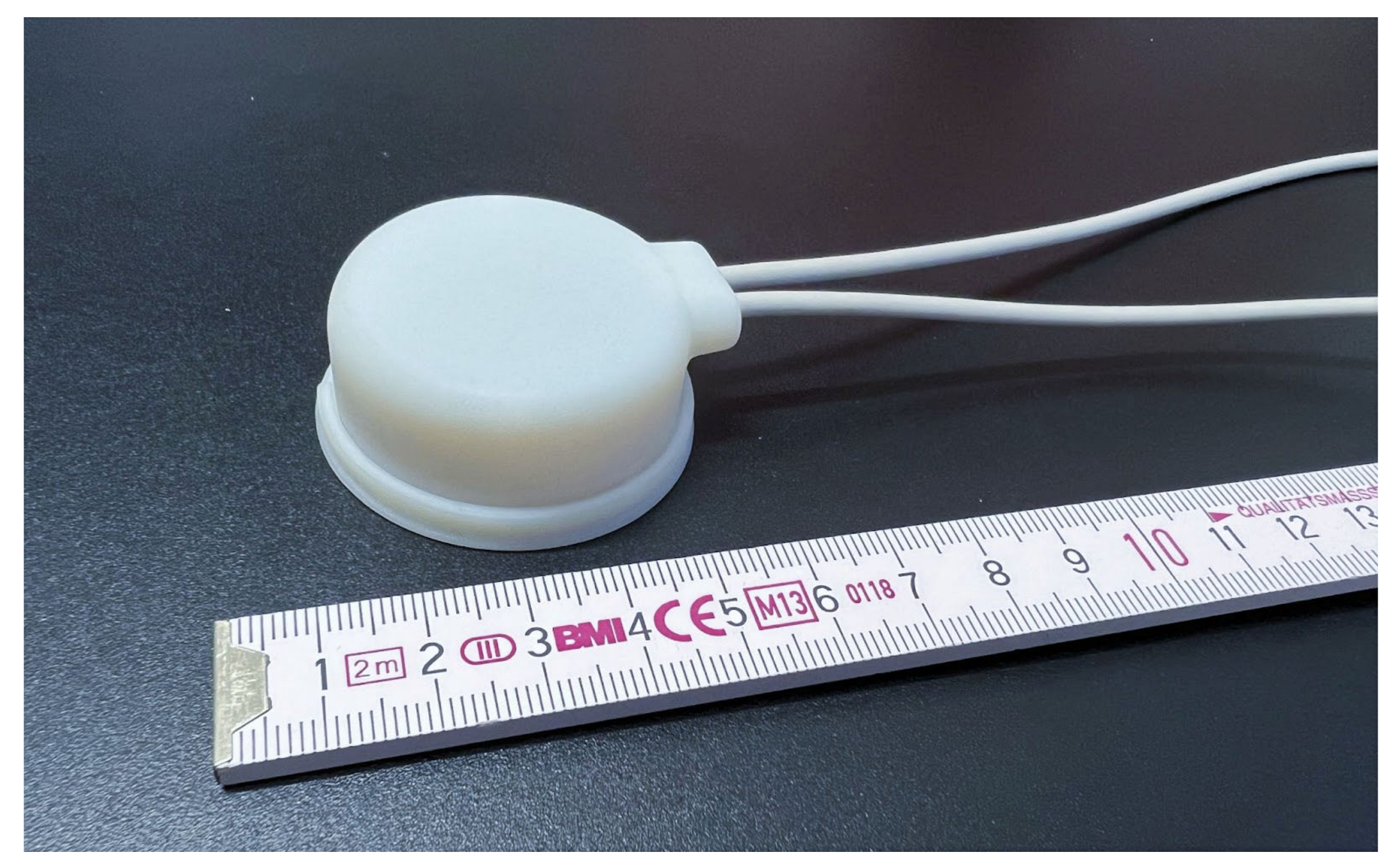
2.3. Materials
2.3.1. Affinity for Technology Interaction, German Version
2.3.2. Exercise Adherence Rating Scale
2.3.3. Mockup
2.4. Participant Selection
2.5. Data Collection and Analysis
3. Results
3.1. Research Participant Characteristics
3.1.1. Exercise Adherence
3.1.2. Affinity for Technology Interaction
3.2. Chronic Back Pain Management
3.3. Prior Experience with Segmental Stabilization Exercises
3.4. Prior Experience with Ultrasound in Physiotherapy
3.5. Feedback on Learning of Stabilization Exercises
3.6. Attitudes towards the Future System
3.6.1. Positive Attitudes towards the Future System
“So if it’s going to become part of the routine treatment, I’m convinced that it’s better to use artificial intelligence […] I’m convinced either the person using it [the physiotherapist] doesn’t recognize or doesn’t know exactly what’s really happening, doesn’t know the degree either, or doesn’t have time.” (P06, f, 70 y)
“A person sometimes says, I’ve explained this to you x times, why aren’t you doing it yet? That gets you down. When a technical system says, listen, you’re on the right track, but try a little harder. Then, that’s OK. You don’t have an emotional relationship with the device, you’re just a signal generator, and that’s fine.” (P05, m, 79 y)
3.6.2. Concerns about the Future System
3.7. Usefulness of the Future System
“Yes, yes, it is quite important that there is an objective system behind it. That is precisely the advantage of what you are aiming for here, I think. There are more relaxed physiotherapists and then there are more exact ones who look closely and so on. And that is a very big subjective human factor. And what you are developing here has the advantage that you can objectify it.” (P09, m, 78 y)
“The advantage is that you can really see how the muscles are moving. So before, when I did the exercise, they did show me that I can feel it. However, now it’s more convincing of course, I’m a more visual person.” (P13, m, 77 y)
3.7.1. Usefulness of the Future System in the Physiotherapy Setting
