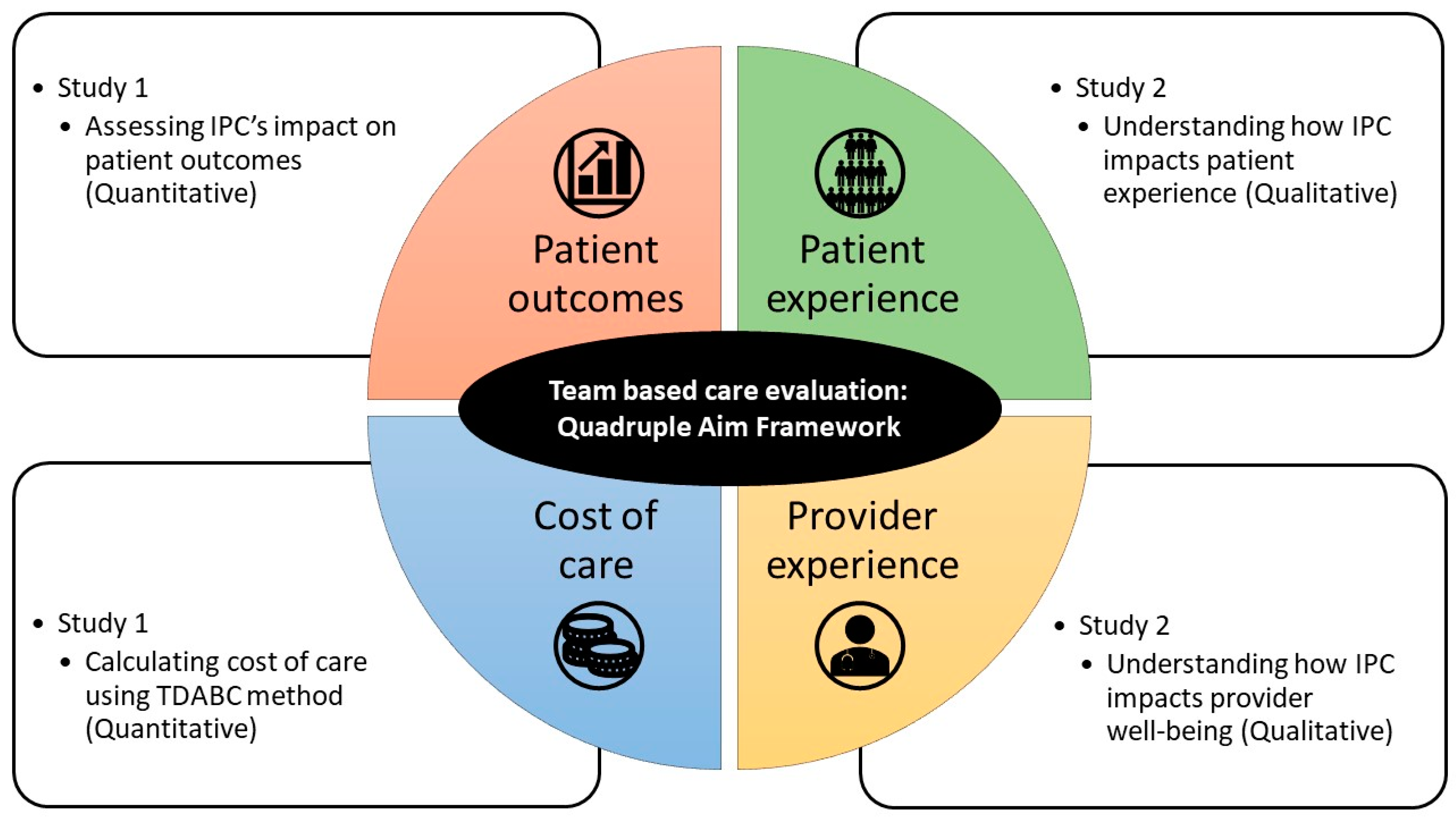
Measuring Interprofessional Collaboration’s Impact on Healthcare Services Using the Quadruple Aim Framework: A Protocol Paper
Abstract
1. Introduction
1.1. Conceptual Framework and Operationalization Issues
1.2. Complex Problem Requiring Multimethod Approach
1.3. Aims of Research Protocol
2. Methods
2.1. Study Setting
2.2. Selection of IPC Teams to Study
2.3. Study 1 Design: Assessing IPC’s Impact on Patient Outcomes and Cost of Care
2.3.1. Design
2.3.2. Study Sample
2.3.3. Measurements and Data Collection Plan
2.3.4. Analysis Plan
2.4. Study 2 Design: Understanding How IPC Impacts Patient Experience and Provider Well-Being
2.4.1. Sampling and Recruitment
2.4.2. Data Collection Plan
2.4.3. Analysis Plan
2.5. Effect of the COVID-19 Pandemic on Data Collection
3. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Martin, J.; Ummenhofer, W.; Manser, T.; Spirig, R. Interprofessional collaboration among nurses and physicians: Making a difference in patient outcome. Swiss Med. Wkly. 2010. [Google Scholar] [CrossRef]
- Reeves, S.; Pelone, F.; Harrison, R.; Goldman, J.; Zwarenstein, M. Interprofessional collaboration to improve professional practice and healthcare outcomes. Cochrane Database Syst. Rev. 2017, 11, 6. [Google Scholar] [CrossRef] [PubMed]
- Cox, M.; Cuff, P.; Brandt, B.; Reeves, S.; Zierler, B. Measuring the impact of interprofessional education on collaborative practice and patient outcomes. J. Interpr. Care 2016, 30, 1–3. [Google Scholar] [CrossRef]
- Institute of Medicine. Measuring the Impact of Interprofessional Education on Collaborative Practice and Patient Outcomes; National Academies Press: Washington, DC, USA, 2015. [Google Scholar]
- Berwick, D.M.; Nolan, T.W.; Whittington, J. The triple aim: Care, health, and cost. Health Aff. 2008, 27, 759–769. [Google Scholar] [CrossRef]
- Brandt, B.; Lutfiyya, M.N.; King, J.A.; Chioreso, C. A scoping review of interprofessional collaborative practice and education using the lens of the triple aim. J. Interpr. Care 2014, 28, 393–399. [Google Scholar] [CrossRef] [PubMed]
- Bodenheimer, T.; Sinsky, C. From triple to quadruple aim: Care of the patient requires care of the provider. Ann. Fam. Med. 2014, 12, 573–576. [Google Scholar] [CrossRef] [PubMed]
- Pomare, C.; Long, J.C.; Churruca, K.; Ellis, L.A.; Braithwaite, J. Interprofessional collaboration in hospitals: A critical, broad-based review of the literature. J. Interpr. Care 2020, 34, 509–519. [Google Scholar] [CrossRef] [PubMed]
- Arling, P.A.; Abrahamson, K.; Miech, E.J.; Inui, T.S.; Arling, G. Communication and effectiveness in a US nursing home quality-improvement collaborative. Nurs. Health Sci. 2014, 16, 291–297. [Google Scholar] [CrossRef]
