Diversity of Studies on Neighborhood Greenspace and Brain Health by Racialized/Ethnic Group and Geographic Region: A Rapid Review
Abstract
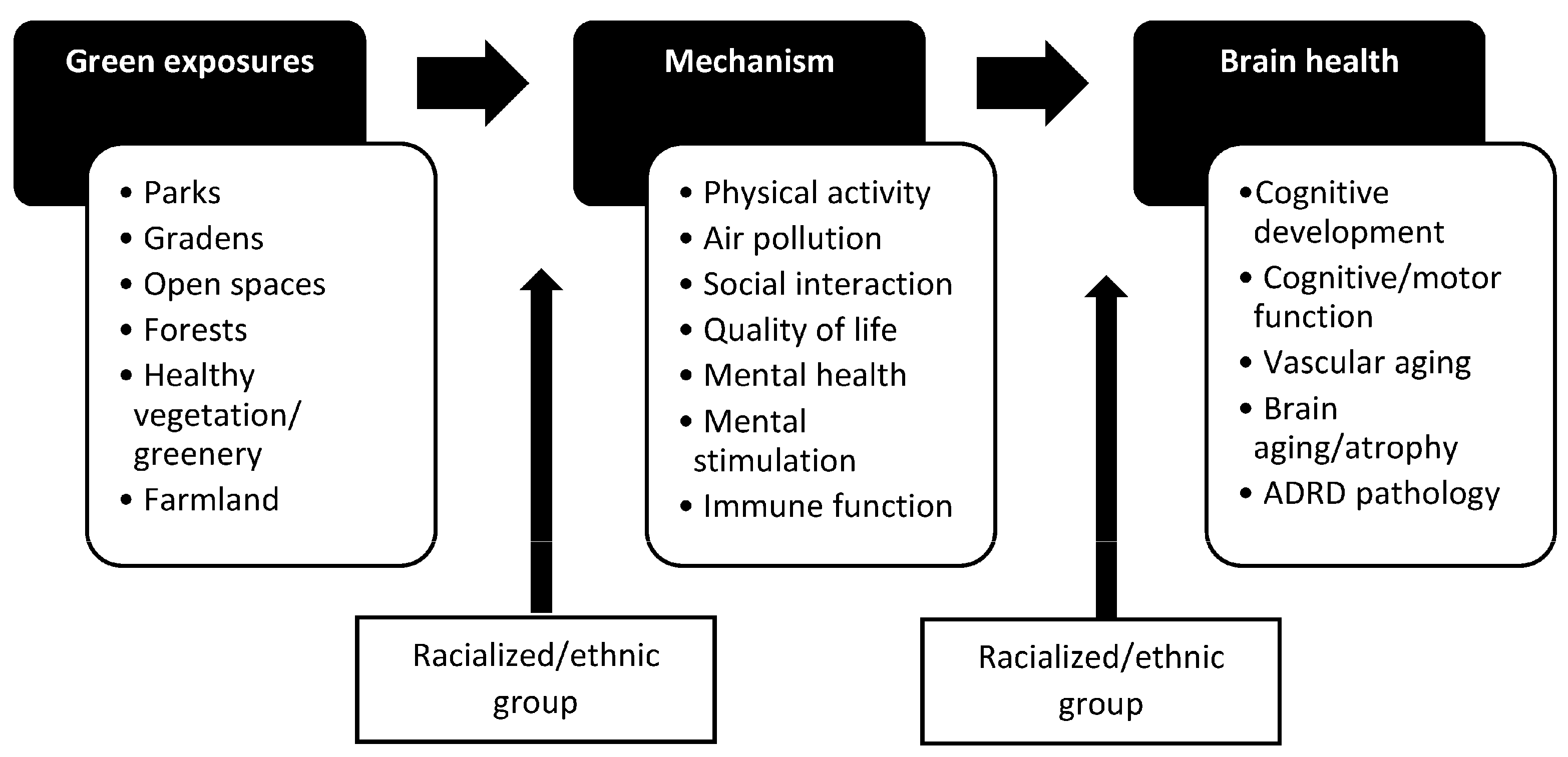
1. Introduction
2. Materials and Methods
- “greenspace or green space or greenness or parks or park or park space or parkspace” AND “cognition or cognitive or memory or brain aging or Alzheimer or Alzheimer’s or dementia or cognitive impairment”
- “neighborhood environment or wilderness or greenery or natural space or natural environment or public garden or recreational resource or normalized difference vegetation index or built environment or open space or woodland” AND “brain volume or brain atrophy or neurodegenerative disease or Alzheimer biomarker or cognition or cognitive or memory or brain aging or Alzheimer or Alzheimer’s or dementia or cognitive impairment”
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- McKhann, G.M.; Knopman, D.S.; Chertkow, H.; Hyman, B.T.; Jack, C.R., Jr.; Kawas, C.H.; Klunk, W.E.; Koroshetz, W.J.; Manly, J.J.; Mayeux, R.; et al. The diagnosis of dementia due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimer’s Dement. 2011, 7, 263–269. [Google Scholar] [CrossRef] [PubMed]
- Barton, B.; Grabli, D.; Bernard, B.; Czernecki, V.; Goldman, J.G.; Stebbins, G.; Dubois, B.; Goetz, C.G. Clinical validation of Movement Disorder Society-recommended diagnostic criteria for Parkinson’s disease with dementia. Mov. Disord. 2012, 27, 248–253. [Google Scholar] [CrossRef] [PubMed]
- Plassman, B.L.; Langa, K.M.; Fisher, G.G.; Heeringa, S.G.; Weir, D.R.; Ofstedal, M.B.; Burke, J.R.; Hurd, M.D.; Potter, G.G.; Rodgers, W.L.; et al. Prevalence of dementia in the United States: The aging, demographics, and memory study. Neuroepidemiology 2007, 29, 125–132. [Google Scholar] [CrossRef]
- Hebert, L.E.; Weuve, J.; Scherr, P.A.; Evans, D.A. Alzheimer disease in the United States (2010–2050) estimated using the 2010 census. Neurology 2013, 80, 1778–1783. [Google Scholar] [CrossRef]
- Frey, W. The US Will Become ‘Minority White’ in 2045, Census Projects. Available online: https://www.brookings.edu/blog/the-avenue/2018/03/14/the-us-will-become-minority-white-in-2045-census-projects/ (accessed on 18 October 2022).
- Hurd, M.D.; Martorell, P.; Langa, K.M. Monetary costs of dementia in the United States. N. Engl. J. Med. 2013, 369, 489–490. [Google Scholar] [CrossRef]
- Dilworth-Anderson, P.; Moon, H.; Aranda, M.P. Dementia Caregiving Research: Expanding and Reframing the Lens of Diversity, Inclusivity, and Intersectionality. Gerontologist 2020, 60, 797–805. [Google Scholar] [CrossRef] [PubMed]
- Matthews, K.A.; Xu, W.; Gaglioti, A.H.; Holt, J.B.; Croft, J.B.; Mack, D.; McGuire, L.C. Racial and ethnic estimates of Alzheimer’s disease and related dementias in the United States (2015–2060) in adults aged ≥65 years. Alzheimer’s Dement. 2019, 15, 17–24. [Google Scholar] [CrossRef]
- Alzheimer’s Association. 2019 Alzheimer’s Disease Facts and Figures. 2019. Available online: https://www.alz.org/media/Documents/alzheimers-facts-and-figures-2019-r.pdf (accessed on 24 June 2019).
