The Mediation Effect of Pain on the Relationship between Kinesiophobia and Lumbar Joint Position Sense in Chronic Low Back Pain Individuals: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Settings
2.2. Subjects
2.3. Outcome Measures
2.3.1. Pain Intensity
2.3.2. Kinesiophobia
2.3.3. Lumbar Joint Position Sense
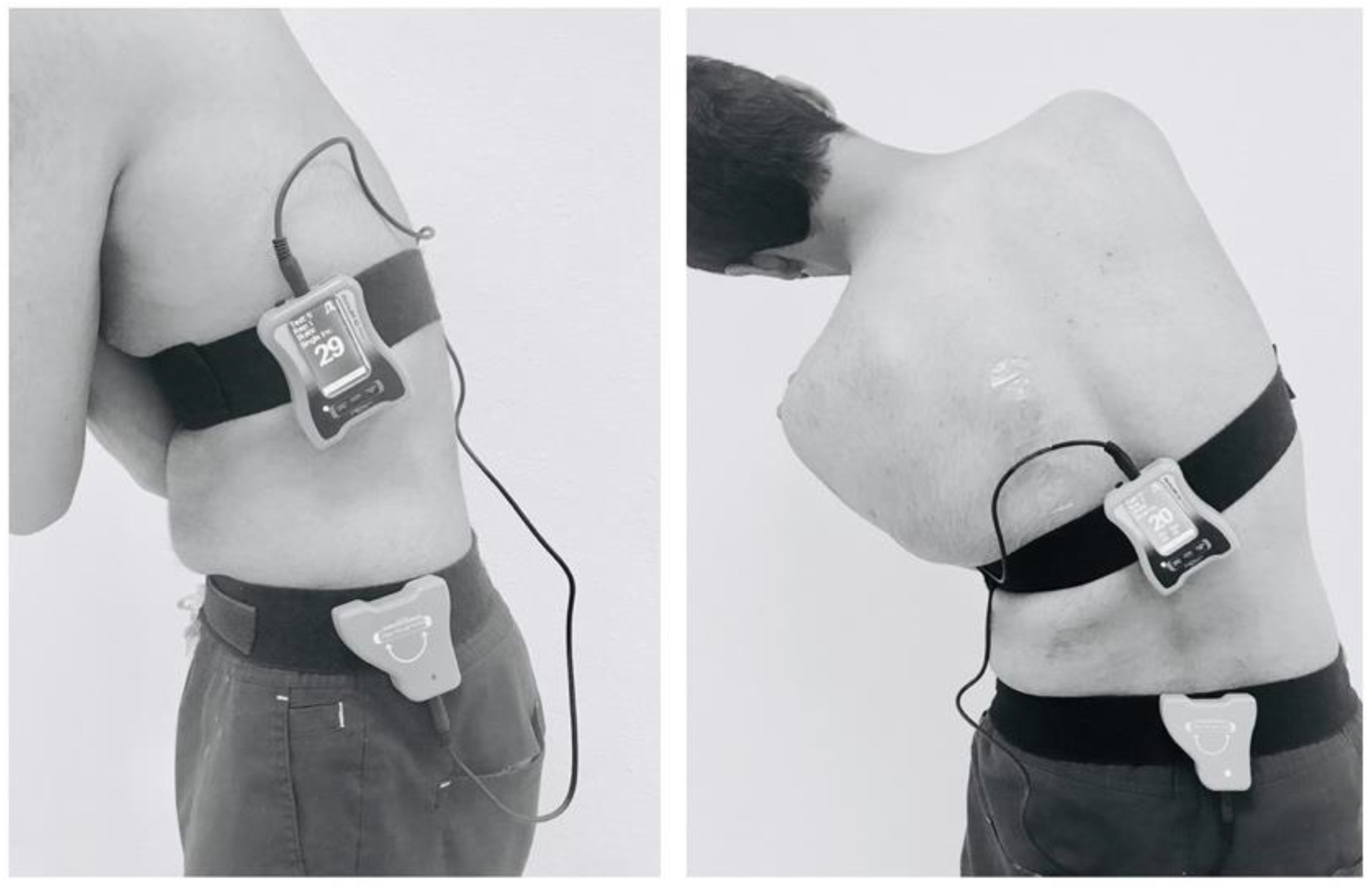
2.4. Sample Size
2.5. Statistical Analysis
3. Results
4. Discussion
4.1. Practical Clinical Implications
4.2. Future Research Implications
4.3. Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kamper, S.J.; Logan, G.; Copsey, B.; Thompson, J.; Machado, G.C.; Abdel-Shaheed, C.; Williams, C.M.; Maher, C.G.; Hall, A.M. What is usual care for low back pain? A systematic review of health care provided to patients with low back pain in family practice and emergency departments. Pain 2020, 161, 694–702. [Google Scholar] [CrossRef] [PubMed]
- Carregaro, R.L.; Tottoli, C.R.; Rodrigues, D.d.S.; Bosmans, J.E.; da Silva, E.N.; van Tulder, M. Low back pain should be considered a health and research priority in Brazil: Lost productivity and healthcare costs between 2012 to 2016. PLoS ONE 2020, 15, e0230902. [Google Scholar] [CrossRef] [PubMed]
- Fatoye, F.; Gebrye, T.; Odeyemi, I. Real-world incidence and prevalence of low back pain using routinely collected data. Rheumatol. Int. 2019, 39, 619–626. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, C.B.; Pinheiro, M.B.; Teixeira, R.J.; Franco, M.R.; Silva, F.G.; Hisamatsu, T.M.; Ferreira, P.H.; Pinto, R.Z. Physical activity as a prognostic factor of pain intensity and disability in patients with low back pain: A systematic review. Eur. J. Pain 2019, 23, 1251–1263. [Google Scholar] [CrossRef] [PubMed]
- Urits, I.; Burshtein, A.; Sharma, M.; Testa, L.; Gold, P.A.; Orhurhu, V.; Viswanath, O.; Jones, M.R.; Sidransky, M.A.; Spektor, B. Low back pain, a comprehensive review: Pathophysiology, diagnosis, and treatment. Curr. Pain Headache Rep. 2019, 23, 23. [Google Scholar] [CrossRef]
- Ranger, T.A.; Cicuttini, F.M.; Jensen, T.S.; Manniche, C.; Heritier, S.; Urquhart, D.M. Catastrophization, fear of movement, anxiety, and depression are associated with persistent, severe low back pain and disability. Spine J. 2020, 20, 857–865. [Google Scholar] [CrossRef]
- Luque-Suarez, A.; Martinez-Calderon, J.; Navarro-Ledesma, S.; Morales-Asencio, J.M.; Meeus, M.; Struyf, F. Kinesiophobia is associated with pain intensity and disability in chronic shoulder pain: A cross-sectional study. J. Manip. Physiol. Ther. 2020, 43, 791–798. [Google Scholar] [CrossRef]
