Abstract
Community-based chronic disease prevention programs can have long-term, broad public health benefits. Yet, only 40 to 60% of evidence-based health programs are sustained. Using established frameworks and evidence-based tools to characterize sustainability allows programs to develop structures and processes to leverage resources effectively to sustain effective program activities and systems. This study used a mixed-methods, partner-engaged approach to identify barriers and facilitators to sustaining a community network (the Alliance program) aimed to increase participation in evidence-based lifestyle change programs delivered in the community. Surveys and qualitative interviews were conducted with the Alliance partners based on the Program Sustainability Assessment Tool and Consolidated Framework for Implementation Research. Overall, partners felt Alliance had a high capacity for sustainability. Strategic planning, communication, and partnerships were areas partners prioritized to improve the potential for sustaining the program. Results informed the co-development of a sustainability action plan. This paper furthers our understanding of factors critical for the sustainability of community-based programs for chronic disease prevention and health equity and presents a process for developing action plans to build sustainability capacity.
1. Introduction
Evidence-based chronic disease prevention programs that are offered in the community can have long-term, broad public health benefits and reduce health disparities [1]. Despite substantial investments in the development and implementation of these programs, sustainability can be challenging due to shifts in priorities, fiscal changes, or political climates [2]. Research shows that only 40–60% of health promotion programs are sustained [3,4]. When initial implementation supports or resources are withdrawn, program delivery is diminished or discontinued entirely. Therefore, long-term positive health impacts are often not realized from public health programs or are not achieved equitably across a range of settings and populations, which may further health disparities. This may be especially true for programs targeting chronic diseases, such as diabetes and heart disease, that often require more intensive, maintained programming for mitigation [5]. Furthermore, the frequent discontinuation of effective programs may result in distrust and diminished community support that are critical to engaging community members, especially those in historically marginalized populations, in effective public health programs [6].
Research on ways to improve public health program sustainability has grown over the past decade [7]. There have been substantial increases in knowledge, frameworks, and tools to promote longer-term programs [2,4]. Program sustainability capacity is defined as “the ability to maintain programming and its benefits over time” [2]. Using established frameworks and evidence-based tools to characterize sustainability allows programs to develop structures and processes to leverage resources effectively to sustain effective program activities and systems [8,9]. Sustainability can help to ensure long-term impact, enhance accountability, promote adaptive management, and support learning and improvement. Ultimately, this practice ensures that interventions and programs are designed and implemented with a focus on these core areas and ensures resources needed for investment in these interventions. The Diabetes Prevention Program (DPP) established in 2010 is an example of a sustained program; yet, its reach and impact on under-resourced residents and health disparities are less clear [10].
The St. Louis region is the largest metropolitan area in Missouri and, like many urban areas, faces significant racial and economic disparity challenges. Poverty affects close to 1 in 3 African Americans versus less than 1 in 10 whites in St. Louis City and St. Louis County [11]. The St. Louis Promise Zone and other impoverished areas in the region suffer from inadequate neighborhood and food environments and lack of access to healthcare. Such environments make people in these areas at even higher risk for chronic disease and less likely to attend evidence-based programs to help prevent their disease [12]. Despite seven organizations offering evidence-based lifestyle change programs (LCPs) at multiple locations in St. Louis and virtually, there is a need to create and sustain better referral, enrollment, and retention to support participation among those living in impoverished, high-risk areas.
The Alliance program, which began in 2018, is a collaboration among healthcare, public health, and community organizations [13]. The Alliance was formed to improve referral, enrollment, and successful completion of evidence-based LCPs, particularly among under-resourced residents, to reduce health disparities in St. Louis. The program focuses on two evidence-based LCPs—the DPP and the Blood Pressure Self-Monitoring program. The DPP is an evidenced-based LCP that has demonstrated effective lifestyle change to prevent or delay the onset of type 2 diabetes. The Blood Pressure Self-Monitoring program was developed by the Centers for Disease Prevention and Control (CDC) to help participants measure their blood pressure correctly and consistently and educate them on healthy eating [14]. The self-monitoring of blood pressure is supported by numerous national agencies (e.g., American Heart Association) and can improve the management of hypertension. The Alliance provides a training platform for frontline workers (e.g., community health workers) to help them engage with patients, refer them to evidence-based LCPs, and assess social barriers that might keep them from attending or successfully completing LCPs. The Alliance also partners with community agencies who could provide resources for social barriers such as food, transportation, childcare, or broadband internet for program participants.
Sustainability of the collaborations and systems of the Alliance will help extend its positive impact. In planning for implementation beyond the initial 5-year project funded by the CDC [15], it was critical to systematically assess factors impacting the program’s sustainability capacity and develop a sustainability plan with actionable strategies. The purpose of this article is to present results of a mixed-methods, partner-engaged approach to identify barriers and facilitators to sustainability and develop a sustainability plan for the Alliance program.
2. Materials and Methods
This project used a parallel convergent mixed-methods approach that simultaneously collected quantitative survey data and qualitative interview data to provide a holistic understanding of sustainability of the Alliance program [16]. This understanding was used to co-develop a sustainability plan. This study was approved by the Institutional Review Board at Washington University in St. Louis, IRB # 202207142.
