Developing Medication Review Competency in Undergraduate Pharmacy Training: A Self-Assessment by Third-Year Students
Abstract
:1. Introduction
2. Methods
Ethical Considerations
3. Results
3.1. Prescription Review Competency

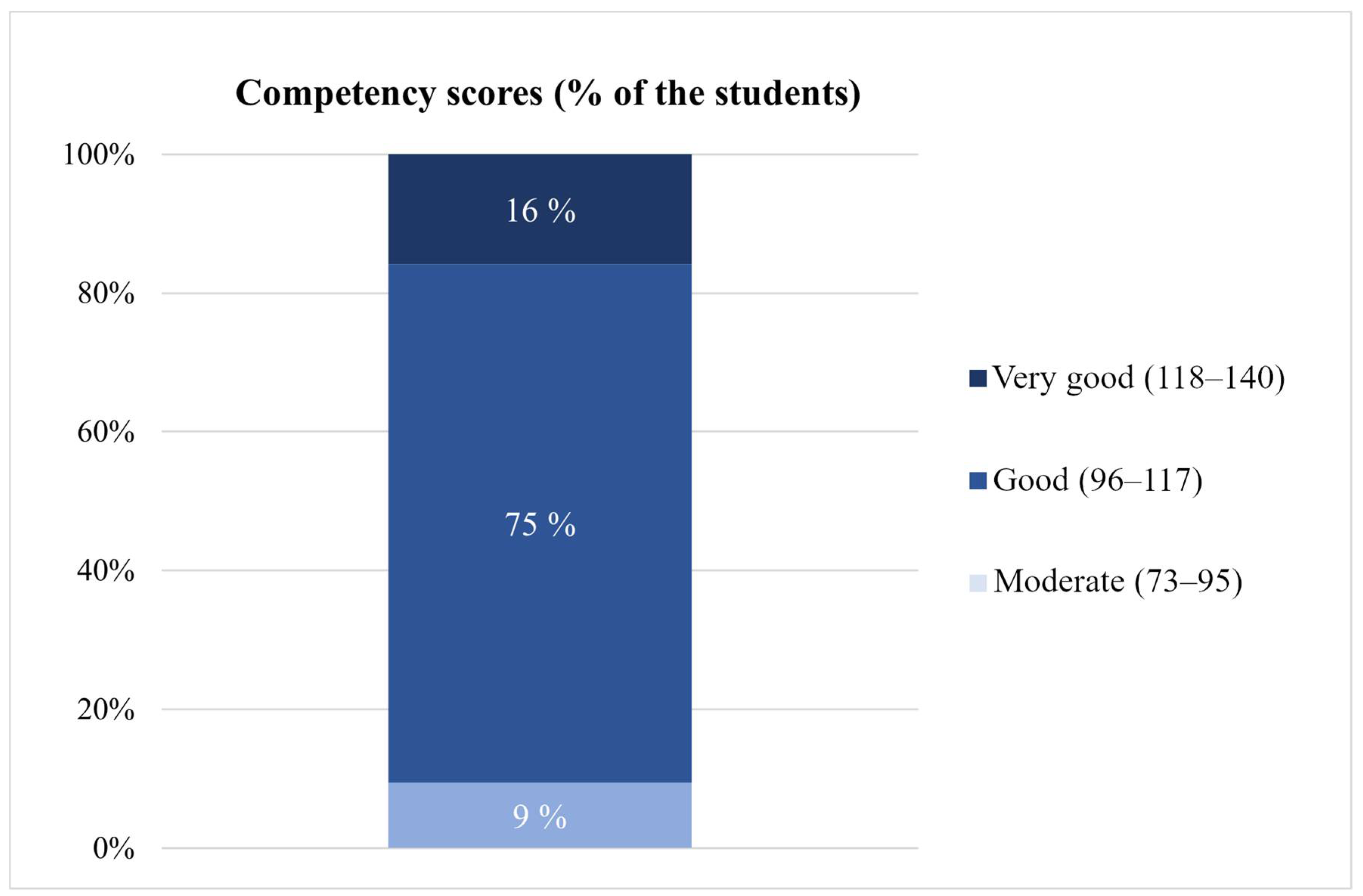
3.2. Medication Review Competency

4. Discussion
4.1. Strengths and Limitations
4.2. Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Purpose of the Medication Review | Patient Participation in the Medication Review | Use of Patient Information from Patient Records | Coverage of Both Prescription and Over-The-Counter Medicines | Review of Medicines/Medication Use and/or Condition | |
|---|---|---|---|---|---|
| Type 1: Prescription review | To address the technical and therapeutic issues related to the prescription and medication list to the extent that can be resolved based on information available in the prescription and in the pharmacy/care unit. The review should cover the issues to be recorded in the prescription while prescribing according to the Regulation by Ministry of Social Affairs and Health, and the items to be checked while dispensing as required by the Finnish Medicines Agency. If possible, the review will reconcile the patient’s medication list, documenting also medication-related issues requiring changes. These issues (e.g., dose adjustments) should be discussed with the patient or a person responsible for his/her care. | Not necessary | Possible (used to the extent available) | No, but both can be used if they are included in the medication list or the information is otherwise available (e.g., by interviewing the patient) | Medication: Medication in use and up-to-datedness of the medication list |
| Type 2: Medication review | To review the appropriateness of medication and identify and resolve therapeutically significant medication-related problems, where appropriate in collaboration with the attending physician and other care team. Based on the medication review, the patient’s medication list is reconciled, and key medication observations recorded in co-operation with the physician and other care team in an agreed manner. Changes and findings are discussed with the patient or other care provider and agreed upon to implement and monitor the changes. | The patient or the person responsible for the care is actively involved, considering the stage of medication care (initiation vs. follow-up) | Possible (used to the extent available) | Yes | Medication use: Ensuring appropriate medication use, adherence and self-management |
