Procrastination and Stress: A Conceptual Review of Why Context Matters
Abstract
:1. Procrastination and Stress: A Conceptual Review of Why Context Matters
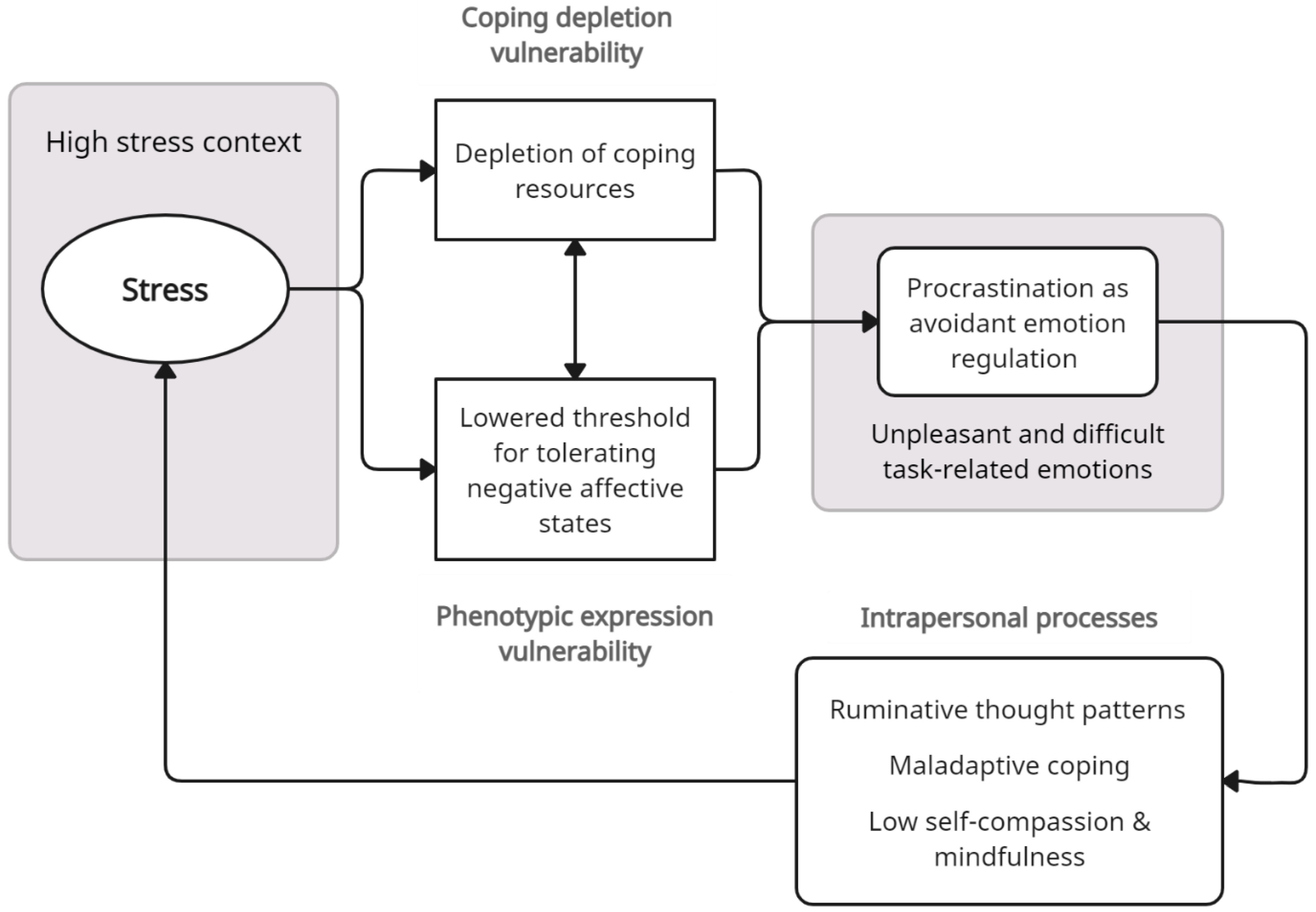
2. Procrastination, Stress, and Emotion Regulation
3. Stressful Contexts and Vulnerability for Procrastination
3.1. Coping Depletion Vulnerability
3.2. Phenotypic Expression Vulnerability
4. COVID-19 Stress and Vulnerability for Procrastination
4.1. Health Threats
4.2. Social Isolation and Loneliness
4.3. Remote Working
4.4. Financial Insecurity
5. Applications of a Stress Context Vulnerability Model of Procrastination
6. Implications and Future Directions
7. Conclusions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Ferrari, J.R.; Tice, D.M. Procrastination as a self-handicap for men and women: A task-avoidance strategy in a laboratory setting. J. Res. Personal. 2000, 34, 73–83. [Google Scholar] [CrossRef] [Green Version]
- Sirois, F.M.; Pychyl, T.A. Procrastination and the priority of short-term mood regulation: Consequences for future self. Soc. Personal. Psychol. Compass 2013, 7, 115–127. [Google Scholar] [CrossRef]
- Sirois, F.M.; Pychyl, T.A. (Eds.) Procrastination, Health, and Well-Being; Elsevier: Geneva, Switzerland, 2016. [Google Scholar]
- Flett, G.L.; Stainton, M.; Hewitt, P.; Sherry, S.; Lay, C. Procrastination automatic thoughts as a personality construct: An analysis of the procrastinatory cognitions inventory. J. Ration. Emot. Cogn. Behav. Ther. 2012, 30, 223–236. [Google Scholar] [CrossRef]
- Sirois, F.M. “I’ll look after my health, later”: A replication and extension of the procrastination–health model with community-dwelling adults. Personal. Individ. Differ. 2007, 43, 15–26. [Google Scholar] [CrossRef]
- Tice, D.M.; Baumeister, R.F. Longitudinal study of procrastination, performance, stress, and health: The costs and benefits of dawdling. Psychol. Sci. 1997, 8, 454–458. [Google Scholar] [CrossRef] [Green Version]
- Stead, R.; Shanahan, M.J.; Neufeld, R.W.J. “I’ll go to therapy, eventually”: Procrastination, stress and mental health. Personal. Individ. Differ. 2010, 49, 175–180. [Google Scholar] [CrossRef]
- Beutel, M.E.; Klein, E.M.; Aufenanger, S.; Brähler, E.; Dreier, M.; Müller, K.W.; Quiring, O.; Reinecke, L.; Schmutzer, G.; Stark, B.; et al. Procrastination, distress and life satisfaction across the age range—A German representative community study. PLoS ONE 2016, 11, e0148054. [Google Scholar] [CrossRef] [Green Version]