2.1. Quantitative Data Collection and Analysis
A survey was distributed electronically via REDCap to all Alliance partners (Table 1) including community health workers, clinicians, community resource coordinators (termed “frontline workers” for this paper), organization managers, program leadership, and funders (N = 74). After the original invitation email, we sent two subsequent reminders in weeks two and three. Participants were offered a USD 20 gift card to a local grocery store as an incentive. There were two main components to the survey: (1) assessment of sustainability capacity based on the 8 domains in the Program Sustainability Framework [2]; and (2) assessment of the inner-organizational factors using validated survey items from the Consolidated Framework for Implementation Research (CFIR) [17].

Table 1.
Alliance partners.
The Program Sustainability Framework identifies a set of organizational and contextual domains that help build the capacity for maintaining a program. Sustainability capacity is defined as the ability to maintain programming and its benefits over time. To improve this capacity, it is important to strengthen structures and processes that exist within the program. The first step is to build an understanding of the factors that impact the sustainability capacity of a program using the eight key domains: environmental support, funding stability, partnerships, organizational capacity, program evaluation, program adaptation, communication, and strategic planning [2]. The Program Sustainability Assessment Tool (PSAT) was used to collect quantitative data across the eight domains [2]. The PSAT has established reliability for public health programs and has been applied to a variety of public health programs, such as tobacco control, community health, and healthcare programs [18,19,20]. PSAT questions used a 7-point Likert Scale to assess the extent to which each respondent and organization agreed with a series of statements. Scores of 7 indicate agreeing “to a very great extent”, while scores of 1 indicate agreeing “little to no extent”. Responses of 8, indicating “I don’t know/unsure”, were coded as missing and removed prior to quantitative analysis.
The CFIR is a conceptual framework that was developed to guide the systematic assessment of multi-level contextual factors that may influence the implementation and effectiveness of an intervention or program [21,22]. CFIR assesses barriers and facilitators at five levels: intervention characteristics, outer setting, inner setting, characteristics of individuals, and process of implementation. This study uses a CFIR-derived, validated, and reliable survey, developed by Fernandez and colleagues (2018), to measure inner-organizational factors that may impact implementation and sustainability [17]. While the PSAT includes organizational capacity, we used this CFIR-derived measure to further understand three inner-setting factors (implementation climate, culture stress, and available resources) that may be particularly relevant to the sustainability of the Alliance. CFIR questions were asked on a 5-point Likert Scale (1 = strongly disagree to 5 = strongly agree) to assess the extent of agreement with a series of statements about the respondent’s organizational climate, culture stress, and resources. Higher scores indicate a more positive implementation environment, with culture stress reverse-coded.
Survey results were analyzed using Microsoft Excel using published methods [2]. We calculated means for each item. Domain means were generated by averaging item scores for each of the PSAT and CFIR domains. Items within each domain were bolded if they scored below the domain mean to indicate potential areas for improvement. An overall sustainability score was generated by averaging the 8 PSAT domain scores. Scores were also calculated for each organization by averaging item scores for each respondent within an organization and averaging within each domain. Standard deviations were calculated to show variability within and across organizations.
2.2. Qualitative Data Collection and Analysis
We developed interview questions to expand on the PSAT’s eight critical sustainability domains to assess the perception of maintaining the networks and systems developed through the Alliance program beyond the funded grant period. The evaluation team created a general interview guide with a core set of questions, and then added questions tailored for the roles of frontline workers and managers/leaders. We pilot-tested the interview questions internally and with one Alliance partner. No substantive changes to the interview guides were made.
The research team conducted interviews via Zoom video conference. Participants were offered a USD 20 gift card to a local grocery store for participating. The conversations were audio-recorded and transcribed verbatim. After an initial reading of all transcripts, two team members developed a coding tool which was then tested on two transcripts and finalized. Two team members independently coded each transcript and met to ensure inter-rater reliability and address reflexivity in their qualitative interpretation. In these meetings, inconsistencies were reviewed, discussed, and rectified. Coded text was summarized into themes based on PSAT domains. Interview results were presented in our Alliance monthly Zoom meeting with all partners to ensure our analysis and summary accurately captured their perspectives.
2.3. Partner-Engaged Sustainability Action Planning
To generate a sustainability action plan, we conducted a modified version of an evidence-based sustainability action planning process shown to improve sustainability capacity in the eight PSAT domains [23]. To prepare the team, quantitative and qualitative results were presented to Alliance partners during a team meeting and a summary was shared to all partners. Following this presentation, all partners were invited to attend a 3 h interactive in-person session to write our sustainability plan. This session focused on deciding what to sustain, choosing which domains were most important and feasible to address, and writing objectives and clear steps. The group also discussed how the plan would be implemented, monitored, and reassessed.
3. Results
A total of 17 (9 frontline workers and 8 managers) of the 74 Alliance partners (23%) participated in a survey about the sustainability of the program. Respondents represented seven (78%) of the partner agencies of Alliance. We asked survey respondents (n = 17) if they would be willing to participate in a one-on-one interview with a member of the Alliance evaluation team. A total of 11 expressed interest and agreed to participate in an interview, with 9 (4 frontline workers and 5 managers) completing the interview process within our timeframe. The interviews lasted an average of 21 min. Quantitative and qualitative PSAT results are presented below by domain in descending order of the average score and in Table 2. The communication domain does not have quantitative results, due to an error in REDCap during data collection that generated unusable data. CFIR survey results are summarized below and presented in Table 3.

