Enhancing Behavioural Changes: A Narrative Review on the Effectiveness of a Multifactorial APP-Based Intervention Integrating Physical Activity
Abstract
1. Introduction
2. Material and Methods
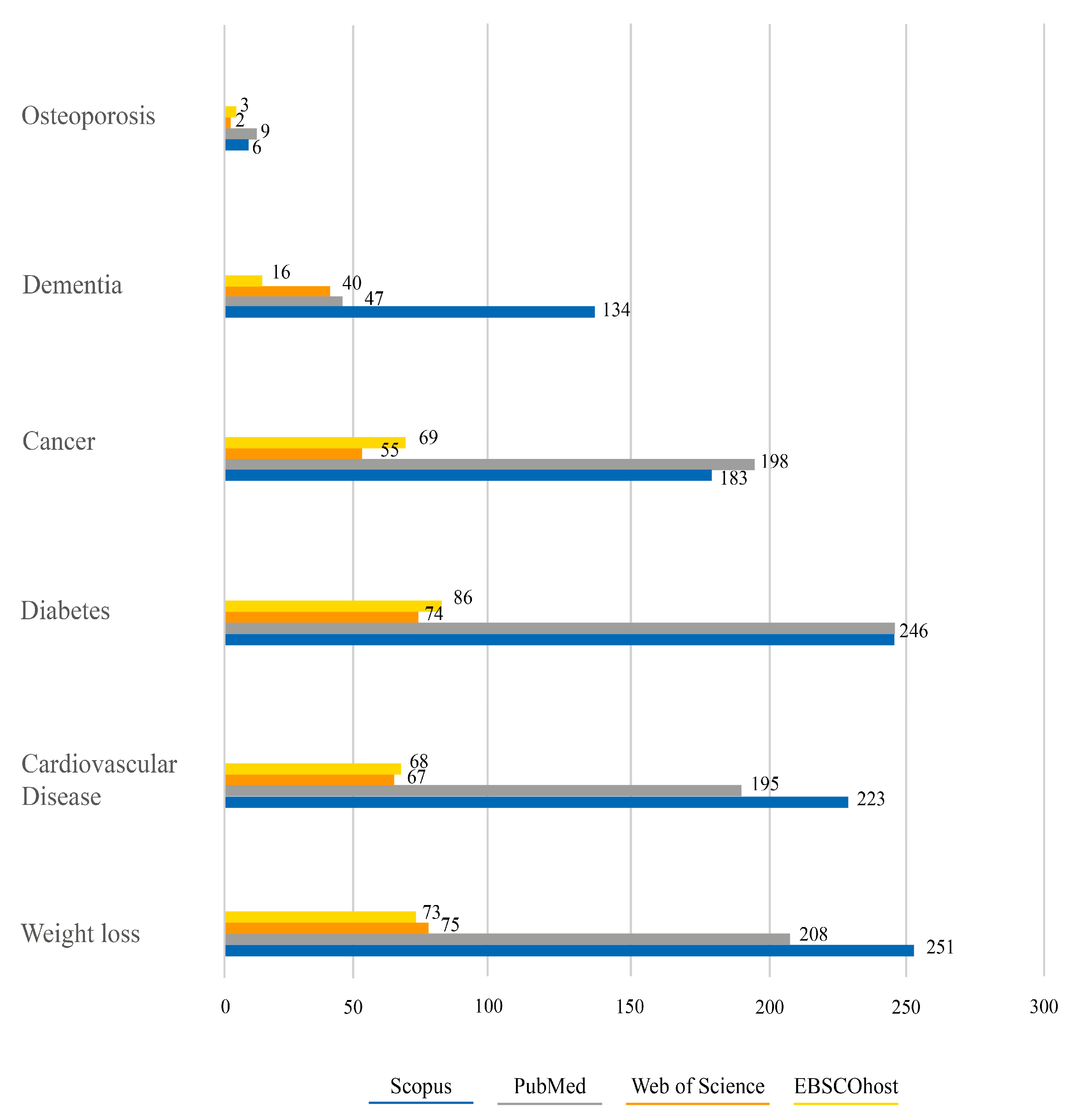
Information Sources and Search Strategy
3. Results
3.1. Weight Loss and Counteracting Obesity through Tele-Exercise
3.2. Advanced Strategies for Cardiovascular Disease Control
3.3. Diabetes Self-Management through Mobile APP-Based Interventions
3.4. Promoting Regular Physical Activity via APPs for Cancer Patients
3.5. Self-Management of Osteoporosis: Telemedicine as an Optimal Strategy
3.6. App for Cognitive Training in Dementia
4. Conclusions
- Generalising the results may overlook individual and population differences.
