Abstract
Background: The COVID-19 lockdown had a profound effect on everyday life, including sleep health. This systematic review and meta-analysis evaluated changes in quantitative sleep parameters during the first lockdown compared with pre-lockdown in the general population. Methods: A search in scientific databases was performed to identify eligible observational studies from inception to 8 February 2023. We performed a random effects meta-analysis of those studies reporting (a) means of sleep duration, time in bed (TIB), and sleep timing (bedtime and wake-up time); (b) the percentages of atypical sleep duration before and during the lockdown; (c) the percentages of change in sleep duration and sleep timing. Results: A total of 154 studies were included. A small increase in sleep duration (0.25 standardized mean difference, 95% CI 0.180–0.315) was found, with 55.0% of the individuals reporting changes, predominantly an increase (35.2%). The pooled relative risk for sleeping more than 8/9 h per night was 3.31 (95% IC 2.60–4.21). There was a moderately significant delay in sleep timing and a surge in napping. Conclusion: An increase in sleep duration and napping, and delayed sleep timing were observed. High-quality studies should evaluate whether these parameters have now become chronic or have returned to pre-lockdown values.
1. Introduction
The COVID-19 pandemic, caused by the SARS-CoV-2 virus, has brought about profound changes globally, impacting public health, society, economy, and daily life for billions. The rapid spread of cases prompted a global health emergency declaration by the World Health Organization (WHO) on 30 January 2020 [1]. Measures such as hand hygiene, face masks, isolation, quarantine, and lockdowns were implemented in order to limit the diffusion of the virus and to mitigate the burden on health systems, causing a drastic shift in social dynamics [2]. Physical distancing and isolation affected daily habits, including work schedules, exposure to natural light, and reduced physical exercise opportunities [3]. Stress levels rose due to fear of the unknown disease, health concerns, and economic repercussions [3]. Changes in routines disrupted daily rhythms and energy balance, affecting various biological clock regulators [4].
Specifically, considering the vulnerability of the sleep system to cognitive-physiological stress (also known as sleep reactivity), sleep health was significantly compromised during the COVID-19 lockdown [5]. In fact, it is known that ruminating on stressful factors can activate processes that disrupt sleep, and that sleeping difficulty during stressful periods promotes repetitive thinking as the inability to fall asleep creates an unstructured stressful period in bed [5]. Sleep disturbances can present in various forms, including insomnia, disrupted sleep, daytime symptoms such as involuntary drowsiness, difficulty falling or staying asleep, delayed bedtime, abnormal sleep behaviors, and nightmares [5]. According to several systematic reviews and meta-analyses, sleep disturbances were common in different segments of the population during the COVID-19 pandemic [6,7,8,9,10].
Our previous systematic review and meta-analysis found a worsened sleep quality and increased sleep disturbances in the general population during the COVID-19 lockdown compared with pre-lockdown levels [11]. The COVID-19 pandemic and confinement measures led to changes in other relevant sleep parameters, such as delayed bedtime and increased sleep duration in the general population [12,13,14]. This pattern has been confirmed by two systematic reviews and meta-analyses evaluating the impact of the COVID-19 pandemic on sleep health [15,16]. Al-Ajlouni reported a negative impact on sleep with an increase in the prevalence of short or long sleep duration among different populations residing in the Middle East and North Africa (MENA) [15]. Cui’s systematic review and meta-analysis uncovered an increase in sleep duration among healthy adults during the COVID-19 lockdown [16]. However, both works have limitations: the former focused exclusively on the MENA region, limiting its generalizability [15], while the latter included only six studies that evaluated changes in sleep duration [16]. Moreover, there are no systematic reviews that investigated changes in other sleep dimensions, such as napping habits and atypical sleep duration.
The current systematic review and meta-analysis aims to overcome these limitations by providing a more comprehensive understanding of the changes in several quantitative sleep parameters during the first COVID-19 lockdown in the general population. We chose to concentrate on the first lockdown period, as investigations conducted thereafter may have been susceptible to the mitigation of restrictions, potentially resulting in varied effects on people’s sleep patterns. In particular, we evaluated changes in sleep duration, time in bed (TIB), sleep timing (bedtime and wake-up time), and napping habits during versus before the first COVID-19 lockdown.
2. Materials and Methods
This systematic review and meta-analysis was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [17], and it was registered in PROSPERO, CRD42021256378.
2.1. Search Strategy and Selection Criteria
We systematically searched four academic electronic databases (PubMed, Cochrane Library, Ebsco, and Web of Science-WOS), a preprint server (MedRxiv), and a gray literature database (OpenGrey) from inception to 28 May 2021; an updated search through 8 February 2023 was also carried out (PubMed and WOS). The full search strategy and the search terms used for each database are described in Appendix A (Table A1). The reference lists of relevant systematic reviews and articles were manually searched for additional studies. All the references were downloaded into Zotero, and this citation manager software was used for every stage of the selection process, from downloading and removing duplicates to screening the abstract titles and the full-texts. The abstract titles and full-texts were screened independently by three authors (E.P., F.R., and F.L.). Any disagreements were solved by consulting the senior authors (S.M., C.T., F.P., and M.N.).
2.2. Inclusion and Exclusion Criteria
Original observational cross-sectional or longitudinal studies that assessed changes in sleep characteristics (using self-reported or objective measures) during the first COVID-19 lockdown (hereafter lockdown) compared with before the lockdown (hereafter before) in the general adult population (adults ≥ 18 years) were considered eligible for inclusion.
Studies were excluded if they: (1) were not observational; (2) were reported in languages other than English, Italian, or Spanish; (3) evaluated changes only in subjects with specific diseases (e.g., obesity, diabetes, neuromuscular disease, cancer, osteoarthritis, and dementia) or in specific groups of individuals (e.g., healthcare workers, professional athletes); (4) collected data outside the timeframe of the first lockdown.
2.3. Outcomes
The current work is the continuum of a previous systematic review and meta-analysis on sleep quality and sleep disturbances in the general population from before to during the COVID-19 lockdown [11].
In particular, this study focuses on changes in the following quantitative sleep parameters:
- Sleep duration, i.e., the amount of time that a person sleeps;
- Sleep timing, which refers to bedtime, the time the person goes to bed, and wake-up time, the time the person awakes in the morning;
- The total duration spent in bed, namely TIB, encompassing both the time dedicated to sleep and any additional time spent lying in bed, whether awake or in a state of rest;
- Napping habits that refer to the sleep time beyond the main sleep period (percentage of participants tacking nap, length, and frequency).
2.4. Data Extraction
Data were extracted by four authors (F.R., E.P., F.L., and P.S.) using a pre-designed Excel spreadsheet. For each included study, the following information was recorded: first author’s name, year of publication, country, study design, assessment period, outcome, population, sample size, percentage of women, participants’ age (mean, median, or interval/age range), data collection method, type of recruitment, and type of measures utilized. The corresponding author was contacted whenever any study appeared incomplete or needed clarification on the presented data.
2.5. Risk of Bias Assessment
The Newcastle Ottawa Scale (NOS) for longitudinal [18] and cross-sectional studies [19] was used by two independent authors (F.R. and E.P.) to evaluate the risk of bias. The NOS allows one to judge a study based on three aspects: the selection of the study groups, the comparability of the groups, and the ascertainment of the outcome of interest. Cross-sectional studies can achieve a score of 0–10, and longitudinal studies can achieve a score of 0–9, with higher scores corresponding to a lower risk of bias. Studies whose NOS < 5 are classified as having a low quality and a high risk of bias [20]. A third author (M.N.) was involved in resolving any discrepancies.
2.6. Data Analysis
A meta-analysis was performed for data on outcomes that were sufficiently homogenous in terms of statistical and methodological characteristics. Additionally, a qualitative synthesis was performed to synthesize the findings of the studies that were not included in the meta-analysis. A random-effects meta-analysis was carried out for the sleep duration, TIB, and sleep timing (bedtime and wake-up time) outcomes, using the DerSimonian and Laird method; the studies were weighted according to the inverse of the standard error using the MedCalc Statistical Software version 20.118 [21].
Studies reporting the following data were included in the meta-analysis:
- Mean sleep duration, TIB, and sleep timing before and during the lockdown;
- The percentages of change in sleep duration (increased, decreased, no change) or in bedtime, and wake-up time (delayed, earlier, no change) during the lockdown vs. before; the percentage of atypical sleep duration (short sleep duration < 7 h/night and long sleep duration > 8 h/night) before and during the lockdown.
For each data type, the effect was expressed as a standardized mean difference (SMD)—this effect was interpreted using Cohen J. 1988 as 0.2 < small < 0.5, 0.5 ≤ medium < 0.8, large ≥ 0.8 [22], proportions, or relative risks. The between-study heterogeneity was analyzed using the I² statistic, where a value of 0% indicates no observed heterogeneity, and higher values show increasing heterogeneity [23]. The publication bias was assessed using Egger’s test [24], and, in case of possible bias (Egger’s p ≤ 0.05), we conducted one-study-removed sensitivity analyses.
2.7. Subgroup Analysis
Whenever possible, we stratified the meta-analysis by the risk of bias (NOS < 5 vs. NOS ≥ 5) and by country’s area. Countries were grouped into 7 areas: North America (Canada, USA), South America (Argentina, Brazil, Mexico, Peru), Central Asia (Bangladesh, India, Malaysia, Nepal, Pakistan), East Asia (China, Japan, Singapore), West Asia (Iran, Jordan, Kuwait, Lebanon, Saudi Arabia, United Arab Emirates), Europe (France, Germany, Hungary, Netherlands, Poland, Romania, UK), Mediterranean Europe (Cyprus, Greece, Italy, Portugal, Spain, Catalonia, Turkey). T-test and Chi-squared tests were used to compare subgroups.
3. Results
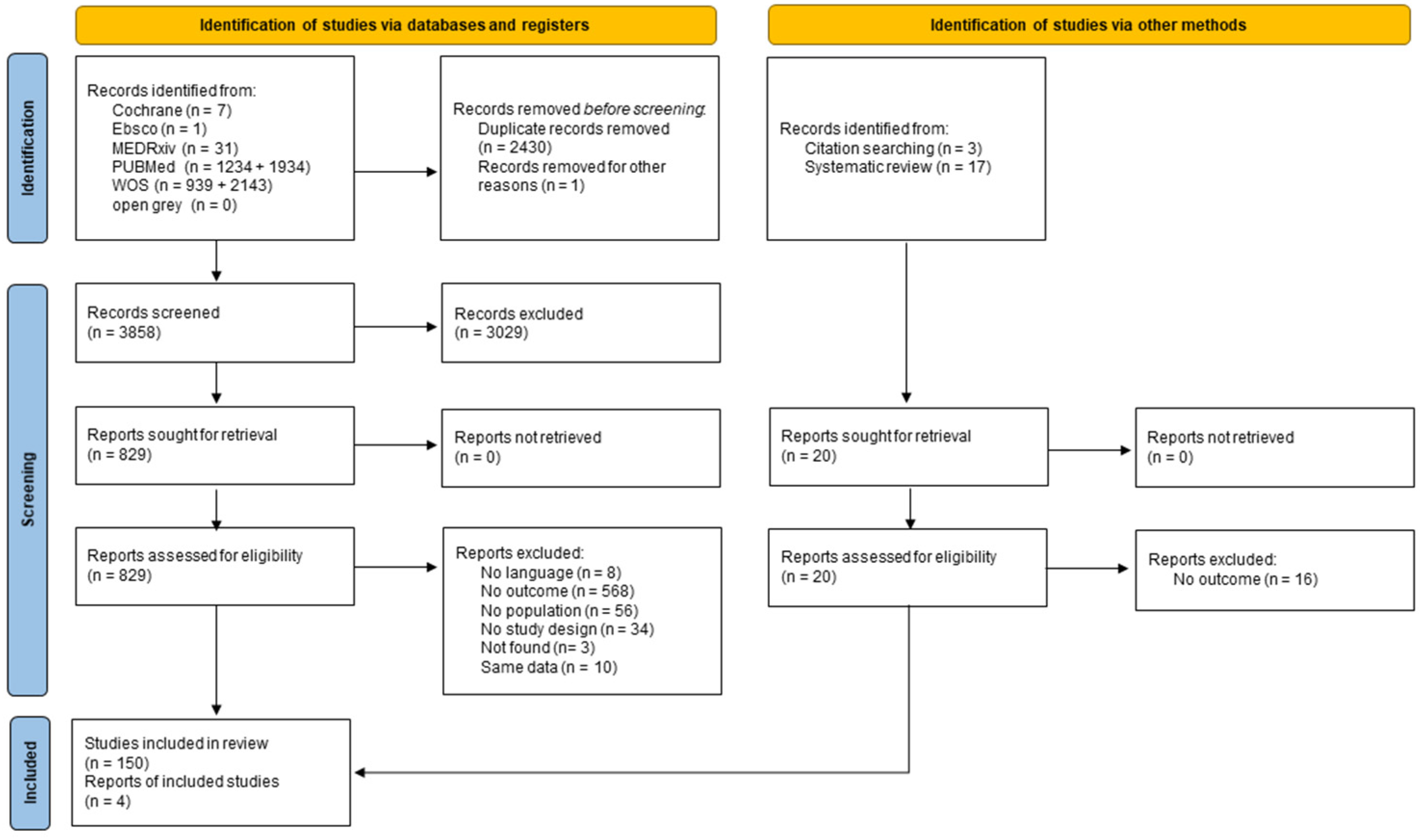
Overall, 6289 records were retrieved via databases and registers and 20 additional studies were identified via citation searches and systematic reviews. After the two-steps screening process, a total of 154 records were included (for the PRISMA flow diagram, please see Figure 1). The characteristics of the included studies are shown in Table 1 [25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140,141,142,143,144,145,146,147,148,149,150,151,152,153,154,155,156,157,158,159,160,161,162,163,164,165,166,167,168,169,170,171,172,173,174,175,176,177,178]. Studies were conducted in Argentina (N = 3), Australia (N = 3), Austria (N = 1), Bangladesh (N = 2), Brazil (N = 4), Canada (N = 2), China (N = 6), Colombia (N = 1), Croatia (N = 2), Cyprus (N = 1), Egypt (N = 1), France (N = 6), Germany (N = 2), Greece (N = 4), Hungary (N = 1), India (N = 8), Iran (N = 2), Italy (N = 14), Japan (N = 2), Jordan (N = 2), Kuwait (N = 1), Lebanon (N = 1), Libya (N = 1), Malaysia (N = 1), Mexico (N = 6), Morocco (N = 1), Nepal (N = 1), Netherlands (N = 1), New Zealand (N = 1), Pakistan (N = 3), Peru (N = 1), Poland (N = 4), Portugal (N = 1), Romania (N = 1), Russia (N = 2), Saudi Arabia (N = 5), Singapore (N = 2), South Africa (N = 1), Spain (N = 15), Turkey (N = 1), UK (N = 9), Ukraine (N = 1), United Arab Emirates (N = 2), USA (N = 13), and 12 were carried out in multiple countries. Due to the lockdown, most studies collected data via online surveys. One hundred and forty-five studies used self-reported instruments [25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,53,54,55,56,57,58,59,60,61,62,63,64,65,66,68,90,91,92,93,94,95,96,97,98,99,100,101,102,104,105,106,107,109,110,111,112,113,114,115,116,117,118,119,120,121,123,124,125,127,129,130,131,132,133,134,135,136,137,138,139,140,141,142,143,144,145,147,148,149,150,151,152,153,154,155,156,157,158,159,160,161,162,163,164,165,166,167,168,169,170,171,172,173,174,175,176,177,178]; seven studies used objective measures [67,69,103,108,122,128,146]; and two studies used both [52,126]. One hundred and thirty studies were cross-sectional, whereas twenty-four were longitudinal.
