Exploring Future Signals of COVID-19 and Response to Information Diffusion Using Social Media Big Data
Abstract
1. Introduction
2. Materials and Methods
2.1. Data
2.2. Text Mining
2.3. Future Signal Analysis
- NN: total number of documents;
- TF: term frequency;
- DF: document frequency;
- tw: time weight (time weight of 0.05 was applied);
- n: entire time segment;
- j: time point;
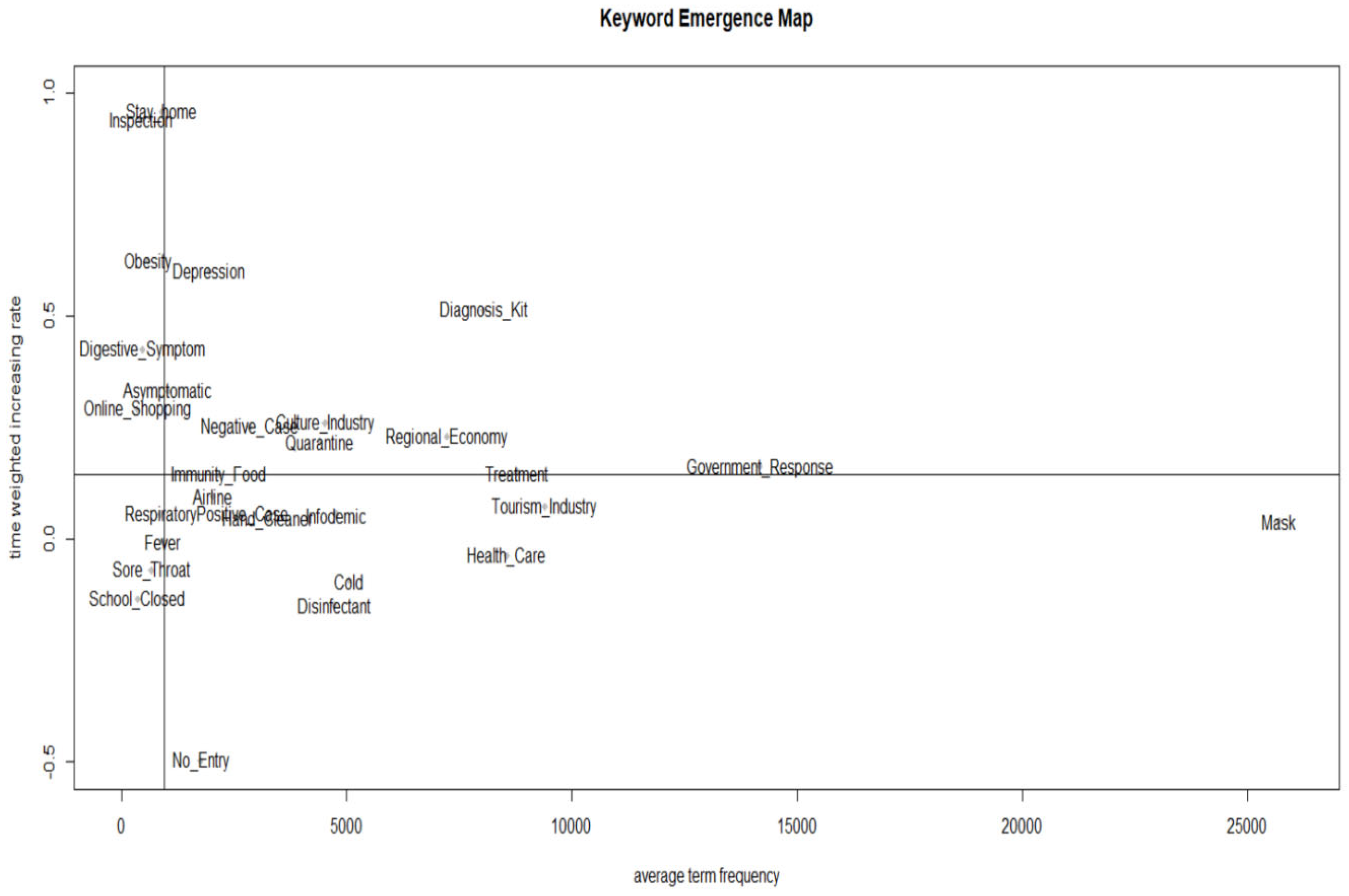
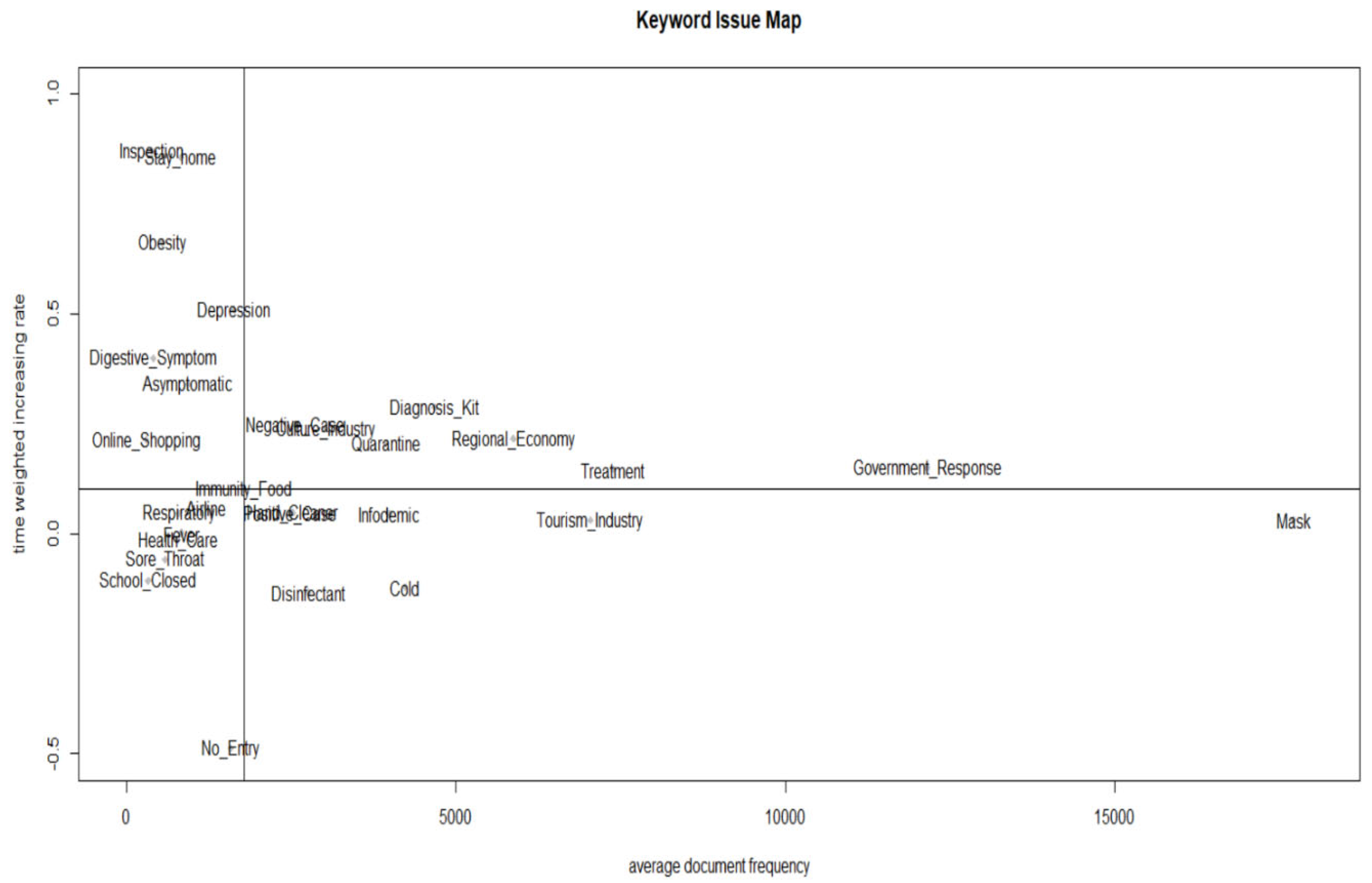
- “{1 − tw × (n − j)}” is a function that weakens its influence as time passes, thus determining the scale of the time weight [37]. Keyword emergence map (KEM) and Keyword Issue Map (KIM) were examined by visualizing the frequency of emergence and the time-weighted rate of the increase in topics [35,37].
