Effectiveness of Nonpharmacological Interventions in the Field of Ventilation: An Umbrella Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Review Questions
2.2. Inclusion Criteria
2.3. Search Strategy
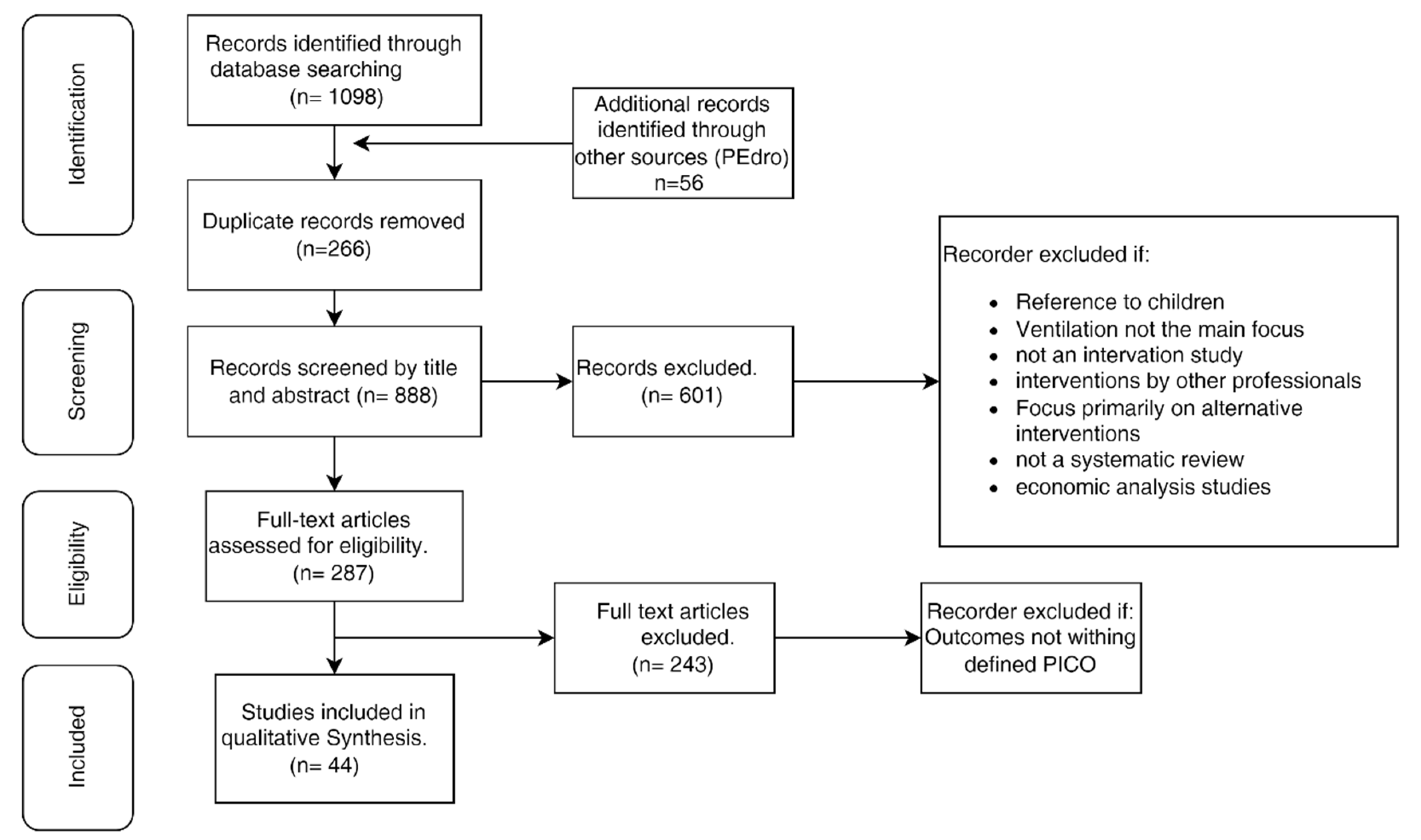
2.4. Study Selection
2.5. Data Extraction
2.6. Data Synthesis
3. Results
3.1. Review Selection
3.2. Methodological Quality
3.3. Intervention Characteristics (Type/Frequency/Duration/Intensity)
3.4. Review Findings—Effects of Compromised Ventilation: Spirometry, Pulmonary Function, and Pimax/Pemax
3.5. Frequency and Breathing Rate, Tidal Volume, Oxygen Saturation, and Dyspnea
3.6. Functional Capacity
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Donner, C.; Ambrosino, N.; Goldstein, R. Pulmonary Rehabilitation, 2nd ed.; CRC Press: London, UK, 2020. [Google Scholar] [CrossRef]
- Dean, E.; Frownfelter, D.L. Cardiovascular and Pulmonary Physical Therapy: Evidence and Practice, 5th ed.; Mosby: St. Louis, MO, USA, 2005. [Google Scholar]
- International Council of Nurses. ICNP Browser. 2019. Available online: https://www.icn.ch/what-we-do/projects/ehealth-icnptm/icnp-browser (accessed on 20 March 2022).
- Frownfelter, D.L.; Dean, E.; Stout, M.; Kruger, R.; Anthony, J. Cardiovascular and Pulmonary Physical Therapy: Evidence and Practice; St. Mosby Elsevier: New York, NY, USA, 2021. [Google Scholar]
- ICN. Classificação Internacional Para a Prática de Enfermagem Versão 2; Ordem dos Enfermeiros: Lisboa, Portugal, 2011. [Google Scholar]
- SNOMED. Guia Técnico de Mapeamento CID-10 (PT). Available online: https://confluence.ihtsdotools.org/display/DOCICDMGPT (accessed on 5 December 2022).