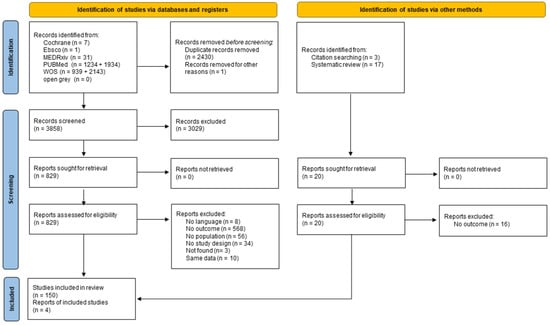
Figure 1.
PRISMA flow diagram of study selection.

Table 1.
Descriptive characteristics of the studies included.
The mean NOS score for the cross-sectional studies was 4.4 (SD = 1.3; range 2−8), and it was 6.2 (SD = 1.3; range 3−9) for the longitudinal ones (Appendix A Table A2). Overall, 53.9% had a good quality and had a low risk of bias (NOS ≥ 5), representing 96% of the longitudinal and 46% of the cross-sectional studies.
3.1. Sleep Duration
Among the 132 studies that examined sleep duration, 107 were included in the meta-analysis, and 25 were narratively described [25,48,55,75,80,87,88,102,104,106,108,113,123,126,128,132,141,144,145,156,159,162,163,169,171].
3.1.1. Meta-Analytic Changes in Sleep Duration: Means before and during the Lockdown
The changes in sleep duration were evaluated considering 69 outcomes reported in 44 studies [27,32,39,40,44,45,46,49,50,51,52,57,63,66,68,70,74,81,85,93,95,97,103,107,111,112,114,115,119,120,122,129,130,136,137,143,146,153,160,161,173,176,177,178].
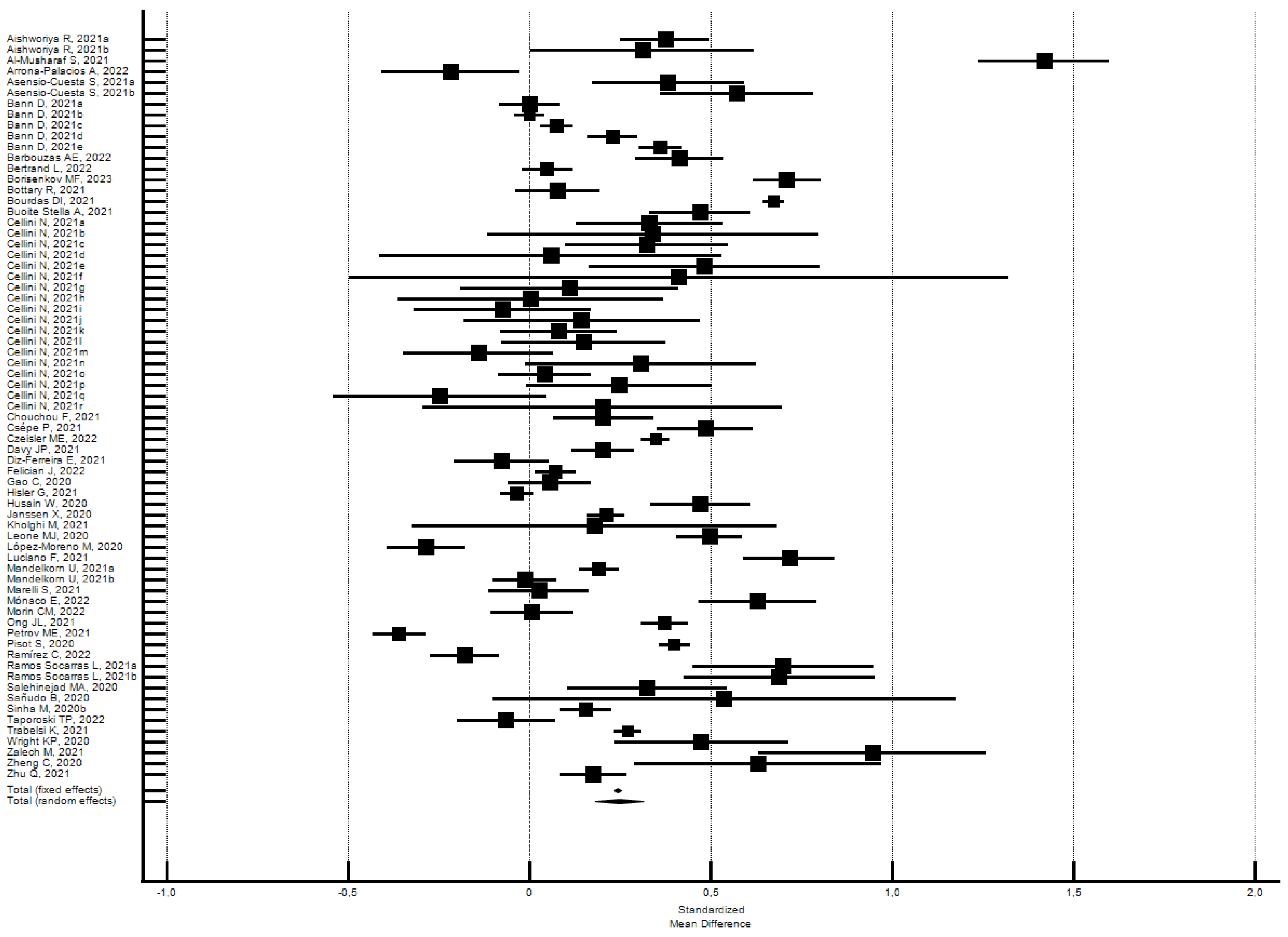
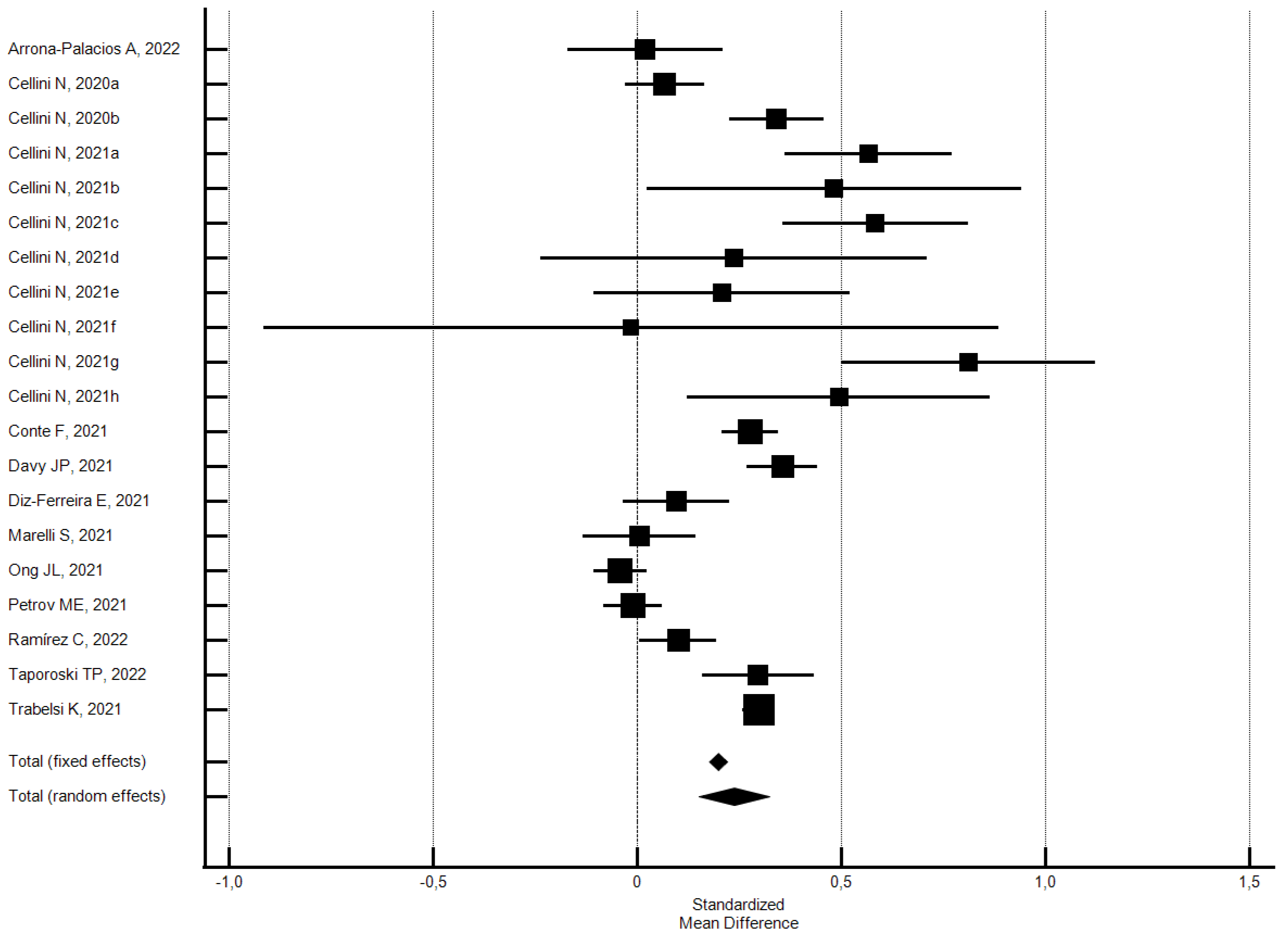
The participants reported a small increase in sleep duration (hours) (SMD = 0.25; 95% CI 0.18–0.32; I2 = 97.2%) (Figure 2); the analysis did not show a significant publication bias (Egger’s p = 0.63).
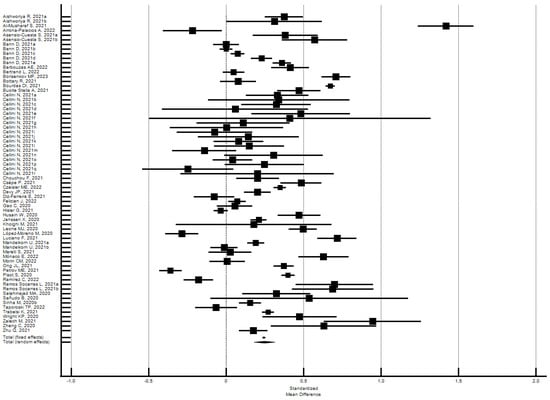
Figure 2.
