Evaluating Exoskeletons for WMSD Prevention: A Systematic Review of Applications and Ergonomic Approach in Occupational Settings
Abstract
1. Introduction
2. Materials and Methods
2.1. Information Source, Screening, and Eligibility Criteria
2.2. Data Extraction and Analysis
3. Results and Discussion
3.1. Overview of the Year, Participants, and Study Context
| Authors (Year) | Number of Participants | Study Context |
|---|---|---|
| Moyon et al. (2018) [42] | n = 9 (♂5; ♀4); Age: 20–40, Height N.A., Weight: N.A. | On-site |
| Schmalz et al. (2019) [43] | n = 12 (♂6; ♀6); Age: 24.0, Height 176.0 cm, Weight: 73.0 kg | Laboratory |
| Perez Luque et al. (2020) [9] | n = 17 (♂11; ♀6); Age: 25, Height 174.0, Weight: N.A. | Simulated On-site |
| Alabdulkarim et al. (2020) [44] | n = 16 (♂16; ♀0); Age: 34.3 Height 164.4 cm, Weight: 70.0 kg | Laboratory |
| Cardoso et al. (2020) [76] | n = 5 (♂2; ♀3); Age: 29.0, Height 165.0 cm, Weight: 76.0 kg | On-site |
| Lazzaroni et al. (2020) [24] | n = 9 (♂9; ♀0); Age: 27.3, Height 182.0 cm, Weight: 73.8 kg | Laboratory |
| Kong et al. (2021) [23] | n = 20 (♂13 Age: 22.5, Height 176.4 cm, Weight: 72.0 kg; ♀7); Age: 20.7, Height 165.5 cm, Weight: 57.2 kg) | Laboratory |
| Schwartz et al. (2021) [45] | n = 29 (♂15 Age: 23.0, Height 179.0 cm, Weight: 77.0 Kg; ♀14 Age: 22.0, Height 167.0 cm, Weight: 58.0 kg) | Laboratory |
| Lazzaroni et al. (2021) [46] | n = 10 (♂10; ♀0); Age: 29.8, Height 177.8 cm, Weight: 74.4 kg | Laboratory |
| Yin et al. (2021) [22] | n = 10 (♂10; ♀0); Age: 24.7, Height 174.8 cm, Weight: 68.3 kg | Laboratory |
| Weston et al. (2022) [47] | n = 6 (♂10 Age: 21.2, Height 179.5 cm, Weight: 79.8 kg; ♀6 Age: 22.5, Height 165.5 cm, Weight: 57.6.4 kg) | Laboratory |
| vam der Have et al. (2022) [48] | n = 16 (♂8; ♀8); Age: 21.9, Height N.A., Weight: N.A. | Laboratory |
| Kong et al. (2022) [49] | n = 20 (♂20; ♀0); Age: 24.8, Height 176.4 cm, Weight: 78.8 kg | Laboratory |
| Iranzo et al. (2022) [50] | n = 8 (♂4; ♀4); Age: 35.0, Height 175.6 cm, Weight: 67.9 kg | Laboratory |
| Latella et al. (2022) [11] | n = 12 (♂12; ♀0); Age: 23.2, Height 179.3 cm, Weight: 72.7 kg | Laboratory |
| De Bock et al. (2022) [51] | n = 22 (♂22; ♀0); Age: 23.7, Height 181.6 cm, Weight: 75.9 kg | Laboratory |
| Goršič et al. (2022) [52] | n = 10 (♂5; ♀5); Age: 28.4, Height 170.0 cm, Weight: 71.2 kg | Laboratory |
| Sierotowicz et al. (2022) [53] | n = 12 (♂9; ♀3); Age: 27.6, Height 176.0 cm, Weight: 71.9 kg | Laboratory |
| Mitterlehner et al. (2023) [54] | n = 30 (♂22; ♀8); Age: 29.0, Height 180.2 cm, Weight: 74.8 kg | Laboratory |
| R. M. Van Sluijs et al. (2023) [55] | n = 14 (♂5; ♀9); Age: 25.3, Height 170.0 cm, Weight: 70.7 kg | Laboratory |
| Garosi et al. (2023) [18] | n = 14 (♂14; ♀0); Age: 28, Height 176.0 cm, Weight: 71.6 kg | Laboratory |
| Walter et al. (2023) [56] | n = 14 (♂11; ♀3); Age: 22.3, Height 177.7 cm, Weight: 71.9 kg | Laboratory |
| Kong et al. (2023) [57] | n = 20 (♂20; ♀0); Age: 24.4, Height 176.0 cm, Weight: 78.0 kg | Laboratory |
| Shim et al. (2023) [58] | n = 20 (♂20; ♀0); Age: 24.4, Height 176.0 cm, Weight: 78.0 kg | Laboratory |
| Brunner et al. (2023) [59] | n = 32 (♂17; ♀15); Age: 26.7, Height 174.0 cm, Weight: 72.1 kg | Laboratory |
| Öçal et al. (2023) [21] | n = 3 (♂2; ♀1); Age: 33.3, Height 179.0 cm, Weight: 71.6 kg | Laboratory |
| Schrøder Jakobsen et al. (2023) [61] | Control: n = 10 (♂N.A.; ♀N.A.); Age: 32.2, Height 180.3 cm, Weight: 82.4 kg; Intervention n = 10 (♂N.A.; ♀N.A.); Age: 33.3, Height 181.9 cm, Weight: 87.4 kg | On-site |
| Govaerts et al. (2023) [60] | n = 16 (♂10; ♀6); Age: 35.0, Height 173.9 cm, Weight: 72.4 kg | Laboratory |
| Verdel et al. (2023) [62] | n = 19 (♂12; ♀7); Age: 24.0, Height 173.0 cm, Weight: 66.7 kg | Laboratory |
| Reimeir et al. (2023) [63] | n = 12 (♂9; ♀3); Age: 27.2, Height 179.4 cm, Weight: 75.3 kg | Laboratory |
| R.M. van Sluijs et al. (2023) [16] | n = 30 (♂22; ♀8); Age: 27.0, Height 178.0 cm, Weight: 72.9 kg | Laboratory |
| Park et al. (2023) [17] | n = 5 (♂3; ♀2); Age: 28.8, Height 175.0 cm, Weight: 65.4 kg | Laboratory |
| Ding et al. (2023) [25] | n = 9 (♂9; ♀0); Age: 24.6, Height 176.3 cm, Weight: 72.2 kg | Laboratory |
| Cuttilan et al. (2023) [64] | n = 10 (♂N.A.; ♀N.A.); Age: N.A., Height 170.0 cm, Weight: N.A. | Laboratory |
| De Bock et al. (2023) [65] | n = 16 (♂16; ♀0); Age: 29.3, Height 181.0 cm, Weight: 81.4.5 kg | Laboratory |