- Weuve, J.; Barnes, L.L.; Mendes de Leon, C.F.; Rajan, K.B.; Beck, T.; Aggarwal, N.T.; Hebert, L.E.; Bennett, D.A.; Wilson, R.S.; Evans, D.A. Cognitive Aging in Black and White Americans: Cognition, Cognitive Decline, and Incidence of Alzheimer Disease Dementia. Epidemiology 2018, 29, 151–159. [Google Scholar] [CrossRef]
- Froehlich, T.E.; Bogardus, S.T., Jr.; Inouye, S.K. Dementia and race: Are there differences between African Americans and Caucasians? J. Am. Geriatr. Soc. 2001, 49, 477–484. [Google Scholar] [CrossRef]
- Hachinski, V.; Einhäupl, K.; Ganten, D.; Alladi, S.; Brayne, C.; Stephan, B.C.M.; Sweeney, M.D.; Zlokovic, B.; Iturria-Medina, Y.; Iadecola, C.; et al. Preventing dementia by preventing stroke: The Berlin Manifesto. Alzheimer’s Dement. 2019, 15, 961–984. [Google Scholar] [CrossRef]
- GBD 2019 Dementia Forecasting Collaborators. Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: An analysis for the Global Burden of Disease Study 2019. Lancet Public Health 2022, 7, e105–e125. [Google Scholar] [CrossRef] [PubMed]
- Alzheimer’s Association. 2022 Alzheimer’s Disease Facts and Figures. Available online: https://www.alz.org/media/Documents/alzheimers-facts-and-figures.pdf (accessed on 17 January 2023).
- Galvin, J.E.; Chrisphonte, S.; Chang, L.C. Medical and Social Determinants of Brain Health and Dementia in a Multicultural Community Cohort of Older Adults. J. Alzheimer’s Dis. 2021, 84, 1563–1576. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. About Social Determinants of Health (SDOH). Available online: https://www.cdc.gov/socialdeterminants/about.html (accessed on 18 October 2022).
- Walker, R.J.; Williams, J.S.; Egede, L.E. Influence of Race, Ethnicity and Social Determinants of Health on Diabetes Outcomes. Am. J. Med. Sci. 2016, 351, 366–373. [Google Scholar] [CrossRef]
- Forde, A.T.; Lewis, T.T.; Kershaw, K.N.; Bellamy, S.L.; Diez Roux, A.V. Perceived Discrimination and Hypertension Risk Among Participants in the Multi-Ethnic Study of Atherosclerosis. J. Am. Heart Assoc. 2021, 10, e019541. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Brain Health. Available online: https://www.who.int/health-topics/brain-health#tab=tab_1 (accessed on 18 October 2022).
- Livingston, G.; Huntley, J.; Sommerlad, A.; Ames, D.; Ballard, C.; Banerjee, S.; Brayne, C.; Burns, A.; Cohen-Mansfield, J.; Cooper, C.; et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet 2020, 396, 413–446. [Google Scholar] [CrossRef] [PubMed]
- Norton, S.; Matthews, F.E.; Barnes, D.E.; Yaffe, K.; Brayne, C. Potential for primary prevention of Alzheimer’s disease: An analysis of population-based data. Lancet Neurol. 2014, 13, 788–794. [Google Scholar] [CrossRef]
- Nianogo, R.A.; Rosenwohl-Mack, A.; Yaffe, K.; Carrasco, A.; Hoffmann, C.M.; Barnes, D.E. Risk Factors Associated With Alzheimer Disease and Related Dementias by Sex and Race and Ethnicity in the US. JAMA Neurol. 2022, 79, 584–591. [Google Scholar] [CrossRef]
- Krieger, N. Theories for social epidemiology in the 21st century: An ecosocial perspective. Int. J. Epidemiol. 2001, 30, 668–677. [Google Scholar] [CrossRef]
- Besser, L. Outdoor green space exposure and brain health measures related to Alzheimer’s disease: A rapid review. BMJ Open 2021, 11, e043456. [Google Scholar] [CrossRef]
- Zagnoli, F.; Filippini, T.; Jimenez, M.P.; Wise, L.A.; Hatch, E.E.; Vinceti, M. Is Greenness Associated with Dementia? A Systematic Review and Dose-Response Meta-analysis. Curr. Environ. Health Rep. 2022, 9, 574–590. [Google Scholar] [CrossRef]
- Cherrie, M.P.C.; Shortt, N.K.; Mitchell, R.J.; Taylor, A.M.; Redmond, P.; Thompson, C.W.; Starr, J.M.; Deary, I.J.; Pearce, J.R. Green space and cognitive ageing: A retrospective life course analysis in the Lothian Birth Cohort 1936. Soc. Sci. Med. 2018, 196, 56–65. [Google Scholar] [CrossRef]
- Besser, L.M.; Chang, L.C.; Evenson, K.R.; Hirsch, J.A.; Michael, Y.L.; Galvin, J.E.; Rapp, S.R.; Fitzpatrick, A.L.; Heckbert, S.R.; Kaufman, J.D.; et al. Associations between neighborhood park access and longitudinal change in cognition in older adults: The Multi-Ethnic Study of Atherosclerosis. J. Alzheimer’s Dis. 2021, 82, 221–233. [Google Scholar] [CrossRef] [PubMed]
- Jimenez, M.P.; Elliott, E.G.; DeVille, N.V.; Laden, F.; Hart, J.E.; Weuve, J.; Grodstein, F.; James, P. Residential Green Space and Cognitive Function in a Large Cohort of Middle-Aged Women. JAMA Netw. Open 2022, 5, e229306. [Google Scholar] [CrossRef] [PubMed]
- de Keijzer, C.; Tonne, C.; Basagaña, X.; Valentín, A.; Singh-Manoux, A.; Alonso, J.; Antó, J.M.; Nieuwenhuijsen, M.J.; Sunyer, J.; Dadvand, P. Residential Surrounding Greenness and Cognitive Decline: A 10-Year Follow-up of the Whitehall II Cohort. Environ. Health Perspect. 2018, 126, 077003. [Google Scholar] [CrossRef] [PubMed]
- Dadvand, P.; Pujol, J.; Macià, D.; Martínez-Vilavella, G.; Blanco-Hinojo, L.; Mortamais, M.; Alvarez-Pedrerol, M.; Fenoll, R.; Esnaola, M.; Dalmau-Bueno, A.; et al. The Association between Lifelong Greenspace Exposure and 3-Dimensional Brain Magnetic Resonance Imaging in Barcelona Schoolchildren. Environ. Health Perspect. 2018, 126, 027012. [Google Scholar] [CrossRef]
- Kühn, S.; Düzel, S.; Eibich, P.; Krekel, C.; Wüstemann, H.; Kolbe, J.; Martensson, J.; Goebel, J.; Gallinat, J.; Wagner, G.G.; et al. In search of features that constitute an “enriched environment” in humans: Associations between geographical properties and brain structure. Sci. Rep. 2017, 7, 11920. [Google Scholar] [CrossRef] [PubMed]
- De Keijzer, C.; Gascon, M.; Nieuwenhuijsen, M.J.; Dadvand, P. Long-Term Green Space Exposure and Cognition Across the Life Course: A Systematic Review. Curr. Environ. Health Rep. 2016, 3, 468–477. [Google Scholar] [CrossRef]
- Casey, J.A.; James, P.; Cushing, L.; Jesdale, B.M.; Morello-Frosch, R. Race, Ethnicity, Income Concentration and 10-Year Change in Urban Greenness in the United States. Int. J. Environ. Res. Public. Health 2017, 14, 1546. [Google Scholar] [CrossRef]