| Type 3: Comprehensive medication review | To ensure the appropriateness of the patient’s medication considering his/her medical conditions and illnesses. Based on the comprehensive medication review (CMR), clinically significant problems related to the medication and health status will be resolved in collaboration with the attending physician and other care team members. The procedure requires CMR Qualification from the pharmacists. The procedure includes physician’s decision whether the medication-related changes suggested by the pharmacist will be implemented. It also includes a plan for monitoring medication changes. Where appropriate, pharmacists will be involved in implementing these changes. | The patient or the person responsible for the care actively participates in the medication review process, the therapeutic interview frame is utilized (e.g., the one designed for CMR or other suitable interview frame), a home visit is made if necessary | Yes (if necessary, additional patient information can be asked from the attending physician or nurse with the consent of the patient or his/her representative) | Yes | Medication use and condition: Appropriateness of medication, taking into consideration the patient’s diseases and medical condition |
References
- Pellegrino, A.; Martin, M.; Tilton, J.; Touchette, D. Medication Therapy Management Services. Drugs 2009, 69, 393–406. [Google Scholar] [CrossRef] [PubMed]
- Leikola, S.; Tuomainen, L.; Peura, S.; Laurikainen, A.; Lyles, A.; Savela, E.; Airaksinen, M. Comprehensive medication review development of a collaborative procedure. Int. J. Clin. Pharm. 2012, 34, 510–514. [Google Scholar] [CrossRef] [PubMed]
- Bulajeva, A.; Labberton, L.; Leikola, S.; Pohjanoksa-Mäntylä, M.; Geurts, M.M.E.; de Gier, J.J.; Airaksinen, M. Medication review practices in European countries. Res. Soc. Adm. Pharm. 2014, 10, 731–740. [Google Scholar] [CrossRef]
- Kiiski, A.; Kallio, S.; Pohjanoksa-Mäntylä, M.; Kumpusalo-Vauhkonen, A.; Järvensivu, T.; Airaksinen, M.; Mäntylä, A. Iäkkäiden Lääkehoidon Järkeistäminen Moniammatillisena Yhteistyönä. Systematic Review. The Ministry of Social Affairs and Health. 2016. Available online: http://urn.fi/URN:ISBN:978-952-00-3704-8 (accessed on 16 August 2022).
