Abstract
In China, HIV testing is the important first step of HIV prevention and treatment cascades but is not widely adopted by men who have sex with men (MSM). However, social media has been increasingly used to promote and improve HIV testing. This study aimed to assess the impact of social media use on HIV testing and explore the mediator in the relationship between social media and HIV testing. The authors conducted a cross-sectional study among 935 MSM participants in 11 cities in Shandong Province from 14 September to 6 December 2020. Multivariable regression was conducted to assess the relationship between social media use and HIV testing uptake, and mediation analysis was used to assess the mediation effect of HIV testing self-efficacy in the relationship between social media use and HIV testing. The present study findings showed that social media use was related to HIV testing (aOR = 3.024, 95% CI: 1.869, 4.892) and HIV self-testing uptake (aOR = 1.894, 95% CI: 1.228, 2.922), but was not related to HIV facility-based testing (aOR = 1.709, 95% CI: 0.806, 3.625, p = 0.162). A mediation effect of HIV testing self-efficacy was found between social media use and HIV testing (indirect effect: 0.13, 95% CI: 0.01, 0.29), facility-based testing (indirect effect: 0.05, 95% CI: 0.003, 0.16), and self-testing uptake (indirect effect: 0.07, 95% CI: 0.01, 0.16). Social media could be an effective tool to improve HIV testing, and healthcare providers should pay more attention to HIV testing self-efficacy in HIV testing promotion.
1. Introduction
The human immunodeficiency virus (HIV) epidemic is a global issue that affects all races, tribes, and social economic backgrounds. In 2020, there were roughly 1.5 million new HIV infections worldwide [1]. IDU (injection drug use) and MSM (men who have sex with men) seem to be the groups most affected by the HIV epidemic. However, in terms of the raw number of HIV cases, the MSM epidemic is by far the most severe. MSM represent a significant group for HIV infection and transmission, particularly in China, where the MSM had the fastest-rising HIV infection rates over the previous ten years [2]. In China, MSM accounted for 23.0% of new reported HIV infection cases in October 2019, which increased from 14.7% of new HIV cases in 2011 [3]. Due to multiple partners and high-risk sexual activities, MSM are 25 times more likely to be infected with HIV than the general population [4]. According to data from China’s HIV surveillance system, the prevalence of HIV among MSM has increased by about 8% over the last five years, and MSM have become a crucial population for HIV prevention and control [5].
HIV testing is anticipated to be a crucial step in HIV prevention and treatment cascade. The Joint United Nations Program on HIV/AIDS endorsed the 90-90-90 target in 2014 for bringing the HIV epidemic under worldwide control. The first 90 target, representing 90% of all persons living with HIV who know their HIV status, is the most difficult to meet, even in high-income countries. To reach this target, it is essential to increase HIV testing uptake and frequency among key populations such as MSM [6]. MSM should be tested for HIV at least once a year, according to the Centers for Disease Control and Prevention (CDC) recommendations, but ideally, every three to six months if they have had a new sexual partner since their last test [7]. However, only 47% of MSM in China have willingly visited HIV testing facilities [8,9]. HIV testing uptake is still low [10], and effective strategies should be taken to improve HIV testing uptake.
Furthermore, considering that many MSM use social networking platforms to find sex partners worldwide [11], healthcare practitioners increasingly rely on social media to create health promotion materials, disseminate information, and create peer-mentored education programs [12]. In addition, a Taiwanese study discovered that popular internet opinion leaders could help promote HIV testing among MSM through social media networks [13]. Similarly, England created an internet-based social marketing effort to encourage MSM to be tested for HIV [14]. Furthermore, previous studies in China also conducted programs to improve HIV testing uptake using social media among MSM [15,16,17]. However, a previous study highlighted concerns about the impact of social media use on HIV testing among MSM, who may be less likely to frequently test for HIV while also engaging in more unprotected behaviors [18].
Given that there are conflicting findings regarding the relationship between using social media and HIV testing, and that few studies in China have examined the potential mediator in this relationship, this study surveyed MSM in 11 cities in Shandong Province, China, to determine the effect of social media use on HIV testing and to investigate the mediator in this relationship.
