Burden of Disease Due to Air Pollution in Afghanistan—Results from the Global Burden of Disease Study 2019
Abstract
1. Introduction
2. Methods
2.1. Data Source
2.2. Main Input Data
2.3. Measures
2.4. Air Pollution—Level 2 Risk
3. Results
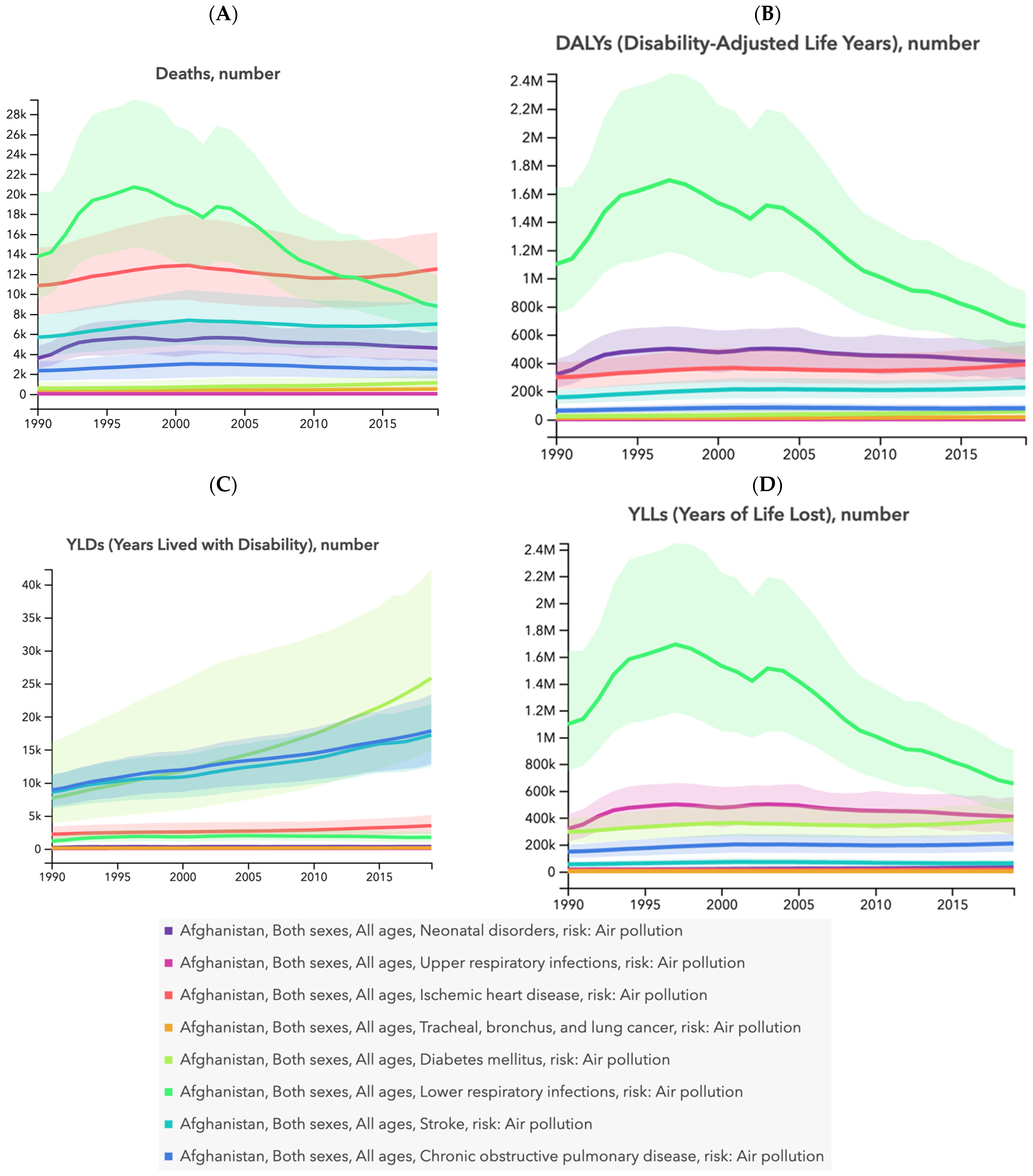
3.1. Air Pollution and All-Cause Measures
3.2. Air Pollution and Measures for Communicable, Maternal, Neonatal, and Nutritional Diseases (CMNNDs) and Non-Communicable Diseases (NCDs)
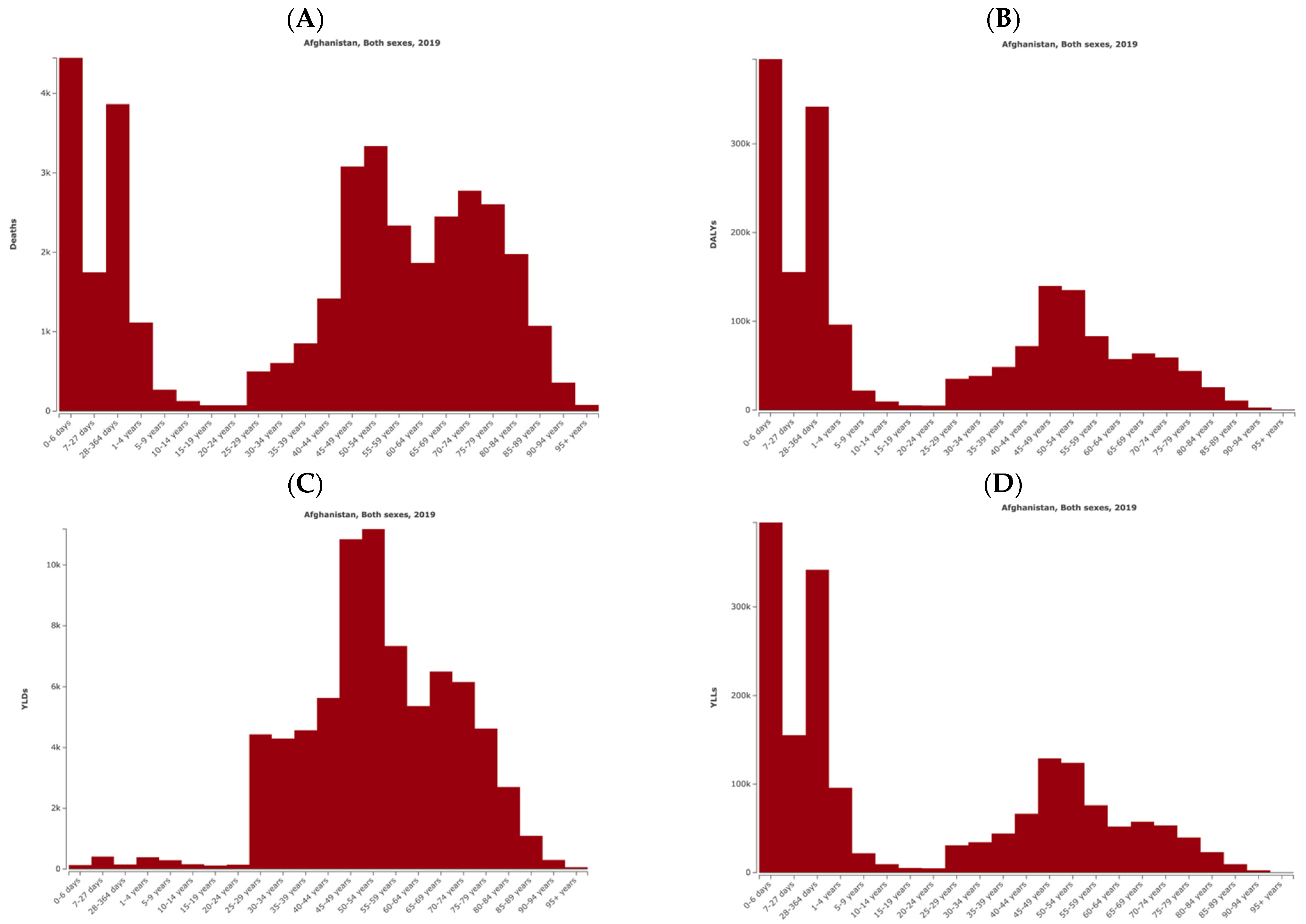