- Anderegg, M.D.; Gums, T.H.; Uribe, L.; Coffey, C.S.; James, P.A.; Carter, B.L. Physician–pharmacist collaborative management. Hypertension 2016, 68, 1314–1320. [Google Scholar] [CrossRef]
- Dixon, D.L.; Sisson, E.M.; Parod, E.D.; Van Tassell, B.W.; Nadpara, P.A.; Carl, D.; W. Dow, A. Pharmacist-physician collaborative care model and time to goal blood pressure in the uninsured population. J. Clin. Hypertens. 2018, 20, 88–95. [Google Scholar] [CrossRef]
- Matzke, G.R.; Moczygemba, L.R.; Williams, K.J.; Czar, M.J.; Lee, W.T. Impact of a pharmacist–physician collaborative care model on patient outcomes and health services utilization. Am. J. Heal. Pharm. 2018, 75, 1039–1047. [Google Scholar] [CrossRef]
- Sisson, E.M.; Dixon, D.L.; Kildow, D.C.; Van Tassell, B.W.; Carl, D.E.; Varghese, D.; Electricwala, B.; Carroll, N.V. Effectiveness of a pharmacist-physician team-based collaboration to improve long-term blood pressure control at an inner-city safety-net clinic. Pharmacother. J. Hum. Pharmacol. Drug Ther. 2016, 36, 342–347. [Google Scholar] [CrossRef] [PubMed]
- Nagelkerk, J.; Thompson, M.E.; Bouthillier, M.; Tompkins, A.; Baer, L.J.; Trytko, J.; Booth, A.; Stevens, A.; Groeneveld, K. Improving outcomes in adults with diabetes through an interprofessional collaborative practice program. J. Interpr. Care 2018, 32, 4–13. [Google Scholar] [CrossRef] [PubMed]
- Shrader, S.; Jernigan, S.; Nazir, N.; Zaudke, J. Determining the impact of an interprofessional learning in practice model on learners and patients. J. Interpr. Care 2018, 1–8. [Google Scholar] [CrossRef]
- O’Leary, K.J.; Killarney, A.; Hansen, L.O.; Jones, S.; Malladi, M.; Marks, K.; M Shah, H. Effect of patient-centred bedside rounds on hospitalised patients’ decision control, activation and satisfaction with care. BMJ Qual. Saf. 2016, 25, 921–928. [Google Scholar] [CrossRef]
- Meyers, D.J.; Chien, A.T.; Nguyen, K.H.; Li, Z.; Singer, S.J.; Rosenthal, M.B. Association of team-based primary care with health care utilization and costs among chronically Ill patients. JAMA Intern. Med. 2019, 179, 54. [Google Scholar] [CrossRef]
- Anderson, J.E.; Lavelle, M.; Reedy, G. Understanding adaptive teamwork in health care: Progress and future directions. J. Health Serv. Res. Policy. 2021, 28, 208–214. [Google Scholar] [CrossRef]
- Todres, L.; Galvin, K.T.; Holloway, I. The humanization of healthcare: A value framework for qualitative research. Int. J. Qual. Stud. Health Well-being 2009, 4, 68–77. [Google Scholar] [CrossRef]
- Arana, M.; Harper, L.; Qin, H.; Mabrey, J. Reducing length of stay, direct cost, and readmissions in total joint arthroplasty patients with an outcomes manager-led interprofessional team. Orthop. Nurs. 2017, 36, 279–284. [Google Scholar] [CrossRef]
