Nature and Mental Health in Urban Texas: A NatureScore-Based Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Setting and Study Design
2.1.1. Texas Outpatient Encounters Data
2.1.2. Rural-Urban Commuting Area (RUCA) Codes
2.1.3. U.S. Census Data
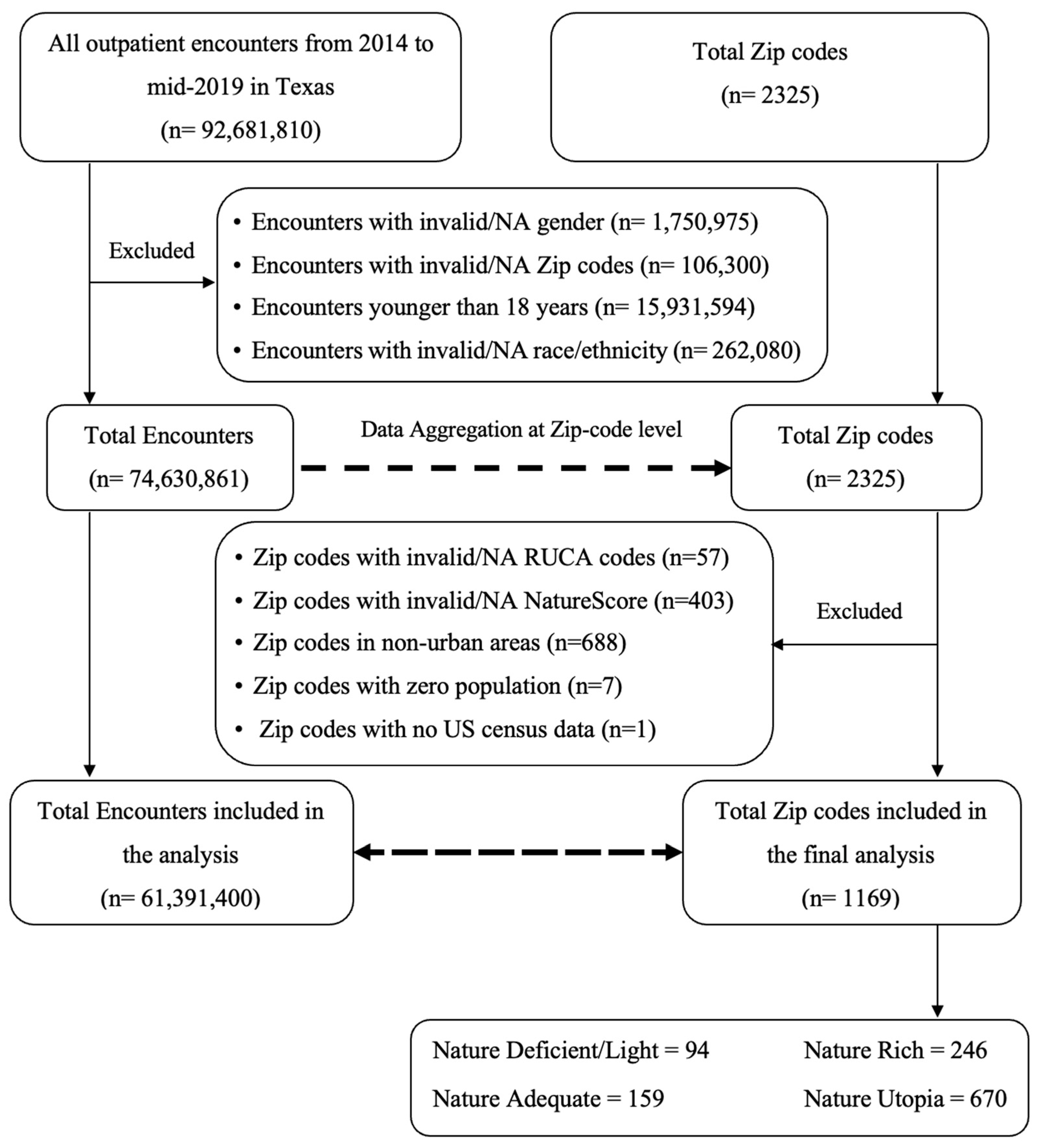
2.2. Study Population
2.3. Study Variables
2.3.1. Exposure of Interest: NatureScore
2.3.2. Outcome of Interest: Mental Health Encounters per 100,000 Population
2.3.3. Covariates
2.4. Statistical Analyses
3. Results
3.1. NatureScore
3.2. Demographic and Socioeconomic Factors
3.3. Mental Health and NatureScore
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nguyen, P.Y.; Astell-Burt, T.; Rahimi-Ardabili, H.; Feng, X. Effect of nature prescriptions on cardiometabolic and mental health, and physical activity: A systematic review. Lancet Planet Health 2023, 7, e313–e328. [Google Scholar] [CrossRef]
- Yau, K.K.; Loke, A.Y. Effects of forest bathing on pre-hypertensive and hypertensive adults: A review of the literature. Environ. Health Prev. Med. 2020, 25, 23. [Google Scholar] [CrossRef] [PubMed]
- Birch, J.; Rishbeth, C.; Payne, S.R. Nature doesn’t judge you—How urban nature supports young people’s mental health and wellbeing in a diverse UK city. Health Place 2020, 62, 102296. [Google Scholar] [CrossRef]
- de Bell, S.; White, M.; Griffiths, A.; Darlow, A.; Taylor, T.; Wheeler, B.; Lovell, R. Spending time in the garden is positively associated with health and wellbeing: Results from a national survey in England. Landsc. Urban Plan. 2020, 200, 103836. [Google Scholar] [CrossRef]
- Remme, R.P.; Frumkin, H.; Guerry, A.D.; King, A.C.; Mandle, L.; Sarabu, C.; Bratman, G.N.; Giles-Corti, B.; Hamel, P.; Han, B.; et al. An ecosystem service perspective on urban nature, physical activity, and health. Proc. Natl. Acad. Sci. USA 2021, 118, e2018472118. [Google Scholar] [CrossRef] [PubMed]
- Substance Abuse and Mental Health Services Administration (SAMHSA). Key Substance Use and Mental Health Indicators in the United States: Results from the 2019 National Survey on Drug Use and Health; Substance Abuse and Mental Health Services Administration (SAMHSA): Rockville, MD, USA, 2020. [Google Scholar]