Forest plot showing pooled changes in sleep duration (hours) between before and during the lockdown. Caption: error bars = 95% confidence interval; square boxes = individual study point estimates; diamond box = pooled point estimates. Aishworiya R., 2021a: female; Aishworiya R., 2021b: male; Asensio-Cuesta S., 2021a: male; Asensio-Cuesta S., 2021b: female; Bann D., 2021a: 1946; Bann D., 2021b: 1958; Bann D., 2021c: 1970; Bann D., 2021d: 1990; Bann D., 2021e: 2001; Cellini N., 2021a: Belgian regular workers, female; Cellini N., 2021b: Belgian regular workers, male; Cellini N., 2021c: Belgian remote workers, female; Cellini N., 2021d: Belgian remote workers, male; Cellini N., 2021e: Belgian students, female; Cellini N., 2021f: Belgian students, male; Cellini N., 2021g: Belgian unemployed/retired, female; Cellini N., 2021h: Belgian unemployed/retired, male; Cellini N., 2021i: Italian regular workers, female; Cellini N., 2021j: Italian regular workers, male; Cellini N., 2021k: Italian remote workers, female; Cellini N., 2021l: Italian remote workers, male; Cellini N., 2021m: Italian Stop working, female; Cellini N., 2021n: Italian Stop working, male; Cellini N., 2021o: Italian students, female; Cellini N., 2021p: Italian students, male; Cellini N., 2021q: Italian unemployed/retired, female; Cellini N., 2021r: Italian unemployed/retired, male; Mandelkorn U., 2021a: Study 1; Mandelkorn U., 2021b: Study 2; Ramos Socarras L., 2021a: 18–21-years old; Ramos Socarras L., 2021b: 22–25-years old.
Subgroups analysis by the risk of bias did not find significant differences. The studies with a low risk of bias produced a higher effect on sleep duration than the overall set of studies, while those with a high risk of bias produced a lower effect. Specifically, the 54 outcomes of the 30 studies [27,32,40,44,49,50,51,52,57,68,70,81,85,93,97,103,107,115,120,122,129,130,136,137,146,153,160,173,176,177] with a low risk of bias (NOS ≥ 5) showed a significant increase of 0.26 SMD in sleep duration (95% CI 0.18–0.34; I2 = 97.5%; not significant Egger’s publication bias). Instead, the 15 outcomes of the 14 studies [39,45,46,63,66,74,95,111,112,114,119,143,161,178] with a high risk of bias (NOS < 5) showed a significant increase of 0.22 SMD in sleep duration (95% CI 0.11–0.33; I2 = 95.4%; not significant Egger’s publication bias).
3.1.2. Meta-Analytic Changes: Percentage of Change in Sleep Duration
The percentage change in sleep duration during lockdown with respect to before was evaluated by 51 studies [28,29,31,33,38,41,44,46,47,53,54,60,65,71,73,77,78,79,83,85,89,90,91,94,96,97,98,99,101,105,109,121,124,131,133,135,138,139,140,142,150,154,155,157,164,166,168,172,174,175,178].
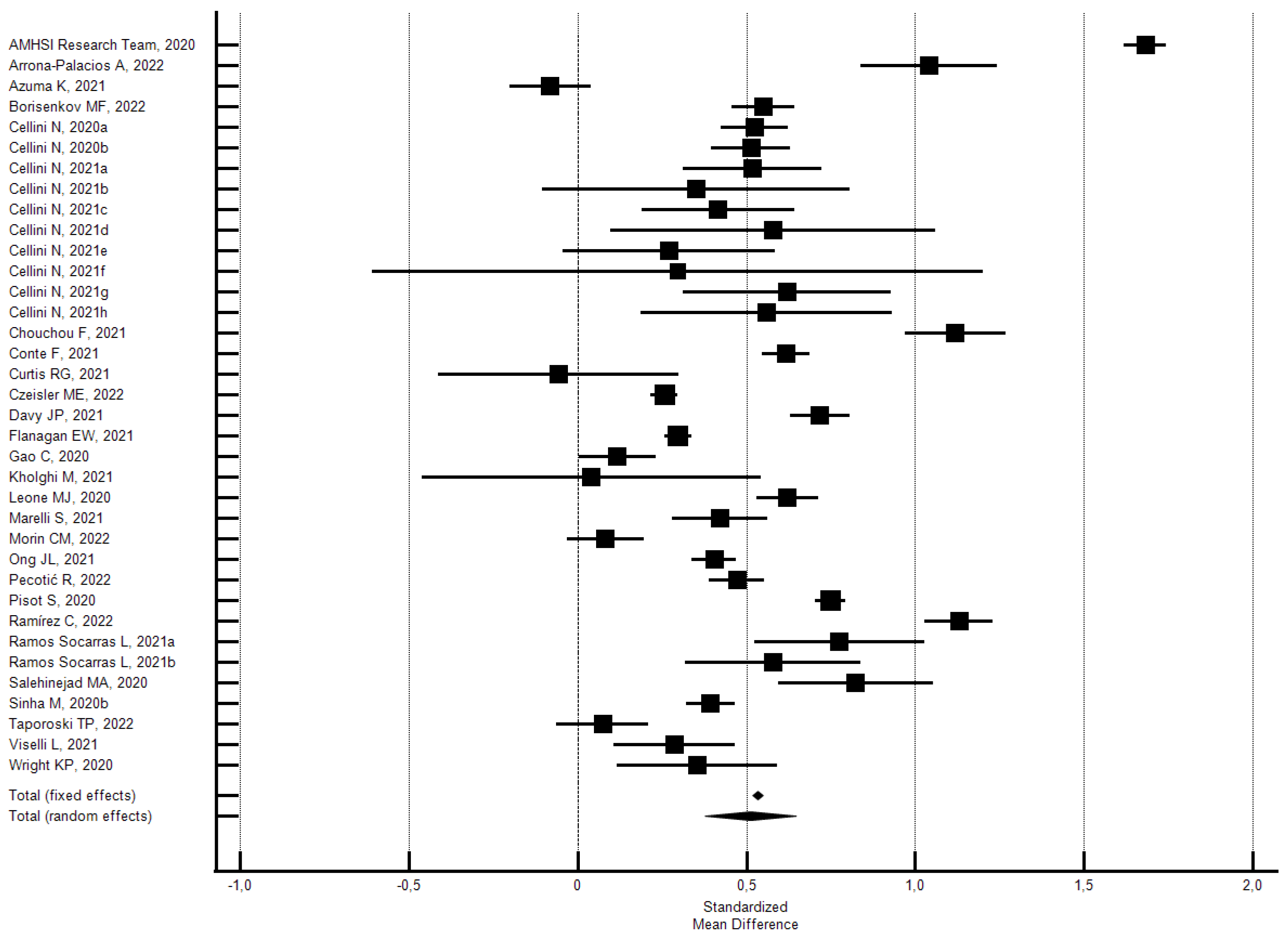
As shown in Figure 3, the random effects model showed that 55.0% (95% CI 49.84–60.07; I2 = 99.6%) of the participants reported a change in sleep duration (hours). In particular, 19.7% reported a decrease (95% CI 16.80–22.87; I2 = 99.3%) and 35.2% reported an increase (95% CI 32.09–38.44; I2 = 99.2). Significant Eggers’s publication bias emerged for the above outcomes, but the sensitivity analyses confirmed the main findings.
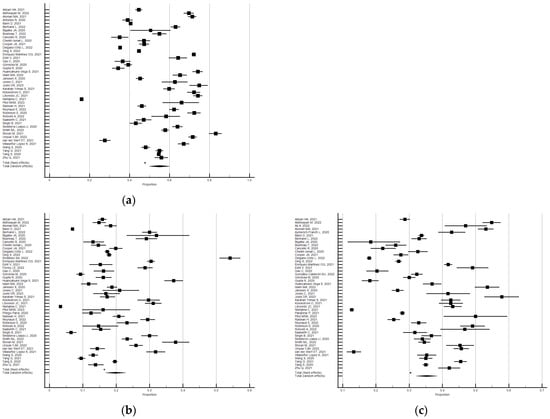
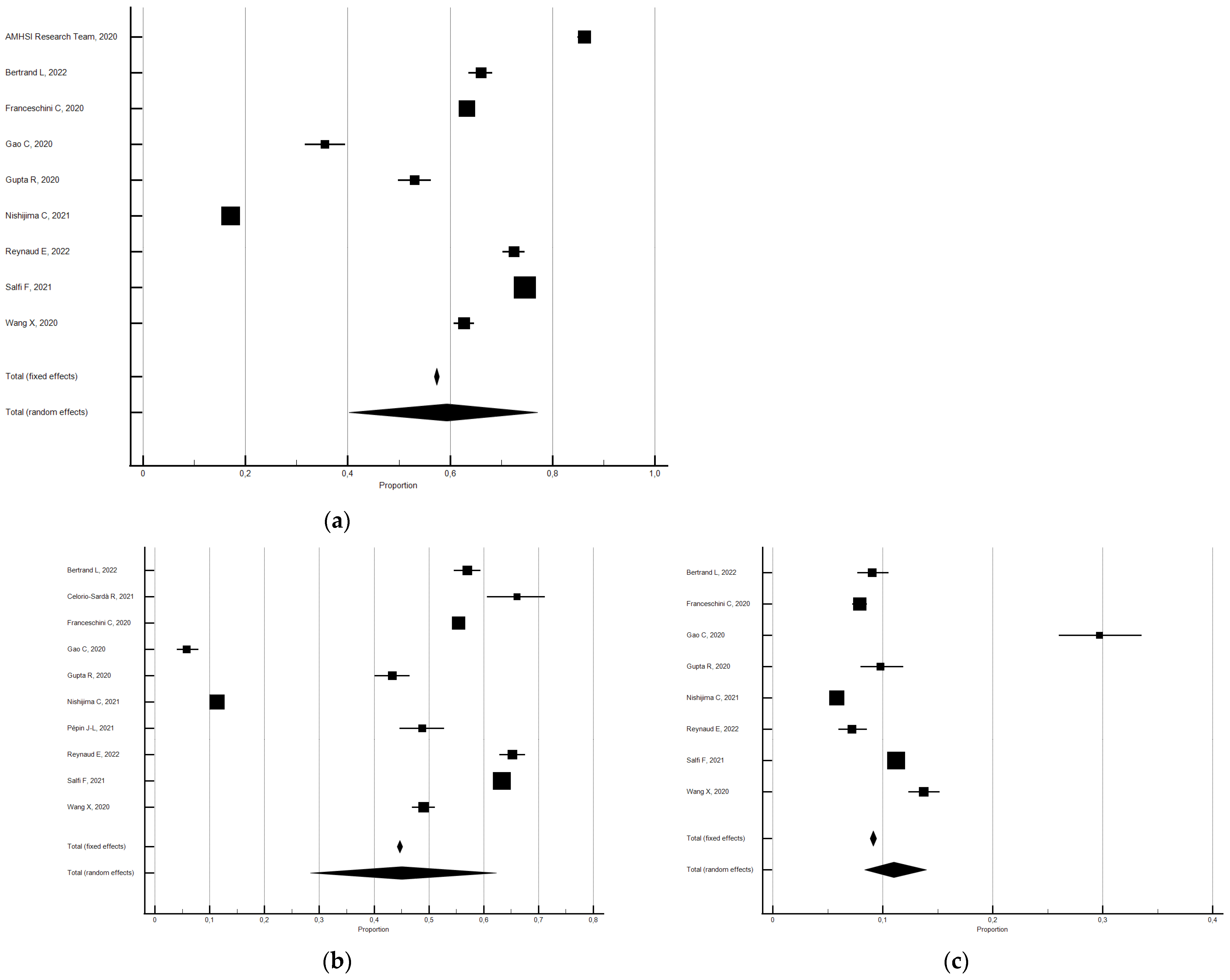
Figure 3.
Forest plot showing a pooled percentage of changes in sleep duration from before to during the lockdown: changes (a), decrease (b), and increase (c). Caption: error bars = 95% confidence interval; square boxes = individual point estimates; diamond box = pooled point estimates.
Subgroup analysis by risk of bias uncovered significant differences. The studies with a low risk of bias produced a lower percentage of changes in sleep duration compared with the overall studies, while those with a high risk of bias produced a higher percentage. Specifically, the 24 studies [28,31,38,44,60,65,71,73,77,78,83,85,90,91,94,97,99,121,135,157,166,168,174,175] with a low risk of bias (NOS ≥ 5) showed that 48.8% of the participants reported a change in sleep duration (95% CI 41.54–56.12, I2 = 99.8%; significant Egger’s publication bias), 30.7% reported an increase (95% CI 26.13–35.41; I2 = 99.5%; not significant Egger’s publication bias), and 19.7% reported a decrease (95% CI 15.29–24.47; I2 = 99.6%; not significant Egger’s publication bias). Instead, the 27 studies [29,33,41,46,47,53,54,79,89,96,98,101,105,109,124,131,133,138,139,140,142,150,154,155,164,172,178] with a high risk of bias (NOS < 5), showed that 60.8% of the participants reported a change in sleep duration (95% CI 56.64–64.85, I2 = 97.7%; not significant Egger’s publication bias), 39.1% reported an increase (95% CI 35.54–42.73; I2 = 98.0%; significant Egger’s publication bias), and 19.8% reported a decrease (95% CI 16.78–23.01; I2 = 97.3%; not significant Egger’s publication bias).