- Nardone, A.; Rudolph, K.E.; Morello-Frosch, R.; Casey, J.A. Redlines and Greenspace: The Relationship between Historical Redlining and 2010 Greenspace across the United States. Environ. Health Perspect. 2021, 129, 017006. [Google Scholar] [CrossRef]
- Locke, D.H.; Hall, B.; Grove, J.M.; Pickett, S.T.A.; Ogden, L.A.; Aoki, C.; Boone, C.G.; O’Neil-Dunne, J.P.M. Residential housing segregation and urban tree canopy in 37 US Cities. npj Urban Sustain. 2021, 1, 15. [Google Scholar] [CrossRef]
- Wen, M.; Zhang, X.; Harris, C.D.; Holt, J.B.; Croft, J.B. Spatial disparities in the distribution of parks and green spaces in the USA. Ann. Behav. Med. 2013, 45 (Suppl. S1), S18–S27. [Google Scholar] [CrossRef] [PubMed]
- Dai, D. Racial/ethnic and socioeconomic disparities in urban green space accessibility: Where to intervene? Landsc. Urban Plan. 2011, 102, 234–244. [Google Scholar] [CrossRef]
- Moore, L.V.; Diez Roux, A.V.; Evenson, K.R.; McGinn, A.P.; Brines, S.J. Availability of recreational resources in minority and low socioeconomic status areas. Am. J. Prev. Med. 2008, 34, 16–22. [Google Scholar] [CrossRef] [PubMed]
- Duncan, D.T.; Kawachi, I.; White, K.; Williams, D.R. The geography of recreational open space: Influence of neighborhood racial composition and neighborhood poverty. J. Urban Health 2013, 90, 618–631. [Google Scholar] [CrossRef]
- Boone, C.G.; Buckley, G.L.; Grove, J.M.; Sister, C. Parks and People: An Environmental Justice Inquiry in Baltimore, Maryland. Ann. Assoc. Am. Geogr. 2009, 99, 767–787. [Google Scholar] [CrossRef]
- Chen, B.; Wu, S.B.A.; Song, Y.M.; Webster, C.; Xu, B.; Gong, P. Contrasting inequality in human exposure to greenspace between cities of Global North and Global South. Nat. Commun. 2022, 13, 4636. [Google Scholar] [CrossRef]
- Temple University. What is a Rapid Review? Systematic Reviews and Other Review Types. Available online: https://guides.temple.edu/c.php?g=78618&p=4156608#:~:text=%22Rapid%20reviews%20are%20a%20form,in%20less%20than%205%20weeks (accessed on 18 October 2022).
- Giedd, J.N.; Blumenthal, J.; Jeffries, N.O.; Castellanos, F.X.; Liu, H.; Zijdenbos, A.; Paus, T.; Evans, A.C.; Rapoport, J.L. Brain development during childhood and adolescence: A longitudinal MRI study. Nat. Neurosci. 1999, 2, 861–863. [Google Scholar] [CrossRef]
- Tierney, A.L.; Nelson, C.A., 3rd. Brain Development and the Role of Experience in the Early Years. Zero Three 2009, 30, 9–13. [Google Scholar]
- Irwin, K.; Sexton, C.; Daniel, T.; Lawlor, B.; Naci, L. Healthy Aging and Dementia: Two Roads Diverging in Midlife? Front. Aging Neurosci. 2018, 10, 275. [Google Scholar] [CrossRef]
- United Nations. Statistical Annex: Country Classifications. Available online: https://www.un.org/development/desa/dpad/wp-content/uploads/sites/45/WESP2022_ANNEX.pdf (accessed on 21 February 2023).
- Brown, S.C.; Perrino, T.; Lombard, J.; Wang, K.; Toro, M.; Rundek, T.; Gutierrez, C.M.; Dong, C.; Plater-Zyberk, E.; Nardi, M.I.; et al. Health Disparities in the Relationship of Neighborhood Greenness to Mental Health Outcomes in 249,405 U.S. Medicare Beneficiaries. Int. J. Environ. Res. Public. Health 2018, 15, 430. [Google Scholar] [CrossRef]
- Cherrie, M.P.C.; Shortt, N.K.; Ward Thompson, C.; Deary, I.J.; Pearce, J.R. Association Between the Activity Space Exposure to Parks in Childhood and Adolescence and Cognitive Aging in Later Life. Int. J. Environ. Res. Public. Health 2019, 16, 632. [Google Scholar] [CrossRef] [PubMed]
- Clarke, P.J.; Ailshire, J.A.; House, J.S.; Morenoff, J.D.; King, K.; Melendez, R.; Langa, K.M. Cognitive function in the community setting: The neighbourhood as a source of ‘cognitive reserve’? J. Epidemiol. Community Health 2012, 66, 730–736. [Google Scholar] [CrossRef] [PubMed]
- Dadvand, P.; Nieuwenhuijsen, M.J.; Esnaola, M.; Forns, J.; Basagaña, X.; Alvarez-Pedrerol, M.; Rivas, I.; López-Vicente, M.; De Castro Pascual, M.; Su, J.; et al. Green spaces and cognitive development in primary schoolchildren. Proc. Natl. Acad. Sci. USA 2015, 112, 7937–7942. [Google Scholar] [CrossRef] [PubMed]
- Dadvand, P.; Tischer, C.; Estarlich, M.; Llop, S.; Dalmau-Bueno, A.; López-Vicente, M.; Valentín, A.; de Keijzer, C.; Fernández-Somoano, A.; Lertxundi, N.; et al. Lifelong Residential Exposure to Green Space and Attention: A Population-based Prospective Study. Environ. Health Perspect. 2017, 125, 097016. [Google Scholar] [CrossRef]
- Dzhambov, A.M.; Bahchevanov, K.M.; Chompalov, K.A.; Atanassova, P.A. A feasibility study on the association between residential greenness and neurocognitive function in middle-aged Bulgarians. Arh. Hig. Rada Toksikol. 2019, 70, 173–185. [Google Scholar] [CrossRef]
- Flouri, E.; Papachristou, E.; Midouhas, E. The role of neighbourhood greenspace in children’s spatial working memory. Brit. J. Educ. Psychol. 2019, 89, 359–373. [Google Scholar] [CrossRef]
- Hystad, P.; Payette, Y.; Noisel, N.; Boileau, C. Green space associations with mental health and cognitive function: Results from the Quebec CARTaGENE cohort. Environ. Epidemiol. 2019, 3, e040. [Google Scholar] [CrossRef]
- Liao, J.; Zhang, B.; Xia, W.; Cao, Z.; Zhang, Y.; Liang, S.; Hu, K.; Xu, S.; Li, Y. Residential exposure to green space and early childhood neurodevelopment. Environ. Int. 2019, 128, 70–76. [Google Scholar] [CrossRef]
- Reuben, A.; Arseneault, L.; Belsky, D.W.; Caspi, A.; Fisher, H.L.; Houts, R.M.; Moffitt, T.E.; Odgers, C. Residential neighborhood greenery and children’s cognitive development. Soc. Sci. Med. 2019, 230, 271–279. [Google Scholar] [CrossRef]
- Wang, D.; Lau, K.K.; Yu, R.; Wong, S.Y.S.; Kwok, T.T.Y.; Woo, J. Neighbouring green space and mortality in community-dwelling elderly Hong Kong Chinese: A cohort study. BMJ Open 2017, 7, e015794. [Google Scholar] [CrossRef]
- Ward, J.S.; Duncan, J.S.; Jarden, A.; Stewart, T. The impact of children’s exposure to greenspace on physical activity, cognitive development, emotional wellbeing, and ability to appraise risk. Health Place 2016, 40, 44–50. [Google Scholar] [CrossRef]
