Objectively-Assessed Ultraviolet Radiation Exposure and Sunburn Occurrence
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedures
2.3. Measures
3. Results
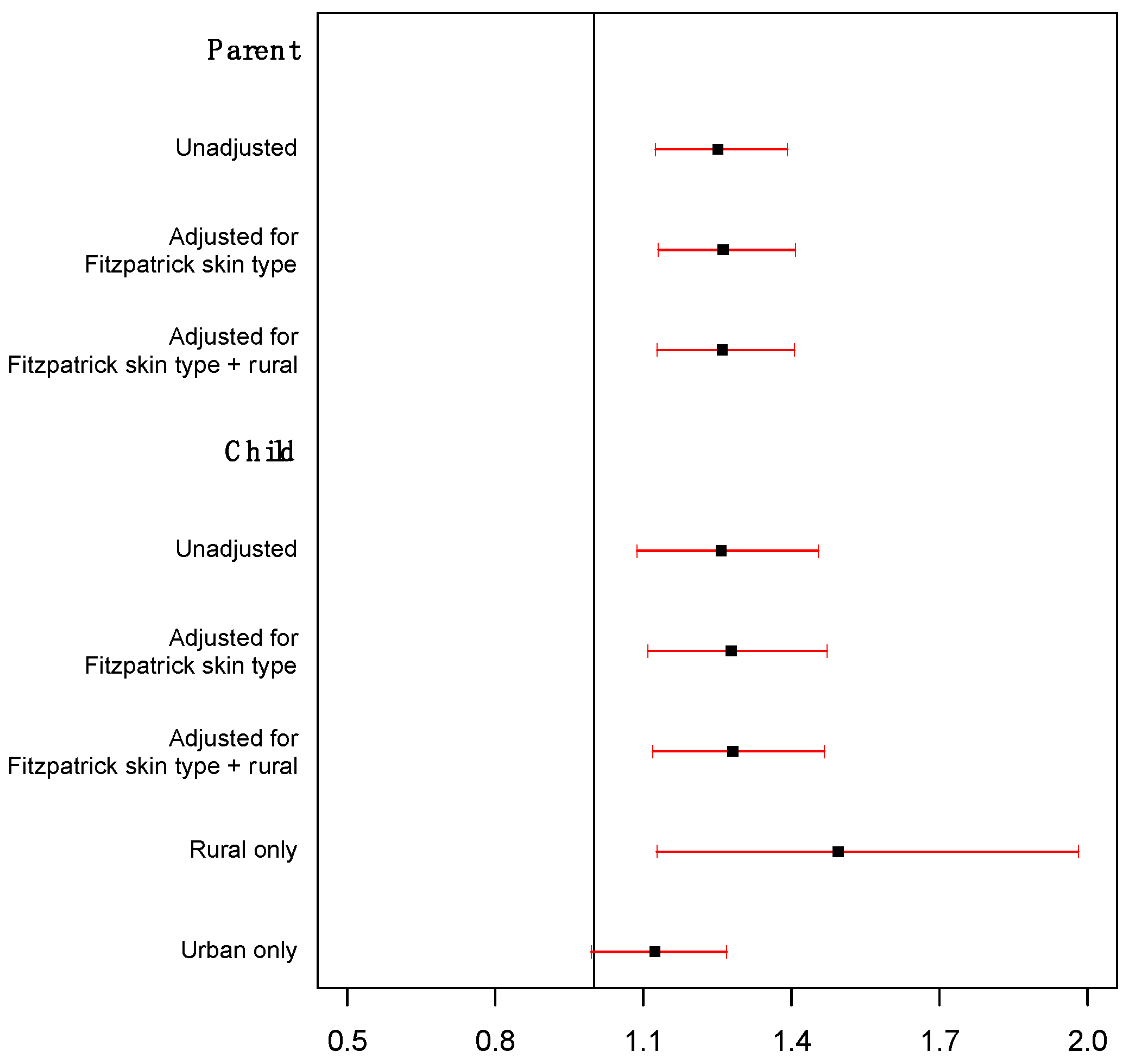
Objectively Measured UVR Exposure and Sunburn Occurrence
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Fitzpatrick Skin Type |
| Parent Baseline (Self) Parent Baseline (Reported on child) Child (Self) |
| Your eye color is: |
| Light blue, light gray, or light green Blue, gray, or green Hazel or light brown Dark brown Brownish black |
| Your natural hair color is: |
| Red or light blonde Blonde Dark blonde or light brown Dark brown Black |
| Your natural skin color (before sun exposure) is: |
| Ivory white Fair or pale Fair to beige, with golden undertone Olive or light brown Dark brown or black |
| How many freckles do you have on unexposed areas of your skin? |
| Many Several A few Very few None |
| How does your skin respond to the sun? |
| Always burns, blisters, and peels Often burns, blisters, and peels Burns moderately Burns rarely, if at all Never burns |
| Does your skin tan? |
| Never—I always burn Seldom Sometimes Often Always |
| How deeply do you tan? |
| Not at all or very little Lightly Moderately Deeply My skin is naturally dark |
| How sensitive is your face to the sun? |
| Very sensitive Sensitive Normal Resistant Very resistant/never had a problem |
| Compliance Answered about self | ||
| Did you wear the Shade device today? | ||
| Yes No | ||
| When did you wear the Shade device today? | ||
| I put it on in the morning and wore it all day (except in the shower or while swimming), and took it off again in the evening I wore it most of the time I only wore it when I went outside I only wore it if the sun was shining Other (specify) | ||
| Sunburn Answered about self Answered by parent about child | ||
| Yes | No | |
| Today, did you get a red OR painful sunburn? | ||
References
- Rogers, H.W.; Weinstock, M.A.; Feldman, S.R.; Coldiron, B.M. Incidence Estimate of Nonmelanoma Skin Cancer (Keratinocyte Carcinomas) in the U.S. Population, 2012. JAMA Dermatol. 2015, 151, 1081–1086. [Google Scholar] [CrossRef]
- Apalla, Z.; Lallas, A.; Sotiriou, E.; Lazaridou, E.; Ioannides, D. Epidemiological trends in skin cancer. Dermatol. Pr. Concept. 2017, 7, 1–6. [Google Scholar] [CrossRef] [PubMed]
- CDC. Centers for Disease Control and Prevention. Melanoma Incidence and Mortality, United States—2012–2016; USCS Data Brief. 2019. Available online: https://www.cdc.gov/cancer/uscs/pdf/USCS-DataBrief-No9-July2019-h.pdf (accessed on 12 January 2023).