- Mwoka, M.; Biermann, O.; Ettman, C.K.; Abdalla, S.M.; Ambuko, J.; Pearson, M.; Rashid, S.F.; Zeinali, Z.; Galea, S.; Valladares, L.M.; et al. Housing as a Social Determinant of Health: Evidence from Singapore, the UK, and Kenya: The 3-D Commission. J. Urban Health 2021, 98, 15–30. [Google Scholar] [CrossRef]
- Prokosch, C.; Fertig, A.R.; Ojebuoboh, A.R.; Trofholz, A.C.; Baird, M.; Young, M.; de Brito, J.N.; Kunin-Batson, A.; Berge, J.M. Exploring associations between social determinants of health and mental health outcomes in families from socioeconomically and racially and ethnically diverse households. Prev. Med. 2022, 161, 107150. [Google Scholar] [CrossRef]
- Feng, X.; Toms, R.; Astell-Burt, T. The nexus between urban green space, housing type, and mental health. Soc. Psychiatry Psychiatr. Epidemiol. 2022, 57, 1917–1923. [Google Scholar] [CrossRef] [PubMed]
- Gonzales-Inca, C.; Pentti, J.; Stenholm, S.; Suominen, S.; Vahtera, J.; Käyhkö, N. Residential greenness and risks of depression: Longitudinal associations with different greenness indicators and spatial scales in a Finnish population cohort. Health Place 2022, 74, 102760. [Google Scholar] [CrossRef]
- Perrino, T.; Lombard, J.; Rundek, T.; Wang, K.; Dong, C.; Gutierrez, C.M.; Toro, M.; Byrne, M.M.; Nardi, M.I.; Kardys, J.; et al. Neighbourhood greenness and depression among older adults. Br. J. Psychiatry 2019, 215, 476–480. [Google Scholar] [CrossRef]
- Klompmaker, J.O.; Hart, J.E.; Bailey, C.R.; Browning, M.H.; Casey, J.A.; Hanley, J.R.; Minson, C.T.; Ogletree, S.S.; Rigolon, A.; Laden, F. Racial, ethnic, and socioeconomic disparities in multiple measures of blue and green spaces in the United States. Environ. Health Perspect. 2023, 131, 017007. [Google Scholar] [CrossRef]
- Texas Department of State Health Services, Center for Health Statistics. Texas Outpatient Public Use Data File: Quarters 1–4: Years 2014–2018. Quarters 1–2: Year 2019; Texas Department of State Health Services, Center for Health Statistics: Austin, TX, USA, [cited October 2020]. Available online: https://www.dshs.texas.gov/texas-health-care-information-collection/health-data-researcher-information/texas-outpatient-public-use (accessed on 1 January 2023).