- Wu, Y.T.; Prina, A.M.; Jones, A.; Matthews, F.E.; Brayne, C.; Medical Research Council Cognitive Function and Ageing Study Collaboration. The Built Environment and Cognitive Disorders: Results From the Cognitive Function and Ageing Study II. Am. J. Prev. Med. 2017, 53, 25–32. [Google Scholar] [CrossRef]
- Wu, Y.T.; Prina, A.M.; Jones, A.P.; Barnes, L.E.; Matthews, F.E.; Brayne, C.; Medical Research Council Cognitive Function and Ageing Study. Community environment, cognitive impairment and dementia in later life: Results from the Cognitive Function and Ageing Study. Age Ageing 2015, 44, 1005–1011. [Google Scholar] [CrossRef] [PubMed]
- Yu, R.; Wang, D.; Leung, J.; Lau, K.; Kwok, T.; Woo, J. Is Neighborhood Green Space Associated With Less Frailty? Evidence From the Mr. and Ms. Os (Hong Kong) Study. J. Am. Med. Dir. Assoc. 2018, 19, 528–534. [Google Scholar] [CrossRef]
- Yuchi, W.; Sbihi, H.; Davies, H.; Tamburic, L.; Brauer, M. Road proximity, air pollution, noise, green space and neurologic disease incidence: A population-based cohort study. Environ. Health 2020, 19, 8. [Google Scholar] [CrossRef]
- Zhu, A.; Yan, L.; Shu, C.; Zeng, Y.; Ji, J.S. APOE epsilon4 Modifies Effect of Residential Greenness on Cognitive Function among Older Adults: A Longitudinal Analysis in China. Sci. Rep. 2020, 10, 82. [Google Scholar] [CrossRef] [PubMed]
- Zijlema, W.L.; Triguero-Mas, M.; Smith, G.; Cirach, M.; Martinez, D.; Dadvand, P.; Gascon, M.; Jones, M.; Gidlow, C.; Hurst, G.; et al. The relationship between natural outdoor environments and cognitive functioning and its mediators. Environ. Res. 2017, 155, 268–275. [Google Scholar] [CrossRef]
- Aitken, W.W.; Lombard, J.; Wang, K.; Toro, M.; Byrne, M.; Nardi, M.I.; Kardys, J.; Parrish, A.; Dong, C.; Szapocznik, J.; et al. Relationship of Neighborhood Greenness to Alzheimer’s Disease and Non-Alzheimer’s Dementia Among 249,405 U.S. Medicare Beneficiaries. J. Alzheimer’s Dis. 2021, 81, 597–606. [Google Scholar] [CrossRef] [PubMed]
- Almeida, D.Q.; Barros, H.; Ribeiro, A.I. Residential and school green and blue spaces and intelligence in children: The Generation XXI birth cohort. Sci. Total. Environ. 2022, 813, 151859. [Google Scholar] [CrossRef]
- Anabitarte, A.; Ibarluzea, J.; García-Baquero, G.; Santa Marina, L.; Fernández-Somoano, A.; Tardón, A.; Nieuwenhuijsen, M.; de Castro, M.; Dadvand, P.; Lertxundi, A. Effects of residential greenness on attention in a longitudinal study at 8 and 11-13 years. Environ. Res. 2022, 210, 112994. [Google Scholar] [CrossRef]
- Asta, F.; Michelozzi, P.; Cesaroni, G.; De Sario, M.; Davoli, M.; Porta, D. Green spaces and cognitive development at age 7 years in a rome birth cohort: The mediating role of nitrogen dioxide. Environ. Res. 2021, 196, 110358. [Google Scholar] [CrossRef] [PubMed]
- Astell-Burt, T.; Navakatikyan, M.A.; Feng, X. Urban green space, tree canopy and 11-year risk of dementia in a cohort of 109,688 Australians. Environ. Int. 2020, 145, 106102. [Google Scholar] [CrossRef] [PubMed]
- Astell-Burt, T.; Feng, X. Greener neighbourhoods, better memory? A longitudinal study. Health Place 2020, 65, 102393. [Google Scholar] [CrossRef] [PubMed]
- Besser, L.M.; Hirsch, J.; Galvin, J.E.; Renne, J.; Park, J.; Evenson, K.R.; Kaufman, J.D.; Fitzpatrick, A.L. Associations between neighborhood park space and cognition in older adults vary by US location: The Multi-Ethnic Study of Atherosclerosis. Health Place 2020, 66, 102459. [Google Scholar] [CrossRef]
- Besser, L.M.; Lovasi, G.S.; Michael, Y.L.; Garg, P.; Hirsch, J.A.; Siscovick, D.; Hurvitz, P.; Biggs, M.L.; Galvin, J.E.; Bartz, T.M.; et al. Associations between neighborhood greenspace and brain imaging measures in non-demented older adults: The Cardiovascular Health Study. Soc. Psychiatry Psychiatr. Epidemiol. 2021, 56, 1575–1585. [Google Scholar] [CrossRef]
- EBijnens, M.; Derom, C.; Thiery, E.; Weyers, S.; Nawrot, T.S. Residential green space and child intelligence and behavior across urban, suburban, and rural areas in Belgium: A longitudinal birth cohort study of twins. PLoS Med. 2020, 17, e1003213. [Google Scholar] [CrossRef]
- Bijnens, E.M.; Vos, S.; Verheyen, V.V.; Bruckers, L.; Covaci, A.; De Henauw, S.; Den Hond, E.; Loots, I.; Nelen, V.; Plusquin, M.; et al. Higher surrounding green space is associated with better attention in Flemish adolescents. Environ. Int. 2022, 159, 107016. [Google Scholar] [CrossRef]
- Binter, A.C.; Bernard, J.Y.; Mon-Williams, M.; Andiarena, A.; González-Safont, L.; Vafeiadi, M.; Lepeule, J.; Soler-Blasco, R.; Alonso, L.; Kampouri, M.; et al. Urban environment and cognitive and motor function in children from four European birth cohorts. Environ. Int. 2022, 158, 106933. [Google Scholar] [CrossRef]
- Cerin, E.; Barnett, A.; Shaw, J.E.; Martino, E.; Knibbs, L.D.; Tham, R.; Wheeler, A.J.; Anstey, K.J. From urban neighbourhood environments to cognitive health: A cross-sectional analysis of the role of physical activity and sedentary behaviours. BMC Public Health 2021, 21, 2320. [Google Scholar] [CrossRef]
- Crous-Bou, M.; Gascon, M.; Gispert, J.D.; Cirach, M.; Sánchez-Benavides, G.; Falcon, C.; Arenaza-Urquijo, E.M.; Gotsens, X.; Fauria, K.; Sunyer, J.; et al. Impact of urban environmental exposures on cognitive performance and brain structure of healthy individuals at risk for Alzheimer’s dementia. Environ. Int. 2020, 138, 105546. [Google Scholar] [CrossRef]
- Dockx, Y.; Bijnens, E.M.; Luyten, L.; Peusens, M.; Provost, E.; Rasking, L.; Sleurs, H.; Hogervorst, J.; Plusquin, M.; Casas, L.; et al. Early life exposure to residential green space impacts cognitive functioning in children aged 4 to 6years. Environ. Int. 2022, 161, 107094. [Google Scholar] [CrossRef] [PubMed]
- Falcón, C.; Gascon, M.; Molinuevo, J.L.; Operto, G.; Cirach, M.; Gotsens, X.; Fauria, K.; Arenaza-Urquijo, E.M.; Pujol, J.; Sunyer, J.; et al. Brain correlates of urban environmental exposures in cognitively unimpaired individuals at increased risk for Alzheimer’s disease: A study on Barcelona’s population. Alzheimer’s Dement. 2021, 13, e12205. [Google Scholar] [CrossRef]