Table 2.
Program Sustainability Assessment Tool (PSAT) survey results and qualitative quotes.
3.1. Program Sustainability Assessment Tool (PSAT) Results
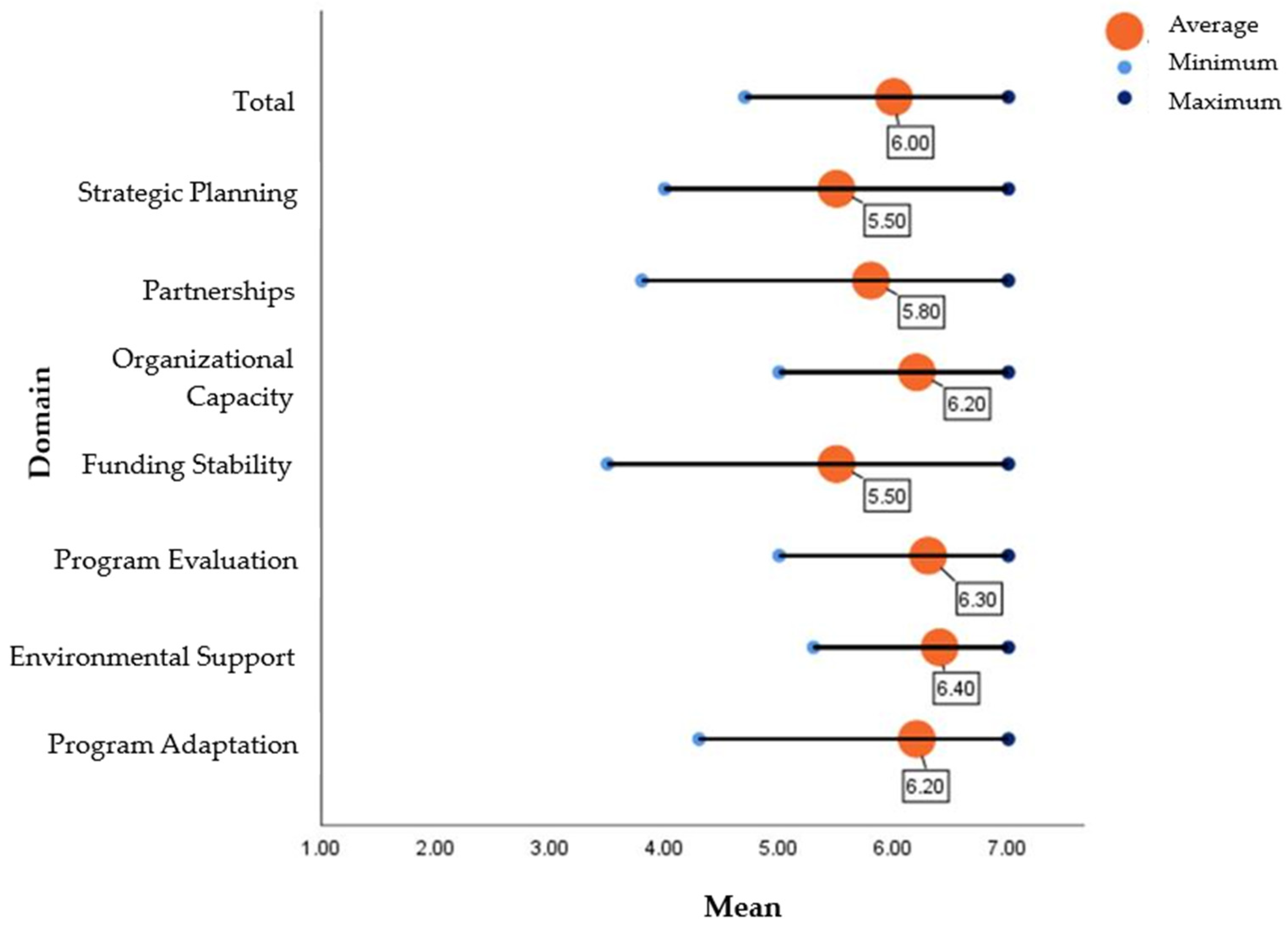
The PSAT survey results indicated an overall mean score of 6.0 (range: 4.7 to 7.0) for capacity for sustainability based on the 7-point Likert Scale (Table 2, Figure 1). Both managers and frontline staff seemed positive about the potential for sustaining existing work with the Alliance. They noted the long journey of establishing the existing systems of organizational collaboration and support to connect patients into evidence-based disease prevention and management programs. The Alliance frontline staff most often cited the benefits to the community as the reason it should continue. They noted the importance of providing ways to improve health and well-being in places where health inequities exist, and community stakeholder investment.