3.3. Air Pollution and Age-Specific Measures
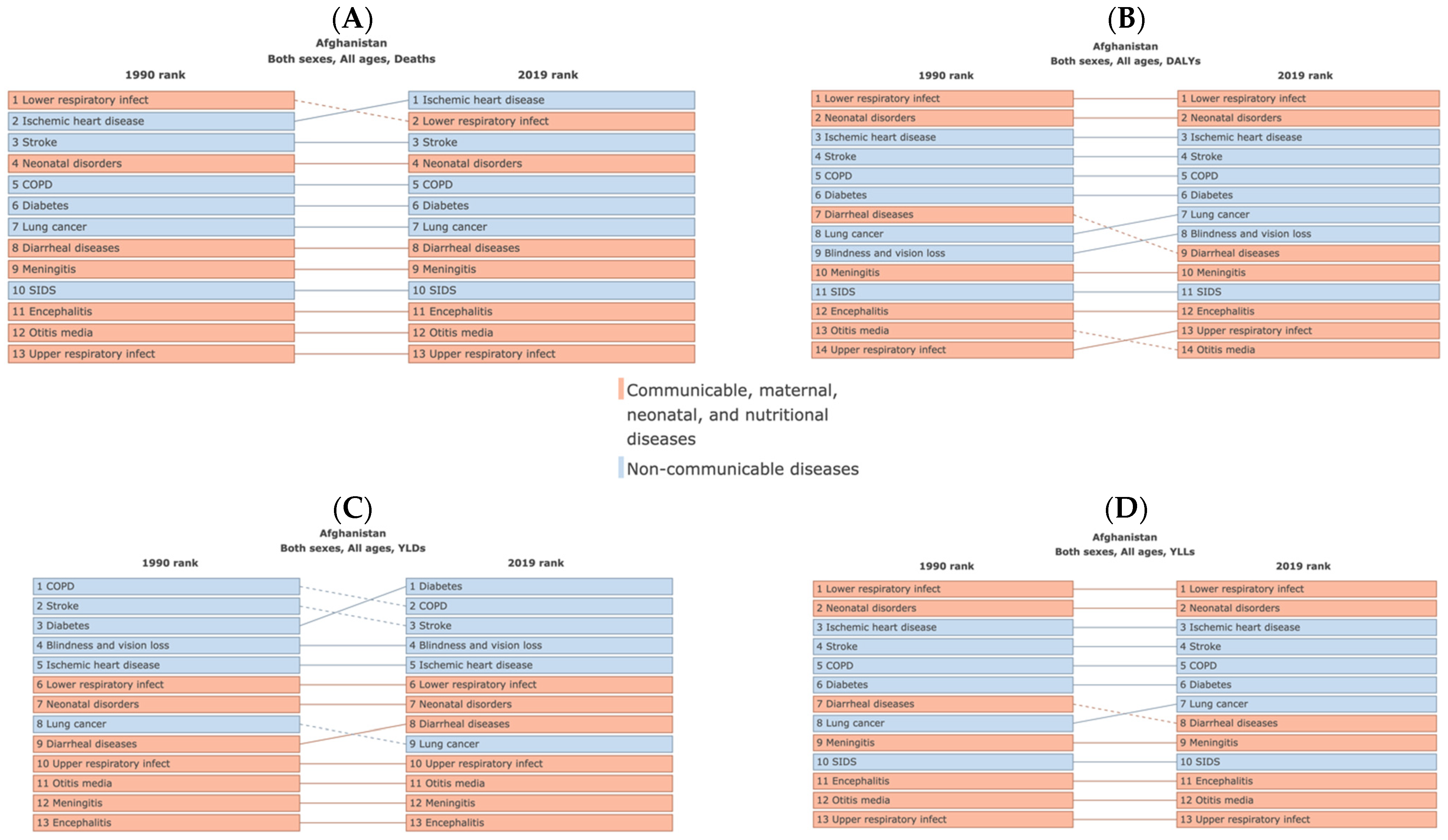
3.4. Air Pollution and Cause-Related Measures
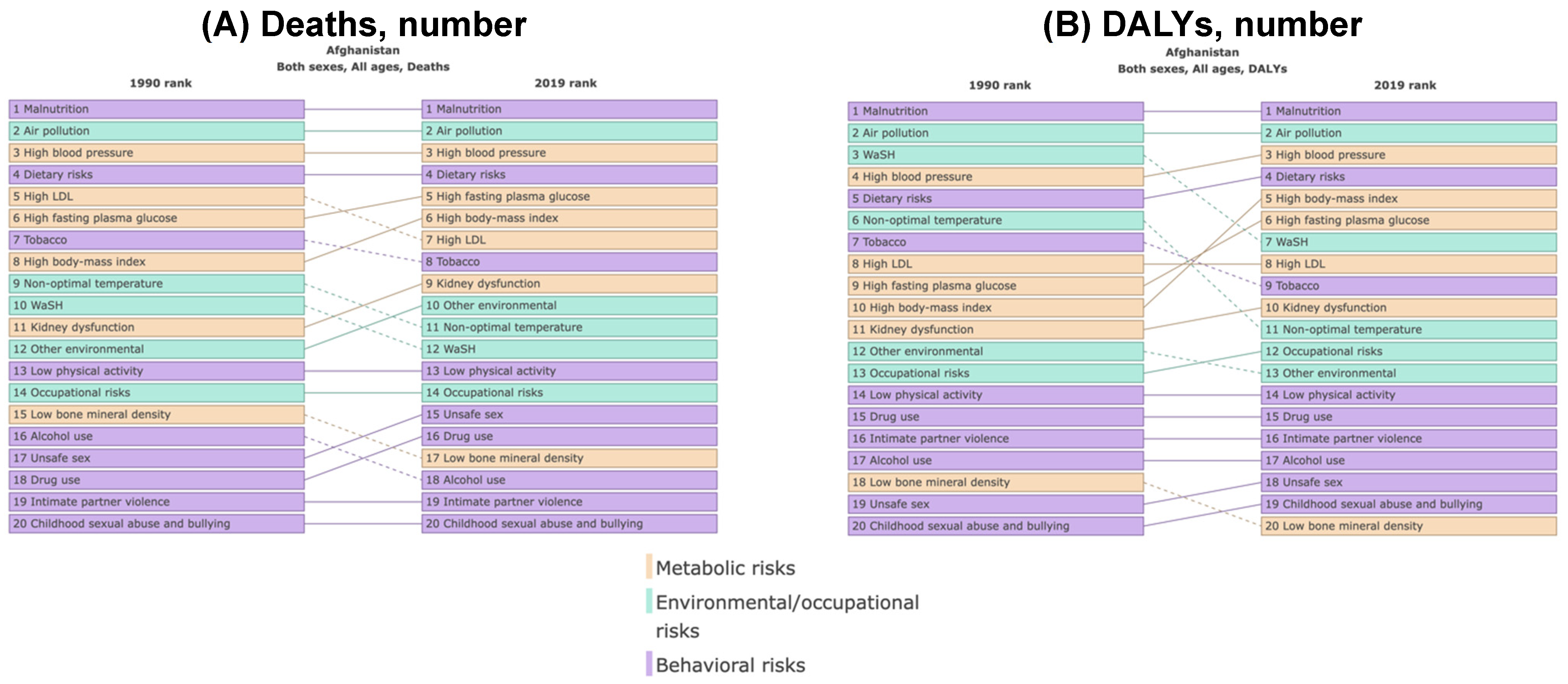
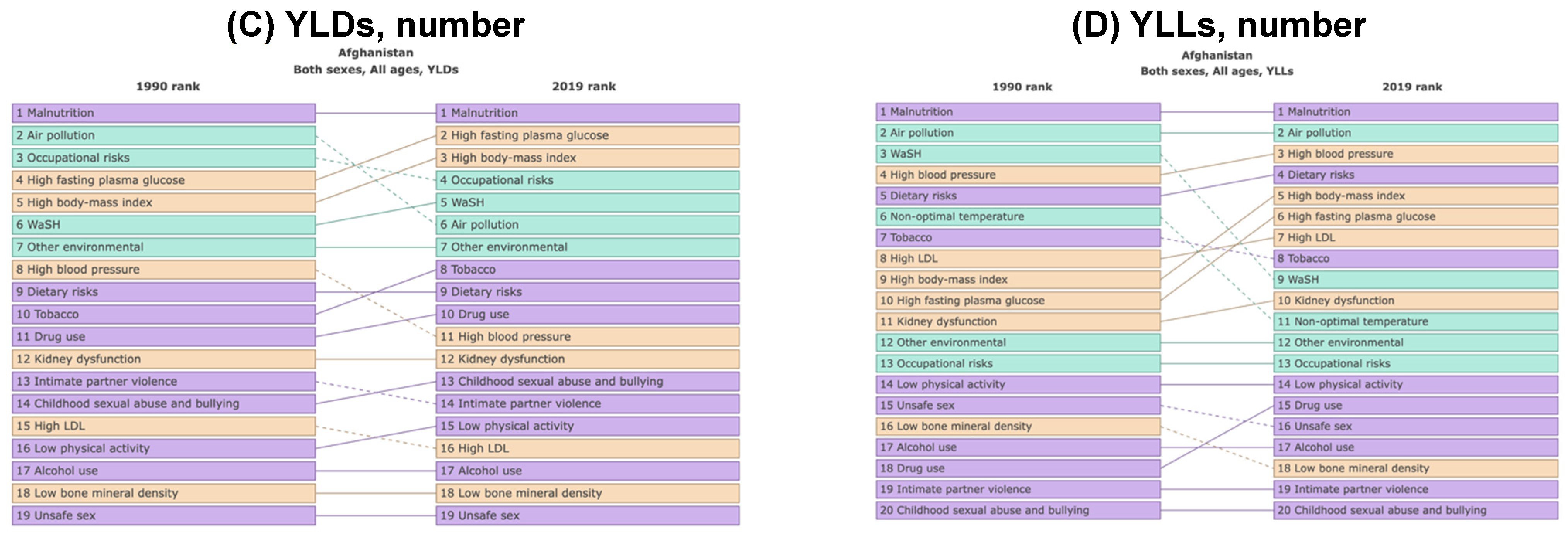
3.5. Ranking of Risk Factors
3.6. Air Pollution and Country-Specific Measures
4. Discussion
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Air Pollution. Available online: https://www.who.int/health-topics/air-pollution#tab=tab_1 (accessed on 10 January 2024).