2. Materials and Methods
2.1. Participants and Recruitment
A cross-sectional study was conducted from 14 September to 6 December 2020, among MSM in 11 cities of Shandong Province, China. The eligibility criteria to participate were: (1) be 18 years old or older, (2) live in the study city, (3) have not been tested for HIV in the past three months, (4) not be living with HIV or have never been tested for HIV, and (5) be willing to provide informed consent.
Participants were recruited online through Blued, a banner advertisement considered the biggest gay dating application in China, and recruited by the staff of community-based organizations (CBOs) in each study city. Eligible participants were encouraged to invite no more than 5 MSM from their social network. An online questionnaire was developed using software called Sojump, and all participants were emailed a link to the questionnaire via WeChat (a popular social contact application). Participants were informed of the study’s terms and conditions, including privacy and confidentiality. All participants who filled out the questionnaire could get an allowance of 8 USD.
2.2. Measurements
The socio-demographic characteristics of participants were assessed, including age, time of living in the study city, marital status, monthly income, educational degree, sexual orientation, disclosure of sexual orientation to others (including family members, friends, sexual partners or other people except for doctors), and disclosure of sexual orientation to doctors. Behavioral variables consisted of condomless sex and a self-reported history of HIV testing (including both facility-based and self-testing). Likert scales were used to evaluate psychological traits such as HIV testing self-efficacy, social norms around HIV testing, and stigma associated with HIV. Participants were also questioned regarding the purpose of seeking information online and the platforms they usually used.
2.3. Statistical Analysis
Descriptive analysis was performed to assess the participant characteristics, the specific purpose of searching for information about HIV testing online, and the platforms used. To identify the covariates when evaluating the relationships between social media use and HIV testing uptake, including HIV facility-based testing and self-testing, the correlations were examined between demographic characteristics, sexual behaviors, social media use, and HIV testing uptake in the participants’ lifetimes. The variables related to social media use and HIV testing were included as covariates in logistic regression.
To assess the mediation effect of HIV testing self-efficacy in the relationship between social media use and HIV testing, we conducted a mediation analysis using PROCESS in SPSS 26.0. The estimate of the mediated effect and 95% confidence interval (CI) were reported. The mediated effect was defined as statistically significant when the 95% CI did not contain zero. For stratified analysis, we evaluated the effect of social media use on different types of HIV testing, including facility-based testing and self-testing. A two-sided significance level of alpha = 0.05 was used for all analyses in SPSS software, version 26.0.
3. Results
3.1. Participants and Social Media Use
A total of 935 participants were enrolled in this study. Most participants were younger than 30 years old (64.3%), never married (72.8%), and had a college degree or higher (67.3%). Most participants ever searched for information on HIV testing through the Internet (89.2%) and tested for HIV (84.0) in their lifetime (Table 1).

Table 1.
Characteristics of participants.
The main purpose of searching through the Internet was to search the information and knowledge about HIV testing (68.3%), followed by searching the locations of HIV testing facilities and discussing HIV testing with others (Table 2). The common platforms participants used to search for information were Baidu and Sogou. Moreover, they used social media, particularly MSM-focused websites, the Centers for Disease Control and Prevention’s official website, application websites, and Q&A websites (Table 3).

Table 2.
The purpose of searching through the Internet.

Table 3.
The platforms used to search for information about HIV testing.
3.2. Relationship between Social Media Use and HIV Testing Uptake
Social media use was found to be correlated with marital status, educational level, reported sexual behavior with men to doctors, condom-free sexual behavior, and HIV testing self-efficacy (p < 0.05). HIV testing uptake was associated with age, income, sexual orientation, disclosed sexual behaviors with men to others and doctors, condomless sexual behaviors, HIV testing self-efficacy, and social media use (p < 0.05). Thus, disclosed sexual behaviors with men to doctors, condomless sexual behaviors, and HIV testing self-efficacy were identified as covariates when exploring the effect of social media use on HIV testing uptake (Figure 1).