- Johansson, F.; Rozental, A.; Edlund, K.; Côté, P.; Sundberg, T.; Onell, C.; Rudman, A.; Skillgate, E. Associations between Procrastination and Subsequent Health Outcomes Among University Students in Sweden. JAMA Netw. Open 2023, 6, e2249346. [Google Scholar] [CrossRef]
- Sirois, F.M.; Kitner, R. Less adaptive or more maladaptive? A meta-analytic investigation of procrastination and coping. Eur. J. Personal. 2015, 29, 433–444. [Google Scholar] [CrossRef]
- Kelly, S.M.; Walton, H.R. “I’ll work out tomorrow”: The Procrastination in Exercise Scale. J. Health Psychol. 2021, 26, 2613–2625. [Google Scholar] [CrossRef]
- Sirois, F.M.; Melia-Gordon, M.L.; Pychyl, T.A. “I’ll look after my health, later”: An investigation of procrastination and health. Personal. Individ. Differ. 2003, 35, 1167–1184. [Google Scholar] [CrossRef]
- Sirois, F.M.; Giguère, B. Giving in when feeling less good: Procrastination, action control, and social temptations. Br. J. Soc. Psychol. 2018, 57, 404–427. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Buxton, O.M.; Kim, Y.; Haneuse, S.; Kawachi, I. Do procrastinators get worse sleep? Cross-sectional study of US adolescents and young adults. SSM Popul. Health 2020, 10, 100518. [Google Scholar] [CrossRef] [PubMed]
- Sirois, F.M.; Van Eerde, W.; Argiropoulou, M.I. Is procrastination related to sleep quality? Testing an extension of the procrastination-health model. Cogent Psychol. OA 2015, 2, 1074776. [Google Scholar] [CrossRef]
- Sirois, F.M.; Tosti, N. Lost in the moment? An investigation of procrastination, mindfulness, and well-being. J. Ration. Emot. Cogn. Behav. Ther. 2012, 30, 237–248. [Google Scholar] [CrossRef] [Green Version]
- Sirois, F.M. Is procrastination a vulnerability factor for hypertension and cardiovascular disease? Testing an extension of the procrastination-health model. J. Behav. Med. 2015, 38, 578–589. [Google Scholar] [CrossRef] [Green Version]
- Giguère, B.; Sirois, F.M.; Vaswani, M. Delaying things and feeling bad about it? A norm-based approach to procrastination. In Procrastination, Health, and Well-Being; Sirois, F.M., Pychyl, T.A., Eds.; Academic Press: San Diego, CA, USA, 2016; pp. 189–212. [Google Scholar]
- Pychyl, T.A.; Sirois, F.M. Procrastination, emotion regulation, and well-being. In Procrastination, Health, and Well-Being; Sirois, F.M., Pychyl, T., Eds.; Academic Press: London, UK, 2016; pp. 163–188. [Google Scholar]
- WHO. Coronavirus Disease (COVID-19) Pandemic. Available online: https://www.who.int/europe/emergencies/situations/covid-19 (accessed on 3 March 2023).