- Rose, O.; Mennemann, H.; John, C.; Lautenschläger, M.; Mertens-Keller, D.; Richling, K.; Waltering, I.; Hamacher, S.; Felsch, M.; Herich, L.; et al. Priority Setting and Influential Factors on Acceptance of Pharmaceutical Recommendations in Collaborative Medication Reviews in an Ambulatory Care Setting—Analysis of a Cluster Randomized Controlled Trial (WestGem-Study). PLoS ONE 2016, 11, e0156304. [Google Scholar] [CrossRef] [Green Version]
- Aronson, J. Medication reconciliation. BMJ 2017, 356, i5336. [Google Scholar] [CrossRef] [PubMed]
- Saastamoinen, L.; Verho, K. Register-based indicators for potentially inappropriate medication in high-cost patients with excessive polypharmacy. Pharmacoepidemiol. Drug. Saf. 2015, 24, 610–618. [Google Scholar] [CrossRef] [PubMed]
- Chen, T. Pharmacist-Led Home Medicines Review and Residential Medication Management Review: The Australian Model. Drugs Aging 2016, 33, 199–204. [Google Scholar] [CrossRef] [PubMed]
- Toivo, T.; Dimitrow, M.; Puustinen, J.; Savela, E.; Pelkonen, K.; Kiuru, V.; Suominen, T.; Kinnunen, S.; Uunimäki, M.; Kivelä, S.; et al. Coordinating resources for prospective medication risk management of older home care clients in primary care: Procedure development and RCT study design for demonstrating its effectiveness. BMC Geriatr. 2018, 18, 74–83. [Google Scholar] [CrossRef] [Green Version]
- Dimitrow, M. Development and Validation of a Drug-Related Problem Risk Assessment Tool for Use by Practical Nurses Working with Community-Dwelling Aged. Ph.D. Thesis, University of Helsinki, Helsinki, Finland, 2016. Available online: http://urn.fi/URN:ISBN:978-951-51-2618-4 (accessed on 16 August 2022).
- Keijsers, C.; Hensbergen, L.; Jacobs, L.; Brouwers, J.; Wildt, D.; Cate, O.; Jansen, P. Geriatric pharmacology and pharmacotherapy education for health professionals and students: A systematic review. Br. J. Clin. Pharmacol. 2012, 74, 762–773. [Google Scholar] [CrossRef] [Green Version]
- Aronpuro, K.; Kähkönen, A.; Rouvinen, M.; Kiiski, A.; Pietilä, K.; Airaksinen, M. Development of competences needed in medication reviews during pharmacy internships. Dosis 2017, 33, 40–54. Available online: https://dosis.fi/wp-content/uploads/2018/03/Dosis_1_2017.pdf (accessed on 16 August 2022).
- Pharmaceutical Society of Australia PSA. National Competency Standards Framework for Pharmacists in Australia. 2016. Available online: https://www.psa.org.au/wp-content/uploads/2018/06/National-Competency-Standards-Framework-for-Pharmacists-in-Australia-2016-PDF-2mb.pdf (accessed on 16 August 2022).
- Pharmaceutical Care Network Europe PCNE (2013): Statement on Medication Review. Available online: http://www.pcne.org/upload/files/150_20160504_PCNE_MedRevtypes.pdf (accessed on 16 August 2022).
- European Expertise Centre for Pharmacy Education and Training EEC-PET. Competency Framework. 2016. Available online: http://eec-pet.eu/pharmacy-education/competency-framework/ (accessed on 16 August 2022).
- American College of Clinical Pharmacy ACCP. Clinical Pharmacist Competencies. Pharmacotherapy 2017, 37, 630–636. [Google Scholar] [CrossRef] [PubMed]
- British Columbia Pharmacy Association BCPA. Medication Review Services. 2017. Available online: https://www.bcpharmacy.ca/resource-centre/health-issues/medication-review-services (accessed on 16 August 2022).
- Pharmaceutical Services Negotiating Committee PSNC. Competency Framework for the Assessment of Pharmacists Providing the Medicines Use Review (MUR) and Prescription Intervention Service. Available online: https://psnc.org.uk/wp-content/uploads/2013/07/advanced_service_competency_framework.pdf (accessed on 16 August 2022).
- The National Coordination Group of Professional Development of Pharmacy Services AATE. Medication review competence recommendations for pharmacists working in community pharmacies and other health care settings. Dosis 2017, 33, 199–209. Available online: https://dosis.fi/wp-content/uploads/2018/03/Dosis_3_2017.pdf (accessed on 16 August 2022).
- Clyne, W.; Blenkinsopp, A.; Seal, R. A Guide to Medication Review. The National Prescribing Centre, the Medicines Partnership Programme. 2008. Available online: www.cff.org.br/userfiles/52%20-%20CLYNE%20W%20A%20guide%20to%20medication%20review%202008.pdf (accessed on 16 August 2022).
- University of Eastern Finland Aducate—Centre for Training and Development. Available online: www.uef.fi/en/web/aducate (accessed on 16 August 2022).
- Hämeen-Anttila, K.; Närhi, U.; Tahvanainen, H. Rational Pharmacotherapy Action Plan 2018–2022. The Ministry of Social Affairs and Health. 2018. Available online: http://urn.fi/URN:ISBN:978-952-00-3915-8 (accessed on 16 August 2022).