| Bhardwaj et al. (2023) [66] | n = 10 (♂16; ♀0); Age: 21–28, Height 171.1 cm, Weight: 71.2 kg | Laboratory |
| Thang (2023) [67] | n = 10 (♂10; ♀0); Age: 18–22, Height 170.0 cm, Weight: 70 kg | Laboratory |
| Schwartz et al. (2023) [68] | n = 29 (♂15 Age: 25.0, Height 180.0 cm, Weight: 74.9.kg; ♀0); Age: 24.0, Height 166.0 cm, Weight: 63.6.5 kg | Laboratory |
| Musso et al. (2024) [14] | n = 18 (♂18; ♀0); Age: 27.11, Height 179.5 cm, Weight: 78.67 kg | Laboratory |
| Schrøder Jakobsen et al. (2024) [69] | Control: n = 10 (♂7; ♀3); Age: 30.3, Height 177.9 cm, Weight: 81.1 kg; Intervention n = 9 (♂7; ♀2); Age: 29.8, Height 181.0 cm, Weight: 81.8 kg | On-site |
| Rafique et al. (2024) [10] | n = 9 (♂7; ♀2); Age: 30.0, Height 160.0–185.0 cm, Weight: 160.0–180.0 kg | Laboratory |
| Davoudi Kakhki et al. (2024) [70] | n = 22 (♂10; ♀12); Age: 20.5, Height N.A., Weight: 66.3 kg | Laboratory |
| van Sluijs et al. (2024) [71] | n = 31 (♂16; ♀15); Age: 28.0, Height 176.3 cm, Weight: 76.4 kg | Laboratory |
| Favennec et al. (2024) [72] | n = 18 (♂18; ♀0); Age: 21.5, Height 178.3 cm, Weight: 69.6 kg | Laboratory |
| Lee et al. (2024) [73] | n = 5 (♂5; ♀0); Age: 27.0, Height 174.8 cm, Weight: 70.0 kg | Laboratory |
| Gräf et al. (2024) [15] | n = 10 (♂5; ♀5); Age: 25.3, Height 174.6 cm, Weight: N.A. | Laboratory |
| Govaerts et al. (2024) [74] | n = 18 (♂10; ♀8); Age: 33.0, Height 173.5 cm, Weight: 70.6 kg | Laboratory |
| Bär et al. (2024) [75] | n = 36 (♂36; ♀0); Age: 25.9, Height 178.7 cm, Weight: 73.5 kg | Laboratory |
| Cardoso et al. (2024) [20] | n = 2 (♂1; ♀1); Age: 25.5, Height 176.0 cm, Weight: 77.5 kg | Simulated On-site |
3.2. Overview of the Exoskeletons Studied
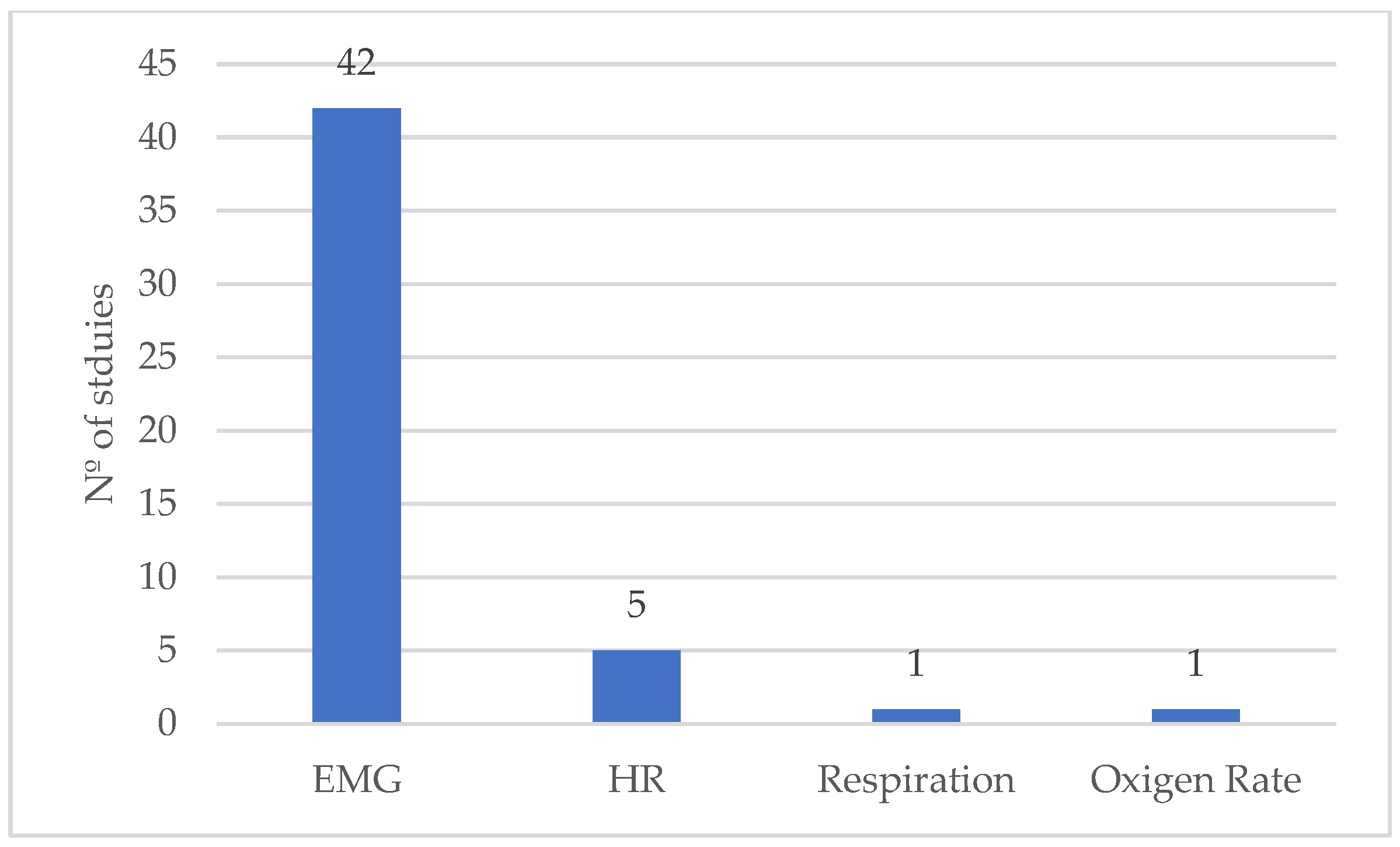
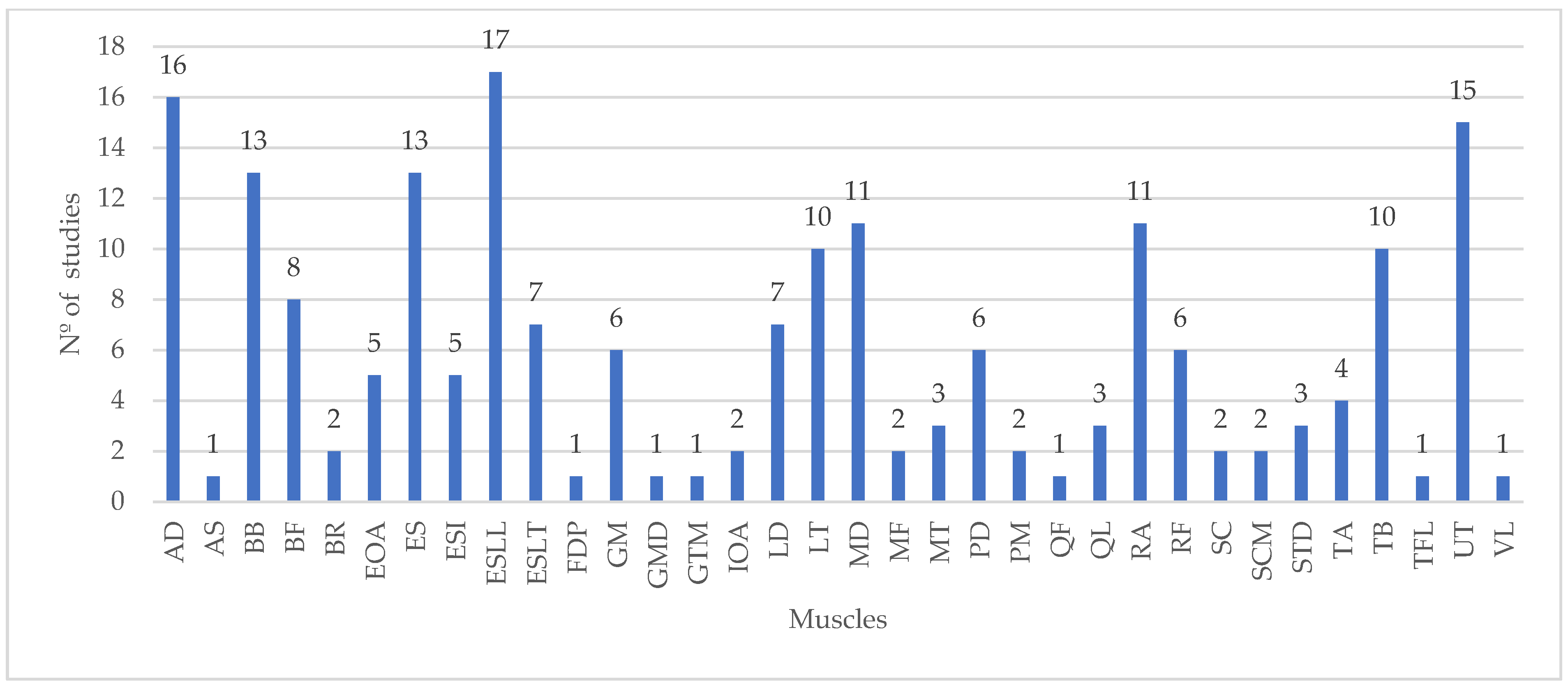
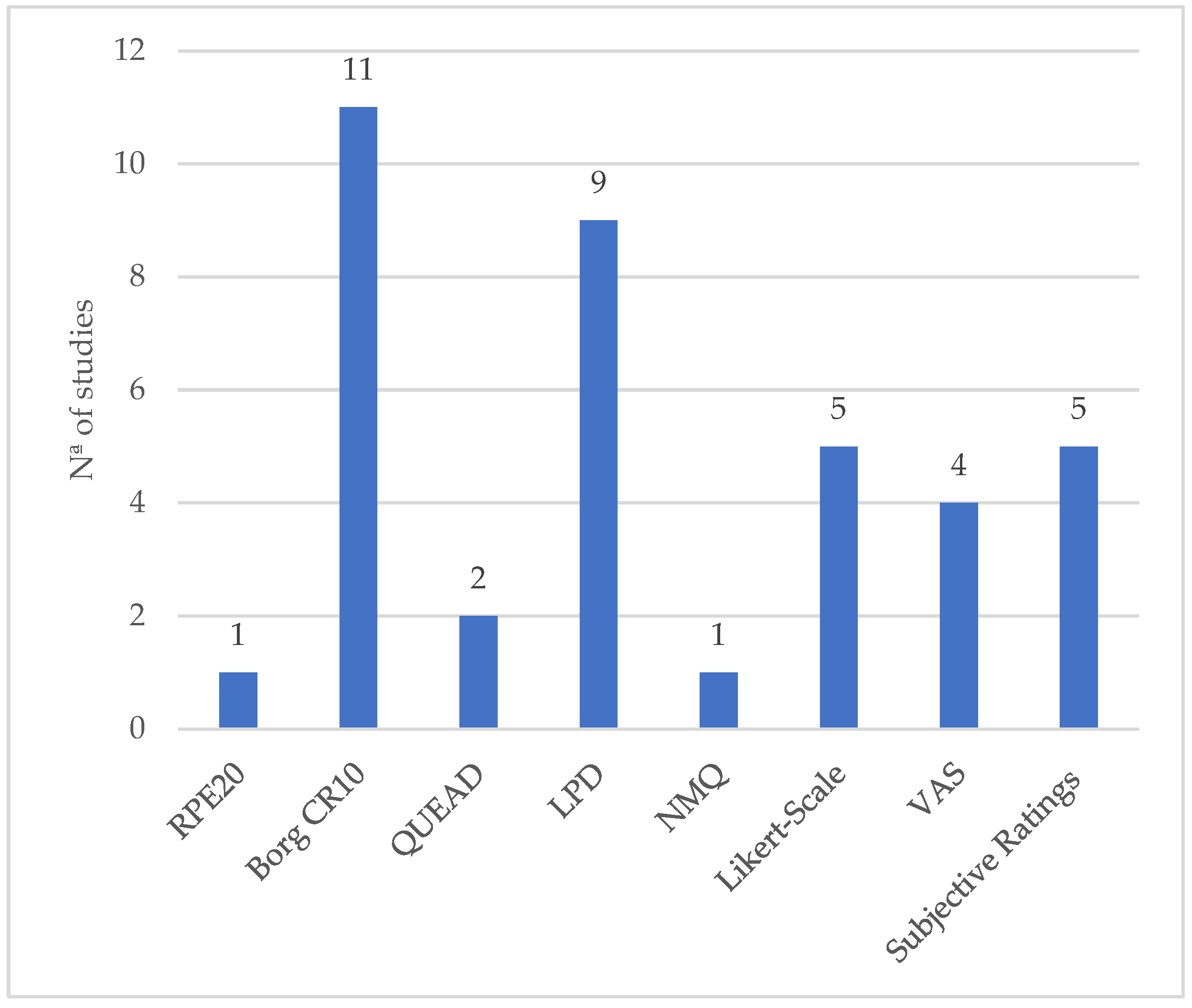
3.3. Overview of the Methodological Approach
3.4. Overview of the Main Conclusions of the Reviewed Studies
- Effectiveness in reducing muscle activity and physical strain: The majority of the studies demonstrate that exoskeletons—whether for the upper body, back, or lower limbs—significantly reduce muscle activity and physical strain during specific tasks. For example, studies such as those by Yin et al. (2021) [22] and Kong et al. (2021) [23] show reductions in upper-limb muscle activity, while Lazzaroni et al. (2020) [24] and Ding et al. (2023) [25] highlight the reduction in lumbar load during manual lifting tasks;
- Constraints and trade-offs: Although exoskeletons often reduce muscle fatigue and improve ergonomics, many studies report trade-offs in comfort, range of motion, and usability. For instance, Perez Luque et al. (2020) [9] and Cardoso et al. (2020) [76] indicate that while exoskeletons help to reduce strain, they also impose constraints on the range of motion and increase discomfort during prolonged use. This suggests that while beneficial for specific tasks, the long-term comfort and adaptability of these devices remain a challenge;
- Task-specific benefits: Several studies underscore the importance of selecting exoskeletons based on the specific demands of the task. For example, Kong et al. (2021) [23] and Schwartz et al. (2021) [45] show that passive exoskeletons provide significant benefits for overhead tasks but can increase strain during tasks performed at higher or lower heights. Shim et al. (2023) [58] and Schrøder Jakobsen et al. (2024) [69] highlight how the efficacy of these devices depends on task-specific requirements such as task height and lifting technique;
- Active vs. passive exoskeletons: Some studies compare active and passive exoskeletons, revealing that active systems often provide more substantial reductions in muscle activity but may hinder mobility or task performance, particularly during dynamic tasks. For instance, Schwartz et al. (2023) [68] report that active exoskeletons provide greater reductions in trunk muscle activity but may alter trunk kinematics and affect performance in dynamic environments;
- User experience and ergonomics: Several studies emphasize the need for improvements in the design and user experience of exoskeletons. Govaerts et al. (2024) [74] and Rafique et al. (2024) [10] suggest that while exoskeletons can reduce physical strain, there is a need for better design to enhance comfort, usability, and biomechanical compatibility for long-term use. This includes optimizing factors like device-to-body forces and ensuring that the exoskeleton does not interfere with the natural movement patterns of workers.