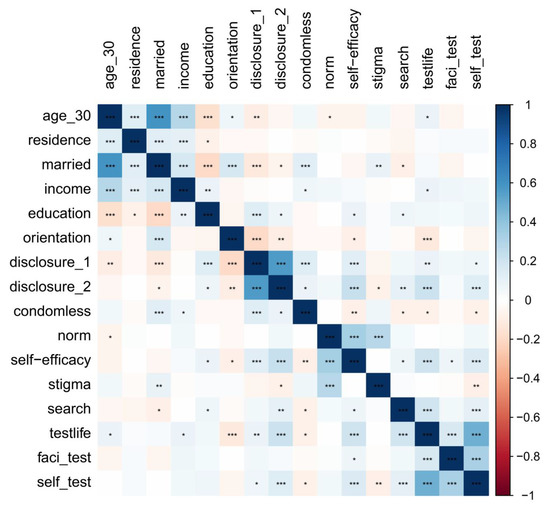
Figure 1.
Correlation between demographic characteristics, sexual behaviours, social media use, and HIV testing uptake. Note. ***, p < 0.001; **, p < 0.01; *, p < 0.05.
Table 4 shows the results of the multivariate regression analysis after adjusting the covariates. Participants who searched for information on HIV testing through the Internet were more likely to test for HIV (aOR = 3.024, 95% CI: 1.869, 4.892, p < 0.001). In stratified analysis across the type of HIV testing, searching for information on HIV testing through the Internet was related to HIV self-testing uptake (aOR = 1.894, 95% CI: 1.228, 2.922, p = 0.004) but was not related to HIV facility-based testing (aOR = 1.709, 95% CI: 0.806, 3.625, p = 0.162).

Table 4.
Factors related to HIV testing in their lifetime among MSM.
3.3. The Mediator in the Relationship between Social Media Use and HIV Testing Uptake
Figure 2 shows the path of the mediated effect of HIV testing self-efficacy in the relationship between social media use and HIV testing (including HIV facility-based testing and self-testing), only HIV facility-based testing, and only HIV self-testing. Table 5 presents the estimates and 95% CIs for the “a” path, “b” path, and the mediated effects of HIV testing self-efficacy in these relationships. In the relationship between social media use and HIV testing uptake, the mediated effect of HIV testing self-efficacy was statistically significant (indirect effect: 0.13, 95% CI: 0.01,0.29). The mediated effect of HIV testing self-efficacy was also statistically significant in the relationships between social media use and HIV self-testing (indirect effect: 0.05, 95% CI: 0.003,0.16), and between social media use and HIV facility-based testing uptake (indirect effect: 0.07, 95% CI: 0.01,0.16).
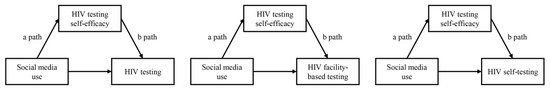
Figure 2.
The path of the mediated effect of HIV testing self-efficacy in the relationship between social media use and HIV testing.

Table 5.
Mediation effect of HIV self-efficacy between the relationship between social media use and HIV testing.
4. Discussion
This cross-sectional study surveyed MSM in 11 cities in Shandong Province, China, to assess the impact of social media use on HIV testing and explore the mediator in the relationship between social media and HIV testing. In summary, social media use positively impacts HIV testing, and HIV testing self-efficacy has a mediated effect on this relationship. This research provides insights on HIV testing promotion through social media among MSM.