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Liu, P.L. COVID-19 Information Seeking on Digital Media and Preventive Behaviors: The Mediation Role of Worry. Cyberpsychology Behav. Soc. Netw. 2020, 23, 677–682. [Google Scholar] [CrossRef] [PubMed]
- Guan, W.-J.; Ni, Z.-Y.; Hu, Y.; Liang, W.; Ou, C.; He, J.; Liu, L.; Shan, H.; Lei, C.; Hui, D.; et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef] [PubMed]
- Chen, N.; Zhou, M.; Dong, X.; Qu, J.; Gong, F.; Han, Y.; Qiu, Y.; Wang, J.; Liu, Y.; Wei, Y.; et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 2020, 395, 507–513. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Coronavirus. Available online: www.who.int/health-topics/coronavirus#tab=tab1 (accessed on 12 August 2020).
- Pan, L.; Mu, M.; Yang, P.; Sun, Y.; Wang, R.; Yan, J.; Li, P.; Hu, B.; Wang, J.; Hu, C.; et al. Clinical Characteristics of COVID-19 Patients with Digestive Symptoms in Hubei, China: A Descriptive, Cross-Sectional, Multicenter Study. Am. J. Gastroenterol. 2020, 115, 766–773. [Google Scholar] [CrossRef]
- Carfì, A.; Bernabei, R.; Landi, F. Group ftGAC-P-ACS. Persistent Symptoms in Patients After Acute COVID-19. JAMA 2020, 324, 603–605. [Google Scholar] [CrossRef]
- Tian, S.; Hu, N.; Lou, J.; Chen, K.; Kang, X.; Xiang, Z.; Chen, H.; Wang, D.; Liu, N.; Liu, D.; et al. Characteristics of COVID-19 infection in Beijing. J. Infect. 2020, 80, 401–406. [Google Scholar] [CrossRef]
- Ji, W.; Huh, K.; Kang, M.; Hong, J.; Bae, G.H.; Lee, R.; Na, Y.; Choi, H.; Gong, S.Y.; Choi, Y.-H.; et al. Effect of Underlying Comorbidities on the Infection and Severity of COVID-19 in Korea: A Nationwide Case-Control Study. J. Korean Med. Sci. 2020, 35, e237. [Google Scholar] [CrossRef]
- Christensen, D.M.; Strange, J.E.; Gislason, G.; Torp-Pedersen, C.; Gerds, T.; Fosbøl, E.; Phelps, M. Charlson Comorbidity Index Score and Risk of Severe Outcome and Death in Danish COVID-19 Patients. J. Gen. Intern. Med. 2020, 35, 2801–2803. [Google Scholar] [CrossRef]
- Guan, W.-J.; Liang, W.-H.; Zhao, Y.; Liang, H.-R.; Chen, Z.-S.; Li, Y.-M.; Liu, X.-Q.; Chen, R.-C.; Tang, C.-L.; Wang, T.; et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: A nationwide analysis. Eur. Respir. J. 2020, 55, 2000547. [Google Scholar] [CrossRef]
- Salathé, M.; Kazandjieva, M.; Lee, J.W.; Levis, P.; Feldman, M.W.; Jones, J.H. A high-resolution human contact network for infectious disease transmission. Proc. Natl. Acad. Sci. USA 2010, 107, 22020–22025. [Google Scholar] [CrossRef]
- He, S.; Peng, Y.; Sun, K. SEIR modeling of the COVID-19 and its dynamics. Nonlinear Dyn. 2020, 101, 1667–1680. [Google Scholar] [CrossRef] [PubMed]
- Abou-Ismail, A. Compartmental Models of the COVID-19 Pandemic for Physicians and Physician-Scientists. SN Compr. Clin. Med. 2020, 2, 852–858. [Google Scholar] [CrossRef] [PubMed]
