Health Professionals’ Chronotype Association with Salivary Cortisol and Occupational Stress in Neonatal Intensive Care Units
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Procedure
2.3.1. Sociodemographic Information, Work Conditions, and Lifestyle Habits
2.3.2. Burnout Characterization Scale
2.3.3. Morningness–Eveningness Questionnaire
2.3.4. Salivary Cortisol
2.3.5. Anthropometric Profile
2.3.6. Statistical Analysis
2.4. Ethical Approval
3. Results
3.1. Health Professionals’ Work Characteristics
3.2. Health Professionals’ Subjective and Objective Stress Levels
3.3. Health Professionals’ Chronotype and Associated Sociodemographic Factors
3.4. Health Professionals’ Burnout Syndrome, Salivary Cortisol, and Chronotype
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Da Silva Ferreira, L.B.; Ribeiro, R.D.C.H.M.; Pompeo, D.A.; Contrin, L.M.; Werneck, A.L.; Ribeiro, R.M.; Sousa, C.N. Nível de Estresse e Avaliação Preliminar da Síndrome de Burnout Em Enfermeiro Da UTI Na COVID-19-Estudo de Caso. Res. Soc. Dev. 2022, 11, e31111225658. [Google Scholar] [CrossRef]
- Lima, P.C.; de Oliveira Gouveia, M.T.; Sabino, K.C.V.; Fernandes, M.A.; Avelino, F.V.S.D. Fatores Estressores e as Estratégias de Enfrentamento Utilizadas Por Enfermeiros Hospitalares: Revisão. Investig. En Enfermería Imagen Y Desarro. 2015, 17, 51–65. [Google Scholar] [CrossRef]
- Pineda, R.; Durant, P.; Mathur, A.; Inder, T.; Wallendorf, M.; Schlaggar, B.L. Auditory Exposure in the Neonatal Intensive Care Unit: Room Type and Other Predictors. J. Pediatr. 2017, 183, 56–66.e3. [Google Scholar] [CrossRef] [PubMed]
- Friganović, A.; Kovačević, I.; Ilić, B.; Žulec, M.; Krikšić, V.; Bile, C.G. Healthy Settings in Hospital—How to Prevent Burnout Syndrome in Nurses: Literature Review. Acta Clin. Croat. 2017, 56, 292–298. [Google Scholar] [CrossRef]
- Teixeira, L.B.; Veloso, L.U.P.; Ribeiro, Í.A.P.; Oliveira, T.N.d.; Cortez, A.C.L. Estresse Ocupacional Na Enfermagem Atuante Na Unidade de Terapia Intensiva. Investig. En Enfermería Imagen Y Desarro. 2017, 19, 195. [Google Scholar] [CrossRef]
- Nantsupawat, A.; Nantsupawat, R.; Kunaviktikul, W.; Turale, S.; Poghosyan, L. Nurse Burnout, Nurse-Reported Quality of Care, and Patient Outcomes in Thai Hospitals. J. Nurs. Scholarsh. 2016, 48, 83–90. [Google Scholar] [CrossRef]
- Vahedian-Azimi, A.; Hajiesmaeili, M.; Kangasniemi, M.; Fornés-Vives, J.; Hunsucker, R.L.; Rahimibashar, F.; Pourhoseingholi, M.A.; Farrokhvar, L.; Miller, A.C. Effects of Stress on Critical Care Nurses: A National Cross-Sectional Study. J. Intensive Care Med. 2019, 34, 311–322. [Google Scholar] [CrossRef]
- Briguglio, G.; Teodoro, M.; Italia, S.; Verduci, F.; Pollicino, M.; Coco, M.; De Vita, A.; Micali, E.; Alibrandi, A.; Lembo, G.; et al. Salivary Biomarkers and Work-Related Stress in Night Shift Workers. Int. J. Environ. Res. Public Health 2021, 18, 3184. [Google Scholar] [CrossRef]
- Maslach, C.; Schaufeli, W.B.; Leiter, M.P. Job Burnout. Annu. Rev. Psychol. 2001, 52, 397–422. [Google Scholar] [CrossRef]
- Harbs, T.; Rodrigues, T.; Quadros, V. Estresse da Equipe de Enfermagem Em Um Centro de Urgência e Emergência. Bol. Enferm. 2008, 1, 41–56. [Google Scholar]