- Münzel, T.; Hahad, O.; Daiber, A.; Lelieveld, J. Luftverschmutzung und Herz-Kreislauf-Erkrankungen. Herz 2021, 46, 120–128. [Google Scholar] [CrossRef]
- Hahad, O.; Kuntic, M.; Frenis, K.; Chowdhury, S.; Lelieveld, J.; Lieb, K.; Daiber, A.; Munzel, T. Physical Activity in Polluted Air-Net Benefit or Harm to Cardiovascular Health? A Comprehensive Review. Antioxidants 2021, 10, 1787. [Google Scholar] [CrossRef]
- Hahad, O.; Lelieveld, J.; Birklein, F.; Lieb, K.; Daiber, A.; Munzel, T. Ambient Air Pollution Increases the Risk of Cerebrovascular and Neuropsychiatric Disorders through Induction of Inflammation and Oxidative Stress. Int. J. Mol. Sci. 2020, 21, 4306. [Google Scholar] [CrossRef]
- Landrigan, P.J.; Fuller, R.; Acosta, N.J.R.; Adeyi, O.; Arnold, R.; Basu, N.N.; Balde, A.B.; Bertollini, R.; Bose-O’Reilly, S.; Boufford, J.I.; et al. The Lancet Commission on pollution and health. Lancet 2018, 391, 462–512. [Google Scholar] [CrossRef] [PubMed]
- Lelieveld, J.; Pozzer, A.; Poschl, U.; Fnais, M.; Haines, A.; Munzel, T. Loss of life expectancy from air pollution compared to other risk factors: A worldwide perspective. Cardiovasc. Res. 2020, 116, 1910–1917. [Google Scholar] [CrossRef] [PubMed]
- Ambient Air Pollution: A Global Assessment of Exposure and Burden of Disease. Available online: http://apps.who.int/iris/bitstream/10665/250141/1/9789241511353-eng.pdf?ua=1 (accessed on 10 January 2024).
- Preventing Disease through Healthy Environments. Available online: https://www.who.int/quantifying_ehimpacts/publications/preventingdisease.pdf (accessed on 10 January 2024).