- The Bologna Declaration of 19 June 1999. Joint Declaration of the European Ministers of Education. Available online: http://www.ehea.info/media.ehea.info/file/Ministerial_conferences/02/8/1999_Bologna_Declaration_English_553028.pdf (accessed on 16 August 2022).
- European Parliament Directive 2005/36/EC: The Recognition of Professional Qualifications. Available online: http://eur-lex.europa.eu/legal-content/EN/TXT/?uri=CELEX:32005L0036 (accessed on 16 August 2022).
- Pitkä, K.; Löfhjelm, U.; Passi, S.; Airaksinen, M. Integrating Internships with Professional Study in Pharmacy Education in Finland. Am. J. Pharm. Educ. 2014, 78, 173. [Google Scholar] [CrossRef] [PubMed]
- Dawoud, D.M.; Haines, A.; Wonderling, D.; Ashe, J.; Hill, J.; Varia, M.; Dyer, P.; Bion, J. Cost Effectiveness of Advanced Pharmacy Services Provided in the Community and Primary Care Settings: A Systematic Review. Pharmacoeconomics 2019, 37, 1241–1260. [Google Scholar] [CrossRef]
- International Pharmaceutical Federation. Medication Review and Medicines Use Review: A Toolkit for Pharmacists. 2022. Available online: https://www.fip.org/file/5100 (accessed on 15 October 2022).
- Lias, N.; Lindholm, T.; Pohjanoksa-Mäntylä, M.; Westerholm, A.; Airaksinen, M. Developing and piloting a self-assessment tool for medication review competence of practicing pharmacists based on nationally set competence criteria. BMC Health Serv. Res. 2021, 21, 1274. [Google Scholar] [CrossRef]
- Finnish Advisory Board on Research Integrity. Ethical Principles of Research in the Humanities and Social and Behavioural Sciences and Proposals for Ethical Review. 2009. Available online: http://www.tenk.fi/en (accessed on 16 August 2022).
- Ethical Review Board in the Humanities and Social and Behavioural Sciences, University of Helsinki. Instructions for Researchers. Available online: https://www.helsinki.fi/en/research/services-researchers/ethical-review-research/humanities-social-sciences-and-behavioural-sciences (accessed on 16 August 2022).
- Nuffer, W.; Gilliam, E.; Thompson, M.; Griend, J.V. Establishment and Implementation of a Required Medication Therapy Management Advanced Pharmacy Practice Experience. Am. J. Pharm. Educ. 2017, 81, 36. [Google Scholar] [CrossRef]
- Melody, K.; Harris, E.; Grover, A. Development and evaluation of an elective course that incorporates a standard medication therapy management certificate program. Curr. Pharm. Teach. Learn. 2018, 10, 1104–1112. [Google Scholar] [CrossRef]
- Atayee, R.; Awdishu, L.; Namba, J. Using Simulation to Improve First-Year Pharmacy Students’ Ability to Identify Medication Errors Involving the Top 100 Prescription Medications. Am. J. Pharm. Educ. 2016, 80, 86. Available online: https://www.ajpe.org/doi/10.5688/ajpe80586 (accessed on 16 August 2022). [CrossRef] [Green Version]
- Kuhn, C.; Powell, P.; Sterrett, J. Elective Course on Medication Therapy Management Services. Am. J. Pharm. Educ. 2010, 74, 40. [Google Scholar] [CrossRef] [Green Version]
- Eukel, H.; Skoy, E.; Frenzel, J. Provision of Medication Therapy Management to University Faculty and Staff Members by Third-year Pharmacy Students. Am. J. Pharm. Educ. 2010, 74, 182. [Google Scholar] [CrossRef] [Green Version]
- Poole, T.; Kodali, L.; Pace, A. Integrating Medication Therapy Management Education into a Core Pharmacy Curriculum. Am. J. Pharm. Educ. 2016, 80, 70. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alshehri, A.M.; Barner, J.C.; Rush, S. The impact of a required course on third year pharmacy students’ perceived abilities and intentions in providing medication therapy management. Curr. Pharm. Teach. Learn. 2019, 11, 94–105. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.Y.; Soriano, R.P.; Fallar, R.; Ramaswamy, R. Assessment of medication management competency among medical students using standardized patients. J. Am. Geriatr. Soc. 2020, 68, E4–E6. [Google Scholar] [CrossRef] [PubMed]