- Block, P.; Hoffman, M.; Raabe, I.J.; Dowd, J.B.; Rahal, C.; Kashyap, R.; Mills, M.C. Social network-based distancing strategies to flatten the COVID-19 curve in a post-lockdown world. Nat. Hum. Behav. 2020, 4, 588–596. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.Y. COVID-19 in South Korea. Postgrad. Med. J. 2020, 96, 399–402. [Google Scholar] [CrossRef]
- Noh, J.Y.; Seong, H.; Yoon, J.G.; Song, J.Y.; Cheong, H.J.; Kim, W.J. Social Distancing against COVID-19: Implication for the Control of Influenza. J. Korean Med. Sci. 2020, 35, e182. [Google Scholar] [CrossRef]
- Newbold, S.C.; Finnoff, D.; Thunström, L.; Ashworth, M.; Shogren, J.F. Effects of Physical Distancing to Control COVID-19 on Public Health, the Economy, and the Environment. Environ. Resour. Econ. 2020, 76, 705–729. [Google Scholar] [CrossRef]
- Siedner, M.J.; Harling, G.; Reynolds, Z.; Gilbert, R.F.; Haneuse, S.; Venkataramani, A.S.; Tsai, A.C. Social distancing to slow the US COVID-19 epidemic: Longitudinal pretest–posttest comparison group study. PLoS Med. 2020, 17, e1003244. [Google Scholar] [CrossRef]
- Central Disaster and Safety Countermeasure Headquarters of the Republic of Korea. Rules and guidelines for distancing in daily life to control coronavirus disease 2019 in Korea: 3rd version, announced on 3 July 2020. J. Educ. Eval. Health Prof. 2020, 17, 20. [Google Scholar] [CrossRef]
- Zhao, D.; Sun, J.; Tan, Y.; Wu, J.; Dou, Y. An extended SEIR model considering homepage effect for the information propagation of online social networks. Phys. A Stat. Mech. Its Appl. 2018, 512, 1019–1031. [Google Scholar] [CrossRef]
- Tasnim, S.; Hossain, M.; Mazumder, H. Impact of Rumors and Misinformation on COVID-19 in Social Media. J. Prev. Med. Public Health 2020, 53, 171–174. [Google Scholar] [CrossRef]
- Zeroual, A.; Harrou, F.; Dairi, A.; Sun, Y. Deep learning methods for forecasting COVID-19 time-Series data: A Comparative study. Chaos Solitons Fractals 2020, 140, 110121. [Google Scholar] [CrossRef] [PubMed]
- Tuli, S.; Tuli, S.; Tuli, R.; Gill, S.S. Predicting the growth and trend of COVID-19 pandemic using machine learning and cloud computing. Internet Things 2020, 11, 100222. [Google Scholar] [CrossRef]
- Panagiotopoulos, P.; Barnett, J.; Bigdeli, A.Z.; Sams, S. Social media in emergency management: Twitter as a tool for communicating risks to the public. Technol. Forecast. Soc. Chang. 2016, 111, 86–96. [Google Scholar] [CrossRef]
- Chatfield, A.T.; Reddick, C.G. All hands on deck to tweet #sandy: Networked governance of citizen coproduction in turbulent times. Gov. Inf. Q. 2018, 35, 259–272. [Google Scholar]
- Wukich, C. Government Social Media Messages across Disaster Phases. J. Conting. Crisis Manag. 2016, 24, 230–243. [Google Scholar] [CrossRef]
- Yum, S. Social Network Analysis for Coronavirus (COVID-19) in the United States. Soc. Sci. Q. 2020, 101, 1642–1647. [Google Scholar] [CrossRef]
- Jurgens, M.; Helsloot, I. The effect of social media on the dynamics of (self) resilience during disasters: A literature review. J. Conting. Crisis Manag. 2018, 26, 79–88. [Google Scholar] [CrossRef]