- Reinecke, L.; Meier, A.; Beutel, M.E.; Schemer, C.; Stark, B.; Wölfling, K.; Müller, K.W. The Relationship between Trait Procrastination, Internet Use, and Psychological Functioning: Results from a Community Sample of German Adolescents. Front. Psychol. 2018, 9, 913. [Google Scholar] [CrossRef] [PubMed]
- Sirois, F.M. Procrastination and stress: Exploring the role of self-compassion. Self Identity 2014, 13, 128–145. [Google Scholar] [CrossRef]
- Reinecke, L.; Meier, A.; Aufenanger, S.; Beutel, M.E.; Dreier, M.; Quiring, O.; Stark, B.; Wölfling, K.; Müller, K.W. Permanently online and permanently procrastinating? The mediating role of Internet use for the effects of trait procrastination on psychological health and well-being. New Media Soc. 2018, 20, 862–880. [Google Scholar] [CrossRef]
- Sirois, F.M.; Stride, C.; Pychyl, T.A. Procrastination and Health: A longitudinal Test of the Roles of Stress and Health Behaviours. Br. J. Health Psychol. 2023, forthcoming. [Google Scholar]
- Smyth, J.; Zawadzki, M.; Gerin, W. Stress and Disease: A Structural and Functional Analysis. Soc. Personal. Psychol. Compass 2013, 7, 217–227. [Google Scholar] [CrossRef] [Green Version]
- Stainton, M.; Lay, C.H.; Flett, G.L. Trait procrastinators and behavior/trait-specific cognitions. J. Soc. Behav. Personal. 2000, 15, 297–312. [Google Scholar]
- Phillips, W.J.; Hine, D.W. Self-compassion, physical health, and health behaviour: A meta-analysis. Health Psychol. Rev. 2019, 1–27. [Google Scholar] [CrossRef]
- Pascoe, M.C.; Thompson, D.R.; Jenkins, Z.M.; Ski, C.F. Mindfulness mediates the physiological markers of stress: Systematic review and meta-analysis. J. Psychiatr. Res. 2017, 95, 156–178. [Google Scholar] [CrossRef]
- Blunt, A.; Pychyl, T.A. Project systems of procrastinators: A personal project-analytic and action control perspective. Personal. Individ. Differ. 2005, 38, 1771–1780. [Google Scholar] [CrossRef]
- Haghbin, M.; McCaffrey, A.; Pychyl, T.A. The complexity of the relation between fear of failure and procrastination. J. Ration. Emot. Cogn. Behav. Ther. 2012, 30, 249–263. [Google Scholar] [CrossRef]
- Blunt, A.; Pychyl, T.A. Task aversiveness and procrastination: A multi-dimensional approach to task aversiveness across stages of personal projects. Personal. Individ. Differ. 2000, 24, 837–846. [Google Scholar] [CrossRef]
- Wohl, M.J.A.; Pychyl, T.A.; Bennett, S.H. I forgive myself, now I can study: How self-forgiveness for procrastinating can reduce future procrastination. Personal. Individ. Differ. 2010, 48, 803–808. [Google Scholar] [CrossRef]
- Eckert, M.; Ebert, D.D.; Lehr, D.; Sieland, B.; Berking, M. Overcome procrastination: Enhancing emotion regulation skills reduce procrastination. Learn. Individ. Differ. 2016, 52, 10–18. [Google Scholar] [CrossRef] [Green Version]
- Rad, H.S.; Samadi, S.; Sirois, F.M.; Goodarzi, H. Mindfulness intervention for academic procrastination: A randomized control trial. Learn. Individ. Differ. 2023, 101, 102244. [Google Scholar] [CrossRef]
- Tice, D.M.; Bratslavsky, E. Giving in to feel good: The place of emotion regulation in the context of general self-control. Psychol. Inq. 2000, 11, 149–159. [Google Scholar] [CrossRef]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal, and Coping; Springer: New York, NY, USA, 1984. [Google Scholar]