- Fangfang, H.; Xiao, H.; Shuai, Z.; Qiong, W.; Jingya, Z.; Guodong, S.; Yan, Z. Living Environment, Built Environment and Cognitive Function among Older Chinese Adults: Results from a Cross-Sectional Study. J. Prev. Alzheimer’s Dis. 2022, 9, 126–135. [Google Scholar] [CrossRef] [PubMed]
- Finlay, J.; Esposito, M.; Li, M.; Colabianchi, N.; Zhou, H.; Judd, S.; Clarke, P. Neighborhood active aging infrastructure and cognitive function: A mixed-methods study of older Americans. Prev. Med. 2021, 150, 106669. [Google Scholar] [CrossRef] [PubMed]
- Jimenez, M.P.; Shoaff, J.; Kioumourtzoglou, M.A.; Korrick, S.; Rifas-Shiman, S.L.; Hivert, M.F.; Oken, E.; James, P. Early-Life Exposure to Green Space and Mid-Childhood Cognition in the Project Viva Cohort, Massachusetts. Am. J. Epidemiol. 2022, 191, 115–125. [Google Scholar] [CrossRef]
- Jin, X.; Shu, C.; Zeng, Y.; Liang, L.; Ji, J.S. Interaction of greenness and polygenic risk score of Alzheimer’s disease on risk of cognitive impairment. Sci. Total Environ. 2021, 796, 148767. [Google Scholar] [CrossRef] [PubMed]
- Ju, Y.J.; Lee, J.E.; Lee, S.Y. Perceived environmental pollution and subjective cognitive decline (SCD) or SCD-related functional difficulties among the general population. Environ. Sci. Pollut. Res. Int. 2021, 28, 31289–31300. [Google Scholar] [CrossRef]
- Julvez, J.; López-Vicente, M.; Warembourg, C.; Maitre, L.; Philippat, C.; Gützkow, K.B.; Guxens, M.; Evandt, J.; Andrusaityte, S.; Burgaleta, M.; et al. Early life multiple exposures and child cognitive function: A multi-centric birth cohort study in six European countries. Environ. Pollut. 2021, 284, 117404. [Google Scholar] [CrossRef]
- Lee, K.S.; Kim, B.N.; Cho, J.; Jang, Y.Y.; Choi, Y.J.; Lee, W.S.; Han, C.; Bae, H.J.; Lim, Y.H.; Kim, J.I.; et al. Associations between surrounding residential greenness and intelligence quotient in 6-year-old children. Sci. Total Environ. 2021, 759, 143561. [Google Scholar] [CrossRef]
- Lega, C.; Gidlow, C.; Jones, M.; Ellis, N.; Hurst, G. The relationship between surrounding greenness, stress and memory. Urban For. Urban Green. 2021, 59, 126974. [Google Scholar] [CrossRef]
- Liu, C.C.; Li, C.Y.; Kung, S.F.; Kuo, H.W.; Huang, N.C.; Sun, Y.; Hu, S.C. Association of Environmental Features and the Risk of Alzheimer’s Dementia in Older Adults: A Nationwide Longitudinal Case-Control Study. Int. J. Environ. Res. Public. Health 2019, 16, 2828. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.C.; Sun, Y.; Kung, S.F.; Kuo, H.W.; Huang, N.C.; Li, C.Y.; Hu, S.C. Effects of physical and social environments on the risk of dementia among Taiwanese older adults: A population-based case-control study. BMC Geriatr. 2020, 20, 226. [Google Scholar] [CrossRef] [PubMed]
- Paul, L.A.; Hystad, P.; Burnett, R.T.; Kwong, J.C.; Crouse, D.L.; van Donkelaar, A.; Tu, K.; Lavigne, E.; Copes, R.; Martin, R.V.; et al. Urban green space and the risks of dementia and stroke. Environ. Res. 2020, 186, 109520. [Google Scholar] [CrossRef] [PubMed]
- Slawsky, E.D.; Hajat, A.; Rhew, I.C.; Russette, H.; Semmens, E.O.; Kaufman, J.D.; Leary, C.S.; Fitzpatrick, A.L. Neighborhood greenspace exposure as a protective factor in dementia risk among US adults 75 years or older: A cohort study. Environ. Health 2022, 21, 14. [Google Scholar] [CrossRef]
- Tani, Y.; Hanazato, M.; Fujiwara, T.; Suzuki, N.; Kondo, K. Neighborhood Sidewalk Environment and Incidence of Dementia in Older Japanese Adults. Am. J. Epidemiol. 2021, 190, 1270–1280. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.T.; Brayne, C.; Liu, Z.; Huang, Y.; Sosa, A.L.; Acosta, D.; Prina, M. Neighbourhood environment and dementia in older people from high-, middle- and low-income countries: Results from two population-based cohort studies. BMC Public Health 2020, 20, 1330. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Jackson, L. Greenspace Inversely Associated with the Risk of Alzheimer’s Disease in the Mid-Atlantic United States. Earth 2021, 2, 140–150. [Google Scholar] [CrossRef]
- Zhu, A.; Wu, C.; Yan, L.L.; Wu, C.D.; Bai, C.; Shi, X.; Zeng, Y.; Ji, J.S. Association between residential greenness and cognitive function: Analysis of the Chinese Longitudinal Healthy Longevity Survey. BMJ Nutr. Prev. Health 2019, 2, 72–79. [Google Scholar] [CrossRef]
- Bagheri, N.; Mavoa, S.; Tabatabaei-Jafari, H.; Knibbs, L.D.; Coffee, N.T.; Salvador-Carulla, L.; Anstey, K.J. The Impact of Built and Social Environmental Characteristics on Diagnosed and Estimated Future Risk of Dementia. J. Alzheimer’s Dis. 2021, 84, 621–632. [Google Scholar] [CrossRef]
- Pirani, M.; Booth, E.R.; Shen, C.; Milligan, B.; Jones, E.K.; Toledano, M.B. Benefit of woodland and other natural environments for adolescents’ cognition and mental health. Nat. Sustain. 2021, 4, 851–858. [Google Scholar] [CrossRef]
- Sylvers, D.L.; Hicken, M.; Esposito, M.; Manly, J.; Judd, S.; Clarke, P. Walkable Neighborhoods and Cognition: Implications for the Design of Health Promoting Communities. J. Aging Health 2022, 34, 893–904. [Google Scholar] [CrossRef] [PubMed]
- Vaughan, C.A.; Cohen, D.A.; Han, B. How Do Racial/Ethnic Groups Differ in Their Use of Neighborhood Parks? Findings from the National Study of Neighborhood Parks. J. Urban Health 2018, 95, 739–749. [Google Scholar] [CrossRef]
- Hamlin, A.M.; Kraal, A.Z.; Sol, K.; Morris, E.P.; Martino, A.G.; Zaheed, A.B.; Zahodne, L.B. Social engagement and its links to cognition differ across non-Hispanic Black and White older adults. Neuropsychology 2022, 36, 640–650. [Google Scholar] [CrossRef]
- Matthews, S.A.; Yang, T.C. Spatial Polygamy and Contextual Exposures (SPACEs): Promoting Activity Space Approaches in Research on Place and Health. Am. Behav. Sci. 2013, 57, 1057–1081. [Google Scholar] [CrossRef] [PubMed]
- National Institute on Aging. National Strategy for Recruitment and Participation in Alzheimer’s and Related Dementias Clinical Research. Available online: https://www.nia.nih.gov/research/recruitment-strategy (accessed on 18 October 2022).
