Center of Pressure Deviation during Posture Transition in Athletes with Chronic Ankle Instability
Abstract
1. Introduction
2. Participants and Methods
2.1. Participants
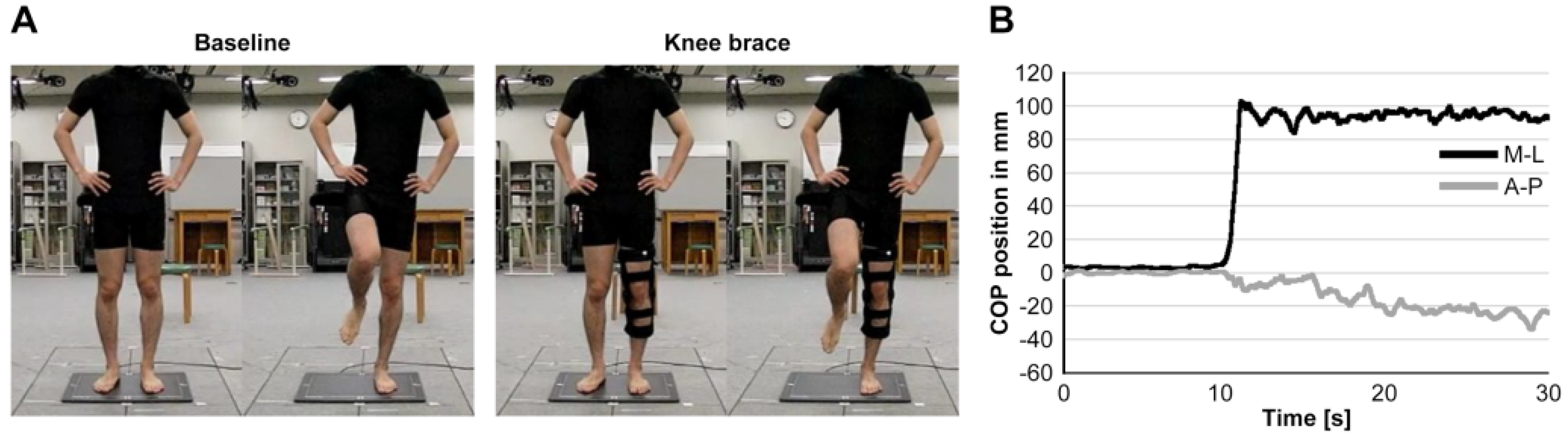
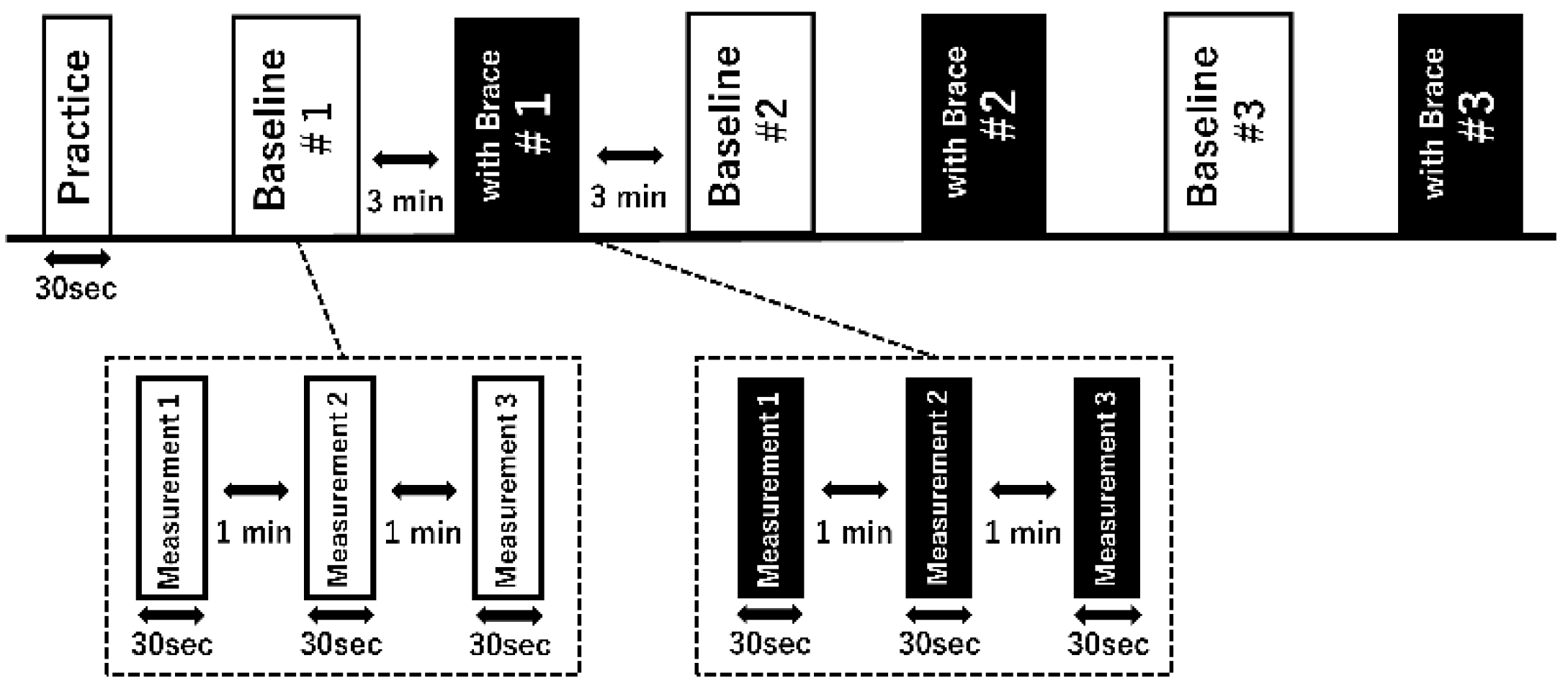
2.2. Procedure
2.3. Data Analysis
2.4. Statistics
3. Results
3.1. Correlation Analysis
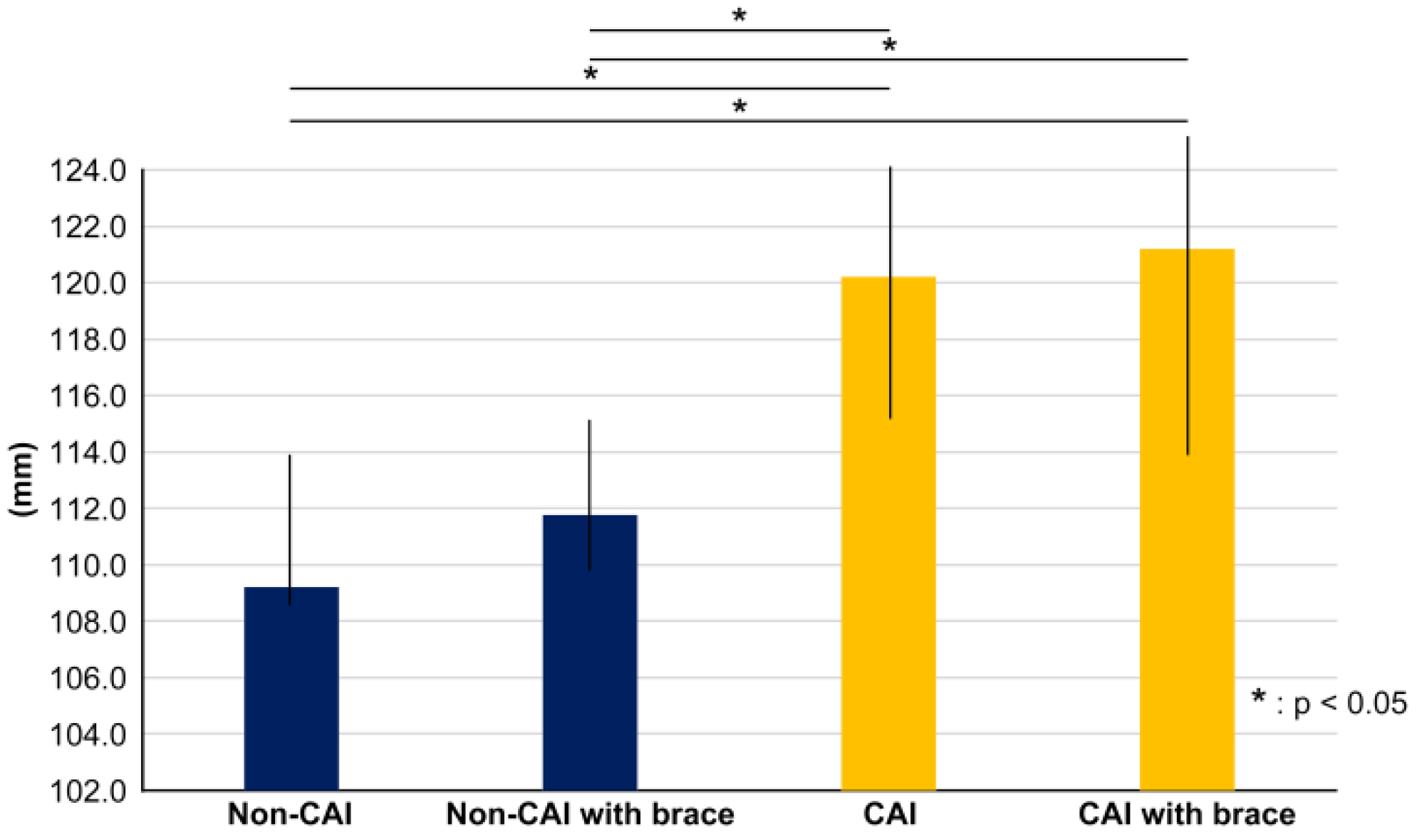
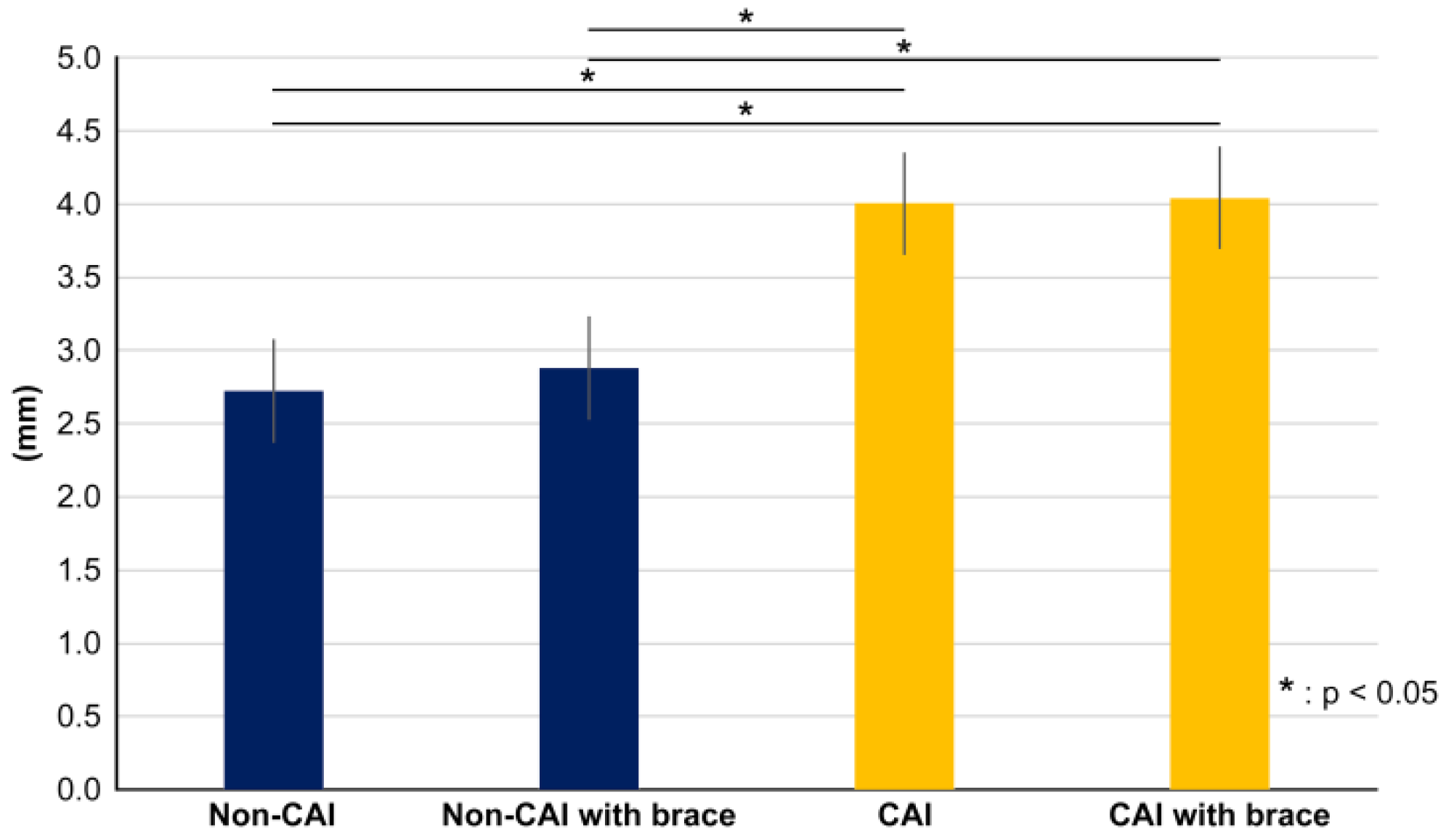
3.2. Movement Range (D) and Sway Range (N) of Center of Pressure
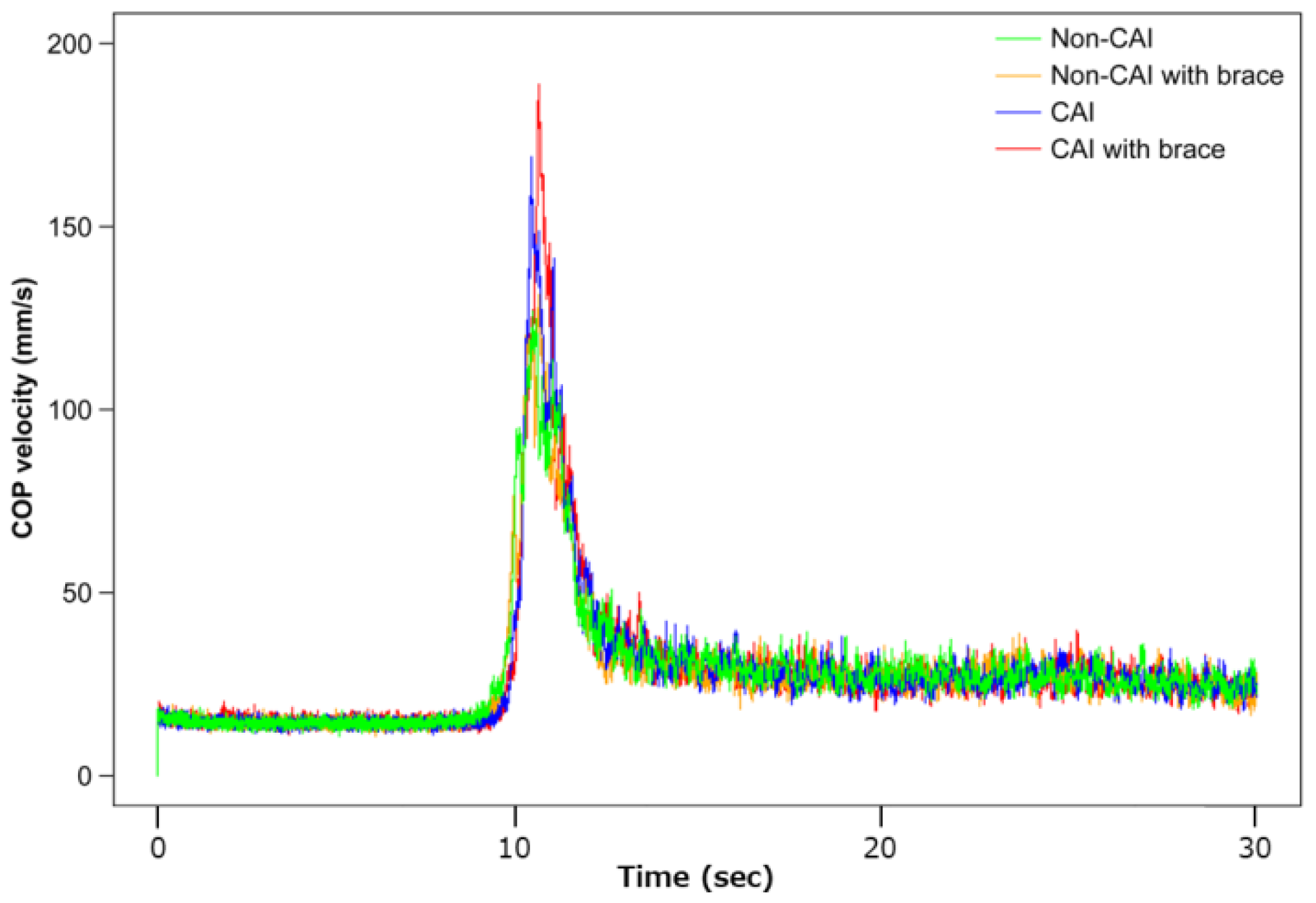
3.3. COP Acceleration during the Transition to SLS
3.4. Movement Index of Difficulty (ID) of Center of Pressure
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hootman, J.M.; Dick, R.; Agel, J. Epidemiology of collegiate injuries for 15 sports: Summary and recommendations for injury prevention initiatives. J. Athl. Train. 2007, 42, 311–319. [Google Scholar] [PubMed]
- Knowles, S.B.; Marshall, S.W.; Miller, T.; Spicer, R.; Bowling, J.M.; Loomis, D.; Millikan, R.W.; Yang, J.; Mueller, F.O. Cost of injuries from a prospective cohort study of North Carolina high school athletes. Inj. Prev. 2007, 13, 416–421. [Google Scholar] [CrossRef] [PubMed]
- Hubbard-Turner, T.; Turner, M.J. Physical activity levels in college students with chronic ankle instability. J. Athl. Train. 2015, 50, 742–747. [Google Scholar] [CrossRef] [PubMed]