4. Conclusions
4.1. Key Findings
4.2. Implications for Practice
4.3. Limitations
4.4. Future Work
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Section and Topic | Item # | Checklist Item | Reported on Page # |
|---|---|---|---|
| Title | |||
| Title | 1 | Identify the report as a systematic review. | 1 |
| Abstract | |||
| Abstract | 2 | See the PRISMA 2020 for Abstracts checklist. | 1 |
| Introduction | |||
| Rationale | 3 | Describe the rationale for the review in the context of existing knowledge. | 2 |
| Objectives | 4 | Provide an explicit statement of the objective(s) or question(s) the review addresses. | 3 |
| Methods | |||
| Eligibility criteria | 5 | Specify the inclusion and exclusion criteria for the review and how studies were grouped for the syntheses. | 3–5 |
| Information sources | 6 | Specify all databases, registers, websites, organisations, reference lists and other sources searched or consulted to identify studies. Specify the date when each source was last searched or consulted. | 3 |
| Search strategy | 7 | Present the full search strategies for all databases, registers and websites, including any filters and limits used. | 3–5 |
| Selection process | 8 | Specify the methods used to decide whether a study met the inclusion criteria of the review, including how many reviewers screened each record and each report retrieved, whether they worked independently, and if applicable, details of automation tools used in the process. | 3–5 |
| Data collection process | 9 | Specify the methods used to collect data from reports, including how many reviewers collected data from each report, whether they worked independently, any processes for obtaining or confirming data from study investigators, and if applicable, details of automation tools used in the process. | 3–5 |
| Data items | 10a | List and define all outcomes for which data were sought. Specify whether all results that were compatible with each outcome domain in each study were sought (e.g., for all measures, time points, analyses), and if not, the methods used to decide which results to collect. | 4 |
| 10b | List and define all other variables for which data were sought (e.g., participant and intervention characteristics, funding sources). Describe any assumptions made about any missing or unclear information. | 4 | |
| Study risk of bias assessment | 11 | Specify the methods used to assess risk of bias in the included studies, including details of the tool(s) used, how many reviewers assessed each study and whether they worked independently, and if applicable, details of automation tools used in the process. | 28 |
| Effect measures | 12 | Specify for each outcome the effect measure(s) (e.g., risk ratio, mean difference) used in the synthesis or presentation of results. | 3–5 |
| Synthesis methods | 13a | Describe the processes used to decide which studies were eligible for each synthesis (e.g., tabulating the study intervention characteristics and comparing against the planned groups for each synthesis (item #5)). | 3–5 |
| 13b | Describe any methods required to prepare the data for presentation or synthesis, such as handling of missing summary statistics, or data conversions. | 3–5 | |
| 13c | Describe any methods used to tabulate or visually display results of individual studies and syntheses. | 3–5 | |
| 13d | Describe any methods used to synthesize results and provide a rationale for the choice(s). If meta-analysis was performed, describe the model(s), method(s) to identify the presence and extent of statistical heterogeneity, and software package(s) used. | 3–5 | |
| 13e | Describe any methods used to explore possible causes of heterogeneity among study results (e.g., subgroup analysis, meta-regression). | - | |
| 13f | Describe any sensitivity analyses conducted to assess robustness of the synthesized results. | - | |
| Reporting bias assessment | 14 | Describe any methods used to assess risk of bias due to missing results in a synthesis (arising from reporting biases). | 28 |
| Certainty assessment | 15 | Describe any methods used to assess certainty (or confidence) in the body of evidence for an outcome. | - |
| Results | |||
| Study selection | 16a | Describe the results of the search and selection process, from the number of records identified in the search to the number of studies included in the review, ideally using a flow diagram. | 3–5 |
| 16b | Cite studies that might appear to meet the inclusion criteria, but which were excluded, and explain why they were excluded. | - | |
| Study characteristics | 17 | Cite each included study and present its characteristics. | 5–7 |
| Risk of bias in studies | 18 | Present assessments of risk of bias for each included study. | 28 |
| Results of individual studies | 19 | For all outcomes, present, for each study: (a) summary statistics for each group (where appropriate) and (b) an effect estimate and its precision (e.g., confidence/credible interval), ideally using structured tables or plots. | 5–7 |
| Results of syntheses | 20a | For each synthesis, briefly summarise the characteristics and risk of bias among contributing studies. | 28 |
| 20b | Present results of all statistical syntheses conducted. If meta-analysis was done, present for each the summary estimate and its precision (e.g., confidence/credible interval) and measures of statistical heterogeneity. If comparing groups, describe the direction of the effect. | - | |
| 20c | Present results of all investigations of possible causes of heterogeneity among study results. | - | |
| 20d | Present results of all sensitivity analyses conducted to assess the robustness of the synthesized results. | - | |
| Reporting biases | 21 | Present assessments of risk of bias due to missing results (arising from reporting biases) for each synthesis assessed. | 28 |
| Certainty of evidence | 22 | Present assessments of certainty (or confidence) in the body of evidence for each outcome assessed. | - |
| Discussion | |||
| Discussion | 23a | Provide a general interpretation of the results in the context of other evidence. | 27 |
| 23b | Discuss any limitations of the evidence included in the review. | 28 | |
| 23c | Discuss any limitations of the review processes used. | 28 | |
| 23d | Discuss implications of the results for practice, policy, and future research. | 27 | |
| Other Information | |||
| Registration and protocol | 24a | Provide registration information for the review, including register name and registration number, or state that the review was not registered. | 28 |
| 24b | Indicate where the review protocol can be accessed, or state that a protocol was not prepared. | 28 | |
| 24c | Describe and explain any amendments to information provided at registration or in the protocol. | 28 | |
| Support | 25 | Describe sources of financial or non-financial support for the review, and the role of the funders or sponsors in the review. | 29 |
| Competing interests | 26 | Declare any competing interests of review authors. | 29 |
| Availability of data, code and other materials | 27 | Report which of the following are publicly available and where they can be found: template data collection forms; data extracted from included studies; data used for all analyses; analytic code; any other materials used in the review. | - |
References
- Russo, F.; Di Tecco, C.; Fontana, L.; Adamo, G.; Papale, A.; Denaro, V.; Iavicoli, S. Prevalence of Work Related Musculoskeletal Disorders in Italian Workers: Is There an Underestimation of the Related Occupational Risk Factors? BMC Musculoskelet. Disord. 2020, 21, 738. [Google Scholar] [CrossRef] [PubMed]
- Williams, A.; Kamper, S.J.; Wiggers, J.H.; O’Brien, K.M.; Lee, H.; Wolfenden, L.; Yoong, S.L.; Robson, E.; McAuley, J.H.; Hartvigsen, J.; et al. Musculoskeletal Conditions May Increase the Risk of Chronic Disease: A Systematic Review and Meta-Analysis of Cohort Studies. BMC Med. 2018, 16, 167. [Google Scholar] [CrossRef]
- European Agency for Safety and Health at Work; de Kok, J.; Vroonhof, P.; Snijders, J.; Roullis, G.; Clarke, M.; Peereboom, K.; van Dorst, P.; Isusi, I. Work-Related Musculoskeletal Disorders: Prevalence, Costs and Demographics in the EU; European Health: Luxembourg, 2019. [Google Scholar]
- Hagberg, M.; Violante, F.S.; Bonfiglioli, R.; Descatha, A.; Gold, J.; Evanoff, B.; Sluiter, J.K. Prevention of Musculoskeletal Disorders in Workers: Classification and Health Surveillance—Statements of the Scientific Committee on Musculoskeletal Disorders of the International Commission on Occupational Health. BMC Musculoskelet. Disord. 2012, 13, 109. [Google Scholar] [CrossRef] [PubMed]
- Colim, A.; Faria, C.; Braga, A.C.; Sousa, N.; Carneiro, P.; Costa, N.; Arezes, P. Towards an Ergonomic Assessment Framework for Industrial Assembly Workstations—A Case Study. Appl. Sci. 2020, 10, 3048. [Google Scholar] [CrossRef]
- Dogbla, L.; Gouvenelle, C.; Thorin, F.; Lesage, F.X.; Zak, M.; Ugbolue, U.C.; Charbotel, B.; Baker, J.S.; Pereira, B.; Dutheil, F. Occupational Risk Factors by Sectors: An Observational Study of 20,000 Workers. Int. J. Environ. Res. Public Health 2023, 20, 3632. [Google Scholar] [CrossRef]