- Aromataris, E.; Fernandez, R.; Godfrey, C.; Holly, C.; Khalil, H.; Tungpunkom, P. Chapter 10: Umbrella Reviews. In JBI Manual for Evidence Synthesis; Aromataris, E., Munn, Z., Eds.; JBI: Adelaide, Australia, 2020. [Google Scholar]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [Green Version]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Guyatt, G.H.; Oxman, A.D.; Vist, G.E.; Kunz, R.; Falck-Ytter, Y.; Alonso-Coello, P.; Schünemann, H.J. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008, 336, 924–926. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McMahon, L.; Blake, C.; Lennon, O. Nonpharmacological interventions for respiratory health in Parkinson’s disease: A systematic review and meta-analysis. Eur. J. Neurol. 2021, 28, 1022–1040. [Google Scholar] [CrossRef]
- Wu, F.; Liu, Y.; Ye, G.; Zhang, Y. Respiratory Muscle Training Improves Strength and Decreases the Risk of Respiratory Complications in Stroke Survivors: A Systematic Review and Meta-analysis. Arch. Phys. Med. Rehabil. 2020, 101, 1991–2001. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Wei, L.; Wang, S.; Ke, L.; Zhao, H.; Mao, J.; Li, J.; Mao, Z. The effects of pursed lip breathing combined with diaphragmatic breathing on pulmonary function and exercise capacity in patients with COPD: A systematic review and meta-analysis. Physiother. Theory Pract. 2020, 38, 847–857. [Google Scholar] [CrossRef]
- Chorattas, A.; Papastavrou, E.; Charalambous, A.; Kouta, C. Home-Based Educational Programs for Management of Dyspnea: A Systematic Literature Review. Home Health Care Manag. Pract. 2020, 32, 211–217. [Google Scholar] [CrossRef]
- Habib, G.M.; Rabinovich, R.; Divgi, K.; Ahmed, S.; Saha, S.K.; Singh, S.; Uddin, A.; Uzzaman, N.; Pinnock, H. Systematic review of clinical effectiveness, components, and delivery of pulmonary rehabilitation in low-resource settings. npj Prim. Care Respir. Med. 2020, 30, 52. [Google Scholar] [CrossRef]
- Hindelang, M.; Kirsch, F.; Leidl, R. Effectiveness of non-pharmacological COPD management on health-related quality of life–A systematic review. Expert Rev. Pharm. Outcomes Res. 2020, 20, 79–91. [Google Scholar] [CrossRef] [PubMed]
- Kokotovic, D.; Berkfors, A.; Gögenur, I.; Ekeloef, S.; Burcharth, J. The effect of postoperative respiratory and mobilization interventions on postoperative complications following abdominal surgery: A systematic review and meta-analysis. Eur. J. Trauma Emerg. Surg. 2020, 47, 975–990. [Google Scholar] [CrossRef]
- Zhang, X.; Zheng, Y.; Dang, Y.; Wang, L.; Cheng, Y.; Zhang, X.; Mao, M.; Lu, X. Can inspiratory muscle training benefit patients after stroke? A systematic review and meta-analysis of randomized controlled trials. Clin. Rehabil. 2020, 34, 866–876. [Google Scholar] [CrossRef]
- Rosa Silva, J.P.; Júnior, J.B.S.; dos Santos, E.L.; de Carvalho, F.O.; Costa, I.M.P.D.F.; de Mendonça, D.M.F. Quality of life and functional independence in amyotrophic lateral sclerosis: A systematic review. Neurosci. Biobehav. Rev. 2020, 111, 1–11. [Google Scholar] [CrossRef] [PubMed]
- van de Wetering-van Dongen, V.A.; Kalf, J.G.; van der Wees, P.J.; Bloem, B.R.; Nijkrake, M.J. The Effects of Respiratory Training in Parkinson’s Disease: A Systematic Review. J. Park. Dis. 2020, 10, 1315–1333. [Google Scholar] [CrossRef] [PubMed]
- Machado, A.; Silva, P.M.; Afreixo, V.; Caneiras, C.; Burtin, C.; Marques, A. Design of pulmonary rehabilitation programmes during acute exacerbations of COPD: A systematic review and network meta-analysis. Eur. Respir. Rev. 2020, 29, 200039. [Google Scholar] [CrossRef] [PubMed]
- Desjardins, M.; Bonilha, H.S. The Impact of Respiratory Exercises on Voice Outcomes: A Systematic Review of the Literature. J. Voice 2019, 34, 648.e1–648.e39. [Google Scholar] [CrossRef] [PubMed]
- Sadek, Z.; Salami, A.; Joumaa, W.H.; Awada, C.; Ahmaidi, S.; Ramadan, W. Best mode of inspiratory muscle training in heart failure patients: A systematic review and meta-analysis. Eur. J. Prev. Cardiol. 2018, 25, 1691–1701. [Google Scholar] [CrossRef]
- Bolger, J.C.; Loughney, L.; Tully, R.; Cunningham, M.; Keogh, S.; McCaffrey, N.; Hickey, W.; Robb, W.B. Perioperative prehabilitation and rehabilitation in esophagogastric malignancies: A systematic review. Dis. Esophagus 2019, 32, doz058. [Google Scholar] [CrossRef]
- Yu, X.; Li, X.; Wang, L.; Liu, R.; Xie, Y.; Li, S.; Li, J. Pulmonary Rehabilitation for Exercise Tolerance and Quality of Life in IPF Patients: A Systematic Review and Meta-Analysis. BioMed Res. Int. 2019, 2019, 8498603 . [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.Q.; Liu, X.; Jia, Y.; Xie, J. Impact of breathing exercises in subjects with lung cancer undergoing surgical resection: A systematic review and meta-analysis. J. Clin. Nurs. 2018, 28, 717–732. [Google Scholar] [CrossRef]