- Madan, A.; Borckardt, J.J.; Barth, K.S.; Romagnuolo, J.; Morgan, K.A.; Adams, D.B. Interprofessional collaborative care reduces excess service utilization among individuals with chronic pancreatitis. J. Healthc. Qual. 2013, 35, 41–46. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, R.S.; Anderson, S.R. Time-driven activity-based costing. Harv. Bus. Rev. 2004, 82, 131–138. [Google Scholar] [CrossRef] [PubMed]
- Martin, J.A.; Mayhew, C.R.; Morris, A.J.; Bader, A.M.; Tsai, M.H.; Urman, R.D. Using time-driven activity-based costing as a key component of the value platform: A pilot analysis of colonoscopy, aortic valve replacement and carpal tunnel release procedures. J. Clin. Med. Res. 2018, 10, 314–320. [Google Scholar] [CrossRef]
- Patton, M.Q. Qualitative Research & Evaluation Methods: Integrating Theory and Practice, 4th ed.; SAGE Publications: Thousand Oaks, CA, USA, 2014. [Google Scholar]
- Bradley, E.H.; Curry, L.A.; Ramanadhan, S.; Rowe, L.; Nembhard, I.M.; Krumholz, H.M. Research in action: Using positive deviance to improve quality of health care. Implement. Sci. 2009, 4, 25. [Google Scholar] [CrossRef] [PubMed]
- Rose, A.J.; McCullough, M.B. A practical guide to using the positive deviance method in health services research. Health Serv. Res. 2017, 52, 1207–1222. [Google Scholar] [CrossRef]
- Foo, Y.Y.; Tan, K.; Rao, J.; Lim, W.S.; Xin, X.; Cheng, Q.; Lum, E.; Tan, N.C. Viewing interprofessional collaboration through the lens of networked ecological systems theory. J. Interpr. Care 2022, 36, 777–785. [Google Scholar] [CrossRef]
- Antonacci, G.; Lennox, L.; Barlow, J.; Evans, L.; Reed, J. Process mapping in healthcare: A systematic review. BMC Health Serv. Res. 2021, 21, 342. [Google Scholar] [CrossRef]
- Rubin, H.J.; Rubin, I.S. Qualitative Interviewing: The Art of Hearing Data; SAGE Publications: Thousand Oaks, CA, USA, 2012. [Google Scholar]
- Kendall, M.; Murray, S.A.; Carduff, E.; Worth, A.; Harris, F.; Lloyd, A.; Cavers, D.; Grant, L.; Boyd, K.; Sheikh, A. Use of multiperspective qualitative interviews to understand patients’ and crers’ beliefs, experiences, and needs. Natl. Libr. Med. 2009, 339, 122. [Google Scholar] [CrossRef]
- Pinnock, H.; Kendall, M.; Murray, S.A.; Worth, A.; Levack, P.; Porter, M.; MacNee, W.; Sheikh, A. Living and dying with severe chronic obstructive pulmonary disease: Multi-perspective longitudinal qualitative study. Support. Palliat. Care 2011, 1, 174–183. [Google Scholar] [CrossRef]
- Lingard, L.A.; McDougall, A.; Schulz, V.; Shadd, J.; Marshall, D.; Strachan, P.H.; Tait, G.R.; Arnold, J.M.; Kimel, G. Understanding palliative care on the heart failure care team: An innovative research methodology. J. Pain Symptom Manage. 2013, 45, 901–911. [Google Scholar] [CrossRef] [PubMed]