- Ejiogu, N.; Norbeck, J.H.; Mason, M.A.; Cromwell, B.C.; Zonderman, A.B.; Evans, M.K. Recruitment and retention strategies for minority or poor clinical research participants: Lessons from the Healthy Aging in Neighborhoods of Diversity across the Life Span study. Gerontologist 2011, 51 (Suppl. S1), S33–S45. [Google Scholar] [CrossRef] [PubMed]
- Kimble, J. Insuring inequality: The role of the federal housing administration in the urban ghettoization of African Americans. Law Soc. Inq. 2007, 32, 399–434. [Google Scholar] [CrossRef]
- Kushner, J.A. Apartheid in America—A Historical and Legal Analysis of Contemporary Racial Segregation in the United-States. Mich. Law Rev. 1981, 79, 856–858. [Google Scholar] [CrossRef]
- Galea, S. Moving Beyond the Social Determinants of Health. Int. J. Health Serv. 2022, 52, 423–427. [Google Scholar] [CrossRef]
- Arias, E.; Tejada-Vera, B.; Ahmad, F.; Kochanek, K.D. Provisional Life Expectancy Estimages for 2021; National Center for Health Statistics: Hyattsville, MA, USA, 2002; Volume 23.
- Lin, P.J.; Daly, A.T.; Olchanski, N.; Cohen, J.T.; Neumann, P.J.; Faul, J.D.; Fillit, H.M.; Freund, K.M. Dementia Diagnosis Disparities by Race and Ethnicity. Med. Care 2021, 59, 679–686. [Google Scholar] [CrossRef]
- Loukaitou-Sideris, A.; Levy-Storms, L.; Chen, L.; Brozen, M. Parks for an Aging Population: Needs and Preferences of Low-Income Seniors in Los Angeles. J. Am. Plan. Assoc. 2016, 82, 236–251. [Google Scholar] [CrossRef]
- Tinsley, H.E.A.; Tinsley, D.J.; Croskeys, C.E. Park usage, social milieu, and psychosocial benefits of park use reported by older urban park users from four ethnic groups. Leisure Sci. 2002, 24, 199–218. [Google Scholar] [CrossRef]
- Knapp, M.; Gustat, J.; Darensbourg, R.; Myers, L.; Johnson, C. The Relationships between Park Quality, Park Usage, and Levels of Physical Activity in Low-Income, African American Neighborhoods. Int. J. Environ. Res. Public. Health 2018, 16, 85. [Google Scholar] [CrossRef]
- Chu, Y.T.; Li, D.; Chang, P.J. Effects of Urban Park Quality, Environmental Perception, and Leisure Activity on Well-Being among the Older Population. Int. J. Environ. Res. Public. Health 2021, 18, 11402. [Google Scholar] [CrossRef] [PubMed]
- Gianattasio, K.Z.; Prather, C.; Glymour, M.M.; Ciarleglio, A.; Power, M.C. Racial disparities and temporal trends in dementia misdiagnosis risk in the United States. Alzheimer’s Dement. 2019, 5, 891–898. [Google Scholar] [CrossRef] [PubMed]
- Bernstein Sideman, A.; Al-Rousan, T.; Tsoy, E.; Piña Escudero, S.D.; Pintado-Caipa, M.; Kanjanapong, S.; Mbakile-Mahlanza, L.; Okada de Oliveira, M.; De la Cruz-Puebla, M.; Zygouris, S.; et al. Facilitators and Barriers to Dementia Assessment and Diagnosis: Perspectives From Dementia Experts Within a Global Health Context. Front. Neurol. 2022, 13, 769360. [Google Scholar] [CrossRef]
- Zahodne, L.B.; Manly, J.J.; Azar, M.; Brickman, A.M.; Glymour, M.M. Racial Disparities in Cognitive Performance in Mid- and Late Adulthood: Analyses of Two Cohort Studies. J. Am. Geriatr. Soc. 2016, 64, 959–964. [Google Scholar] [CrossRef]
- Glymour, M.M.; Manly, J.J. Lifecourse Social Conditions and Racial and Ethnic Patterns of Cognitive Aging. Neuropsychol. Rev. 2008, 18, 223–254. [Google Scholar] [CrossRef]
- Besser, L.M.; Brenowitz, W.D.; Meyer, O.L.; Hoermann, S.; Renne, J. Methods to Address Self-Selection and Reverse Causation in Studies of Neighborhood Environments and Brain Health. Int. J. Environ. Res. Public. Health 2021, 18, 6484. [Google Scholar] [CrossRef] [PubMed]
- Lemelin, E.T.; Diez Roux, A.V.; Franklin, T.G.; Carnethon, M.; Lutsey, P.L.; Ni, H.; O’Meara, E.; Shrager, S. Life-course socioeconomic positions and subclinical atherosclerosis in the multi-ethnic study of atherosclerosis. Soc. Sci. Med. 2009, 68, 444–451. [Google Scholar] [CrossRef]
- Helbich, M.; O’Connor, R.C.; Nieuwenhuijsen, M.; Hagedoorn, P. Greenery exposure and suicide mortality later in life: A longitudinal register-based case-control study. Environ. Int. 2020, 143, 105982. [Google Scholar] [CrossRef]
- DeFrank, J.T.; Bowling, J.M.; Rimer, B.K.; Gierisch, J.M.; Skinner, C.S. Triangulating differential nonresponse by race in a telephone survey. Prev. Chronic Dis. 2007, 4, A60. [Google Scholar]
- Giuliano, A.R.; Mokuau, N.; Hughes, C.; Tortolero-Luna, G.; Risendal, B.; Ho, R.C.S.; Prewitt, T.E.; McCaskill-Stevens, W.J. Participation of minorities in cancer research: The influence of structural, cultural, and linguistic factors. Ann. Epidemiol. 2000, 10 (Suppl. S8), S22–S34. [Google Scholar] [CrossRef]
- Scharff, D.P.; Mathews, K.J.; Jackson, P.; Hoffsuemmer, J.; Martin, E.; Edwards, D. More than Tuskegee: Understanding mistrust about research participation. J. Health Care Poor Underserved. 2010, 21, 879–897. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, A.L.; Alsan, M.; Morris, A.A.; Halpern, S.D. Why Diverse Clinical Trial Participation Matters. N. Engl. J. Med. 2023, 388, 1252–1254. [Google Scholar] [CrossRef] [PubMed]
- Mooldijk, S.S.; Licher, S.; Wolters, F.J. Characterizing Demographic, Racial, and Geographic Diversity in Dementia Research: A Systematic Review. JAMA Neurol. 2021, 78, 1255–1261. [Google Scholar] [CrossRef] [PubMed]
- Jelks, N.O.; Jennings, V.; Rigolon, A. Green Gentrification and Health: A Scoping Review. Int. J. Environ. Res. Public. Health 2021, 18, 907. [Google Scholar] [CrossRef]
- Besser, L.M.; Mitsova, D.P. Neighborhood Green Land Cover and Neighborhood-Based Walking in U.S. Older Adults. Am. J. Prev. Med. 2021, 61, e13–e20. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Healthy Places: Strategies. Available online: https://www.cdc.gov/healthyplaces/healthtopics/gentrification_strategies.htm (accessed on 18 October 2022).