- Katz, S.; Arish, N.; Rokach, A.; Zaltzman, Y.; Marcus, E.-L. The effect of body position on pulmonary function: A systematic review. BMC Pulm. Med. 2018, 18, 1–16. [Google Scholar] [CrossRef]
- Lee, E.N.; Kim, M.J. Meta-analysis of the Effect of a Pulmonary Rehabilitation Program on Respiratory Muscle Strength in Patients with Chronic Obstructive Pulmonary Disease. Asian Nurs. Res. 2019, 13, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vorona, S.; Sabatini, U.; Al-Maqbali, S.; Bertoni, M.; Dres, M.; Bissett, B.; Van Haren, F.; Martin, A.D.; Urrea, C.; Brace, D.; et al. Inspiratory Muscle Rehabilitation in Critically Ill Adults. A Systematic Review and Meta-Analysis. Ann. Am. Thorac. Soc. 2018, 15, 735–744. [Google Scholar] [CrossRef] [PubMed]
- Torres-Sánchez, I.; Cruz-Ramírez, R.; Cabrera-Martos, I.; Díaz-Pelegrina, A.; Valenza, M.C. Results of Physiotherapy Treatments in Exacerbations of Chronic Obstructive Pulmonary Disease: A Systematic Review. Physiother. Can. 2017, 69, 122–132. [Google Scholar] [CrossRef] [Green Version]
- Narayanan, A.L.; Hamid, S.R.; Supriyanto, E. Evidence regarding patient compliance with incentive spirometry interventions after cardiac, thoracic and abdominal surgeries: A systematic literature review. Can. J. Respir. Ther. 2016, 52, 17–26. [Google Scholar] [PubMed]
- Volpe, M.S.; Aleixo, A.A.; De Almeida, P.R.M.N. Influence of inspiratory muscle training on weaning patients from mechanical ventilation: A systematic review. Fisioter. Em Mov. 2016, 29, 173–182. [Google Scholar] [CrossRef] [Green Version]
- Gomes Neto, M.; Martinez, B.P.; Reis, H.F.; Carvalho, V. Pre- and postoperative inspiratory muscle training in patients undergoing cardiac surgery: Systematic review and meta-analysis. Clin. Rehabil. 2016, 31, 454–464. [Google Scholar] [CrossRef]
- Macpherson, C.; Bassile, C.C. Pulmonary Physical Therapy Techniques to Enhance Survival in Amyotrophic Lateral Sclerosis: A Systematic Review. J. Neurol. Phys. Ther. 2016, 40, 165–175. [Google Scholar] [CrossRef]
- Mohammed, J.; Da Silva, H.; Van Oosterwijck, J.; Calders, P. Effect of respiratory rehabilitation techniques on the autonomic function in patients with chronic obstructive pulmonary disease: A systematic review. Chronic Respir. Dis. 2016, 14, 217–230. [Google Scholar] [CrossRef] [Green Version]
- Elkins, M.; Dentice, R. Inspiratory muscle training facilitates weaning from mechanical ventilation among patients in the intensive care unit: A systematic review. J. Physiother. 2015, 61, 125–134. [Google Scholar] [CrossRef] [Green Version]
- Martín-Valero, R.; Almeida, M.D.L.C.; Casuso-Holgado, M.J.; Heredia-Madrazo, A. Systematic Review of Inspiratory Muscle Training After Cerebrovascular Accident. Respir. Care 2015, 60, 1652–1659. [Google Scholar] [CrossRef] [Green Version]
- Mans, C.M.; Reeve, J.C.; Elkins, M.R. Postoperative outcomes following preoperative inspiratory muscle training in patients undergoing cardiothoracic or upper abdominal surgery: A systematic review and meta analysis. Clin. Rehabil. 2014, 29, 426–438. [Google Scholar] [CrossRef] [PubMed]
- Montemezzo, D.; Fregonezi, G.A.; Pereira, D.A.; Britto, R.R.; Reid, W.D. Influence of Inspiratory Muscle Weakness on Inspiratory Muscle Training Responses in Chronic Heart Failure Patients: A Systematic Review and Meta-Analysis. Arch. Phys. Med. Rehabil. 2014, 95, 1398–1407. [Google Scholar] [CrossRef]
- Neves, L.F.; Reis, M.H.; Plentz, R.D.; Matte, D.L.; Coronel, C.C.; Sbruzzi, G. Expiratory and Expiratory Plus Inspiratory Muscle Training Improves Respiratory Muscle Strength in Subjects With COPD: Systematic Review. Respir. Care 2014, 59, 1381–1388. [Google Scholar] [CrossRef] [Green Version]
- Snowdon, D.; Haines, T.; Skinner, E.H. Preoperative intervention reduces postoperative pulmonary complications but not length of stay in cardiac surgical patients: A systematic review. J. Physiother. 2014, 60, 66–77. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Osterling, K.; MacFadyen, K.; Gilbert, R.; Dechman, G. The effects of high intensity exercise during pulmonary rehabilitation on ventilatory parameters in people with moderate to severe stable COPD: A systematic review. Int. J. Chronic Obstr. Pulm. Dis. 2014, 9, 1069–1079. [Google Scholar] [CrossRef] [Green Version]
- Jácome, C.; Marques, A.S.P. Pulmonary Rehabilitation for Mild COPD: A Systematic Review. Respir. Care 2013, 59, 588–594. [Google Scholar] [CrossRef] [Green Version]