- Da Cunha, S.M.M.; da Silva, V.R.M.; Dendasck, C.V.; De Medeiros Moreira, E.C.; de Oliveira, M.; de Oliveira, E. Estresse Ocupacional da Equipe de Enfermagem Que Atua Em Unidade de Terapia Intensiva. Rev. Científica Multidiscip. Núcleo Do Conhecimento 2017, 4, 68–78. [Google Scholar] [CrossRef]
- Da Silva Campos, M.; Dos Santos Esteves, T.M.; De Oliveira, V.A.S.C.; Garcia, J.R. O Estresse Ocupacional No Enfermeiro Na Unidade de Terapia Intensiva. Rev. Eletrônica E-F@tec 2018, 8, 1–9. [Google Scholar]
- Friganović, A.; Selič, P. Where to Look for a Remedy? Burnout Syndrome and Its Associations with Coping and Job Satisfaction in Critical Care Nurses—A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 4390. [Google Scholar] [CrossRef]
- Wagner, A.; Hammer, A.; Manser, T.; Martus, P.; Sturm, H.; Rieger, M.A. Do Occupational and Patient Safety Culture in Hospitals Share Predictors in the Field of Psychosocial Working Conditions? Findings from a Cross-Sectional Study in German University Hospitals. Int. J. Environ. Res. Public Health 2018, 15, 2131. [Google Scholar] [CrossRef]
- Myhren, H.; Ekeberg, Ø.; Stokland, O. Job Satisfaction and Burnout among Intensive Care Unit Nurses and Physicians. Crit. Care Res. Pract. 2013, 1–6. [Google Scholar] [CrossRef]
- Pejušković, B.; Lečić-Toševski, D.; Priebe, S.; Tošković, O. Burnout Syndrome among Physicians—The Role of Personality Dimensions and Coping Strategies. Psychiatr. Danub. 2011, 23, 389–395. [Google Scholar]
- Sánchez-Moreno, E.; De La Fuente Roldán, I.N.; Gallardo-Peralta, L.P.; Barrón López De Roda, A. Burnout, Informal Social Support and Psychological Distress among Social Workers. Br. J. Soc. Work 2015, 45, 2368–2386. [Google Scholar] [CrossRef]
- Rajcani, J.; Vytykacova, S.; Solarikova, P.; Brezina, I. A Follow-up to the Study: Stress and Hair Cortisol Concentrations in Nurses during the First Wave of the COVID-19 Pandemic. Psychoneuroendocrinology 2021, 133, 105434. [Google Scholar] [CrossRef]
- Moya-Albiol, L.; Serrano, M.Á.; Job, A.S. Satisfaction and Cortisol Awakening Response in Teachers Scoring High and Low on. Burn. Spanish J. Psychol. 2010, 13, 629–636. [Google Scholar] [CrossRef]
- Adam, E.K.; Gunnar, M.R. Relationship Functioning and Home and Work Demands Predict Individual Differences in Diurnal Cortisol Patterns in Women. Psychoneuroendocrinology 2001, 26, 189–208. [Google Scholar] [CrossRef]
- Chida, Y.; Hamer, M. Chronic Psychosocial Factors and Acute Physiological Responses to Laboratory-Induced Stress in Healthy Populations: A Quantitative Review of 30 Years of Investigations. Psychol. Bull. 2008, 134, 829–885. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos Ribeiro, S.; Motta, E.A.P. Associação Entre a Síndrome de Burnout e o Hormônio Cortisol. Rev. CiêncSaúde 2014, 16, 87–93. [Google Scholar]
- Pruessner, J.C.; Wolf, O.T.; Hellhammer, D.H.; Buske-Kirschbaum, A.; Von Auer, K.; Jobst, S.; Kaspers, F.; Kirschbaum, C. Free Cortisol Levels after Awakening: A Reliable Biological Marker for the Assessment of Adrenocortical Activity. Life Sci. 1997, 61, 2539–2549. [Google Scholar] [CrossRef] [PubMed]
- Herman, J.P.; McKlveen, J.M.; Ghosal, S.; Kopp, B.; Wulsin, A.; Makinson, R.; Scheimann, J.; Myers, B. Regulation of the Hypothalamic-Pituitary- Adrenocortical Stress Response. Compr. Physiol. 2016, 6, 603–621. [Google Scholar] [CrossRef] [PubMed]
- Duarte, L.L. Cronótipos Humanos; Editora UFRB: Cruz das Almas, Brazil, 2018. [Google Scholar]
