Australian Women’s Experiences of Establishing Breastfeeding after Caesarean Birth
Abstract
1. Introduction
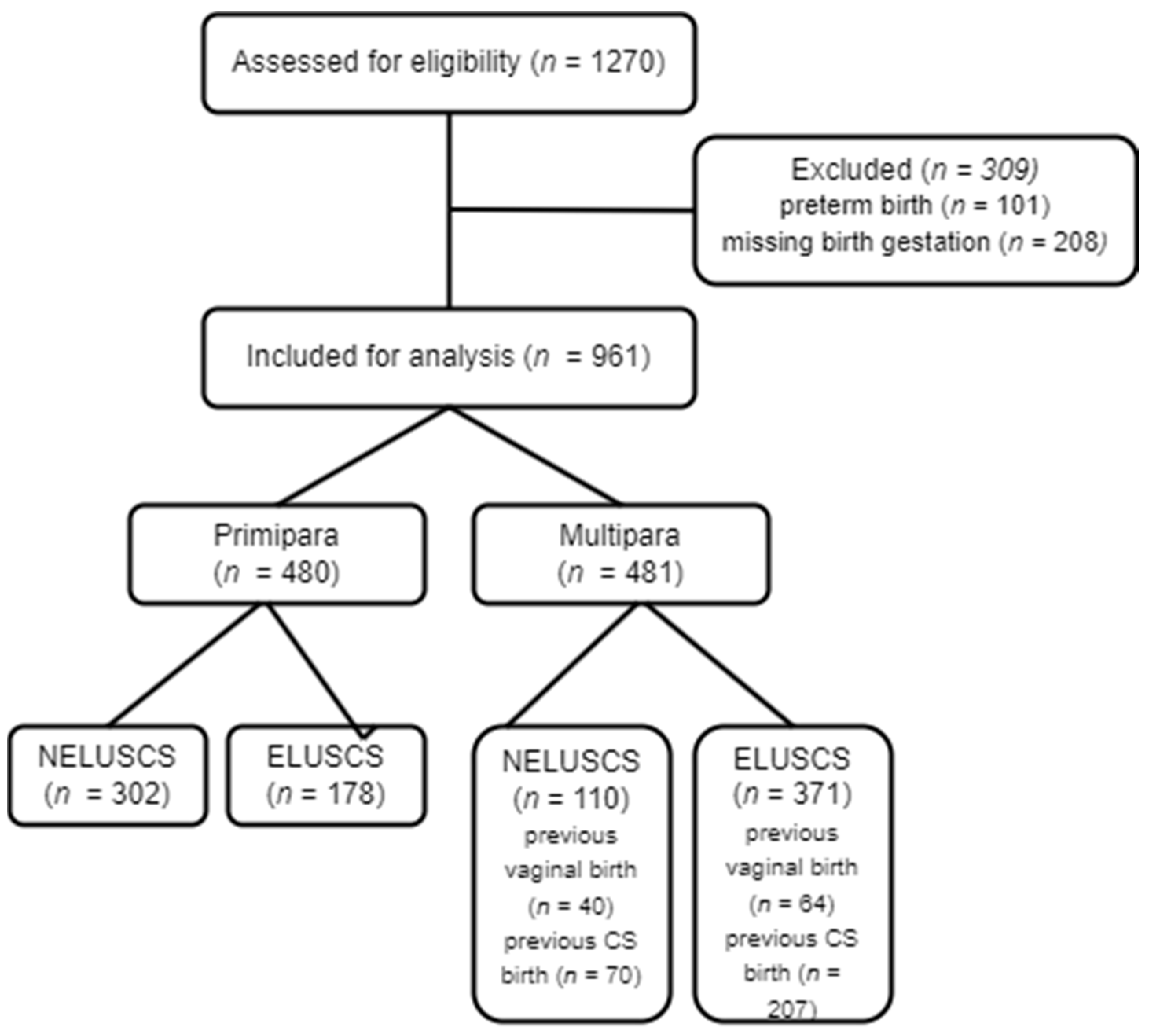
2. Materials and Methods
3. Results
3.1. Quantitative Findings
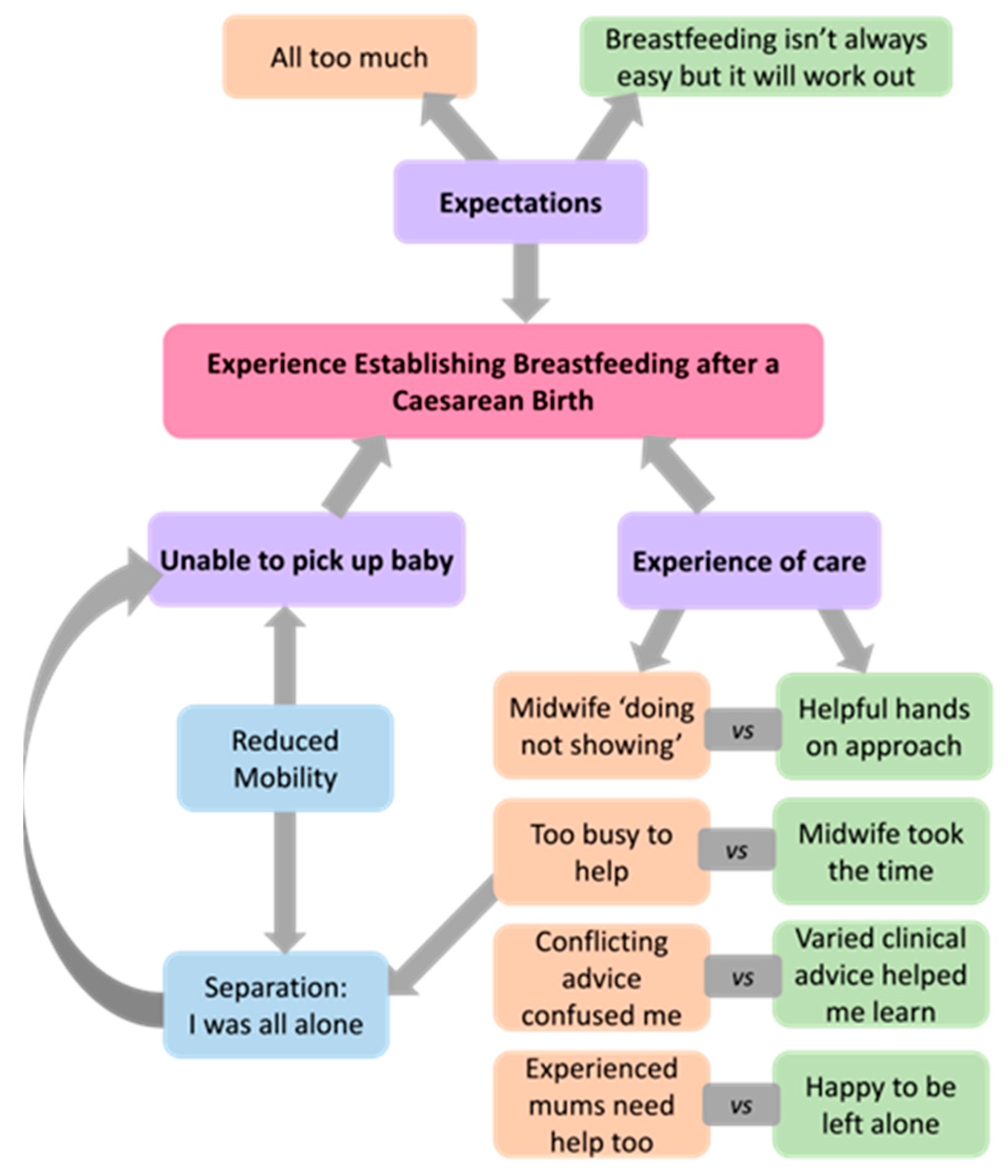
3.2. Qualitative Findings
3.2.1. Theme I. Experience of Care
- ‘Midwives doing, not showing’ versus ‘helpful hands-on approach’.
- ‘Too busy to help’ versus ‘midwife took the time’.
- ‘Conflicting advice confused me’ versus ‘varied clinical advice facilitated my learning’.
‘… each midwife had their different ideas of how it should be done which was sometimes frustrating and not consistent’ (P, ELUSCS).
‘Staff telling me to do different things. I was trying something one midwife suggested, only to be told I was doing it wrong by another midwife. It was confusing. I just wanted to find my groove with my baby, and I would ask if I needed help. But the staff loved to interfere’ (P, ELUSCS).
- ‘Experienced mums need help too’ versus ‘happy to be left alone’.
3.2.2. Theme II: Expectations
- All too much
- Breastfeeding isn’t always easy, but it will work out
3.2.3. Theme III: Unable to Pick Up Baby
- Reduced mobility: a multifaceted barrier
‘After a traumatic birth in a public hospital, my partner was not allowed to stay overnight. I found it exceptionally traumatizing to be left several hours after major abdominal surgery, unable to pluck my baby from his crib and manage him on my own. I was in agony from the caesarean and I didn’t know how to breastfeed’ (P, NELUSCS).