- Martín-Valero, R.; Zamora-Pascual, N.; Armenta-Peinado, J.A. Training of Respiratory Muscles in Patients with Multiple Sclerosis: A Systematic Review. Respir. Care 2014, 59, 1764–1772. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Singh, F.; Newton, R.U.; Galvão, D.A.; Spry, N.; Baker, M.K. A systematic review of pre-surgical exercise intervention studies with cancer patients. Surg. Oncol. 2013, 22, 92–104. [Google Scholar] [CrossRef]
- Scheffers, L.E.; Berg, L.E.M.V.; Ismailova, G.; Dulfer, K.; Takkenberg, J.J.M.; Helbing, W.A. Physical exercise training in patients with a Fontan circulation: A systematic review. Eur. J. Prev. Cardiol. 2020, 28, 1269–1278. [Google Scholar] [CrossRef]
- Silva, I.S.; Fregonezi, G.A.; AL Dias, F.; Ribeiro, C.T.; Guerra, R.O.; Ferreira, G.M. Inspiratory muscle training for asthma. Cochrane Database Syst. Rev. 2013, 2013, CD003792. [Google Scholar] [CrossRef]
- Smart, N.A.; Giallauria, F.; Dieberg, G. Efficacy of inspiratory muscle training in chronic heart failure patients: A systematic review and meta-analysis. Int. J. Cardiol. 2013, 167, 1502–1507. [Google Scholar] [CrossRef]
- Prem, V.; Sahoo, R.C.; Adhikari, P. Effect of diaphragmatic breathing exercise on quality of life in subjects with asthma: A systematic review. Physiother. Theory Pract. 2012, 29, 271–277. [Google Scholar] [CrossRef]
- Grams, S.T.; Ono, L.M.; de Noronha, M.; Schivinski, C.I.S.; Paulin, E. Breathing exercises in upper abdominal surgery: A systematic review and meta-analysis. Braz. J. Phys. Ther. 2012, 16, 345–353. [Google Scholar] [CrossRef] [Green Version]
- Thomas, M.J.; Simpson, J.; Riley, R.; Grant, E. The impact of home-based physiotherapy interventions on breathlessness during activities of daily living in severe COPD: A systematic review. Physiotherapy 2010, 96, 108–119. [Google Scholar] [CrossRef]
- Lewis, L.K.; Williams, M.T.; Olds, T. Short-term effects on outcomes related to the mechanism of intervention and physiological outcomes but insufficient evidence of clinical benefits for breathing control: A systematic review. Aust. J. Physiother. 2007, 53, 219–227. [Google Scholar] [CrossRef] [Green Version]
- Crowe, J.; Reid, W.D.; Geddes, E.L.; O’Brien, K.; Brooks, D. Inspiratory muscle training compared with other rehabilitation interventions in adults with chronic obstructive pulmonary disease: A systematic literature review and meta-analysis. COPD J. Chronic Obstr. Pulm. Dis. 2005, 2, 319–329. [Google Scholar] [CrossRef]
- Lacasse, Y.; Martin, S.; Lasserson, T.J.; Goldstein, R.S. Meta-analysis of respiratory rehabilitation in chronic obstructive pulmonary disease. A Cochrane systematic review. Eura Medicophys. 2007, 43, 475–485. [Google Scholar]
- Campbell, E.; Coulter, E.; Mattison, P.G.; Miller, L.; McFadyen, A.; Paul, L. Physiotherapy Rehabilitation for People with Progressive Multiple Sclerosis: A Systematic Review. Arch. Phys. Med. Rehabil. 2015, 97, 141–151.e3. [Google Scholar] [CrossRef] [Green Version]
- Kendall, F.; Oliveira, J.; Peleteiro, B.; Pinho, P.; Bastos, P.T. Inspiratory muscle training is effective to reduce postoperative pulmonary complications and length of hospital stay: A systematic review and meta-analysis. Disabil. Rehabil. 2017, 40, 864–882. [Google Scholar] [CrossRef]
- Carvalho, C.R.F.; Paisani, D.M.; Lunardi, A. Incentive spirometry in major surgeries: A systematic review. Braz. J. Phys. Ther. 2011, 15, 343–350. [Google Scholar] [CrossRef] [Green Version]
- Azambuja, A.D.C.M.; de Oliveira, L.Z.; Sbruzzi, G. Inspiratory Muscle Training in Patients with Heart Failure: What Is New? Systematic Review and Meta-Analysis. Phys. Ther. 2020, 100, 2099–2109. [Google Scholar] [CrossRef] [PubMed]
- Nepomuceno Júnior, B.R.V.; Gómez, T.B.; Neto, M.G. Use of Powerbreathe® in inspiratory muscle training for athletes: Systematic review. Fisioter. Em Mov. 2016, 29, 821–830. [Google Scholar] [CrossRef] [Green Version]
- Hough, A. Physiotherapy in Respiratory Care: An Evidence-based Approach to Respiratory and Cardiac Management; Nelson Thornes: Cheltenham, UK, 2001. [Google Scholar]
- Holland, A.; Corso, S.; Spruit, M. Pulmonary Rehabilitation; European Respiratory Society: Lausanne, Switzerland, 2021. [Google Scholar]
- West, J.B. Respiratory Physiology: The Essentials, 7th ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2004. [Google Scholar]
- JBI. Joanna Briggs Institute Levels of Evidence and Grades of Recommendation Working Party. JBI Grades of Recommendation. 2013. Available online: https://jbi.global/sites/default/files/2019-05/JBIgrades-of-recommendation_2014.pdf (accessed on 12 May 2022).
- Aromataris, E.; Munn, Z. (Eds.) JBI Manual for Evidence Synthesis; JBI: Adelaide, Australia, 2020; Available online: https://synthesismanual.jbi.global (accessed on 12 May 2022).