- Doherty, C.; Bleakley, C.; Hertel, J.; Caulfield, B.; Ryan, J.; Delahunt, E. Recovery from a first-time lateral ankle sprain and the predictors of chronic ankle instability: A prospective cohort analysis. Am. J. Sports Med. 2016, 44, 995–1003. [Google Scholar] [CrossRef] [PubMed]
- Gribble, P.A.; Delahunt, E.; Bleakley, C.; Caulfield, B.; Docherty, C.L.; Fourchet, F.; Fong, D.; Hertel, J.; Hiller, C.; Kaminski, T.W.; et al. Selection criteria for patients with chronic ankle instability in controlled research: A position statement of the International Ankle Consortium. J. Orthop. Sport. Phys. Ther. 2013, 43, 585–591. [Google Scholar] [CrossRef]
- Thompson, C.; Schabrun, S.; Romero, R.; Bialocerkowski, A.; van Dieen, J.; Marshall, P. Factors contributing to chronic ankle instability: A systematic review and meta-analysis of systematic reviews. Sport. Med. 2018, 48, 189–205. [Google Scholar] [CrossRef]
- Evans, T.; Hertel, J.; Sebastianelli, W. Bilateral deficits in postural control following lateral ankle sprain. Foot Ankle Int. 2004, 25, 833–839. [Google Scholar] [CrossRef]