- Juruena, M.F.; Cleare, A.J.; Pariante, C.M. The Hypothalamic Pituitary Adrenal Axis, Glucocorticoid Receptor Function and Relevance to Depression. Braz. J. Psychiatry 2004, 26, 189–201. [Google Scholar] [CrossRef]
- Castro, M.; Moreira, A.C. Análise Crítica Do Cortisol Salivar Na Avaliação Do Eixo Hipotálamo-Hipófise-Adrenal. Arq. Bras. Endocrinol. Metabol. 2003, 47, 358–367. [Google Scholar] [CrossRef]
- Bozovic, D.; Racic, M.; Ivkovic, N. Salivary Cortisol Levels as a Biological Marker of Stress Reaction. Med. Arh. 2013, 67, 374–377. [Google Scholar] [CrossRef]
- Streckfus, C.F.; Bigler, L.R. Saliva as a diagnostic fluid. Oral Dis. 2002, 8, 69–76. [Google Scholar] [CrossRef]
- Herman, J.P.; Ostrander, M.M.; Mueller, N.K.; Figueiredo, H. Limbic System Mechanisms of Stress Regulation: Hypothalamo-Pituitary-Adrenocortical Axis. Prog. Neuropsychopharmacol. Biol. Psychiatry 2005, 29, 1201–1213. [Google Scholar] [CrossRef]
- Montaruli, A.; Castelli, L.; Mulè, A.; Scurati, R.; Esposito, F.; Galasso, L.; Roveda, E. Biological Rhythm and Chronotype: New Perspectives in Health. Biomolecules 2021, 11, 487. [Google Scholar] [CrossRef]
- Zerón-Rugerio, M.F.; Díez-Noguera, A.; Izquierdo-Pulido, M.; Cambras, T. Higher Eating Frequency Is Associated with Lower Adiposity and Robust Circadian Rhythms: A Cross-Sectional Study. Am. J. Clin. Nutr. 2021, 113, 17–27. [Google Scholar] [CrossRef]
- Nováková, M.; Sládek, M.; Sumová, A. Human Chronotype Is Determined in Bodily Cells under Real-Life Conditions. Chronobiol. Int. 2013, 30, 607–617. [Google Scholar] [CrossRef]
- Adan, A.; Archer, S.N.; Hidalgo, M.P.; Di Milia, L.; Natale, V.; Randler, C. Circadian Typology: A Comprehensive Review. Chronobiol. Int. 2012, 29, 1153–1175. [Google Scholar] [CrossRef]
- Silva, N.N.; Canova, F.B. Trabalhador vs. Estudante: Comparações Entre a Qualidade de Sono e Cronotipos. Revista Científica UMC 2019, 4. 3, Especial Pibic, 1–5. [Google Scholar]
- Sousa, A.C.B. Padrões de Sono-Vigília Em Estudantes Universitários: Análises Longitudinais Entre Aulas e Exames. Master’s Thesis, University of Coimbra, Coimbra, Portugal, 2018. [Google Scholar]
- López-Soto, P.J.; Fabbian, F.; Cappadona, R.; Zucchi, B.; Manfredini, F.; García-Arcos, A.; Carmona-Torres, J.M.; Manfredini, R.; Rodríguez-Borrego, M.A. Chronotype, Nursing Activity, and Gender: A Systematic Review. J. Adv. Nurs. 2019, 75, 734–748. [Google Scholar] [CrossRef]
- De Castro Corrêa, C.; de Oliveira, F.K.; Pizzamiglio, D.S.; Ortolan, E.V.P.; Weber, S.A.T. Qualidade de Sono Em Estudantes de Medicina: Comparação Das Diferentes Fases Do Curso. J. Bras. Pneumol. 2017, 43, 285–289. [Google Scholar] [CrossRef]
- Torquati, L.; Mielke, G.I.; Brown, W.J.; Burton, N.W.; Kolbe-Alexander, T.L. Shift Work and Poor Mental Health: A Meta-Analysis of Longitudinal Studies. Am. J. Public Health 2019, 109, e13. [Google Scholar] [CrossRef]
- Benedito-Silva, A.A.; Menna-Barreto, L.; Marques, N.; Tenreiro, S. A Self Assessment Questionnaire for the Determination of Morningness-Eveningness Types in Brazil. Prog. Clin. Biol. Res. 1990, 341 Pt B, 89–98. [Google Scholar]
- Sarstedt, A. Catálogo de Produtos. Available online: https://www.sarstedt.com/pt/produtos/diagnostico/salivaexcrecao/product/51.1534.500/ (accessed on 25 November 2022).