- Islam, A.K.M.N.; Laato, S.; Talukder, S.; Sutinen, E. Misinformation sharing and social media fatigue during COVID-19: An affordance and cognitive load perspective. Technol. Forecast. Soc. Chang. 2020, 159, 120201. [Google Scholar] [CrossRef]
- Song, J.; Song, T.M.; Seo, D.C.; Jin, D.L.; Kim, J.S. Social Big Data Analysis of Information Spread and Perceived Infection Risk During the 2015 Middle East Respiratory Syndrome Outbreak in South Korea. Cyberpsychol. Behav. Soc. Netw. 2017, 20, 22–29. [Google Scholar] [CrossRef]
- Cuan-Baltazar, J.Y.; Muñoz-Perez, M.J.; Robledo-Vega, C.; Pérez-Zepeda, M.F.; Soto-Vega, E. Misinformation of COVID-19 on the Internet: Infodemiology Study. JMIR Public Health Surveill. 2020, 6, e18444. [Google Scholar] [CrossRef]
- Pazzanese, C. Battling the ‘Pandemic of Misinformation’. The Harvard Gazette, 8 May 2020. Available online: https://news.harvard.edu/gazette/story/2020/05/social-media-used-to-spread-create-covid-19-falsehoods/ (accessed on 2 July 2020).
- OECD Policy Responses to Coronavirus (COVID-19), Using Artificial Intelligence to Help Combat COVID-19, Updated 23 April 2020. Available online: https://www.oecd.org/coronavirus/policy-responses/using-artificial-intelligence-to-help-combat-covid-19-ae4c5c21/ (accessed on 13 December 2020).
- Hiltunen, E. The future sign and its three dimensions. Futures 2008, 40, 247–260. [Google Scholar] [CrossRef]
- Yoon, J. Detecting weak signals for long-term business opportunities using text mining of Web news. Expert Syst. Appl. 2012, 39, 12543–12550. [Google Scholar] [CrossRef]
- Kim, H.-Y.; Park, H.-A.; Min, Y.H.; Jeon, E. Development of an obesity management ontology based on the nursing process for the mobile-device domain. J. Med. Internet Res. 2013, 15, e130. [Google Scholar] [CrossRef] [PubMed]
- Song, J.; Han, Y.; Kim, K.; Song, T.M. Social big data analysis of future signals for bullying in South Korea: Application of general strain theory. Telemat. Inform. 2020, 54, 101472. [Google Scholar] [CrossRef]
- Le Brocq, S.; Clare, K.; Bryant, M.; Roberts, K.; Tahrani, A.A. Obesity and COVID-19: A call for action from people living with obesity. Lancet Diabetes Endocrinol. 2020, 8, 652–654. [Google Scholar] [CrossRef] [PubMed]
- Sattar, N.; Ho, F.K.; Gill, J.; Ghouri, N.; Gray, S.; Celis-Morales, C.; Katikireddi, S.V.; Berry, C.; Pell, J.P.; Mcmurray, J.; et al. BMI and future risk for COVID-19 infection and death across sex, age and ethnicity: Preliminary findings from UK biobank. Diabetes Metab. Syndr. 2020, 14, 1149–1151. [Google Scholar] [CrossRef] [PubMed]
| Keyword | DoV | Mean Increase Rate | Mean Term Frequency | |||
|---|---|---|---|---|---|---|
| 2020 February | 2020 March | 2020 April | 2020 May | |||
| Mask | 27,771 | 44,034 | 17,173 | 13,812 | 0.041 | 25,698 |
| Government Response | 12,714 | 20,865 | 13,540 | 9572 | 0.162 | 14,173 |