Subgroup analysis by country’s area was only possible for the percentages of change in sleep duration. As we can see from Table 2, the percentage of change in sleep duration was very high in South America (72%), lower in East Asia (45%), and it was around values above 50% in other areas. The change concerned the increase in sleep hours in all areas, especially in Central Asia (44%) and South America (40%), and it was around values above 30% in other areas. Significant differences were observed among all areas except North America (30.5%) vs. Europe (30.8%), and East Asia (33.3%) vs. Mediterranean Europe (33.8%).

Table 2.
Percentages of change in sleep duration from before to during the lockdown by country’s area.
3.1.3. Meta-Analytic Changes: Percentage of Atypical Sleep Duration before and during the Lockdown
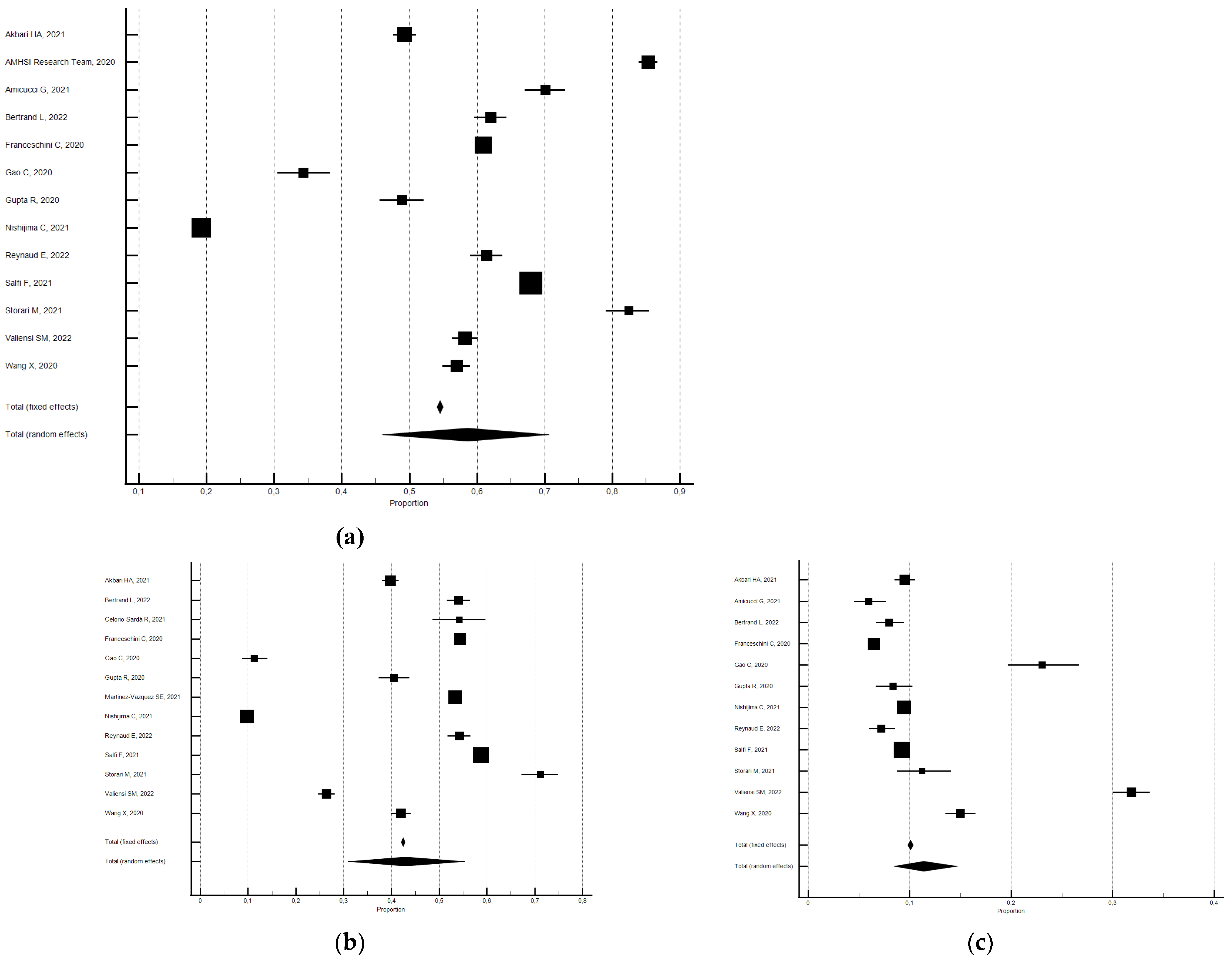
Changes in the percentage of participants with atypical sleep duration were evaluated in 18 studies [26,30,34,44,45,59,60,61,62,72,86,92,93,134,138,151,158,167].
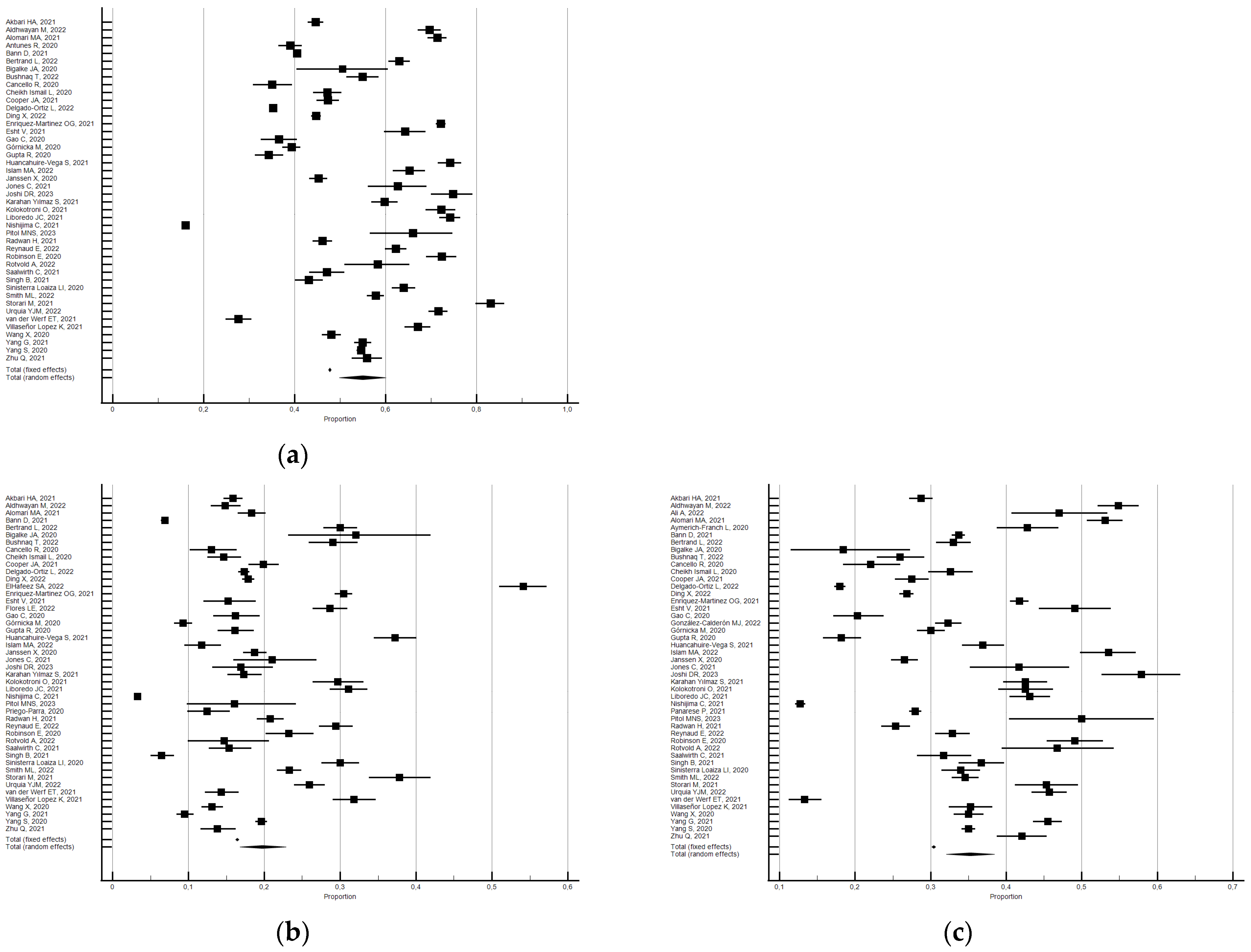
Compared with the pre-lockdown period, the percentage of participants with atypical sleep duration increased by approximately 17% during the lockdown (pooled relative risk = 1.17, 95% CI 1.04–1.31; I2 = 98.2; not significant publication bias) (see Figure 4).
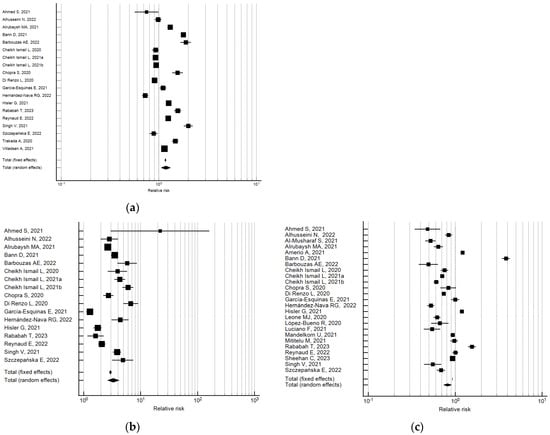
Figure 4.
Forest plot showing pooled changes in atypical sleep duration from before to during the lockdown: atypical (a), decrease (b), increase (c). Caption: error bars = 95% confidence interval; square boxes = individual study point estimates; diamond box = pooled point estimates.
Data analysis showed that the percentage of those participants who slept more than 8/9 h increased during lockdown; a pooled relative risk of 3.31 was observed (95% CI 2.60–4.21; I2 = 95.2, not significant publication bias) [26,30,34,44,45,59,60,61,62,72,86,92,93,134,138,151,158].
Data analysis also uncovered that, with respect to before, the percentage of participants who slept less than 6/7 h decreased during lockdown; a pooled relative risk of 0.82 was observed (95% CI 0.73–0.91; I2 = 98.7; not significant publication bias) [26,30,32,34,35,44,45,59,60,61,62,72,86,92,93,107,110,112,114,117,134,138,149,158].
3.2. Time in Bed
Among the 15 studies that examined TIB, 12 were included in the meta-analysis and 3 were narratively described [69,88,126].
Meta-Analytic Changes in Time in Bed: Means before and during the Lockdown
The changes in TIB were evaluated considering 20 outcomes derived from 12 studies [39,56,57,64,70,74,115,122,129,136,160,161]. The participants reported a small increase in TIB (SMD = 0.24; 95% CI 0.151–0.32; I2 = 90.6%; not significant Egger’s publication bias) (see Figure 5).
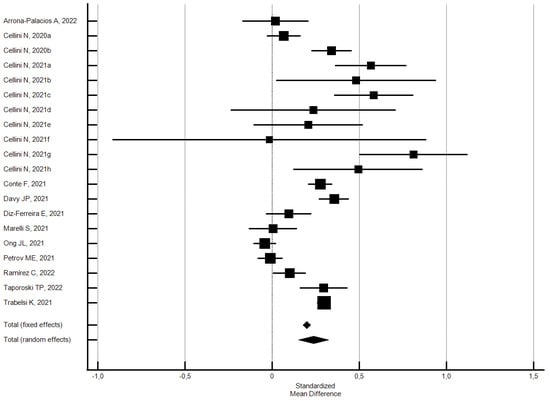
Figure 5.
Forest plot showing pooled changes in TIB from before to during the lockdown: increase, decrease. Caption: error bars = 95% confidence interval; square boxes = individual point estimates; diamond box = pooled point estimates. Cellini N., 2020a: student; Cellini N., 2020b: worker; Cellini N., 2021a: Belgian regular workers, female; Cellini N., 2021b: Belgian regular workers, male; Cellini N., 2021c: Belgian remote workers, female; Cellini N., 2021d: Belgian remote workers, male; Cellini N., 2021e: Belgian students, female; Cellini N., 2021f: Belgian students, male; Cellini N., 2021g: Belgian unemployed/retired, female; Cellini N., 2021h: Belgian unemployed/retired, male.
Subgroup analysis by risk of bias showed no significant differences in TIB: the studies with a low risk of bias produced a lower effect compared with the overall studies, while those with a high risk of bias produced a higher effect. Specifically, the 17 outcomes of the 9 studies [56,57,64,70,115,122,129,136,160] with a low risk of bias (NOS ≥ 5) showed a small but significant increase in TIB (SMD 0.26; 95% CI 0.16–036; I2 = 91.8%; not significant Egger’s publication bias); while the three studies [39,74,161] with a high risk of bias (NOS < 5) showed a small but not significant lower increase (SMD 0.15; 95% CI −0.03–0.34; I2 = 87.1%; not significant Egger’s publication bias).
3.3. Sleep Timing
Out of the 45 studies that examined bedtime, 30 were included in the meta-analysis and 15 were narratively described [27,37,42,50,76,88,100,119,126,127,146,156,159,169,171]. Out of the 51 studies that examined wake-up time, 36 were included in the meta-analysis, 14 were narratively described [27,37,42,74,76,88,100,106,119,146,148,156,169,171], and one study provided data both for the meta-analysis and the qualitative synthesis [126].
