Caregiver Perceptions of Autism and Neurodevelopmental Disabilities in New Delhi, India
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Study Procedures
2.3. Ethical Approval
2.4. Analysis
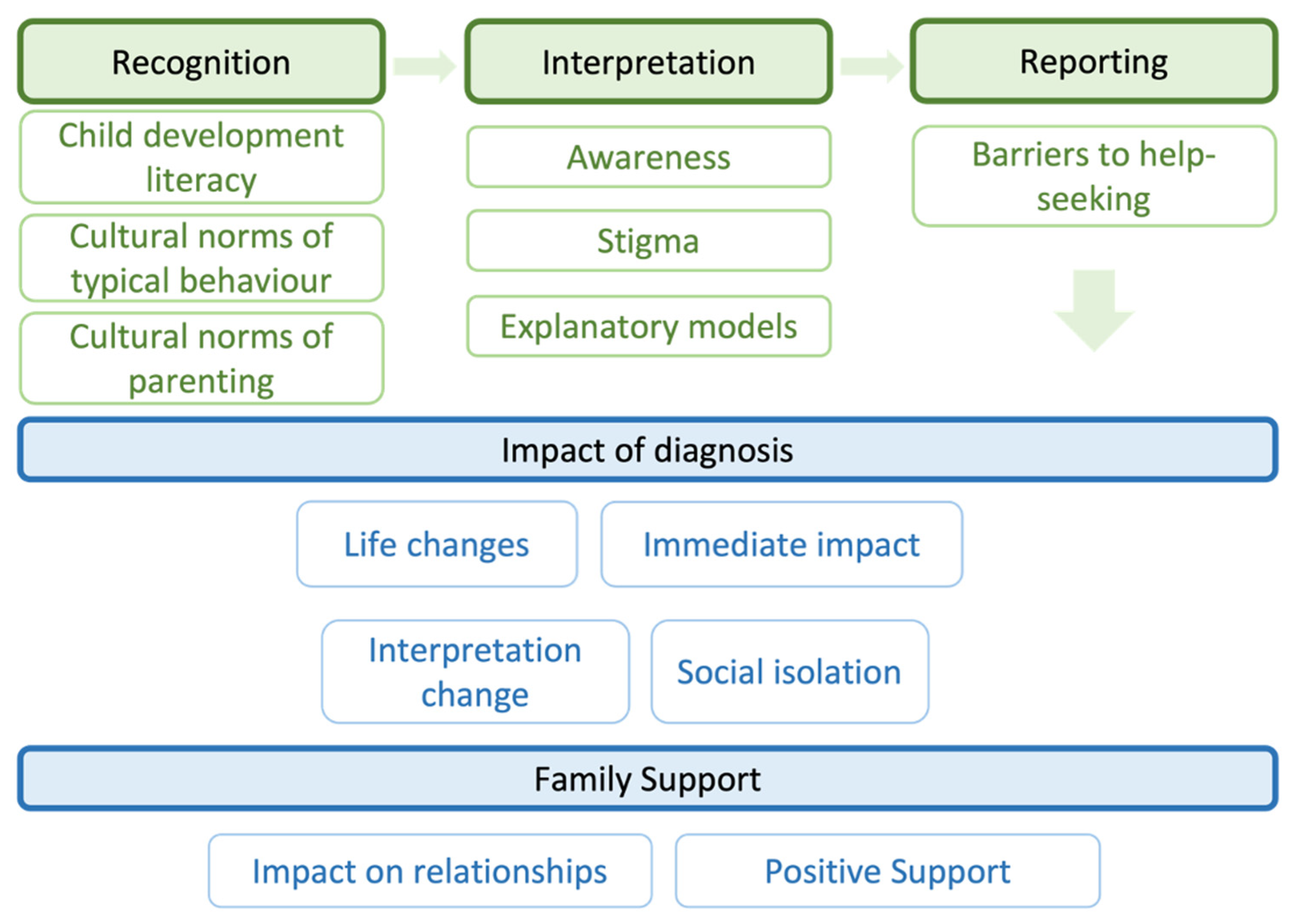
3. Results
3.1. Recognition
3.1.1. Child Development Literacy
“Parents are either uneducated or are unaware… They won’t be knowing that these things [autism, developmental delay] exist and so how would they know what is happening [with their child].”.(mother of a child meeting their developmental milestones)
“They [parents] would have realized late that our child is behaving in an unusual way. Else… [thinks]. This could be the only reason. Might be, they don’t pay much attention to the child. They would be thinking “it is normal.”.(mother of a child meeting their developmental milestones)
“We have seen this problem for the first time … we never heard that children have such problem.”.(mother of a child with an ASD diagnosis)
3.1.2. Cultural Norms of Typical Behaviour
“Such children are not like the normal children. They don’t do things as those are meant to be done.”.(mother of a child meeting their developmental milestones)
“No one can say by looking at him that he might have any problem.”.(mother of a child with an ASD diagnosis)
“Like other normal children, he is learning to speak. He is like a normal child.”.(child at 6 years, mother of a child with an ID diagnosis)
3.1.3. Cultural Norms of Parenting
“I talked to my housemaid in [name of the hometown state]. She told me to consult the doctor otherwise the problem will progress… I talked to her first….”.(mother of a child with an ID diagnosis)
3.2. Interpretation
3.2.1. Awareness
“His brain is like that of a young child… he would be 27–28 years old. He behaves like a child.”.(mother of a child meeting their developmental milestones)
“No one thought that it could be an autism symptom.”.(mother of child with ASD diagnosis)
“Normal kids can’t also do everything. Every kid has different abilities.”.(mother of a child with an ASD diagnosis)
3.2.2. Explanatory Models
“If a pregnant mother doesn’t eat specific medicine or dose [e.g., iron tablets etc], it leads to such or any other problems in child.”.(mother of a child meeting their developmental milestones)
“Society thinks they give birth to the child but are not taking care of them.”.(mother of a child meeting their developmental milestones)
“[The child] is unable to develop due to some weakness.”.(mother of a child with an ID diagnosis)
“The environment of the house also makes a difference. Joint family produces more growth, nuclear less.”.(mother of a child with an ASD diagnosis)
“I also didn’t pay regular attention. We can’t be with the child every time—sometimes when we are busy with our work,… It happens by being alone.”.(mother of a child with an ASD diagnosis)
“I was very stressed during pregnancy so my maternal aunt usually says, ‘You took stress during pregnancy which has affected the child.”.(mother of a child with an ASD diagnosis)
3.2.3. Stigma
“Some says, ‘you were proud [arrogant] of giving birth to an adorable boy [and so this happened]’.”.(mother of a child with an ASD diagnosis)