- Koh, H.K.; Geller, A.C.; Miller, D.R.; Grossbart, T.A.; Lew, R.A. Prevention and early detection strategies for melanoma and skin cancer. Current status. Arch. Dermatol. 1996, 132, 436–443. [Google Scholar] [CrossRef] [PubMed]
- Parkin, D.M.; Mesher, D.; Sasieni, P. 13. Cancers attributable to solar (ultraviolet) radiation exposure in the UK in 2010. Br. J. Cancer 2011, 105 (Suppl. S2), S66–S69. [Google Scholar] [CrossRef]
- Armstrong, B.K.; Kricker, A. The epidemiology of UV induced skin cancer. J. Photochem. Photobiol. B Biol. 2001, 63, 8–18. [Google Scholar] [CrossRef]
- Balk, S.J. Ultraviolet radiation: A hazard to children and adolescents. Pediatrics 2011, 127, e791–e817. [Google Scholar] [CrossRef]
- Rodriguez-Acevedo, A.J.; Green, A.C.; Sinclair, C.; van Deventer, E.; Gordon, L.G. Indoor tanning prevalence after the International Agency for Research on Cancer statement on carcinogenicity of artificial tanning devices: Systematic review and meta-analysis. Br. J. Dermatol. 2020, 182, 849–859. [Google Scholar] [CrossRef]
- Geller, A.C.; Colditz, G.; Oliveria, S.; Emmons, K.; Jorgensen, C.; Aweh, G.N.; Frazier, A.L. Use of sunscreen, sunburning rates, and tanning bed use among more than 10,000 US children and adolescents. Pediatrics 2002, 109, 1009–1014. [Google Scholar] [CrossRef] [PubMed]
- Morton, R.L.; Asher, R.; Peyton, E.; Tran, A.; Smit, A.K.; Butow, P.N.; Kimlin, M.G.; Dobbinson, S.J.; Wordsworth, S.; Keogh, L.; et al. Risk attitudes and sun protection behaviour: Can behaviour be altered by using a melanoma genomic risk intervention? Cancer Epidemiol. 2019, 61, 8–13. [Google Scholar] [CrossRef]
- Stump, T.K.; Spring, B.; Marchese, S.H.; Alshurafa, N.; Robinson, J.K. Toward a precision behavioral medicine approach to addressing high-risk sun exposure: A qualitative analysis. JAMIA Open 2019, 2, 547–553. [Google Scholar] [CrossRef]
- Parsons, B.G.; Nagelhout, E.S.; Wankier, A.P.; Hu, N.; Lensink, R.; Zhu, A.; Nottingham, K.; Grossman, D.; Jensen, J.D.; Wu, Y.P. Reactivity to UV Radiation Exposure Monitoring Using Personal Exposure Devices for Skin Cancer Prevention: Longitudinal Observational Study. JMIR mHealth uHealth 2021, 9, e29694. [Google Scholar] [CrossRef]
- Xu, S.; Stump, T.K.; Jain, J.; Alshurafa, N.; Robinson, J.K. Variation in daily ultraviolet radiation exposure and sun protection behaviours of melanoma survivors: An observational single-arm pilot study with a wearable sensor. Br. J. Dermatol. 2019, 180, 413–414. [Google Scholar] [CrossRef]