- Gross, J.J.; Thompson, R.A. Emotion regulation: Conceptual foundations. In Handbook of Emotion Regulation; Gross, J.J., Ed.; Guilford Press: New York, NY, USA, 2007; pp. 3–24. [Google Scholar]
- Carver, C.S.; Scheier, M.F.; Weintraub, J.K. Assessing coping strategies: A theoretically based approach. J. Personal. Soc. Psychol. 1989, 56, 267–283. [Google Scholar] [CrossRef]
- Taylor, S.E.; Sirois, F.M.; Molnar, D.M. Health Psychology, 5th ed.; McGraw-Hill Ryerson: Toronto, ON, USA, 2020. [Google Scholar]
- Hirotsu, C.; Tufik, S.; Andersen, M.L. Interactions between sleep, stress, and metabolism: From physiological to pathological conditions. Sleep Sci. 2015, 8, 143–152. [Google Scholar] [CrossRef] [Green Version]
- Cohen, S.; Janicki-Deverts, D.; Doyle, W.J.; Miller, G.E.; Frank, E.; Rabin, B.S.; Turner, R.B. Chronic stress, glucocorticoid receptor resistance, inflammation, and disease risk. Proc. Natl. Acad. Sci. USA 2012, 109, 5995–5999. [Google Scholar] [CrossRef] [Green Version]
- Carver, C.S.; Connor-Smith, J. Personality and coping. Annu. Rev. Psychol. 2010, 61, 679–704. [Google Scholar] [CrossRef] [Green Version]
- Matthews, G.; Campbell, S.E. Task-Induced Stress and Individual Differences in Coping. Proc. Hum. Factors Ergon. Soc. Annu. Meet. 1998, 42, 821–825. [Google Scholar] [CrossRef]
- Erbiçer, E.S.; Metin, A.; Çetinkaya, A.; Şen, S. The Relationship between Fear of COVID-19 and Depression, Anxiety, and Stress. Eur. Psychol. 2021, 26, 323–333. [Google Scholar] [CrossRef]
- Zheng, J.; Morstead, T.; Sin, N.; Klaiber, P.; Umberson, D.; Kamble, S.; DeLongis, A. Psychological distress in North America during COVID-19: The role of pandemic-related stressors. Soc. Sci. Med. 2021, 270, 113687. [Google Scholar] [CrossRef]
- Strauss, G.P.; Ossenfort, K.L.; Whearty, K.M. Reappraisal and Distraction Emotion Regulation Strategies Are Associated with Distinct Patterns of Visual Attention and Differing Levels of Cognitive Demand. PLoS ONE 2016, 11, e0162290. [Google Scholar] [CrossRef]
- Charles, S.T. Strength and vulnerability integration: A model of emotional well-being across adulthood. Psychol. Bull. 2010, 136, 1068–1091. [Google Scholar] [CrossRef] [Green Version]
- Holahan, C.J.; Moos, R.H.; Holahan, C.K.; Brennan, P.L.; Schutte, K.K. Stress generation, avoidance coping, and depressive symptoms: A 10-year model. J. Consult. Clin. Psychol. 2005, 73, 658–666. [Google Scholar] [CrossRef] [Green Version]
- Gustavson, D.E.; Miyake, A.; Hewitt, J.K.; Friedman, N.P. Genetic relations among procrastination, impulsivity, and goal-management ability: Implications for the evolutionary origin of procrastination. Psychol. Sci. 2014, 25, 1178–1188. [Google Scholar] [CrossRef] [Green Version]
- Briley, D.A.; Tucker-Drob, E.M. Genetic and environmental continuity in personality development: A meta-analysis. Psychol. Bull. 2014, 140, 1303–1331. [Google Scholar] [CrossRef] [Green Version]
- Coricelli, G.; Critchley, H.D.; Joffily, M.; O’Doherty, J.P.; Sirigu, A.; Dolan, R.J. Regret and its avoidance: A neuroimaging study of choice behavior. Nat. Neurosci. 2005, 8, 1255–1262. [Google Scholar] [CrossRef] [Green Version]
- Kashani, M.; Eliasson, A.; Vernalis, M. Perceived stress correlates with disturbed sleep: A link connecting stress and cardiovascular disease. Stress 2012, 15, 45–51. [Google Scholar] [CrossRef]
- Lund, H.G.; Reider, B.D.; Whiting, A.B.; Prichard, J.R. Sleep patterns and predictors of disturbed sleep in a large population of college students. J. Adolesc. Health 2010, 46, 124–132. [Google Scholar] [CrossRef]