3.3. Reporting
“Some don’t have money or some don’t have time. It could be either of them.”.(mother of a child meeting their developmental milestones)
“It would be financial problem, what else… One can’t leave the child just like that. They will go. They will try. But if one doesn’t have money then till where they can go.”.(mother of a child meeting their developmental milestones)
“There could be some problem at home or we don’t get the reservation [for tickets]… We might be late if have any family problem otherwise we visit on the scheduled date of appointment.”.(mother of a child with an ID diagnosis)
“It seemed to me that there was some problem. But no one in the society listens to us ladies, no matters how much educated we are (sic).”.(mother of a child with an ASD diagnosis)
“I knew if I disclose it [child’s diagnosis]… then no one will allow my child and me to come in.”.(mother of a child with an ASD diagnosis)
3.4. Impact of Diagnosis
3.4.1. Immediate Impact of Diagnosis
“I didn’t make food for three days [when hearing of diagnosis] [Mother felt overwhelmed and almost cried]. He was young that time. I didn’t do anything except lying on bed and crying.”.(mother of a child with an ASD diagnosis)
“It hurts you deeply that your child is suffering so much. You feel sad.”.(mother of a child with an ID diagnosis)
3.4.2. Social Isolation
“You are not able to say anything to anyone. Society isolate(s) you. No one wants to talk to you.”.(mother of a child with an ASD diagnosis)
“No one will allow me in their home.”.(mother of a child with an ASD diagnosis)
3.4.3. Life Changes, including Financial
“I quit my job and spent time with her.”.(mother of a child with an ASD diagnosis)
“Such a child costs a lot.”.(mother of a child with an ASD diagnosis)
3.4.4. Change in Interpretation of Neurodevelopmental Disorder
“Now I understand it better than before… Earlier I used to think that either it will be or it won’t be. … Earlier these features [symptoms] were normal for me.”.(mother of a child with an ASD diagnosis)
3.5. Family Support
3.5.1. Impact on Relationships between Partner and Families
“Everyone loves her.”.(mother of a child with an ID diagnosis)
“No one discriminates.”.(mother of a child with an ID diagnosis)
“I had no support system from the family… I mean no one accepts, even your brothers and sisters.”.(mother of a child with an ASD diagnosis)
“In family.... lack acceptance. They didn’t accept. Even when I told my mother.”.(mother of a child with an ASD diagnosis)
3.5.2. Positive Support
“Someone who loves me truly is (child’s name) and at present I am very happy.”.(mother of a child with an ASD diagnosis)
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- American Psychiatric Association. DSM-5; American Psychiatric Association [APA]: Washington, DC, USA, 2013. [Google Scholar]
- Ilias, K.; Cornish, K.; Kummar, A.S.; Park, M.S.-A.; Golden, K.J. Parenting Stress and Resilience in Parents of Children With Autism Spectrum Disorder (ASD) in Southeast Asia: A Systematic Review. Front. Psychol. 2018, 9, 280. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Divan, G.; Vajaratkar, V.; Desai, M.U.; Strik-Lievers, L.; Patel, V. Challenges, Coping Strategies, and Unmet Needs of Families with a Child with Autism Spectrum Disorder in Goa, India: Impact of Autism on families in Goa, India. Autism Res. 2012, 5, 190–200. [Google Scholar] [CrossRef] [PubMed]