- Yang, F.; Di, N.; Guo, W.-W.; Ding, W.-B.; Jia, N.; Zhang, H.; Li, D.; Wang, D.; Wang, R.; Zhang, D.; et al. The Prevalence and Risk Factors of Work Related Musculoskeletal Disorders among Electronics Manufacturing Workers: A Cross-Sectional Analytical Study in China. BMC Public. Health 2023, 23, 10. [Google Scholar] [CrossRef]
- Schwerha, D.J.; McNamara, N.; Nussbaum, M.A.; Kim, S. Adoption Potential of Occupational Exoskeletons in Diverse Enterprises Engaged in Manufacturing Tasks. Int. J. Ind. Ergon. 2021, 82, 103103. [Google Scholar] [CrossRef]
- Perez Luque, E.; Hogberg, D.; Iriondo Pascual, A.; Lamkull, D.; Garcia Rivera, F. Motion Behavior and Range of Motion When Using Exoskeletons in Manual Assembly Tasks. In Advances in Transdisciplinary Engineering; IOS Press BV: Amsterdam, The Netherlands, 2020; Volume 13, pp. 217–228. [Google Scholar]
- Rafique, S.; Rana, S.M.; Bjorsell, N.; Isaksson, M. Evaluating the Advantages of Passive Exoskeletons and Recommendations for Design Improvements. J. Rehabil. Assist. Technol. Eng. 2024, 11, 20556683241239875. [Google Scholar] [CrossRef]
- Latella, C.; Tirupachuri, Y.; Tagliapietra, L.; Rapetti, L.; Schirrmeister, B.; Bornmann, J.; Gorjan, D.; Camernik, J.; Maurice, P.; Fritzsche, L.; et al. Analysis of Human Whole-Body Joint Torques During Overhead Work with a Passive Exoskeleton. IEEE Trans. Hum. Mach. Syst. 2022, 52, 1060–1068. [Google Scholar] [CrossRef]
- Flor-Unda, O.; Casa, B.; Fuentes, M.; Solorzano, S.; Narvaez-Espinoza, F.; Acosta-Vargas, P. Exoskeletons: Contribution to Occupational Health and Safety. Bioengineering 2023, 10, 1039. [Google Scholar] [CrossRef]
- Botti, L.; Melloni, R. Occupational Exoskeletons: Understanding the Impact on Workers and Suggesting Guidelines for Practitioners and Future Research Needs. Appl. Sci. 2024, 14, 84. [Google Scholar] [CrossRef]
- Musso, M.; Oliveira, A.S.; Bai, S. Influence of an Upper Limb Exoskeleton on Muscle Activity during Various Construction and Manufacturing Tasks. Appl. Ergon. 2024, 114, 104158. [Google Scholar] [CrossRef]
- Gräf, J.; Grospretre, S.; Argubi-Wollesen, A.; Wollesen, B. Impact of a Passive Upper-Body Exoskeleton on Muscular Activity and Precision in Overhead Single and Dual Tasks: An Explorative Randomized Crossover Study. Front. Neurol. 2024, 15, 1405473. [Google Scholar] [CrossRef] [PubMed]
- van Sluijs, R.M.; Wehrli, M.; Brunner, A.; Lambercy, O. Evaluation of the Physiological Benefits of a Passive Back-Support Exoskeleton during Lifting and Working in Forward Leaning Postures. J. Biomech. 2023, 149, 111489. [Google Scholar] [CrossRef] [PubMed]
- Park, D.; Di Natali, C.; Sposito, M.; Caldwell, D.G.; Ortiz, J. Elbow-SideWINDER (Elbow-Side Wearable INDustrial Ergonomic Robot): Design, Control, and Validation of a Novel Elbow Exoskeleton. Front. Neurorobot 2023, 17, 1168213. [Google Scholar] [CrossRef] [PubMed]
- Garosi, E.; Kazemi, Z.; Mazloumi, A.; Keihani, A. Changes in Neck and Shoulder Muscles Fatigue Threshold When Using a Passive Head/Neck Supporting Exoskeleton During Repetitive Overhead Tasks. Hum. Factors 2023, 66, 2269–2282. [Google Scholar] [CrossRef]
- de Looze, M.P.; Bosch, T.; Krause, F.; Stadler, K.S.; O’Sullivan, L.W. Exoskeletons for Industrial Application and Their Potential Effects on Physical Work Load. Ergonomics 2016, 59, 671–681. [Google Scholar] [CrossRef]
- Cardoso, A.; Colim, A.; Carneiro, P.; Costa, N.; Gomes, S.; Pires, A.; Arezes, P. Assessing the Short-Term Effects of Dual Back-Support Exoskeleton within Logistics Operations. Safety 2024, 10, 56. [Google Scholar] [CrossRef]
- Öçal, A.E.; Lekesiz, H.; Çetin, S.T. The Development of an Innovative Occupational Passive Upper Extremity Exoskeleton and an Investigation of Its Effects on Muscles. Appl. Sci. 2023, 13, 6763. [Google Scholar] [CrossRef]
- Yin, P.; Yang, L.; Qu, S. Development of an Ergonomic Wearable Robotic Device for Assisting Manual Workers. Int. J. Adv. Robot. Syst. 2021, 18, 172988142110467. [Google Scholar] [CrossRef]
- Kong, Y.K.; Park, C.W.; Cho, M.U.; Kim, S.Y.; Kim, M.J.; Hyun, D.J.; Bae, K.; Choi, J.K.; Ko, S.M.; Choi, K.H. Guidelines for Working Heights of the Lower-Limb Exoskeleton (Cex) Based on Ergonomic Evaluations. Int. J. Environ. Res. Public Health 2021, 18, 5199. [Google Scholar] [CrossRef]
- Lazzaroni, M.; Tabasi, A.; Toxiri, S.; Caldwell, D.G.; De Momi, E.; Van Dijk, W.; De Looze, M.P.; Kingma, I.; Van Dieën, J.H.; Ortiz, J. Evaluation of an Acceleration-Based Assistive Strategy to Control a Back-Support Exoskeleton for Manual Material Handling. Wearable Technol. 2020, 1, e9. [Google Scholar] [CrossRef]
- Ding, S.; Reyes, F.A.; Bhattacharya, S.; Seyram, O.; Yu, H. A Novel Passive Back-Support Exoskeleton with a Spring-Cable-Differential for Lifting Assistance. IEEE Trans. Neural Syst. Rehabil. Eng. 2023, 31, 3781–3789. [Google Scholar] [CrossRef]
- David, G.C. Ergonomic Methods for Assessing Exposure to Risk Factors for Work-Related Musculoskeletal Disorders. Occup. Med. 2005, 55, 190–199. [Google Scholar] [CrossRef] [PubMed]
- Takala, E.P.; Pehkonen, I.; Forsman, M.; Hansson, G.Å.; Mathiassen, S.E.; Neumann, W.P.; Sjøgaard, G.; Veiersted, K.B.; Westgaard, R.H.; Winkel, J. Systematic Evaluation of Observational Methods Assessing Biomechanical Exposures at Work. Scand. J. Work. Environ. Health 2010, 36, 3–24. [Google Scholar] [CrossRef] [PubMed]
- Anacleto Filho, P.C.; Colim, A.; Jesus, C.; Lopes, S.I.; Carneiro, P. Digital and Virtual Technologies for Work-Related Biomechanical Risk Assessment: A Scoping Review. Safety 2024, 10, 79. [Google Scholar] [CrossRef]
- Cardoso, A.; Colim, A.; Bicho, E.; Braga, A.; Pereira, D.; Monteiro, S.; Carneiro, P.; Costa, N.; Arezes, P. Enhancing Worker Well-Being: A Study on Assistive Assembly to Mitigate Work-Related Musculoskeletal Disorders and Modulate Cobot Assistive Behavior. In Proceedings of the Human Systems Engineering and Design (IHSED2024) Future Trends and Applications, Split, Croatia, 24–26 September 2024; AHFE International: Split, Croatia, 2024; Volume 158. [Google Scholar]
- Kuorinka, I.; Jonsson, B.; Kilbom, A.; Vinterberg, H.; Biering-S6rensen, F.; Andersson, G.; J6rgensen, K. Standardised Nordic Questionnaires for the Analysis of Musculoskeletal Symptoms. Appl. Ergon. 1987, 18, 233–237. [Google Scholar] [CrossRef]
- Occupational Safety and Health Administration (OSHA). Ergonomic Assessment Checklist. Available online: https://www.osha.gov/sites/default/files/2018-12/fy14_sh-26336-sh4_Ergonomic-Assessment-Checklist.pdf (accessed on 5 December 2022).
- Hignett, S.; McAtamney, L. Rapid Entire Body Assessment (REBA). Appl. Ergon. 2000, 31, 201–205. [Google Scholar] [CrossRef] [PubMed]
- BauA. Key Indicator Method for Assessing and Designing Physical Workloads during Manual Handling Operations. BAuA 2019, 1, 1–4. [Google Scholar]
- Colim, A.; Arezes, P.; Flores, P.; Monteiro, P.R.R.; Mesquita, I.; Braga, A.C. Obesity Effects on Muscular Activity during Lifting and Lowering Tasks. Int. J. Occup. Saf. Ergon. 2021, 27, 217–225. [Google Scholar] [CrossRef]
- Colim, A.; Pereira, D.; Lima, P.; Cardoso, A.; Almeida, R.; Fernandes, D.; Mould, S.; Arezes, P. Designing a User-Centered Inspection Device’s Handle for the Aircraft Manufacturing Industry. Appl. Sci. 2023, 13, 11584. [Google Scholar] [CrossRef]
- Colim, A.; Cardoso, A.; Arezes, P.; Braga, A.C.; Peixoto, A.C.; Peixoto, V.; Wolbert, F.; Carneiro, P.; Costa, N.; Sousa, N. Digitalization of Musculoskeletal Risk Assessment in a Robotic-Assisted Assembly Workstation. Safety 2021, 7, 74. [Google Scholar] [CrossRef]
- Kranenborg, S.E.; Greve, C.; Reneman, M.F.; Roossien, C.C. Side-Effects and Adverse Events of a Shoulder- and Back-Support Exoskeleton in Workers: A Systematic Review. Appl. Ergon. 2023, 111, 104042. [Google Scholar] [CrossRef] [PubMed]
- Kermavnar, T.; de Vries, A.W.; de Looze, M.P.; O’Sullivan, L.W. Effects of Industrial Back-Support Exoskeletons on Body Loading and User Experience: An Updated Systematic Review. Ergonomics 2021, 64, 685–711. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.T.; Altman, D.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Duarte, J.; Torres Marques, A.; Santos Baptista, J. Occupational Accidents Related to Heavy Machinery: A Systematic Review. Safety 2021, 7, 21. [Google Scholar] [CrossRef]
- Gualtieri, L.; Rauch, E.; Vidoni, R. Emerging Research Fields in Safety and Ergonomics in Industrial Collaborative Robotics: A Systematic Literature Review. Robot. Comput. Integr. Manuf. 2021, 67, 101998. [Google Scholar] [CrossRef]
- Moyon, A.; Poirson, E.; Petiot, J.F. Experimental Study of the Physical Impact of a Passive Exoskeleton on Manual Sanding Operations. In Procedia CIRP; Elsevier B.V.: Amsterdam, The Netherlands, 2018; Volume 70, pp. 284–289. [Google Scholar]
- Schmalz, T.; Schändlinger, J.; Schuler, M.; Bornmann, J.; Schirrmeister, B.; Kannenberg, A.; Ernst, M. Biomechanical and Metabolic Effectiveness of an Industrial Exoskeleton for Overhead Work. Int. J. Environ. Res. Public Health 2019, 16, 4792. [Google Scholar] [CrossRef]
- Alabdulkarim, S.A.; Farhan, A.M.; Ramadan, M.Z. Development and Investigation of a Wearable Aid for a Load Carriage Task. Int. J. Environ. Res. Public Health 2020, 17, 749. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, M.; Theurel, J.; Desbrosses, K. Effectiveness of Soft versus Rigid Back-Support Exoskeletons during a Lifting Task. Int. J. Environ. Res. Public Health 2021, 18, 8062. [Google Scholar] [CrossRef] [PubMed]