- U.S. Department of Agriculture Economic Research Service (USDA-ERS). Rural-Urban Commuting Area (RUCA) Codes, ZIP Code File (Last Updated 17 August 2020). Available online: https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes.aspx (accessed on 1 January 2023).
- Robertson, B.D.; McConnel, C.E. Town-level comparisons may be an effective alternative in comparing rural and urban differences: A look at accidental traumatic brain injuries in North Texas children. Rural. Remote Health 2011, 11, 65–74. [Google Scholar] [CrossRef]
- Robertson, B. Differences in Service Delivery and Patient Outcome between Rural and Urban Areas: The Case of Traumatic Brain Injury at a Level I Pediatric Trauma Center in North Texas; UMI/ProQuest: Ann Arbor, MI, USA, 2010. [Google Scholar]
- United States Census Bureau. American Community Survey 5-Year Estimates (2016–2020). Available online: https://www.census.gov/programs-surveys/acs (accessed on 1 January 2023).
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Theobald, D.M. A general model to quantify ecological integrity for landscape assessments and US application. Landsc. Ecol. 2013, 28, 1859–1874. [Google Scholar] [CrossRef]
- Browning, M.H.E.M.; Hanley, J.R.; Bailey, C.R.; Beatley, T.; Gailey, S.; Hipp, J.A.; Larson, L.R.; James, P.; Jennings, V.; Jimenez, M.P.; et al. Quantifying Nature: Introducing NatureScoreTM and NatureDoseTM as Health Analysis and Promotion Tools. Am. J. Health Promot. 2024, 38, 126–134. [Google Scholar] [CrossRef] [PubMed]
- Feng, X.; Astell-Burt, T. Residential green space quantity and quality and symptoms of psychological distress: A 15-year longitudinal study of 3897 women in postpartum. BMC Psychiatry 2018, 18, 348. [Google Scholar] [CrossRef]
- Pasanen, T.; Johnson, K.; Lee, K.; Korpela, K. Can Nature Walks with Psychological Tasks Improve Mood, Self-Reported Restoration, and Sustained Attention? Results from Two Experimental Field Studies. Front. Psychol. 2018, 9, 2057. [Google Scholar] [CrossRef]
- Ojala, A.; Korpela, K.; Tyrväinen, L.; Tiittanen, P.; Lanki, T. Restorative effects of urban green environments and the role of urban-nature orientedness and noise sensitivity: A field experiment. Health Place 2019, 55, 59–70. [Google Scholar] [CrossRef] [PubMed]
- White, M.P.; Alcock, I.; Grellier, J.; Wheeler, B.W.; Hartig, T.; Warber, S.L.; Bone, A.; Depledge, M.H.; Fleming, L.E. Spending at least 120 minutes a week in nature is associated with good health and wellbeing. Sci. Rep. 2019, 9, 7730. [Google Scholar] [CrossRef]
- Hunter, M.R.; Gillespie, B.W.; Chen, S.Y. Urban Nature Experiences Reduce Stress in the Context of Daily Life Based on Salivary Biomarkers. Front. Psychol. 2019, 10, 722. [Google Scholar] [CrossRef]
- Hunter, R.F.; Christian, H.; Veitch, J.; Astell-Burt, T.; Hipp, J.A.; Schipperijn, J. The impact of interventions to promote physical activity in urban green space: A systematic review and recommendations for future research. Soc. Sci. Med. 2015, 124, 246–256. [Google Scholar] [CrossRef] [PubMed]
- Mytton, O.T.; Townsend, N.; Rutter, H.; Foster, C. Green space and physical activity: An observational study using Health Survey for England data. Health Place 2012, 18, 1034–1041. [Google Scholar] [CrossRef] [PubMed]
- Washington State Department of Health; Hailu, A.; Wasserman, C. Guidelines for Using Rural-Urban Classification Systems for Community Health Assessment. Available online: https://doh.wa.gov/sites/default/files/legacy/Documents/1500//RUCAGuide.pdf (accessed on 1 January 2023).