- Thieden, E.; Philipsen, P.A.; Sandby-Møller, J.; Wulf, H.C. Sunburn Related to UV Radiation Exposure, Age, Sex, Occupation, and Sun Bed Use Based on Time-Stamped Personal Dosimetry and Sun Behavior Diaries. Arch. Dermatol. 2005, 141, 482–488. [Google Scholar] [CrossRef] [PubMed]
- Matsumura, Y.; Ananthaswamy, H.N. Toxic effects of ultraviolet radiation on the skin. Toxicol. Appl. Pharmacol. 2004, 195, 298–308. [Google Scholar] [CrossRef] [PubMed]
- Chalada, M.; Ramlogan-Steel, C.A.; Dhungel, B.P.; Layton, C.J.; Steel, J.C. The Impact of Ultraviolet Radiation on the Aetiology and Development of Uveal Melanoma. Cancers 2021, 13, 1700. [Google Scholar] [CrossRef]
- Kutlubay, Z.; Sevim, A.; Engin, B.; Tuzun, Y. Photodermatoses, including phototoxic and photoallergic reactions (internal and external). Clin. Dermatol. 2014, 32, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Yam, J.C.S.; Kwok, A.K.H. Ultraviolet light and ocular diseases. Int. Ophthalmol. 2014, 34, 383–400. [Google Scholar] [CrossRef] [PubMed]
- Lozzi, F.; Di Raimondo, C.; Lanna, C.; Diluvio, L.; Mazzilli, S.; Garofalo, V.; Dika, E.; Dellambra, E.; Coniglione, F.; Bianchi, L.; et al. Latest Evidence Regarding the Effects of Photosensitive Drugs on the Skin: Pathogenetic Mechanisms and Clinical Manifestations. Pharmaceutics 2020, 12, 1104. [Google Scholar] [CrossRef] [PubMed]
- Nagelhout, E.S.; Lensink, R.; Zhu, A.; Parsons, B.G.; Jensen, J.D.; Wu, Y.P. The feasibility and acceptability of using a wearable UV radiation exposure monitoring device in adults and children: Cross-sectional questionnaire study. J. Med. Internet Res. Dermatol. 2020, 3, e15711. [Google Scholar] [CrossRef]
- Wu, Y.P.; Parsons, B.G.; Jo, Y.; Chipman, J.; Haaland, B.A.; Nagelhout, E.S.; Carrington, J.; Wankier, A.P.; Brady, H.L.; Grossman, D. Outdoor activities and sunburn among urban and rural families: Implications for skin cancer prevention. Prev. Med. Rep. 2022, 29, 101914. [Google Scholar] [CrossRef]
- Nagelhout, E.S.; Lensink, R.; Zhu, A.; Parsons, B.G.; Haaland, B.; Hashibe, M.; Grossman, D.; VanDerslice, J.; Gren, L.H.; Jensen, J.D.; et al. Higher ultraviolet radiation exposure among rural-dwelling versus urban-dwelling adults and children: Implications for skin cancer prevention. J. Community Health 2021, 46, 147–155. [Google Scholar] [CrossRef] [PubMed]
- Whiteman, D.; Green, A. Melanoma and sunburn. Cancer Causes Control 1994, 5, 564–572. [Google Scholar] [CrossRef]
- Climate Prediction Center. Daily UV Index, Salt Lake City, UT. 2017. Available online: https://www.cpc.ncep.noaa.gov/products/stratosphere/uv_index/gif_files/slc_17.png (accessed on 28 February 2023).
