A Case-Finding Protocol for High Cardiovascular Risk in a Primary Care Dental School—Model with Integrated Care
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethical Aspects
2.2. Data Recording
2.3. Participants and Recruitment
- Triage sessions, in which people without a current dentist are assessed by dental school staff for their suitability as patients for dental school students. These sessions were set up and supported by clinical staff members of the Peninsula Dental School/PDSE.
- Student/Staff clinics, which invited participants already undergoing treatment at the dental school to book an appointment for our case-finding clinic.
- Phone recruitment, which recruited participants who were missed at triage clinics or on the waiting list for triage clinics to optimise participant uptake. This involved sending participants the information sheet via email or letter after discussing the study with them via phone.
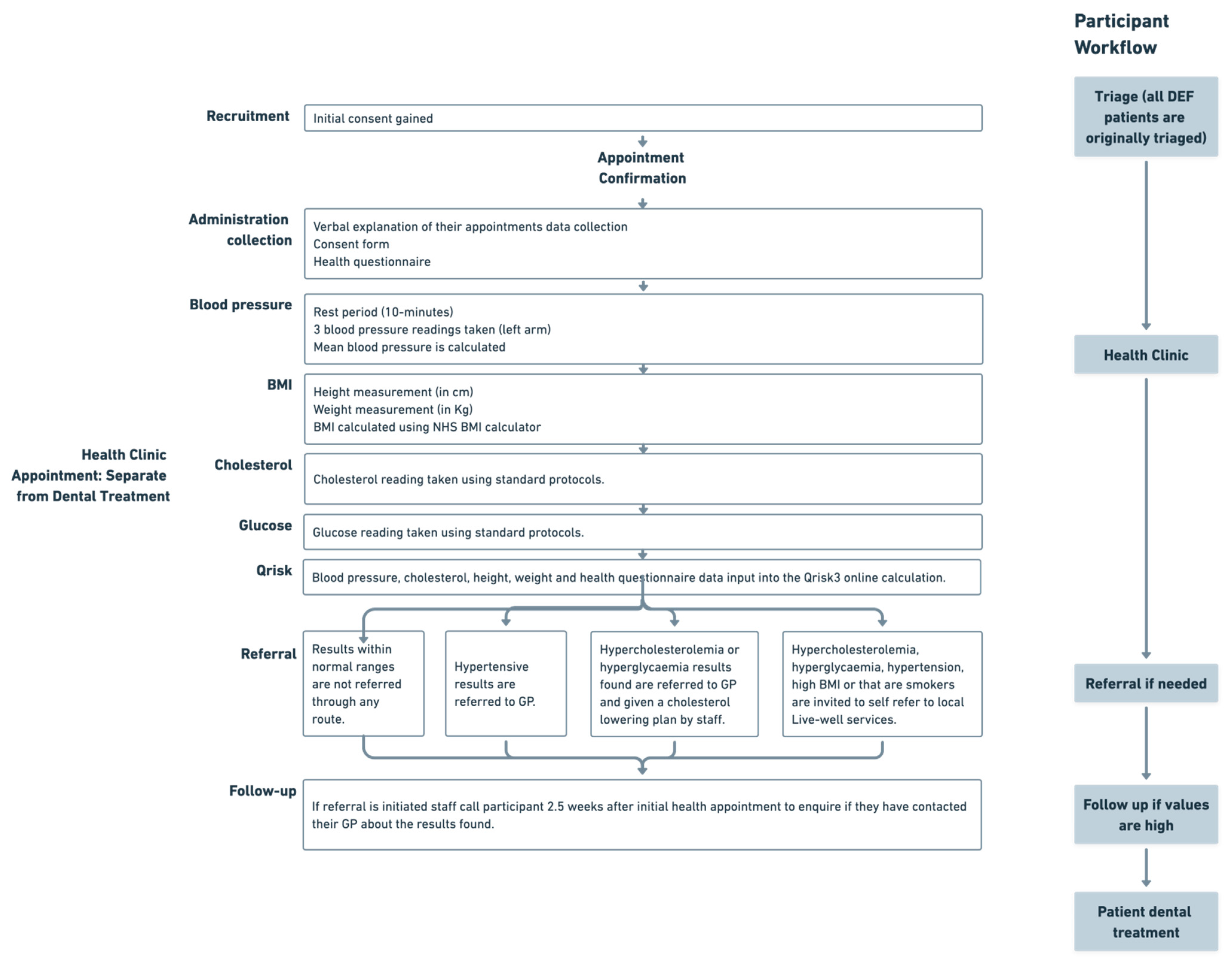
2.4. Applied Model
2.5. Referral and Follow Up
2.6. Identification and Management of Variables
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Robson, J.; Dostal, I.; Sheikh, A.; Eldridge, S.; Madurasinghe, V.; Griffiths, C.; Coupland, C.; Hippisley-Cox, J. The NHS Health Check in England: An evaluation of the first 4 years. BMJ Open 2015, 6, e008840. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Atkins, L.; Stefanidou, C.; Chadborn, T.; Thompson, K.; Michie, S.; Lorencatto, F. Influences on NHS Health Check behaviours: A systematic review. BMC Public Health 2020, 17, 1359. [Google Scholar] [CrossRef] [PubMed]
- NHS England. Missed GP Appointments Costing NHS Millions; NHS England. 2019. Available online: https://www.england.nhs.uk/2019/01/missed-gp-appointments-costing-nhs-millions/ (accessed on 2 February 2023).