- Heys, M.; Alexander, A.; Medeiros, E.; Tumbahangphe, K.M.; Gibbons, F.; Shrestha, R.; Manandhar, M.; Wickenden, M.; Shrestha, M.; Costello, A.; et al. Understanding parents’ and professionals’ knowledge and awareness of autism in Nepal. Autism 2017, 21, 436–449. [Google Scholar] [CrossRef]
- Arora, N.K.; Nair, M.K.C.; Gulati, S.; Deshmukh, V.; Mohapatra, A.; Mishra, D.; Patel, V.; Pandey, R.M.; Das, B.C.; Divan, G.; et al. Neurodevelopmental disorders in children aged 2–9 years: Population-based burden estimates across five regions in India. PLoS Med. 2018, 15, e1002615. [Google Scholar] [CrossRef] [Green Version]
- Olusanya, B.O.; Davis, A.C.; Wertlieb, D.; Boo, N.-Y.; Nair, M.K.C.; Halpern, R.; Kuper, H.; Breinbauer, C.; De Vries, P.J.; Gladstone, M.; et al. Developmental disabilities among children younger than 5 years in 195 countries and territories, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Glob. Health 2018, 6, e1100–e1121. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- de Vries, P.J. Thinking globally to meet local needs: Autism spectrum disorders in Africa and other low-resource environments. Curr. Opin. Neurol. 2016, 29, 130–136. [Google Scholar] [CrossRef]
- Durkin, M.S.; Elsabbagh, M.; Barbaro, J.; Gladstone, M.; Happe, F.; Hoekstra, R.A.; Lee, L.; Rattazzi, A.; Stapel-Wax, J.; Stone, W.L.; et al. Autism screening and diagnosis in low resource settings: Challenges and opportunities to enhance research and services worldwide. Autism Res. 2015, 8, 473–476. [Google Scholar] [CrossRef] [Green Version]
- de Leeuw, A.; Happé, F.; Hoekstra, R.A. A Conceptual Framework for Understanding the Cultural and Contextual Factors on Autism Across the Globe. Autism Res. 2020, 13, 1029–1050. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rice, C.E.; Lee, L.-C. Expanding the global reach of research in autism. Autism 2017, 21, 515–517. [Google Scholar] [CrossRef] [Green Version]
- Bhavnani, S.; Estrin, G.L.; Arora, R.; Kumar, D.; Kakra, M.; Vajaratkar, V.; Juneja, M.; Gulati, S.; Patel, V.; Green, J.; et al. “I was Confused … and Still am” Barriers Impacting the Help-Seeking Pathway for an Autism Diagnosis in Urban North India: A Mixed Methods Study. J. Autism Dev. Disord. 2022, 52, 1778–1788. [Google Scholar] [CrossRef]
- Perry, A. A Model of Stress in Families of Children with Developmental Disabilities: Clinical and Research Applications. J. Dev. Disabil. 2004, 11, 1–16. [Google Scholar]
- Patra, S.; Kar, S.K. Autism spectrum disorder in India: A scoping review. Int. Rev. Psychiatry 2021, 33, 81–112. [Google Scholar] [CrossRef] [PubMed]
- Hahler, E.-M.; Elsabbagh, M. Autism: A Global Perspective. Curr. Dev. Disord. Rep. 2015, 2, 58–64. [Google Scholar] [CrossRef] [Green Version]
- Lord, C.; Charman, T.; Havdahl, A.; Carbone, P.; Anagnostou, E.; Boyd, B.; Carr, T.; de Vries, P.J.; Dissanayake, C.; Divan, G.; et al. The Lancet Commission on the future of care and clinical research in autism. Lancet 2022, 399, 271–334. [Google Scholar] [CrossRef]