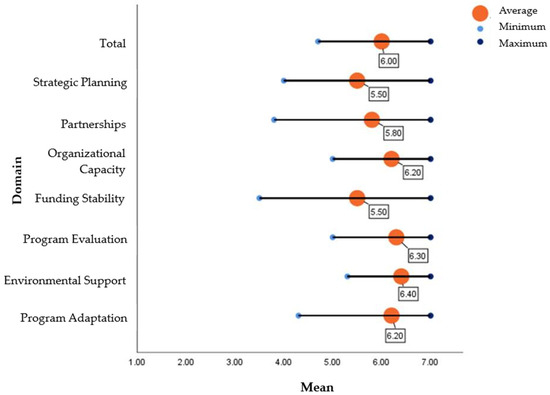
Figure 1.
Average sustainability scores by domain.
3.1.1. Environmental Support
Environmental support was the highest ranked domain (mean = 6.4). The item “The Alliance has strong champions with the ability to garner resources” fell slightly below the domain mean (6.2). Having a supportive internal and external climate for the Alliance work is vital to sustainability. One related issue that emerged qualitatively in both frontline staff and managers was the impact of the COVID-19 pandemic. The Alliance brought organizations together, but the COVID pandemic weakened the collaborations and caused a setback in progress. Despite the setbacks, one manager noted the patience that partners had throughout the process of keeping Alliance work going during this time.
3.1.2. Program Evaluation
The mean score for program evaluation was 6.3, with no items scoring below the mean. The importance of using data for the Alliance and its sustainability was noted yet was also perceived as under-appreciated for its contribution by partners. The assessment of social determinants of health was acknowledged by managers as a challenge for frontline workers but necessary to demonstrate the success of the Alliance. One manager mentioned that quarterly meeting updates should include more qualitative data or success stories to get partners engaged in evaluation.
3.1.3. Organizational Capacity
Internal support and resources are needed to effectively manage and sustain programs. This domain scored relatively high with a mean score of 6.2. The item that scored below the mean was the “organization has adequate staff to complete the Alliance goals” (5.8). Qualitatively, it was noted that to achieve Alliance goals and utilize the consistent systems and practices of the Alliance, additional frontline staff are needed. Even when managers were positive about the sustainability of Alliance, they mentioned the silos in which organizations work. Without prioritization and buy-in within these organizations, Alliance activities might be difficult to maintain. Less tangible resources such as capacity for and enthusiasm for the Alliance were mentioned. Regrouping after COVID took time and some momentum was lost. Re-establishing the energy that existed early on may help Alliance in the future. Relatedly, the lack of consistent systems (e.g., electronic health records or social service resource locators) is a significant barrier to collective Alliance work. This was not only noted about referrals into programs, but also for the differences in assessing and addressing social determinants of health which is core to Alliance work.
3.1.4. Program Adaptation
Program adaptation scored high with a mean of 6.2. Items that scored below the mean were “the Alliance adapted to new science” (6.1) and “the Alliance makes decisions about which components are ineffective and should not continue” (6.0). The interview participants talked about the importance of Alliance adaptability and flexibility. All of those interviewed mentioned how the COVID-19 pandemic resulted in adaptations to the Alliance program. Managers mentioned that the move to virtual programs facilitated an acceptance of telehealth, which was a strong benefit to the communities and Alliance as a whole. However, they noted that the pandemic hampered frontline workers’ ability to refer patients due to competing priorities and reduced interactions with the community.
Partners also suggested that Alliance could adapt to better connect with other organizations that provide social services in future efforts. They also mentioned immense needs in the communities they serve, some of which Alliance tries to address and others which were outside of the scope of the project. A broader need for both transportation and food support was noted by several staff and noted as essential for success in disease prevention and management programs. Several frontline staff also talked about mental health needs, especially in the post-COVID era. Several mentioned the need for addressing basic social needs in addition to other Alliance work, especially since many of the people in the program’s target population lack basic tools that would help them be more successful in an LCP.
3.1.5. Partnerships
Partnerships had a mean score of 5.8. Two items scored below the mean: “the Alliance communicates with community leaders” (5.5) and “community leaders are involved with the Alliance” (5.5). This was supported qualitatively as partners felt the Alliance has many internal and external partners, and these partnerships were described as a benefit to the program by all participants. Managers who were interviewed perceived the development and continuation of collaborations and partnerships as crucial to current and future Alliance efforts. The partnerships among public health, healthcare centers, pharmacies, and community resource providers are key to community health impact. They saw Alliance partnerships as key to making a collective impact in their communities, while acknowledging the differences in the ways each organization does this. Frontline staff also talked about the strength in efforts when working collectively and appreciated that Alliance connected them together. There was a common recommendation for the future of Alliance to broaden partnerships within the community. Other community organizations that provide resources, especially food resources, would be helpful in broadening the scope and reach of Alliance.
3.1.6. Strategic Planning
Strategic planning scored 5.5. Items that were indicated as areas for improvement were “the Alliance has a long-term financial plan” (5.3) and “the Alliance’s goals are understood by all partners” (5.0). Qualitative interviews highlighted the need for internal communication that may impact program effectiveness and help build and maintain buy-in with stakeholders. Both managers and frontline workers perceived the need for better ways for the group to communicate within Alliance. More in-person meetings (versus videoconference) were suggested.
3.1.7. Funding Stability
Funding stability (5.5) was among the domains that ranked lowest. Qualitatively, partners expressed that a core component of sustainability is establishing a consistent and reliable financial base for programming. Both frontline staff and managers noted concerns about the continued efforts of Alliance without dedicated grant funds. They noted fears that regardless of how good the work is, it may be difficult to keep the group together without the grant funding. Several participants mentioned that some frontline worker positions are funded by the project, so securing these jobs is integral to sustained Alliance success.