- Fisher, R.F.; Croxson, C.H.; Ashdown, H.F.; Hobbs, F.R. GP views on strategies to cope with increasing workload: A qualitative interview study. Br. J. Gen. Pract. 2017, 67, e148–e156. [Google Scholar] [CrossRef] [PubMed]
- Kypridemos, C.; Allen, K.; Hickey, G.L.; Guzman-Castillo, M.; Bandosz, P.; Buchan, I.; Capewell, S.; O’Flaherty, M. Cardiovascular screening to reduce the burden from cardiovascular disease: Microsimulation study to quantify policy options. BMJ Open 2016, 353, i2793. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Edwards, L.A.; Campbell, P.; Taylor, D.J.; Shah, R.; Edgar, D.F.; Crabb, D.P. Healthy shopper? Blood pressure testing in a shopping centre Pop-Up in England. BMC Public Health 2019, 19, 42. [Google Scholar] [CrossRef] [PubMed]
- NICE. CVD Prevention: Detecting and Treating Hypertension 2022. Available online: https://stpsupport.nice.org.uk/cvd-prevention-hypertension/index.html#:~:text=Around%205.5%20million%20people%20in,among%20those%20who%20are%20diagnosed (accessed on 14 January 2023).
- British Heart Foundation. UK Factsheet. British Heart Foundation. 2022. Available online: https://www.bhf.org.uk/-/media/files/for-professionals/research/heart-statistics/bhf-cvd-statistics-uk-factsheet.pdf?rev=e771367bf0654a4dae85cbc9dbefae17&hash=76C0182379BB6EE118EC6F76FA35A158 (accessed on 2 February 2023).
- Deshpande, A.; Harris-Hayes, M.; Schootman, M. Epidemiology of Diabetes and Diabetes-Related Complications. Phys. Ther. 2008, 88, 1254–1264. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ohishi, M. Hypertension with diabetes mellitus: Physiology and pathology. Hypertens. Res. 2018, 41, 389–393. [Google Scholar] [CrossRef] [PubMed]
- British Heart Foundation. CVD Statistics BHF 2022, Chapter 2 Morbidity. British Heart Foundation. 2022. Available online: https://www.bhf.org.uk/what-we-do/our-research/heart-statistics/heart-statistics-publications/cardiovascular-disease-statistics-2022 (accessed on 2 February 2023).
- Fatima, S.; Mahmood, S. Combatting a silent killer—The importance of self-screening of blood pressure from an early age. EXCLI J. Exp. Clin. Sci. 2021, 20, 1326–1327. [Google Scholar]
- NHS. NHS Dental Statistics for England, 2021–2022, Annual Report. NHS Dental Statistics for England—2021–22: Annex 1 (Tables and Charts)—Table 4a. NHS Dental Statistics. 2022. Available online: https://digital.nhs.uk/data-and-information/publications/statistical/nhs-dental-statistics/2021-22-annual-report (accessed on 2 February 2023).