- The quality of the APPs is not thoroughly discussed, and attention to the long-term sustainability of interventions is limited. User adherence to APP recommendations and the potential for alteration are acknowledged.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wilke, J.; Mohr, L. Chronic Effects of High-Intensity Functional Training on Motor Function: A Systematic Review with Multilevel Meta-Analysis. Sci. Rep. 2020, 10, 21680. [Google Scholar] [CrossRef] [PubMed]
- Bonilla, D.A.; Peralta-Alzate, J.O.; Bonilla-Henao, J.A.; Cannataro, R.; Cardozo, L.A.; Vargas-Molina, S.; Stout, J.R.; Kreider, R.B.; Petro, J.L. Insights into Non-Exercise Physical Activity on Control of Body Mass: A Review with Practical Recommendations. J. Funct. Morphol. Kinesiol. 2023, 8, 44. [Google Scholar] [CrossRef] [PubMed]
- An, H.-Y.; Chen, W.; Wang, C.-W.; Yang, H.-F.; Huang, W.-T.; Fan, S.-Y. The Relationships between Physical Activity and Life Satisfaction and Happiness among Young, Middle-Aged, and Older Adults. Int. J. Env. Res. Public. Health 2020, 17, 4817. [Google Scholar] [CrossRef]
- Wilke, J.; Mohr, L.; Yuki, G.; Bhundoo, A.K.; Jiménez-Pavón, D.; Laiño, F.; Murphy, N.; Novak, B.; Nuccio, S.; Ortega-Gómez, S.; et al. Train at Home, but Not Alone: A Randomised Controlled Multicentre Trial Assessing the Effects of Live-Streamed Tele-Exercise during COVID-19-Related Lockdowns. Br. J. Sports Med. 2022, 56, 667–675. [Google Scholar] [CrossRef]
- Wiese, C.W.; Kuykendall, L.; Tay, L. Get Active? A Meta-Analysis of Leisure-Time Physical Activity and Subjective Well-Being. J. Posit. Psychol. 2018, 13, 57–66. [Google Scholar] [CrossRef]
- Stavrou, V.T.; Astara, K.; Ioannidis, P.; Vavougios, G.D.; Daniil, Z.; Gourgoulianis, K.I. Tele-Exercise in Non-Hospitalized versus Hospitalized Post-COVID-19 Patients. Sports 2022, 10, 179. [Google Scholar] [CrossRef]
- Marasco, I.; Niro, G.; Demir, S.M.; Marzano, L.; Fachechi, L.; Rizzi, F.; Demarchi, D.; Motto Ros, P.; D’Orazio, A.; Grande, M.; et al. Wearable Heart Rate Monitoring Device Communicating in 5G ISM Band for IoHT. Bioengineering 2023, 10, 113. [Google Scholar] [CrossRef]
- Concheiro-Moscoso, P.; Groba, B.; Alvarez-Estevez, D.; Miranda-Duro, M.d.C.; Pousada, T.; Nieto-Riveiro, L.; Mejuto-Muiño, F.J.; Pereira, J. Quality of Sleep Data Validation From the Xiaomi Mi Band 5 Against Polysomnography: Comparison Study. J. Med. Int. Res. 2023, 25, e42073. [Google Scholar] [CrossRef]
- Paulauskaite-Taraseviciene, A.; Siaulys, J.; Sutiene, K.; Petravicius, T.; Navickas, S.; Oliandra, M.; Rapalis, A.; Balciunas, J. Geriatric Care Management System Powered by the IoT and Computer Vision Techniques. Healthcare 2023, 11, 1152. [Google Scholar] [CrossRef]
- Thorne, C.S.; Gatt, A.; DeRaffaele, C.; Bazena, A.; Formosa, C. Innovative Single-Sensor, in-Shoe Pressure and Temperature Monitoring Device: A Dynamic Laboratory Validation Study. Gait Posture 2023, 100, 70–74. [Google Scholar] [CrossRef]
- Tison, G.H.; Avram, R.; Kuhar, P.; Abreau, S.; Marcus, G.M.; Pletcher, M.J.; Olgin, J.E. Worldwide Effect of COVID-19 on Physical Activity: A Descriptive Study. Ann. Intern. Med. 2020, 173, 767–770. [Google Scholar] [CrossRef] [PubMed]
- Ozaslan, B.; Patek, S.D.; Breton, M.D. Impact of Daily Physical Activity as Measured by Commonly Available Wearables on Mealtime Glucose Control in Type 1 Diabetes. Diabetes Technol. Ther. 2020, 22, 742–748. [Google Scholar] [CrossRef]
- Ho, V.; Merchant, R.A. The Acceptability of Digital Technology and Tele-Exercise in the Age of COVID-19: Cross-Sectional Study. JMIR Aging 2022, 5, e33165. [Google Scholar] [CrossRef]
- Rejeb, A.; Rejeb, K.; Treiblmaier, H.; Appolloni, A.; Alghamdi, S.; Alhasawi, Y.; Iranmanesh, M. The Internet of Things (IoT) in Healthcare: Taking Stock and Moving Forward. Internet Things 2023, 22, 100721. [Google Scholar] [CrossRef]
- Novatchkov, H.; Baca, A. Artificial Intelligence in Sports on the Example of Weight Training. J. Sports Sci. Med. 2013, 12, 27–37. [Google Scholar]
- Simek, E.M.; McPhate, L.; Haines, T.P. Adherence to and Efficacy of Home Exercise Programs to Prevent Falls: A Systematic Review and Meta-Analysis of the Impact of Exercise Program Characteristics. Prev. Med. 2012, 55, 262–275. [Google Scholar] [CrossRef] [PubMed]
- Fiorilli, G.; Buonsenso, A.; Di Martino, G.; Crova, C.; Centorbi, M.; Grazioli, E.; Tranchita, E.; Cerulli, C.; Quinzi, F.; Calcagno, G.; et al. Impact of Active Breaks in the Classroom on Mathematical Performance and Attention in Elementary School Children. Healthcare 2021, 9, 1689. [Google Scholar] [CrossRef]
- Böhm, B.; Karwiese, S.D.; Böhm, H.; Oberhoffer, R. Effects of Mobile Health Including Wearable Activity Trackers to Increase Physical Activity Outcomes Among Healthy Children and Adolescents: Systematic Review. JMIR Mhealth Uhealth 2019, 7, e8298. [Google Scholar] [CrossRef]
- Helbostad, J.; Vereijken, B.; Becker, C.; Todd, C.; Taraldsen, K.; Pijnappels, M.; Aminian, K.; Mellone, S. Mobile Health Applications to Promote Active and Healthy Ageing. Sensors 2017, 17, 622. [Google Scholar] [CrossRef]
- Valenzuela, T.; Okubo, Y.; Woodbury, A.; Lord, S.R.; Delbaere, K. Adherence to Technology-Based Exercise Programs in Older Adults: A Systematic Review. J. Geriatr. Phys. Ther. 2018, 41, 49–61. [Google Scholar] [CrossRef]
- Klenk, S.; Reifegerste, D.; Renatus, R. Gender Differences in Gratifications from Fitness App Use and Implications for Health Interventions. Mob. Media Commun. 2017, 5, 178–193. [Google Scholar] [CrossRef]
- Xu, P.; Chen, J.-S.; Chang, Y.-L.; Wang, X.; Jiang, X.; Griffiths, M.D.; Pakpour, A.H.; Lin, C.-Y. Gender Differences in the Associations Between Physical Activity, Smartphone Use, and Weight Stigma. Front. Public Health 2022, 10, 862829. [Google Scholar] [CrossRef]
- Emmer, C.; Bosnjak, M.; Mata, J. The Association between Weight Stigma and Mental Health: A Meta-analysis. Obes. Rev. 2020, 21, e12935. [Google Scholar] [CrossRef]
- Branca, F.; Ursu, P.; Aguayo, V. A Plan for Accelerated Action on Obesity. Lancet Glob. Health 2023, 11, e1170–e1171. [Google Scholar] [CrossRef]
- Jospe, M.R.; Roy, M.; Brown, R.C.; Williams, S.M.; Osborne, H.R.; Meredith-Jones, K.A.; McArthur, J.R.; Fleming, E.A.; Taylor, R.W. The Effect of Different Types of Monitoring Strategies on Weight Loss: A Randomized Controlled Trial. Obesity 2017, 25, 1490–1498. [Google Scholar] [CrossRef]
- Mensah, G.A.; Roth, G.A.; Fuster, V. The Global Burden of Cardiovascular Diseases and Risk Factors. J. Am. Coll. Cardiol. 2019, 74, 2529–2532. [Google Scholar] [CrossRef] [PubMed]
- Tzenios, N.; Tazanios, M.E.; Chahine, M. The Impact of Body Mass Index on Prostate Cancer: An Updated Systematic Review and Meta-Analysis. Medicine 2022, 101, e30191. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Global Health Estimates 2020: Deaths by Cause, Age, Sex, by Country and by Region, 2000–2019; WHO: Geneva, Switzerland, 2020.