- Chiu, S.K.; Collier, C.P.; Clark, A.F.; Wynn-Edwards, K.E. Salivary Cortisol on ROCHE Elecsys Immunoassay System: Pilot Biological Variation Studies. Clin. Biochem. 2003, 36, 211–214. [Google Scholar] [CrossRef]
- Nery, A.L.P.; Baader, W.J. Quimioflorescencia. Quim. Nova 2001, 24, 626–636. [Google Scholar] [CrossRef]
- Miller, R.; Stalder, T.; Jarczok, M.; Almeida, D.M.; Badrick, E.; Bartels, M.; Boomsma, D.I.; Coe, C.L.; Dekker, M.C.J.; Donzella, B.; et al. The CIRCORT Database: Reference Ranges and Seasonal Changes in Diurnal Salivary Cortisol Derived from a Meta-Dataset Comprised of 15 Field Studies. Psychoneuroendocrinology 2016, 73, 16–23. [Google Scholar] [CrossRef]
- Raso, V.; Greve, J.M.D.A.; Polito, M.D. Obesidade No Adulto. In Pollock: Fisiologia Clínica do Exercício; Editora Manole: Sao Paulo, Brazil, 2013; pp. 467–614. [Google Scholar]
- Perreault, L.; Laferrere, B. Overweight and Obesity in Adults: Health Consequences—UpToDate. Uptodate. Available online: https://www.uptodate.com/contents/overweight-and-obesity-in-adults-health-consequences?topicRef=5372&source=see_link (accessed on 2 December 2022).
- Vidotti, V.; Ribeiro, R.P.; Galdino, M.J.Q.; Martins, J.T. Burnout Syndrome and Shift Work among the Nursing Staff. Rev. Lat. Am. Enferm. 2018, 26, 2–6. [Google Scholar] [CrossRef] [PubMed]
- Nogueira, C.J.; Cortez, A.C.L.; de Oliveira Leal, S.M.; Dantas, E.H.M. Recomendações Para a Prática de Exercício Físico Em Face Do COVID-19: Uma Revisão Integrativa. Rev. Bras. De Fisiol. Do Exerc. 2021, 20, 101–124. [Google Scholar] [CrossRef]
- Pereira, A.L.; de Santos, A.H.; Ribeiro, A.C.S.; dos Santos, C.C.; de Sousa Pereira, D.O.; de Sousa, D.; Pereira, E.M.C.; da Mota Pimentel, E.; de Souza Santos, J. Fatores Geradores de Estresse Ocupacional e Seus Impactos Na Saúde Dos Profissionais de Enfermgem Que Atuam Na Linha de Frente Do COVID-19: Uma Revisão Bibliográfica. Enferm. Desafios e Perspect. Para A Integr. Do Cuid. 2021, 1, 190–201. [Google Scholar] [CrossRef]
- De Humerez, D.C.; Ohl, R.I.B.; da Silva, M.C.N. Mental Health of Brazilian Nursing Professionals in the Context of the COVID-19 Pandemic: Action of the Nursing Federal Council. Cogitare Enferm. 2020, 25, e74115. [Google Scholar] [CrossRef]
- Pereira, M.D.; Torres, E.C.; Pereira, M.D.; Antunes, P.F.S.; Costa, C.F.T. Sofrimento Emocional Dos Enfermeiros No Contexto Hospitalar Frente à Pandemia de COVID-19. Res. Soc. Dev. 2020, 9, e67985121. [Google Scholar] [CrossRef]
- Ibar, C.; Fortuna, F.; Gonzalez, D.; Jamardo, J.; Jacobsen, D.; Pugliese, L.; Giraudo, L.; Ceres, V.; Mendoza, C.; Repetto, E.M.; et al. Evaluation of Stress, Burnout and Hair Cortisol Levels in Health Workers at a University Hospital during COVID-19 Pandemic. Psychoneuroendocrinology 2021, 128, 105213. [Google Scholar] [CrossRef]
- Lima da Silva, J.L.; Dos Santos Costa, F.; Ferreira de Souza, R.; De Lyra Sousa, J.; De Souza Oliveira, R. O Ruído Causando Danos e Estresse: Possibilidade de Atuação Para a Enfermagem Do Trabalho. Av. En Enfermería 2014, 32, 124–138. [Google Scholar] [CrossRef]
- Carlotto, M.S. Síndrome de Burnout Em Professores: Prevalência e Fatores Associados. Psicol. Teor. E Pesqui. 2011, 27, 403–410. [Google Scholar] [CrossRef]