- Pazzinatto, M.F.; Rio, E.K.; Crossley, K.M.; Coburn, S.L.; Johnston, R.; Jones, D.M.; Kemp, J.L. The relationship between kinesiophobia and self-reported outcomes and physical function differs between women and men with femoroacetabular impingement syndrome. Braz. J. Phys. Ther. 2022, 26, 100396. [Google Scholar] [CrossRef]
- Bilgin, S.; Cetin, H.; Karakaya, J.; Kose, N. Multivariate analysis of risk factors predisposing to kinesiophobia in persons with chronic low back and neck pain. J. Manip. Physiol. Ther. 2019, 42, 565–571. [Google Scholar] [CrossRef]
- Lüning Bergsten, C.; Lundberg, M.; Lindberg, P.; Elfving, B. Change in kinesiophobia and its relation to activity limitation after multidisciplinary rehabilitation in patients with chronic back pain. Disabil. Rehabil. 2012, 34, 852–858. [Google Scholar] [CrossRef]
- Silva, M.C.d.M.; Tottoli, C.R.; Mascarenhas, K.; Marques, Y.A.; Toledo, A.M.; Carregaro, R.L. Is kinesiophobia associated with disturbances in dynamic balance in individuals with chronic non-specific low back pain? BrJP 2022, 5, 47–51. [Google Scholar]
- Palacios-Ceña, D.; Albaladejo-Vicente, R.; Hernández-Barrera, V.; Lima-Florencio, L.; Fernández-de-Las-Peñas, C.; Jimenez-Garcia, R.; López-de-Andrés, A.; de Miguel-Diez, J.; Perez-Farinos, N. Female Gender Is Associated with a Higher Prevalence of Chronic Neck Pain, Chronic Low Back Pain, and Migraine: Results of the Spanish National Health Survey, 2017. Pain Med. 2020, 22, 382–395. [Google Scholar] [CrossRef]
- Peterson, G.E.; Ludvigsson, M.H.L.; O’Leary, S.P.; Dedering, Å.M.; Wallman, T.; Jönsson, M.I.; Peolsson, A.L. The effect of 3 different exercise approaches on neck muscle endurance, kinesiophobia, exercise compliance, and patient satisfaction in chronic whiplash. J. Manip. Physiol. Ther. 2015, 38, 465–476.e464. [Google Scholar] [CrossRef]
- Palomo-López, P.; Becerro-de-Bengoa-Vallejo, R.; Losa-Iglesias, M.E.; López-López, D.; Rodríguez-Sanz, D.; Romero-Morales, C.; Calvo-Lobo, C.; Mazoteras-Pardo, V. Kinesiophobia and pain intensity are increased by a greater hallux valgus deformity degree-kinesiophobia and pain intensity in hallux valgus. Int. J. Environ. Res. Public Health 2020, 17, 626. [Google Scholar] [CrossRef]
- Ouchi, K.; Watanabe, M.; Tomiyama, C.; Nikaido, T.; Oh, Z.; Hirano, T.; Akazawa, K.; Mandai, N. Emotional effects on factors associated with chronic low back pain. J. Pain Res. 2019, 12, 3343. [Google Scholar] [CrossRef]
- Azadinia, F.; Kingma, I.; Mazaheri, M. Effect of external lumbar supports on joint position sense, postural control, and postural adjustment: A systematic review. Disabil. Rehabil. 2022, 45, 753–771. [Google Scholar] [CrossRef]
- Alsufiany, M.B.; Lohman, E.B.; Daher, N.S.; Gang, G.R.; Shallan, A.I.; Jaber, H.M. Non-specific chronic low back pain and physical activity: A comparison of postural control and hip muscle isometric strength: A cross-sectional study. Medicine 2020, 99, e18544. [Google Scholar] [CrossRef]