- Liu, J.C.J.; Verhulst, S.; Massar, S.A.A.; Chee, M.W.L. Sleep Deprived and Sweating It Out: The Effects of Total Sleep Deprivation on Skin Conductance Reactivity to Psychosocial Stress. Sleep 2015, 38, 155–159. [Google Scholar] [CrossRef]
- Goldstein, A.N.; Walker, M.P. The Role of Sleep in Emotional Brain Function. Annu. Rev. Clin. Psychol. 2014, 10, 679–708. [Google Scholar] [CrossRef] [Green Version]
- Schwarz, J.; Axelsson, J.; Gerhardsson, A.; Tamm, S.; Fischer, H.; Kecklund, G.; Åkerstedt, T. Mood impairment is stronger in young than in older adults after sleep deprivation. J. Sleep Res. 2019, 28, e12801. [Google Scholar] [CrossRef] [Green Version]
- Kechter, A.; Leventhal, A.M. Longitudinal Association of Sleep Problems and Distress Tolerance during Adolescence. Behav. Med. 2019, 45, 240–248. [Google Scholar] [CrossRef]
- Folkman, S. Personal control and stress and coping processes: A theoretical analysis. J. Personal. Soc. Psychol. 1984, 46, 839–852. [Google Scholar] [CrossRef]
- Monnig, M.A.; Clark, S.E.; Avila, J.C.; Sokolovsky, A.W.; Treloar Padovano, H.; Goodyear, K.; Aston, E.R.; Haass-Koffler, C.L.; Tidey, J.W.; Ahluwalia, J.S.; et al. COVID-19-Related Stressors and Clinical Mental Health Symptoms in a Northeast US Sample. Int. J. Environ. Res. Public Health 2023, 20, 1367. [Google Scholar] [CrossRef] [PubMed]
- Fostervold, K.I.; Ludvigsen, S.; Strømsø, H.I. Students’ time management and procrastination in the wake of the pandemic. Educ. Psychol. 2022, 42, 1223–1240. [Google Scholar] [CrossRef]
- Unda-López, A.; Osejo-Taco, G.; Vinueza-Cabezas, A.; Paz, C.; Hidalgo-Andrade, P. Procrastination during the COVID-19 Pandemic: A Scoping Review. Behav. Sci. 2022, 12, 38. [Google Scholar] [CrossRef] [PubMed]
- Shanahan, L.; Steinhoff, A.; Bechtiger, L.; Murray, A.L.; Nivette, A.; Hepp, U.; Ribeaud, D.; Eisner, M. Emotional distress in young adults during the COVID-19 pandemic: Evidence of risk and resilience from a longitudinal cohort study. Psychol. Med. 2022, 52, 824–833. [Google Scholar] [CrossRef] [PubMed]
- von Keyserlingk, L.; Yamaguchi-Pedroza, K.; Arum, R.; Eccles, J.S. Stress of university students before and after campus closure in response to COVID-19. J. Community Psychol. 2022, 50, 285–301. [Google Scholar] [CrossRef] [PubMed]
- Taylor, S. COVID Stress Syndrome: Clinical and Nosological Considerations. Curr. Psychiatry Rep. 2021, 23, 19. [Google Scholar] [CrossRef]
- Vindegaard, N.; Benros, M.E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav. Immun. 2020, 89, 531–542. [Google Scholar] [CrossRef]
- Wong, A.K.F.; Kim, S.; Kim, J.; Han, H. How the COVID-19 pandemic affected hotel Employee stress: Employee perceptions of occupational stressors and their consequences. Int. J. Hosp. Manag. 2021, 93, 102798. [Google Scholar] [CrossRef]
- Sirois, F.M.; Owens, J. Factors associated with psychological distress in health-care workers during an infectious disease outbreak: A rapid systematic review of the evidence. Front. Psychiatry 2021, 11, 589545. [Google Scholar] [CrossRef]
- Garfin, D.R.; Silver, R.C.; Holman, E.A. The novel coronavirus (COVID-2019) outbreak: Amplification of public health consequences by media exposure. Health Psychol. 2020, 39, 355–357. [Google Scholar] [CrossRef] [PubMed]