- Guh, D.P.; Zhang, W.; Bansback, N.; Amarsi, Z.; Birmingham, C.L.; Anis, A.H. The Incidence of Co-Morbidities Related to Obesity and Overweight: A Systematic Review and Meta-Analysis. BMC Public Health 2009, 9, 88. [Google Scholar] [CrossRef] [PubMed]
- Raber, M.; Liao, Y.; Rara, A.; Schembre, S.M.; Krause, K.J.; Strong, L.; Daniel-MacDougall, C.; Basen-Engquist, K. A Systematic Review of the Use of Dietary Self-Monitoring in Behavioural Weight Loss Interventions: Delivery, Intensity and Effectiveness. Public Health Nutr. 2021, 24, 5885–5913. [Google Scholar] [CrossRef]
- Berglind, D.; Yacaman-Mendez, D.; Lavebratt, C.; Forsell, Y. The Effect of Smartphone Apps Versus Supervised Exercise on Physical Activity, Cardiorespiratory Fitness, and Body Composition Among Individuals With Mild-to-Moderate Mobility Disability: Randomized Controlled Trial. JMIR Mhealth Uhealth 2020, 8, e14615. [Google Scholar] [CrossRef] [PubMed]
- Balk-Møller, N.C.; Poulsen, S.K.; Larsen, T.M. Effect of a Nine-Month Web- and App-Based Workplace Intervention to Promote Healthy Lifestyle and Weight Loss for Employees in the Social Welfare and Health Care Sector: A Randomized Controlled Trial. J. Med. Internet Res. 2017, 19, e108. [Google Scholar] [CrossRef]
- Fukuoka, Y.; Gay, C.L.; Joiner, K.L.; Vittinghoff, E. A Novel Diabetes Prevention Intervention Using a Mobile App. Am. J. Prev. Med. 2015, 49, 223–237. [Google Scholar] [CrossRef]
- Stephens, J.D.; Yager, A.M.; Allen, J. Smartphone Technology and Text Messaging for Weight Loss in Young Adults. J. Cardiovasc. Nurs. 2017, 32, 39–46. [Google Scholar] [CrossRef]
- Hernández-Reyes, A.; Cámara-Martos, F.; Molina-Luque, R.; Moreno-Rojas, R. Effect of an MHealth Intervention Using a Pedometer App With Full In-Person Counseling on Body Composition of Overweight Adults: Randomized Controlled Weight Loss Trial. JMIR Mhealth Uhealth 2020, 8, e16999. [Google Scholar] [CrossRef]
- Recio-Rodriguez, J.I.; Agudo-Conde, C.; Martin-Cantera, C.; González-Viejo, M.N.; Fernandez-Alonso, M.D.C.; Arietaleanizbeaskoa, M.S.; Schmolling-Guinovart, Y.; Maderuelo-Fernandez, J.-A.; Rodriguez-Sanchez, E.; Gomez-Marcos, M.A.; et al. Short-Term Effectiveness of a Mobile Phone App for Increasing Physical Activity and Adherence to the Mediterranean Diet in Primary Care: A Randomized Controlled Trial (EVIDENT II Study). J. Med. Internet Res. 2016, 18, e331. [Google Scholar] [CrossRef]
- Hutchesson, M.; Callister, R.; Morgan, P.; Pranata, I.; Clarke, E.; Skinner, G.; Ashton, L.; Whatnall, M.; Jones, M.; Oldmeadow, C.; et al. A Targeted and Tailored EHealth Weight Loss Program for Young Women: The Be Positive Be Healthe Randomized Controlled Trial. Healthcare 2018, 6, 39. [Google Scholar] [CrossRef]
- Naimark, J.S.; Madar, Z.; Shahar, D.R. The Impact of a Web-Based App (EBalance) in Promoting Healthy Lifestyles: Randomized Controlled Trial. J. Med. Internet Res. 2015, 17, e56. [Google Scholar] [CrossRef]
- Lugones-Sanchez, C.; Sanchez-Calavera, M.A.; Repiso-Gento, I.; Adalia, E.G.; Ramirez-Manent, J.I.; Agudo-Conde, C.; Rodriguez-Sanchez, E.; Gomez-Marcos, M.A.; Recio-Rodriguez, J.I.; Garcia-Ortiz, L. Effectiveness of an MHealth Intervention Combining a Smartphone App and Smart Band on Body Composition in an Overweight and Obese Population: Randomized Controlled Trial (EVIDENT 3 Study). JMIR Mhealth Uhealth 2020, 8, e21771. [Google Scholar] [CrossRef] [PubMed]
- Cadmus-Bertram, L.A.; Marcus, B.H.; Patterson, R.E.; Parker, B.A.; Morey, B.L. Randomized Trial of a Fitbit-Based Physical Activity Intervention for Women. Am. J. Prev. Med. 2015, 49, 414–418. [Google Scholar] [CrossRef] [PubMed]
- Pradal-Cano, L.; Lozano-Ruiz, C.; Pereyra-Rodríguez, J.J.; Saigí-Rubió, F.; Bach-Faig, A.; Esquius, L.; Medina, F.X.; Aguilar-Martínez, A. Using Mobile Applications to Increase Physical Activity: A Systematic Review. Int. J. Env. Res. Public Health 2020, 17, 8238. [Google Scholar] [CrossRef] [PubMed]
- Chew, H.S.J.; Rajasegaran, N.N.; Chin, Y.H.; Chew, W.S.N.; Kim, K.M. Effectiveness of Combined Health Coaching and Self-Monitoring Apps on Weight-Related Outcomes in People With Overweight and Obesity: Systematic Review and Meta-Analysis. J. Med. Internet Res. 2023, 25, e42432. [Google Scholar] [CrossRef]
- Milne-Ives, M.; Homer, S.R.; Andrade, J.; Meinert, E. Potential Associations between Behavior Change Techniques and Engagement with Mobile Health Apps: A Systematic Review. Front. Psychol. 2023, 14. [Google Scholar] [CrossRef]