- Lazzaroni, M.; Poliero, T.; Sposito, M.; Toxiri, S.; Caldwell, D.G.; Di Natali, C.; Ortiz, J. Back-Support Exoskeleton Control Strategy for Pulling Activities: Design and Preliminary Evaluation. Designs 2021, 5, 39. [Google Scholar] [CrossRef]
- Weston, E.B.; Alizadeh, M.; Hani, H.; Knapik, G.G.; Souchereau, R.A.; Marras, W.S. A Physiological and Biomechanical Investigation of Three Passive Upper-Extremity Exoskeletons during Simulated Overhead Work. Ergonomics 2022, 65, 105–117. [Google Scholar] [CrossRef] [PubMed]
- van der Have, A.; Rossini, M.; Rodriguez-Guerrero, C.; Van Rossom, S.; Jonkers, I. The Exo4Work Shoulder Exoskeleton Effectively Reduces Muscle and Joint Loading during Simulated Occupational Tasks above Shoulder Height. Appl. Ergon. 2022, 103, 103800. [Google Scholar] [CrossRef]
- Kong, Y.K.; Choi, K.H.; Cho, M.U.; Kim, S.Y.; Kim, M.J.; Shim, J.W.; Park, S.S.; Kim, K.R.; Seo, M.T.; Chae, H.S.; et al. Ergonomic Assessment of a Lower-Limb Exoskeleton through Electromyography and Anybody Modeling System. Int. J. Environ. Res. Public Health 2022, 19, 8088. [Google Scholar] [CrossRef]
- Iranzo, S.; Piedrabuena, A.; García-Torres, F.; Martinez-De-juan, J.L.; Prats-Boluda, G.; Sanchis, M.; Belda-Lois, J.M. Assessment of a Passive Lumbar Exoskeleton in Material Manual Handling Tasks under Laboratory Conditions. Sensors 2022, 22, 4060. [Google Scholar] [CrossRef] [PubMed]
- De Bock, S.; Rossini, M.; Lefeber, D.; Rodriguez-Guerrero, C.; Geeroms, J.; Meeusen, R.; De Pauw, K. An Occupational Shoulder Exoskeleton Reduces Muscle Activity and Fatigue During Overhead Work. IEEE Trans. Biomed. Eng. 2022, 69, 3008–3020. [Google Scholar] [CrossRef] [PubMed]
- Goršič, M.; Song, Y.; Dai, B.; Novak, V.D. Short-Term Effects of the Auxivo LiftSuit during Lifting and Static Leaning. Appl. Ergon. 2022, 102, 103765. [Google Scholar] [CrossRef] [PubMed]
- Sierotowicz, M.; Brusamento, D.; Schirrmeister, B.; Connan, M.; Bornmann, J.; Gonzalez-Vargas, J.; Castellini, C. Unobtrusive, Natural Support Control of an Adaptive Industrial Exoskeleton Using Force Myography. Front. Robot. AI 2022, 9, 919370. [Google Scholar] [CrossRef]
- Mitterlehner, L.; Li, Y.X.; Wolf, M. Objective and Subjective Evaluation of a Passive Low-Back Exoskeleton during Simulated Logistics Tasks. Wearable Technol. 2023, 4, e24. [Google Scholar] [CrossRef]
- Van Sluijs, R.M.; Rodriguez-Cianca, D.; Sanz-Morère, C.B.; Massardi, S.; Bartenbach, V.; Torricelli, D. A Method to Quantify the Reduction of Back and Hip Muscle Fatigue of Lift-Support Exoskeletons. Wearable Technol. 2023, 4, e2. [Google Scholar] [CrossRef] [PubMed]
- Walter, T.; Stutzig, N.; Siebert, T. Active Exoskeleton Reduces Erector Spinae Muscle Activity during Lifting. Front. Bioeng. Biotechnol. 2023, 11, 1143926. [Google Scholar] [CrossRef] [PubMed]
- Kong, Y.K.; Kim, J.H.; Shim, H.H.; Shim, J.W.; Park, S.S.; Choi, K.H. Efficacy of Passive Upper-Limb Exoskeletons in Reducing Musculoskeletal Load Associated with Overhead Tasks. Appl. Ergon. 2023, 109, 103965. [Google Scholar] [CrossRef]
- Shim, H.H.; Choi, K.H.; Keum, H.; Son, S.; Kim, J.H.; Seo, M.T.; Kim, S.Y.; Park, D.; Kong, Y.K. Evaluation of the Effects of Passive Lower-Limb Exoskeletons on Muscle Activities According to Working Heights. Appl. Sci. 2023, 13, 11754. [Google Scholar] [CrossRef]
- Brunner, A.; Van Sluijs, R.; Luder, T.; Camichel, C.; Kos, M.; Bee, D.; Bartenbach, V.; Lambercy, O. Effect of Passive Shoulder Exoskeleton Support during Working with Arms over Shoulder Level. Wearable Technol. 2023, 4, e26. [Google Scholar] [CrossRef] [PubMed]
- Govaerts, R.; Turcksin, T.; Vanderborght, B.; Roelands, B.; Meeusen, R.; De Pauw, K.; De Bock, S. Evaluating Cognitive and Physical Work Performance: A Comparative Study of an Active and Passive Industrial Back-Support Exoskeleton. Wearable Technol. 2023, 4, e27. [Google Scholar] [CrossRef] [PubMed]
- Schrøder Jakobsen, L.; de Zee, M.; Samani, A.; Desbrosses, K.; Madeleine, P. Biomechanical Changes, Acceptance, and Usability of a Passive Shoulder Exoskeleton in Manual Material Handling. A Field Study. Appl. Ergon. 2023, 113, 104104. [Google Scholar] [CrossRef] [PubMed]
- Verdel, D.; Sahm, G.; Bruneau, O.; Berret, B.; Vignais, N. A Trade-Off between Complexity and Interaction Quality for Upper Limb Exoskeleton Interfaces. Sensors 2023, 23, 4122. [Google Scholar] [CrossRef]
- Reimeir, B.; Calisti, M.; Mittermeier, R.; Ralfs, L.; Weidner, R. Effects of Back-Support Exoskeletons with Different Functional Mechanisms on Trunk Muscle Activity and Kinematics. Wearable Technol. 2023, 4, e12. [Google Scholar] [CrossRef] [PubMed]
- Cuttilan, A.N.; Natividad, R.F.; Yeow, R.C.H. Fabric-Based, Pneumatic Exosuit for Lower-Back Support in Manual-Handling Tasks. Actuators 2023, 12, 273. [Google Scholar] [CrossRef]
- De Bock, S.; Ampe, T.; Rossini, M.; Tassignon, B.; Lefeber, D.; Rodriguez-Guerrero, C.; Roelands, B.; Geeroms, J.; Meeusen, R.; De Pauw, K. Passive Shoulder Exoskeleton Support Partially Mitigates Fatigue-Induced Effects in Overhead Work. Appl. Ergon. 2023, 106, 103903. [Google Scholar] [CrossRef]
- Bhardwaj, S.; Shinde, A.B.; Singh, R.; Vashista, V. Manipulating Device-to-Body Forces in Passive Exosuit: An Experimental Investigation on the Effect of Moment Arm Orientation Using Passive Back-Assist Exosuit Emulator. Wearable Technol. 2023, 4, e17. [Google Scholar] [CrossRef] [PubMed]
- Thang, L.T. Effect Valuation of Passive Exoskeleton for Overhead Work. SSRG Int. J. Mech. Eng. 2023, 10, 1–6. [Google Scholar] [CrossRef]
- Schwartz, M.; Desbrosses, K.; Theurel, J.; Mornieux, G. Biomechanical Consequences of Using Passive and Active Back-Support Exoskeletons during Different Manual Handling Tasks. Int. J. Environ. Res. Public Health 2023, 20, 6468. [Google Scholar] [CrossRef] [PubMed]
- Schrøder Jakobsen, L.; Samani, A.; Desbrosses, K.; de Zee, M.; Madeleine, P. In-Field Training of a Passive Back Exoskeleton Changes the Biomechanics of Logistic Workers. IISE Trans. Occup. Ergon. Hum. Factors 2024, 12, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Davoudi Kakhki, F.; Moghadam, A.; Nieto, A.; Vora, H. Evaluating the Efficacy of a Passive Exoskeleton for Enhancing Ergonomics in Manufacturing. Appl. Sci. 2024, 14, 5810. [Google Scholar] [CrossRef]
- van Sluijs, R.; Scholtysik, T.; Brunner, A.; Kuoni, L.; Bee, D.; Kos, M.; Bartenbach, V.; Lambercy, O. Design and Evaluation of the OmniSuit: A Passive Occupational Exoskeleton for Back and Shoulder Support. Appl. Ergon. 2024, 120, 104332. [Google Scholar] [CrossRef] [PubMed]
- Favennec, A.; Frère, J.; Mornieux, G. Changes in Human Motor Behavior during the Familiarization with a Soft Back-Support Occupational Exoskeleton. Appl. Sci. 2024, 14, 1160. [Google Scholar] [CrossRef]
- Lee, H.H.; Yoon, K.T.; Lim, H.H.; Lee, W.K.; Jung, J.H.; Kim, S.B.; Choi, Y.M. A Novel Passive Shoulder Exoskeleton Using Link Chains and Magnetic Spring Joints. IEEE Trans. Neural Syst. Rehabil. Eng. 2024, 32, 708–717. [Google Scholar] [CrossRef] [PubMed]
- Govaerts, R.; De Bock, S.; Provyn, S.; Vanderborght, B.; Roelands, B.; Meeusen, R.; De Pauw, K. The Impact of an Active and Passive Industrial Back Exoskeleton on Functional Performance. Ergonomics 2024, 67, 597–618. [Google Scholar] [CrossRef] [PubMed]
- Bär, M.; Luger, T.; Seibt, R.; Rieger, M.A.; Steinhilber, B. Using a Passive Back Exoskeleton During a Simulated Sorting Task: Influence on Muscle Activity, Posture, and Heart Rate. Hum. Factors 2024, 66, 40–55. [Google Scholar] [CrossRef]
- Cardoso, A.; Colim, A.; Sousa, N. The Effects of a Passive Exoskeleton on Muscle Activity and Discomfort in Industrial Tasks. Stud. Syst. Decis. Control. 2020, 277, 237–245. [Google Scholar] [CrossRef]
- Lee, H.; Kim, W.; Han, J.; Han, C. The Technical Trend of the Exoskeleton Robot System for Human Power Assistance. Int. J. Precis. Eng. Manuf. 2012, 13, 1491–1497. [Google Scholar] [CrossRef]
- Graham, R.B.; Agnew, M.J.; Stevenson, J.M. Effectiveness of an On-Body Lifting Aid at Reducing Low Back Physical Demands during an Automotive Assembly Task: Assessment of EMG Response and User Acceptability. Appl. Ergon. 2009, 40, 936–942. [Google Scholar] [CrossRef]
- Sauter, M.; Barthelme, J.; Müller, C.; Liebers, F. Manual Handling of Heavy Loads and Low Back Pain among Different Occupational Groups: Results of the 2018 BIBB/BAuA Employment Survey. BMC Musculoskelet. Disord. 2021, 22, 956. [Google Scholar] [CrossRef]
- Govaerts, R.; Tassignon, B.; Ghillebert, J.; Serrien, B.; De Bock, S.; Ampe, T.; El Makrini, I.; Vanderborght, B.; Meeusen, R.; De Pauw, K. Prevalence and Incidence of Work-Related Musculoskeletal Disorders in Secondary Industries of 21st Century Europe: A Systematic Review and Meta-Analysis. BMC Musculoskelet. Disord. 2021, 22, 751. [Google Scholar] [CrossRef]
- Salmon, P.M.; Read, G.J.M. Many Model Thinking in Systems Ergonomics: A Case Study in Road Safety. Ergonomics 2019, 62, 612–628. [Google Scholar] [CrossRef]
- Miniato, A.M.; Anand, P.; Varacallo, M. Anatomy, Shoulder and Upper Limb, Shoulder. Available online: https://www.ncbi.nlm.nih.gov/books/NBK536933/ (accessed on 20 August 2024).