- Health Resources and Services Administration (HRSA). Defining Rural Population. Available online: https://www.hhs.gov/guidance/document/defining-rural-population (accessed on 1 January 2023).
- Burke, B.T.; Miller, B.F.; Proser, M.; Petterson, S.M.; Bazemore, A.W.; Goplerud, E.; Phillips, R.L. A needs-based method for estimating the behavioral health staff needs of community health centers. BMC Health Serv. Res. 2013, 13, 245. [Google Scholar] [CrossRef] [PubMed]


| Summary Statistics, Mean (SD) | ||||||
|---|---|---|---|---|---|---|
| Total | Nature Deficient/Nature Light | Nature Adequate | Nature Rich | Nature Utopia | p-Value # | |
| No. of Zipcodes | 1169 | 94 (8%) | 159 (14%) | 246 (21%) | 670 (57%) | |
| Total outpatient encounters | 61,391,398 | 3,826,697 (6.2%) | 10,485,831 (17.1%) | 18,408,516 (30%) | 28,670,354 (46.7%) | |
| NatureScore + | 85.8 (64.8–94.7) | 30.35 (19.5–36.8) | 50.3 (46.7–57.0) | 71.5 (66.6–75.9) | 93.4 (89.1–97.4) | <0.001 + |
| Demographics | ||||||
| Total population (18+) from Census data, No. | 18,677,889 | 1,189,009 | 3,289,630 | 5,870,487 | 8,328,763 | |
| Population (18+) per Zipcode, Mean (SD) | 15,978 (15,566) | 12,649 (14,181) | 20,689 (15,529) | 23,864 (15,494) | 12,431 (14,419) | <0.001 |
| Women, % | 63.07 (4.38) | 60.72 (8.02) | 64.25 (4.25) | 64.62 (3.43) | 62.55 (3.70) | <0.001 |
| Age 18–44, % | 34.21 (10.35) | 39.96 (13.41) | 38.06 (11.28) | 36.65 (9.68) | 31.60 (8.96) | <0.001 |
| Age 45–64, % | 35.82 (4.83) | 34.77 (7.22) | 35.16 (5.70) | 36.23 (4.61) | 35.97 (4.20) | 0.02 |
| Age 65+, % | 29.97 (9.25) | 25.27 (10.54) | 26.78 (9.15) | 27.12 (8.35) | 32.43 (8.61) | <0.001 |
| White, % | 54.09 (24.98) | 36.17 (19.85) | 39.51 (21.47) | 45.46 (23.22) | 63.23 (22.83) | <0.001 |
| Black, % | 12.15 (15.96) | 11.37 (12.85) | 12.61 (14.58) | 16.70 (18.24) | 10.48 (15.46) | <0.001 |
| Asian, % | 1.63 (2.57) | 1.34 (1.79) | 2.58 (3.92) | 2.52 (2.89) | 1.12 (1.91) | <0.001 |
| Hispanic, % | 15.21 (17.79) | 31.12 (23.64) | 22.48 (22.02) | 14.72 (16.35) | 11.43 (14.15) | <0.001 |
| Socioeconomic Factors | ||||||
| Bachelor’s degree or above, % | 26.79 (18.07) | 27.94 (21.28) | 27.65 (20.47) | 32.14 (19.46) | 24.46 (15.91) | <0.001 |
| Employment, % | 58.36 (11.41) | 55.74 (15.85) | 59.87 (12.16) | 62.14 (9.17) | 56.98 (10.86) | <0.001 |
| Poverty, % | 14.43 (10.64) | 20.89 (12.74) | 18.65 (12.87) | 14.68 (9.40) | 12.45 (9.46) | <0.001 |
| Median Household Income, $ | 66,268 (27,112) | 52,289 (22,075) | 57,140 (23,427) | 69,468 (32,471) | 69,237 (25,261) | <0.001 |
| Lack of insurance, % | 17.03 (9.25) | 19.61 (9.88) | 19.79 (9.76) | 17.89 (9.46) | 15.71 (8.70) | <0.001 |