| First Author (Year) | Sample Size | Age Groups Included | Geographic Location | The Study Included the Following Racialized/Ethnic Group(s) ** | Association | ||||
|---|---|---|---|---|---|---|---|---|---|
| White/European | Black/ African American | Hispanic/ LatinX | Asian Pacific Islander | Did Not Specify Any | |||||
| Aitken (2021) (CS) [65] | 249,405 | ≥65 years | US | Yes | Yes | Yes | No | No | Grness-Dx: + Grness-Dx: N |
| Almeida (2022) (CS) [66] | 3827 | <18 years | Portugal | No | No | No | No | Yes | GrSp-Cog: + GrSp-Cog: N Grness-Cog: − Grness-Cog: N |
| Anabitarte (2022) (LC) [67] | 751 | <18 years | Spain | No | No | No | No | Yes | Grness-Cog: + Grness-Cog: N GrSp-Cog: N |
| Asta (2021) (CS) [68] | 465 | <18 years | Italy | No | No | No | No | Yes | Grness-Cog: + Grness-Cog: N |
| Astell-Burt (2020) (LC) [9] | 45,644 | 45–64 years, ≥65 years | Australia | No | No | No | No | Yes | OthGr-SubCog: + OthGr-SubCog: N |
| Astell-Burt (2020) (LC) [70] | 109,688 | 45–64 years, ≥65 years | Australia | No | No | No | No | Yes | GrSp-Dx: − GrSp-Dx: + GrSp-Dx: N |
| Bagheri (2021) (CS) [96] | 25,511 | ≥65 years | Australia | No | No | No | No | Yes | GrSp-Dx: + GrSp-Dx: N |
| Besser (2020) (CS) [71] | 4084 | 45–64 years, ≥65 years | US | Yes | Yes | Yes | Yes | No | GrSp-Cog: + GrSp-Cog: − GrSp-Cog: N |
| Besser (2021) (LC) [27] | 1733 | 45–64 years, ≥65 years | US | Yes | Yes | Yes | Yes | No | GrSp-Cog: + GrSp-Cog: N |
| Besser (2021) (CS) [72] | 1125 | ≥65 years | US | Yes | Yes | No | No | Yes | GrSp-Img: N |
| Bijnens (2020) (CS) [73] | 620 | <18 years | Belgium | No | No | No | No | Yes | GrSp-Cog: + GrSp-Cog: N |
| Bijnens (2022) (CS) [74] | 596 | <18 years | Belgium | No | No | No | No | Yes | GrSp-Cog: + GrSp-Cog: N |
| Binter (2022) (CS) [75] | 5403 | <18 years | UK, France, Spain, Greece | No | No | No | No | Yes | Grness-Cog: + Grness-Cog: N GrSp-Cog: N |
| Brown (2018) (CS) [47] | 249,405 | ≥65 years | US | Yes | Yes | Yes | No | No | Grness-Dx: + |
| Cerin (2021) (CS) [76] | 4141 | 18–44 years, 45–64 years, ≥65 years | Australia | No | No | No | No | Yes | GrSp-Cog: + |
| Cherrie (2018) (LC) [26] | 281 | <18 years, 18–44 years, 45–64 years, ≥65 years | UK | No | No | No | No | Yes | GrSp-Cog: + GrSp-Cog: N |
| Cherrie (2019) (LC) [48] | 281 | ≥65 years | UK | No | No | No | No | Yes | GrSp-Cog: + GrSp-Cog: N |
| Clarke (2012) (CS) [49] | 949 | 45–64 years, ≥65 years | US | Yes | Yes | Yes | No | No | GrSp-Cog: N |
| Crous-Bou (2020) (CS) [77] | 958 | 45–64 years, ≥65 years | Spain | No | No | No | No | Yes | Grness-Cog: N Grness-Img: + Grness-Img: N |
| Dadvand (2015) (LC) [50] | 2593 | <18 years | Spain | No | No | No | No | Yes | Grness-Cog: + Grness-Cog: N |
| Dadvand (2017) (LC) [51] | 987 | <18 years | Spain | No | No | No | No | Yes | Grness-Cog: + Grness-Cog: N |
| Dadvand (2018) (CS) [30] | 253 | <18 years | Spain | No | No | No | No | Yes | Grness-Img: + Grness-Img: N |
| De Keijzer (2018) (LC) [29] | 6506 | 45–64 years, ≥65 years | UK | No | No | No | No | Yes | Grness-Cog: + Grness-Cog: N |
| Dockx (2022) (CS) [78] | 456 | <18 years | Belgium | No | No | No | No | Yes | GrSp-Cog: + GrSp-Cog: N |
| Dzhambov (2019) (CS) [52] | 112 | <18 years | Bulgaria | No | No | No | No | Yes | Grness-Cog: + Grness-Cog: N Grness-Img: + Grness-Img: N |
| Falcon (2021) (CS) [79] | 212 | 45–64 years, ≥65 years | Spain | No | No | No | No | Yes | Grness-Img: + Grness-Img: N |
| FangFang (2022) (CS) [80] | 5848 | 45–64 years, ≥65 years | China | No | No | No | No | Yes | GrSp-Cog: N |
| Finlay (2021) (CS) [81] | 21,151 (quantitative) 125 (qualitative) | 45–64 years, ≥65 years | US | Yes | Yes | No | No | Yes | GrSp-Cog: + |
| Flouri (2019) (CS) [53] | 4758 | <18 years | UK | No | No | No | No | Yes | GrSp-Cog: + |
| Hystad (2019) (CS) [54] | 6658 | 18–44 years, 45–64 years, ≥65 years | Canada | No | No | No | No | Yes | Grness-Cog: − Grness-Cog: N |
| Jimenez (2022) (CS) [82] | 857 | <18 years | US | Yes | No | No | No | Yes | Grness-Cog: + Grness-Cog: N |
| Jin (2021) (CS) [83] | 1199 | ≥65 years | China | No | No | No | Yes | No | Grness-Cog: + Grness-Cog: N |
| Ju (2021) (CS) [84] | 191,054 | 18–44 years, 45–64 years, ≥65 years | Korea | No | No | No | No | Yes | OthGr-SubCog: N |
| Julvez (2021) (CS) [85] | 1298 | <18 years | UK, France, Spain, Lithuania, Norway, Greece | No | No | No | No | Yes | Grness-Cog: + Grness-Cog: − Grness-Cog: N |
| Kuhn (2017) (CS) [31] | 341 | 45–64 years, ≥65 years | Germany | No | No | No | No | Yes | GrSp-Img: + GrSp-Img: N |
| Lee (2021) (CS) [86] | 189 | <18 years | Korea | No | No | No | No | Yes | Grness-Cog: + Grness-Cog: N |
| Lega (2021) (CS) [87] | 185 | 18–44 years, 45–64 years, ≥65 years | UK | No | No | No | No | Yes | Grness-Cog: + Grness-Cog: N |
| Liao (2019) (CS) [55] | 1312 | <18 years | China | No | No | No | No | Yes | Grness-Cog: + |
| Liu (2019) (LC) [88] | 24,802 | ≥65 years | Taiwan | No | No | No | No | Yes | GrSp-dx: N |
| Liu (2020) (LC) [89] | 52,412 | ≥65 years | Taiwan | No | No | No | No | Yes | GrSp-dx: N |
| Maes (2021) (LC) [97] | 3568 | <18 years | UK | Yes | Yes | No | Yes | Yes | GrSp-Cog: + GrSp-Cog: N |
| Paul (2020) (LC) [90] | 1.74 million dementia cohort, 4.25 million stroke cohort | 18–44 years, 45–64 years, ≥65 years | Canada | No | No | No | No | Yes | Grness-Dx: + |
| Reuben (2019) (LC) [56] | 1658 | <18 years | UK | No | No | No | No | Yes | Grness-Cog: N |
| Slawsky (2022) (LC) [91] | 3047 | ≥65 years | US | Yes | No | No | No | Yes | OthGr-Dx: + |
| Sylvers (2022) (CS) [98] | 10,289 | 45–64 years, ≥65 years | US | Yes | Yes | No | No | No | GrSp-Cog: + GrSp-Cog: N |
| Tani (2021) (LC) [92] | 76,053 | ≥65 years | Japan | No | No | No | No | Yes | GrSp-Dx: N |
| Wang (2017 (CS) [57] | 3544 | ≥65 years | China | No | No | No | No | Yes | Grness-Cog: N |
| Ward (2016) (CS) [58] | 72 | <18 years | New Zealand | No | No | No | No | Yes | OthGr-Cog: N |
| Wu (2015) (CS) [60] | 2424 | ≥65 years | UK | No | No | No | No | Yes | GrSp-Cog: − GrSp-Dx: − |
| Wu (2017) (CS) [59] | 7505 | ≥65 years | UK | No | No | No | No | Yes | GrSp-Cog: − GrSp-Dx: N |
| Wu (2020) (CS) [93] | CFAS: 4955 10/66: 3386 | ≥65 years | UK China, Dominican Republic, Mexico | No | No | No | No | Yes | GrSp-Dx: − GrSp-Dx: N |