- Williams, N. The Borg Rating of Perceived Exertion (RPE) Scale. Occup. Med. 2017, 67, 404–405. [Google Scholar] [CrossRef]
- Schmidtler, J.; Bengler, K. A Questionnaire for the Evaluation of Physical Assistive Devices (QUEAD)—Testing Usability and Acceptance in physical Human-Robot Interaction. In Proceedings of the IEEE International Conference on Systems, Man, and Cybernetics, Banff, AB, Canada, 5–8 October 2017; pp. 876–881. [Google Scholar]
- Cardoso, A.; Colim, A.; Bicho, E.; Braga, A.C.; Arezes, P. A Novel Human-Centered Methodology for Assessing Manual-to-Collaborative Safe Conversion of Workstations. Saf. Sci. 2025, 181, 106685. [Google Scholar] [CrossRef]
- Iranzo, S.; Piedrabuena, A.; Iordanov, D.; Martinez-Iranzo, U.; Belda-Lois, J.M. Ergonomics Assessment of Passive Upper-Limb Exoskeletons in an Automotive Assembly Plant. Appl. Ergon. 2020, 87, 103120. [Google Scholar] [CrossRef]



| Authors (Year) | Exoskeleton | Actuation | Supported Body Part |
|---|---|---|---|
| Moyon et al. (2018) [42] | Pad | Passive | Upper arm |
| Schmalz et al. (2019) [43] | Paexo | Passive | Upper arm |
| Perez Luque et al. (2020) [9] | EksoEvo Ottobock’s Paexo Comau Mate | Passive | Upper arm |
| Alabdulkarim et al. (2020) [44] | (b–e) assistive device | Passive | Back and upper arm |
| Cardoso et al. (2020) [76] | Laevo v2 | Passive | Back |
| Lazzaroni et al. (2020) [24] | XoTrunk | Active | Back |
| Kong et al. (2021) [23] | Cex | Passive | Legs |
| Schwartz et al. (2021) [45] | Corfor V2 Laevo V1 | Passive | Back |
| Lazzaroni et al. (2021) [46] | XoTrunk | Active | Back |
| Yin et al. (2021) [22] | PUES_PGBA | Passive | Upper arm |
| Weston et al. (2022) [47] | EksoVest Airframe Shoulder X | Passive | Upper arm |
| vam der Have et al. (2022) [48] | Shoulder exoskeleton Prototype | Passive | Upper arm |
| Kong et al. (2022) [49] | Cex | Passive | Legs |
| Iranzo et al. (2022) [50] | Laevo v2 | Passive | Back |
| Latella et al. (2022) [11] | Paexo | Passive | Upper arm |
| De Bock et al. (2022) [51] | Shoulder exoskeleton prototype (Exo4Work) | Passive | Upper arm |
| Goršič et al. (2022) [52] | Auxivo LiftSuit V1.1 | Passive | Back |
| Sierotowicz et al. (2022) [53] | Paexo | Passive | Upper arm |
| Mitterlehner et al. (2023) [54] | Paexo | Passive | Back |
| Van Sluijs et al. (2023) [55] | Auxivo LiftSuit v2.0 | Passive | Back |
| Garosi et al. (2023) [18] | Head/neck supporting exoskeleton | Passive | Head and neck |
| Walter et al. (2023) [56] | Cray X | Active | Back |
| Kong et al. (2023) [57] | Vex AirFrame | Passive | Upper arm |
| Shim et al. (2023) [58] | Cex Chairless Chair | Passive | Legs |
| Brunner et al. (2023) [59] | DeltaSuit prototype | Passive | Upper arm |
| Öçal et al. (2023) [21] | Exoskeleton prototype | Passive | Upper arm |
| Schrøder Jakobsen et al. (2023) [61] | Shoulder X V3 | Passive | Upper arm |
| Govaerts et al. (2023) [60] | Paexo CrayX | Passive Active | Back |
| Verdel et al. (2023) [62] | Able | Active | Upper arm |
| Reimeir et al. (2023) [63] | Rakunie N-Ippin BionicBack hTRIUS SoftExo Lift Hunic Japet.W Japet Cray X | Passive Passive Passive Active Active | Back |
| van Sluijs et al. (2023) [16] | Auxivo LiftSuit v2.0 | Passive | Back |
| Park et al. (2023) [17] | Elbow-sideWINDER | Active | Elbow |
| Ding et al. (2023) [25] | SE prototype | Passive | Back |
| Cuttilan et al. (2023) [64] | AirLevate | Passive | Back |
| De Bock et al. (2023) [65] | Shoulder exoskeleton prototype (Exo4Work) | Passive | Upper arm |
| Bhardwaj et al. (2023) [66] | BASE emulator exoskleton prototype | Passive | Back |
| Thang (2023) [67] | Passive exoskeleton with a mechanical arm | Passive | Upper arm |
| Schwartz et al. (2023) [68] | BackX Exoback V1 Cray X | Passive Active Active | Back |
| Musso et al. (2024) [14] | Skelex 360 | Passive | Upper arm |
| Schrøder Jakobsen et al. (2024) [69] | BackX | Passive | Back |
| Rafique et al. (2024) [10] | EksoVest SuitX | Passive | Upper arm Legs |
| Davoudi Kakhki et al. (2024) [70] | BackX | Passive | Back |
| van Sluijs et al. (2024) [71] | OmniSuit | Passive | Back and upper arm |
| Favennec et al. (2024) [72] | Corfor | Passive | Back |
| Lee et al. (2024) [73] | Shoulder exoskeleton prototype | Passive | Upper arm |
| Gräf et al. (2024) [15] | Skelex 360 | Passive | Upper arm |
| Govaerts et al. (2024) [74] | Paexo CrayX | Passive Active | Back |
| Bär et al. (2024) [75] | Laevo V2 | Passive | Back |
| Cardoso et al. (2024) [20] | Auxivo lift suit V2 BionicBack hTRIUS | Passive | Back |
| Authors (Year) | Tasks Assessed | WMSD Risk Assessment Methods Applied | |||
|---|---|---|---|---|---|
| Direct Measurement | Observational Methods | Self-Reports and Checklists | |||
| Biomechanical | Physiological | ||||
| Moyon et al. (2018) [42] | Overhead tasks | N.A. | Heart rate | N.A. | Borg CR10 |
| Schmalz et al. (2019) [43] | Overhead tasks | Kinematics: 3D motion capture system | Oxygen rate; unilateral EMG: AD, MD, PD, UT, MT, LT, BB, AS, LD, EOA muscles | N.A. | N.A. |
| Perez Luque et al. (2020) [9] | Overhead tasks | Kinematics: IMU tracking system | N.A. | N.A. | Subjective ratings questionnaire |
| Alabdulkarim et al. (2020) [44] | Push and pulling tasks-Light (15%) and Heavy (30%) of the participant weight | N.A. | Unilateral EMG: FDP, BB, AD, ES | N.A. | Borg CR10 |
| Cardoso et al. (2020) [76] | Lifting tasks (~2 kg) | N.A. | Bilateral EMG: UT, ESI, ESLL | N.A. | Borg CR10, LPD and VAS |
| Lazzaroni et al. (2020) [24] | Lifting tasks (7.5–15 kg) | Kinematics: 3D motion capture system | Bilateral EMG: RA, EOA, IOA, ESLL, ESLT, ESI muscles | N.A. | N.A. |
| Kong et al. (2021) [23] | Task on lower height | N.A. | Unilateral EMG: UT, ES, MD, TB, BB, BF, RF, TA muscles | N.A. | Borg CR10 |
| Schwartz et al. (2021) [45] | Lifting tasks (8 kg) | Kinematics: IMU tracking system | Bilateral EMG: ES muscle | N.A. | N.A. |
| Lazzaroni et al. (2021) [46] | Pulling tasks (10 kg–20 kg) | N.A. | Bilateral EMG: ESI, ESLL muscles | N.A. | VAS |
| Yin et al. (2021) [22] | Overhead tasks | N.A. | Unilateral EMG: AD, BB, TB, BR muscles | N.A. | N.A. |
| Weston et al. (2022) [47] | Overhead tasks | Kinematics: 3D motion capture system | Bilateral EMG: ESLL, IOA, LD, EOA, RA muscles | N.A. | Subjective ratings questionnaire |
| vam der Have et al. (2022) [48] | Lifting tasks (10 kg) and overhead tasks | Kinematics: 3D motion capture system | Unilateral EMG: LT, AD, MD, BB muscles | N.A. | N.A. |
| Kong et al. (2022) [49] | Task on lower height | Kinematics: IMU tracking system; Force: dynamometer | Unilateral EMG: MD, BB, TB, UT, ESLL, RF, TA, BF muscles | N.A. | N.A. |
| Iranzo et al. (2022) [50] | Lifting tasks (7–9 kg) | Kinematics: IMU tracking system | Unilateral EMG; ES, GMD, QF, STD muscles | N.A. | N.A. |
| Latella et al. (2022) [11] | Overhead tasks | Kinematics: IMU tracking system; Force: sensorized shoes | N.A. | N.A. | N.A. |
| De Bock et al. (2022) [51] | Lifting tasks (5 kg), overhead task and walking | N.A. | Bilateral EMG: AD, BB, TB, UT, ESLL, PM, LD muscles; heart rate; respiration | N.A. | LPD |
| Goršič et al. (2022) [52] | Lifting tasks (6.8–13.6 kg) and forward leaning tasks | Kinematics: 3D motion capture system | Bilateral EMG: ES, RA, MT muscles | N.A. | LPD |
| Sierotowicz et al. (2022) [53] | Overhead tasks | N.A. | Unilateral EMG: AD, MD, PD muscles | N.A. | N.A. |
| Mitterlehner et al. (2023) [54] | lifting, holding, carrying, bending, pushing, pulling, and walking tasks | N.A. | Heart rate | N.A. | NMQ and VAS |
| R. M. Van Sluijs et al. (2023) [55] | Forward leaning task (11 kg) | Kinematics: IMU tracking system | Unilateral EMG: ESLT, ESLL, QL, GM muscles | N.A. | N.A. |
| Garosi et al. (2023) [18] | Overhead tasks | N.A. | Bilateral EMG: SCM, SC, UT, AD muscles | N.A. | N.A. |
| Walter et al. (2023) [56] | Lifting tasks (15 kg) | N.A. | Bilateral EMG: ESL muscle | N.A. | RPE20 |
| Kong et al. (2023) [57] | Overhead tasks | N.A. | Unilateral EMG: UT, MD, BB, TB, ES, RF, BF, TA muscles | N.A. | Borg CR10 and LPD |
| Shim et al. (2023) [58] | Task on lower height | N.A. | Unilateral EMG UT, MD, TB, BB, ES, RF, BF, TA muscles | N.A. | LPD |
| Brunner et al. (2023) [59] | Lifting tasks and overhead tasks | N.A. | Heart Rate; Unilateral EMG: BB, AD, MD, TB, PD, LT, LD, ES, RA muscles | N.A. | Borg CR10 and LPD |
| Öçal et al. (2023) [21] | Overhead tasks | N.A. | Unilateral EMG: TB, BB, PM, AD, MD, PD, UT, MT, LT, LD muscles | N.A. | N.A. |
| Schrøder Jakobsen et al. (2023) [61] | Lifting tasks (4.6–17.6 kg) and overhead tasks | Kinematics: 3D motion capture system | Bilateral EMG: ESLL, UT, AD muscles | N.A. | LPD and QUEAD |
| Govaerts et al. (2023) [60] | Lifting tasks (7 kg), walking, and range of motion movements | Kinematics: 3D motion capture system | N.A. | N.A. | LPD |
| Verdel et al. (2023) [62] | Reaching tasks | Kinematics: 3D motion capture system | Unilateral EMG: BR, BB, TB, AD, PD muscles | N.A. | Subjective ratings questionnaire |
| Reimeir et al. (2023) [63] | Lifting tasks (13 kg) | Kinematics: IMU tracking system | Unilateral EMG: LD, ES, MF, EOA muscles | N.A. | N.A. |
| R.M. van Sluijs et al. (2023) [16] | Forward leaning task (6–20 kg) | Kinematics: 3D motion capture system | Unilateral EMG: ESLL, ESLT, QL, GM, BF, STD, RA muscles | N.A. | Likert scale |
| Park et al. (2023) [17] | Lifting tasks (2–7 kg) | Kinematics: IMU tracking system | Unilateral EMG: BB, TB muscles | N.A. | N.A. |
| Ding et al. (2023) [25] | Lifting tasks (10 kg) and walking | N.A. | Unilateral EMG: ESI, ESLL, RF, BF muscles | N.A. | N.A. |
| Cuttilan et al. (2023) [64] | Lifting tasks (5 kg–20 kg) | Kinematics: 3D motion capture system | Bilateral EMG: ESI, ESLT muscles | N.A. | Subjective ratings questionnaire |
| De Bock et al. (2023) [65] | Lifting tasks and overhead tasks | Kinematics: 3D motion capture system | Unilateral EMG: ESLT, ESLL, QL, GM, BF, STD, RA muscles | N.A. | N.A. |
| Bhardwaj et al. (2023) [66] | Lifting tasks (20% of the participant’s body weight) | N.A. | Bilateral EMG: MF, ESLL, LD, RA muscles | N.A. | LPD and VAS |
| Thang (2023) [67] | Overhead tasks | Kinematics: IMU tracking system | Bilateral EMG: ESLL, LT, UT muscles | N.A. | Borg CR10 and Likert scale |
| Schwartz et al. (2023) [68] | Lifting tasks (10 kg) and overhead tasks | Kinematics: IMU tracking system | Bilateral EMG: BF, GM; ES, LD, LT muscles | N.A. | N.A. |
| Musso et al. (2024) [14] | Lifting tasks (10 kg) andoverhead tasks | N.A. | Bilateral EMG: SCM, SC, UT, AD muscles | N.A. | N.A. |
| Schrøder Jakobsen et al. (2024) [69] | Lifting tasks | Kinematics: IMU tracking system | Bilateral EMG: ESL, LT, UT muscles | N.A. | Borg CR10 Likert scale and QUEAD |
| Rafique et al. (2024) [10] | Lifting tasks (5–10 kg) and overhead tasks | N.A. | EMG: thighs and calf muscles | N.A. | N.A. |
| Davoudi Kakhki et al. (2024) [70] | Lifting tasks (7 kg), carrying task and walking | N.A. | N.A. | N.A. | Borg CR10 and subjective ratings questionnaire |
| van Sluijs et al. (2024) [71] | Lifting tasks and overhead tasks | N.A. | Unilateral EMG: MD, AD, LT, ESLL, ESI, ESLT, RA, GM muscles | N.A. | Likert scale |
| Favennec et al. (2024) [72] | Lifting tasks (10 kg) and overhead tasks | Kinematics: 3D motion capture system | Unilateral EMG: GM. TFL, EOA, RA, ES muscles | N.A. | Likert scale |
| Lee et al. (2024) [73] | Lifting tasks (5 kg) and overhead tasks | N.A. | Unilateral EMG: AD, MD, PD, UT, ES muscles | N.A. | N.A. |
| Gräf et al. (2024) [15] | Overhead tasks | N.A. | Unilateral EMG: ESLL, AD, LT muscles | N.A. | N.A. |
| Govaerts et al. (2024) [74] | Lifting, holding, carrying, bending, pushing, pulling, and walking tasks | N.A. | N.A. | N.A. | VAS |
| Bär et al. (2024) [75] | Forward leaning tasks | Kinematics: dimensional gravimetric position sensors | Unilateral EMG: ES, BF, RA, VL, GTM, LT muscles; Heart Rate | N.A. | N.A. |
| Cardoso et al. (2024) [20] | Lifting tasks (4 kg) | N.A. | Bilateral EMG: ESI, ESLL, RA muscles | REBA | Borg CR10 |
| Authors (Year) | Objective | Main Conclusions |
|---|---|---|
| Moyon et al. (2018) [42] | To evaluate the physical impact of a passive exoskeleton on manual sanding operations. | The use of the exoskeleton significantly reduced cardiac cost and physical workload during sanding tasks, especially in postures with hands above shoulder level, improving overall ergonomics and reducing fatigue. However, users also noted areas for improvement in comfort and usability for longer-term use. |
| Schmalz et al. (2019) [43] | To evaluate the biomechanical and metabolic effectiveness of a passive exoskeleton in supporting overhead work and reducing the physiological and musculoskeletal strain on workers. | The exoskeleton significantly reduces muscle activity in the shoulder and upper arm, as well as heart rate and oxygen consumption, thereby alleviating the physical burden during overhead tasks, while not imposing unnatural movement patterns, making it a promising solution for reducing WMSD in overhead work. |