- dos Santos, A.A.; Nascimento Sobrinho, C.L. Revisão Sistemática Da Prevalência Da Síndrome de Burnout Em Professores Do Ensino Fundamental e Médio. Rev. Baiana Saúde Pública 2012, 35, 299. [Google Scholar] [CrossRef]
- Da Silva, R.A.D.; Araújo, B.; Morais, C.C.A.; Campos, S.L.; de Andrade, A.D.; Brandão, D.C. Síndrome de Burnout: Realidade Dos Fisioterapeutas Intensivistas? Fisioter. E Pesqui. 2018, 25, 388–394. [Google Scholar] [CrossRef]
- Chati, R.; Huet, E.; Grimberg, L.; Schwarz, L.; Tuech, J.J.; Bridoux, V. Factors Associated with Burnout among French Digestive Surgeons in Training: Results of a National Survey on 328 Residents and Fellows. Am. J. Surg. 2017, 213, 754–762. [Google Scholar] [CrossRef]
- West, C.P.; Dyrbye, L.N.; Shanafelt, T.D. Physician Burnout: Contributors, Consequences and Solutions. J. Intern. Med. 2018, 283, 516–529. [Google Scholar] [CrossRef]
- de Oliveira, A.M.C.; Dantas, L.F.; dos Santos, D.N.R.; Araújo, A.B.; Santos, M.M.A.; de Barroso, B.I.L. Síndrome de Burnout Em Docentes Universitários: Mapeamento e Reflexões Acerca Do Trabalho. Res. Soc. Dev. 2021, 10, e309101220322. [Google Scholar] [CrossRef]
- Bae, S.H.; Fabry, D. Assessing the Relationships between Nurse Work Hours/Overtime and Nurse and Patient Outcomes: Systematic Literature Review. Nurs. Outlook 2014, 62, 138–156. [Google Scholar] [CrossRef]
- De Assis, D.C.; de Resende, D.V.; Marziale, M.H.P. Association between Shift Work, Salivary Cortisol Levels, Stress and Fatigue in Nurses: Integrative Review. Esc. Anna Nery 2018, 22, 2018. [Google Scholar] [CrossRef]
- Bracci, M.; Ciarapica, V.; Copertaro, A.; Barbaresi, M.; Manzella, N.; Tomasetti, M.; Gaetani, S.; Monaco, F.; Amati, M.; Valentino, M.; et al. Peripheral Skin Temperature and Circadian Biological Clock in Shift Nurses after a Day Off. Int. J. Mol. Sci. 2016, 17, 623. [Google Scholar] [CrossRef]
- D’ettorre, G.; Pellicani, V.; Caroli, A.; Greco, M.; D’ettorre, G.; Pellicani, V.; Caroli, A.; Greco, M. Shift Work Sleep Disorder and Job Stress in Shift Nurses: Implications for Preventive Interventions. Med. Lav. 2020, 111, 195–202. [Google Scholar] [CrossRef]
- Anjum, B.; Verma, N.S.; Tiwari, S.; Singh, R.; Mahdi, A.A.; Singh, R.B.; Singh, R.K. Association of Salivary Cortisol with Chronomics of 24 Hours Ambulatory Blood Pressure/Heart Rate among Night Shift Workers. Biosci. Trends 2011, 5, 182–188. [Google Scholar] [CrossRef]
- Kim, K.M.; Han, S.M.; Heo, K.; Kim, W.J.; Chu, M.K. Sex Differences in the Association between Chronotype and Risk of Depression. Sci. Rep. 2020, 10, 18512. [Google Scholar] [CrossRef]
- da Silva, R.M.; Zeitoune, R.C.G.; Beck, C.L.C.; de Martino, M.M.F.; Prestes, F.C.; Loro, M.M. Chronotype and Work Shift in Nursing Workers of University Hospitals. Rev. Bras. Enferm. 2017, 70, 958–964. [Google Scholar] [CrossRef] [PubMed]
- de Souza, S.B.C.; Tavares, J.P.; Macedo, A.B.T.; Moreira, P.W.; Lautert, L. Influência Do Turno de Trabalho e Cronotipo Na Qualidade de Vida Dos Trabalhadores de Enfermagem. Rev. Gaúcha Enferm. 2012, 33, 79–85. [Google Scholar] [CrossRef] [PubMed]
- Cappuccio, F.P.; Cooper, D.; Delia, L.; Strazzullo, P.; Miller, M.A. Sleep Duration Predicts Cardiovascular Outcomes: A Systematic Review and Meta-Analysis of Prospective Studies. Eur. Heart J. 2011, 32, 1484–1492. [Google Scholar] [CrossRef] [PubMed]