| Citation | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Quality |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| McMahon, L., Blake, C., & Lennon, O. (2021) [11] | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | High |
| Wu F, Liu Y, Ye G, Zhang Y (2020) [12] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | High |
| Ying Yang, Liuyi Wei, Shizhen Wang, et al. (2020) [13] | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | High |
| Chorattas A; Papastavrou, E; Charalambous A; Kouta C (2020) [14] | Y | Y | Y | Y | Y | Y | U | Y | Y | Y | Y | High |
| Habib GMM, Rabinovich R, Divgi K, et al. (2020) [15] | N | Y | Y | Y | U | Y | Y | N | N | Y | Y | Moderate |
| Michael Hindelang, Florian Kirsch & Reiner Leidl (2020) [16] | Y | Y | Y | Y | N | Y | Y | N | Y | Y | Y | High |
| Kokotovic, D.; Berkfors, A.; Gögenur, I.; et al. (2020) [17] | U | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | High |
| Zhang, X.; Zheng, Y.; Dang, Y.; et al (2020) [18] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | High |
| Rosa Silva JP, Santiago Júnior JB, Dos Santos, et al. (2020) [19] | Y | Y | Y | Y | Y | Y | N | N | N | Y | Y | Moderate |
| van de Wetering-van Dongen, V. A., Kalf, J. G., van der Wees, P. J., Bloem, B. R., & Nijkrake, M. J. (2020) [20] | N | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | High |
| Machado A, Matos Silva P, Afreixo V, Caneiras C, Burtin C, Marques A.(2020) [21] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | High |
| Desjardins, M., & Bonilha, H. S. (2020) [22] | Y | Y | N | Y | Y | Y | N | N | U | Y | Y | Moderate |
| Azambuja, A., de Oliveira, L. Z., & Sbruzzi, G. (2020) [23] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | High |
| Bolger JC, Loughney L, Tully R, et al. (2019) [24] | Y | Y | Y | Y | Y | Y | N | N | N | U | Y | Moderate |
| Yu X, Li X, Wang L, et al. (2019) [25] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | High |
| Wang YQ, Liu X, Jia Y, Xie J. (2018). [26] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | High |
| Katz, S., Arish, N., Rokach, A., Zaltzman, Y., & Marcus, E. L. (2018) [27] | U | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | High |
| Sadek Z, Salami A, Joumaa WH, et al. (2018) [23] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | High |
| Lee, E.N.;Kim M.J. (2019) [28] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | High |
| Vorona S, Sabatini U, Al-Maqbali S, et al. (2018) [29] | U | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | High |
| Torres-Sánchez I, Cruz-Ramírez R, Cabrera-Martos I, et al (2017) [30] | Y | Y | N | Y | Y | Y | N | N | N | Y | Y | Moderate |
| Narayanan AL, Hamid SR, Supriyanto E. (2016) [31] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | High |
| Volpe MS, Aleixo AA, Negreiros de Almeida PR (2016) [32] | Y | Y | Y | Y | Y | Y | Y | Y | U | Y | Y | High |
| Gomes Neto M, Martinez BP, Reis HF, Carvalho VO. (2016) [33] | Y | Y | Y | Y | Y | Y | Y | Y | U | Y | Y | High |
| Macpherson CE, Bassile CC (2016) [34] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | High |
| Mohammed J, Da Silva H, Van Oosterwijck J, Calders P. (2016) [35] | N | Y | Y | Y | Y | Y | N | U | Y | Y | Moderate | |
| Elkins M, Dentice R. (2015) [36] | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | Y | High |
| Martín-Valero R, De La Casa Almeida M, Casuso-Holgado MJ, Heredia-Madrazo A. (2015) [37]. | Y | Y | Y | Y | Y | Y | Y | Y | U | Y | Y | High |
| Mans, C. M., Reeve, J. C., & Elkins, M. R. (2015) [38] | Y | Y | Y | Y | Y | U | Y | Y | U | U | Y | Moderate |
| Montemezzo D, Fregonezi GA, Pereira DA, Britto RR, Reid WD. (2014) [39] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | High |
| Neves LF, Reis MH, Plentz RD, Matte DL, Coronel CC, Sbruzzi G. (2014) [40] | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | High |
| Snowdon D, Haines TP, Skinner EH. (2014) [41] | Y | Y | Y | Y | Y | Y | Y | Y | N | N | Y | Moderate |
| Osterling K, MacFadyen K, Gilbert R, Dechman G. (2014) [42] | Y | Y | N | Y | Y | Y | N | U | Y | Y | Y | Moderate |
| Jácome, C; Marques, A. (2014) [43] | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | High |
| Martín-Valero, R., Zamora-Pascual, N., & Armenta-Peinado, J. A. (2014) [44] | Y | Y | Y | Y | Y | Y | Y | N | N | Y | Y | Moderate |
| Singh F, Newton RU, Galvão DA, Spry N, Baker MK. (2013) [45] | U | Y | Y | Y | Y | Y | U | N | N | Y | Y | Moderate |
| O’Doherty AF, West M, Jack S, Grocott MP. (2013) [46] | Y | Y | Y | U | Y | Y | N | N | N | Y | Y | Moderate |
| Silva IS, Fregonezi GA, Dias FA, Ribeiro CT, Guerra RO, Ferreira GM. (2013) [47] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | High |
| Smart NA, Giallauria F, Dieberg G. (2013) [48] | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | High |
| Prem V, Sahoo RC, Adhikari P. (2013) [49] | Y | Y | Y | U | Y | Y | Y | Y | Y | Y | Y | High |
| Grams ST, Ono LM, Noronha MA, Schivinski CI, Paulin E. (2012) [50] | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | High |
| Thomas MJ, Simpson J, Riley R, Grant E. (2010) [51] | Y | Y | Y | Y | Y | Y | U | Y | N | Y | Y | Moderate |
| Lewis LK, Williams MT, Olds T. (2007) [52] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | High |
| Crowe J, Reid WD, Geddes EL, O’Brien K, Brooks D. (2005) [53] | Y | Y | Y | U | N | Y | Y | Y | N | Y | Y | Moderate |
| % | 84 | 100 | 93 | 93 | 93 | 98 | 77 | 72 | 51 | 91 | 100 | |