This result joins the previous studies conducted in different cities in China, which also found an association between social media use and HIV testing uptake, and found that social media acts as a useful tool to promote HIV testing [17,19]. A nationwide cross-sectional survey in China showed that social media use, particularly on multifunctional platforms and with contributing behaviors, is correlated with HIV testing among MSM [17]. Another cluster randomized controlled trial demonstrated that interventions delivered through social media could increase the HIV testing uptake among MSM in China [19]. Social media was demonstrated to be a useful tool in increasing knowledge about HIV testing and improving the perception of the risk of HIV infection, and then promoting the uptake of HIV testing among MSM. Compared with traditional methods, social media, and dating applications could reach more MSM due to their convenience and privacy protection. Therefore, social media should be used more for health promotion. These results are also applicable to other high-risk populations. In addition, this present study also indicated that the main purpose of searching using social media was to search for information and knowledge about HIV testing, and the main platforms used were Baidu and Sougou, inconsistent with a previous study, which demonstrated that social media could be used to push pop-up advertisements about HIV testing [20]. Given that a previous study also indicated that internet technologies are becoming more prevalent and that they might increase sexual risk behaviors, particularly among high-risk groups [21], it was suggested that healthcare providers should publish more authoritative knowledge on HIV testing, and at the same time, the intensive supervision of the knowledge on HIV testing online should be strengthened, especially on popular search engines among MSM. In order to better meet the needs of MSM for information about HIV testing, official healthcare institutions could provide HIV testing counselling services through social media platforms, such as an official website or WeChat official account, which makes it possible for MSM to obtain information without disclosing their sexual orientation or privacy.
Few studies have explored the mediator in the relationship between social media use and HIV testing. This study found that HIV testing self-efficacy was a mediator in the relationship between social media use and HIV testing (HIV self-testing and HIV facility-based testing), which implied that HIV testing self-efficacy might be a crucial factor in increasing HIV testing. HIV testing self-efficacy refers to a person’s expectation of being able to conduct HIV testing [22]. According to Bandura’s theory, the higher the individual’s self-efficacy, the higher the possibility of completing a certain behavior [23]. Previous studies also pointed out that HIV testing self-efficacy is an important psychological factor in promoting HIV testing [24]. These findings provide a guide for healthcare providers in HIV testing promotion using social media. Information to improve HIV testing self-efficacy should be given more attention on social media, including publishing others’ experiences with HIV testing, a peer-leader call for having a test on social networks, and publishing instructions for an HIV self-testing kit.
This study also found an association between disclosed orientation to the doctors and HIV testing. Referrals for MSM who disclosed their sexual orientation to their healthcare provider might get more recommendations for HIV testing than those who did not disclose. A previous survey conducted in China also indicated that men who disclosed to healthcare professionals were more likely to test for HIV compared to men who disclosed to family members [25]. In this study, 64.8% of participants disclosed their orientation to others, and 37.0% did not disclose it to doctors. A systematic review evaluated that the disclosure rates varied across subgroups and study settings, ranging from 16% to 90%, with a median of 61% [26]. It was suggested that the disclosure rate to doctors should be improved in China. Effective strategies should be implemented to encourage MSM to disclose same-sex behaviors and meet their specific medical needs, including providing appropriate training for healthcare providers and creating gay-friendly clinical settings [26].
This study is subject to several limitations. First, due to the cross-sectional design, this study can indicate the correlation but can not test the causality relationship. Second, most participants were recruited online using Blued and by the staff of CBOs. These conclusions therefore cannot be extended to MSM who do not utilize Blued or contact CBOs. Third, using the self-reported HIV testing status can lead to information bias. However, the anonymous questionnaire could reduce this bias to some extent.
5. Conclusions
Social media could be an effective tool to improve HIV testing, and healthcare providers should pay more attention to HIV testing self-efficacy in HIV testing promotion. Our findings will help plan the promotion of HIV testing and improve the HIV testing rate.
Author Contributions
D.A.S.M.: conceptualization, investigation, writing—original draft. Y.L.: conceptualization, investigation, writing—review and editing. L.F.: writing—review and editing. W.M.: conceptualization, writing—review and editing, project administration, and funding acquisition. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by grant 2017YFE0103800 from the National Key Research and Development Program of China, grant NIAID 1R01AI114310.
Institutional Review Board Statement
This study was approved by the Institutional Review Board at the School of Public Health, Shandong University (20190210).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
All data was included in the manuscript. You can contact the corresponding author for more information by writing.