- Leon, A.S.; Franklin, B.A.; Costa, F.; Balady, G.J.; Berra, K.A.; Stewart, K.J.; Thompson, P.D.; Williams, M.A.; Lauer, M.S. Cardiac Rehabilitation and Secondary Prevention of Coronary Heart Disease. Circulation 2005, 111, 369–376. [Google Scholar] [CrossRef]
- di Cagno, A.; Fiorilli, G.; Buonsenso, A.; Di Martino, G.; Centorbi, M.; Angiolillo, A.; Calcagno, G.; Komici, K.; Di Costanzo, A. Long-Term Physical Activity Effectively Reduces the Consumption of Antihypertensive Drugs: A Randomized Controlled Trial. J. Cardiovasc. Dev. Dis. 2023, 10, 285. [Google Scholar] [CrossRef]
- Murtagh, E.M.; Nichols, L.; Mohammed, M.A.; Holder, R.; Nevill, A.M.; Murphy, M.H. The Effect of Walking on Risk Factors for Cardiovascular Disease: An Updated Systematic Review and Meta-Analysis of Randomised Control Trials. Prev. Med. 2015, 72, 34–43. [Google Scholar] [CrossRef]
- Delva, S.; Mendez, K.J.W.; Cajita, M.; Koirala, B.; Shan, R.; Wongvibulsin, S.; Vilarino, V.; Gilmore, D.R.; Han, H.-R. Efficacy of Mobile Health for Self-Management of Cardiometabolic Risk Factors. J. Cardiovasc. Nurs. 2021, 36, 34–55. [Google Scholar] [CrossRef]
- Sequi-Dominguez, I.; Alvarez-Bueno, C.; Martinez-Vizcaino, V.; Fernandez-Rodriguez, R.; del Saz Lara, A.; Cavero-Redondo, I. Effectiveness of Mobile Health Interventions Promoting Physical Activity and Lifestyle Interventions to Reduce Cardiovascular Risk Among Individuals With Metabolic Syndrome: Systematic Review and Meta-Analysis. J. Med. Internet Res. 2020, 22, e17790. [Google Scholar] [CrossRef] [PubMed]
- Patterson, K.; Davey, R.; Keegan, R.; Kunstler, B.; Woodward, A.; Freene, N. Behaviour Change Techniques in Cardiovascular Disease Smartphone Apps to Improve Physical Activity and Sedentary Behaviour: Systematic Review and Meta-Regression. Int. J. Behav. Nutr. Phys. Act. 2022, 19, 81. [Google Scholar] [CrossRef] [PubMed]
- Burke, L.E.; Ma, J.; Azar, K.M.J.; Bennett, G.G.; Peterson, E.D.; Zheng, Y.; Riley, W.; Stephens, J.; Shah, S.H.; Suffoletto, B.; et al. Current Science on Consumer Use of Mobile Health for Cardiovascular Disease Prevention. Circulation 2015, 132, 1157–1213. [Google Scholar] [CrossRef] [PubMed]
- Schorr, E.N.; Gepner, A.D.; Dolansky, M.A.; Forman, D.E.; Park, L.G.; Petersen, K.S.; Still, C.H.; Wang, T.Y.; Wenger, N.K. Harnessing Mobile Health Technology for Secondary Cardiovascular Disease Prevention in Older Adults: A Scientific Statement From the American Heart Association. Circ. Cardiovasc. Qual. Outcomes 2021, 14, e000103. [Google Scholar] [CrossRef] [PubMed]
- Lai, W.X.; Visaria, A.; Østbye, T.; Malhotra, R. Prevalence and Correlates of Use of Digital Technology for Managing Hypertension among Older Adults. J. Hum. Hypertens. 2023, 37, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Dunlay, S.M.; Weston, S.A.; Killian, J.M.; Bell, M.R.; Jaffe, A.S.; Roger, V.L. Thirty-Day Rehospitalizations After Acute Myocardial Infarction. Ann. Intern. Med. 2012, 157, 11. [Google Scholar] [CrossRef]
- Johnston, N.; Bodegard, J.; Jerström, S.; Åkesson, J.; Brorsson, H.; Alfredsson, J.; Albertsson, P.A.; Karlsson, J.-E.; Varenhorst, C. Effects of Interactive Patient Smartphone Support App on Drug Adherence and Lifestyle Changes in Myocardial Infarction Patients: A Randomized Study. Am. Heart J. 2016, 178, 85–94. [Google Scholar] [CrossRef] [PubMed]
- Saleh, Z.T.; Elshatarat, R.A.; Almarwani, A.M.; Alzahrani, N.S.; Alhowaymel, F.M.; Elhefnawy, K.A.; Elneblawi, N.H.; Ibrahim, A.M.; Zaghamir, D.E.; Shawashi, T.O. Predictors of Physical Activity Behavior Change among Patients with Heart Failure Enrolled in Home-Based Cardiac Rehabilitation Intervention. Heart Lung 2023, 61, 16–21. [Google Scholar] [CrossRef]
- Zhou, M.; Xu, Y.; Zhang, L.; Yang, Y.; Zheng, J. Effectiveness of Smartphone-Assisted Cardiac Rehabilitation: A Systematic Review and Meta-Analysis. Disabil. Rehabil. 2023, 1–10. [Google Scholar] [CrossRef]
- Kanejima, Y.; Kitamura, M.; Izawa, K.P. Self-Monitoring to Increase Physical Activity in Patients with Cardiovascular Disease: A Systematic Review and Meta-Analysis. Aging Clin. Exp. Res. 2019, 31, 163–173. [Google Scholar] [CrossRef]
- Hägglund, E.; Lyngå, P.; Frie, F.; Ullman, B.; Persson, H.; Melin, M.; Hagerman, I. Patient-Centred Home-Based Management of Heart Failure. Scand. Cardiovasc. J. 2015, 49, 193–199. [Google Scholar] [CrossRef]