| Y. Yes, N. No, U. Unclear. |
| ID | Intervention | Duration | Length of Session, Frequency | Intensity |
|---|---|---|---|---|
| Ana Machado, et al. (2020) [21] | Inspiratory muscle training | 12 weeks | Two sessions per week to five sessions per day. Duration of sessions varied from < 15 min to 2 h. | |
| Desjardins, M., & Bonilha, H. S. (2020) [22] | Respiratory muscle training/IMT/EMT/ Incentive spirometry | 3 and 7 times a week | Five sets of five breaths with a pause between each set. | The threshold pressure was based on the participants’ maximum expiratory pressure (MEP) in the case of EMST and maximum inspiratory pressure (MIP) in the case of IMST. (75% MEP and 80% MIP). |
| Zhang, X.; et al. (2020) [18] | Respiratory muscle training | 3 weeks | Three repetitions per week for more than 20 min per day. | |
| van de Wetering-van Dongen, et al. (2020) [20] | Inspiratory muscle training | 4 to 12 weeks | Training frequency of 5 sets and 5 repetitions 6 days a week complemented by postural techniques. | A total of 75% MEP. |
| Lee, E.N; Kim, M.J. (2018) [28] | Respiratory muscle training | A total of 10 sessions for 90 min twice a week to daily. | ||
| Zahra Sadek, et al. (2018) [23] | Inspiratory muscle training | 6 to 12 weeks. | Three, six, or seven times per week for 15 to 30 min. | Intensity ranging from 30% to 60%. We can consider 60% of PImax to be the best intensity to apply. |
| Nepomuceno Jr BRV, et al. (2016) [59] | Inspiratory muscle training | 11 weeks | A total of 1 series of 30 breaths repeated twice daily. | Inspiratory load of approximately 50% of maximal inspiratory pressure (MIP). |
| Gomes Neto, M. et al. (2016) [33] | Inspiratory muscle training | A total of 3 to 5 series for 20–30 min with 10 repetitions. | A total of 15% to 60% of maximal inspiratory pressure. | |
| Chelsea E. Machpherson, Clare C. Bassile (2016) [34] | Inspiratory muscle training | A total of 10 min per day 2 to 3 times a day, which could be progressively increased. | ||
| Klefbeck and Hamrah Nedjad, 2003 in Campbell E.; et al (2015) [55] | Inspiratory muscle training | 10 weeks | A total of 3 sets of 10 repetitions twice every second day (n = 7). | |
| Martín-Valero, R., et al. (2015). [37] | Respiratory muscle training and inspiratory muscle protocol | 8-week training | A total of 5 d/week for 30 min/d. | Started with an intensity of 30% of PImax and increased 2 cm H2O. |
| Martín-Valero, R., et al. (2015). [37] | Program of conventional neurological rehabilitation that was supplemented with an inspiratory muscle training protocol with a threshold value | 6 weeks | A total of 2 sessions/d 6 times/week with each session lasting 15 min. | Started with an initial load of 40% until they reached 60% of the Pimax. |
| Martín-Valero, R. et al. (2014) [44] | Respiratory muscle training | 10 weeks to 3 months | Frequency of 7 d/week with 1 or 2 daily sessions consisting of 3 sets with 10 or 15 repetitions per set. | A total of 0–60% of the subject’s maximum expiratory pressure. |
| Citation | Oxygen Saturation | RR/HR/ I:E Ratio | VM /VC | Dyspnea | Spirometry/Pulmonary Function | Peak Flow Rate | Pimax/Pemax | Diffusion | Respiratory Muscle Strength | Walking Test | Quality of Life | Duration of Ventilation/Duration of Weaning | Chest Expansion (Manual Physical Examination) | Decreased Respiratory Comp. |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| McMahon, L., et al. (2021) [11] | X | X | X | X | X | X | ||||||||
| Wu F, Liu Y, et al. (2020) [12] | X | X | X | X | X | x | ||||||||
| Ying Yang, et al. (2020) [13] | X | X | ||||||||||||
| Chorattas A; et al. (2020)” [14] | X | x | X | X | X | X | X | |||||||
| GM Monsur Habib; et al. (2020) [15] | X | X | X | |||||||||||
| Michael Hindelang, et al. (2020) [16] | X | X | ||||||||||||
| Dunja Kokotovic, et al. (2020) [17] | x | |||||||||||||
| Xintong Zhang, et al. (2020) [18] | x | x | X | X | X | X | X | X | ||||||
| Rosa Silva JP, et al. (2020) [19] | X | X | X | X | X | |||||||||
| van de Wetering-van Dongen, et al. (2020) [20] | X | X | X | X | X | X | X | X | ||||||
| Machado A, et al. (2020) [21] | X | X | X | X | X | |||||||||
| Desjardins, et al. (2020) [22] | X | X | X | X | X | |||||||||
| Azambuja, et al. (2020) [23] | X | X | X | X | X | X | X | X | ||||||
| Bolger JC, et al. (2019) [24] | X | X | X | X | X | X | ||||||||
| Yu X, Li X, et al. (2019) [25] | X | X | X | |||||||||||
| Wang YQ, et al. (2019) [26] | X | X | X | X | X | X | X | |||||||
| Katz, S., et al. (2018) [27] | X | X | X | X | ||||||||||
| Sadek Z, et al. (2018) [23] | X | X | X | X | X | |||||||||
| Eun Nam Lee, Moon Ja Kim (2018) [59] | X | X | X | X | ||||||||||
| Vorona S, et al. (2018) [29] | X | X | x | X | ||||||||||
| Torres-Sánchez I, et al.(2017) [30] | X | X | X | |||||||||||
| Narayanan AL, et al. (2016) [31] | ||||||||||||||
| Volpe MS, et al. (2016) [32] | X | X | X | |||||||||||
| Gomes Neto M, et al. (2016) [33] | X | X | X | X | X | X | X | X | ||||||
| Macpherson CE, Bassile CC (2016) [34] | X | X | X | X | X | X | X | X | ||||||
| Mohammed J, et al. (2016) [35] | X | X | ||||||||||||
| Elkins M, Dentice R. (2015) [36] | X | X | X | |||||||||||
| Martín-Valero et al. (2015) [37] | X | X | X | X | X | X | ||||||||
| Mans, C. M., Reeve, J. C., & Elkins, M. R. (2015) [38] | X | X | X | X | X | X | X | X | ||||||
| Montemezzo D, et al. (2014) [39] | X | X | X | X | X | X | ||||||||