- Borujeni, B.G.; Yalfani, A. Reduction of postural sway in athletes with chronic low back pain through eight weeks of inspiratory muscle training: A randomized controlled trial. Clin. Biomech. 2019, 69, 215–220. [Google Scholar] [CrossRef]
- Linton, S.J. A review of psychological risk factors in back and neck pain. Spine 2000, 25, 1148–1156. [Google Scholar] [CrossRef]
- Alahmari, K.A.; Reddy, R.S.; Silvian, P.S.; Ahmad, I.; Kakaraparthi, V.N.; Alam, M.M. Association of age on cervical joint position error. J. Adv. Res. 2017, 8, 201–207. [Google Scholar] [CrossRef]
- Hodges, P.W. Pain and motor control: From the laboratory to rehabilitation. J. Electromyogr. Kinesiol. 2011, 21, 220–228. [Google Scholar] [CrossRef] [PubMed]
- Reddy, R.S.; Alahmari, K.A.; Samuel, P.S.; Tedla, J.S.; Kakaraparthi, V.N.; Rengaramanujam, K. Intra-rater and inter-rater reliability of neutral and target lumbar positioning tests in subjects with and without non-specific lower back pain. J. Back Musculoskelet. Rehabil. 2021, 34, 289–299. [Google Scholar] [CrossRef] [PubMed]
- Ghamkhar, L.; Kahlaee, A.H. Pain and pain-related disability associated with proprioceptive impairment in chronic low back pain patients: A systematic review. J. Manip. Physiol. Ther. 2019, 42, 210–217. [Google Scholar] [CrossRef] [PubMed]
- Comachio, J.; Magalhães, M.O.; Silva, A.P.d.M.C.C.; Marques, A.P. A cross-sectional study of associations between kinesiophobia, pain, disability, and quality of life in patients with chronic low back pain. Adv. Rheumatol. 2019, 58, 8. [Google Scholar] [CrossRef]
- Varallo, G.; Giusti, E.M.; Scarpina, F.; Cattivelli, R.; Capodaglio, P.; Castelnuovo, G. The association of kinesiophobia and pain catastrophizing with pain-related disability and pain intensity in obesity and chronic lower-back pain. Brain Sci. 2020, 11, 11. [Google Scholar] [CrossRef]
- Kandakurti, P.K.; Arulsingh, W.; S Patil, S. Influence of kinesiophobia on pain intensity, disability, muscle endurance, and position sense in patients with chronic low back pain—A case-control study. Trials 2022, 23, 469. [Google Scholar] [CrossRef]
- Varallo, G.; Scarpina, F.; Giusti, E.M.; Cattivelli, R.; Guerrini Usubini, A.; Capodaglio, P.; Castelnuovo, G. Does kinesiophobia mediate the relationship between pain intensity and disability in individuals with chronic low-back pain and obesity? Brain Sci. 2021, 11, 684. [Google Scholar] [CrossRef]
- Leeuw, M.; Goossens, M.E.; Linton, S.J.; Crombez, G.; Boersma, K.; Vlaeyen, J.W. The fear-avoidance model of musculoskeletal pain: Current state of scientific evidence. J. Behav. Med. 2007, 30, 77–94. [Google Scholar] [CrossRef]