- Persell, S.D.; Peprah, Y.A.; Lipiszko, D.; Lee, J.Y.; Li, J.J.; Ciolino, J.D.; Karmali, K.N.; Sato, H. Effect of Home Blood Pressure Monitoring via a Smartphone Hypertension Coaching Application or Tracking Application on Adults With Uncontrolled Hypertension. JAMA Netw. Open 2020, 3, e200255. [Google Scholar] [CrossRef]
- Su, J.J.; Liu, J.Y.W.; Cheung, D.S.K.; Wang, S.; Christensen, M.; Kor, P.P.K.; Tyrovolas, S.; Leung, A.Y.M. Long-Term Effects of e-Health Secondary Prevention on Cardiovascular Health: A Systematic Review and Meta-Analysis. Eur. J. Cardiovasc. Nurs. 2023, 22, 562–574. [Google Scholar] [CrossRef]
- Widmer, R.J.; Allison, T.G.; Lerman, L.O.; Lerman, A. Digital Health Intervention as an Adjunct to Cardiac Rehabilitation Reduces Cardiovascular Risk Factors and Rehospitalizations. J. Cardiovasc. Transl. Res. 2015, 8, 283–292. [Google Scholar] [CrossRef]
- Ter Hoeve, N.; Sunamura, M.; Stam, H.J.; Boersma, E.; Geleijnse, M.L.; van Domburg, R.T.; van den Berg-Emons, R.J.G. Effects of Two Behavioral Cardiac Rehabilitation Interventions on Physical Activity: A Randomized Controlled Trial. Int. J. Cardiol. 2018, 255, 221–228. [Google Scholar] [CrossRef]
- Kitsiou, S.; Paré, G.; Jaana, M.; Gerber, B. Effectiveness of MHealth Interventions for Patients with Diabetes: An Overview of Systematic Reviews. PLoS ONE 2017, 12, e0173160. [Google Scholar] [CrossRef]
- Saeedi, P.; Petersohn, I.; Salpea, P.; Malanda, B.; Karuranga, S.; Unwin, N.; Colagiuri, S.; Guariguata, L.; Motala, A.A.; Ogurtsova, K.; et al. Global and Regional Diabetes Prevalence Estimates for 2019 and Projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9th Edition. Diabetes Res Clin Pr. 2019, 157, 107843. [Google Scholar] [CrossRef] [PubMed]
- Nundy, S.; Dick, J.J.; Chou, C.-H.; Nocon, R.S.; Chin, M.H.; Peek, M.E. Mobile Phone Diabetes Project Led To Improved Glycemic Control And Net Savings For Chicago Plan Participants. Health Aff. 2014, 33, 265–272. [Google Scholar] [CrossRef]
- Herman, W.H.; Petersen, M.; Kalyani, R.R. Response to Comment on American Diabetes Association. Standards of Medical Care in Diabetes—2017. Diabetes Care 2017;40(Suppl. 1):S1–S135. Diabetes Care 2017, 40, e94–e95. [Google Scholar] [CrossRef]
- MacPherson, M.M.; Merry, K.J.; Locke, S.R.; Jung, M.E. Effects of Mobile Health Prompts on Self-Monitoring and Exercise Behaviors Following a Diabetes Prevention Program: Secondary Analysis From a Randomized Controlled Trial. JMIR Mhealth Uhealth 2019, 7, e12956. [Google Scholar] [CrossRef]
- Wu, Y.; Yao, X.; Vespasiani, G.; Nicolucci, A.; Dong, Y.; Kwong, J.; Li, L.; Sun, X.; Tian, H.; Li, S. Mobile App-Based Interventions to Support Diabetes Self-Management: A Systematic Review of Randomized Controlled Trials to Identify Functions Associated with Glycemic Efficacy. JMIR Mhealth Uhealth 2017, 5, e35. [Google Scholar] [CrossRef]
- Kim, E.K.; Kwak, S.H.; Jung, H.S.; Koo, B.K.; Moon, M.K.; Lim, S.; Jang, H.C.; Park, K.S.; Cho, Y.M. The Effect of a Smartphone-Based, Patient-Centered Diabetes Care System in Patients With Type 2 Diabetes: A Randomized, Controlled Trial for 24 Weeks. Diabetes Care 2019, 42, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Dobson, R.; Whittaker, R.; Jiang, Y.; Maddison, R.; Shepherd, M.; McNamara, C.; Cutfield, R.; Khanolkar, M.; Murphy, R. Effectiveness of Text Message Based, Diabetes Self Management Support Programme (SMS4BG): Two Arm, Parallel Randomised Controlled Trial. BMJ 2018, 361, k1959. [Google Scholar] [CrossRef]
- Alonso-Domínguez, R.; García-Ortiz, L.; Patino-Alonso, M.; Sánchez-Aguadero, N.; Gómez-Marcos, M.; Recio-Rodríguez, J. Effectiveness of A Multifactorial Intervention in Increasing Adherence to the Mediterranean Diet among Patients with Diabetes Mellitus Type 2: A Controlled and Randomized Study (EMID Study). Nutrients 2019, 11, 162. [Google Scholar] [CrossRef]
- Saffari, M.; Ghanizadeh, G.; Koenig, H.G. Health Education via Mobile Text Messaging for Glycemic Control in Adults with Type 2 Diabetes: A Systematic Review and Meta-Analysis. Prim. Care Diabetes 2014, 8, 275–285. [Google Scholar] [CrossRef]
- Duruturk, N.; Özköslü, M.A. Effect of Tele-Rehabilitation on Glucose Control, Exercise Capacity, Physical Fitness, Muscle Strength and Psychosocial Status in Patients with Type 2 Diabetes: A Double Blind Randomized Controlled Trial. Prim. Care Diabetes 2019, 13, 542–548. [Google Scholar] [CrossRef]
- Conroy, D.E.; Yang, C.-H.; Maher, J.P. Behavior Change Techniques in Top-Ranked Mobile Apps for Physical Activity. Am. J. Prev. Med. 2014, 46, 649–652. [Google Scholar] [CrossRef]