| Tourism Industry | 13,536 | 10,974 | 6573 | 6529 | 0.072 | 9403 |
| Treatment | 7302 | 13,276 | 9705 | 4843 | 0.150 | 8782 |
| Health Care | 11,051 | 11,884 | 6653 | 4623 | −0.038 | 8553 |
| Diagnosis Kit | 3945 | 15,485 | 9801 | 2945 | 0.513 | 8044 |
| Regional Economy | 5944 | 10,024 | 7704 | 5223 | 0.231 | 7224 |
| Cold | 8294 | 6408 | 3017 | 2537 | −0.093 | 5064 |
| Infodemic | 5107 | 7627 | 3576 | 2804 | 0.056 | 4779 |
| Disinfectant | 6557 | 6689 | 3764 | 1896 | −0.148 | 4727 |
| Culture Industry | 4563 | 5396 | 4076 | 4057 | 0.260 | 4523 |
| Quarantine | 3382 | 6178 | 5897 | 2150 | 0.219 | 4402 |
| Hand Cleaner | 3919 | 4241 | 2817 | 2061 | 0.045 | 3260 |
| 3204 | 4697 | 1486 | 2027 | 0.252 | 2854 | |
| 2714 | 4387 | 2169 | 1500 | 0.055 | 2693 | |
| Immunity Food | 2274 | 2877 | 1927 | 1601 | 0.145 | 2170 |
| Airline | 2102 | 2689 | 2091 | 1259 | 0.097 | 2035 |
| Depression | 1064 | 2618 | 2054 | 2064 | 0.600 | 1950 |
| Negative Case | 3296 | 2888 | 693 | 190 | −0.497 | 1767 |
| Positive Case | 739 | 1470 | 1129 | 824 | 0.333 | 1041 |
| Fever | 1256 | 1260 | 639 | 550 | −0.004 | 926 |
| Stay home | 348 | 958 | 1778 | 516 | 0.958 | 900 |
| Respiratory | 1037 | 1139 | 769 | 563 | 0.056 | 877 |
| Sore Throat | 1043 | 989 | 342 | 325 | −0.070 | 675 |
| Obesity | 369 | 662 | 617 | 739 | 0.623 | 597 |
| Digestive Symptom | 379 | 722 | 347 | 449 | 0.425 | 474 |
| Inspection | 153 | 617 | 586 | 412 | 0.937 | 442 |
| School Closed | 555 | 621 | 160 | 135 | −0.135 | 368 |
| Online Shopping | 530 | 340 | 231 | 326 | 0.292 | 357 |
| Median | 0.145 | 2693 | ||||
| Keyword | DoD | Mean Increase Rate | Mean Document Frequency | |||
|---|---|---|---|---|---|---|
| 2020 February | 2020 March | 2020 April | 2020 May | |||
| Mask | 19,399 | 27,900 | 13,314 | 10,225 | 0.031 | 17,710 |
| Government Response | 10,880 | 17,898 | 11,728 | 8115 | 0.150 | 12,155 |
| Treatment | 6150 | 11,124 | 8079 | 4194 | 0.146 | 7387 |
| Tourism Industry | 10,477 | 8182 | 4847 | 4679 | 0.031 | 7046 |
| Regional Economy | 4891 | 8227 | 6082 | 4307 | 0.216 | 5877 |
| Diagnosis Kit | 2910 | 8835 | 5211 | 1774 | 0.287 | 4683 |
| Cold | 6898 | 5497 | 2509 | 2038 | −0.121 | 4236 |
| Infodemic | 4266 | 6265 | 3100 | 2357 | 0.045 | 3997 |
| Quarantine | 3010 | 5567 | 5226 | 1944 | 0.206 | 3937 |
| Culture Industry | 3090 | 3654 | 2635 | 2702 | 0.239 | 3020 |
| Disinfectant | 3760 | 3980 | 2101 | 1206 | −0.133 | 2762 |
| Negative Case | 2914 | 4175 | 1348 | 1856 | 0.246 | 2573 |
| Hand Cleaner | 2928 | 3285 | 2285 | 1616 | 0.048 | 2529 |
| Positive Case | 2563 | 4060 | 1951 | 1395 | 0.044 | 2492 |
| Immunity Food | 2001 | 2367 | 1504 | 1281 | 0.101 | 1788 |
| Depression | 990 | 2315 | 1614 | 1628 | 0.510 | 1637 |
| No Entry | 2921 | 2587 | 648 | 181 | −0.488 | 1584 |
| Airline | 1289 | 1583 | 1276 | 700 | 0.060 | 1212 |
| Asymptomatic | 664 | 1313 | 1010 | 778 | 0.340 | 941 |
| Fever | 1117 | 1137 | 576 | 511 | 0.002 | 835 |