Acknowledgments
We would like to thank all participants for their participation and the local CDCs in the study cities for their help with this study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Zhou, J.; Yang, L.; Ma, J.; Jiang, S.; Liu, Y.; Sun, Z. Factors associated with HIV testing among MSM in Guilin, China: Results from a cross-sectional study. Int. J. Public Health 2022, 67, 1604612. [Google Scholar] [CrossRef] [PubMed]
- HIV by Group. Centers for Disease Control and Prevention. 2022. Available online: https://www.cdc.gov/hiv/group/index.html (accessed on 12 January 2023).
- Liau, A.; Millett, G.; Marks, G. Meta-analytic examination of online sex-seeking and sexual risk behavior among men who have sex with men. Sex. Transm. Dis. 2006, 33, 576–584. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; Cui, Y.; Hu, Q.; Mubarik, S.; Yang, D.; Jiang, Y.; Yao, Y.; Yu, C. Long-term changes of HIV/AIDS incidence rate in China and the U.S. population from 1994 to 2019: A join-point and age-period-cohort analysis. Front. Public Health 2021, 9, 652868. [Google Scholar] [CrossRef] [PubMed]
- Shan, D.; Yu, M.H.; Yang, J.; Zhuang, M.H.; Ning, Z.; Liu, H.; Liu, L.; Han, M.J.; Zhang, D.P. Correlates of HIV infection among transgender women in two Chinese cities. Infect. Dis. Poverty 2018, 7, 123. [Google Scholar] [CrossRef] [PubMed]
- Shi, Y.; Qiu, J.; Yang, Q.; Chen, T.; Lu, Y.; Chen, S.; Fan, X.; Lin, Z.; Han, Z.; Lu, J.; et al. Increasing the HIV testing among MSM through HIV test result exchange mechanism: Study protocol for a cluster randomized controlled trial. BMC Infect. Dis. 2021, 21, 764. [Google Scholar] [CrossRef] [PubMed]
- Wray, T.B.; Chan, P.A.; Celio, M.A.; Pérez, A.E.; Adia, A.C.; Simpanen, E.M.; Woods, L.A.; Monti, P.M. HIV testing among men who have sex with men in the Northeastern United States. AIDS Behav. 2018, 22, 531–537. [Google Scholar] [CrossRef]
- Xu, J.J.; Han, M.J.; Jiang, Y.J.; Ding, H.B.; Li, X.; Han, X.X.; Lv, F.; Chen, Q.F.; Zhang, Z.N.; Cui, H.L.; et al. Prevention and control of HIV/AIDS in China: Lessons from the past three decades. Chin. Med. J. 2021, 134, 2799–2809. [Google Scholar] [CrossRef]
- Dong, W.Z.C.; Ge, L.; Li, D.; Wu, Z.; Rou, K. Implementation of intervention programs on AIDS-related sexual transmission in China. Chin J. Epidemiol. 2015, 36, 1337–1340. (In Chinese) [Google Scholar]
- Xu, W.; Zheng, Y.; Kaufman, M.R. Predictors of recent HIV testing among Chinese men who have sex with men: A barrier perspective. AIDS Patient Care STDs 2018, 32, 408–417. [Google Scholar] [CrossRef]
- Grov, C.; Breslow, A.S.; Newcomb, M.E.; Rosenberger, J.G.; Bauermeister, J.A. Gay and bisexual men’s use of the Internet: Research from the 1990s through 2013. J. Sex Res. 2014, 51, 390–409. [Google Scholar] [CrossRef]
- Tso, L.S.; Tang, W.; Li, H.; Yan, H.Y.; Tucker, J.D. Social media interventions to prevent HIV: A review of interventions and methodological considerations. Curr. Opin. Psychol. 2016, 9, 6–10. [Google Scholar] [CrossRef]
- Ko, N.Y.; Hsieh, C.H.; Wang, M.C.; Lee, C.; Chen, C.L.; Chung, A.C.; Hsu, S.T. Effects of Internet popular opinion leaders (iPOL) among Internet-using men who have sex with men. J. Med. Internet Res. 2013, 15, e40. [Google Scholar] [CrossRef]