“The ratio of suffering older adults to physiotherapists is changing, yes. There are more and more old people and back pain patients and in relation to that there are less and less physiotherapists, that’s why I think you developed the system.” (P09, m, 78 y)
“Then, he [the physiotherapist] doesn’t have to be confronted with the new system. That is also an effort for the physiotherapist. If he has so and so many patients and has to apply the system, then he has extra work, that’s clear.” (P05, m, 79 y)
3.7.2. Usefulness of the Future System at Home
“Yes, but in itself, you don’t even need the physiotherapist, I think. If you have mastered the exercises. You can do them even better than the physiotherapist or more often or at the right time. For example, if you do it lying down, in the morning after you get up. You can’t do that with a physiotherapist.” (P09, m, 78 y)
“I can’t imagine that most people would get it right away […] there would have to be someone, at least in the initial phase. […] So there should be an initial control, that the person really does it right.” (P05, m, 79 y)
3.8. Requirements towards the Usage Scenario of the Future System
“After all, you have to do two things at once, one is the physical, doing the exercises. And secondly, you have to visually pay attention to when to relax and contract the muscles. It’s probably a matter of habit and then it works automatically.” (P05, m, 79 y)
4. Discussion
Strength and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| LBP | Lower-back pain |
| SSEs | Segmental stabilization exercises |
| TrA | Transverse abdominis muscle |
| LM | Lumbar multifidus muscle |
| IO | Internal abdominal oblique muscle |
| EO | External abdominal oblique muscle |
| RUSI | Rehabilitative ultrasound imaging |
| CBP | Chronic back pain |
| CBPP | Chronic back pain patients |
Appendix A
- What measures do you use with regard to your back pain?
- In therapy, deep muscle activation (e.g., abdominal muscles) is often taught to back pain patients.
- a.
- Did you have any prior experience with such stabilization exercises?
- b.
- Have you found the exercises to be effective?
- 3.
- How do your physical limitations or psychological barriers restrict you from exercising?
- 4.
- Have you already experienced the exercise in this or a similar kind with a physiotherapist?