- Larsson, C.; Ekvall Hansson, E.; Sundquist, K.; Jakobsson, U. Kinesiophobia and its relation to pain characteristics and cognitive affective variables in older adults with chronic pain. BMC Geriatr. 2016, 16, 128. [Google Scholar] [CrossRef]
- Pagé, M.G.; Tousignant-Laflamme, Y.; Dorais, M.; Beaudry, H.; Fernet, M. Characteristics of Persons Seeking Care for Moderate to Severe Pain Due to Chronic Low Back Pain and Osteoarthritis: A Cross-Sectional Study. J. Pain Res. 2022, 15, 1125. [Google Scholar] [CrossRef]
- Wong, C.K.; Mak, R.Y.; Kwok, T.S.; Tsang, J.S.; Leung, M.Y.; Funabashi, M.; Macedo, L.G.; Dennett, L.; Wong, A.Y. Prevalence, incidence, and factors associated with non-specific chronic low back pain in community-dwelling older adults aged 60 years and older: A systematic review and meta-analysis. J. Pain 2022, 23, 509–534. [Google Scholar] [CrossRef]
- Peng, X.; Bao, X.; Xie, Y.; Zhang, X.; Huang, J.; Liu, Y.; Cheng, M.; Liu, N.; Wang, P. The mediating effect of pain on the association between multimorbidity and disability and impaired physical performance among community-dwelling older adults in southern China. Aging Clin. Exp. Res. 2020, 32, 1327–1334. [Google Scholar] [CrossRef]
- Alshahrani, M.S.; Reddy, R.S.; Tedla, J.S.; Asiri, F.; Alshahrani, A. Association between kinesiophobia and knee pain intensity, joint position sense, and functional performance in individuals with bilateral knee osteoarthritis. Healthcare 2022, 10, 120. [Google Scholar] [CrossRef]
- Asiri, F.; Reddy, R.S.; Tedla, J.S.; ALMohiza, M.A.; Alshahrani, M.S.; Govindappa, S.C.; Sangadala, D.R. Kinesiophobia and its correlations with pain, proprioception, and functional performance among individuals with chronic neck pain. PLoS ONE 2021, 16, e0254262. [Google Scholar] [CrossRef]
- Alahmari, K.A.; Rengaramanujam, K.; Reddy, R.S.; Samuel, P.S.; Tedla, J.S.; Kakaraparthi, V.N.; Ahmad, I. The immediate and short-term effects of dynamic taping on pain, endurance, disability, mobility and kinesiophobia in individuals with chronic non-specific low back pain: A randomized controlled trial. PLoS ONE 2020, 15, e0239505. [Google Scholar] [CrossRef]
- Alshahrani, M.S.; Reddy, R.S. Relationship between Kinesiophobia and Ankle Joint Position Sense and Postural Control in Individuals with Chronic Ankle Instability—A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 2792. [Google Scholar] [CrossRef]
- Asiri, F.; Reddy, R.S.; Alshahrani, M.S.; Tedla, J.S.; Dixit, S.; Alshahrani, A.; Gular, K.; Raizah, A. Mediation Effect of Pain on the Relationship between Kinesiophobia and Postural Control: Comparison and Correlations in Individuals with Fibromyalgia Syndrome and Asymptomatic Individuals—A Cross-Sectional Study. Life 2023, 13, 175. [Google Scholar] [CrossRef]