| Stay home | 337 | 924 | 1596 | 475 | 0.857 | 833 |
| Respiratory | 957 | 1028 | 695 | 522 | 0.047 | 801 |
| Health Care | 1060 | 982 | 615 | 469 | −0.014 | 782 |
| Sore Throat | 887 | 866 | 304 | 295 | −0.058 | 588 |
| Obesity | 321 | 604 | 574 | 716 | 0.662 | 554 |
| Digestive Symptom | 341 | 629 | 295 | 385 | 0.400 | 413 |
| Inspection | 141 | 508 | 523 | 368 | 0.871 | 385 |
| School Closed | 495 | 572 | 142 | 128 | −0.107 | 334 |
| Online Shopping | 424 | 314 | 207 | 263 | 0.214 | 302 |
| Median | 0.101 | 1788 | ||||
| Future Signal | Latent Signal | Weak Signal | Strong Signal | Strong But Low Increasing Signal |
|---|---|---|---|---|
| KEM | Fever, Sore Throat, School Closed, Positive Case, Respiratory, Immunity Food, No Entry | Stay home, Inspection, Obesity, Digestive Symptom, Online Shopping, Asymptomatic | Depression, Culture Industry, Quarantine, Negative Case, Diagnosis Kit, Regional Economy, Treatment, Government Response | Airline, Infodemic, Cold, Disinfectant, Hand Cleaner Tourism Industry, Health Care, Mask |
| KIM | Fever, Sore Throat, School Closed, Respiratory, Immunity Food, No Entry, Airline, Health Care | Stay home, Inspection, Obesity, Digestive Symptom, Online Shopping, Asymptomatic, Depression | Culture Industry, Quarantine, Negative Case, Diagnosis Kit, Regional Economy, Treatment, Government Response | Infodemic, Cold, Disinfectant, Hand Cleaner, Tourism Industry, Mask, Positive Case, |
| Common signal | Fever, Sore Throat, School Closed, Respiratory, Immunity Food, No Entry | Stay home, Inspection, Obesity, Digestive Symptom, Online Shopping, Asymptomatic | Culture Industry, Quarantine, Negative Case, Diagnosis Kit, Regional Economy, Treatment, Government Response | Infodemic, Cold, Disinfectant, Hand Cleaner, Tourism Industry, Mask |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Song, J.; Jin, D.-L.; Song, T.M.; Lee, S.H. Exploring Future Signals of COVID-19 and Response to Information Diffusion Using Social Media Big Data. Int. J. Environ. Res. Public Health 2023, 20, 5753. https://doi.org/10.3390/ijerph20095753
Song J, Jin D-L, Song TM, Lee SH. Exploring Future Signals of COVID-19 and Response to Information Diffusion Using Social Media Big Data. International Journal of Environmental Research and Public Health. 2023; 20(9):5753. https://doi.org/10.3390/ijerph20095753
Chicago/Turabian StyleSong, Juyoung, Dal-Lae Jin, Tae Min Song, and Sang Ho Lee. 2023. "Exploring Future Signals of COVID-19 and Response to Information Diffusion Using Social Media Big Data" International Journal of Environmental Research and Public Health 20, no. 9: 5753. https://doi.org/10.3390/ijerph20095753
APA StyleSong, J., Jin, D.-L., Song, T. M., & Lee, S. H. (2023). Exploring Future Signals of COVID-19 and Response to Information Diffusion Using Social Media Big Data. International Journal of Environmental Research and Public Health, 20(9), 5753. https://doi.org/10.3390/ijerph20095753