- Creanor, S.; Millward, B.A.; Demaine, A.; Price, L.; Smith, W.; Brown, N.; Creanor, S.L. Patients attitudes towards screening for diabeties and other medical conditions in the dental setting. Br. Dent. J. 2014, 216, E2. [Google Scholar] [CrossRef] [PubMed]
- Sproat, C.; Beheshti, S.; Harwood, A.N.; Crossbie, D. Should we screen for hypertension in general dental practice? BDJ 2009, 207, 275–277. [Google Scholar] [CrossRef] [PubMed]
- Greenberg, B.L.; Glick, M.; Goodchild, J.; Duda, P.W.; Conte, N.R.; Conte, M. Screening for cardiovascular risk factors in a dental setting. J. Am. Dent. Assoc. 2007, 138, 798–804. [Google Scholar] [CrossRef] [PubMed]
- Plymouth-City-Council. Index of Multiple Deprivation (IMD) 2019—Plymouth Summary Analsysis Plymouth City Council; Plymouth-City-Council; 2019. Available online: https://www.plymouth.gov.uk/sites/default/files/IMD%202019%20report%20Final%200.1.pdf (accessed on 2 February 2023).
- Kawabata, Y.; Ekuni, D.; Miyai, H.; Kataoka, K.; Yamane, M.; Mizutani, S.; Irie, K.; Azuma, T.; Tomofuji, T.; Iwasaki, Y.; et al. Relationship Between Prehypertension/Hypertension and Periodontal Disease: A Prospective Cohort Study. Am. J. Hypertens. 2016, 29, 388–396. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martin-Cabezas, R.; Seelam, N.; Petit, C.; Agossa, K.; Gaertner, S.; Tenenbaum, H.; Davideau, J.L.; Huck, O. Association between periodontitis and arterial hypertension: A systematic review and meta-analysis. Am. Heart J. 2016, 180, 98–112. [Google Scholar] [CrossRef] [PubMed]
- Plymouth-City-Council. Area Profile: Devonport Ward: Office of the Director of Public Health, Plymouth City Council. 2020. Available online: https://www.plymouth.gov.uk/sites/default/files/Devonport%20ward%20Profile_0.pdf (accessed on 22 December 2022).
- NHS. The NHS Long Term Plan: NHS. 2019. Available online: https://www.longtermplan.nhs.uk/about/ (accessed on 14 January 2023).
- Collaboration NRF. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: A pooled analysis of 1201 population-representative studies with 104 million participants. Lancet 2021, 398, 957–980. [Google Scholar] [CrossRef] [PubMed]
- Roche Diagnostics. Accutrend Plus Users Manual. 2012. Available online: https://beta-static.fishersci.com/content/dam/fishersci/en_US/documents/programs/healthcare/technical-documents/user-manuals/roche-accutrend-plus-users-manual.pdf (accessed on 2 February 2023).
- Qrisk. Qrisk3-2018. ClinRisk Ltd.. 2018. Available online: https://qrisk.org/ (accessed on 2 February 2023).
- NICE. Scenario: Management of People with an Estimated Risk of 10% or More. NICE. 2023. Available online: https://cks.nice.org.uk/topics/cvd-risk-assessment-management/management/cvd-risk-10percent-or-more/ (accessed on 2 February 2023).
- Andersson, H.; Hedstrom, L.; Berghm, H. White-coat hypertension detected during opportunistic blood pressure screening in a dental healthcare setting. Scand. J. Prim. Health Care 2021, 39, 348–354. [Google Scholar] [CrossRef] [PubMed]
- Livewell. Specialists in Community Health and Care: Livewell. 2022. Available online: https://www.livewellsouthwest.co.uk/ (accessed on 2 February 2023).
- Charity HUTC. Ultimate Cholesterol Loweing Plan. Heart UK The Cholesterol Charity. 2019. Available online: https://www.heartuk.org.uk/downloads/uclp-consumer-booklet.pdf (accessed on 2 February 2023).
- NICE. Hypertension in Adults: Diagnosis and Management NICE: NICE. 2022. Available online: https://www.nice.org.uk/guidance/ng136 (accessed on 14 January 2023).
- UK H. Understanding Your Cholesterol Test Results 2022. Available online: https://www.heartuk.org.uk/cholesterol/understanding-your-cholesterol-test-results-#triglycerides (accessed on 2 March 2023).
- NHS. High Blood Sugar (Hyperglycaemia): NHS. 2022. Available online: https://www.nhs.uk/conditions/high-blood-sugar-hyperglycaemia/ (accessed on 2 March 2023).