| Perez Luque et al. (2020) [9] | To evaluate and compare how the use of three different passive upper body exoskeletons affects the range of motion of workers during overhead manual assembly tasks. | The tested exoskeletons can effectively reduce the risk of musculoskeletal disorders in overhead tasks, different models impose varying limitations on range of motion, and further development is needed to minimize these limitations and improve overall comfort and usability for a broader range of tasks. |
| Alabdulkarim et al. (2020) [44] | To develop a low-cost exoskeleton designed to assist with anterior load carriage tasks and to evaluate its effectiveness in reducing physical demands during walking tasks with different load weights. | The exoskeleton significantly reduced muscle activity, while slightly increasing perceived discomfort in the lower back. |
| Cardoso et al. (2020) [76] | To assess the effects of a passive back-support exoskeleton on muscle activity and discomfort during industrial tasks. | The exoskeleton provides back support and reduces muscle activity by 0.8% to 3.8%; it also limits movement, interferes with task performance, and increases discomfort in various body regions, suggesting that it may not be well-suited for tasks requiring a wide range of motions. |
| Lazzaroni et al. (2020) [24] | To investigate the effects of an acceleration-based assistive strategy for controlling a back-support exoskeleton during manual lifting tasks, focusing on spine kinematics, muscle activation, and lumbar compression. | The exoskeleton reduced peak compression force on the L5S1 disk by up to 16%, with all control strategies showing similar effectiveness in reducing lumbar load. |
| Kong et al. (2021) [23] | To establish ergonomic guidelines for the use of a passive lower-limb exoskeleton by evaluating muscle activities and discomfort levels at various working heights. | The exoskeleton significantly reduces muscle activity and discomfort at working heights below 100 cm, making it beneficial for tasks performed at low heights, while its effectiveness diminishes and even increases discomfort and muscle activity at higher working heights (100–140 cm). |
| Schwartz et al. (2021) [45] | To compare the effectiveness of soft versus rigid back-support exoskeletons in reducing ES muscle activity during a dynamic lifting and lowering task, considering different trunk sagittal inclinations. | The soft exoskeleton significantly reduced ES muscle activity (by up to 11.1%) across most of the trunk inclinations, while the rigid exoskeleton showed minimal reductions and even increased muscle activity in certain positions, particularly during deep trunk flexion, suggesting that the soft design may offer better overall support during lifting tasks. |
| Lazzaroni et al. (2021) [46] | To design and evaluate a control strategy for an active back-support exoskeleton to assist with pulling tasks. | The exoskeleton control strategy significantly reduced spinal muscle activity (up to 38% reduction in mean activation) during pulling tasks, with positive subjective feedback regarding comfort, ease of use, and perceived assistance, indicating the strategy’s effectiveness in mitigating low back pain risks associated with pulling activities. |
| Yin et al. (2021) [22] | To design and test a passive upper-arm exoskeleton to reduce muscle effort in the upper limbs during repetitive manual tasks. | The exoskeleton significantly reduced muscle fatigue, particularly in the biceps brachii (up to 67.8%), and improved efficiency during both static and dynamic overhead tasks, demonstrating its effectiveness in reducing upper limb strain and the risk of WMSD. |
| Weston et al. (2022) [47] | To evaluate the physiological and biomechanical effects of three passive upper-arm exoskeletons during simulated overhead work. | The exoskeletons provided little to no significant physiological benefit in terms of tissue oxygenation during the tasks, with only one instance of statistically significant improvement. No significant increases in spinal loading or discomfort were observed, suggesting that while the exoskeletons do not substantially reduce fatigue, they also do not introduce additional strain. |
| vam der Have et al. (2022) [48] | To evaluate the Exo4Work shoulder exoskeleton’s effectiveness in reducing muscle and joint loading during simulated occupational tasks performed above shoulder height, and to examine its impact on neighboring joints. | The Exo4Work exoskeleton significantly reduces musculoskeletal loading in the shoulder and elbow during overhead tasks without increasing the load on the lower back, hip, or knee, but may increase loading during tasks performed below shoulder height, indicating its suitability primarily for overhead work. |
| Kong et al. (2022) [49] | To assess the reduction in muscle loads during bolting tasks when using a lower-limb passive exoskeleton. | Wearing the lower-limb exoskeleton significantly reduces muscle activity in the lower extremities (up to 82.4–89.4%), indicating its effectiveness in alleviating physical strain during bolting tasks, especially at lower working heights. |
| Iranzo et al. (2022) [50] | To evaluate the effectiveness of a passive lumbar exoskeleton in reducing muscle activity and fatigue during manual material handling tasks. | The exoskeleton significantly reduces muscle activity (8% to 10.2%). It also decreases fatigue, particularly in the STD muscle, while causing only minimal restrictions on the range of motion, demonstrating its potential to alleviate physical strain in tasks involving manual material handling. |
| Latella et al. (2022) [11] | To analyze the effects of using a passive upper-arm exoskeleton on whole-body joint torques during overhead work, aiming to assess the reduction in internal biomechanical loads on various body regions. | The exoskeleton significantly reduces the joint effort in the shoulders and torso (up to 86% reduction), but this effort is partially transferred to the lower limbs, particularly the hips and thighs, highlighting both the benefits and redistribution of mechanical loads across the body. |
| De Bock et al. (2022) [51] | To assess the effects of a passive shoulder exoskeleton on muscle activity, muscle fatigue, and subjective experiences during overhead and non-overhead industrial tasks. | The exoskeleton significantly reduces muscle activity and fatigue in the anterior deltoid (up to 16% reduction in muscle activity and 41% reduction in fatigue) during isometric overhead work. However, it minimally impacts dynamic tasks and can increase discomfort at body-exoskeleton contact points. |
| Goršič et al. (2022) [52] | To evaluate the short-term effects of passive back support exoskeleton on muscle activity and user comfort during lifting and static leaning task. | The reduced electromyographic activity in the ES and MT muscles during both lifting and leaning tasks. However, it was found to be suboptimal for long-term use, as participants reported mild to moderate discomfort, particularly around the hips, due to the stiffness of the exoskeleton design. |
| Sierotowicz et al. (2022) [53] | To assess the effectiveness of an adaptive industrial exoskeleton using force myography to adjust support levels in real-time during overhead work. | The adaptive control system successfully reduced shoulder muscle activity by up to 31% during lifting tasks by adjusting the level of assistance based on the weight lifted, leading to improved shoulder stability and reduced strain without compromising user comfort or range of motion. |
| Mitterlehner et al. (2023) [54] | To evaluate both the objective and subjective effects of a passive low-back exoskeleton during simulated logistics tasks, focusing on heart rate, trunk kinematics, throughput, and user experience. | While the exoskeleton showed minimal impact on heart rate and throughput, it significantly reduced trunk acceleration and inclination in certain tasks, although users reported moderate discomfort and restrictions in movement, suggesting the need for task-specific adaptations and improvements in usability. |
| R. M. Van Sluijs et al. (2023) [55] | To develop a method to quantify the reduction in back and hip muscle fatigue provided by lift-support exoskeletons during static forward-leaning task. | The exoskeleton significantly reduced muscle activity in the ESLT and ESLL muscles (by 33% and 13.2%, respectively) and the GM muscle (16.3%). Additionally, the exoskeleton delayed muscle fatigue, particularly in the GM and QL muscles, demonstrating its effectiveness in reducing physical strain during lifting tasks. |
| Garosi et al. (2023) [18] | To investigate the effects of a passive head/neck supporting exoskeleton on the electromyographic fatigue threshold of neck and shoulder muscles during repetitive overhead tasks. | The exoskeleton significantly delayed the onset of muscle fatigue in the sternocleidomastoid and trapezius muscles, suggesting its potential as an ergonomic intervention to reduce musculoskeletal risks, although further studies are needed to evaluate its broader application. |
| Walter et al. (2023) [56] | To examine how an active exoskeleton reduces erector spinae muscle activity during lifting tasks and to assess its impact on muscle activation and perceived exertion under different support levels. | The active exoskeleton significantly reduces ES muscle activity and perceived exertion during lifting tasks, with greater reductions observed as the support level increases, indicating the exoskeleton’s potential to lower physical strain and mitigate the risk of musculoskeletal disorders. |
| Kong et al. (2023) [57] | To evaluate the efficacy of two passive upper-arm exoskeletons in reducing musculoskeletal load and muscle activity during overhead tasks in industrial settings. | The passive upper-arm exoskeletons significantly reduce muscle activity in the upper limb muscles, indicating their potential as an effective intervention for reducing physical exertion and WMSD risks during overhead tasks, although the effects on subjective discomfort were minimal. |
| Shim et al. (2023) [58] | To evaluate the effects of passive lower-limb exoskeletons on muscle activity during tasks performed at various working heights, focusing on both upper and lower-limb muscle responses and discomfort levels. | Passive lower-limb exoskeletons significantly reduce muscle activity in the lower limbs, particularly at lower working heights, while increasing upper-limb muscle activity at higher working heights, suggesting that the use of these exoskeletons is more beneficial at working heights of 85 cm or lower to optimize ergonomic benefits. |
| Brunner et al. (2023) [59] | To evaluate the effect of a passive shoulder exoskeleton, on muscle activity, cardiac cost, and perceived exertion during overhead tasks, aiming to reduce the physical strain associated with WMSD. | Significantly reduced muscle activity (up to 64% in the deltoideus medius), cardiac cost (15%), and perceived exertion (21.5%) during overhead tasks, without increasing the load on the lower back or abdomen, demonstrating its potential as an effective intervention for workers at high WMSD risk. |
| Öçal et al. (2023) [21] | To develop an innovative passive upper-arm exoskeleton and investigate its effects on muscle activity during overhead and extended forearm tasks. | The exoskeleton significantly reduces muscle activity, with up to a 55% reduction in the middle deltoid and 48% in the anterior deltoid during overhead tasks, showing its potential for improving worker comfort and reducing WMSD risk. |
| Schrøder Jakobsen et al. (2023) [61] | To evaluate the biomechanical changes, acceptance, and usability of a passive shoulder exoskeleton during manual material handling tasks in a logistics environment, focusing on muscle activity, perceived effort, and user feedback, after a five-week familiarization period. | The exoskeleton significantly reduced muscle activity in the AD (13–39%) and UT muscle (16–60%), along with a reduction in perceived effort. However, the familiarization period showed low adherence, and workers expressed decreased positive emotions towards the exoskeleton, raising concerns about its suitability for long-term use in logistics. |
| Govaerts et al. (2023) [60] | To compare the effects of an active and passive industrial back-support exoskeleton on physical work performance during simulated material handling tasks. | Both exoskeletons hindered physical work performance by increasing movement duration compared to no exoskeleton, particularly in tasks involving walking and trunk bending. |