- Wang, H.K.; Chen, C.H.; Shiang, T.Y.; Jan, M.H.; Lin, K.H. Risk-factor analysis of high school basketball-player ankle injuries: A prospective controlled cohort study evaluating postural sway, ankle strength, and flexibility. Arch. Phys. Med. Rehabil. 2006, 87, 821–825. [Google Scholar] [CrossRef]
- Tropp, H.; Odenrick, P. Postural control in single-limb stance. J. Orthop. Res. 1988, 6, 833–839. [Google Scholar] [CrossRef]
- Abe, Y.; Sugaya, T.; Sakamoto, M. Postural control characteristics during single leg standing of individuals with a history of ankle sprain: Measurements obtained using a gravicorder and head and foot accelerometry. J. Phys. Ther. Sci. 2014, 26, 447–450. [Google Scholar] [CrossRef]
- Manchester, D.; Woollacott, M.; Zederbauer-Hylton, N.; Marin, O. Visual, vestibular and somatosensory contributions to balance control in the older adult. J. Gerontol. 1989, 44, M118–M127. [Google Scholar] [CrossRef] [PubMed]
- Sakanaka, T.E.; Lakie, M.; Reynolds, R.F. Individual differences in intrinsic ankle stiffness and their relationship to body sway and ankle torque. PLoS ONE 2021, 16, e0244993. [Google Scholar] [CrossRef]
- Noé, F.; Hachard, B.; Ceyte, H.; Bru, N.; Paillard, T. Relationship between the level of mental fatigue induced by a prolonged cognitive task and the degree of balance disturbance. Exp. Brain Res. 2021, 239, 2273–2283. [Google Scholar] [CrossRef] [PubMed]