3.1.8. Communication
Participants presented an understanding that external communications build greater visibility and support from stakeholders in the community. Frontline staff are well integrated into the communities in which they serve and mentioned many ways they reach out to find people who could be referred into the Alliance disease prevention and management programs. They noted the need for more outward-facing communication to help in informing communities about the great work that Alliance does, as well as to recruit other organizations that can help meet the needs of our communities to join the Alliance.
3.2. Consolidated Framework for Implementation Research (CFIR) Inner-Setting Results
The Implementation Climate, which is the shared receptivity and extent to which the program will be rewarded, supported, and expected within an organization, scored highest with a mean of 4.3 (Table 3). Two items that scored below the mean were “organization staff get the support they need to improve enrollment and retention in behavior support programs and primary medical care” (4.1) and “Increasing enrollment and retention in behavior support programs and primary medical care is a top priority of the organization” (4.2; Table 3). Available resources scored 4.1, with budget or financial resources (3.8) and patient awareness/need (4.0) as identified areas that are lacking. Culture stress—which was reverse-coded—scored lowest with a mean of 3.8. The lowest item mean in this domain was 3.6 for “staff members often show signs of stress and strain”, followed by “the heavy workload here reduces program effectiveness”, (3.8) and “staff frustration is common here” (3.8; Table 3).

Table 3.
Inner-organizational factors using the Consolidated Framework for Implementation Research.
Table 3.
Inner-organizational factors using the Consolidated Framework for Implementation Research.
| Domain (Definition) | Domain Mean (SD) | Items | Item Mean (SD) |
|---|---|---|---|
| Implementation climate (Shared receptivity and the extent to which the program will be rewarded, supported, and expected within their organization.) | 4.3 (0.5) | Our organization staff are expected to help the Alliance meet its goal (improve enrollment and retention in behavior support programs and/or primary medical care) | 4.4 (0.5) |
| Organization staff get the support they need to improve enrollment and retention in behavior support programs and primary medical care | 4.1 (1.0) | ||
| Organization staff gets recognition for participating in the Alliance. | 4.4 (0.6) | ||
| Increasing enrollment and retention in behavior support programs and primary medical care is a top priority of the organization. | 4.2 (0.8) | ||
| Available resources (Resources dedicated for implementing the program and ongoing operations-e.g., money, training, space, time) | 4.1 (0.3) | In general, when there is agreement that change needs to happen we have the necessary support in terms of: | |
| budget or financial resources | 3.8 (0.7) | ||
| training | 4.3 (0.7) | ||
| staffing | 4.1 (0.7) | ||
| The following are available to make Alliance work in our organization: | |||
| equipment and materials | 4.2 (0.6) | ||
| patient awareness/need | 4.0 (0.8) | ||
| frontline buy-in | 4.1 (0.9) | ||
| Culture stress (Perceived stain, stress and role overload) | 3.8 (0.2) | I am under too many pressures to do my job effectively | 4.1 (0.9) |
| Staff members often show signs of stress and strain | 3.6 (1.0) | ||
| The heavy workload here reduces program effectiveness | 3.8 (1.1) | ||
| Staff frustration is common here | 3.8 (1.0) |
All items are on a 5-point Likert Scale (strongly disagree to strongly agree). Higher scores indicate a more positive implementation environment, with culture stress reverse-coded. Bolded items indicate those that scored below the domain mean, indicating areas for developing capacity.
3.3. Sustainability Plan Results
Twelve partners attended the action planning meeting and collectively prioritized PSAT domains by importance and feasibility. Funding stability ranked highest in importance, followed by partnerships and communication. Strategic planning, program adaptation, and program evaluation were rated highest for feasibility. The Alliance partners modified the mission, vision, and values of the Alliance to make it clear what was being sustained and generated objectives and activities for the next year (Supplementary Materials). Partnerships, communication, and strategic planning were selected as the three areas of focus for the next year. The team identified what success would look like for each activity (i.e., how it would be monitored), who would be responsible for completing the activity, and when it would be completed. The group also discussed the ongoing nature of this document and how the team may build on this beyond the one-year period.
4. Discussion
As part of a broader evaluation of the Alliance program, we used quantitative surveys and qualitative interviews to evaluate sustainability capacity. These data informed the development of a partner-driven sustainability action plan that will increase the likelihood that the Alliance program continues to make an impact on health disparities in St. Louis. Over the project period, the Alliance program engaged with close to 10,000 St. Louis residents making 1715 referrals to LCPs. About half (52%) of those individuals referred lived in the Promise Zone, a low-resourced, impoverished area. Of those referred, 796 were eligible and enrolled in an LCP. Overall, partners felt that the program has a high capacity for sustaining this network of referral and support into LCPs. Maintaining and expanding partnerships, strategic planning, and communication were areas where partners chose to focus on to enhance program sustainability. Activities that expand partnerships may address inner-organization weakness (Table 3) by increasing resource availability and staff. Communication activities are intended to increase awareness and buy-in among community leaders and patients who may benefit from LCPs. Despite some inner-organizational weaknesses, partners felt that there are strong champions and environmental support, evaluation, and organizational leadership capacity for the Alliance program.