- Chiarotto, A.; Maxwell, L.J.; Ostelo, R.W.; Boers, M.; Tugwell, P.; Terwee, C.B. Measurement properties of visual analogue scale, numeric rating scale, and pain severity subscale of the brief pain inventory in patients with low back pain: A systematic review. J. Pain 2019, 20, 245–263. [Google Scholar] [CrossRef]
- Vlaeyen, J.W.; Kole-Snijders, A.M.; Boeren, R.G.; Van Eek, H. Fear of movement/(re) injury in chronic low back pain and its relation to behavioral performance. Pain 1995, 62, 363–372. [Google Scholar] [CrossRef]
- Rosenbloom, B.N.; Pagé, M.G.; Isaac, L.; Campbell, F.; Stinson, J.N.; Cribbie, R.; Katz, J. Fear of movement in children and adolescents undergoing major surgery: A psychometric evaluation of the Tampa Scale for Kinesiophobia. Eur. J. Pain 2020, 24, 1999–2014. [Google Scholar] [CrossRef]
- Lundberg, M.; Larsson, M.; Ostlund, H.; Styf, J. Kinesiophobia among patients with musculoskeletal pain in primary healthcare. J. Rehabil. Med. 2006, 38, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Díaz, D.; Romeu, M.; Velasco-González, C.; Martínez-Amat, A.; Hita-Contreras, F. The effectiveness of 12 weeks of Pilates intervention on disability, pain and kinesiophobia in patients with chronic low back pain: A randomized controlled trial. Clin. Rehabil. 2018, 32, 1249–1257. [Google Scholar] [CrossRef] [PubMed]
- Georgy, E.E. Lumbar repositioning accuracy as a measure of proprioception in patients with back dysfunction and healthy controls. Asian Spine J. 2011, 5, 201–207. [Google Scholar] [CrossRef] [PubMed]
- Romero-Franco, N.; Montaño-Munuera, J.A.; Fernández-Domínguez, J.C.; Jiménez-Reyes, P. Validity and reliability of a digital inclinometer to assess knee joint position sense in an open kinetic chain. J. Sport Rehabil. 2019, 28, 332–338. [Google Scholar] [CrossRef]
- Kang, H. Sample size determination and power analysis using the G* Power software. J. Educ. Eval. Health Prof. 2021, 18, 17. [Google Scholar] [CrossRef]
- Osumi, M.; Sumitani, M.; Otake, Y.; Morioka, S. Fear of movement modulates the feedforward motor control of the affected limb in complex regional pain syndrome (CRPS): A single-case study. Med. Hypotheses 2018, 110, 114–119. [Google Scholar] [CrossRef]
- Demoulin, C.; Huijnen, I.P.; Somville, P.-R.; Grosdent, S.; Salamun, I.; Crielaard, J.-M.; Vanderthommen, M.; Volders, S. Relationship between different measures of pain-related fear and physical capacity of the spine in patients with chronic low back pain. Spine J. 2013, 13, 1039–1047. [Google Scholar] [CrossRef]
- Larivière, C.; Bilodeau, M.; Forget, R.; Vadeboncoeur, R.; Mecheri, H. Poor back muscle endurance is related to pain catastrophizing in patients with chronic low back pain. Spine 2010, 35, E1178–E1186. [Google Scholar] [CrossRef]