- Kunugi, S.; Masunari, A.; Noh, B.; Mori, T.; Yoshida, N.; Miyakawa, S. Cross-cultural adaptation, reliability, and validity of the Japanese version of the Cumberland ankle instability tool. Disabil. Rehabil. 2017, 39, 50–58. [Google Scholar] [CrossRef]
- Low, D.C.; Dixon, S.J. Footscan pressure insoles: Accuracy and reliability of force and pressure measurements in running. Gait Posture 2010, 32, 664–666. [Google Scholar] [CrossRef] [PubMed]
- Błaszczyk, J.W.; Fredyk, A.; Błaszczyk, P.M.; Ashtiani, M. Step response of human motor system as a measure of postural stability in children. IEEE Trans. Neural Syst. Rehabil. Eng. 2020, 28, 895–903. [Google Scholar] [CrossRef]
- Sternad, D.; Abe, M.O.; Hu, X.; Müller, H. Neuromotor noise, error tolerance and velocity-dependent costs in skilled performance. PLoS Comput. Biol. 2011, 7, e1002159. [Google Scholar] [CrossRef]
- Yamamoto, A.; Sasagawa, S.; Oba, N.; Nakazawa, K. Behavioral effect of knee joint motion on body’s center of mass during human quiet standing. Gait Posture 2015, 41, 291–294. [Google Scholar] [CrossRef]
- Abe, Y.; Sakamoto, M.; Nakazawa, R.; Shirakura, K. Relationship between joint motion and acceleration during single-leg standing in healthy male adults. J. Phys. Ther. Sci. 2015, 27, 1251–1256. [Google Scholar] [CrossRef]