| Wu (2021) (LC) [94] | ~106,763 | ≥65 years | US | Yes | Yes | No | No | No | GrSp-Dx: + |
| Yu (2018) (CS) [61] | 3240 | ≥65 years | China | No | No | No | No | Yes | Grness-Cog: N |
| Yuchi (2020) (LC) [62] | 678,000 | 45–64 years, ≥65 years | Canada | No | No | No | No | Yes | Grness-Dx: + Grness-Dx: − |
| Zhu (2019) (LC) [95] | 38,327 | ≥65 years | China | No | No | No | No | Yes | Grness-Cog: + Grness-Cog: N |
| Zhu (2020) (LC) [63] | 6994 | ≥65 years | China | No | No | No | Yes | No | Grness-Cog: + |
| Zijlema (2017) (CS) [64] | 1628 | 18–44 years, 45–64 years, ≥65 years | Spain, Netherlands, UK | No | No | No | No | Yes | GrSp-Cog: + GrSp-Cog: N Grness-Cog: N OthGr-Cog: N |
| Total studies by racialized/ethnic group | 14 | 10 | 5 | 5 | 41 | -- | |||
| Studies with positive associations | 42 | ||||||||
| Studies with inverse associations | 9 | ||||||||
| Studies with null associations | 46 (11 had only null associations) | ||||||||
| Total | 57 studies | ||||||||
| Citation | Method | Finding |
|---|---|---|
| Aitken et al. (2021) [65] | Interaction term testing (e.g., NDVI x racialized/ethnic group) | No interaction was indicated between NDVI and racialized/ethnic group (Non-Hispanic White, Hispanic, Black) in relation to the odds of ADRD diagnosis (results not reported). |
| Besser et al. (2021) [27] | Stratification by racialized/ethnic group and interaction term testing (i.e., percentage park space x racialized/ethnic group) | Among Black participants, neighborhood percentage park space was borderline associated with maintained/improved global cognition. No association for White participants. The interaction term was not statistically significant. |
| Wu & Jackson (2021) [94] | Stratification by racialized/ethnic group | Neighborhood percentage greenspace associated with reduced Alzheimer’s risk in both Black and White individuals. No difference in association based on racialized/ethnic group. |
| Hystad et al. (2019) [54] | Stratification by racialized/ethnic group | No difference in the association between neighborhood greenness (NDVI) and cognitive functioning (reasoning, visual memory, and reaction time) between White and non-White participants. |
| Concern/Topic | Details |
|---|---|
| Segregation of neighborhoods by racialized/ethnic group | Residential neighborhood correlated with individual’s racialized/ethnic group, amount and type/quality of neighborhood greenspace, and individual and neighborhood SES. Difficult to disentangle these factors. |
| Insufficient recruitment of diverse cohorts | Lack of focus on recruiting diverse samples from the start (not a priority). Difficulty in recruiting diverse samples due to lack of experience/knowledge/effort by investigators, lack of trust of investigators, and lack of diverse researchers/study team. |
| Differential attrition by racialized/ethnic group | Racialized/ethnic groups are often less likely to enroll in studies and more likely to drop out over time due to social determinants. |
| Overemphasis on statistical significance and comparison with the White reference group (e.g., testing differences using interaction terms) | Heterogeneity within racialized/ethnic groups is often ignored with a preference for a comparison group. |
| Differences in greenspace exposure and quality by racialized/ethnic group | Measuring the amount of neighborhood greenspace/greenness may obscure differences in true exposure to greenspace or quality that may significantly differ by racialized/ethnic group (e.g., differences in preference for greenspaces or time spent in neighborhoods due to differences in transportation modes) |
| Neuropsychological tests developed primarily for the majority (e.g., White individuals) | Inadequate accounting for cultural differences that affect testing/scores and historical, upstream factors that affect cognitive test scores differential by racialized/ethnic group. |
| Differences in residential moves and neighborhood self-selection by racialized/ethnic group | Important to consider the context of residential moves and how it likely differs depending on racialized/ethnic group (e.g., out of choice or necessity). Many studies emphasize potential bias from self-selection into greener neighborhoods that promote physical activity, but this may not be as common for minoritized groups. |
| Challenges in obtaining detailed or technology-based measures of the complex, multi-faceted environmental exposures (e.g., spatial polygamy [101]) | Studies requiring long-term, detailed, or technologically intensive data acquisition can be a deterrent to participation for minoritized racialized/ethnic groups. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Besser, L.M.; Jimenez, M.P.; Reimer, C.J.; Meyer, O.L.; Mitsova, D.; George, K.M.; Adkins-Jackson, P.B.; Galvin, J.E. Diversity of Studies on Neighborhood Greenspace and Brain Health by Racialized/Ethnic Group and Geographic Region: A Rapid Review. Int. J. Environ. Res. Public Health 2023, 20, 5666. https://doi.org/10.3390/ijerph20095666
Besser LM, Jimenez MP, Reimer CJ, Meyer OL, Mitsova D, George KM, Adkins-Jackson PB, Galvin JE. Diversity of Studies on Neighborhood Greenspace and Brain Health by Racialized/Ethnic Group and Geographic Region: A Rapid Review. International Journal of Environmental Research and Public Health. 2023; 20(9):5666. https://doi.org/10.3390/ijerph20095666
Chicago/Turabian StyleBesser, Lilah M., Marcia Pescador Jimenez, Cameron J. Reimer, Oanh L. Meyer, Diana Mitsova, Kristen M. George, Paris B. Adkins-Jackson, and James E. Galvin. 2023. "Diversity of Studies on Neighborhood Greenspace and Brain Health by Racialized/Ethnic Group and Geographic Region: A Rapid Review" International Journal of Environmental Research and Public Health 20, no. 9: 5666. https://doi.org/10.3390/ijerph20095666
APA StyleBesser, L. M., Jimenez, M. P., Reimer, C. J., Meyer, O. L., Mitsova, D., George, K. M., Adkins-Jackson, P. B., & Galvin, J. E. (2023). Diversity of Studies on Neighborhood Greenspace and Brain Health by Racialized/Ethnic Group and Geographic Region: A Rapid Review. International Journal of Environmental Research and Public Health, 20(9), 5666. https://doi.org/10.3390/ijerph20095666