- 5.
- Did the exercises cause you any difficulties?
- a.
- If yes, what was the difficulty of this task?
- 6.
- Has ultrasound been used in one of your prior physiotherapy sessions to help you visualize the contraction of the deep abdominal muscles?
- a.
- If yes, how did you feel about that experience?
- 7.
- What is your first impression of the system?
- 8.
- What do you think about the use of such a system within physiotherapy treatment?
- 9.
- If you think about the exercises you performed earlier:
- a.
- Do you think ultrasound imaging would help you in learning how to achieve targeted contraction of your deep abdominal muscles?
- b.
- Do you think the demonstration changed your perception of your abdominal muscles?
- 10.
- Do you have any concerns about using ultrasound in your physiotherapy treatment?
- 11.
- Do you have any general concerns using the ULTRAWEAR system?
- 19.
- Could you imagine using the system at home on your own without the supervision of a physiotherapist?
- 20.
- Do you have any further remarks you would like to share with us or issues you would like us to consider as we move forward with our project?
References
- Dionne, C.E.; Dunn, K.M.; Croft, P.R.; Nachemson, A.L.; Buchbinder, R.; Walker, B.F.; Wyatt, M.; Cassidy, J.D.; Rossignol, M.; Leboeuf-Yde, C.; et al. A Consensus Approach toward the Standardization of Back Pain Definitions for Use in Prevalence Studies. Spine (Phila Pa 1976) 2008, 33, 95–103. [Google Scholar] [CrossRef] [PubMed]
- Von Der Lippe, E.; Krause, L.; Prost, M.; Wengler, A.; Leddin, J.; Müller, A.; Zeisler, M.-L.; Anton, A.; Rommel, A.; BURDEN 2020 Study Group Prävalenz von Rücken- und Nackenschmerzen in Deutschland. Ergebnisse der Krankheitslast-Studie BURDEN 2020. J. Health Monit. 2021, 6, 2–14. [Google Scholar] [CrossRef] [PubMed]
- Stetts, D.M.; Freund, J.E.; Allison, S.C.; Carpenter, G. A Rehabilitative Ultrasound Imaging Investigation of Lateral Abdominal Muscle Thickness in Healthy Aging Adults. J. Geriatr. Phys. Ther. 2009, 32, 16–22. [Google Scholar] [CrossRef]
- Knauer, S.R.; Freburger, J.K.; Carey, T.S. Chronic Low Back Pain Among Older Adults: A Population-Based Perspective. J. Aging Health 2010, 22, 1213–1234. [Google Scholar] [CrossRef] [PubMed]
- Hayden, J.A.; Ellis, J.; Ogilvie, R.; Malmivaara, A.; van Tulder, M.W. Exercise Therapy for Chronic Low Back Pain. Cochrane Database Syst. Rev. 2021, 9, CD009790. [Google Scholar] [CrossRef] [PubMed]
- Vadalà, G.; Russo, F.; De Salvatore, S.; Cortina, G.; Albo, E.; Papalia, R.; Denaro, V. Physical Activity for the Treatment of Chronic Low Back Pain in Elderly Patients: A Systematic Review. J. Clin. Med. 2020, 9, 1023. [Google Scholar] [CrossRef]
- Wong, A.Y.; Karppinen, J.; Samartzis, D. Low Back Pain in Older Adults: Risk Factors, Management Options and Future Directions. Scoliosis Spinal Disord. 2017, 12, 14. [Google Scholar] [CrossRef]