- Banerjee, S.; Hoch, E.G.; Kaplan, P.D.; Dumont, E.L. A comparative study of wearable ultraviolet radiometers. In Proceedings of the 2017 IEEE Life Sciences Conference (LSC), Sydney, Australia, 13–15 December 2017; pp. 9–12. [Google Scholar]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef]
- WWAMI Rural Health Research Center. Rural Urban Commuting Area Codes. Available online: http://depts.washington.edu/uwruca/ (accessed on 18 March 2020).
- Fitzpatrick, T.B. The validity and practicality of sun-reactive skin types I through VI. Arch. Dermatol. 1988, 124, 869–871. [Google Scholar] [CrossRef]
- Glanz, K.; Yaroch, A.L.; Dancel, M.; Saraiya, M.; Crane, L.A.; Buller, D.B.; Manne, S.; O’Riordan, D.L.; Heckman, C.J.; Hay, J.; et al. Measures of Sun Exposure and Sun Protection Practices for Behavioral and Epidemiologic Research. Arch. Dermatol. 2008, 144, 217–222. [Google Scholar] [CrossRef]
- Diffey, B.L.; Jansen, C.T.; Urbach, F.; Wulf, H.C. The standard erythema dose: A new photobiological concept. Photodermatol. Photoimmunol. Photomed. 1997, 13, 64–66. [Google Scholar] [CrossRef]
- Zeger, S.L.; Liang, K.-Y.; Albert, P.S. Models for longitudinal data: A generalized estimating equation approach. Biometrics 1988, 44, 1049–1060. [Google Scholar] [CrossRef] [PubMed]
- Jewett, P.I.; Lazovich, D.; Wehelie, H.; Boull, C.; Vogel, R.I. Sun exposure and protection behaviors in urban and rural long-term melanoma survivors. Arch. Dermatol. Res. 2020, 312, 413–420. [Google Scholar] [CrossRef] [PubMed]
- Vogel, R.I.; Jewett, P.I.; Ahmed, R.L.; Lazovich, D. Comparison of sun exposure and protection behaviors between urban and rural residents without a history of melanoma in the Midwestern United States. J. Am. Acad. Dermatol. 2021, 86, 229–232. [Google Scholar] [CrossRef]
- Zahnd, W.E.; Goldfarb, J.; Scaife, S.L.; Francis, M.L. Rural-urban differences in behaviors to prevent skin cancer: An analysis of the Health Information National Trends Survey. J. Am. Acad. Dermatol. 2010, 62, 950–956. [Google Scholar] [CrossRef]
- Henning, A.; Downs, N.; Vanos, J.K. Wearable ultraviolet radiation sensors for research and personal use. Int. J. Biometeorol. 2022, 66, 627–640. [Google Scholar] [CrossRef] [PubMed]
- Hacker, E.; Horsham, C.; Vagenas, D.; Jones, L.; Lowe, J.; Janda, M. A Mobile Technology Intervention With Ultraviolet Radiation Dosimeters and Smartphone Apps for Skin Cancer Prevention in Young Adults: Randomized Controlled Trial. JMIR mHealth uHealth 2018, 6, e199. [Google Scholar] [CrossRef] [PubMed]
- Robinson, J.K.; Durst, D.A.; Gray, E.; Kwasny, M.; Heo, S.Y.; Banks, A.; Rogers, J.A. Sun exposure reduction by melanoma survivors with wearable sensor providing real-time UV exposure and daily text messages with structured goal setting. Arch. Dermatol. Res. 2021, 313, 685–694. [Google Scholar] [CrossRef]
- Horsham, C.; Antrobus, J.; Olsen, C.M.; Ford, H.; Abernethy, D.; Hacker, E. Testing Wearable UV Sensors to Improve Sun Protection in Young Adults at an Outdoor Festival: Field Study. JMIR mHealth uHealth 2020, 8, e21243. [Google Scholar] [CrossRef] [PubMed]
- Schmalwieser, A.W.; Casale, G.R.; Colosimo, A.; Schmalwieser, S.S.; Siani, A.M. Review on Occupational Personal Solar UV Exposure Measurements. Atmosphere 2021, 12, 142. [Google Scholar] [CrossRef]
- Schmalwieser, A.W.; Siani, A.M. Review on Nonoccupational Personal Solar UV Exposure Measurements. Photochem. Photobiol. 2018, 94, 900–915. [Google Scholar] [CrossRef] [PubMed]