‘My husband was not allowed to stay outside of visiting hours. This coupled with the midwifes [sic] being very busy at night left me feeling like I had no support… The main motivation for me leaving the hospital so soon after birth was the fact I would have help from my husband at home’ (P, NELUSCS).
‘I was in the public hospital so I couldn’t get my husband to stay and help me with the baby overnight … that was absolutely complicate and really bad experience I never felt more lonely in pain, no available to move by myself … I need help for stand up and look after the baby, nurses no was all the time there … so much easier if I have my husband in there helping me, was hard to hold the baby, stand up with a c section to clean the baby many times overnight try to teach him to eat from my breast. Was absolutely traumatic and sad be by myself that 2 nights without husband…because the sistem rules he can’t stay to help so it affect my breastfeeding I think and I stop producing milk because was under stress’ (P, NELUSCS).
- Separation from baby
‘I spent the first night in the ICU following a postpartum haemorrhage as they did not think they could monitor me adequately on the maternity ward. They said they would bring my baby to me regularly for feeding, but they were busy and didn’t…’ (P, NELUSCS).
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Thirukumar, P.; Coates, D.; Henry, A. Women’s experiences of intrapartum care and recovery in relation to planned caesarean sections: An interview study. Women Birth 2021, 34, e248–e254. [Google Scholar] [CrossRef]
- Sandall, J.; Tribe, R.M.; Avery, L.; Mola, G.; Visser, G.H.; Homer, C.S.; Gibbons, D.; Kelly, N.M.; Kennedy, H.P.; Kidanto, H.; et al. Short-term and long-term effects of caesarean section on the health of women and children. Lancet 2018, 392, 1349–1357. [Google Scholar] [CrossRef]
- Singh, J.; Scime, N.V.; Chaput, K.H. Association of Caesarean delivery and breastfeeding difficulties during the delivery hospitalization: A community-based cohort of women and full-term infants in Alberta, Canada. Can. J. Public Health 2023, 114, 104–112. [Google Scholar] [CrossRef] [PubMed]
- Andrew, M.S.; Selvaratnam, R.J.; Davies-Tuck, M.; Howland, K.; Davey, M. The association between intrapartum interventions and immediate and ongoing breastfeeding outcomes: An Australian retrospective population-based cohort study. Int. Breastfeed. J. 2022, 17, 48. [Google Scholar] [CrossRef]
- Li, Z.; Mannava, P.; Murray, J.C.S.; Sobel, H.L.; Jatobatu, A.; Calibo, A.; Tsevelmaa, B.; Saysanasongkham, B.; Ogaoga, D.; Waramin, E.J.; et al. Association between early essential newborn care and breastfeeding outcomes in eight countries in Asia and the Pacific: A cross-sectional observational-study. BMJ Glob. Health 2020, 5, e002581. [Google Scholar] [CrossRef]
- Hobbs, A.J.; Mannion, C.A.; McDonald, S.W.; Brockway, M.; Tough, S.C. The impact of caesarean section on breastfeeding initiation, duration and difficulties in the first four months postpartum. BMC Pregnancy Childbirth 2016, 16, 90. [Google Scholar] [CrossRef] [PubMed]
- Vaz, J.S.; Maia, M.F.S.; Neves, P.A.R.; Santos, T.M.; Vidaletti, L.P.; Victora, C. Monitoring breastfeeding indicators in high-income countries: Levels, trends and challenges. Matern. Child. Nutr. 2021, 17, e13137. [Google Scholar] [CrossRef]
- Wu, Y.; Wang, Y.; Huang, J.; Zhang, Z.; Wang, J.; Zhou, L.; Ni, Z.; Hao, L.; Yang, N.; Yang, X. The association between caesarean delivery and the initiation and duration of breastfeeding: A prospective cohort study in China. Eur. J. Clin. Nutr. 2018, 72, 1644–1654. [Google Scholar] [CrossRef] [PubMed]