- Lingard, L.; Sue-Chue-Lam, C.; Tait, G.R.; Bates, J.; Shadd, J.; Schulz, V. Pulling together and pulling apart: Influences of convergence and divergence on distributed healthcare teams. Adv. Heal. Sci. Educ. 2017, 22, 1085–1099. [Google Scholar] [CrossRef]
- Marcus-Aiyeku, U.; DeBari, M.; Salmond, S. Assessment of the patient-centered and family-centered care experience of total joint replacement patients using a shadowing technique. Orthop. Nurs. 2015, 34, 269–277. [Google Scholar] [CrossRef] [PubMed]
- Wilson, J.W.; Baer, R.D.; Villalona, S. Patient shadowing: A useful research method, teaching tool, and approach to student professional development for premedical undergraduates. Acad. Med. 2019, 94, 1722–1727. [Google Scholar] [CrossRef] [PubMed]
- Paradis, E.; Sutkin, G. Beyond a good story: From Hawthorne effect to reactivity in health professions education research. Med. Edu. 2017, 51, 31–39. [Google Scholar] [CrossRef]
- Gum, L.F.; Sweet, L.; Greenhill, J.; Prideaux, D. Exploring interprofessional education and collaborative practice in Australian rural health services. J. Interpr. Care 2020, 34, 173–183. [Google Scholar] [CrossRef] [PubMed]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Willig, C.; Rogers, W.S. The SAGE Handbook of Qualitative Research in Psychology; SAGE Publications Ltd: Thousand Oaks, CA, USA, 2017; pp. 17–37. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Foo, Y.Y.; Xin, X.; Rao, J.; Tan, N.C.K.; Cheng, Q.; Lum, E.; Ong, H.K.; Lim, S.M.; Freeman, K.J.; Tan, K. Measuring Interprofessional Collaboration’s Impact on Healthcare Services Using the Quadruple Aim Framework: A Protocol Paper. Int. J. Environ. Res. Public Health 2023, 20, 5704. https://doi.org/10.3390/ijerph20095704
Foo YY, Xin X, Rao J, Tan NCK, Cheng Q, Lum E, Ong HK, Lim SM, Freeman KJ, Tan K. Measuring Interprofessional Collaboration’s Impact on Healthcare Services Using the Quadruple Aim Framework: A Protocol Paper. International Journal of Environmental Research and Public Health. 2023; 20(9):5704. https://doi.org/10.3390/ijerph20095704
Chicago/Turabian StyleFoo, Yang Yann, Xiaohui Xin, Jai Rao, Nigel C. K. Tan, Qianhui Cheng, Elaine Lum, Hwee Kuan Ong, Sok Mui Lim, Kirsty J. Freeman, and Kevin Tan. 2023. "Measuring Interprofessional Collaboration’s Impact on Healthcare Services Using the Quadruple Aim Framework: A Protocol Paper" International Journal of Environmental Research and Public Health 20, no. 9: 5704. https://doi.org/10.3390/ijerph20095704
APA StyleFoo, Y. Y., Xin, X., Rao, J., Tan, N. C. K., Cheng, Q., Lum, E., Ong, H. K., Lim, S. M., Freeman, K. J., & Tan, K. (2023). Measuring Interprofessional Collaboration’s Impact on Healthcare Services Using the Quadruple Aim Framework: A Protocol Paper. International Journal of Environmental Research and Public Health, 20(9), 5704. https://doi.org/10.3390/ijerph20095704