- NHS. Can I Eat and Drink before Having a Blood Test? NHS. 2021. Available online: https://www.nhs.uk/common-health-questions/operations-tests-and-procedures/can-i-eat-and-drink-before-having-a-blood-test/ (accessed on 2 March 2023).
- NICE. Type 1 Diabetes in Adults: Diagnosis and management. NICE. 2015. Available online: https://www.nice.org.uk/guidance/ng17/resources/type-1-diabetes-in-adults-diagnosis-and-management-1837276469701 (accessed on 2 February 2023).
- NICE. Type 2 Diabetes in Adults: Management: NICE. 2022. Available online: https://www.nice.org.uk/guidance/ng28 (accessed on 2 March 2023).
- NHS. What Is the Body Mass Index (BMI)? 2019. Available online: https://www.nhs.uk/common-health-questions/lifestyle/what-is-the-body-mass-index-bmi/ (accessed on 14 January 2023).
- NHS. NHS BMI Calculator. NHS BMI. 2022. Available online: https://www.nhs.uk/live-well/healthy-weight/bmi-calculator/ (accessed on 2 February 2023).
- NHS. Health Survey for England, 2019: Data Tables—Health Survey for England, 2019: Adults Health Data Tables; NHS Digital: Leeds, UK, 2020. [Google Scholar]
- Blok, S.; Haggenburg, S.; Collard, D.; Van Der Linden, E.L.; Galenkamp, H.; Moll van Charante, E.P.; Agyemang, C.; Van Den Born, B.H. The association between socioeconomic status and prevalence, awareness, treatment and control of hypertension in different ethnic groups: The Healthy Life in an Urban Setting study. J. Hypertens. 2022, 40, 897–907. [Google Scholar] [CrossRef] [PubMed]
- Kellogg, S.D.; Gobetti, J.P. Hypertension in a Dental School Patient Population. J. Dent. Educ. 2004, 68, 956–964. [Google Scholar] [CrossRef] [PubMed]
- NHS. Health Survey for England, 2019: Data Tables—Health Survey for England, 2019: Overweight and Obesity in Adults and Children Data Tables. NHS Digital. 2020. Available online: https://digital.nhs.uk/data-and-information/publications/statistical/health-survey-for-england/2019 (accessed on 2 February 2023).
- Al-Zahrami, M. Prehypertension and undiagnosed hypertension in a sample of dental school female patients. Int. J. Dent. Hyg. 2009, 9, 74–78. [Google Scholar] [CrossRef] [PubMed]
- GOV.UK. Ministry of Housing, UK. The English Indices of Deprivation 2019 (IoD2019). 2019. Available online: https://www.gov.uk/government/statistics/english-indices-of-deprivation-2019 (accessed on 2 February 2023).
- Eşer, I.; Khorshid, L.; Güneş, U.Y.; Demir, Y. The effect of different body positions on blood pressure. J. Clin. Nurs. 2007, 16, 1137–1140. [Google Scholar] [CrossRef] [PubMed]
- Abdul Aziz, A.F.; Mohd-Dom, T.N.; Mustafa, N.; Said, A.H.; Ayob, R.; Mohamed Isa, S.; Hatah, E.; Wan Puteh, S.E.; Mohd Alwi, M.F.F. Screening for type 2 diabetes and periodontitis patients(CODAPT-My@). A multidiciplinary care approach. BMC Health Serv. Res. 2022, 22, 1034. [Google Scholar] [CrossRef] [PubMed]
- MayoClinic. A1c Test MayoClinic Test Procedures: MayoClinic. 2022. Available online: https://www.mayoclinic.org/tests-procedures/a1c-test/about/pac-20384643 (accessed on 2 March 2023).
- British Medical Association. Pressures in General Practice Data Analysis. BMA. 2023. Available online: https://www.bma.org.uk/advice-and-support/nhs-delivery-and-workforce/pressures/pressures-in-general-practice-data-analysis (accessed on 2 February 2023).