- Simon, C.B.; Hicks, G.E. Paradigm Shift in Geriatric Low Back Pain Management: Integrating Influences, Experiences, and Consequences. Phys. Ther. 2018, 98, 434–446. [Google Scholar] [CrossRef]
- Bae, C.-R.; Jin, Y.; Yoon, B.-C.; Kim, N.-H.; Park, K.-W.; Lee, S.-H. Effects of Assisted Sit-up Exercise Compared to Core Stabilization Exercise on Patients with Non-Specific Low Back Pain: A Randomized Controlled Trial. J. Back Musculoskelet. Rehabil. 2018, 31, 871–880. [Google Scholar] [CrossRef]
- Kliziene, I.; Sipaviciene, S.; Klizas, S.; Imbrasiene, D. Effects of Core Stability Exercises on Multifidus Muscles in Healthy Women and Women with Chronic Low-Back Pain. J. Back Musculoskelet. Rehabil. 2015, 28, 841–847. [Google Scholar] [CrossRef]
- Hlaing, S.S.; Puntumetakul, R.; Khine, E.E.; Boucaut, R. Effects of Core Stabilization Exercise and Strengthening Exercise on Proprioception, Balance, Muscle Thickness and Pain Related Outcomes in Patients with Subacute Nonspecific Low Back Pain: A Randomized Controlled Trial. BMC Musculoskelet Disord 2021, 22, 998. [Google Scholar] [CrossRef] [PubMed]
- Akodu, A.; Akinbo, S.; Odebiyi, D. Effect of Stabilization Exercise on Lumbar Multifidus Muscle Thickness in Patients with Non-Specific Chronic Low Back Pain. Iran. Rehabil. J. 2014, 12, 6–10. [Google Scholar]
- Madokoro, S.; Yokogawa, M.; Miaki, H. Effect of the Abdominal Draw-In Maneuver and Bracing on Abdominal Muscle Thickness and the Associated Subjective Difficulty in Healthy Individuals. Healthcare 2020, 8, 496. [Google Scholar] [CrossRef] [PubMed]
- Basler, H.-D.; Luckmann, J.; Wolf, U.; Quint, S. Fear-Avoidance Beliefs, Physical Activity, and Disability in Elderly Individuals with Chronic Low Back Pain and Healthy Controls. Clin. J. Pain 2008, 24, 604–610. [Google Scholar] [CrossRef]
- Shaughnessy, M.; Caulfield, B. A Pilot Study to Investigate the Effect of Lumbar Stabilisation Exercise Training on Functional Ability and Quality of Life in Patients with Chronic Low Back Pain. Int. J. Rehabil. Res. 2004, 27, 297–301. [Google Scholar] [CrossRef]
- Richardson, C. Therapeutic Exercise for Spinal Segmental Stabilization: In Lower Back Pain; Churchill Livingstone: Edinburgh, UK, 1998; ISBN 978-0-443-05802-8. [Google Scholar]
- Rackwitz, B.; de Bie, R.; Limm, H.; von Garnier, K.; Ewert, T.; Stucki, G. Segmental Stabilizing Exercises and Low Back Pain. What Is the Evidence? A Systematic Review of Randomized Controlled Trials. Clin. Rehabil. 2006, 20, 553–567. [Google Scholar] [CrossRef] [PubMed]
- Mödinger, M.; Woll, A.; Wagner, I. Video-Based Visual Feedback to Enhance Motor Learning in Physical Education—A Systematic Review. Ger. J. Exerc. Sport Res. 2022, 52, 447–460. [Google Scholar] [CrossRef]
- Mannion, A.F.; Pulkovski, N.; Gubler, D.; Gorelick, M.; O’Riordan, D.; Loupas, T.; Schenk, P.; Gerber, H.; Sprott, H. Muscle Thickness Changes during Abdominal Hollowing: An Assessment of between-Day Measurement Error in Controls and Patients with Chronic Low Back Pain. Eur. Spine J. 2008, 17, 494–501. [Google Scholar] [CrossRef]