- Luo, F.; Ghanei Gheshlagh, R.; Dalvand, S.; Saedmoucheshi, S.; Li, Q. Systematic Review and Meta-Analysis of Fear of COVID-19. Front. Psychol. 2021, 12, 661078. [Google Scholar] [CrossRef]
- Doğanülkü, H.A.; Korkmaz, O.; Griffiths, M.D.; Pakpour, A.H. Fear of COVID-19 lead to procrastination among Turkish university students: The mediating role of intolerance of uncertainty. BMC Psychol. 2021, 9, 178. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sepúlveda-Loyola, W.; Rodríguez-Sánchez, I.; Pérez-Rodríguez, P.; Ganz, F.; Torralba, R.; Oliveira, D.V.; Rodríguez-Mañas, L. Impact of Social Isolation Due to COVID-19 on Health in Older People: Mental and Physical Effects and Recommendations. J. Nutr. Health Aging 2020, 24, 938–947. [Google Scholar] [CrossRef]
- Hamza, C.A.; Ewing, L.; Heath, N.L.; Goldstein, A.L. When social isolation is nothing new: A longitudinal study on psychological distress during COVID-19 among university students with and without preexisting mental health concerns. Can. Psychol. /Psychol. Can. 2021, 62, 20–30. [Google Scholar] [CrossRef]
- Elmer, T.; Mepham, K.; Stadtfeld, C. Students under lockdown: Comparisons of students’ social networks and mental health before and during the COVID-19 crisis in Switzerland. PLoS ONE 2020, 15, e0236337. [Google Scholar] [CrossRef]
- de Jong-Gierveld, J. Developing and testing a model of loneliness. J. Pers. Soc. Psychol. 1987, 53, 119–128. [Google Scholar] [CrossRef]
- Lee, C.M.; Cadigan, J.M.; Rhew, I.C. Increases in Loneliness among Young Adults during the COVID-19 Pandemic and Association With Increases in Mental Health Problems. J. Adolesc. Health 2020, 67, 714–717. [Google Scholar] [CrossRef]
- Buecker, S.; Horstmann, K.T.; Krasko, J.; Kritzler, S.; Terwiel, S.; Kaiser, T.; Luhmann, M. Changes in daily loneliness for German residents during the first four weeks of the COVID-19 pandemic. Soc. Sci. Med. 2020, 265, 113541. [Google Scholar] [CrossRef]
- McHugh, J.E.; Lawlor, B.A. Perceived stress mediates the relationship between emotional loneliness and sleep quality over time in older adults. Br. J. Health Psychol. 2013, 18, 546–555. [Google Scholar] [CrossRef] [PubMed]
- Hawkley, L.C.; Cacioppo, J.T. Loneliness and pathways to disease. Brain Behav. Immun. 2003, 17, 98–105. [Google Scholar] [CrossRef] [PubMed]
- Szkody, E.; Stearns, M.; Stanhope, L.; McKinney, C. Stress-Buffering Role of Social Support during COVID-19. Fam. Process 2021, 60, 1002–1015. [Google Scholar] [CrossRef] [PubMed]
- Shi, X.; Wang, S.; Liu, S.; Zhang, T.; Chen, S.; Cai, Y. Are procrastinators psychologically healthy? Association between psychosocial problems and procrastination among college students in Shanghai, China: A syndemic approach. Psychol. Health Med. 2019, 24, 570–577. [Google Scholar] [CrossRef] [PubMed]
- Yildiz, B.; Iskender, M. The secure attachment style oriented psycho-educational program for reducing intolerance of uncertainty and academic procrastination. Curr. Psychol. 2021, 40, 1850–1863. [Google Scholar] [CrossRef]
- Toscano, F.; Zappalà, S. Social Isolation and Stress as Predictors of Productivity Perception and Remote Work Satisfaction during the COVID-19 Pandemic: The Role of Concern about the Virus in a Moderated Double Mediation. Sustainability 2020, 12, 9804. [Google Scholar] [CrossRef]
- Fourtounas, A.; Thomas, S.J. Cognitive factors predicting checking, procrastination and other maladaptive behaviours: Prospective versus Inhibitory Intolerance of Uncertainty. J. Obs. Compuls. Relat. Disord. 2016, 9, 30–35. [Google Scholar] [CrossRef]