- Hooda, R.; Malik, N.; Pathak, P.; More, H.; Singh, V. Impact of Postoperative Pain on Early Initiation of Breastfeeding and Ambulation After Cesarean Section: A Randomized Trial. Breastfeed. Med. 2023, 18, 132–137. [Google Scholar] [CrossRef]
- Patil, D.S.; Pundir, P.; Dhyani, V.S.; Krishnan, J.B.; Parsekar, S.S.; D’Souza, S.M.; Ravishankar, N.; Renjith, V. A mixed-methods systematic review on barriers to exclusive breastfeeding. Nutr. Health 2020, 26, 323–346. [Google Scholar] [CrossRef]
- Vehling, L.; Chan, D.; McGavock, J.; Becker, A.B.; Subbarao, P.; Moraes, T.J.; Mandhane, P.J.; Turvey, S.E.; Lefebvre, D.L.; Sears, M.R.; et al. Exclusive breastfeeding in hospital predicts longer breastfeeding duration in Canada: Implications for health equity. Birth 2018, 45, 440–449. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Yan, Y.; Gao, X.; Xiang, S.; He, Q.; Zeng, G.; Liu, S.; Sha, T.; Li, L. Influences of Cesarean Delivery on Breastfeeding Practices and Duration: A Prospective Cohort Study. J. Hum. Lact. 2018, 34, 526–534. [Google Scholar] [CrossRef] [PubMed]
- Nagel, E.M.; Howland, M.A.; Pando, C.; Stang, J.; Mason, S.M.; Fields, D.A.; Demerath, E.W. Maternal Psychological Distress and Lactation and Breastfeeding Outcomes: A Narrative Review. Clin. Ther. 2022, 44, 215–227. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Lai, X.; Zhou, L.; Retnakaran, R.; Wen, S.W.; Krewski, D.; Huang, L.; Li, M.; Xie, R.H. Association between exclusive breastfeeding and postpartum post-traumatic stress disorder. Int. Breastfeed. J. 2022, 17, 78. [Google Scholar] [CrossRef] [PubMed]
- Shepherd, L.; Walbey, C.; Lovell, B. The Role of Social-Cognitive and Emotional Factors on Exclusive Breastfeeding Duration. J. Hum. Lact. 2017, 33, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Betran, A.P.; Ye, J.; Moller, A.B.; Souza, J.P.; Zhang, J. Trends and projections of caesarean section rates: Global and regional estimates. BMJ Glob. Health 2021, 6, e005671. [Google Scholar] [CrossRef]
- Renjith, V.; Yesodharan, R.; Noronha, J.A.; Ladd, E.; George, A. Qualitative Methods in Health Care Research. Int. J. Prev. Med. 2021, 12, 20. [Google Scholar]
- The Royal Australian and New Zealand College of Obstetricians and Gynaecologists. Categorisation of Urgency for Caesarean Section. 2019. Available online: https://ranzcog.edu.au/RANZCOG_SITE/media/RANZCOG-MEDIA/Women%27s%20Health/Statement%20and%20guidelines/Clinical-Obstetrics/Categorisation-of-urgency-for-caesarean-section--(C-Obs-14).pdf?ext=.pdf (accessed on 30 July 2023).
- Altuntug, K.; Kiyak, S.; Ege, E. Relationship between birth memories and recall and perception of traumatic birth in women in the postpartum one-year period and affecting factors. Curr. Psychol. 2023, 43, 876–884. [Google Scholar] [CrossRef]
- Li, R.; Ingol, T.T.; Smith, K.; Oza-Frank, R.; Keim, S.A. Reliability of Maternal Recall of Feeding at the Breast and Breast Milk Expression 6 Years after Delivery. Breastfeed. Med. 2020, 15, 224–236. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J.; et al. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inform. 2019, 95, 103208. [Google Scholar] [CrossRef] [PubMed]
- Perez-Escamilla, R.; Tomori, C.; Hernandez-Cordero, S.; Baker, P.; Barros, A.J.D.; Begin, F.; Chapman, D.J.; Grummer-Strawn, L.M.; McCoy, D.; Menon, P.; et al. Breastfeeding: Crucially important, but increasingly challenged in a market-driven world. Lancet 2023, 401, 472–485. [Google Scholar] [CrossRef]