- Teyhen, D.; Koppenhaver, S. Rehabilitative Ultrasound Imaging. J. Physiother. 2011, 57, 196. [Google Scholar] [CrossRef]
- Taghipour, M.; Mohseni-Bandpei, M.A.; Behtash, H.; Abdollahi, I.; Rajabzadeh, F.; Pourahmadi, M.R.; Emami, M. Reliability of Real-Time Ultrasound Imaging for the Assessment of Trunk Stabilizer Muscles: A Systematic Review of the Literature. J. Ultrasound. Med. 2019, 38, 15–26. [Google Scholar] [CrossRef]
- Valera-Calero, J.A.; Fernández-de-las-Peñas, C.; Varol, U.; Ortega-Santiago, R.; Gallego-Sendarrubias, G.M.; Arias-Buría, J.L. Ultrasound Imaging as a Visual Biofeedback Tool in Rehabilitation: An Updated Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 7554. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Han, S.; Lee, D. Comparison of Abdominal Muscle Thickness According to Feedback Method Used during Abdominal Hollowing Exercise. J. Phys. Ther. Sci. 2016, 28, 2519–2521. [Google Scholar] [CrossRef] [PubMed]
- Critchley, D.J.; Coutts, F.J. Abdominal Muscle Function in Chronic Low Back Pain Patients: Measurement with Real-Time Ultrasound Scanning. Physiotherapy 2002, 88, 322–332. [Google Scholar] [CrossRef]
- Lin, S.; Zhu, B.; Zheng, Y.; Huang, G.; Zeng, Q.; Wang, C. Effect of Real-Time Ultrasound Imaging for Biofeedback on Trunk Muscle Contraction in Healthy Subjects: A Preliminary Study. BMC Musculoskelet. Disord. 2021, 22, 142. [Google Scholar] [CrossRef]
- Van, K.; Hides, J.A.; Richardson, C.A. The Use of Real-Time Ultrasound Imaging for Biofeedback of Lumbar Multifidus Muscle Contraction in Healthy Subjects. J. Orthop. Sport Phys. 2006, 36, 920–925. [Google Scholar] [CrossRef] [PubMed]
- Saleh, A.; Laradji, I.H.; Lammie, C.; Vazquez, D.; Flavell, C.A.; Azghadi, M.R. A Deep Learning Localization Method for Measuring Abdominal Muscle Dimensions in Ultrasound Images. IEEE J. Biomed. Health Inf. 2021, 25, 3865–3873. [Google Scholar] [CrossRef] [PubMed]
- Gillett, J.G.; Barrett, R.S.; Lichtwark, G.A. Reliability and Accuracy of an Automated Tracking Algorithm to Measure Controlled Passive and Active Muscle Fascicle Length Changes from Ultrasound. Comput. Methods Biomech. Biomed. Eng. 2013, 16, 678–687. [Google Scholar] [CrossRef]
- Turkistani, H.; AlMohimeed, I.; Ono, Y. Continuous Monitoring of Muscle Thickness Changes During Isometric Contraction Using a Wearable Ultrasonic Sensor. CMBES Proc. 2013, 36. [Google Scholar]
- Huang, Z.-H.; Ma, C.Z.-H.; Wang, L.-K.; Wang, X.-Y.; Fu, S.-N.; Zheng, Y.-P. Real-Time Visual Biofeedback via Wearable Ultrasound Imaging Can Enhance the Muscle Contraction Training Outcome of Young Adults. J. Strength Cond. Res. 2022, 36, 941. [Google Scholar] [CrossRef]
- Berner, F.; Endter, C.; Hagen, C. Older People and Digitisation, Findings and Recommendations from the Eighth Government Report on Older People; Government Report on Older People; Federal Ministry for Family Affairs, Senior Citizens, Women and Youth: Berlin, Germany, 2020; p. 52.