3.3.1. Meta-Analytic Changes in Bedtime: Means before and during the Lockdown
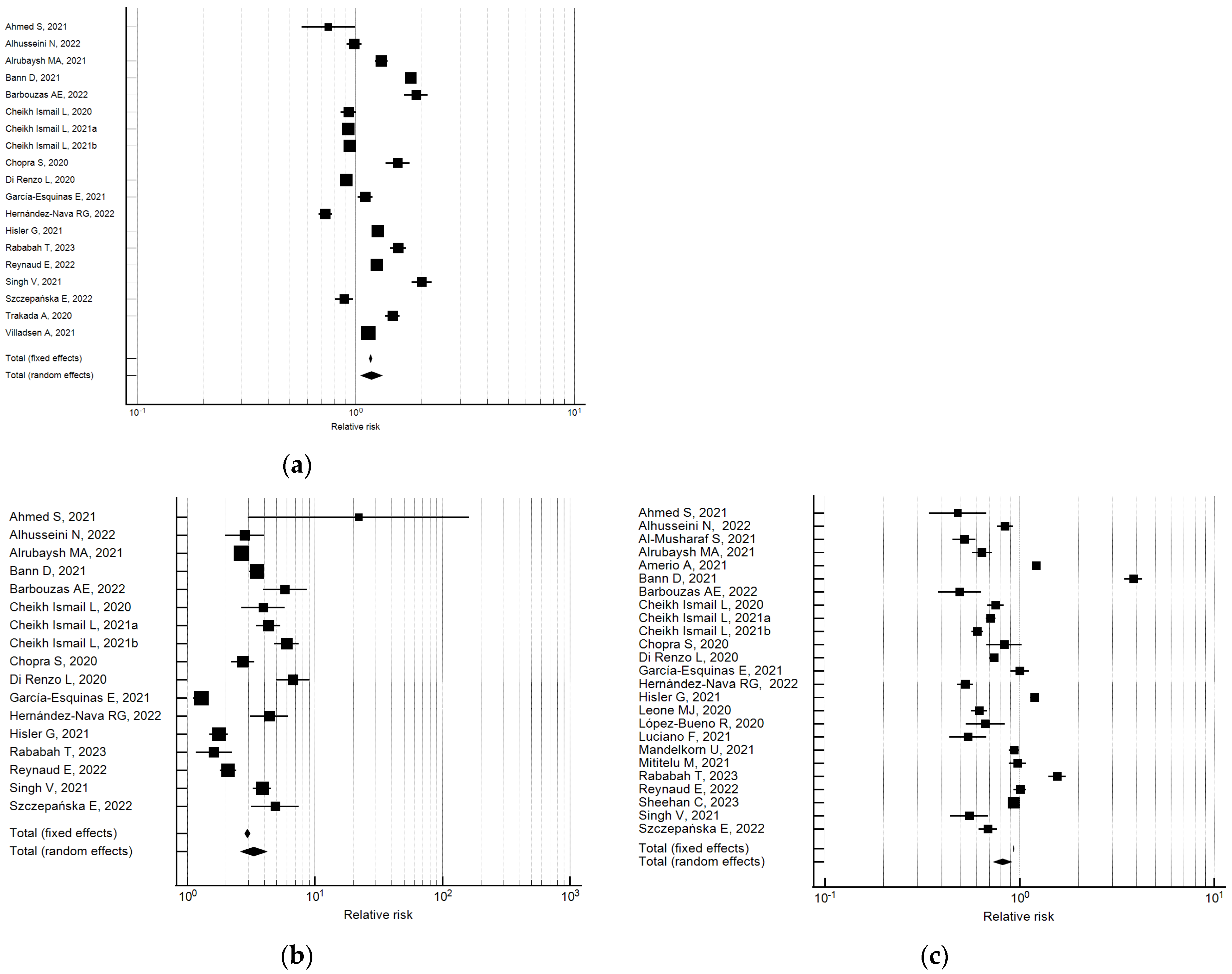
Changes in bedtime were evaluated considering 45 outcomes reported in 27 studies [36,39,43,49,56,57,63,64,67,68,70,82,85,103,107,115,120,122,125,130,136,137,143,153,160,170,173]. The participants reported a medium significant delay in bedtime (hours) of 0.51 SMD (95%CI 0.38–0.64; I2 = 98.5%; not significant Egger’s publication bias) (see Figure 6).
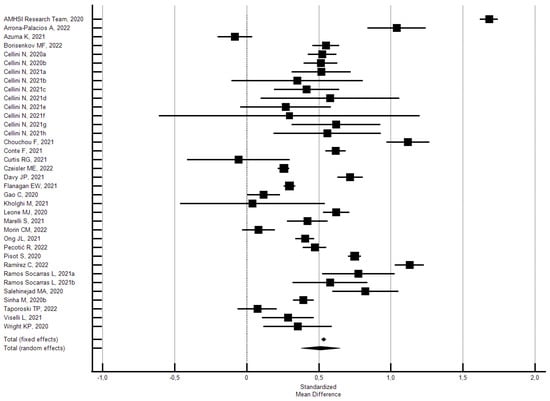
Figure 6.
Forest plot showing pooled changes in bedtime from before to during the lockdown. Caption: error bars = 95% confidence interval; square boxes = individual study point estimates; diamond box = pooled point estimates. Cellini N., 2020a: student; Cellini N., 2020b: worker; Cellini N., 2021a: Belgian regular workers, female; Cellini N., 2021b: Belgian regular workers, male; Cellini N., 2021c: Belgian remote workers, female; Cellini N., 2021d: Belgian remote workers, male; Cellini N., 2021e: Belgian students, female; Cellini N., 2021f: Belgian students, male; Cellini N., 2021g: Belgian unemployed/retired, female; Cellini N., 2021h: Belgian unemployed/retired, male; Ramos Socarras L., 2021a: 18–21-years old; Ramos Socarras L., 2021b: 22–25-years old.
Subgroup analysis by risk of bias uncovered no significant differences. Specifically, the 32 outcomes of the 23 studies [36,43,49,56,57,64,67,68,70,82,85,103,107,115,120,122,125,130,136,137,153,160,173] with a low risk of bias (NOS ≥ 5) showed a small but significant delay of 0.47 SMD in bedtime (95% CI 0.33–0.62; I2 = 98.6%; not significant Egger’s publication bias). The four studies [39,63,143,170] with a high risk of bias (NOS < 5) showed that there was a large significant delay of 0.82 SMD in bedtime (95% CI 0.42–1.21; I2 = 94.4%; not significant Egger’s publication bias).
3.3.2. Meta-Analytic Changes in Bedtime: Percentage of Change
The percentage of participants who changed or maintained the same bedtime during the lockdown compared with the pre-lockdown period were evaluated by 14 studies [28,36,46,58,84,85,91,116,121,138,144,157,165,172]. As shown in Figure 7, the random effects model showed that 57.6% (95% CI 44.41–70.27, I2 = 99.97; not significant Egger’s publication bias) of the participants reported a change in bedtime. In particular, 42.9% reported a delayed bedtime (95% CI 30.93–55.29; I2 = 99.9; not significant Egger’s publication bias) and 11.9% said they went to bed earlier (95% CI 8.79–15.50; I2 = 99.1; not significant Egger’s publication bias).
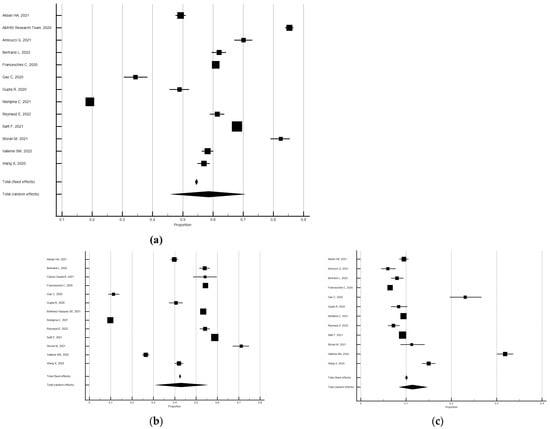
Figure 7.
Forest plot showing pooled changes in bedtime from before to during the lockdown: changes (a), delayed (b), earlier (c). Caption: error bars = 95% confidence interval; square boxes = individual point estimates; diamond box = pooled point estimates.
Subgroup analysis by risk of bias revealed significant differences. Specifically, the seven studies [28,36,84,85,91,121,157] with a low risk of bias (NOS ≥ 5) showed that 54.9% of the participants reported a change in bedtime (95% CI 33.32–75.56, I2 = 99.9%; not significant Egger’s publication bias), 36.1% said they had a delayed bedtime (95% CI 16.02–59.14; I2 = 99.9%; not significant Egger’s publication bias), whereas 10.7% reported an earlier bedtime (95% CI 8.26–13.45; I2 = 96.8%; not significant Egger’s publication bias). Instead, the seven studies [46,58,116,138,144,165,172] with a high risk of bias (NOS < 5), revealed that 61.4% of the participants reported a change in bedtime (95% CI 56.16–66.47, I2 = 97.8%; significant Egger’s publication bias), 48.8% a delayed bedtime (95% CI 40.51–57.14; I2 = 99.5%; not significant Egger’s publication bias), and 13.3% an earlier one (95% CI 6.62–21.81; I2 = 99.5%; not significant Egger’s publication bias).
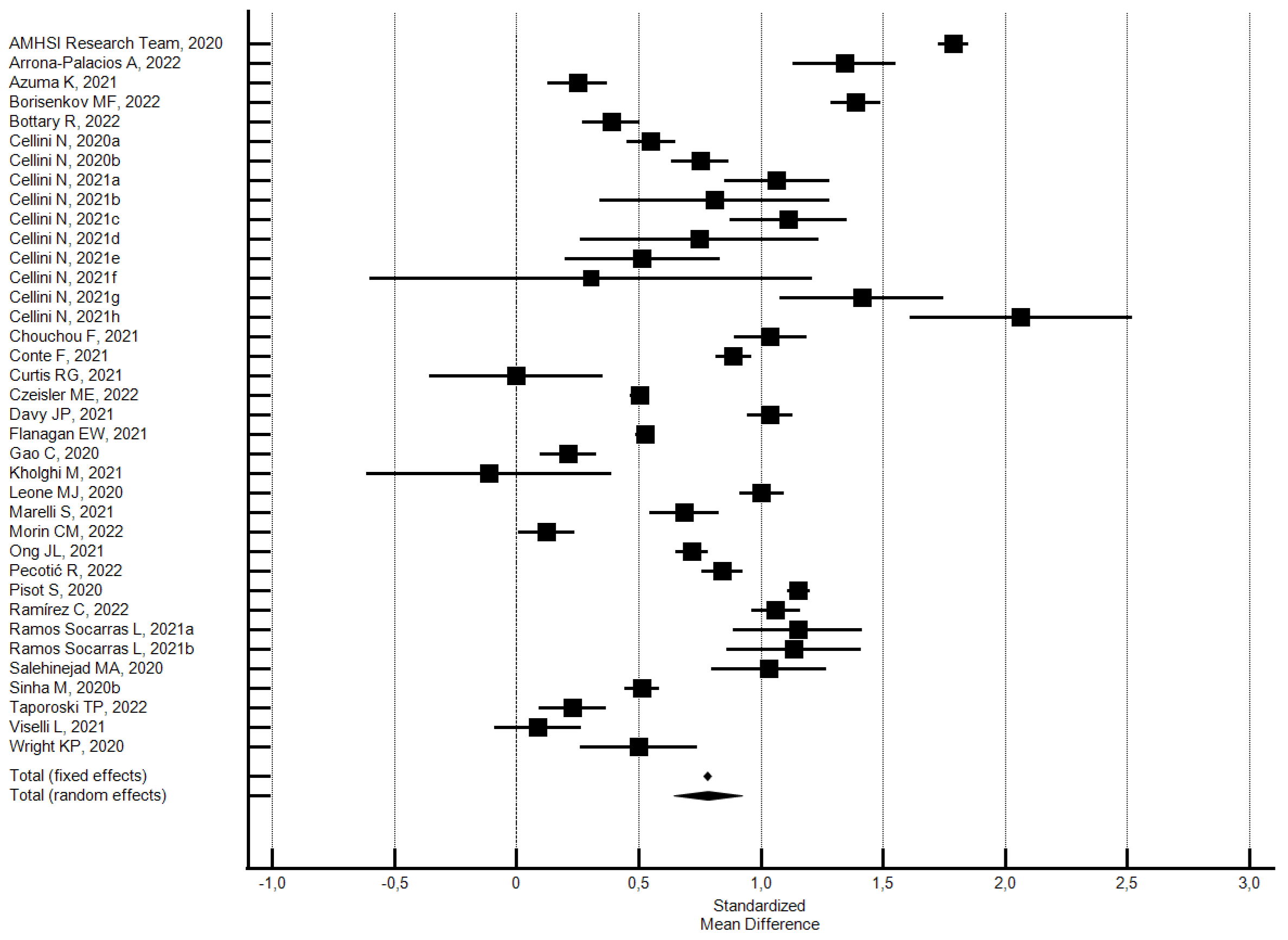
3.3.3. Meta-Analytic Changes in Wake-Up Time: Percentage of Change
Changes in the wake-up time were evaluated considering 37 outcomes reported in 28 studies [36,39,43,49,50,56,57,63,64,67,68,70,82,85,103,107,115,120,122,125,130,136,137,143,153,160,170,173]. Participants reported a medium significant delay in wake-up time of 0.78 SMD (95% CI 0.64–0.92; I2 = 98.5%; not significant Egger’s publication bias) (see Figure 8).