- Li, L.; Wan, W.; Zhu, C. Breastfeeding after a cesarean section: A literature review. Midwifery 2021, 103, 103117. [Google Scholar] [CrossRef]
- Hadisuyatmana, S.; Has, E.M.M.; Sebayang, S.K.; Efendi, F.; Astutik, E.; Kuswanto, H.; Arizona, I. Women’s Empowerment and Determinants of Early Initiation of Breastfeeding: A Scoping Review. J. Pediatr. Nurs. 2021, 56, e77–e92. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.H.; Hsieh, Y.J.; Wei, K.H.; Sun, W.Z.; Tsao, S.L. A comparison of spinal and epidural anesthesia for cesarean section following epidural labor analgesia: A retrospective cohort study. Acta Anaesthesiol. Taiwan. 2015, 53, 7–11. [Google Scholar] [CrossRef]
- Babazade, R.; Vadhera, R.B.; Krishnamurthy, P.; Varma, A.; Doulatram, G.; Saade, G.R.; Turan, A. Acute postcesarean pain is associated with in-hospital exclusive breastfeeding, length of stay and post-partum depression. J. Clin. Anesth. 2020, 62, 109697. [Google Scholar] [CrossRef]
- Yimer, H.; Woldie, H. Incidence and Associated Factors of Chronic Pain After Caesarean Section: A Systematic Review. J. Obstet. Gynaecol. Can. 2019, 41, 840–854. [Google Scholar] [CrossRef] [PubMed]
- Wright, S.A.; Higgins, C.; Carson, J.; Kinnear, M.; Smith, P.; Mary, N.; Westall, E.; Arshad, S. Self-administration of medications in inpatient postnatal women: An opportunity to empower self-care, improved medicines knowledge and adherence utilising clinical pharmacists and midwifery workforce and use of a midwife formulary. Eur. J. Hosp. Pharm. 2023, 30, 279–283. [Google Scholar] [CrossRef]
- Zimpel, S.A.; Torloni, M.R.; Porfirio, G.J.; Flumignan, R.L.; da Silva, E.M. Complementary and alternative therapies for post-caesarean pain. Cochrane Database Syst. Rev. 2020, 9, CD011216. [Google Scholar] [CrossRef]
- Borges, N.C.; Pereira, L.V.; de Moura, L.A.; Silva, T.C.; Pedroso, C.F. Predictors for Moderate to Severe Acute Postoperative Pain after Cesarean Section. Pain. Res. Manag. 2016, 2016, 5783817. [Google Scholar] [CrossRef]
- Sangkum, L.; Thamjamrassri, T.; Arnuntasupakul, V.; Chalacheewa, T. The Current Consideration, Approach, and Management in Postcesarean Delivery Pain Control: A Narrative Review. Anesthesiol. Res. Pract. 2021, 2021, 2156918. [Google Scholar] [CrossRef] [PubMed]
- Tully, K.P.; Ball, H.L. Maternal accounts of their breast-feeding intent and early challenges after caesarean childbirth. Midwifery 2014, 30, 712–719. [Google Scholar] [CrossRef]
- Chaplin, J.; Kelly, J.; Kildea, S. Maternal perceptions of breastfeeding difficulty after caesarean section with regional anaesthesia: A qualitative study. Women Birth 2016, 29, 144–152. [Google Scholar] [CrossRef] [PubMed]
- Ohrn, U.; Parment, H.; Hildingsson, I. Quality improvement in postnatal care: Findings from two cohorts of women in Sweden. Eur. J. Midwifery 2020, 4, 45. [Google Scholar] [CrossRef] [PubMed]
- Davidson, E.L.; Ollerton, R.L. Partner behaviours improving breastfeeding outcomes: An integrative review. Women Birth 2020, 33, e15–e23. [Google Scholar] [CrossRef]
- Sakalidis, V.S.; Perrella, S.L.; Prosser, S.A.; Geddes, D.T. Breastfeeding in a COVID-19 world. Curr. Opin. Clin. Nutr. Metab. Care 2022, 25, 188–194. [Google Scholar] [CrossRef]
- Crippa, B.L.; Consales, A.; Morniroli, D.; Lunetto, F.; Bettinelli, M.E.; Sannino, P.; Rampini, S.; Zanotta, l.; Marchisio, P.; Plevani, L.; et al. From dyad to triad: A survey on fathers’ knowledge and attitudes toward breastfeeding. Eur. J. Pediatr. 2022, 180, 2861–2869. [Google Scholar] [CrossRef]