| Mental Health Encounters, per 100,000 population * | ||||||
| Any Mental Illness | 2532.17 (4532.91) | 4044.86 (5859.35) | 3439.97 (9807.87) | 2056.48 (1141.47) | 2279.16 (2690.77) | <0.001 |
| Depression | 548.35 (946.24) | 1212.44 (2622.31) | 582.41 (1031.99) | 487.42 (334.89) | 469.48 (494.84) | <0.001 |
| Bipolar | 196.54 (579.02) | 553.25 (1647.49) | 226.69 (588.05) | 165.74 (128.29) | 150.64 (315.85) | <0.001 |
| Anxiety/Stress | 1787.28 (3858.40) | 2279.16 (2001.52) | 2630.87 (9128.61) | 1403.33 (868.01) | 1659.04 (2281.28) | 0.006 |
| Univariable Regression Analysis | ||||
| Any Mental Health | Depression | Bipolar | Anxiety/Stress | |
| RR (95%CI) | RR (95%CI) | RR (95%CI) | RR (95%CI) | |
| No. of Zipcodes | 1161 $ | 1118 + | 1017 # | 1159 β |
| NatureScore Categories | ||||
| Nature Deficient/Nature Light | Reference | Reference | Reference | Reference |
| Nature Adequate | 0.856 (0.504–1.453) | 0.485 ** (0.291–0.811) | 0.368 ** (0.180–0.751) | 1.162 (0.660–2.046) |
| Nature Rich | 0.510 ** (0.378–0.689) | 0.405 ** (0.260–0.630) | 0.265 ** (0.145–0.482) | 0.618 ** (0.510–0.750) |
| Nature Utopia | 0.569 ** (0.419–0.771) | 0.401 ** (0.258–0.623) | 0.270 ** (0.146–0.498) | 0.737 ** (0.600–0.904) |
| Demographics | ||||
| Women % | 0.220 (0.017–2.896) | 0.013 ** (0.002–0.074) | 0.005 ** (0.000–0.076) | 1.030 (0.059–17.959) |
| Age 18–44 % | 0.838 (0.219–3.203) | 4.434 ** (1.507–13.049) | 3.588 (0.654–19.681) | 0.335 (0.091–1.239) |
| Age 45–64 % | 4.977 (0.269–91.987) | 4.495 (0.213–94.769) | 10.103 (0.055–1844.009) | 3.487 (0.124–98.133) |
| Age 65+ % | 0.891 (0.256–3.102) | 0.168 ** (0.075–0.377) | 0.224 * (0.055–0.919) | 2.879 (0.704–11.765) |
| White, % | 0.500 ** (0.345–0.724) | 0.577 ** (0.415–0.802) | 0.528 * (0.290–0.959) | 0.497 ** (0.325–0.761) |
| Black % | 1.655 (0.940–2.915) | 5.390 ** (2.667–10.895) | 7.225 ** (2.722–19.178) | 0.963 (0.545–1.703) |
| Asian % | 0.001 ** (0.000–0.003) | 0.004 ** (0.001–0.015) | 0.001 ** (0.000–0.004) | 0.000 ** (0.000–0.002) |
| Hispanic % | 3.091 ** (1.722–5.548) | 0.720 (0.455–1.141) | 0.901 (0.370–2.192) | 4.571 ** (2.576–8.110) |
| Socioeconomic Factors | ||||
| Employment % | 0.990 * (0.983–0.998) | 0.996 (0.987–1.004) | 0.997 (0.988–1.007) | 0.987 ** (0.979–0.995) |
| Bachelor’s degree or above % | 0.995 (0.987–1.003) | 0.998 (0.991–1.004) | 0.998 (0.990–1.005) | 0.994 (0.985–1.003) |
| Poverty % | 1.013 ** (1.005–1.021) | 1.013 ** (1.004–1.023) | 1.017 * (1.002–1.033) | 1.012 ** (1.004–1.020) |
| Multivariable Regression Analysis | ||||
| Any Mental health | Depression | Bipolar | Anxiety/Stress | |