- Löfhjelm, U.; Pitkä, K.; Passi, S.; Airaksinen, M. Preceptors’ Need for Support in Tutoring Pharmacy Students in Finnish Community Pharmacies. Innov. Pharm. 2016, 7, 13. [Google Scholar] [CrossRef] [Green Version]
- Schepel, L.; Aronpuro, K.; Kvarnström, K.; Holmström, A.; Lehtonen, L.; Lapatto-Reiniluoto, O.; Laaksonen, R.; Carlsson, K.; Airaksinen, M. Strategies for improving medication safety in hospitals: Evolution of clinical pharmacy services. Res. Soc. Adm. Pharm. 2019, 15, 873–882. [Google Scholar] [CrossRef] [Green Version]
- Pitkä, K.; Airaksinen, M.; Pohjanoksa-Mäntylä, M. Use and accessibility of health and medication information sources among pharmacy students during their community pharmacy internship. Curr. Pharm. Teach. Learn. 2018, 10, 1041–1047. [Google Scholar] [CrossRef] [Green Version]
- Pennycook, G.; Ross, R.; Koehler, D.; Fugelsang, J. Dunning–Kruger effects in reasoning: Theoretical implications of the failure to recognize incompetence. Psychon. Bull. Rev. 2017, 24, 1774–1784. [Google Scholar] [CrossRef] [Green Version]
- University of Helsinki. Pharmacy Curriculum Reform 2014—Final Report of the Planning Group; Faculty of Pharmacy: Helsinki, Finland, 2014. [Google Scholar]
- Faculty of Pharmacy, University of Helsinki. Työ Opiksi! [In English: Learning by Doing!]. Available online: https://www.helsinki.fi/fi/ohjelmat/kandi/farmaseutin-koulutusohjelma/opiskelu/apteekkiharjoittelu#section-42697 (accessed on 16 August 2022).

| Variable | ||
|---|---|---|
| Curriculum, n (%) | 95 (100) | |
| Bachelor’s degree | 74 (78) | |
| Master’s degree | 21 (22) | |
| Years studied | Mean | Range |
| BSc (Pharm) students | 3.2 | 3–6 |
| MSc (Pharm) students | 3.0 | 3–4 |
| Previous degrees, n (%) | 95 (100) | |
| No previous degrees | 66 (70) | |
| Bachelor’s or master’s degree, university | 12 (13) | |
| Bachelor’s degree, university of applied sciences | 8 (8) | |
| Vocational qualification | 7 (7) | |
| PhD or equal | 2 (2) | |
| Grades in obligatory courses laying foundation in clinical pharmacy (grade 1–5, 5 being the highest) | Mean grade | SD |
| Medication Counselling and Pharmacotherapy (4 ECTS credits) | 4.3 | 0.7 |
| Pathology and Nutrition (4 ECTS credits) | 3.1 | 1.2 |
| Systematic Pharmacology (12 ECTS credits) | 2.4 | 1.3 |
| Has the student taken the elective course “Comprehensive medication review and clinical pharmacy” (4 ECTS credits), n (%) | 95 (100) | |
| Yes | 3 (3) | |
| No | 92 (97) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Westerholm, A.; Leiman, K.; Kiiski, A.; Pohjanoksa-Mäntylä, M.; Mistry, A.; Airaksinen, M. Developing Medication Review Competency in Undergraduate Pharmacy Training: A Self-Assessment by Third-Year Students. Int. J. Environ. Res. Public Health 2023, 20, 5079. https://doi.org/10.3390/ijerph20065079
Westerholm A, Leiman K, Kiiski A, Pohjanoksa-Mäntylä M, Mistry A, Airaksinen M. Developing Medication Review Competency in Undergraduate Pharmacy Training: A Self-Assessment by Third-Year Students. International Journal of Environmental Research and Public Health. 2023; 20(6):5079. https://doi.org/10.3390/ijerph20065079
Chicago/Turabian StyleWesterholm, Aleksi, Katja Leiman, Annika Kiiski, Marika Pohjanoksa-Mäntylä, Anita Mistry, and Marja Airaksinen. 2023. "Developing Medication Review Competency in Undergraduate Pharmacy Training: A Self-Assessment by Third-Year Students" International Journal of Environmental Research and Public Health 20, no. 6: 5079. https://doi.org/10.3390/ijerph20065079
APA StyleWesterholm, A., Leiman, K., Kiiski, A., Pohjanoksa-Mäntylä, M., Mistry, A., & Airaksinen, M. (2023). Developing Medication Review Competency in Undergraduate Pharmacy Training: A Self-Assessment by Third-Year Students. International Journal of Environmental Research and Public Health, 20(6), 5079. https://doi.org/10.3390/ijerph20065079