- Qian, Q.L.; Darwin, G.; Alpha, A.G. Postural Control and Adaptation Strategy of Young Adults on Unstable Surface. Motor Control 2022, 10, 179–193. [Google Scholar]
- McKeon, J.M.M.; McKeon, P.O. Evaluation of joint position recognition measurement variables associated with chronic ankle instability: A meta-analysis. J. Athl. Train. 2012, 47, 444–456. [Google Scholar] [CrossRef]
- Wright, C.J.; Arnold, B.L. Fatigue’s effect on eversion force sense in individuals with and without functional ankle instability. J. Sport Rehabil. 2012, 21, 127–136. [Google Scholar] [CrossRef] [PubMed]
- Hoch, M.C.; Mullineaux, D.R.; Andreatta, R.D.; English, R.A.; Medina-McKeon, J.M.; Mattacola, C.G.; McKeon, P.O. Effect of a 2-week joint mobilization intervention on single-limb balance and ankle arthrokinematics in those with chronic ankle instability. J. Sport Rehabil. 2014, 23, 18–26. [Google Scholar] [CrossRef] [PubMed]
- Tropp, H.; Ekstrand, J.; Gillquist, J. Stabilometry in functional instability of the ankle and its value in predicting injury. Med. Sci. Sport. Exerc. 1984, 16, 64–66. [Google Scholar] [CrossRef]


| CAI | Non-CAI | p-Value | |
|---|---|---|---|
| N (foot) | 10 | - | |
| Age (year) | 20.5 ± 0.5 | - | |
| Height (cm) | 180.1 ± 1.5 | - | |
| Body mass (kg) | 83.0 ± 1.0 | - | |