| Neves LF, Reis MH, et al. (2014) [40] | X | X | X | X | X | |||||||||
| Snowdon D, Haines TP, Skinner EH. (2014) [41] | X | X | ||||||||||||
| Osterling K, et al. (2014) [42] | X | X | X | X | X | X | ||||||||
| Jácome, C; Marques, A. (2014) [43] | X | X | X | |||||||||||
| Martín-Valero, R., et al. (2014) [44] | X | X | X | X | X | X | ||||||||
| Singh F, Newton RU, et al. (2013) [45] | X | X | X | X | ||||||||||
| O’Doherty AF, et al. (2013) [46] | X | X | X | |||||||||||
| Silva IS, Fregonezi GA, et al.(2013) [47] | X | X | X | X | ||||||||||
| Smart NA, Giallauria F, Dieberg G. (2013) [48] | X | X | X | X | ||||||||||
| Prem V, Sahoo RC, Adhikari P. (2013) [49] | X | X | X | X | ||||||||||
| Grams ST, et al. (2012) [50] | X | X | X | |||||||||||
| Thomas MJ, et al. (2010) [51] | X | X | ||||||||||||
| Lewis LK, Williams MT, Olds T. (2007) [52] | X | X | X | X | X | X | X | X | X | X | ||||
| Crowe J, et al. (2005) [53] | X | X | X | X | X |
| Interventions | Included Systematic Reviews | Outcomes | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Oxygen Saturation | Dyspnea | I:E Ratio and FR | Spirometry | Peak Flow | Pimax and Pemax | Diffusion | Respiratory Muscle Strength | Walking Test | ||
| Inspiratory muscle training | McMahon, L. et al. (2021) [11] Wu, F. et al. (2020) [12] Van de Wetering-van Dongen et al. (2020) [20] Azambuja, A. et al. (2020). [23] Xintong Z et al. (2020) [18] Bolger, J.C. et al. (2019) [24] Sadek, Z. et al. (2018) [23] Eun Nam Lee, et al. (2018) [59] Gomes Neto M, et al. (2016). [33] Mans, C. M., et al. (2014) [38] Neves, L.F. et al. (2014) [40] Martín-Valero, R. et al. (2014) [44] Silva IS, et al. (2013) [47] Montemezzo D, et al. (2014) [39] Smart N.A. et al. (2013) [48] Crowe J, et al. (2005) [53] | |||||||||
| Breathing control (relaxed breathing, pursed-lip breathing, and diaphragmatic breathing exercises) | Lewis LK. et al. (2007) [52] Grams ST, et al. (2012) [50] Prem V. et al. (2013) [49] Wang YQ. et al. (2019) [26] Ying Yang, et al. (2020) [13] Chorattas A. et al. (2020) [14] | |||||||||
| Respiratory expansion exercise (deep breathing exercise) | Grams ST, et al. (2012) [50] Wang YQ. et al. (2019) [26] Chorattas A. et al. (2020) [14] | |||||||||
| Thoracic expansion exercises | Grams ST, et al. (2012) [50] Wang YQ. et al. (2019) [26] Chorattas A. et al. (2020) [14] | |||||||||
| Positioning to optimize ventilation | Katz, S., et al. (2018) [27] | |||||||||
| Outcomes | Impact | Nº of Participants (Studies) | Certainty of the Evidence (GRADE) |
|---|---|---|---|
| Inspiratory Muscle Training | |||
| Oxygen saturation | Effective improvement with small positive effects * | 2740 (10 reviews) | ⨁⨁⨁◯ MODERATE due to inconsistency (due to significant heterogeneity) |
| Dyspnea (several instruments were used to measure this outcome) | Effective improvement with moderate positive effects ** | 2740 (10 reviews) | ⨁⨁⨁⨁ HIGH |
| Respiratory rate | Effective improvement with small positive effects * | 371 (1 review) | ⨁⨁⨁⨁ HIGH |
| Inspiration:expiration ratio (I:E) | Effective improvement with small positive effects * | 371(1 review) | ⨁⨁⨁⨁ HIGH |
| Respiratory muscle strength | Effective improvement with moderate positive effects ** | 2541 (6 reviews) | ⨁⨁⨁⨁ HIGH |
| Maximum expiratory pressure (MEP)/ maximum inspiratory pressure (MIP) | Effective improvement with moderate positive effects ** | 2656 (8 reviews) | ⨁⨁⨁⨁ HIGH |
| Pulmonary function testing (several instruments were used to measure this outcome) | Effective improvement with moderate positive effects ** | 4414 (10 reviews) | ⨁⨁⨁⨁ HIGH |
| Peak expiratory flow | Effective improvement with moderate positive effects ** | 1619 (5 reviews) | ⨁⨁⨁⨁ HIGH |
| 6 min walking test (6 MWT) | Effective improvement with small positive effects * | 2709 (9 reviews) | ⨁⨁⨁◯ MODERATE due to inconsistency (due to significant heterogeneity) |
| Diffusion | Effective improvement with moderate positive effects ** | 1369 (3 reviews) | ⨁⨁⨁◯ MODERATE due to inconsistency (due to significant heterogeneity) |
| Quality of life | Effective improvement with small positive effects * | 958 (2 reviews) | ⨁⨁⨁⨁ HIGH |
| Postoperative outcomes (respiratory as primary endpoint) | Effective improvement with moderate positive effects ** | 708 (1 review) | ⨁⨁◯◯ LOW |
| Adverse events | Effective improvement with small positive effects * | 330 (1 review) | ⨁⨁⨁◯ MODERATE due to inconsistency (due to significant heterogeneity) |
| Inspiratory muscle training in critical care | |||
| Duration of postoperative mechanical ventilation | Effective improvement with small positive effects * | 330 (1 review) | ⨁⨁⨁◯ MODERATE due to inconsistency (due to significant heterogeneity) |
| Rapid shallow breathing index | Effective improvement with moderate positive effects ** | 105 (1 review) | ⨁⨁⨁⨁ HIGH |
| Maximum expiratory pressure (MEP)/ maximum inspiratory pressure (MIP) | Effective improvement with moderate positive effects ** | 1846 (3 reviews) | ⨁⨁⨁⨁ HIGH |
| Length of stay | Effective improvement with small positive effects* | 291 (1 review) | ⨁⨁⨁⨁ HIGH |
| Postoperative pulmonary complications | Effective improvement with moderate positive effects ** | 291 (1 review) | ⨁⨁⨁⨁ HIGH |
| Time to extubation | Effective improvement with moderate positive effects ** | 291 (1 review) | ⨁⨁⨁⨁ HIGH |
| Reduced duration of weaning from mechanical ventilation | Effective improvement with moderate positive effects ** | 1185 (1 review | ⨁⨁⨁⨁ HIGH |