- Stamm, O.; Perotti, L. Expert Requirements for an Ultrasound-Based Wearable Using Deep Learning for Exercise Feedback in Older Chronic Back Pain Patients. In HCI International 2022—Late Breaking Papers: HCI for Health, Well-being, Universal Access and Healthy Aging; Duffy, V.G., Gao, Q., Zhou, J., Antona, M., Stephanidis, C., Eds.; Lecture Notes in Computer Science; Springer Nature: Cham, Switzerland, 2022; Volume 13521, pp. 158–173. ISBN 978-3-031-17901-3. [Google Scholar]
- Mayring, P. Qualitative Content Analysis: Theoretical Background and Procedures. In Approaches to Qualitative Research in Mathematics Education: Examples of Methodology and Methods; Bikner-Ahsbahs, A., Knipping, C., Presmeg, N., Eds.; Advances in Mathematics Education; Springer: Dordrecht, The Netherlands, 2015; pp. 365–380. ISBN 978-94-017-9181-6. [Google Scholar]
- Wessel, D.; Attig, C.; Franke, T. ATI-S—An Ultra-Short Scale for Assessing Affinity for Technology Interaction in User Studies. In Proceedings of the Proceedings of Mensch und Computer 2019; ACM: Hamburg, Germany, 2019; pp. 147–154. [Google Scholar]
- Newman-Beinart, N.A.; Norton, S.; Dowling, D.; Gavriloff, D.; Vari, C.; Weinman, J.A.; Godfrey, E.L. The Development and Initial Psychometric Evaluation of a Measure Assessing Adherence to Prescribed Exercise: The Exercise Adherence Rating Scale (EARS). Physiotherapy 2017, 103, 180–185. [Google Scholar] [CrossRef]
- Richardson, C.; Hodges, P.W.; Hides, J.; Richardson, C. Therapeutic Exercise for Lumbopelvic Stabilization: A Motor Control Approach for the Treatment and Prevention of Low Back Pain, 2nd ed.; Churchill Livingstone: Edinburgh, UK; New York, NY, USA, 2004; ISBN 978-0-443-07293-2. [Google Scholar]
- Kelley, J.F. An Empirical Methodology for Writing User-Friendly Natural Language Computer Applications. In Proceedings of the SIGCHI Conference on Human Factors in Computing Systems—CHI ’83; ACM Press: Boston, MA, USA, 1983; pp. 193–196. [Google Scholar]
- Green, P.; Wei-Haas, L. The Rapid Development of User Interfaces: Experience with the Wizard of OZ Method. Proc. Hum. Factors Soc. Annu. Meet. 1985, 29, 470–474. [Google Scholar] [CrossRef]
- Franke, T.; Attig, C.; Wessel, D. A Personal Resource for Technology Interaction: Development and Validation of the Affinity for Technology Interaction (ATI) Scale. Int. J. Hum. Comput. Interact. 2019, 35, 456–467. [Google Scholar] [CrossRef]
- Meade, L.B.; Bearne, L.M.; Godfrey, E.L. Comprehension and Face Validity of the Exercise Adherence Rating Scale in Patients with Persistent Musculoskeletal Pain. Musculoskelet. Care 2018, 16, 409–412. [Google Scholar] [CrossRef] [PubMed]
- Krippendorff, K. Computing Krippendorff’s Alpha-Reliability. Dep. Pap. (ASC) 2011, 1–10. [Google Scholar]
- Krippendorff, K. Content Analysis: An Introduction to Its Methodology, 2nd ed.; Sage: Thousand Oaks, CA, USA, 2004; ISBN 978-0-7619-1544-7. [Google Scholar]
- Von Korff, M.; Ormel, J.; Keefe, F.J.; Dworkin, S.F. Grading the Severity of Chronic Pain. Pain 1992, 50, 133–149. [Google Scholar] [CrossRef] [PubMed]
- Haefeli, M.; Elfering, A. Pain Assessment. Eur. Spine J. 2006, 15, S17–S24. [Google Scholar] [CrossRef]