| aRR (95%CI) | aRR (95%CI) | aRR (95%CI) | aRR (95%CI) | |
| No. of Zipcodes | 1159 | 1116 | 1016 | 1157 |
| NatureScore Categories | ||||
| Nature Deficient/Nature Light | Reference | Reference | Reference | Reference |
| Nature Adequate | 1.053 (0.689–1.608) | 0.926 (0.643–1.332) | 0.743 (0.439–1.259) | 1.265 (0.901–1.778) |
| Nature Rich | 0.746 (0.512–1.087) | 0.769 (0.546–1.082) | 0.725 (0.439–1.198) | 0.883 (0.690–1.131) |
| Nature Utopia | 0.734 (0.507–1.064) | 0.683 * (0.490–0.950) | 0.594 * (0.355–0.994) | 0.910 (0.712–1.163) |
| Demographics | ||||
| Women % | 0.107 ** (0.025–0.468) | 0.023 ** (0.004–0.125) | 0.001 ** (0.000–0.016) | 0.230 * (0.054–0.977) |
| Age 45–64 % | 4.570 (0.852–24.501) | 1.092 (0.118–10.124) | 3.943 (0.313–49.670) | 4.137 (0.918–18.636) |
| Age 65+ % | 1.667 (0.729–3.816) | 0.410 (0.139–1.206) | 8.513 ** (1.688–42.948) | 2.072 (0.964–4.456) |
| Black % | 2.881 ** (1.765–4.704) | 3.279 ** (2.105–5.109) | 9.819 ** (3.964–24.323) | 2.312 ** (1.338–3.995) |
| Asian % | 0.004 ** (0.000–0.026) | 0.006 ** (0.001–0.046) | 0.034 * (0.001–0.952) | 0.004 ** (0.000–0.030) |
| Hispanic % | 2.216 ** (1.516–3.241) | 0.584 * (0.387–0.881) | 0.723 (0.435–1.201) | 3.502 ** (2.315–5.296) |
| Socioeconomic Factors | ||||
| Employment % | 1.002 (0.993–1.012) | 0.993 (0.980–1.007) | 1.014 (0.999 - 1.030) | 1.001 (0.993–1.009) |
| Bachelor’s degree or above % | 0.994 * (0.989–0.999) | 0.997 (0.991–1.003) | 0.989 ** (0.983 - 0.994) | 0.993 ** (0.988–0.998) |
| Poverty % | 1.004 (0.995–1.013) | 0.998 (0.986–1.010) | 1.019 ** (1.007 - 1.032) | 1.001 (0.993–1.009) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Makram, O.M.; Pan, A.; Maddock, J.E.; Kash, B.A. Nature and Mental Health in Urban Texas: A NatureScore-Based Study. Int. J. Environ. Res. Public Health 2024, 21, 168. https://doi.org/10.3390/ijerph21020168
Makram OM, Pan A, Maddock JE, Kash BA. Nature and Mental Health in Urban Texas: A NatureScore-Based Study. International Journal of Environmental Research and Public Health. 2024; 21(2):168. https://doi.org/10.3390/ijerph21020168
Chicago/Turabian StyleMakram, Omar M., Alan Pan, Jay E. Maddock, and Bita A. Kash. 2024. "Nature and Mental Health in Urban Texas: A NatureScore-Based Study" International Journal of Environmental Research and Public Health 21, no. 2: 168. https://doi.org/10.3390/ijerph21020168
APA StyleMakram, O. M., Pan, A., Maddock, J. E., & Kash, B. A. (2024). Nature and Mental Health in Urban Texas: A NatureScore-Based Study. International Journal of Environmental Research and Public Health, 21(2), 168. https://doi.org/10.3390/ijerph21020168