- Wang, B.; Liu, Y.; Qian, J.; Parker, S.K. Achieving Effective Remote Working During the COVID-19 Pandemic: A Work Design Perspective. Appl. Psychol. 2021, 70, 16–59. [Google Scholar] [CrossRef]
- Xiang, S.; Rasool, S.; Hang, Y.; Javid, K.; Javed, T.; Artene, A.E. The Effect of COVID-19 Pandemic on Service Sector Sustainability and Growth. Front. Psychol. 2021, 12, 1178. [Google Scholar] [CrossRef] [PubMed]
- Kim, O.S.; Parker, J.A.; Schoar, A. Revenue Collapses and the Consumption of Small Business Owners in the Early Stages of the COVID-19 Pandemic. Natl. Bur. Econ. Res. Work. Pap. Ser. 2020, 28151. [Google Scholar] [CrossRef]
- Cheng, Z.; Mendolia, S.; Paloyo, A.R.; Savage, D.A.; Tani, M. Working parents, financial insecurity, and childcare: Mental health in the time of COVID-19 in the UK. Rev. Econ. Househ. 2021, 19, 123–144. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.R.; Previtero, A. Procrastination, Present-Biased Preferences, and Financial Behaviors. In Proceedings of the Prepared for the 16th Annual Joint Meeting of the Retirement Research Consortium, Washington, DC, USA, 7–8 August 2014. [Google Scholar]
- Gamst-Klaussen, T.; Steel, P.; Svartdal, F. Procrastination and Personal Finances: Exploring the Roles of Planning and Financial Self-Efficacy. Front. Psychol. 2019, 10, 775. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Topa, G.; Lunceford, G.; Boyatzis, R.E. Financial Planning for Retirement: A Psychosocial Perspective. Front. Psychol. 2018, 8, 2238. [Google Scholar] [CrossRef] [PubMed]
- Klontz, B.T.; Zabek, F.; Taylor, C.D.; Bivens, A.; Horwitz, E.; Klontz, P.T.; Tharp, D.T.; Lurtz, M. The Sentimental Savings Study: Using Financial Psychology to Increase Personal Savings. J. Financ. Plan. 2019, 32, 44–55. [Google Scholar]
- De Cock, D.; Doumen, M.; Vervloesem, C.; Van Breda, A.; Bertrand, D.; Pazmino, S.; Westhovens, R.; Verschueren, P. Psychological stress in rheumatoid arthritis: A systematic scoping review. Semin. Arthritis Rheum. 2022, 55, 152014. [Google Scholar] [CrossRef]
- Sirois, F.M.; Toussaint, L.; Hirsch, J.K.; Kohls, N.; Weber, A.; Offenbächer, M. Trying to be perfect in an imperfect world: A person-centred test of perfectionism and health in fibromyalgia patients versus healthy controls. Personal. Individ. Differ. 2019, 137, 27–32. [Google Scholar] [CrossRef]
- Sirois, F.M.; Molnar, D.S. Perfectionism and maladaptive coping styles in patients with chronic fatigue syndrome, irritable bowel syndrome and fibromyalgia/arthritis and in healthy controls. Psychother. Psychosom. 2014, 83, 384–385. [Google Scholar] [CrossRef]
- Voth, J.; Sirois, F.M. The role of self-blame and responsibility in adjustment to inflammatory bowel disease. Rehabil. Psychol. 2009, 54, 99–108. [Google Scholar] [CrossRef]
- Choi, S.L.; Heo, W.; Cho, S.H.; Lee, P. The links between job insecurity, financial well-being and financial stress: A moderated mediation model. Int. J. Consum. Stud. 2020, 44, 353–360. [Google Scholar] [CrossRef]
- De Witte, H.; Pienaar, J.; De Cuyper, N. Review of 30 Years of Longitudinal Studies on the Association between Job Insecurity and Health and Well-Being: Is There Causal Evidence? Aust. Psychol. 2016, 51, 18–31. [Google Scholar] [CrossRef]
- Brandt, L.; Liu, S.; Heim, C.; Heinz, A. The effects of social isolation stress and discrimination on mental health. Transl. Psychiatry 2022, 12, 398. [Google Scholar] [CrossRef]