- Krebs, E.E.; Lorenz, K.A.; Bair, M.J.; Damush, T.M.; Wu, J.; Sutherland, J.M.; Asch, S.M.; Kroenke, K. Development and Initial Validation of the PEG, a Three-Item Scale Assessing Pain Intensity and Interference. J. Gen. Intern. Med. 2009, 24, 733–738. [Google Scholar] [CrossRef]
- de Lira, M.R.; de Oliveira, A.S.; França, R.A.; Pereira, A.C.; Godfrey, E.L.; Chaves, T.C. The Brazilian Portuguese Version of the Exercise Adherence Rating Scale (EARS-Br) Showed Acceptable Reliability, Validity and Responsiveness in Chronic Low Back Pain. BMC Musculoskelet. Disord. 2020, 21, 294. [Google Scholar] [CrossRef]
- Luca, C.; Luca, Z. The use of support ultrasound as a working tool for the physiotherapist a review of the literature. JAHC 2021, 38–48. [Google Scholar] [CrossRef]
- Lacroix, A.; Hortobágyi, T.; Beurskens, R.; Granacher, U. Effects of Supervised vs. Unsupervised Training Programs on Balance and Muscle Strength in Older Adults: A Systematic Review and Meta-Analysis. Sport. Med. 2017, 47, 2341–2361. [Google Scholar] [CrossRef]
- Mannion, A.F.; Helbling, D.; Pulkovski, N.; Sprott, H. Spinal Segmental Stabilisation Exercises for Chronic Low Back Pain: Programme Adherence and Its Influence on Clinical Outcome. Eur. Spine J. 2009, 18, 1881–1891. [Google Scholar] [CrossRef]
- Cooper, K.; Smith, B.H.; Hancock, E. Patients’ Perceptions of Self-Management of Chronic Low Back Pain: Evidence for Enhancing Patient Education and Support. Physiotherapy 2009, 95, 43–50. [Google Scholar] [CrossRef] [PubMed]
- Hodges, P.W. Core Stability Exercise in Chronic Low Back Pain. Orthop. Clin. 2003, 34, 245–254. [Google Scholar] [CrossRef]
- Waddell, G. The Back Pain Revolution, 2nd ed.; Churchill Livingstone: Edinburgh, UK; New York, NY, USA, 2004; ISBN 978-0-443-07227-7. [Google Scholar]
- Galea, M.; Tisseverasinghe, S. A Randomised Controlled Trial of Transabdominal Ultrasound Biofeedback for Pelvic Floor Muscle Training in Older Women with Urinary Incontinence. Aust. Cont. J. 2013, 19, 38–44. [Google Scholar]
- Franco, M.R.; Howard, K.; Sherrington, C.; Ferreira, P.H.; Rose, J.; Gomes, J.L.; Ferreira, M.L. Eliciting Older People’s Preferences for Exercise Programs: A Best-Worst Scaling Choice Experiment. J. Physiother. 2015, 61, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Coombs, C.; Wilkinson, A.; Loan-Clarke, J.; Arnold, J.; Preston, D. Attractiveness of Physiotherapy in the National Health Service as a Career Choice. Physiotherapy 2003, 89, 575–583. [Google Scholar] [CrossRef]
- Kamper, S.J.; Apeldoorn, A.T.; Chiarotto, A.; Smeets, R.J.E.M.; Ostelo, R.W.J.G.; Guzman, J.; van Tulder, M.W. Multidisciplinary Biopsychosocial Rehabilitation for Chronic Low Back Pain: Cochrane Systematic Review and Meta-Analysis. BMJ 2015, 350, h444. [Google Scholar] [CrossRef] [PubMed]
- Herbert, W.J.; Heiss, D.G.; Basso, D.M. Influence of Feedback Schedule in Motor Performance and Learning of a Lumbar Multifidus Muscle Task Using Rehabilitative Ultrasound Imaging: A Randomized Clinical Trial. Phys. Ther. 2008, 88, 261–269. [Google Scholar] [CrossRef]
- Stanković, A.; Žikić, O.; Kocić, M.; Zlatanović, D.; Stanković, I. Overcoming Fear Avoidance Behavours and Kinesiophobia In Patients With Chronic Low Back Pain. FU Med. Biol. 2022, 24, 19–26. [Google Scholar] [CrossRef]