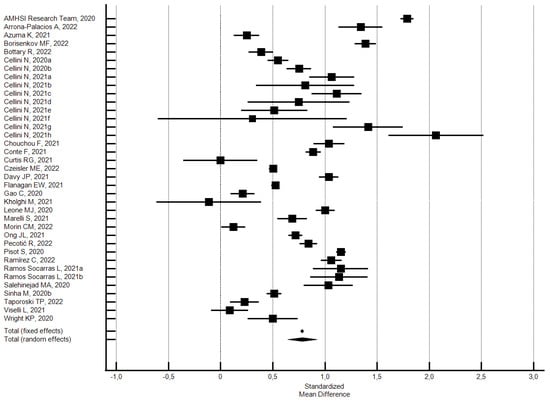
Figure 8.
Forest plot showing pooled changes in wake-up time from before to during the lockdown. Caption: error bars = 95% confidence interval; square boxes = individual study point estimates; diamond box = pooled point estimates. Cellini N., 2020a: student; Cellini N., 2020b: worker; Cellini N., 2021a: Belgian regular workers, female; Cellini N., 2021b: Belgian regular workers, male; Cellini N., 2021c: Belgian remote workers, female; Cellini N., 2021d: Belgian remote workers, male; Cellini N., 2021e: Belgian students, female; Cellini N., 2021f: Belgian students, male; Cellini N., 2021g: Belgian unemployed/retired, female; Cellini N., 2021h: Belgian unemployed/retired, male; Ramos Socarras L., 2021a: 18–21-years old; Ramos Socarras L., 2021b: 22–25-years old.
Subgroup analysis by risk of bias uncovered no significant differences. However, the 33 outcomes of the 21 studies [36,43,49,64,67,68,70,82,85,103,107,115,120,122,125,130,136,137,153,160,173] with a low risk of bias (NOS ≥ 5) showed a medium significant delay in wake-up time of 0.77 SMD (95% CI 0.63–0.92; I2 = 98.7%; not significant Egger’s publication bias). The four studies [39,63,143,170] with a high risk of bias (NOS < 5) showed a large significant delay in wake-up time of 0.87 SMD (95% CI 0.33–1.42; I2 = 97.0%; not significant Egger’s publication bias).
3.3.4. Meta-Analytic Changes in Wake-Up Time: Percentage of Change
The percentage change in wake-up time during the lockdown was evaluated by 11 studies [36,46,58,84,85,91,121,126,138,144,172]. As shown in Figure 9, the random effects model showed that 59.3% of the participants reported a change in wake-up time (95% CI 40.26–77.07, I2 = 99.9%; not significant Egger’s publication bias). In particular, 45.0% reported a delayed wake-up time (95% CI 28.38–62.30; I2 = 99.9%; not significant Egger’s publication bias) and 11.01% reported an earlier one (95% CI 8.35–13.98; I2 = 98.5%; not significant Egger’s publication bias).
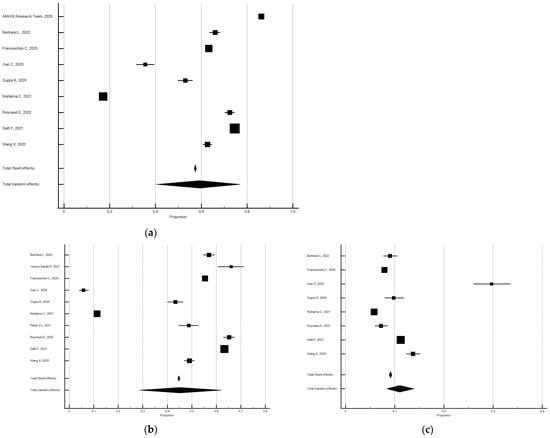
Figure 9.
Forest plot showing pooled changes in wake-up time from before to during the lockdown: changes (a), delayed (b), earlier (c). Caption: error bars = 95% confidence interval; square boxes = individual point estimates; diamond box = pooled point estimates.
Subgroup analysis by risk of bias showed significant differences. The studies with a low risk of bias produced lower percentages of change with respect to the overall studies, but those with a high risk of bias produced higher percentages of change. Specifically, the six studies [36,84,85,91,121,126] with a low risk of bias (NOS ≥ 5) showed that 51.3% of the participants reported a change in wake-up time (95% CI 21.75–80.35, I2 = 99.9%; not significant Egger’s publication bias), 30.4% reported a delayed wake-up time (95% CI 9.16–57.43; I2 = 99.9%; not significant Egger’s publication bias) and 12.0% reported an earlier one (95% 7.26–17.65; I2 = 98.9%; not significant Egger’s publication bias). Instead, the five studies [46,58,138,144,172] with a high risk of bias (NOS < 5) revealed that 69.1% of the participants reported a change in wake-up time (95% CI 62.82–74.96, I2 = 98.2%; not significant Egger’s publication bias) with 60.1% reporting a delayed wake-up time (95% CI 53.82–66.11; I2 = 97.9%; not significant Egger’s publication bias) and 10.2% an earlier one (95% CI 8.07–12.62; I2 = 94.2%; not significant Egger’s publication bias).
3.4. Qualitative Synthesis
3.4.1. Synthesis of Sleep Duration
Twenty-five studies not included in the meta-analysis evaluated changes in sleep duration (see Table 3). Fifteen reported an increase [25,48,75,102,106,108,126,128,141,145,156,159,162,163], four reported no changes [55,88,132,169], and three reported a decrease in sleep duration [80,87,123]. One study found an increase in sleep duration among students but a decrease among office workers [113]; another study reported an increased duration in the young and middle-aged participants but not in the older ones [104], and one study found longer sleep duration in the evening-type chronotype compared to the neither-type and morning-type groups [144]. These findings are consistent with the overall results of our meta-analysis.

Table 3.
Synthesis of changes in outcomes from before to during the lockdown.
3.4.2. Synthesis of Time in Bed
The three studies not included in the meta-analysis regarding changes in TIB found an increase during the lockdown compared to the pre-lockdown period [69,88,126] (see Table 3).
3.4.3. Synthesis of Sleep Timing
Fifteen studies not included in the meta-analysis evaluated changes in the bedtime (see Table 3). Ten reported delayed bedtime [27,37,42,50,76,88,119,159,169,171] and two earlier one [146,156]; two of the studies were unable to detect a clear change [100,127]. Finally, one study found no change in the overall sample but a greater delay in the evening chronotype group compared to the morning one [126].
Sixteen studies not included in the meta-analysis evaluated changes in the wake-up time (see Table 3). Eleven reported a delayed wake-up time [27,37,42,76,88,119,146,148,156,169,171] and one an earlier wake-up time [74]. Two of the studies were unable to identify a clear change [100,147] and two reported no change [106,126].
These findings are in line with the results of the meta-analysis, which found a delayed bedtime and wake-up time.
3.4.4. Synthesis of Napping Habits
The napping habits, evaluated in twenty-three studies, were only narratively described (see Table 3) [33,36,42,63,64,81,84,86,91,100,107,113,118,119,120,129,136,144,145,147,152,165,169].
Most studies found an increase in the frequency and length of naps as well as in the percentage of participants taking naps. According to Franceschini, while the good sleepers did not change or reduce the length of naps, the poor sleepers increased it [84]. Finally, Salfi found that a significantly higher proportion of the evening-type chronotype subjects reported changes in their napping habits with respect to the morning-type and neither-type chronotype subjects [144].
4. Discussion
This systematic review and meta-analysis uncovered significant changes in several quantitative sleep parameters of the general population from before to during the first COVID-19 lockdown. An increase in both sleep duration and the percentage of individuals with atypical sleep duration was detected. Moreover, the frequency of individuals reporting long sleep duration increased (≥8/9 h), as well as the time in bed and napping habits. Subgroup analysis by country’s area showed an increased sleep duration in all areas considered (North America, South America, Central Asia, East Asia, West Asia, Europe, Mediterranean Europe), prevalently in Central Asia and South America. In addition, we detected significant differences among all areas except for North America vs. Europe and East Asia vs. Mediterranean Europe. The most striking change that emerged from this study regards the sleep–wake cycle. Indeed, more than 40% of the participants reported a significant delay in bedtime and wake-up time.
When reading these data, it is necessary to consider that most of the studies are cross-sectional and have a high risk of bias that can lead to unreliable interpretations. In addition, due to the lockdown restrictions, most of the studies used self-reported data, which tend to be subject to recall and social desirability biases. This issue may have led to a selection bias by excluding non-regular Internet users, such as older people.
The shift to remote work and virtual classes due to the lockdown forced the majority to go slower and extend their timelines, allowing more time for sleep [179,180]. Considering the worldwide prevalence of insufficient sleep, this increased time to sleep could be seen as a beneficial effect of restrictive measures [181]. However, it is unclear whether the increase in sleep duration corresponded to better sleep quality, as some studies reported a worse sleep quality during the lockdown compared with the pre-lockdown levels [11,56]. Moreover, the finding of an increased time in bed should be interpreted with caution. In fact, several works reported a decrease in sleep efficiency, leading to the hypothesis that an increase in the time spent in bed did not necessarily correspond to a longer sleep duration [11,57].
Our findings align with previous systematic reviews and meta-analyses [15,16], as well as certain original studies [12,13,14], which have documented extended sleep duration and delayed bedtime patterns within the general population. However, comparing our results across geographical regions poses challenges [13]. For instance, Robbins et al. observed significant variations in sleep duration both before and during the COVID-19 pandemic, noting a lesser increase in Seoul compared to New York City, Los Angeles, London, and Stockholm [13]. When juxtaposed with the evolution of sleep parameters across the different phases of the COVID-19 pandemic, our study reveals several differences. For instance, a longitudinal investigation unveiled a shift in bedtime during the initial lockdown compared to the pre-lockdown period, followed by a reversal during subsequent lockdowns, eventually reverting to pre-pandemic norms. Similarly, the duration of time spent in bed mirrored this trend. Intriguingly, afternoon napping habits remained largely unaffected during these periods of lockdown [64]. These trends suggest an adaptation to the progression of restrictive measures, with researchers hypothesizing that this adaptation stems from the normalization of lifestyle routines. In contrast, delays in both bedtime and wake-up times were noted during both lockdowns compared to the pre-lockdown scenario in the Belgian population, especially among individuals under 24 years old [182]. Another longitudinal study conducted in Italy highlighted a reduction in sleep duration during both the first and second waves of the pandemic [183].
Below, we analyze the potential primary effects on overall health and seek to explore the possible causes of alterations in quantitative sleep parameters.
4.1. The Consequences of Quantitative Sleep Parameters Alterations on General Health
Sleep represents an essential biological process for life and optimal health and it is well known that healthy sleep patterns are characterized by adequate duration, good quality, appropriate timing, and regularity, and the absence of sleep disturbances and problems [184]. The changes in quantitative sleep parameters that emerged from this work are of pivotal relevance, given their potentially harmful impact on the immune system, and other health outcomes. Sleep plays a critical role in maintaining the balance of the immune system, and any alterations in its duration and quality can impact its susceptibility to infections and the effectiveness of vaccinations [185,186]. In the context of SARS-CoV-2 vaccination, studies have indicated a positive association between regular sleep duration and antibody levels [185,187]. Specifically, ensuring sufficient sleep, especially within the first week after booster vaccination, is essential for optimal antibody production [188]. However, it is important to consider that while a higher frequency of daytime napping per week initially showed a negative correlation with antibody levels in one study, this association vanished after adjusting for confounding factors, underscoring the intricate nature of the relationship between sleep and post-vaccination immune response [184,187].
Alterations in sleep timing may have important consequences on multiple health variables. Later sleep timing in adults has been associated with depression, adverse brain health outcomes, cognitive impairment, obesity, higher cardiometabolic risk, osteopenia and osteoporosis [189]. An earlier bedtime was associated with a higher risk of diabetes, stroke, obesity, hypertension, and cardiovascular diseases (CVDs) [190].
A sleep duration of 7–8 h has a beneficial impact on general health with both shorter and longer sleep durations than 7–8 h are associated with poor outcomes such as mortality, diabetes, CVD, coronary heart disease, obesity, and stroke [191,192]. A prolonged time spent in bed appears to be linked to a greater decline in physical function and a higher risk of motor disability in the older population [193].
The impact of napping on health is still a debated topic. Indeed, napping seems to have both positive and negative effects on health and its effects appear to depend not only on the duration of the nap itself but also on other factors such as sex and age. Overall, naps showed significant beneficial effects on several cognitive functions [194], but in older people, only short or moderate duration of naps compared with both non-napping and long napping are associated with cognitive benefits in older adults [195]. Depression seems to be associated with long afternoon naps (≥90 min) in middle-aged women, and with short naps (<30 min) in older men [196]. Daytime napping restricted to 30 min/d for adults (aged < 60 years) has no negative effect on cardiovascular health, while it seems not to be beneficial for older adults [197].