- Kandakurti, P.K.; Reddy, R.S.; Kakarparthy, V.N.; Rengaramanujam, K.; Tedla, J.S.; Dixit, S.; Gautam, A.P.; Silvian, P.; Gular, K.; Eapen, C. Comparison and Association of Neck Extensor Muscles’ Endurance and Postural Function in Subjects with and without Chronic Neck Pain—A Cross-Sectional Study. Phys. Med. Rehabil. Kurortmed. 2021, 31, 295–301. [Google Scholar] [CrossRef]
- Saeed Alshahrani, M.; Reddy, R.S.; Asiri, F.; Tedla, J.S.; Alshahrani, A.; Kandakurti, P.K.; Kakaraparthi, V.N. Correlation and comparison of quadriceps endurance and knee joint position sense in individuals with and without unilateral knee osteoarthritis. BMC Musculoskelet. Disord. 2022, 23, 444. [Google Scholar] [CrossRef]
- Criss, C.R. Central Nervous System Contributions to Subjective and Objective Measures of Function after Anterior Cruciate Ligament Reconstruction; Ohio University: Athens, OH, USA, 2021. [Google Scholar]
- Pakzad, M.; Fung, J.; Preuss, R. Pain catastrophizing and trunk muscle activation during walking in patients with chronic low back pain. Gait Posture 2016, 49, 73–77. [Google Scholar] [CrossRef]
- Aydoğdu, O.; Zübeyir, S. The association between kinesiophobia and proprioception, postural stability, activity level, knee function, and quality of life following anterior cruciate ligament reconstruction. J. Exerc. Ther. Rehabil. 2020, 7, 247–252. [Google Scholar]
- Muthukrishnan, R.; Shenoy, S.D.; Jaspal, S.S.; Nellikunja, S.; Fernandes, S. The differential effects of core stabilization exercise regime and conventional physiotherapy regime on postural control parameters during perturbation in patients with movement and control impairment chronic low back pain. BMC Sport. Sci. Med. Rehabil. 2010, 2, 13. [Google Scholar] [CrossRef]
- Reddy, R.S.; Meziat-Filho, N.; Ferreira, A.S.; Tedla, J.S.; Kandakurti, P.K.; Kakaraparthi, V.N. Comparison of neck extensor muscle endurance and cervical proprioception between asymptomatic individuals and patients with chronic neck pain. J. Bodyw. Mov. Ther. 2021, 26, 180–186. [Google Scholar] [CrossRef]
- Karayannis, N.V.; Smeets, R.J.; van den Hoorn, W.; Hodges, P.W. Fear of movement is related to trunk stiffness in low back pain. PLoS ONE 2013, 8, e67779. [Google Scholar] [CrossRef]
- Bonanni, R.; Cariati, I.; Tancredi, V.; Iundusi, R.; Gasbarra, E.; Tarantino, U. Chronic pain in musculoskeletal diseases: Do you know your enemy? J. Clin. Med. 2022, 11, 2609. [Google Scholar] [CrossRef]
- Hasenbring, M.I.; Andrews, N.E.; Ebenbichler, G. Overactivity in chronic pain, the role of pain-related endurance and neuromuscular activity: An interdisciplinary, narrative review. Clin. J. Pain 2020, 36, 162–171. [Google Scholar] [CrossRef]