- Schobinger, E.; Vanetti, M.; Ramelet, A.S.; Horsch, A. Social support needs of first-time parents in the early-postpartum period: A qualitative study. Front. Psychiatry 2022, 13, 1043990. [Google Scholar] [CrossRef]
- Mabele, O.M.; Benedict, M.O.A.; Steinberg, W.J.; Reji, E.; Van Rooyen, C.; Adefuye, A.O. Knowledge, attitudes and practices of men in a South African rural community in relation to exclusive breastfeeding. S. Afr. Fam. Pract. 2022, 64, e1–e8. [Google Scholar] [CrossRef]
- Tully, K.P.; Ball, H.L. Postnatal unit bassinet types when rooming-in after cesarean birth: Implications for breastfeeding and infant safety. J. Hum. Lact. 2012, 28, 495–505. [Google Scholar] [CrossRef]
- Perrella, S.L.; Miraudo, J.; Rea, A.; Geddes, D.T.; Prosser, S.A. Maternal Evaluation of a Team-Based Maternity Care Model for Women of Low Obstetric Risk. J. Patient Exp. 2022, 9, 23743735221092606. [Google Scholar] [CrossRef]
- Malouf, R.; Henderson, J.; Alderdice, F. Expectations and experiences of hospital postnatal care in the UK: A systematic review of quantitative and qualitative studies. BMJ Open 2019, 9, e022212. [Google Scholar] [CrossRef]
- Turner, L.; Ball, J.; Culliford, D.; Kitson-Reynolds, E.; Griffiths, P. Exploring the relationship between women’s experience of postnatal care and reported staffing measures: An observational study. PLoS ONE 2022, 17, e0266638. [Google Scholar] [CrossRef]
- Gavine, A.; Shinwell, S.C.; Buchanan, P.; Farre, A.; Wade, A.; Lynn, F.; Marshall, J.; Cumming, S.E.; Dare, S.; McFadden, A. Support for healthy breastfeeding mothers with healthy term babies. Cochrane Database Syst. Rev. 2022, 10, CD001141. [Google Scholar] [CrossRef]
- Thompson, D.; Leach, M.; Smith, C.; Fereday, J.; May, E. How nurses and other health professionals use learning principles in parent education practice: A scoping review of the literature. Heliyon 2020, 6, e03564. [Google Scholar] [CrossRef] [PubMed]
- Lojander, J.; Mäkelä, H.; Niela-Vilén, H. Maternal perceptions and experiences of breastfeeding support in Baby-Friendly hospitals: An integrative review. Int. J. Nurs. Stud. Adv. 2022, 4, 100105. [Google Scholar] [CrossRef]
- Perez-Escamilla, R.; Martinez, J.L.; Segura-Perez, S. Impact of the Baby-friendly Hospital Initiative on breastfeeding and child health outcomes: A systematic review. Matern. Child Nutr. 2016, 12, 402–417. [Google Scholar] [CrossRef]
- Orovou, E.; Iliadou, M.; Chatzopoulou, M.T.; Dagla, M.; Eskitzis, P.; Rigas, N.; Antoniou, E. The Relation between Birth with Cesarean Section and Posttraumatic Stress in Postpartum Women. Maedica 2023, 18, 615–622. [Google Scholar] [PubMed]
- Green, G.; Tesler, R.; Marques, A. Primiparous and Multiparous Women’s Mode of Birth and Negative Emotions. Int. J. Environ. Res. Public Health 2022, 19, 5189. [Google Scholar] [CrossRef]
- Urbanová, E.; Škodová, Z.; Bašková, M. The Association between Birth Satisfaction and the Risk of Postpartum Depression. Int. J. Environ. Res. Public Health 2021, 18, 10458. [Google Scholar] [CrossRef]
- Webb, R.; Ayers, S.; Bogaerts, A.; Jelicic, L.; Pawlicka, P.; Van Haeken, S.; Uddin, N.; Xuereb, R.; Kolesnikova, N.; COST Action CA18211:DEVoTION Team. When birth is not as expected: A systematic review of the impact of a mismatch between expectations and experiences. BMC Pregnancy Childbirth 2021, 21, 475. [Google Scholar] [CrossRef] [PubMed]