- Urbach, F. Geographic pathology of skin cancer. In The Biologic Effects of Ultraviolet Radiation with Emphasis on the Skin; Urbach, F., Ed.; Pergamon Press: Oxford, UK, 1969; pp. 635–650. [Google Scholar]
- Challoner, A.V.; Corless, D.; Davis, A.; Deane, G.H.; Diffey, B.L.; Gupta, S.P.; Magnus, I.A. Personnel monitoring of exposure to ultraviolet radiation. Clin. Exp. Dermatol. 1976, 1, 175–179. [Google Scholar] [CrossRef]
- Diffey, B.L.; Kerwin, M.; Davis, A. The anatomical distribution of sunlight. Br. J. Dermatol. 1977, 97, 407–410. [Google Scholar] [CrossRef]
- Heydenreich, J.; Wulf, H.C. Miniature personal electronic UVR dosimeter with erythema response and time-stamped readings in a wristwatch. Photochem. Photobiol. 2005, 81, 1138–1144. [Google Scholar] [CrossRef]
- Thieden, E.; Philipsen, P.A.; Heydenreich, J.; Wulf, H.C. UV radiation exposure related to age, sex, occupation, and sun behavior based on time-stamped personal dosimeter readings. Arch. Dermatol. 2004, 140, 197–203. [Google Scholar] [CrossRef]
- Oliveria, S.A.; Saraiya, M.; Geller, A.C.; Heneghan, M.K.; Jorgensen, C. Sun exposure and risk of melanoma. Arch. Dis. Child. 2006, 91, 131–138. [Google Scholar] [CrossRef] [PubMed]
- Yu, C.L.; Li, Y.; Freedman, D.M.; Fears, T.R.; Kwok, R.; Chodick, G.; Alexander, B.; Kimlin, M.G.; Kricker, A.; Armstrong, B.K.; et al. Assessment of Lifetime Cumulative Sun Exposure Using a Self-Administered Questionnaire: Reliability of Two Approaches. Cancer Epidemiol. Biomark. Prev. 2009, 18, 464–471. [Google Scholar] [CrossRef] [PubMed]
- Stump, T.K.; Aspinwall, L.G.; Drummond, D.M.; Taber, J.M.; Kohlmann, W.; Champine, M.; Cassidy, P.B.; Petrie, T.; Liley, B.; Leachman, S.A. CDKN2A testing and genetic counseling promote reductions in objectively measured sun exposure one year later. Genet. Med. 2020, 22, 26–34. [Google Scholar] [CrossRef] [PubMed]
- Casale, G.R.; Siani, A.M.; Diemoz, H.; Agnesod, G.; Parisi, A.V.; Colosimo, A. Extreme UV index and solar exposures at Plateau Rosa (3500 m.a.s.l.) in Valle d’Aosta Region, Italy. Sci. Total Environ. 2015, 512, 622–630. [Google Scholar] [CrossRef] [PubMed]
- Diffey, B.L.; Oakley, A.M. The onset of ultraviolet erythema. Br. J. Dermatol. 1987, 116, 183–187. [Google Scholar] [CrossRef]
- Beattie, P.E.; Dawe, R.S.; Ferguson, J.; Ibbotson, S.H. Dose-response and time-course characteristics of UV-A1 erythema. Arch. Dermatol. 2005, 141, 1549–1555. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stump, T.K.; Fastner, S.; Jo, Y.; Chipman, J.; Haaland, B.; Nagelhout, E.S.; Wankier, A.P.; Lensink, R.; Zhu, A.; Parsons, B.; et al. Objectively-Assessed Ultraviolet Radiation Exposure and Sunburn Occurrence. Int. J. Environ. Res. Public Health 2023, 20, 5234. https://doi.org/10.3390/ijerph20075234
Stump TK, Fastner S, Jo Y, Chipman J, Haaland B, Nagelhout ES, Wankier AP, Lensink R, Zhu A, Parsons B, et al. Objectively-Assessed Ultraviolet Radiation Exposure and Sunburn Occurrence. International Journal of Environmental Research and Public Health. 2023; 20(7):5234. https://doi.org/10.3390/ijerph20075234
Chicago/Turabian StyleStump, Tammy K., Suzanne Fastner, Yeonjung Jo, Jonathan Chipman, Benjamin Haaland, Elizabeth S. Nagelhout, Ali P. Wankier, Riley Lensink, Angela Zhu, Bridget Parsons, and et al. 2023. "Objectively-Assessed Ultraviolet Radiation Exposure and Sunburn Occurrence" International Journal of Environmental Research and Public Health 20, no. 7: 5234. https://doi.org/10.3390/ijerph20075234