- Paudel, M.L.; Taylor, B.C.; Ancoli-Israel, S.; Stone, K.L.; Tranah, G.; Redline, S.; Barrett-Connor, E.; Stefanick, M.L.; Ensrud, K.E. Rest/Activity Rhythms and Cardiovascular Disease in Older Men. Chronobiol. Int. 2011, 28, 258–266. [Google Scholar] [CrossRef]
- Jackson, C.L.; Redline, S.; Kawachi, I.; Hu, F. Association between Sleep Duration and Diabetes in Black and White Adults. Diabetes Care 2013, 36, 3557–3565. [Google Scholar] [CrossRef]
- Vitale, J.A.; Bonato, M.; Galasso, L.; La Torre, A.; Merati, G.; Montaruli, A.; Roveda, E.; Carandente, F. Sleep Quality and High Intensity Interval Training at Two Different Times of Day: A Crossover Study on the Influence of the Chronotype in Male Collegiate Soccer Players. Chronobiol. Int. 2017, 34, 260–268. [Google Scholar] [CrossRef]
- Aita, M.; Héon, M.; Lavallée, A.; De Clifford Faugère, G.; Altit, G.; Le May, S.; Dorval, V.; Lippé, S.; Larone Juneau, A.; Remmer, E.; et al. Nurturing and Quiet Intervention (NeuroN-QI) on Preterm Infants’ Neurodevelopment and Maternal Stress and Anxiety: A Pilot Randomized Clinical Trial Protocol. J. Adv. Nurs. 2021, 77, 3192–3203. [Google Scholar] [CrossRef]

| Parameter | Sample (n = 256) |
|---|---|
| Age, years (n = 251) | 39.4 ± 9.8 |
| Gender (n = 256) | |
| Male | 13 (5.1) |
| Female | 243 (94.9) |
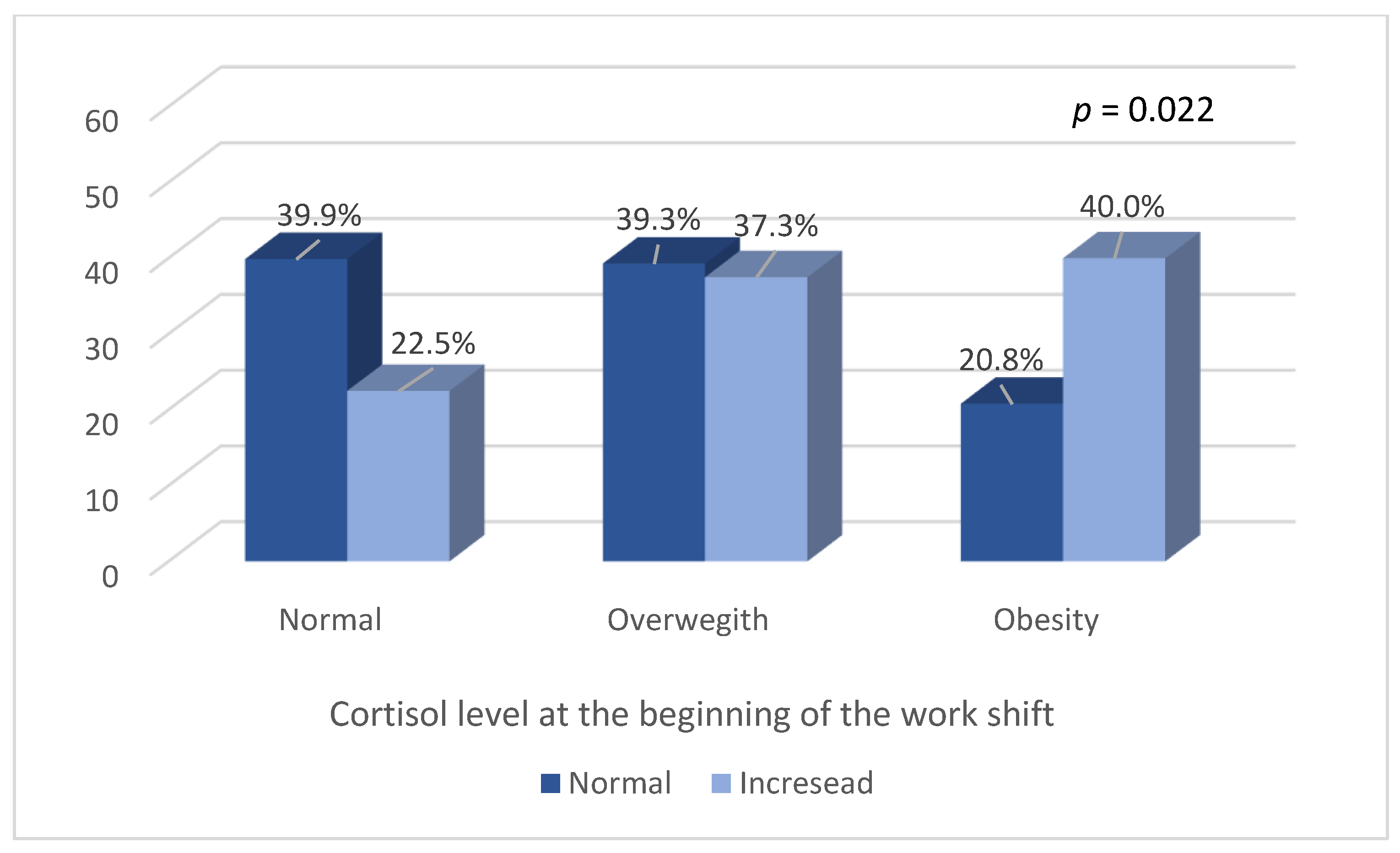
| Body Mass Index (n = 244) | |
| Mild thinness | 1 (0.4) |
| Normal | 89 (36.5) |
| Overweight | 94 (38.5) |
| Obese | 60 (24.6) |
| Marital status (n = 251) | |
| Married | 130 (51.8) |
| Stable union | 21 (8.4) |
| Single | 83 (33.1) |
| Divorced | 17 (6.8) |
| Children (n = 251) | |
| Yes | 163 (64.9) |
| No | 88 (35.1) |
| How many children (n = 163) | |
| 1 to 2 | 131 (80.4) |
| 3 or more | 32 (19.6) |
| Schooling (n = 251) | |
| Middle level | 78 (31.1) |
| Higher level | 67 (26.7) |
| Postgraduate | 105 (41.8) |
| Function (n = 251) | |
| Doctor | 57 (22.7) |
| Nurse | 48 (19.1) |
| Nursing technician | 130 (51.8) |
| Physiotherapist or Speech Therapist | 16 (6.4) |
| Time working in NICU (n = 251) | |
| Less than 5 years | 105 (41.8) |
| 5 to 10 years | 43 (17.1) |
| 10 to 20 years | 86 (34.3) |
| 20 years or more | 17 (6.8) |
| Disease (n = 251) | |
| Yes | 107 (42.6) |
| No | 144 (57.4) |
| Medication (n = 247) | |
| Yes | 91 (36,8) |
| No | 156 (63.2) |
| Smoking (n = 251) | |
| Yes | 4 (1.6) |
| No | 247 (98.4) |
| Alcohol (n = 251) | |
| Yes | 76 (30.3) |
| No | 175 (69.7) |
| Physical activity (n = 250) | |
| Yes | 96 (38.4) |
| No | 154 (61.6) |
| Intensity of physical activity (n = 84) | |
| Mild | 121 (25) |
| Moderately | 55 (65.5) |
| Intense | 8 (9.5) |
| Characteristics | Sample (n = 256) |
|---|---|
| Place (n = 256) | |
| Hospital 1 | 24 (9.4) |
| Hospital 2 | 103 (40.2) |
| Hospital 3 | 85 (33.2) |
| Hospital 4 | 44 (17.2) |
| Type and duration of work shift (n = 256) | |
| Morning—6 h | 35 (13.7) |
| Afternoon—6 h | 23 (9.0) |
| Daytime—12 h | 109 (42.6) |
| Nighttime—12 h | 89 (34.8) |
| Time spent commuting (min) (n = 249) | |
| <30 | 95 (38.2) |
| 30–60 | 105 (42.2) |
| 61 or more | 49 (19.7) |
| Having another job (n = 250) | |
| Yes | 92 (36.8) |
| No | 158 (63.2) |
| Coming to work from another job (n = 251) | |
| Yes | 40 (15.9) |
| No | 211 (84.1) |
| Continuous hours of work (n = 36) | |
| 6 h | 6 (16.7) |