| Cumberland Ankle Instability Tool | 20.5 ± 0.5 | 28.0 ± 1.0 | <0.05 |
| Time since last ankle sprain (month) | 3.0 ± 0.5 | 18.0 ± 2.5 | <0.01 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kikumoto, T.; Suzuki, S.; Takabayashi, T.; Kubo, M. Center of Pressure Deviation during Posture Transition in Athletes with Chronic Ankle Instability. Int. J. Environ. Res. Public Health 2023, 20, 5506. https://doi.org/10.3390/ijerph20085506
Kikumoto T, Suzuki S, Takabayashi T, Kubo M. Center of Pressure Deviation during Posture Transition in Athletes with Chronic Ankle Instability. International Journal of Environmental Research and Public Health. 2023; 20(8):5506. https://doi.org/10.3390/ijerph20085506
Chicago/Turabian StyleKikumoto, Takanori, Shunsuke Suzuki, Tomoya Takabayashi, and Masayoshi Kubo. 2023. "Center of Pressure Deviation during Posture Transition in Athletes with Chronic Ankle Instability" International Journal of Environmental Research and Public Health 20, no. 8: 5506. https://doi.org/10.3390/ijerph20085506
APA StyleKikumoto, T., Suzuki, S., Takabayashi, T., & Kubo, M. (2023). Center of Pressure Deviation during Posture Transition in Athletes with Chronic Ankle Instability. International Journal of Environmental Research and Public Health, 20(8), 5506. https://doi.org/10.3390/ijerph20085506