- Davis, A.M.B.; Sclafani, V. Birth Experiences, Breastfeeding, and the Mother-Child Relationship: Evidence from a Large Sample of Mothers. Can. J. Nurs. 2022, 54, 518–529. [Google Scholar] [CrossRef] [PubMed]
- Whitaker, C.; Stevelink, S.; Fear, N. The Use of Facebook in Recruiting Participants for Health Research Purposes: A Systematic Review. J. Med. Internet Res. 2017, 19, e290. [Google Scholar] [CrossRef]
- Pramono, A.; Smith, J.; Desborough, J.; Bourke, S. Social value of maintaining baby-friendly hospital initiative accreditation in Australia: Case study. Int. J. Equity Health 2021, 20, 22. [Google Scholar] [CrossRef] [PubMed]
| Overall (n = 961) | NELUSCS (n = 412) | ELUSCS (n = 549) | |
|---|---|---|---|
| BMI category | |||
| Underweight (<18.5) | 17 (1.8) | 5 (1.2) | 12 (2.2) |
| Normal (18.5–24.9) | 435 (45.3) | 182 (44.2) | 253 (46.1) |
| Overweight (25.0–29.9) | 258 (26.8) | 115 (27.9) | 143 (26.0) |
| Obese (≥30.0) | 241 (25.1) | 105 (25.5) | 136 (24.8) |
| Missing | 10 (1.0) | 5 (1.2) | 5 (0.9) |
| SEIFA index percentile | |||
| 0–30 most disadvantaged | 96 (10.0) | 41 (10.0) | 55 (10.0) |
| 30–70 | 415 (43.2) | 193 (46.8) | 222 (40.4) |
| 70–100 least disadvantaged | 444 (46.2) | 177 (43.0) | 267 (48.6) |
| Missing | 6 (0.6) | 1 (0.2) | 5 (0.9) |
| Ethnic group | |||
| Australian | 722 (75.1) | 307 (74.5) | 415 (75.6) |
| British | 108 (11.2) | 49 (11.9) | 59 (10.7) |
| Aboriginal or TSI | 23 (2.4) | 14 (3.4) | 9 (1.6) |
| Other | 217 (22.6) | 98 (23.8) | 430 (78.3) |
| Overall | NELUSCS | ELUSCS | Primipara | Multipara | |
|---|---|---|---|---|---|
| (n = 961) | (n = 412) | (n = 549) | (n = 480) | (n = 481) | |
| Birth at public hospital | 493 (51.3) | 263 (63.8) | 230 (41.9) | 237 (49.4) | 256 (53.2) |
| Caesarean anaesthesia | |||||
| Spinal block | 517 (53.8) | 99 (24.0) | 418 (76.1) | 194 (40.4) | 323 (67.2) |
| Epidural | 221 (23.0) | 177 (43.0) | 44 (8.0) | 152 (31.7) | 69 (14.3) |
| Combined | 148 (15.4) | 88 (21.4) | 60 (10.9) | 99 (20.6) | 49 (10.2) |
| General anaesthetic | 32 (3.3) | 28 (6.8) | 4 (0.7) | 15 (3.1) | 17 (3.5) |
| Unsure/missing | 43 (4.4) | 20 (4.8) | 23 (4.2) | 20 (4.1) | 23 (4.7) |
| Pain rating after birth | 6.0 (4.0, 8.0) | 7.0 (5.0, 8.0) | 6.0 (4.0, 7.0) | 6.0 (5.0, 8.0) | 6.0 (4.0, 7.75) |
| Birth complications | |||||
| None | 700 (72.8) | 257 (62.4) | 443 (80.7) | 335 (69.8) | 365 (75.9) |
| Infant resuscitation | 33 (3.4) | 24 (5.8) | 9 (1.6) | 19 (4.0) | 14 (2.9) |
| Neonatal unit admission | 117 (12.2) | 63 (15.3) | 54 (9.8) | 49 (10.2) | 68 (14.2) |
| Postpartum haemorrhage | 68 (7.1) | 41 (10.0) | 27 (4.9) | 31 (6.5) | 37 (7.7) |
| Birth experience rating | |||||
| Quite easy | 444 (46.2) | 58 (14.1) | 386 (70.3) | 172 (35.8) | 272 (56.5) |
| Difficult but overall okay | 221 (23.0) | 127 (30.8) | 94 (17.1) | 120 (25.0) | 101 (21.0) |
| A little traumatic | 197 (20.5) | 140 (34.0) | 57 (10.4) | 123 (25.6) | 74 (15.4) |
| Very traumatic | 99 (10.3) | 87 (21.1) | 12 (2.2) | 65 (13.5) | 34 (7.1) |
| Birth expectations met | 545 (56.7) | 93 (22.6) | 452 (82.3) | 211 (44.0) | 334 (69.4) |
| BF initiated ≤ 1 h birth | 675 (70.2) | 245 (59.5) | 430 (78.3) | 304 (63.4) | 371 (77.1) |
| Covariate | Univariate Analysis Odds Ratio (95% CI) | p | Multivariate Analysis Odds Ratio (95% CI) | p |
|---|---|---|---|---|
| (Intercept) | 5.89 (3.65–9.02) | <0.001 | ||
| CS type: NELUSCS | 0.40 (0.30–0.53) | <0.001 | 0.50 (0.36–0.68) | <0.001 |
| Parity: primipara | 0.50 (0.37–0.66) | <0.001 | 0.68 (0.50–0.94) | 0.02 |
| Pain score after birth | 0.92 (0.86–0.98) | 0.011 | 0.95 (0.89–1.02) | 0.13 |