- Lelieveld, J.; Klingmuller, K.; Pozzer, A.; Poschl, U.; Fnais, M.; Daiber, A.; Munzel, T. Cardiovascular disease burden from ambient air pollution in Europe reassessed using novel hazard ratio functions. Eur. Heart J. 2019, 40, 1590–1596. [Google Scholar] [CrossRef]
- Lelieveld, J.; Haines, A.; Burnett, R.; Tonne, C.; Klingmuller, K.; Munzel, T.; Pozzer, A. Air pollution deaths attributable to fossil fuels: Observational and modelling study. BMJ 2023, 383, e077784. [Google Scholar] [CrossRef]
- Shah, J.; Essar, M.Y.; Qaderi, S.; Rackimuthu, S.; Nawaz, F.A.; Qaderi, F.; Shah, A. Respiratory health and critical care concerns in Afghanistan. Lancet Respir. Med. 2022, 10, 229–231. [Google Scholar] [CrossRef] [PubMed]
- Air Quality in Afghanistan Air Quality Index (AQI) and PM2.5 Air Pollution in Afghanistan. Available online: https://www.iqair.com/afghanistan (accessed on 10 January 2024).
- Waseq, W.M. The Impact of Air Pollution on Human Health and Environment with Mitigation Measures to Reduce Air Pollution in Kabul, Afghanistan. Int. J. Healthc. Sci. 2020, 8, 1–12. [Google Scholar]
- Akbar, K.; Khaksar, T.M. Impact of Air Pollution on Reproductive Health in Afghanistan. J. Adv. Pharm. Sci. Res. 2020, 3, 1. [Google Scholar] [CrossRef]
- Mehrad, A.T. Causes of Air Pollution in Kabul and its Effects on Health. Indian J. Ecol. 2020, 47, 997–1002. [Google Scholar]
- GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1223–1249. [Google Scholar] [CrossRef] [PubMed]
- GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef] [PubMed]
- Plass, D.; Vos, T.; Hornberg, C.; Scheidt-Nave, C.; Zeeb, H.; Kramer, A. Trends in disease burden in Germany: Results, implications and limitations of the Global Burden of Disease study. Dtsch. Arztebl. Int. 2014, 111, 629–638. [Google Scholar] [CrossRef] [PubMed]
- Afghanistan Environmental Health. Available online: https://www.emro.who.int/afg/programmes/eh.html# (accessed on 10 January 2024).
- Kaali, S.; Jack, D.W.; Mujtaba, M.N.; Chillrud, S.N.; Ae-Ngibise, K.A.; Kinney, P.L.; Boamah Kaali, E.; Gennings, C.; Colicino, E.; Osei, M.; et al. Identifying sensitive windows of prenatal household air pollution on birth weight and infant pneumonia risk to inform future interventions. Environ. Int. 2023, 178, 108062. [Google Scholar] [CrossRef] [PubMed]
- Gasping for Air in Kabul. Available online: https://www.unep.org/news-and-stories/story/gasping-air-kabul (accessed on 2 February 2024).
- Lalonde, J.D.; Bradley, M. 11 Years of Air Quality Monitoring in Afghanistan. Available online: https://military-medicine.com/article/3163-11-years-of-air-quality-monitoring-in-afghanistan.html (accessed on 2 February 2024).
- Han, W.; Li, Z.; Guo, J.; Su, T.; Chen, T.; Wei, J.; Cribb, M. The Urban–Rural Heterogeneity of Air Pollution in 35 Metropolitan Regions across China. Remote Sens. 2020, 12, 2320. [Google Scholar] [CrossRef]
- Rohde, R.A.; Muller, R.A. Air Pollution in China: Mapping of Concentrations and Sources. PLoS ONE 2015, 10, e0135749. [Google Scholar] [CrossRef]
- Guttikunda, S.K.; Goel, R.; Pant, P. Nature of air pollution, emission sources, and management in the Indian cities. Atmos. Environ. 2014, 95, 501–510. [Google Scholar] [CrossRef]
- Air Quality Index (AQI) and PM2.5 Air Pollution in Pakistan. Available online: https://www.iqair.com/us/pakistan (accessed on 2 February 2024).