The foundation of the Alliance program is partnerships across healthcare, public health, and community organizations. Partners noted the strength of the collective and multidisciplinary work of the Alliance, which is necessary to generate an impact on chronic disease prevention among the most vulnerable populations to reduce health disparities [24,25]. Yet, the expansion of partnerships was included within the sustainability action plan to improve their capacity to adapt to and meet the unique needs of the community (e.g., include organizations offering mental health resources). Partners identified a need for external communication of our programming to further partnerships and awareness among the community. Managers and frontline staff felt they needed more community resources to adequately and equitably address the needs of community members to reduce health disparities. Furthermore, the level of involvement of community leaders and community members was noted as a weakness of the Alliance. Specifically, involving the community in co-developing the program’s goals and sustainability plans from the start was lacking, yet may generate greater buy-in that partners felt was needed. Our partners noted that concerted efforts to build relationships, infrastructure, and systems that fit within the structures and workflows of all partners is necessary to achieve our program’s goals. While there is an abundance of support for partnerships and rhetoric on their advantages in the literature, there is a lack of an evidence base for what makes a good partnership [26]. Future evaluation of the Alliance may consider iterative evaluation of the strength of the Alliance partnership to iteratively monitor and improve this domain.
As indicated in the Program Sustainability Framework, a variety of funding sources improves sustainability [2]. The Alliance Program was funded by a single five-year grant, which was a substantial concern of the partners. While partners felt hopeful that the Alliance has strong champions with the ability to garner resources, they noted a lack of a long-term financial plan. While specific plans for addressing funding stability were not included in the action plan, the team continues to discuss and apply for various opportunities for funding. Communication to external community leaders and the public was prioritized by partners and may support fund-raising or lead to other supports to increase financial stability. The lack of financial support may be most critical for sustaining the frontline workers within each organization and allocating their time to the goals of the Alliance, two areas identified as lacking within the inner-organizational context. Implementation climate describes inner-organizational factors, such as supporting and prioritizing efforts to engage in and improve lifestyle change program efforts, which have been previously found to be related to local public health efforts to engage in equity-oriented chronic disease prevention [27]. The sustainability scores in the current study indicate that this may be another area for participating organizations to examine ways that internal systems and practices could reduce financial costs of the program and further bolster sustainability.
Strategic planning includes internal communication as well as using processes that guide your program’s directions, goals, and strategies [2]. While partners felt that the evaluation results informed program planning and implementation, they also noted that the program may benefit from more data-driven, strategic decisions about which program components to continue, not continue, or adapt. The Alliance used an iterative evaluation approach. It was noted that the monthly partner reports and sharing of successes and barriers during Alliance partner meetings were critical, in conjunction with the quantitative quarterly evaluation data (e.g., number of referrals made to lifestyle change programs). Partners felt that more opportunities for using qualitative data in the evaluation would improve the ability of the program to adapt as needed. Yet, using these data to inform decisions about the program may not have been transparent or inclusive of all partners. Being intentional about and using established frameworks (such as FRAME) [28] to track program adaptations are critical to sustaining a program. To build capacity for strategic planning, partners felt that it was critical to clarify the program’s goals and each partner’s roles and to develop committees that would focus on sustaining different aspects of the program.
A major strength of our study was the mixed-methods application of the PSAT to understand and assess the sustainability of a complex community network for chronic disease prevention [17]. This study contributes to the literature as few studies have applied mixed methods to understand sustainability capacity and used results to develop an action plan with partners. One known study used open-ended survey questions to gather qualitative data [17], but did not conduct in-depth interviews which allowed us to ask follow-up questions that increase understanding. This study expands PSAT’s organizational capacity domain, using a CFIR-derived measure that examines three inner-setting factors (implementation climate, culture stress, and available resources) that may be particularly relevant to sustainability. While this study comprehensively assessed sustainability, the response rate (23%) for the quantitative survey was low and, therefore, may not fully reflect the perspectives of all partners in the Alliance. This may have generated results that were not as meaningful for sustainability action planning. However, survey respondents did represent all the main Alliance organizations and included an almost equal number of frontline workers and managers/program leadership. Furthermore, partners had additional opportunities to provide their perspectives during Alliance monthly meetings in which results were presented and during discussion at the action planning session. The action planning sessions allowed partners to reach a consensus regarding which domains and specific areas were most critical to address. While we present data for all eight PSAT domains, quantitative survey results were not presented for the communication domain, which limits our ability to compare this domain to others. However, qualitative insights provided a clear need for improved internal and external communication. This was further supported by results in the partnership domain that indicated a need to communicate with community leaders and the strategic planning domain which indicated that, internally, not all alliance partners understand the goals of the program.