4.2. Exploring the Causes of Quantitative Sleep Parameters Alterations
Several variables may have contributed to the sleep changes uncovered by this work. One of the most striking involves the modification to the circadian rhythm. These biological rhythms, operating in 24 h cycles, are strongly influenced by external factors such as social patterns, daily routines, and exposure to sunlight [198]. These stimulating signals were markedly altered during the COVID-19 pandemic due to home confinement and profound lifestyle modification, such as remote work and distance learning, which both contributed to bedtime postponement [12,107,173,199]. The rise in stress and anxiety levels during the lockdown, fueled by psychological distress associated with social isolation, financial challenges, and unemployment, along with growing concerns for personal and loved ones’ well-being, may also have had an impact on sleep health [200]. Finally, although digital platforms such as social media helped to keep people connected during the pandemic and lockdown, the sharp increase in social media usage during the pandemic may also have had an important impact on sleep health [201]. Indeed, according to a systematic review by Drumheller and colleagues, later bedtime and wake-up times and a decrease in sleep duration were found as the screen time use increased [202].
4.3. Strengths and Limitations
Our study has several strengths. Firstly, to the best of our knowledge, this is the first systematic review and meta-analysis that has sought to provide a comprehensive synthesis of changes in quantitative sleep parameters in the general population during the first lockdown compared to pre-lockdown levels. Despite the abundance of research on the topic, existing systematic reviews or meta-analyses do not offer as comprehensive and detailed coverage of these phenomena as provided by our work. Moreover, our research stands out for its thorough analysis of changes associated with atypical sleep duration and napping habits, areas often overlooked or not fully examined in previous studies. A meticulous methodological approach and an extensive literature review were utilized to explore sleep changes. Additionally, using a random-effect model with a more conservative estimation allowed us to at least partially address the heterogeneity between studies, given the differences in socio-cultural realities, methodological aspects (study design and outcome measures), and the severity of the lockdown measures. The study also has many limitations. The heterogeneity of the collected data limited the subgroup analysis exclusively to the risk of bias and to the countries’ areas. The comparison of the areas is also limited to sleep duration. The results of this study refer exclusively to the first lockdown. Finally, the fact that the lockdown measures differed widely across countries could have affected the study’s outcomes.
4.4. Implications of the Results
While the implementation of lockdown measures allowed governments to control the transmission of the SARS-CoV-2 infection, it also had adverse effects on the sleep health of the general population, in particular, on circadian rhythms and sleep–wake cycles. Given the health implications of these changes, and to prepare for possible future pandemics, these findings underline the importance of promoting healthy sleep hygiene, implementing screening programs, and treating sleep disturbances appropriately. However, extending beyond the initial waves of infections, sleep-related issues have persisted in capturing the attention of the scientific community, particularly concerning patients classified as experiencing long COVID. As defined by the WHO, long COVID encompasses a condition emerging in individuals with a history of probable or confirmed SARS-CoV-2 infection. It typically manifests around three months after symptom onset, enduring for at least two months and evading alternative diagnoses. Symptoms may emerge following the initial recovery from acute SARS-CoV-2 infection or persist from the original illness, exhibiting variations and even recurrences over time, often significantly associated with daily functioning. Notably, sleep disturbances are among these symptoms. Consequently, the implications of our findings acquire heightened significance and broad relevance when considered within the broader scope of investigating the intricate complexities of long COVID and its relationship with individuals’ health and well-being. Finally, as there have been other pandemic waves and related lockdowns since that time, it would be essential to uncover whether sleep parameters have returned to pre-pandemic levels or they have become chronic. High-quality, preferably longitudinal, studies are needed to answer these questions.
5. Conclusions
This systematic review and meta-analysis uncovered noteworthy changes in quantitative sleep parameters in the general population during the first COVID-19 lockdown. In particular, an increase in sleep duration and a significant delay in sleep timing were uncovered. COVID-19 pandemic affected several basic life aspects of the general population, influencing overall health with implications for both the immune system efficacy and successful vaccination. High-quality research based on longitudinal studies is needed to evaluate the prolonged effects of lockdown on these sleep parameters. At the same time, health authorities and professionals are called upon to address the problem of poor sleep hygiene and to implement intervention strategies as an integral part of overall health management.
Author Contributions
Conceptualization, F.L., C.T., F.P. and S.M.; methodology, F.L., P.S., C.T., F.P. and S.M.; formal analysis, P.S.; data screening and data extraction F.L., P.S., E.P. and F.R.; investigation, C.C., F.L., P.S. and C.T.; data curation, F.L. and P.S.; writing—original draft preparation, C.C., F.L. and P.S.; writing—review and editing, C.C., F.L., P.S., C.T., M.N., F.C., S.C., E.D.R., E.P., F.R., F.P. and S.M.; visualization, P:S.; supervision, F.L. and M.N. All authors have read and agreed to the published version of the manuscript.
Funding
S.C. and E.P.’s research fellowship was funded by the Ministero della Salute (Bando di Ricerca Finalizzata Giovani Ricercatori 2016, Grant number GR-2016-02361730).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created in this study. Data sharing is not applicable to this article.
Acknowledgments
We would like to thank Linda Inverso Moretti for reviewing the English version of this manuscript.
Conflicts of Interest
The authors declare no conflicts of interest.
Appendix A

Table A1.
Search strategy: changes in sleep characteristics.
Table A1.
Search strategy: changes in sleep characteristics.
| Databases and Registers | Search Terms |
|---|---|
| PubMed | (sleep[MeSH Terms] OR bedtime * OR “wake time” OR waketime * OR Circadian * OR sleep OR sleeping OR insomnia OR snore OR parasomnia* OR “Life Style”[Mesh] OR lifestyle * OR “life style *”) AND (“COVID 19” OR COVID-19 OR Coronavirus OR 2019-nCoV OR “2019 nCoV” OR “SARS CoV 2” OR SARS-CoV-2 OR “COVID-19”[Mesh] OR “COVID-19 pandemic *” OR “COVID 19 pandemic *”) AND (isolation OR lock-down OR lockdown OR self-isolation OR Confinement OR Containment OR Quarantine OR “Quarantine”[Mesh]) |
| Web of Science | (bedtime * OR “wake time” OR waketime * OR Circadian * OR sleep OR sleeping OR insomnia OR snore OR parasomnia * OR lifestyle * OR “life style*”) AND (“COVID 19” OR COVID-19 OR Coronavirus OR 2019-nCoV OR “2019 nCoV” OR “SARS CoV-2” OR SARS-CoV-2 OR “COVID-19 pandemic *” OR “COVID 19 pandemic *”) AND (isolation OR lock-down OR lockdown OR self-isolation OR Confinement OR Containment OR Quarantine) |
| Cochrane Library | (bedtime * OR “wake time” OR waketime * OR Circadian * OR sleep OR sleeping OR insomnia OR snore OR parasomnia* OR lifestyle * OR “life style *”) AND (“COVID 19” OR “COVID-19” OR Coronavirus OR “2019 nCoV” OR “SARS CoV-2” OR “SARS-CoV-2” OR “COVID-19 pandemic *” OR “COVID 19 pandemic *”) AND (isolation OR lock-down OR lockdown OR self-isolation OR Confinement OR Containment OR Quarantine) |
| EBSCOhost | (bedtime * OR “wake time” OR waketime * OR Circadian * OR sleep OR sleeping OR insomnia OR snore OR parasomnia * OR lifestyle * OR “life style *”) AND (“COVID 19” OR COVID-19 OR Coronavirus OR 2019-nCoV OR “2019 nCoV” OR “SARS CoV 2” OR SARS-CoV-2 OR “COVID-19 pandemic *” OR “COVID 19 pandemic *”) AND (isolation OR lock-down OR lockdown OR self-isolation OR Confinement OR Containment OR Quarantine) |
| MedRxiv * | bedtime bedtimes “wake time” waketime waketimes Circadian Circadians sleep sleeping insomnia snore parasomnia lifestyle lifestyles “life style” “life styles” AND COVID-19 AND lockdown |
| OpenGrey | bedtime bedtimes “wake time” waketime waketimes Circadian Circadians sleep sleeping insomnia snore parasomnia lifestyle lifestyles “life style” “life styles” AND coronavirus AND lockdown |
* In Abstract or Title.

Table A2.
Risk of bias assessment.
Table A2.
Risk of bias assessment.
| Author, Year | Study Design | Selection | Comparability | Outcome | Risk of Bias Score | ||||
|---|---|---|---|---|---|---|---|---|---|
| Abouzid M., 2021 [25] | cross-sectional | c) | b) | c) | b) | c) | a) | 3 | |
| Ahmed S., 2021 [26] | cross-sectional | c) | a) | c) | a) | c) | a) | 4 | |
| Aishworiya R., 2021 [27] | cross-sectional | c) | b) | c) | a) | a)b) | c) | a) | 6 |
| Akbari H.A., 2021 [28] | cross-sectional | c) | a) | c) | a) | a) | c) | a) | 5 |
| Aldhwayan M., 2022 [29] | cross-sectional | c) | b) | c) | b) | a) | c) | a) | 4 |
| Alhusseini N., 2022 [30] | cross-sectional | c) | b) | c) | b) | c) | a) | 3 | |
| Ali A., 2021 [31] | cross-sectional | c) | a) | c) | a) | a)b) | c) | a) | 6 |
| Al-Musharaf S., 2021 [32] | longitudinal | c) | a) | a) | a) | a) | c) | a) | 6 |
| Alomari M.A., 2021 [33] | cross-sectional | c) | a) | c) | b) | c) | a) | 4 | |
| Alrubaysh M.A., 2021 [34] | cross-sectional | c) | b) | c) | b) | c) | a) | 3 | |
| Amerio A., 2021 [35] | cross-sectional | a) | b) | c) | a) | a)b) | c) | a) | 6 |
| AMHSI Research Team, 2021 [36] | longitudinal | c) | a) | a) | a) | c) | a) | 5 | |
| Anastasiou E., 2021 [37] | cross-sectional | c) | a) | b) | a) | a)b) | c) | a) | 7 |
| Antunes R., 2020 [38] | cross-sectional | c) | b) | c) | a) | a)b) | c) | a) | 6 |
| Arrona-Palacios A., 2022 [39] | cross-sectional | c) | b) | c) | b) | a) | c) | a) | 4 |
| Asensio-Cuesta S., 2021 [40] | cross-sectional | c) | b) | b) | a) | a) | c) | a) | 5 |
| Aymerich-Franch L., 2020 [41] | cross-sectional | c) | b) | c) | b) | c) | b) | 2 | |
| Azizi A., 2020 [42] | cross-sectional | c) | b) | b) | a) | c) | a) | 4 | |
| Azuma K., 2021 [43] | cross-sectional | c) | b) | b) | a) | a)b) | c) | a) | 6 |
| Bann D., 2021 [44] | cross-sectional | b) | b) | c) | b) | a)b) | c) | a) | 6 |