| 12 h | 11 (30.6) |
| 18 h | 8 (22.2) |
| 24 h | 11 (30.6) |
| Self-perception of physical state at the beginning of the shift (n = 243) | |
| Very tired | 25 (10.3) |
| A little tired | 130 (53.5) |
| Rested | 88 (36.2) |
| Self-perception of physical state at the end of the shift (n = 227) | |
| Very tired | 81 (35.7) |
| A little tired | 103 (45.4) |
| Rested | 43 (18.9) |
| Eventful occurrences during the shift (n = 232) | |
| Yes | 83 (35.8) |
| No | 149 (64.2) |
| Type of eventful occurrences during the shift (n = 70) | |
| Death | 10 (14.3) |
| Reanimation | 13 (18.6) |
| Admission | 11 (15.7) |
| Intubation | 8 (11.4) |
| Critical ones | 28 (40) |
| Do you find the shift tiring? (n = 203) | |
| Yes | 118 (58.1) |
| No | 85 (41.9) |
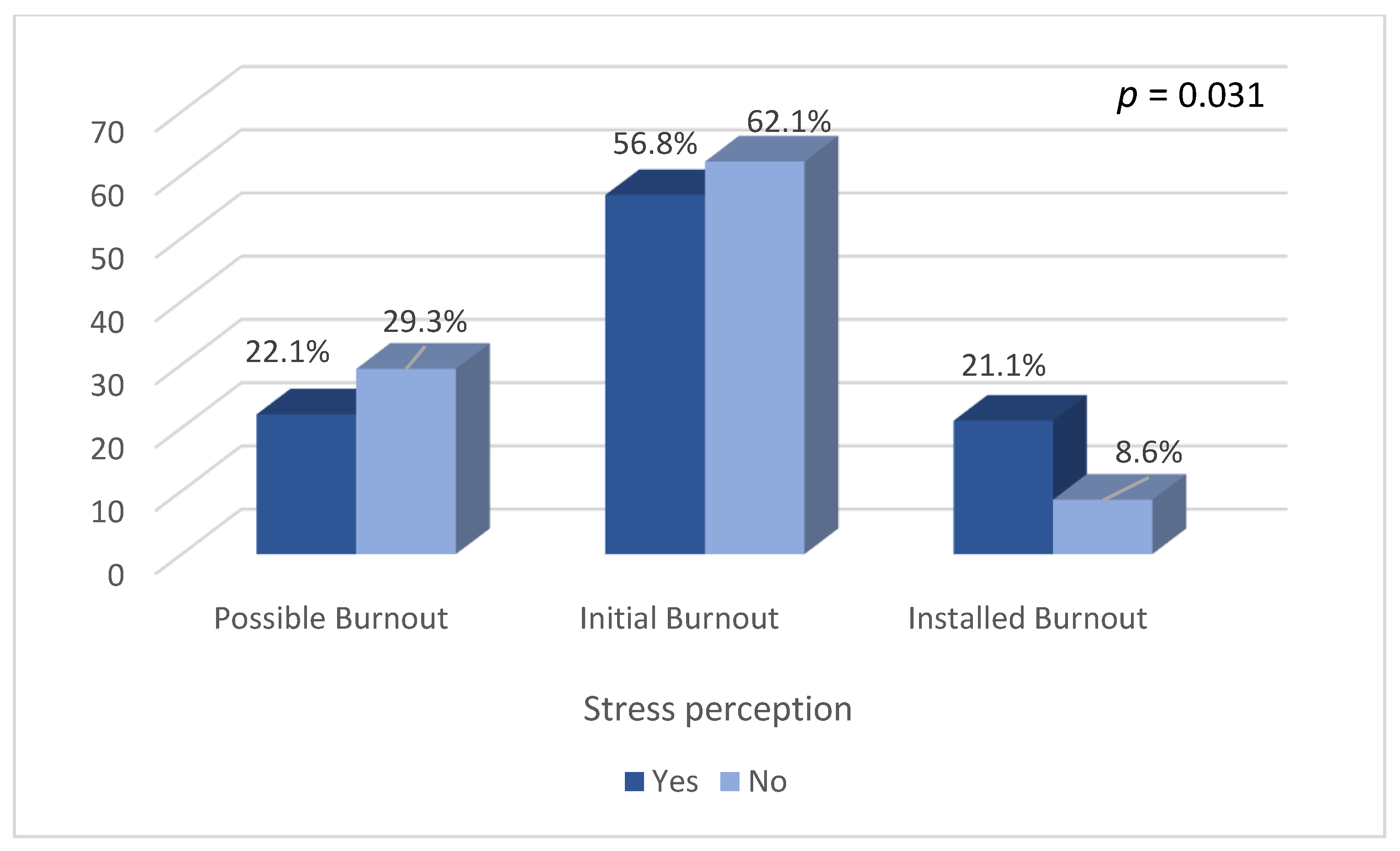
| Do you find the shift stressful? (n = 197) | |
| Yes | 93 (47.2) |
| No | 104 (52.8) |
| Cortisol levels (µg/dL) at beginning of shift (n = 225) | 0.19 (0.11–0.36) |
| Normal | 181 (80.4) |
| Increased | 44 (19.6) |
| Cortisol levels (µg/dL) at end of shift (n = 230) | 0.07 (0.05–0.11) |
| Normal | 222 (96.5) |
| Increased | 8 (3.5) |
| Occurrence of Burnout Syndrome (n = 246) | |
| Possible occurence | 64 (26) |
| Initial phase of Burnout | 145 (59) |
| Installed Burnout | 37 (15) |
| Chronotype (n = 244) | |
| Evening | 17 (7) |
| Intermediate | 114 (46.7) |
| Morning | 113 (46.3) |
| Chronotype Classification | ||||
|---|---|---|---|---|
| Evening (n = 17) | Intermediate (n = 114) | Morning (n = 113) | p | |
| Age (years) | 36 ± 12 | 37 ± 9 | 43 ± 10 | <0.001 a |
| Gender | 0.032 | |||
| Male | 3 (17.6) | 7 (6.1) | 3 (2.7) | |
| Female | 14 (82.4) | 107 (93.9) | 110 (97.3) | |
| Marital Status | 0.014 | |||
| Married | 6 (35.3) | 52 (45.6) | 69 (61.1) | |
| Stable union | 2 (11.8) | 9 (7.9) | 10 (8.8) | |
| Single | 5 (29.4) | 46 (40.4) | 29 (25.7) | |
| Divorced | 4 (23.5) | 7 (6.1) | 5 (4.4) | |
| Have Children | 8 (47.1) | 65 (57) | 83 (73.5) | 0.030 |
| Number of children | 0.051 | |||
| 0 | 9 (52.9) | 47 (42) | 25 (22.9) | |
| 1 to 2 | 7 (41.2) | 54 (48.3) | 64 (58.7) | |
| 3 or more | 1 (5.9) | 11 (9.8) | 20 (18.3) | |
| Financial Dependency | 6 (35.3) | 53 (46.9) | 62 (56.4) | 0.160 |
| Education level | 0.783 | |||
| Postgraduate studies | 8 (47.1) | 43 (37.7) | 52 (46.1) | |
| Higher | 3 (17.7) | 31 (27.2) | 31 (27.5) | |
| High School/Technical | 6 (35.3) | 43 (34.2) | 30 (26.6) | |
| Function | 0.608 | |||
| Doctor | 3 (17.6) | 23 (20.2) | 30 (26.5) | |
| Nurse | 4 (23.5) | 21 (18.4) | 21 (18.6) | |
| nursing technician | 9 (52.9) | 65 (57) | 52 (46) | |
| Physiotherapist and Speech Therapist | 1 (5.9) | 5 (4.4) | 10 (8.8) | |
| Work experience in NICU | 0.025 | |||
| Less than 5 years | 8 (47.1) | 56 (49.1) | 38 (33.6) | |
| 5 to 10 years | 1 (5.9) | 22 (19.3) | 19 (16.8) | |
| 10 to 20 years | 6 (35.3) | 34 (29.8) | 43 (38.1) | |
| More than 20 years | 2 (11.8) | 2 (1.8) | 13 (11.5) | |
| Chronotype Classification | ||||
|---|---|---|---|---|
| Evening (n = 17) | Intermediate (n = 114) | Morning (n = 113) | p | |
| Burnout rating a | 0.316 | |||
| Possible Burnout | 1 (5.9) | 30 (26.3) | 33 (29.7) | |
| Initial Burnout | 12 (70.6) | 68 (59.6) | 61 (55) | |
| Installed Burnout | 4 (23.5) | 16 (14) | 17 (15.3) | |
| Initial cortisol rating a | 0.027 | |||