- Foglietta, J.; Inno, A.; de Iuliis, F.; Sini, V.; Duranti, S.; Turazza, M.; Tarantini, L.; Gori, S. Cardiotoxicity of Aromatase Inhibitors in Breast Cancer Patients. Clin. Breast Cancer 2017, 17, 11–17. [Google Scholar] [CrossRef]
- De Cicco, P.; Catani, M.V.; Gasperi, V.; Sibilano, M.; Quaglietta, M.; Savini, I. Nutrition and Breast Cancer: A Literature Review on Prevention, Treatment and Recurrence. Nutrients 2019, 11, 1514. [Google Scholar] [CrossRef]
- Blair, C.K.; Harding, E.; Wiggins, C.; Kang, H.; Schwartz, M.; Tarnower, A.; Du, R.; Kinney, A.Y. A Home-Based Mobile Health Intervention to Replace Sedentary Time With Light Physical Activity in Older Cancer Survivors: Randomized Controlled Pilot Trial. JMIR Cancer 2021, 7, e18819. [Google Scholar] [CrossRef]
- Coughlin, S.S.; Caplan, L.S.; Williams, V. Home-Based Physical Activity Interventions for Breast Cancer Patients Receiving Primary Therapy: A Systematic Review. Breast Cancer Res. Treat. 2019, 178, 513–522. [Google Scholar] [CrossRef] [PubMed]
- Mishra, S.I.; Scherer, R.W.; Snyder, C.; Geigle, P.M.; Berlanstein, D.R.; Topaloglu, O. Exercise Interventions on Health-Related Quality of Life for People with Cancer during Active Treatment. Cochrane Database Syst. Rev. 2012. [Google Scholar] [CrossRef] [PubMed]
- Rock, C.L.; Doyle, C.; Demark-Wahnefried, W.; Meyerhardt, J.; Courneya, K.S.; Schwartz, A.L.; Bandera, E.V.; Hamilton, K.K.; Grant, B.; McCullough, M.; et al. Nutrition and Physical Activity Guidelines for Cancer Survivors. CA Cancer J. Clin. 2012, 62, 242–274. [Google Scholar] [CrossRef]
- Hutzler, Y.; Sherrill, C. Defining Adapted Physical Activity: International Perspectives. Adapt. Phys. Act. Q. 2007, 24, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Lynch, A.M.; Kilroy, S.; McKee, H.; Sheerin, F.; Epstein, M.; Girault, A.; Gillois, P.; Bosson, J.L.; Rolland, C.; Harkin, M.; et al. Active Older Adults Goal Setting Outcomes for Engaging in a Physical Activity App and the Motivation Characteristics of These Goals (MOVEAGE-ACT). Prev. Med. Rep. 2023, 31, 102084. [Google Scholar] [CrossRef]
- Roberts, A.L.; Potts, H.W.; Koutoukidis, D.A.; Smith, L.; Fisher, A. Breast, Prostate, and Colorectal Cancer Survivors’ Experiences of Using Publicly Available Physical Activity Mobile Apps: Qualitative Study. JMIR Mhealth Uhealth 2019, 7, e10918. [Google Scholar] [CrossRef] [PubMed]
- Cheung, A.T.; Li, W.H.C.; Ho, L.L.K.; Ho, K.Y.; Chan, G.C.F.; Chung, J.O.K. Physical Activity for Pediatric Cancer Survivors: A Systematic Review of Randomized Controlled Trials. J. Cancer Surviv. 2021, 15, 876–889. [Google Scholar] [CrossRef]
- Ha, D.M.; Comer, A.; Dollar, B.; Bedoy, R.; Ford, M.; Gozansky, W.S.; Zeng, C.; Arch, J.J.; Leach, H.J.; Malhotra, A.; et al. Telemedicine-Based Inspiratory Muscle Training and Walking Promotion with Lung Cancer Survivors Following Curative Intent Therapy: A Parallel-Group Pilot Randomized Trial. Support. Care Cancer 2023, 31, 546. [Google Scholar] [CrossRef]
- Chow, E.J.; Doody, D.R.; Di, C.; Armenian, S.H.; Baker, K.S.; Bricker, J.B.; Gopal, A.K.; Hagen, A.M.; Ketterl, T.G.; Lee, S.J.; et al. Feasibility of a Behavioral Intervention Using Mobile Health Applications to Reduce Cardiovascular Risk Factors in Cancer Survivors: A Pilot Randomized Controlled Trial. J. Cancer Surviv. 2021, 15, 554–563. [Google Scholar] [CrossRef]
- van Eenbergen, M.C.; van de Poll-Franse, L.V.; Heine, P.; Mols, F. The Impact of Participation in Online Cancer Communities on Patient Reported Outcomes: Systematic Review. JMIR Cancer 2017, 3, e15. [Google Scholar] [CrossRef] [PubMed]
- Valle, C.G.; Diamond, M.A.; Heiling, H.M.; Deal, A.M.; Hales, D.P.; Nezami, B.T.; Pinto, B.M.; LaRose, J.G.; Rini, C.M.; Tate, D.F. Effect of an MHealth Intervention on Physical Activity Outcomes among Young Adult Cancer Survivors: The IMPACT Randomized Controlled Trial. Cancer 2023, 129, 461–472. [Google Scholar] [CrossRef] [PubMed]
- Short, C.E.; Finlay, A.; Sanders, I.; Maher, C. Development and Pilot Evaluation of a Clinic-Based MHealth App Referral Service to Support Adult Cancer Survivors Increase Their Participation in Physical Activity Using Publicly Available Mobile Apps. BMC Health Serv. Res. 2018, 18, 27. [Google Scholar] [CrossRef]
- Salari, N.; Ghasemi, H.; Mohammadi, L.; Behzadi, M.H.; Rabieenia, E.; Shohaimi, S.; Mohammadi, M. The Global Prevalence of Osteoporosis in the World: A Comprehensive Systematic Review and Meta-Analysis. J. Orthop. Surg. Res. 2021, 16, 609. [Google Scholar] [CrossRef]