5. Conclusions
Understanding what factors are critical for sustaining effective programs and processes for developing action plans to build sustainability capacity is critical to maximizing community health impact and reducing health disparities. Therefore, understanding and planning for sustainability are of interest to researchers, practitioners, and funders [2,5]. Using established frameworks and evidence-based tools to characterize sustainability allows programs to develop structures and processes to leverage resources effectively to sustain effective program activities and systems. Furthermore, this process allows programs to act more efficiently and improve their ability to maintain efforts over the long-term. While the Sustainability Framework highlights critical domains for sustainability, the factors that are necessary and sufficient to ensure sustainability likely differ for intervention types and contexts [3,29]. Using a mixed-methods approach to examine barriers and facilitators of sustaining a complex community network for chronic disease prevention may further our understanding of factors critical for the sustainability of public health programs for chronic disease prevention and health equity.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph21040463/s1, The St. Louis Alliance Sustainability Plan.
Author Contributions
Conceptualization, M.M.K., A.D. and A.A.E.; methodology, M.M.K. and A.A.E.; formal analysis, M.M.K., K.A.S., A.D., A.T., A.A.E. and L.A.; data curation, M.M.K.; writing—original draft preparation, M.M.K., A.D. and A.A.E.; writing—review and editing, M.M.K., A.A.E., A.D., K.A.S., A.T., E.G., A.H., C.S.F., G.C. and L.A.; supervision, M.M.K. and A.A.E.; funding acquisition, A.A.E. and A.H.; project administration, E.G., A.H., C.S.F. and G.C. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the Prevention Research Center at Washington University in St. Louis (no. U48DP006395) and CDC 1817 grant no. HE2021-0202.
Institutional Review Board Statement
This study was approved by the Institutional Review Board at Washington University in St. Louis, IRB # 202207142.
Informed Consent Statement
Consent was waived as no personal identifying information was collected.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available, due to privacy concerns for participating Alliance partners.
Acknowledgments
We acknowledge the contribution of all Alliance partners who contributed to the implementation and evaluation of this project: the Missouri Department of Health and Senior Services, the St. Louis County Department of Public Health, the City of St. Louis Department of Health, the Integrated Health Network, the Missouri Primary Care Association, the Missouri Pharmacy Association, the Fit and Food Connection, and the Gateway Region YMCA.
Conflicts of Interest
The authors declare no conflicts of interest. G.C. founded and directs the Fit and Food Connection. C.S.F. is an employee of the Gateway Region YMCA.
References
- Brownson, R.C.; Fielding, J.E.; Green, L.W. Building Capacity for Evidence-Based Public Health: Reconciling the Pulls of Practice and the Push of Research. Annu. Rev. Public Health 2018, 39, 27–53. [Google Scholar] [CrossRef] [PubMed]
- Luke, D.A.; Calhoun, A.; Robichaux, C.B.; Elliott, M.B.; Moreland-Russell, S. The Program Sustainability Assessment Tool: A new instrument for public health programs. Prev. Chronic Dis. 2014, 11, 130184. [Google Scholar] [CrossRef] [PubMed]
- Scheirer, M.A. Is Sustainability Possible? A Review and Commentary on Empirical STUDIES of Program Sustainability. Am. J. Eval. 2005, 26, 320–347. [Google Scholar] [CrossRef]
- Vitale, R.; Blaine, T.; Zofkie, E.; Moreland-Russell, S.; Combs, T.; Brownson, R.C.; Luke, D.A. Developing an evidence-based program sustainability training curriculum: A group randomized, multi-phase approach. Implement. Sci. 2018, 13, 126. [Google Scholar] [CrossRef]
- Moreland-Russell, S.; Combs, T.; Polk, L.; Dexter, S. Assessment of the Sustainability Capacity of a Coordinated Approach to Chronic Disease Prevention. J. Public Health Manag. Pract. 2018, 24, E17–E24. [Google Scholar] [CrossRef]
- Bowen, F.R.; Epps, F.; Lowe, J.; Guilamo-Ramos, V. Restoring Trust in Research Among Historically Underrepresented Communities: A call to action for antiracism research in nursing. Nurs. Outlook 2022, 70, 5. [Google Scholar] [CrossRef]
- Bodkin, A.; Hakimi, S. Sustainable by design: A systematic review of factors for health promotion program sustainability. BMC Public Health 2020, 20, 964. [Google Scholar] [CrossRef]
- Calhoun, A.; Mainor, A.; Moreland-Russell, S.; Maier, R.C.; Brossart, L.; Luke, D.A. Using the Program Sustainability Assessment Tool to assess and plan for sustainability. Prev. Chronic Dis. 2014, 11, 130185. [Google Scholar] [CrossRef]
- Schell, S.F.; Luke, D.A.; Schooley, M.W.; Elliott, M.B.; Herbers, S.H.; Mueller, N.B.; Bunger, A.C. Public health program capacity for sustainability: A new framework. Implement. Sci. 2013, 8, 15. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. National Diabetes Prevention Program. 2022. Available online: https://www.cdc.gov/diabetes/prevention/index.html (accessed on 1 February 2024).
- US Census Bureau. Social. Explorer. 2012 American Community Survey 1-Year Estimates, Poverty Status in 2012; US Census Bureau: St. Louis, M, USA, 2012. Available online: http://www.socialexplorer.com/explore/tables (accessed on 1 February 2024).
- US Department of Housing and Urban Development. Promise Zones Overview 2022. Available online: https://www.hudexchange.info/programs/promise-zones/promise-zones-overview/ (accessed on 1 February 2024).