| Normal | 13 (81.3) | 75 (72.8) | 87 (87.9) | |
| Changed | 3 (18.8) | 28 (27.2) | 12 (12.1) | |
| Final cortisol rating a | 0.608 | |||
| Normal | 15 (93.8) | 103 (97.2) | 100 (98) | |
| Changed | 1 (6.3) | 3 (2.8) | 2 (2) | |
| Cortisol dosage at the beginning of the shift (µg/dL) b | 0.19 (0.13–0.55) | 0.21 (0.13–0.42) | 0.16 (0.11–0.29) | 0.069 |
| Cortisol dosage at the end of the shift (µg/dL) b | 0.07 (0.05–0.12) | 0.07 (0.05–0.12) | 0.07 (0.05–0.1) | 0.713 |
| Cortisol variation during the shift (µg/dL) b | −0.08 (−0.37–−0.03) | −0.13 (−0.34–−0.03) | −0.09 (−0.19–−0.03) | 0.153 |
| Unfavorable Chronotype | p | ||
|---|---|---|---|
| No (n = 214) | Yes (n = 30) | ||
| Burnout Rating a | 0.226 | ||
| Possible | 55 (25.8) | 9 (31) | |
| Initial Burnout | 128 (60.1) | 13 (44.8) | |
| Installed Burnout | 30 (14.1) | 7 (24.1) | |
| Physical state—Tired at the start? a | 0.761 | ||
| Very | 20 (9.8) | 4 (14.3) | |
| A little | 108 (52.7) | 14 (50) | |
| Rested | 77 (37.6) | 10 (35.7) | |
| Physical state—Tired at the end? a | 0.410 | ||
| Very | 70 (37) | 10 (35.7) | |
| A little | 81 (42.9) | 15 (53.6) | |
| Rested | 38 (20.1) | 3 (10.7) | |
| Eventful occurances on duty a | 73 (37.2) | 9 (33.3) | 0.693 |
| Tiring duty | 109 (57.4) | 14 (53.8) | 0.734 |
| Stressful shift | 86 (46.2) | 9 (39.1) | 0.518 |
| Initial cortisol a | 0.013 | ||
| Normal | 160 (82.9) | 15 (60) | |
| Changed | 33 (17.1) | 10 (40) | |
| Final cortisol rating a | 0.527 | ||
| Normal | 193 (97.5) | 25 (96.2) | |
| Changed | 5 (2.5) | 1 (3.8) | |
| Cortisol dosage at the beginning of the shift (µg/dL) b | 0.18 (0.11–0.31) | 0.33 (0.18–0.60) | 0.006 |
| Cortisol dosage at the end of the shift (µg/dL) b | 0.07 (0.05–0.11) | 0.09 (0.05–0.13) | 0.382 |
| Cortisol variation during the shift (µg/dL) b | −0.10 (−0.21–−0.03) | −0.20 (−0.48–−0.06) | 0.06 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Azevedo Bringel, J.M.; Abreu, I.; Muniz, M.-C.M.C.; de Almeida, P.C.; Silva, M.-R.G. Health Professionals’ Chronotype Association with Salivary Cortisol and Occupational Stress in Neonatal Intensive Care Units. Int. J. Environ. Res. Public Health 2023, 20, 5683. https://doi.org/10.3390/ijerph20095683
de Azevedo Bringel JM, Abreu I, Muniz M-CMC, de Almeida PC, Silva M-RG. Health Professionals’ Chronotype Association with Salivary Cortisol and Occupational Stress in Neonatal Intensive Care Units. International Journal of Environmental Research and Public Health. 2023; 20(9):5683. https://doi.org/10.3390/ijerph20095683
Chicago/Turabian Stylede Azevedo Bringel, Jocélia Maria, Isabel Abreu, Maria-Cláudia Mendes Caminha Muniz, Paulo César de Almeida, and Maria-Raquel G. Silva. 2023. "Health Professionals’ Chronotype Association with Salivary Cortisol and Occupational Stress in Neonatal Intensive Care Units" International Journal of Environmental Research and Public Health 20, no. 9: 5683. https://doi.org/10.3390/ijerph20095683
APA Stylede Azevedo Bringel, J. M., Abreu, I., Muniz, M.-C. M. C., de Almeida, P. C., & Silva, M.-R. G. (2023). Health Professionals’ Chronotype Association with Salivary Cortisol and Occupational Stress in Neonatal Intensive Care Units. International Journal of Environmental Research and Public Health, 20(9), 5683. https://doi.org/10.3390/ijerph20095683