- Lockwood Estrin, G.; Mason, L.; Arora, R.; Bhavnani, S.; Dasgupta, J.; Gulati, S.; Gliga, T.; Johnson, M.H. Attention control in autism: Eye-tracking findings from pre-school children in a low- and middle-income country setting. Autism, 2023; Online ahead of print. [Google Scholar] [CrossRef]
- Estrin, G.L.; Bhavnani, S.; Goodwin, A.; Arora, R.; Divan, G.; Haartsen, R.; Mason, L.; Patel, V.; Johnson, M.H.; Jones, E.J. From the lab to the field: Acceptability of using electroencephalography with Indian preschool children. Wellcome Open. Res. 2022, 7, 99. [Google Scholar] [CrossRef]
- Alpern, G.D. Developmental Profile 3 (DP-3); Western Psychological Services: Los Angeles, CA, USA, 2007. [Google Scholar]
- Gulati, S.; Kaushik, J.S.; Saini, L.; Sondhi, V.; Madaan, P.; Arora, N.K.; Pandey, R.M.; Jauhari, P.; Manokaran, R.K.; Sapra, S.; et al. Development and validation of DSM-5 based diagnostic tool for children with Autism Spectrum Disorder. PLoS ONE 2019, 14, e0213242. [Google Scholar] [CrossRef]
- Dubey, I.; Bishain, R.; Dasgupta, J.; Bhavnani, S.; Belmonte, M.K.; Gliga, T.; Mukherjee, D.; Estrin, G.L.; Johnson, M.H.; Chandran, S.; et al. Using mobile health technology to assess childhood autism in low-resource community settings in India: An innovation to address the detection gap. Psychiatry Clin. Psychol. 2021; preprint. [Google Scholar] [CrossRef]
- Mukherjee, S.B.; Malhotra, M.K.; Aneja, S.; Chakraborty, S.; Deshpande, S. Diagnostic accuracy of Indian Scale for Assessment of Autism (ISAA) in chidren aged 2–9 years. Indian Pediatr. 2015, 52, 212–216. [Google Scholar] [CrossRef]
- Juneja, M.; Inclen Study Group; Mishra, D.; Russell, P.S.S.; Gulati, S.; Deshmukh, V.; Tudu, P.; Sagar, R.; Silberberg, D.; Bhutani, V.K.; et al. INCLEN diagnostic tool for autism spectrum disorder (INDT-ASD): Development and validation. Indian Pediatr. 2014, 51, 359–365. [Google Scholar] [CrossRef]
- Vats, P.; Juneja, M.; Mishra, D. Diagnostic Accuracy of International Epidemiology Network (INCLEN) Diagnostic Tool for Autism Spectrum Disorder (INDT-ASD) in Comparison with Diagnostic and Statistical Manual of Mental Disorders-5 (DSM-5). Indian Pediatr. 2018, 55, 485–487. [Google Scholar] [CrossRef]
- Gale, N.K.; Heath, G.; Cameron, E.; Rashid, S.; Redwood, S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med. Res. Methodol. 2013, 13, 117. [Google Scholar] [CrossRef] [Green Version]
- Ritchie, J.; Spencer, L. Qualitative data analysis for applied policy research. In Analyzing Qualitative Data; Bryman, A., Burgess, R.G., Eds.; Taylor & Francis: Abingdon, UK, 1994; pp. 173–194. [Google Scholar] [CrossRef]
- Daley, T.C.; Sigman, M.D. Diagnostic conceptualization of autism among Indian psychiatrists, psychologists, and pediatricians. J. Autism Dev. Disord. 2002, 32, 13–23. [Google Scholar] [CrossRef]
- Minhas, A.; Vajaratkar, V.; Divan, G.; Hamdani, S.U.; Leadbitter, K.; Taylor, C.; Aldred, C.; Tariq, A.; Tariq, M.; Cardoza, P.; et al. Parents’ perspectives on care of children with autistic spectrum disorder in South Asia—Views from Pakistan and India. Int. Rev. Psychiatry 2015, 27, 247–256. [Google Scholar] [CrossRef] [PubMed]