| Overall (n = 961) | NELUSCS (n = 412) | ELUSCS (n = 549) | Primipara (n = 480) | Multipara (n = 481) | |
|---|---|---|---|---|---|
| Pain rating | |||||
| Mild (≤3) | 158 (16.4) | 42 (10.2) | 116 (21.1) | 62 (12.9) | 96 (20.0) |
| Moderate (4–6) | 351 (36.5) | 146 (35.4) | 205 (37.3) | 176 (36.7) | 175 (36.4) |
| Severe (≥7) | 426 (44.3) | 210 (51.0) | 216 (39.3) | 231 (48.1) | 195 (40.5) |
| Missing | 26 (2.7) | 14 (3.4) | 12 (2.2) | 11 (2.3) | 15 (3.1) |
| Pain impacted BF | |||||
| Yes | 197 (20.5) | 129 (31.3) | 68 (12.4) | 125 (26.0) | 72 (15.0) |
| No | 689 (71.7) | 247 (60.0) | 442 (80.5) | 323 (67.3) | 366 (76.1) |
| Missing | 75 (7.8) | 36 (8.7) | 39 (7.1) | 32 (6.7) | 43 (8.9) |
| Feeding method | |||||
| Breastfeeding | 771 (80.2) | 311 (75.5) | 460 (83.8) | 356 (74.2) | 415 (86.3) |
| Expressed milk | 230 (23.9) | 113 (27.4) | 101 (21.0) | 129 (26.9) | 101 (21.0) |
| Infant formula | 308 (32.1) | 154 (37.4) | 108 (22.5) | 200 (41.7) | 108 (22.5) |
| Hospital stay (days) | 4 (3,5) | 4 (3,5) | 4 (3,5) | 4 (3,5) | 4 (3,5) |
| Missing | 26 (2.7%) | 12 (3.4%) | 12 (2.2%) | 11 (2.3%) | 15 (3.1%) |
| Covariate | Univariate Analysis Odds Ratio (95% CI) | p | Multivariate Analysis Odds ratio (95% CI) | p |
|---|---|---|---|---|
| (Intercept) | 0.37 (0.25–0.56) | <0.001 | ||
| CS type: NELUSCS | 1.40 (1.07–1.82) | 0.013 | 1.02 (0.71–1.47) | 0.91 |
| Parity: primipara | 2.23 (1.71–2.92) | <0.001 | 2.16 (1.60–2.91) | <0.001 |
| Pain score after birth | 1.07 (1.01–1.13) | 0.033 | 1.05 (0.99–1.12) | 0.12 |
| Birth at private hospital | 1.52 (1.17–1.98) | 0.002 | 1.67 (1.25–2.32) | 0.001 |
| Birth complications | 2.16 (1.61–2.90) | <0.001 | 2.25 (1.64–3.10) | <0.001 |
| Unmet birth expectations | 1.26 (0.96–1.63) | 0.091 | 0.91 (0.63–1.31) | 0.61 |
| Covariate | Univariate Analysis Odds Ratio (95% CI) | p | Multivariate Analysis Odds Ratio (95% CI) | p |
|---|---|---|---|---|
| (Intercept) | 0.02 (0.01–0.04) | <0.001 | ||
| CS type: NELUSCS | 11.58 (8.21–16.60) | <0.001 | 10.21 (6.88–15.43) | <0.001 |
| Parity: primipara | 2.34 (1.75–3.14) | <0.001 | 0.98 (0.66–1.44) | 0.92 |
| Pain score after birth | 1.29 (1.20–1.39) | <0.001 | 1.23 (1.13–1.34) | 0.13 |
| Birth complications | 4.80 (3.53–6.55) | <0.001 | 3.95 (2.74–5.72) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Perrella, S.L.; Abelha, S.G.; Vlaskovsky, P.; McEachran, J.L.; Prosser, S.A.; Geddes, D.T. Australian Women’s Experiences of Establishing Breastfeeding after Caesarean Birth. Int. J. Environ. Res. Public Health 2024, 21, 296. https://doi.org/10.3390/ijerph21030296
Perrella SL, Abelha SG, Vlaskovsky P, McEachran JL, Prosser SA, Geddes DT. Australian Women’s Experiences of Establishing Breastfeeding after Caesarean Birth. International Journal of Environmental Research and Public Health. 2024; 21(3):296. https://doi.org/10.3390/ijerph21030296
Chicago/Turabian StylePerrella, Sharon L., Sarah G. Abelha, Philip Vlaskovsky, Jacki L. McEachran, Stuart A. Prosser, and Donna T. Geddes. 2024. "Australian Women’s Experiences of Establishing Breastfeeding after Caesarean Birth" International Journal of Environmental Research and Public Health 21, no. 3: 296. https://doi.org/10.3390/ijerph21030296
APA StylePerrella, S. L., Abelha, S. G., Vlaskovsky, P., McEachran, J. L., Prosser, S. A., & Geddes, D. T. (2024). Australian Women’s Experiences of Establishing Breastfeeding after Caesarean Birth. International Journal of Environmental Research and Public Health, 21(3), 296. https://doi.org/10.3390/ijerph21030296