| Verdel et al. (2023) [62] | To investigate the trade-off between mechanical complexity and interaction quality in upper-limb exoskeleton interfaces by analyzing the influence of passive rotations in the forearm interface during sagittal plane reaching movements. | Incorporating passive degrees of freedom in the forearm interface significantly improves interaction quality by reducing interaction forces and muscle activity without compromising kinematics, offering a promising design solution for balancing complexity and usability in exoskeletons. |
| Reimeir et al. (2023) [63] | To investigate the acute effects of five different back-support exoskeletons (active and passive), on trunk muscle activity and joint kinematics during a combined logistics task. | The exoskeletons significantly reduced muscle activity during lifting tasks, with passive exoskeletons showing a notable reduction in trunk flexion and task duration. However, the support provided by these devices varies depending on their functional mechanisms, highlighting the need for exoskeletons to be assessed according to their designed force paths to ensure long-term injury prevention. |
| R.M. van Sluijs et al. (2023) [16] | To evaluate the physiological benefits of a passive back-support exoskeleton during lifting tasks and forward-leaning postures. | The exoskeleton significantly reduces muscle activity in the back (up to 25.59% during forward leaning and 20.52% during lifting) without affecting leg and abdominal muscle activity or joint kinematics, indicating that the exoskeleton can alleviate physical strain during repetitive lifting and forward-leaning tasks. |
| Park et al. (2023) [17] | To design, control, and validate a novel elbow exoskeleton, aimed at assisting elbow flexion and extension during occupational tasks, while minimizing joint misalignment and discomfort. | The exoskeleton significantly reduces muscle activation in the BB and TB muscles (up to 38.8% and 37%, respectively, for a 2 kg load) without overly restricting elbow range of motion, making it a promising tool for reducing muscle strain during repetitive industrial tasks. |
| Ding et al. (2023) [25] | To develop and validate a novel passive back-support exoskeleton with a spring-cable-differential mechanism, designed to assist with lifting tasks while minimizing resistance during walking, to reduce the risk of lower back injuries. | The exoskeleton effectively reduces ES muscle activation by up to 41% during lifting tasks without significantly affecting leg and back muscle activity during walking, demonstrating its potential to alleviate lower back strain while maintaining comfort during movement. |
| Cuttilan et al. (2023) [64] | To investigate the effectiveness of a fabric-based, pneumatic exoskeleton in reducing lower-back muscle activation and discomfort during manual handling tasks | The exoskeleton significantly reduces muscle activation of the erector spinae at the L5 level (up to 35% during lifting tasks), without limiting the range of motion or increasing discomfort, making it a promising tool for reducing the risk of lower-back. |
| De Bock et al. (2023) [65] | To investigate how a passive shoulder exoskeleton mitigates the effects of physical fatigue on overhead work precision performance, muscle activity, and shoulder kinematics. | The exoskeleton reduces muscle activity in the anterior and medial deltoid muscles and mitigates fatigue-induced changes in shoulder joint kinematics, particularly reducing compensatory movements during overhead work. However, the exoskeleton did not significantly impact precision performance. |
| Bhardwaj et al. (2023) [66] | To investigate the effect of moment arm orientation in a passive back-assist exosuit on device-to-body forces, perceived discomfort, and muscle activity during lifting and lowering tasks. | The moment arm configuration significantly impacts the device-to-body forces, with the C4 configuration reducing forces at the shoulder and waist by up to 44.6% and 22.2%, respectively, while also minimizing perceived discomfort, demonstrating the importance of optimizing exoskeleton design for user comfort and effectiveness. |
| Thang (2023) [67] | To evaluate the effectiveness of a passive exoskeleton in reducing muscle strain and discomfort during overhead lifting tasks. | The passive exoskeleton significantly reduced muscle activity in the anterior and medial deltoid muscles by 30% to 80% across different payloads, with greater reductions observed at heavier loads. The exoskeleton also decreased discomfort in the shoulders and back, demonstrating its potential to reduce the WMSD risk during repetitive overhead tasks. |
| Schwartz et al. (2023) [68] | To evaluate the biomechanical consequences of using passive and active back-support exoskeletons during various manual handling tasks. | Both passive and active exoskeletons reduce trunk extensor muscle activity, but active exoskeletons provide greater reductions (up to 62%) compared to passive ones (up to 27%). Active exoskeletons also tend to alter trunk kinematics more significantly, particularly in dynamic tasks, highlighting the importance of task-specific exoskeleton selection. |
| Musso et al. (2024) [14] | To assess the impact of an upper-limb exoskeleton on muscle activity during various construction and manufacturing tasks, including overhead assembly, bricklaying, and box moving, to determine its potential in reducing. | The exoskeleton effectively reduces shoulder muscle activation during tasks performed above shoulder level, such as overhead assembly, but increases muscle activation for tasks below shoulder level, like bricklaying and box moving, indicating task-specific benefits and limitations that should be considered for ergonomic optimization. |
| Schrøder Jakobsen et al. (2024) [69] | To investigate how on-site training with a passive back exoskeleton affects the biomechanics of logistic workers, specifically focusing on muscle activity, joint kinematics, and the acceptance and comfort of the device after a 5-week training period. | The exoskeleton training optimized the interaction between the workers and the device, resulting in a 6–9% reduction in peak back muscle activity and a decrease in knee flexion, promoting a more stooped lifting technique, which suggests the benefits of incorporating training when implementing passive exoskeletons in logistics to reduce biomechanical load. |
| Rafique et al. (2024) [10] | To evaluate the benefits of passive exoskeletons in reducing muscle effort and preventing WMSD in workers performing physically demanding tasks, and to provide recommendations for design improvements. | The passive exoskeletons significantly reduce muscle activity (up to 66% for upper body tasks and up to 54% for lower body tasks), demonstrating their potential to alleviate the physical strain associated WMSD, although further design enhancements are necessary to improve user comfort and biomechanical compatibility. |
| Davoudi Kakhki et al. (2024) [70] | To evaluate the efficacy of a passive back-support exoskeleton in enhancing ergonomics and reducing physical discomfort during manual handling tasks. | The exoskeleton significantly reduced discomfort and physical exertion in the lower back, shoulders, and knees, demonstrating its potential to improve ergonomic posture and prevent musculoskeletal disorders, although some users reported constraints on movement and moderate physical effort while using the device. |
| van Sluijs et al. (2024) [71] | To present the design and evaluate the effectiveness of a passive multi-joint exoskeleton, in reducing muscle activity and supporting both back and shoulder during full-range vertical lifting tasks. | The exoskeleton significantly reduces muscle activity in the deltoid, trapezius, and ES muscles (by up to 75% for the shoulder and 31% for the back), demonstrating its potential to alleviate physical strain in occupations requiring dynamic movements across a large vertical range. |
| Favennec et al. (2024) [72] | To characterize the familiarization process with a soft back-support occupational exoskeleton and determine the time required for stabilizing biomechanical variables such as joint kinematics, postural stability, muscle activity, and performance during stoop and squat lifting tasks. | The familiarization process for the soft back-support exoskeleton leads to significant changes in thoracic kinematics, pressure perception, and performance, with stabilization occurring after three or four sessions. This suggests that workers need approximately four familiarization sessions, each lasting one hour, for their motor control and exoskeleton perception to stabilize, ensuring accurate long-term assessments of exoskeleton benefits. |
| Lee et al. (2024) [73] | To propose a novel passive shoulder exoskeleton using link chains and magnetic spring joints, aimed at supporting the upper arm during overhead work and reducing musculoskeletal strain in the shoulders. | The exoskeleton significantly reduced shoulder muscle activity (up to 30% for AD muscles during overhead tasks) while providing effective torque assistance without compromising range of motion, making it a promising solution for preventing shoulder injuries during repetitive overhead tasks. |
| Gräf et al. (2024) [15] | To evaluate the impact of a passive upper-body exoskeleton on muscle activity and precision during overhead single and dual tasks. | The exoskeleton significantly reduced muscle activity in the deltoideus and trapezius muscles, particularly under dual-task conditions, and improved precision after fatigue, highlighting its potential to support overhead work while reducing musculoskeletal strain without compromising task accuracy. |
| Govaerts et al. (2024) [74] | To compare the functional performance impacts, perceived task difficulty and general discomfort of active and passive industrial back exoskeletons during various work-related tasks. | The active exoskeleton significantly hindered work performance in multiple tasks (up to 22%), especially in dynamic activities such as walking and stair climbing, while the passive exoskeleton performed comparably to no exoskeleton in most tasks. |
| Bär et al. (2024) [75] | To evaluate the effects of using a passive back exoskeleton during a simulated sorting task that involves a static forward bent posture, focusing on its influence on muscle activity, posture, and heart rate. | The exoskeleton significantly reduced BF muscle activity (by 8.1%) and showed minor reductions in ES muscle activity (by 1.3%), with increased hip and knee flexion angles and a slight decrease in heart rate (by 2.1 bpm), suggesting that the exoskeleton primarily supports hip extension during tasks requiring a forward bent posture. |
| Cardoso et al. (2024) [20] | To assess the short-term effects of using dual passive back-support exoskeletons on WMSD risk factors in logistics operations. | Both exoskeletons reduced perceived exertion, especially during tasks involving trunk flexion, and improved posture during manual lifting tasks. The Htrius exoskeleton showed slightly better performance in reducing lumbar muscle activity and improving comfort, suggesting its potential for reducing WMSD risk in logistics operations. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cardoso, A.; Ribeiro, A.; Carneiro, P.; Colim, A. Evaluating Exoskeletons for WMSD Prevention: A Systematic Review of Applications and Ergonomic Approach in Occupational Settings. Int. J. Environ. Res. Public Health 2024, 21, 1695. https://doi.org/10.3390/ijerph21121695
Cardoso A, Ribeiro A, Carneiro P, Colim A. Evaluating Exoskeletons for WMSD Prevention: A Systematic Review of Applications and Ergonomic Approach in Occupational Settings. International Journal of Environmental Research and Public Health. 2024; 21(12):1695. https://doi.org/10.3390/ijerph21121695
Chicago/Turabian StyleCardoso, André, Andreia Ribeiro, Paula Carneiro, and Ana Colim. 2024. "Evaluating Exoskeletons for WMSD Prevention: A Systematic Review of Applications and Ergonomic Approach in Occupational Settings" International Journal of Environmental Research and Public Health 21, no. 12: 1695. https://doi.org/10.3390/ijerph21121695
APA StyleCardoso, A., Ribeiro, A., Carneiro, P., & Colim, A. (2024). Evaluating Exoskeletons for WMSD Prevention: A Systematic Review of Applications and Ergonomic Approach in Occupational Settings. International Journal of Environmental Research and Public Health, 21(12), 1695. https://doi.org/10.3390/ijerph21121695