- Hickson, F.; Tomlin, K.; Hargreaves, J.; Bonell, C.; Reid, D.; Weatherburn, P. Internet-based cohort study of HIV testing over 1 year among men who have sex with men living in England and exposed to a social marketing intervention promoting testing. Sex. Transm. Infect. 2015, 91, 24–30. [Google Scholar] [CrossRef]
- Wang, L.; Podson, D.; Chen, Z.; Lu, H.; Wang, V.; Shepard, C.; Williams, J.K.; Mi, G. Using social media to increase HIV testing among men who have sex with men-Beijing, China, 2013–2017. MMWR Morb. Mortal. Wkly. Rep. 2019, 68, 478–482. [Google Scholar] [CrossRef]
- Wong, N.S.; Tang, W.; Han, L.; Best, J.; Zhang, Y.; Huang, S.; Zheng, H.; Yang, B.; Wei, C.; Pan, S.W.; et al. MSM HIV testing following an online testing intervention in China. BMC Infect. Dis. 2017, 17, 437. [Google Scholar] [CrossRef]
- Cao, B.; Liu, C.; Durvasula, M.; Tang, W.; Pan, S.; Saffer, A.J.; Wei, C.; Tucker, J.D. Social media engagement and HIV testing among men who have sex with men in China: A nationwide cross-sectional survey. J. Med. Internet Res. 2017, 19, e251. [Google Scholar] [CrossRef]
- Sun, S.; Whiteley, L.; Brown, L.K. HIV testing among Chinese men who have sex with men: The roles of HIV knowledge, online social life, and sexual identity concerns. AIDS Behav. 2020, 24, 437–449. [Google Scholar] [CrossRef]
- Tang, W.; Wei, C.; Cao, B.; Wu, D.; Li, K.T.; Lu, H.; Ma, W.; Kang, D.; Li, H.; Liao, M.; et al. Crowdsourcing to expand HIV testing among men who have sex with men in China: A closed cohort stepped wedge cluster randomized controlled trial. PLoS Med. 2018, 15, e1002645. [Google Scholar] [CrossRef]
- Laranjo, L.; Arguel, A.; Neves, A.L.; Gallagher, A.M.; Kaplan, R.; Mortimer, N.; Mendes, G.A.; Lau, A.Y. The influence of social networking sites on health behavior change: A systematic review and meta-analysis. J. Am. Med. Inform. Assoc. JAMIA. 2015, 22, 243–256. [Google Scholar] [CrossRef]
- Pereira, H.; Esgalhado, G. Sexually Explicit Online Media Use and Sexual Behavior among Sexual Minority Men in Portugal. Behav. Sci. 2021, 11, 38. [Google Scholar] [CrossRef]
- Safiri, S. Knowledge, attitude, self-efficacy and estimation of frequency of condom use among Iranian students based on a crosswise model: More explanation is needed for the crosswise model. Int. J. Adolesc. Med. Health 2017, 29, 20160110. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Social Foundations of Thought and Action: A Social Cognitive Theory; Prentice-Hall: Upper Saddle River, NJ, USA, 1986. [Google Scholar]
- Zhao, P.; Liu, L.; Zhang, Y.; Cheng, H.; Cao, B.; Liu, C.; Wang, C.; Yang, B.; Wei, C.; Tucker, J.D.; et al. The interaction between HIV testing social norms and self-efficacy on HIV testing among Chinese men who have sex with men: Results from an online cross-sectional study. BMC Infect. Dis. 2018, 18, 541. [Google Scholar] [CrossRef] [PubMed]
- Cao, B.; Saffer, A.J.; Yang, C.; Chen, H.; Peng, K.; Pan, S.W.; Durvasula, M.; Liu, C.; Fu, H.; Ong, J.J.; et al. MSM Behavior Disclosure Networks and HIV Testing: An Egocentric Network Analysis Among MSM in China. AIDS Behav. 2019, 23, 1368–1374. [Google Scholar] [CrossRef] [PubMed]
- Qiao, S.; Zhou, G.; Li, X. Disclosure of Same-Sex Behaviors to Health-care Providers and Uptake of HIV Testing for Men Who Have Sex With Men: A Systematic Review. Am. J. Men’s Health 2018, 12, 1197–1214. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).