- Khandker, S.; Mohiuddin, A.S.M.; Ahmad, S.A.; McGushin, A.; Abelsohn, A. Air Pollution in Bangladesh and Its Consequences. Res. Sq. 2023. [Google Scholar] [CrossRef]
- Begum, B.A.; Biswas, S.K.; Hopke, P.K. Key issues in controlling air pollutants in Dhaka, Bangladesh. Atmos. Environ. 2011, 45, 7705–7713. [Google Scholar] [CrossRef]
- Begum, B.A.; Hopke, P.K.; Markwitz, A. Air pollution by fine particulate matter in Bangladesh. Atmos. Pollut. Res. 2013, 4, 75–86. [Google Scholar] [CrossRef]

| Measure | Metric | Value | UI Upper | UI Lower |
|---|---|---|---|---|
| Deaths | Number | 37,033 | 45,042 | 29,774 |
| Percent | 14.72 | 16.56 | 12.93 | |
| Rate | 96.75 | 117.67 | 77.78 | |
| DALYs | Number | 1,849,170 | 2,250,663 | 1,485,560 |
| Percent | 10.80 | 12.67 | 9.08 | |
| Rate | 4830.95 | 5879.85 | 3881.02 | |
| YLDs | Number | 76,858 | 100,685 | 55,152 |
| Percent | 2.07 | 2.55 | 1.68 | |
| Rate | 200.79 | 263.04 | 144.09 | |
| YLLs | Number | 1,772,311 | 2,167,243 | 1,410,827 |
| Percent | 13.23 | 15.28 | 11.27 | |
| Rate | 4630.16 | 5661.92 | 3685.79 |
| Measure | Cause | Metric | Value | UI Upper | UI Lower |
|---|---|---|---|---|---|
| Deaths | CMNNDs | Number | 13,459 | 17,335 | 10,118 |
| Percent | 19.21 | 23.02 | 15.42 | ||
| Rate | 35.16 | 45.29 | 26.43 | ||
| NCDs | Number | 23,573 | 29,828 | 18,157 | |
| Percent | 17.87 | 20.72 | 15.35 | ||
| Rate | 61.59 | 77.93 | 47.44 | ||
| DALYs | CMNNDs | Number | 1,076,385 | 1,403,066 | 793,828 |
| Percent | 17.84 | 21.36 | 14.32 | ||
| Rate | 2812.06 | 3665.51 | 2073.87 | ||
| NCDs | Number | 772,784 | 981,498 | 597,716 | |
| Percent | 10.19 | 12.62 | 8.13 | ||
| Rate | 2018.90 | 2564.16 | 1561.53 | ||
| YLDs | CMNNDs | Number | 2191 | 3152 | 1448 |
| Percent | 0.33 | 0.42 | 0.25 | ||
| Rate | 5.73 | 8.23 | 3.78 | ||
| NCDs | Number | 74,667 | 98,168 | 53,437 | |
| Percent | 3.10 | 3.81 | 2.50 | ||
| Rate | 195.07 | 256.47 | 139.61 | ||
| YLLs | CMNNDs | Number | 1,074,194 | 1,399,321 | 791,590 |
| Percent | 20.04 | 23.98 | 16.08 | ||
| Rate | 2806.33 | 3655.73 | 2068.03 | ||
| NCDs | Number | 698,117 | 906,658 | 525,404 | |
| Percent | 13.56 | 17.31 | 10.55 | ||
| Rate | 1823.83 | 2368.64 | 1372.62 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hahad, O. Burden of Disease Due to Air Pollution in Afghanistan—Results from the Global Burden of Disease Study 2019. Int. J. Environ. Res. Public Health 2024, 21, 197. https://doi.org/10.3390/ijerph21020197
Hahad O. Burden of Disease Due to Air Pollution in Afghanistan—Results from the Global Burden of Disease Study 2019. International Journal of Environmental Research and Public Health. 2024; 21(2):197. https://doi.org/10.3390/ijerph21020197
Chicago/Turabian StyleHahad, Omar. 2024. "Burden of Disease Due to Air Pollution in Afghanistan—Results from the Global Burden of Disease Study 2019" International Journal of Environmental Research and Public Health 21, no. 2: 197. https://doi.org/10.3390/ijerph21020197
APA StyleHahad, O. (2024). Burden of Disease Due to Air Pollution in Afghanistan—Results from the Global Burden of Disease Study 2019. International Journal of Environmental Research and Public Health, 21(2), 197. https://doi.org/10.3390/ijerph21020197