| Characteristic | All Participants (n = 121) | Hypertensive Untreated (n = 22) | Hypertensive Uncontrolled (n = 11) | Hypercholesterolemia Untreated (n = 15) | Hypercholesterolemia Uncontrolled (n = 1) |
|---|---|---|---|---|---|
| Mean (±SD) | |||||
| Age (years) | 57.3 ± 10.4 | 58.0 ± 11.4 | 60.6 ± 10.4 | 53.3 ± 10.7 | 59 ± 0 |
| BMI (kg/cm) | 28.7 ± 6.2 | 28.2 ± 5.3 | 33.6 ± 5.9 | 29.9 ± 5.4 | 32.4 ± 0 |
| Systolic BP (mmHg) | 130.6 ± 17.1 | 148.6 ± 16.4 | 155.5 ± 12.3 | 129.6 ± 12.9 | 137 ± 0 |
| Diastolic BP (mmHg) | 79.0 ± 9.2 | 89.4 ± 8.3 | 84.6 ± 8.5 | 79.1 ± 8.1 | 78 ± 0 |
| n (%) | |||||
| Gender | |||||
| Female | 71 (58.7%) | 9 (40.9%) | 6 (54.5%) | 10 (66.7%) | 0 (0.0%) |
| Male | 50 (41.3%) | 13 (59.1%) | 5 (55.5%) | 5 (33.3%) | 1 (100%) |
| Smoking Status | |||||
| Never | 84 (69.4%) | 7 (31.8%) | 8 (72.7%) | 10 (66.7%) | 1 (100%) |
| Former | 12 (9.9%) | 1 (4.5%) | 2 (18.2%) | 2 (13.3%) | 0 (0.0%) |
| Current | 25 (20.7%) | 4 (18.2%) | 1 (9.1%) | 3 (20.0%) | 0 (0.0%) |
| Vape Use (Never smokers) | 2 (1.7%) | 1 (4.5%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Vape Use (Former smokers) | 4 (3.3%) | 0 (0.0%) | 1 (100%) | 1 (100%) | 0 (0.0%) |
| Race | |||||
| White | 118 (97.5%) | 22 (100%) | 11 (100%) | 15 (100%) | 1 (100%) |
| Other (Chinese, Mixed Race) | 3 (2.5%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| BMI | |||||
| Underweight | 4 (3.3%) | 1 (4.5%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Healthy | 32 (26.4%) | 4 18.2%) | 0 (0.0%) | 4 (26.7%) | 0 (0.0%) |
| Overweight | 43 (35.5%) | 8 (36.4%) | 5 (45.5%) | 5 (33.3%) | 0 (0.0%) |
| Obese | 42 (34.7%) | 9 (40.9%) | 6 (54.5) | 6 (40.0%) | 1 (100%) |
| Education | |||||
| School | 54 (44.6%) | 10 (45.5%) | 5 (45.5%) | 7 (46.7%) | 1(100%) |
| Collage | 17 (14.0%) | 2 (9.1%) | 0 (0.0%) | 2 (13.3%) | 0 (0.0%) |
| University or Higher | 34 (28.1%) | 8 (36.4%) | 3 (27.3%) | 6 (40.0%) | 0 (0.0%) |
| No answer | 16 (13.2%) | 2 (9.1%) | 3 (27.3%) | 0 (0.0%) | 0 (0.0%) |
| Diabetes (all type II) | 15 (12.4%) | 1 (4.5%) | 4 (36.4%) | 1 (6.7%) | 0 (0.0%) |
| Heart attack | 3 (2.5%) | 0 (0.0%) | 0 (0.0%) | 1 (6.7%) | 0 (0.0%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Doble, A.; Bescos, R.; Witton, R.; Shivji, S.; Ayres, R.; Brookes, Z. A Case-Finding Protocol for High Cardiovascular Risk in a Primary Care Dental School—Model with Integrated Care. Int. J. Environ. Res. Public Health 2023, 20, 4959. https://doi.org/10.3390/ijerph20064959
Doble A, Bescos R, Witton R, Shivji S, Ayres R, Brookes Z. A Case-Finding Protocol for High Cardiovascular Risk in a Primary Care Dental School—Model with Integrated Care. International Journal of Environmental Research and Public Health. 2023; 20(6):4959. https://doi.org/10.3390/ijerph20064959
Chicago/Turabian StyleDoble, Amazon, Raul Bescos, Robert Witton, Shabir Shivji, Richard Ayres, and Zoë Brookes. 2023. "A Case-Finding Protocol for High Cardiovascular Risk in a Primary Care Dental School—Model with Integrated Care" International Journal of Environmental Research and Public Health 20, no. 6: 4959. https://doi.org/10.3390/ijerph20064959