- Meier, M.L.; Vrana, A.; Schweinhardt, P. Low back pain: The potential contribution of supraspinal motor control and proprioception. Neuroscientist 2019, 25, 583–596. [Google Scholar] [CrossRef]
- Allah, E.; AbdAlla, M.G.A.; Abdel-Aziz, H.R. Risk of fall and its Contributing Factors among Older adults with Chronic Low Back Pain. Ann. Rom. Soc. Cell Biol. 2021, 25, 18895–18905. [Google Scholar]
- Abit Kocaman, A.; Aydoğan Arslan, S. Comparison of gait speed, dynamic balance, and dual-task balance performance according to kinesiophobia level in older adults. Somatosens. Mot. Res. 2023, 1–7. [Google Scholar] [CrossRef]
- Ito, T.; Sakai, Y.; Nishio, R.; Ito, Y.; Yamazaki, K.; Morita, Y. Relationship between postural stability and fall risk in elderly people with lumbar spondylosis during local vibratory stimulation for proprioception: A retrospective study. Somatosens. Mot. Res. 2020, 37, 133–137. [Google Scholar] [CrossRef] [PubMed]
- Song, Q.; Zhang, X.; Mao, M.; Sun, W.; Zhang, C.; Chen, Y.; Li, L. Relationship of proprioception, cutaneous sensitivity, and muscle strength with the balance control among older adults. J. Sport Health Sci. 2021, 10, 585–593. [Google Scholar] [CrossRef] [PubMed]
- An, H.; He, R.-H.; Zheng, Y.-R.; Tao, R. Cognitive-behavioral therapy. Subst. Non-Subst. Addict. 2017, 491, 321–329. [Google Scholar]
- Murphy, R.; Calugi, S.; Cooper, Z.; Dalle Grave, R. Challenges and opportunities for enhanced cognitive behaviour therapy (CBT-E) in light of COVID-19. Cogn. Behav. Ther. 2020, 13, e14. [Google Scholar] [CrossRef]
- Hajihasani, A.; Rouhani, M.; Salavati, M.; Hedayati, R.; Kahlaee, A.H. The influence of cognitive behavioral therapy on pain, quality of life, and depression in patients receiving physical therapy for chronic low back pain: A systematic review. Pmr 2019, 11, 167–176. [Google Scholar] [CrossRef]

| Variables | CLBP Group (n = 83) | Asymptomatic (n = 95) | p-Value |
|---|---|---|---|
| Age (years) | 48.9 ± 7.5 | 49.4 ± 7.0 | 0.686 |
| Gender (Male/Female) (n%) | 49:34 | 62:33 | 0.727 |
| BMI (kg/m2) | 26.3 ± 7.4 | 25.8 ± 8.6 | 0.198 |
| Duration of back pain (Months) | 22.3 ± 10.8 | - | - |
| Use of medication (yes/No) (n%) | 58 (69.9%)/25 (30.1%) | - | - |
| VAS (0–10 cm) | 4.9 ± 1.8 | - | - |
| ODI (0–100%) | 31.7 ± 5.0 | - | - |
| Kinesiophobia | 41.2 ± 3.2 | - | |
| LJPS in flexion (°) | 4.9 ± 1.4 | 2.4 ± 1.2 | <0.001 |
| LJPS in Extension (°) | 5.2 ± 1.3 | 1.4 ± 1.2 | <0.001 |
| LJPS in side-bending left (°) | 4.8 ± 1.5 | 2.9 ± 0.7 | <0.001 |
| LJPS in side-bending right (°) | 4.8 ± 1.5 | 2.8 ± 0.6 | <0.001 |
| Test Variables | Kinesiophobia (TSK Score) | |
|---|---|---|
| r | p-Value | |