| Ventilator weaning duration | Effective improvement with small positive effects * | 479 (2 reviews) | ⨁⨁⨁⨁ HIGH |
| Success rate in weaning IMV | Effective improvement with small positive effects * | 523 (2 reviews) | ⨁⨁⨁⨁ HIGH |
| Duration of mechanical ventilation | Effective improvement with small positive effects * | 305 (1 review) | ⨁⨁⨁⨁ HIGH |
| Reintubation | Effective improvement with small positive effects * | 117 (1 review) | ⨁⨁⨁⨁ HIGH |
| Breathing Control (relaxed breathing, pursed-lip breathing, and diaphragmatic breathing exercises) | |||
| Pulmonary function testing (several instruments were used to measure this outcome) | Effective improvement with moderate positive effects ** | 963 (6 reviews) | ⨁⨁⨁⨁ HIGH |
| Expiratory flow rate | Effective improvement with small positive effects * | 285 (6 reviews) | ⨁⨁⨁◯ MODERATE due to inconsistency (due to significant heterogeneity) |
| Respiratory muscle strength | Effective improvement with moderate positive effects ** | 132 (1 review) | ⨁⨁⨁⨁ HIGH |
| Dyspnea (several instruments were used to measure this outcome) | Effective improvement with moderate positive effects ** | 803 (2 reviews) | ⨁⨁⨁◯ MODERATE due to inconsistency (due to significant heterogeneity) |
| Respiratory rate | Effective improvement with moderate positive effects ** | 539 (2 reviews) | ⨁⨁⨁◯ MODERATE due to inconsistency (due to significant heterogeneity) |
| Abdominal excursion/diaphragm excursion | Effective improvement with moderate positive effects ** | 285 (1 review) | ⨁⨁⨁◯ MODERATE due to inconsistency (due to significant heterogeneity) |
| Oxygen saturation (Sat O2) (several instruments were used to measure this outcome) | Effective improvement with moderate positive effects ** | 285 (1 review) | ⨁⨁⨁◯ MODERATE due to inconsistency (due to significant heterogeneity) |
| Diffusion | Effective improvement with moderate positive effects ** | 254 (1 review) | ⨁⨁⨁◯ MODERATE due to inconsistency (due to significant heterogeneity) |
| Walk test (MWT) (several instruments were used to measure this outcome) | Effective improvement with moderate positive effects ** | 1961 (3 reviews) | ⨁⨁⨁◯ MODERATE due to inconsistency (due to significant heterogeneity) |
| Postoperative pulmonary complications (PPCs) | Effective improvement with moderate positive effects ** | 1402 (2 reviews) | ⨁⨁⨁⨁ HIGH |
| Respiratory expansion exercise (deep breathing exercise) | |||
| Pulmonary function testing (several instruments were used to measure this outcome) | Effective improvement with moderate positive effects ** | 1270 (2 reviews) | ⨁⨁⨁⨁ HIGH |
| Dyspnea | Effective improvement with moderate positive effects ** | 518 (1 review) | ⨁⨁⨁◯ MODERATE due to inconsistency (due to significant heterogeneity) |
| Respiratory muscle strength | Effective improvement with moderate positive effects ** | 132 (1 review) | ⨁⨁⨁⨁ HIGH |
| 6 min walk test (6 MWT) | Effective improvement with moderate positive effects ** | 1270 (1 review) | ⨁⨁⨁⨁ HIGH |
| Postoperative pulmonary complications (PPCs) | Effective improvement with moderate positive effects ** | 1402 (2 reviews) | ⨁⨁⨁⨁ HIGH |
| Thoracic expansion exercises | |||
| Pulmonary function testing (several instruments were used to measure this outcome) | Effective improvement with moderate positive effects ** | 1402 (2 reviews) | ⨁⨁⨁⨁ HIGH |
| Respiratory muscle strength | Effective improvement with moderate positive effects ** | 132 (1 review) | ⨁⨁⨁⨁ HIGH |
| 6 min walk test (6 MWT) | Effective improvement with moderate positive effects ** | 1270 (1 review) | ⨁⨁⨁⨁ HIGH |
| Postoperative pulmonary complications (PPCs) | Effective improvement with moderate positive effects ** | 1402 (2 reviews) | ⨁⨁⨁⨁ HIGH |
| Positioning to optimize ventilation | |||
| Pulmonary function testing (several instruments were used to measure this outcome) | Effective improvement with small positive effects * | 1 review (38 studies) | ⨁⨁◯◯ LOW |
| PEF | Effective improvement with small positive effects * | 1 review (13 studies) | ⨁⨁◯◯ LOW |
| FRC | Effective improvement with small positive effects * | 1 review (5 studies) | ⨁⨁◯◯ LOW |
| Total Lung Capacity | no evidence | 1 review (2 studies) | ⨁⨁◯◯ LOW |
| Residual Volume | no evidence | 1 review (2 studies) | ⨁⨁◯◯ LOW |
| Pimax/PE max | Effective improvement with small positive effects * | 1 review (6 studies) | ⨁⨁◯◯ LOW |
| DLCO (Diffusion capacity) | Effective improvement with small positive effects * | 1 review (7 studies) | ⨁⨁◯◯ LOW |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reis, N.; Gaspar, L.; Paiva, A.; Sousa, P.; Machado, N. Effectiveness of Nonpharmacological Interventions in the Field of Ventilation: An Umbrella Review. Int. J. Environ. Res. Public Health 2023, 20, 5239. https://doi.org/10.3390/ijerph20075239
Reis N, Gaspar L, Paiva A, Sousa P, Machado N. Effectiveness of Nonpharmacological Interventions in the Field of Ventilation: An Umbrella Review. International Journal of Environmental Research and Public Health. 2023; 20(7):5239. https://doi.org/10.3390/ijerph20075239
Chicago/Turabian StyleReis, Neuza, Luis Gaspar, Abel Paiva, Paula Sousa, and Natália Machado. 2023. "Effectiveness of Nonpharmacological Interventions in the Field of Ventilation: An Umbrella Review" International Journal of Environmental Research and Public Health 20, no. 7: 5239. https://doi.org/10.3390/ijerph20075239