- Zhang, Q.; Cai, W.; Wang, G.; Shen, X. Prevalence and Contributing Factors of Osteoporosis in the Elderly over 70 Years Old: An Epidemiological Study of Several Community Health Centers in Shanghai. Ann. Palliat. Med. 2020, 9, 231–238. [Google Scholar] [CrossRef]
- Curtis, J.R.; Safford, M.M. Management of Osteoporosis among the Elderly with Other Chronic Medical Conditions. Drugs Aging 2012, 29, 549–564. [Google Scholar] [CrossRef]
- Janiszewska, M.; Kulik, T.; Żołnierczuk-Kieliszek, D.; Drop, B.; Firlej, E.; Gajewska, I. General Self-Efficacy Level and Health Behaviours in Women over the Age of 45 Years Who Have Undergone Osteoporosis Treatment. Menopausal Rev. 2017, 3, 86–95. [Google Scholar] [CrossRef] [PubMed]
- Fang, Z.; Ouyang, S. Nursing Effect of Health Monitoring System on Elderly Patients with Osteoporosis. BioMed Res. Int. 2022, 2022, 1447388. [Google Scholar] [CrossRef]
- Ramadan, R.; Hussein, E.; Amr, T. Telenursing of Osteoporosis Self-Management for Women Health. Egypt. J. Nurs. Health Sci. 2020, 1, 42–59. [Google Scholar] [CrossRef]
- Guadalupe-Grau, A.; Fuentes, T.; Guerra, B.; Calbet, J.A.L. Exercise and Bone Mass in Adults. Sports Med. 2009, 39, 439–468. [Google Scholar] [CrossRef]
- Sanchez-Trigo, H.; Maher, C.; Godino, J.G.; Sañudo, B. Effects of an MHealth Physical Activity Intervention to Prevent Osteoporosis in Premenopausal Women. A Randomized Control Trial. J. Sci. Med. Sport. 2023, 26, 545–552. [Google Scholar] [CrossRef]
- Alhussein, G.; Hadjileontiadis, L. Digital Health Technologies for Long-Term Self-Management of Osteoporosis: Systematic Review and Meta-Analysis. JMIR mHealth uHealth 2022, 10, e32557. [Google Scholar] [CrossRef]
- Doshi, K.B.; Moon, S.H.; Whitaker, M.D.; Lockhart, T.E. Assessment of Gait and Posture Characteristics Using a Smartphone Wearable System for Persons with Osteoporosis with and without Falls. Sci. Rep. 2023, 13, 538. [Google Scholar] [CrossRef]
- Tang, Y.; Liu, Z.; Wang, S.; Yi, Q.; Xia, Y.; Geng, B. Development and Validation of a Novel Screening Tool for Osteoporosis in Older US Adults: The NHANES Cross-Sectional Study. Endocrine 2022, 76, 446–456. [Google Scholar] [CrossRef]
- Ryan, P.; Brown, R.L.; Csuka, M.E.; Papanek, P. Efficacy of Osteoporosis Prevention Smartphone App. Nurs. Res. 2020, 69, 31–41. [Google Scholar] [CrossRef]
- Ong, S.C.; Low, J.Z.; Ooi, G.S. Application of Health Belief Model in the Assessment of Factors Affecting Exercise Behaviours in Preventing Osteoporosis. J. Pharm. Health Serv. Res. 2022, 13, 299–307. [Google Scholar] [CrossRef]
- Birkhoff, S.D.; Smeltzer, S.C. Perceptions of Smartphone User-Centered Mobile Health Tracking Apps Across Various Chronic Illness Populations: An Integrative Review. J. Nurs. Scholarsh. 2017, 49, 371–378. [Google Scholar] [CrossRef]
- Livingston, G.; Huntley, J.; Sommerlad, A.; Ames, D.; Ballard, C.; Banerjee, S.; Brayne, C.; Burns, A.; Cohen-Mansfield, J.; Cooper, C.; et al. Dementia Prevention, Intervention, and Care: 2020 Report of the Lancet Commission. Lancet 2020, 396, 413–446. [Google Scholar] [CrossRef]
- Rasmussen, J.; Langerman, H. Alzheimer’s Disease—Why We Need Early Diagnosis. Degener. Neurol. Neuromuscul. Dis. 2019, 9, 123–130. [Google Scholar] [CrossRef] [PubMed]
- Biazus-Sehn, L.F.; Schuch, F.B.; Firth, J.; Stigger, F.d.S. Effects of Physical Exercise on Cognitive Function of Older Adults with Mild Cognitive Impairment: A Systematic Review and Meta-Analysis. Arch. Gerontol. Geriatr. 2020, 89, 104048. [Google Scholar] [CrossRef] [PubMed]
- Parnetti, L.; Chipi, E.; Salvadori, N.; D’Andrea, K.; Eusebi, P. Prevalence and Risk of Progression of Preclinical Alzheimer’s Disease Stages: A Systematic Review and Meta-Analysis. Alzheimers Res. Ther. 2019, 11, 7. [Google Scholar] [CrossRef]
- Thabtah, F.; Peebles, D.; Retzler, J.; Hathurusingha, C. Dementia Medical Screening Using Mobile Applications: A Systematic Review with a New Mapping Model. J. Biomed. Inf. 2020, 111, 103573. [Google Scholar] [CrossRef]
- Shellington, E.M.; Felfeli, T.; Shigematsu, R.; Gill, D.P.; Petrella, R.J. HealtheBrain: An Innovative Smartphone Application to Improve Cognitive Function in Older Adults. Mhealth 2017, 3, 17. [Google Scholar] [CrossRef]
- Kwan, R.Y.; Lee, D.; Lee, P.H.; Tse, M.; Cheung, D.S.; Thiamwong, L.; Choi, K.-S. Effects of an MHealth Brisk Walking Intervention on Increasing Physical Activity in Older People with Cognitive Frailty: Pilot Randomized Controlled Trial. JMIR Mhealth Uhealth 2020, 8, e16596. [Google Scholar] [CrossRef] [PubMed]