- Milačić-Vidojević, I.; Gligorović, M.; Dragojević, N. Tendency towards stigmatization of families of a person with autistic spectrum disorders. Int. J. Soc. Psychiatry 2014, 60, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Obeid, R.; Daou, N.; DeNigris, D.; Shane-Simpson, C.; Brooks, P.J.; Gillespie-Lynch, K. A Cross-Cultural Comparison of Knowledge and Stigma Associated with Autism Spectrum Disorder among College Students in Lebanon and the United States. J. Autism. Dev. Disord. 2015, 45, 3520–3536. [Google Scholar] [CrossRef] [PubMed]
- Patra, S.; Kumar Patro, B. Affiliate stigma among parents of children with autism in eastern India. Asian J. Psychiatry 2019, 44, 45–47. [Google Scholar] [CrossRef]
- Desai, M.U.; Divan, G.; Wertz, F.J.; Patel, V. The discovery of autism: Indian parents’ experiences of caring for their child with an autism spectrum disorder. Transcult. Psychiatry 2012, 49, 613–637. [Google Scholar] [CrossRef] [Green Version]
- Brohan, E.; Slade, M.; Clement, S.; Thornicroft, G. Experiences of mental illness stigma, prejudice and discrimination: A review of measures. BMC Health Serv. Res. 2010, 10, 80. [Google Scholar] [CrossRef] [Green Version]
- Gaebel, W.; Rössler, W.; Sartorius, N. (Eds.) The Stigma of Mental Illness—End of the Story? Springer International Publishing: Cham, Switzerland, 2017. [Google Scholar] [CrossRef]
- Thornicroft, G.; Mehta, N.; Clement, S.; Evans-Lacko, S.; Doherty, M.; Rose, D.; Koschorke, M.; Shidhaye, R.; O’Reilly, C.; Henderson, C. Evidence for effective interventions to reduce mental-health-related stigma and discrimination. Lancet 2016, 387, 1123–1132. [Google Scholar] [CrossRef]
- Tilahun, D.; Fekadu, A.; Tekola, B.; Araya, M.; Roth, I.; Davey, B.; Hanlon, C.; Hoekstra, R.A. Ethiopian community health workers’ beliefs and attitudes towards children with autism: Impact of a brief training intervention. Autism 2019, 23, 39–49. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kleinman, A. Culture, Illness, and Care: Clinical Lessons from Anthropologic and Cross-Cultural Research. Ann. Intern. Med. 1978, 88, 251. [Google Scholar] [CrossRef] [PubMed]
- Gray, D.E. Lay conceptions of autism: Parents’ explanatory models. Med. Anthropol. 1994, 16, 99–118. [Google Scholar] [CrossRef] [PubMed]
- Gona, J.K.; Newton, C.R.; Rimba, K.; Mapenzi, R.; Kihara, M.; Van de Vijver, F.J.R.; Abubakar, A. Parents’ and Professionals’ Perceptions on Causes and Treatment Options for Autism Spectrum Disorders (ASD) in a Multicultural Context on the Kenyan Coast. PLoS ONE 2015, 10, e0132729. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hussein, A.M.; Pellicano, E.; Crane, L. Understanding and awareness of autism among Somali parents living in the United Kingdom. Autism 2019, 23, 1408–1418. [Google Scholar] [CrossRef] [PubMed]
- Wolff, E.R.; Madlon-Kay, D.J. Childhood Vaccine Beliefs Reported by Somali and Non-Somali Parents. J. Am. Board Fam. Med. 2014, 27, 458–464. [Google Scholar] [CrossRef] [Green Version]
- Zhou, T.; Wang, Y.; Yi, C. Affiliate stigma and depression in caregivers of children with Autism Spectrum Disorders in China: Effects of self-esteem, shame and family functioning. Psychiatry Res. 2018, 264, 260–265. [Google Scholar] [CrossRef]