| LJPS in flexion (°) | 0.51 | <0.001 |
| LJPS in extension (°) | 0.41 | <0.001 |
| LJPS in side-bending left (°) | 0.37 | 0.001 |
| LJPS in side-bending right (°) | 0.34 | 0.002 |
| Test Variables | Total Effect—Direct and Indirect | Direct Effect | Indirect Effect | ||||||
|---|---|---|---|---|---|---|---|---|---|
| B | SE | p-Value | B | SE | p-Value | B | SE | p-Value | |
| Pain × LJPS in flexion (°) × TSK | 0.22 | 0.04 | <0.001 | 0.22 | 0.04 | <0.001 | 0.06 | 0.01 | 0.001 |
| Pain × LJPS in extension (°) × TSK | 0.23 | 0.05 | <0.001 | 0.21 | 0.03 | <0.001 | 0.05 | 0.01 | 0.001 |
| Pain × LJPS in side-bending left (°) × TSK | 0.18 | 0.05 | 0.001 | 0.18 | 0.05 | 0.001 | 0.10 | 0.02 | 0.002 |
| Pain × LJPS in side-bending right (°) × TSK | 0.16 | 0.05 | 0.002 | 0.17 | 0.05 | 0.001 | 0.28 | 0.02 | 0.002 |
| Test Variables | Sobel-Test | SE | p-Value |
|---|---|---|---|
| Pain × LJPS in flexion (°) × TSK | 0.29 | 0.03 | 0.030 |
| Pain × LJPS in extension (°) × TSK | 0.24 | 0.02 | 0.020 |
| Pain × LJPS in side-bending left (°) × TSK | 0.15 | 0.03 | 0.018 |
| Pain × LJPS in side-bending right (°) × TSK | 0.78 | 0.08 | 0.024 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
ALMohiza, M.A.; Reddy, R.S.; Asiri, F.; Alshahrani, A.; Tedla, J.S.; Dixit, S.; Gular, K.; Kakaraparthi, V.N. The Mediation Effect of Pain on the Relationship between Kinesiophobia and Lumbar Joint Position Sense in Chronic Low Back Pain Individuals: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2023, 20, 5193. https://doi.org/10.3390/ijerph20065193
ALMohiza MA, Reddy RS, Asiri F, Alshahrani A, Tedla JS, Dixit S, Gular K, Kakaraparthi VN. The Mediation Effect of Pain on the Relationship between Kinesiophobia and Lumbar Joint Position Sense in Chronic Low Back Pain Individuals: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2023; 20(6):5193. https://doi.org/10.3390/ijerph20065193
Chicago/Turabian StyleALMohiza, Mohammad A., Ravi Shankar Reddy, Faisal Asiri, Adel Alshahrani, Jaya Shanker Tedla, Snehil Dixit, Kumar Gular, and Venkata Nagaraj Kakaraparthi. 2023. "The Mediation Effect of Pain on the Relationship between Kinesiophobia and Lumbar Joint Position Sense in Chronic Low Back Pain Individuals: A Cross-Sectional Study" International Journal of Environmental Research and Public Health 20, no. 6: 5193. https://doi.org/10.3390/ijerph20065193
APA StyleALMohiza, M. A., Reddy, R. S., Asiri, F., Alshahrani, A., Tedla, J. S., Dixit, S., Gular, K., & Kakaraparthi, V. N. (2023). The Mediation Effect of Pain on the Relationship between Kinesiophobia and Lumbar Joint Position Sense in Chronic Low Back Pain Individuals: A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 20(6), 5193. https://doi.org/10.3390/ijerph20065193