- Wolff, J.L.; Spillman, B.C.; Freedman, V.A.; Kasper, J.D. A National Profile of Family and Unpaid Caregivers Who Assist Older Adults with Health Care Activities. JAMA Intern. Med. 2016, 176, 372–379. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gonzalez-Guarda, R.M.; Stafford, A.M.; Nagy, G.A.; Befus, D.R.; Conklin, J.L. A Systematic Review of Physical Health Consequences and Acculturation Stress among Latinx Individuals in the United States. Biol. Res. Nurs. 2021, 23, 362–374. [Google Scholar] [CrossRef]
- Zhang, J.; Goodson, P. Predictors of international students’ psychosocial adjustment to life in the United States: A systematic review. Int. J. Intercult. Relat. 2011, 35, 139–162. [Google Scholar] [CrossRef]
- Hauge, L.J.; Skogstad, A.; Einarsen, S. The relative impact of workplace bullying as a social stressor at work. Scand. J. Psychol. 2010, 51, 426–433. [Google Scholar] [CrossRef] [PubMed]
- Neff, K.D. Self-compassion: An alternative conceptualization of a healthy attitude toward oneself. Self Identity 2003, 2, 85–101. [Google Scholar] [CrossRef] [Green Version]
- Breines, J.G.; Thoma, M.V.; Gianferante, D.; Hanlin, L.; Chen, X.; Rohleder, N. Self-compassion as a predictor of interleukin-6 response to acute psychosocial stress. Brain Behav. Immun. 2014, 37, 109–114. [Google Scholar] [CrossRef] [Green Version]
- Arch, J.J.; Brown, K.W.; Dean, D.J.; Landy, L.N.; Brown, K.D.; Laudenslager, M.L. Self-compassion training modulates alpha-amylase, heart rate variability, and subjective responses to social evaluative threat in women. Psychoneuroendocrinology 2014, 42, 49–58. [Google Scholar] [CrossRef] [Green Version]
- Germer, C.K.; Neff, K.D. Self-compassion in clinical practice. J. Clin. Psychol. 2013, 69, 856–867. [Google Scholar] [CrossRef]
- Sharma, M.; Rush, S.E. Mindfulness-based stress reduction as a stress management intervention for healthy individuals: A systematic review. J. Evid. Based Complement. Altern. Med. 2014, 19, 271–286. [Google Scholar] [CrossRef] [Green Version]
- Kriakous, S.A.; Elliott, K.A.; Lamers, C.; Owen, R. The Effectiveness of Mindfulness-Based Stress Reduction on the Psychological Functioning of Healthcare Professionals: A Systematic Review. Mindfulness 2021, 12, 1–28. [Google Scholar] [CrossRef] [PubMed]
- Schutte, N.S.; del Pozo de Bolger, A. Greater Mindfulness is Linked to Less Procrastination. Int. J. Appl. Posit. Psychol. 2020, 5, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Taylor, S.E.; Stanton, A.L. Coping Resources, Coping Processes, and Mental Health. Annu. Rev. Clin. Psychol. 2007, 3, 377–401. [Google Scholar] [CrossRef] [PubMed] [Green Version]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sirois, F.M. Procrastination and Stress: A Conceptual Review of Why Context Matters. Int. J. Environ. Res. Public Health 2023, 20, 5031. https://doi.org/10.3390/ijerph20065031
Sirois FM. Procrastination and Stress: A Conceptual Review of Why Context Matters. International Journal of Environmental Research and Public Health. 2023; 20(6):5031. https://doi.org/10.3390/ijerph20065031
Chicago/Turabian StyleSirois, Fuschia M. 2023. "Procrastination and Stress: A Conceptual Review of Why Context Matters" International Journal of Environmental Research and Public Health 20, no. 6: 5031. https://doi.org/10.3390/ijerph20065031