- Kepper, M.; Stamatakis, K.A.; Mudd, N.; Deitch, A.; Terhaar, A.; Liu, J.; Gates, E.; Williams, B.; Cole, G.; French, C.S.; et al. A Communitywide Collaboration to Increase Enrollment, Retention, and Success in Evidence-Based Lifestyle-Change Programs in Racial and Ethnic Minority Populations. Prev. Chronic Dis. 2023, 20, E67. [Google Scholar] [CrossRef]
- Shimbo, D.; Artinian, N.T.; Basile, J.N.; Krakoff, L.R.; Margolis, K.L.; Rakotz, M.K.; Wozniak, G.; On behalf of the American Heart Association and the American Medical Association; On behalf of the American Heart Association; the American Medical Association. Self-Measured Blood Pressure Monitoring at Home: A Joint Policy Statement From the American Heart Association and American Medical Association. Circulation 2020, 142, e42–e63. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. DP18-1817 | Diabetes | CDC. 2023. Available online: https://www.cdc.gov/diabetes/programs/stateandlocal/funded-programs/dp18-1817.html (accessed on 1 March 2024).
- Edmonds, W.A.; Kennedy, T.D. An Applied Guide to Research Designs: Quantitative, Qualitative, and Mixed Methods; SAGE Publications, Inc.: Thousand Oaks, CA, USA, 2017; Available online: https://methods.sagepub.com/book/an-applied-guide-to-research-designs-2e (accessed on 1 March 2024).
- Fernandez, M.E.; Walker, T.J.; Weiner, B.J.; Calo, W.A.; Liang, S.; Risendal, B.; Friedman, D.B.; Tu, S.P.; Williams, R.S.; Jacobs, S.; et al. Developing measures to assess constructs from the Inner Setting domain of the Consolidated Framework for Implementation Research. Implement. Sci. 2018, 13, 52. [Google Scholar] [CrossRef]
- Stoll, S.; Janevic, M.; Lara, M.; Ramos-Valencia, G.; Stephens, T.B.; Persky, V.; Uyeda, K.; Ohadike, Y.; Malveaux, F. A mixed-method application of the program sustainability assessment tool to evaluate the sustainability of 4 pediatric asthma care coordination programs. Prev. Chronic Dis. 2015, 12, E214. [Google Scholar] [CrossRef]
- Hunter, S.B.; Han, B.; Slaughter, M.E.; Godley, S.H.; Garner, B.R. Associations between implementation characteristics and evidence-based practice sustainment: A study of the Adolescent Community Reinforcement Approach. Implement. Sci. 2015, 10, 173. [Google Scholar] [CrossRef]
- Tabak, R.G.; Duggan, K.; Smith, C.; Aisaka, K.; Moreland-Russell, S.; Brownson, R.C. Assessing Capacity for Sustainability of Effective Programs and Policies in Local Health Departments. J. Public Health Manag. Pract. 2016, 22, 129–137. [Google Scholar] [CrossRef]
- Damschroder, L.J.; Reardon, C.M.; Widerquist, M.A.O.; Lowery, J. The updated Consolidated Framework for Implementation Research based on user feedback. Implement. Sci. 2022, 17, 75. [Google Scholar] [CrossRef]
- Damschroder, L.J.; Aron, D.C.; Keith, R.E.; Kirsh, S.R.; Alexander, J.A.; Lowery, J.C. Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implement. Sci. 2009, 4, 50. [Google Scholar] [CrossRef]
- Moreland-Russell, S.; Combs, T.; Gannon, J.; Jost, E.; Saliba, L.F.; Prewitt, K.; Luke, D.; Brownson, R.C. Action planning for building public health program sustainability: Results from a group-randomized trial. Implement. Sci. 2024, 19, 9. [Google Scholar] [CrossRef]
- Huang, J.; Xu, Y.; Cao, G.; He, Q.; Yu, P. Impact of multidisciplinary chronic disease collaboration management on self-management of hypertension patients: A cohort study. Medicine 2022, 101, e29797. [Google Scholar] [CrossRef]
- Funnell, M.M.; Brown, T.L.; Childs, B.P.; Haas, L.B.; Hosey, G.M.; Jensen, B.; Maryniuk, M.; Peyrot, M.; Piette, J.D.; Reader, D.; et al. National Standards for diabetes self-management education. Diabetes Care 2011, 34 (Suppl. S1), S89–S96. [Google Scholar] [CrossRef]
- Butt, G.; Markle-Reid, M.; Browne, G. Interprofessional partnerships in chronic illness care: A conceptual model for measuring partnership effectiveness. Int. J. Integr. Care 2008, 8, e08. [Google Scholar] [CrossRef]
- Stamatakis, K.A.; Baker, E.A.; McVay, A.; Keedy, H. Development of a measurement tool to assess local public health implementation climate and capacity for equity-oriented practice: Application to obesity prevention in a local public health system. PLoS ONE 2020, 15, e0237380. [Google Scholar] [CrossRef]
- Wiltsey Stirman, S.; Baumann, A.A.; Miller, C.J. The FRAME: An expanded framework for reporting adaptations and modifications to evidence-based interventions. Implement. Sci. 2019, 14, 58. [Google Scholar] [CrossRef]
- Scheirer, M.A. Linking sustainability research to intervention types. Am. J. Public Health 2013, 103, e73–e80. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).