- King, A.C.; Hekler, E.B.; Grieco, L.A.; Winter, S.J.; Sheats, J.L.; Buman, M.P.; Banerjee, B.; Robinson, T.N.; Cirimele, J. Harnessing Different Motivational Frames via Mobile Phones to Promote Daily Physical Activity and Reduce Sedentary Behavior in Aging Adults. PLoS ONE 2013, 8, e62613. [Google Scholar] [CrossRef]
- Lugones-Sanchez, C.; Recio-Rodriguez, J.I.; Agudo-Conde, C.; Repiso-Gento, I.; Adalia, E.G.; Ramirez-Manent, J.I.; Sanchez-Calavera, M.A.; Rodriguez-Sanchez, E.; Gomez-Marcos, M.A.; Garcia-Ortiz, L. Long-Term Effectiveness of a Smartphone App Combined With a Smart Band on Weight Loss, Physical Activity, and Caloric Intake in a Population With Overweight and Obesity (Evident 3 Study): Randomized Controlled Trial. J. Med. Internet Res. 2022, 24, e30416. [Google Scholar] [CrossRef]
- Coelho, C.M.; Reboredo, M.M.; Valle, F.M.; Malaguti, C.; Campos, L.A.; Nascimento, L.M.; Carvalho, E.V.; Oliveira, J.C.A.; Pinheiro, B.V. Effects of an Unsupervised Pedometer-Based Physical Activity Program on Daily Steps of Adults with Moderate to Severe Asthma: A Randomized Controlled Trial. J. Sports Sci. 2018, 36, 1186–1193. [Google Scholar] [CrossRef]
- Norton, K.; Norton, L.; Lewis, N. Effects of Short-Term Physical Activity Interventions on Simple and Choice Response Times. BioMed Res. Int. 2016, 2016, 5613767. [Google Scholar] [CrossRef]
- Haug, S.; Castro, R.P.; Kwon, M.; Filler, A.; Kowatsch, T.; Schaub, M.P. Smartphone Use and Smartphone Addiction among Young People in Switzerland. J. Behav. Addict. 2015, 4, 299–307. [Google Scholar] [CrossRef]
- Pearson, C.; Hussain, Z. Smartphone Use, Addiction, Narcissism, and Personality. Int. J. Cyber Behav. Psychol. Learn. 2015, 5, 17–32. [Google Scholar] [CrossRef]
- Noë, B.; Turner, L.D.; Linden, D.E.J.; Allen, S.M.; Winkens, B.; Whitaker, R.M. Identifying Indicators of Smartphone Addiction Through User-App Interaction. Comput. Hum. Behav. 2019, 99, 56–65. [Google Scholar] [CrossRef] [PubMed]
| Database | Specificities of the Database | Search Strategy |
|---|---|---|
| Scopus PubMed EBSCO Web of Science | Search for title and abstract also includes keywords | (“mHealth” OR “Mobile Health” OR “E-health”) AND (“App” OR “Smartphone application”) AND (“Mobile” OR “Smartphone”) AND (“Physical Activity” OR “Exercise”) AND (“Health Education” OR “Patient Education”) AND (“Self-monitoring” OR “Self-tracking”) AND (“Steps” OR “Step count”) AND (“Disease” OR “Illness” OR “Condition”) AND (“Weight loss” OR “Weight management”) AND (“Cardiovascular disease” OR “Heart disease”) AND (“Diabetes” OR “Diabetic”) AND (“Cancer” OR “Oncology”) AND (“Osteoporosis” OR “Bone health”) AND (“Cognitive decline” OR “Cognitive function”) NOT (“Smartphone” AND “Physical Activity”) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Di Martino, G.; della Valle, C.; Centorbi, M.; Buonsenso, A.; Fiorilli, G.; Calcagno, G.; Iuliano, E.; di Cagno, A. Enhancing Behavioural Changes: A Narrative Review on the Effectiveness of a Multifactorial APP-Based Intervention Integrating Physical Activity. Int. J. Environ. Res. Public Health 2024, 21, 233. https://doi.org/10.3390/ijerph21020233
Di Martino G, della Valle C, Centorbi M, Buonsenso A, Fiorilli G, Calcagno G, Iuliano E, di Cagno A. Enhancing Behavioural Changes: A Narrative Review on the Effectiveness of a Multifactorial APP-Based Intervention Integrating Physical Activity. International Journal of Environmental Research and Public Health. 2024; 21(2):233. https://doi.org/10.3390/ijerph21020233
Chicago/Turabian StyleDi Martino, Giulia, Carlo della Valle, Marco Centorbi, Andrea Buonsenso, Giovanni Fiorilli, Giuseppe Calcagno, Enzo Iuliano, and Alessandra di Cagno. 2024. "Enhancing Behavioural Changes: A Narrative Review on the Effectiveness of a Multifactorial APP-Based Intervention Integrating Physical Activity" International Journal of Environmental Research and Public Health 21, no. 2: 233. https://doi.org/10.3390/ijerph21020233
APA StyleDi Martino, G., della Valle, C., Centorbi, M., Buonsenso, A., Fiorilli, G., Calcagno, G., Iuliano, E., & di Cagno, A. (2024). Enhancing Behavioural Changes: A Narrative Review on the Effectiveness of a Multifactorial APP-Based Intervention Integrating Physical Activity. International Journal of Environmental Research and Public Health, 21(2), 233. https://doi.org/10.3390/ijerph21020233