- Lin, S.; Zhu, B.; Zheng, Y.; Liu, S.; Wang, C. Effect of RUSI-Based Core Stability Exercise on Chronic Non-Specific Low Back Pain Patients: Study Protocol for a Randomised Controlled Trial. BMJ Open 2021, 11, e047317. [Google Scholar] [CrossRef]
- Sarafadeen, R.; Ganiyu, S.O.; Ibrahim, A.A.; Ismail, A.; Akindele, M.O.; Kaka, B.; Awotidebe, A.W. Effectiveness of Lumbar Stabilization Exercise with Real-Time Ultrasound Imaging Biofeedback on Lumbar Multifidus Muscle Cross-Sectional Area in Individuals with Non-Specific Chronic Low Back Pain: A Study Protocol for a Randomized Controlled Trial. Trials 2022, 23, 20. [Google Scholar] [CrossRef] [PubMed]
| Sociodemographic Data | Sample |
|---|---|
| Sample size total [n] Sex (Female/Male) | 15 |
| 8/7 | |
| Age [M (SD)] Age range [min.–max.] | 75.67 (5.04) 69–85 |
| Highest educational attainment [n] | |
| University | 6 |
| Advanced technical college certificate | 6 |
| High school | 1 |
| Secondary school | 1 |
| Main school | 1 |
| Marital status single married divorced widowed cohabiting | 1 10 0 4 0 |
| Pain intensity-NRS [M (SD)] 1 | 4.40 (1.91) |
| Pain Enjoyment of Life and General Activity Scale-PEG [M (SD)] 2 | 3.98 (2.19) |
| Associated diagnoses of chronification (most stated) [n] | |
| Unspecified LBP | 5 |
| Disc herniation | 3 |
| Spinal stenosis | 2 |
| Scoliosis | 2 |
| Comorbidities (most stated) [n] Hypertension Osteoarthritis | 3 2 |
| Code Group | Calculated Krippendorff’s cu-α |
|---|---|
| Chronic back pain management | 0.850 |
| Physical limitations due to chronic back pain | 0.827 |
| Prior experience with SSE | 0.769 |
| Learning of SSE exercises | 0.846 |
| Prior experience with ultrasound imaging | 0.925 |
| Attitudes towards the future system | 0.893 |
| Usefulness and usage scenario of the future system | 0.710 |
| Total score | 0.809 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Perotti, L.; Stamm, O.; Mesletzky, L.; Vorwerg, S.; Fournelle, M.; Müller-Werdan, U. Needs and Attitudes of Older Chronic Back Pain Patients towards a Wearable for Ultrasound Biofeedback during Stabilization Exercises: A Qualitative Analysis. Int. J. Environ. Res. Public Health 2023, 20, 4927. https://doi.org/10.3390/ijerph20064927
Perotti L, Stamm O, Mesletzky L, Vorwerg S, Fournelle M, Müller-Werdan U. Needs and Attitudes of Older Chronic Back Pain Patients towards a Wearable for Ultrasound Biofeedback during Stabilization Exercises: A Qualitative Analysis. International Journal of Environmental Research and Public Health. 2023; 20(6):4927. https://doi.org/10.3390/ijerph20064927
Chicago/Turabian StylePerotti, Luis, Oskar Stamm, Lisa Mesletzky, Susan Vorwerg, Marc Fournelle, and Ursula Müller-Werdan. 2023. "Needs and Attitudes of Older Chronic Back Pain Patients towards a Wearable for Ultrasound Biofeedback during Stabilization Exercises: A Qualitative Analysis" International Journal of Environmental Research and Public Health 20, no. 6: 4927. https://doi.org/10.3390/ijerph20064927
APA StylePerotti, L., Stamm, O., Mesletzky, L., Vorwerg, S., Fournelle, M., & Müller-Werdan, U. (2023). Needs and Attitudes of Older Chronic Back Pain Patients towards a Wearable for Ultrasound Biofeedback during Stabilization Exercises: A Qualitative Analysis. International Journal of Environmental Research and Public Health, 20(6), 4927. https://doi.org/10.3390/ijerph20064927