- Jain, A.; Ahmed, N.; Mahour, P.; Agarwal, V.; Chandra, K.; Shrivatav, N. Burden of care perceived by the principal caregivers of autistic children and adolescents visiting health facilities in Lucknow City. Indian J. Public. Health 2019, 63, 282. [Google Scholar] [CrossRef]
- Khan, T.M.; Ooi, K.; Ong, Y.S.; Jacob, S.A. A meta-synthesis on parenting a child with autism. Neuropsychiatr. Dis. Treat. 2016, 12, 745–762. [Google Scholar] [CrossRef] [Green Version]
- Isman, E.; Ekéus, C.; Berggren, V. Perceptions and experiences of female genital mutilation after immigration to Sweden: An explorative study. Sex. Reprod. Healthc. 2013, 4, 93–98. [Google Scholar] [CrossRef]
| Demographics | Autism Group (n = 5) | Comparison Groups | |||
|---|---|---|---|---|---|
| Child Meeting Their Developmental Milestones (n = 4) | Child with Neurodevelopmental Condition (ID) (n = 4) | ||||
| Child characteristics | Child age (years) | Median (range) | 3.89 (3.57–6.18) | 4.97 (3.05–6.30) | 6.54 (3.47–6.71) |
| Sex | No. Female (Male) | 3 (2) | 3 (1) | 2 (2) | |
| Child development (DP-3, general developmental score) | Median (range) | 53 (<40–71) | 98.5 (91–15) | <40 (<40–62) | |
| ASD traits (INDT total score) | Median (range) | 6 (4–9) | 0 (0) | 1 (0–2) | |
| Social Communication Quotient score | Median (range) | 6 (5–16) | 2.5 (2–6) | 8.5 (3–14) | |
| Family Resources | Mother’s education | Secondary | 1 | 3 | 3 |
| Tertiary | 4 | 1 | 1 | ||
| Father’s education | Secondary | 0 | 4 | 1 | |
| Tertiary | 5 | 0 | 3 | ||
| Mother’s age (years) | Median (range) | 35 (28–36) * | 28 (27–29) * | 29.5 (25–38) | |
| Mother’s occupation | Not working | 3 | 1 | 4 | |
| Professional or skilled job | 2 | 1 | 0 | ||
| Unskilled job | 0 | 2 | 0 | ||
| Father’s occupation | Not working | 0 | 0 | 0 | |
| Professional or skilled job | 4 | 3 | 4 | ||
| Unskilled job | 1 | 1 | 0 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lockwood Estrin, G.; Bhavnani, S.; Arora, R.; Gulati, S.; Divan, G. Caregiver Perceptions of Autism and Neurodevelopmental Disabilities in New Delhi, India. Int. J. Environ. Res. Public Health 2023, 20, 5291. https://doi.org/10.3390/ijerph20075291
Lockwood Estrin G, Bhavnani S, Arora R, Gulati S, Divan G. Caregiver Perceptions of Autism and Neurodevelopmental Disabilities in New Delhi, India. International Journal of Environmental Research and Public Health. 2023; 20(7):5291. https://doi.org/10.3390/ijerph20075291
Chicago/Turabian StyleLockwood Estrin, Georgia, Supriya Bhavnani, Rashi Arora, Sheffali Gulati, and Gauri Divan. 2023. "Caregiver Perceptions of Autism and Neurodevelopmental Disabilities in New Delhi, India" International Journal of Environmental Research and Public Health 20, no. 7: 5291. https://doi.org/10.3390/ijerph20075291
APA StyleLockwood Estrin, G., Bhavnani, S., Arora, R., Gulati, S., & Divan, G. (2023). Caregiver Perceptions of Autism and Neurodevelopmental Disabilities in New Delhi, India. International Journal of Environmental Research and Public Health, 20(7), 5291. https://doi.org/10.3390/ijerph20075291