| Barbouzas A.E., 2022 [45] | cross-sectional | c) | b) | c) | b) | a) | c) | a) | 4 |
| Bertrand L., 2022 [46] | cross-sectional | c) | b) | c) | a) | c) | a) | 4 | |
| Bigalke J.A., 2020 [47] | cross-sectional | c) | b) | c) | b) | a)b) | c) | a) | 5 |
| Blume C., 2021 [48] | cross-sectional | c) | b) | c) | a) | a)b) | c) | a) | 6 |
| Borisenkov M.F., 2022 [49] | cross-sectional | c) | b) | b) | a) | a) | c) | a) | 5 |
| Bottary R., 2022 [50] | cross-sectional | c) | b) | c) | a) | a) | c) | a) | 5 |
| Bourdas D.I., 2021 [51] | cross-sectional | c) | b) | c) | b) | a)b) | c) | a) | 5 |
| Buoite Stella A., 2021 [52] | cross-sectional | c) | b) | c) | b) | a)b) | b) | a) | 6 |
| Bushnaq T., 2022 [53] | cross-sectional | c) | a) | c) | b) | c) | a) | 4 | |
| Cancello R., 2020 [54] | cross-sectional | c) | b) | c) | c) | c) | a) | 2 | |
| Casas R., 2022 [55] | cross-sectional | c) | b) | c) | b) | c) | a) | 3 | |
| Cellini N., 2020 [56] | cross-sectional | c) | b) | c) | a) | a)b) | c) | b) | 5 |
| Cellini N., 2021 [57] | cross-sectional | c) | b) | c) | b) | a)b) | c) | a) | 5 |
| Celorio-Sardà R., 2021 [58] | cross-sectional | c) | b) | c) | a) | c) | b) | 3 | |
| Cheikh Ismail L., 2020 [60] | cross-sectional | c) | b) | c) | b) | a)b) | c) | a) | 5 |
| Cheikh Ismail L., 2021a [61] | cross-sectional | c) | b) | c) | b) | c) | a) | 3 | |
| Cheikh Ismail L., 2021b [59] | cross-sectional | c) | b) | c) | b) | c) | a) | 3 | |
| Chopra S., 2020 [62] | cross-sectional | c) | b) | c) | b) | c) | a) | 3 | |
| Chouchou F., 2021 [63] | cross-sectional | c) | b) | c) | b) | a) | c) | a) | 4 |
| Conte F., 2021 [64] | cross-sectional | c) | b) | c) | b) | a)b) | c) | a) | 5 |
| Cooper J.A., 2021 [65] | cross-sectional | c) | b) | c) | a) | b) | c) | a) | 5 |
| Csépe P., 2021 [66] | cross-sectional | c) | b) | b) | b) | a) | c) | a) | 4 |
| Curtis R.G., 2021 [67] | longitudinal | c) | a) | a) | b) | a) | a) | 6 | |
| Czeisler M.É., 2021 [69] | cross-sectional | c) | b) | c) | a) | c) | a) | 4 | |
| Czeisler M.E., 2022 [68] | longitudinal | c) | a) | a) | b) | a) | a) | b) | 6 |
| Davy J.P., 2021 [70] | cross-sectional | c) | b) | c) | a) | a)b) | c) | a) | 6 |
| Delgado-Ortiz L., 2022 [71] | cross-sectional | b) | a) | a) | a) | a) | c) | a) | 8 |
| Di Renzo L., 2020 [72] | cross-sectional | c) | b) | b) | a) | c) | a) | 4 | |
| Ding X., 2022 [73] | cross-sectional | b) | b) | b) | a) | a) | c) | a) | 6 |
| Diz-Ferreira E., 2021 [74] | cross-sectional | c) | a) | c) | a) | c) | a) | 4 | |
| Dragun R., 2021 [75] | cross-sectional | c) | b) | c) | a) | b) | c) | a) | 5 |
| Elhadi M., 2021 [76] | cross-sectional | c) | a) | c) | c) | c) | a) | 3 | |
| ElHafeez S.A., 2022 [77] | cross-sectional | c) | a) | c) | a) | a) | c) | a) | 5 |
| Enriquez-Martinez O.G., 2021 [78] | cross-sectional | c) | b) | c) | a) | a) | c) | a) | 5 |
| Esht V., 2021 [79] | cross-sectional | c) | a) | c) | a) | c) | a) | 4 | |
| Falkingham J., 2020 [80] | longitudinal | c) | a) | a) | a) | a)b) | c) | a) | 7 |
| Felician J., 2022 [81] | cross-sectional | c) | b) | a) | a) | a)b) | c) | a) | 7 |
| Flanagan E.W., 2021 [82] | cross-sectional | c) | b) | c) | b) | a)b) | c) | a) | 5 |
| Flores L.E., 2022 [83] | cross-sectional | c) | b) | c) | a) | a) | c) | a) | 5 |
| Franceschini C., 2020 [84] | cross-sectional | c) | b) | c) | a) | a) | c) | a) | 5 |
| Gao C., 2020 [85] | longitudinal | c) | a) | c) | a) | c) | a) | 5 | |
| García-Esquinas E., 2021 [86] | longitudinal | b) | a) | a) | a) | c) | a) | 6 | |
| García-Garro P.A., 2022 [87] | cross-sectional | c) | a) | b) | a) | c) | a) | 5 | |
| Gibson R., 2022 [88] | cross-sectional | c) | b) | b) | a) | a) | c) | a) | 5 |
| González-Calderón M.J., 2022 [89] | cross-sectional | c) | b) | c) | b) | a) | c) | a) | 4 |
| Gornicka M., 2020 [90] | cross-sectional | c) | b) | c) | a) | b) | c) | a) | 5 |
| Gupta R., 2020 [91] | cross-sectional | c) | b) | c) | b) | a)b) | c) | a) | 5 |
| Hernández-Nava R.G., 2022 [92] | cross-sectional | c) | a) | c) | c) | a)b) | c) | a) | 5 |
| Hisler G., 2021 [93] | longitudinal | b) | a) | b) | b) | a)b) | c) | a) | 7 |
| Huancahuire-Vega S., 2021 [94] | cross-sectional | c) | b) | c) | a) | a) | c) | a) | 5 |
| Husain W., 2020 [95] | cross-sectional | c) | a) | c) | a) | c) | a) | 4 | |
| Islam M.A., 2022 [96] | cross-sectional | c) | b) | c) | b) | a) | c) | a) | 4 |
| Janssen X., 2020 [97] | longitudinal | c) | a) | a) | a) | c) | a) | 5 | |
| Jones C., 2021 [98] | cross-sectional | c) | b) | c) | b) | c) | a) | 3 | |
| Joshi D.R., 2023 [99] | cross-sectional | c) | b) | c) | a) | a)b) | c) | a) | 6 |
| Kaizi-Lutu M., 2021 [100] | cross-sectional | c) | b) | c) | b) | c) | a) | 3 | |
| Karahan Yılmaz S., 2020 [101] | cross-sectional | c) | b) | c) | c) | c) | a) | 2 | |
| Khojasteh M.R., 2022 [102] | cross-sectional | c) | a) | a) | b) | c) | a) | 5 | |
| Kholghi M., 2021 [103] | longitudinal | c) | a) | a) | a) | a) | a) | a) | 7 |
| Kim A.C.H., 2022 [104] | cross-sectional | c) | b) | c) | b) | a) | c) | a) | 4 |
| Kolokotroni O., 2021 [105] | cross-sectional | c) | b) | c) | a) | c) | a) | 4 | |
| Kontsevaya A.V., 2021 [106] | cross-sectional | c) | b) | c) | a) | a) | c) | a) | 5 |
| Leone M.J., 2020 [107] | longitudinal | c) | a) | a) | a) | a)b) | c) | a) | 7 |
| Li J.W., 2021 [108] | longitudinal | c) | a) | a) | b) | a) | a) | 6 | |
| Liboredo J.C., 2021 [109] | cross-sectional | c) | b) | c) | a) | c) | a) | 4 | |
| Lopez-Bueno R., 2020 [110] | cross-sectional | c) | b) | c) | a) | a)b) | c) | a) | 6 |
| López-Moreno M., 2020 [111] | cross-sectional | c) | b) | c) | b) | c) | a) | 3 | |
| Luciano F., 2020 [112] | cross-sectional | c) | b) | b) | a) | c) | a) | 4 | |
| Majumdar P., 2020 [113] | cross-sectional | c) | b) | c) | b) | a) | c) | b) | 3 |
| Mandelkorn U., 2021 [114] | cross-sectional | c) | b) | c) | c) | c) | a) | 2 | |
| Marelli S., 2021 [115] | cross-sectional | c) | b) | c) | a) | a)b) | c) | a) | 6 |
| Martínez-Vázquez S.E., 2021 [116] | cross-sectional | c) | a) | c) | b) | c) | a) | 4 | |
| Mititelu M., 2021 [117] | cross-sectional | c) | b) | c) | b) | a) | c) | a) | 4 |
| Mohsin A., 2021 [118] | cross-sectional | a) | b) | c) | b) | c) | b) | 3 | |
| Mónaco E., 2022 [119] | longitudinal | c) | a) | a) | a) | c) | b) | 3 | |
| Morin C.M., 2022 [120] | longitudinal | c) | a) | a) | b) | c) | a) | 5 | |
| Nishijima C., 2021 [121] | cross-sectional | b) | b) | c) | a) | a) | c) | a) | 5 |
| Ong J.L., 2021 [122] | longitudinal | a) | a) | a) | b) | a)b) | a) | a) | 9 |
| Pachocka L., 2022 [123] | cross-sectional | c) | b) | c) | b) | c) | a) | 3 | |
| Panarese P., 2021 [124] | cross-sectional | c) | b) | c) | b) | a) | c) | b) | 3 |
| Pecotić R., 2022 [125] | cross-sectional | c) | b) | c) | a) | a)b) | c) | a) | 6 |
| Pépin J.-L., 2021 [126] | longitudinal | c) | a) | a) | b) | a)b) | a) | a) | 8 |
| Perez-Carbonell L., 2020 [127] | cross-sectional | c) | b) | c) | c) | c) | a) | 2 | |
| Peterson M., 2021 [128] | longitudinal | d) | a) | a) | b) | a) | b) | 5 | |
| Petrov M.E., 2021 [129] | cross-sectional | c) | b) | c) | b) | a)b) | c) | a) | 5 |
| Pisot S., 2020 [130] | cross-sectional | c) | b) | c) | a) | b) | c) | a) | 5 |
| Pitol M.N.S., 2023 [131] | cross-sectional | c) | a) | b) | b) | c) | a) | 4 | |
| Pouget M., 2022 [132] | cross-sectional | c) | b) | c) | a) | c) | a) | 4 | |
| Priego-Parra, 2020 [133] | cross-sectional | c) | b) | c) | a) | a)b) | c) | a) | 6 |
| Rababah T., 2023 [134] | cross-sectional | c) | b) | c) | b) | c) | a) | 3 | |
| Radwan H., 2021 [135] | cross-sectional | c) | b) | b) | a) | a)b) | c) | a) | 6 |
| Ramírez C., 2022 [136] | cross-sectional | c) | b) | c) | a) | a) | c) | a) | 5 |
| Ramos Socarras, 2021 [137] | cross-sectional | c) | b) | c) | a) | a)b) | c) | a) | 6 |
| Reynaud E., 2022 [138] | cross-sectional | c) | b) | c) | b) | c) | a) | 3 | |
| Robinson E., 2020 [139] | cross-sectional | c) | b) | b) | a) | c) | b) | 3 | |
| Rotvold A., 2022 [140] | cross-sectional | c) | b) | c) | b) | c) | a) | 3 | |
| Ruiz-Zaldibar C., 2022 [141] | cross-sectional | c) | a) | b) | a) | a) | c) | a) | 6 |
| Saalwirth C., 2021 [142] | cross-sectional | c) | b) | c) | a) | c) | a) | 4 | |
| Salehinejad M.A., 2020 [143] | cross-sectional | c) | b) | c) | b) | a) | c) | a) | 4 |
| Salfi F., 2021 [144] | cross-sectional | c) | b) | c) | b) | a) | c) | a) | 4 |
| Santos-Miranda E., 2021 [145] | cross-sectional | c) | b) | c) | b) | c) | a) | 3 | |
| Sañudo B., 2020 [146] | longitudinal | c) | a) | a) | a) | c) | a) | 5 | |
| Scarpelli S., 2021 [147] | cross-sectional | c) | b) | b) | b) | c) | a) | 3 | |
| Shahzadi K., 2021 [148] | cross-sectional | c) | b) | c) | b) | c) | b) | 2 | |
| Sheehan C., 2023 [149] | cross-sectional | a) | b) | b) | b) | a)b) | c) | a) | 6 |
| Singh B., 2021 [150] | cross-sectional | c) | b) | c) | a) | c) | a) | 4 | |
| Singh V., 2021 [151] | cross-sectional | c) | b) | c) | b) | c) | b) | 2 | |
| Sinha M., 2020a [152] | cross-sectional | c) | b) | c) | b) | a) | c) | a) | 4 |
| Sinha M., 2020b [153] | cross-sectional | c) | b) | c) | a) | a)b) | c) | a) | 6 |
| Sinisterra Loaiza L.I., 2020 [154] | cross-sectional | c) | b) | b) | a) | c) | b) | 3 | |
| Smith M.L., 2022 [155] | cross-sectional | b) | b) | c) | a) | c) | a) | 4 | |
| Souza T.C., 2022 [156] | cross-sectional | c) | b) | b) | a) | c) | a) | 4 | |
| Storari M., 2021 [157] | cross-sectional | c) | b) | c) | a) | a)b) | c) | a) | 6 |
| Szczepańska E., 2022 [158] | cross-sectional | c) | b) | c) | b) | c) | b) | 2 | |
| Tang N.K.Y., 2022 [159] | cross-sectional | c) | a) | b) | a) | a) | c) | a) | 6 |
| Taporoski T.P., 2022 [160] | longitudinal | a) | a) | a) | a) | a)b) | c) | a) | 7 |
| Trabelsi K., 2021 [161] | cross-sectional | c) | a) | b) | b) | c) | a) | 4 | |
| Trakada A., 2020 [162] | cross-sectional | c) | b) | c) | b) | a)b) | c) | a) | 5 |
| Tsigkas G., 2021 [163] | cross-sectional | b) | b) | b) | a) | c) | a) | 5 | |
| Urquia Y.J.M., 2022 [164] | cross-sectional | c) | b) | c) | b) | a) | c) | a) | 4 |
| Valiensi S.M., 2022 [165] | cross-sectional | c) | b) | b) | a) | c) | a) | 4 | |
| Van der Werf E.T., 2021 [166] | cross-sectional | b) | b) | b) | a) | c) | a) | 5 | |
| Villadsen A., 2020 [167] | longitudinal | b) | a) | a) | a) | a)b) | c) | a) | 8 |
| Villasenor Lopez K., 2021 [168] | cross-sectional | c) | b) | b) | a) | a) | c) | a) | 5 |
| Vinogradov O.O., 2022 [169] | cross-sectional | c) | b) | c) | b) | c) | b) | 2 | |
| Viselli L., 2021 [170] | cross-sectional | b) | b) | c) | b) | c) | a) | 4 | |
| Vollmer C., 2022 [171] | cross-sectional | c) | b) | c) | a) | a)b) | c) | a) | 6 |
| Wang X., 2020 [172] | cross-sectional | c) | b) | c) | b) | a) | c) | a) | 4 |
| Wright K.P., 2020 [173] | longitudinal | b) | a) | a) | b) | a) | c) | a) | 6 |
| Yang G., 2021 [174] | cross-sectional | c) | b) | b) | a) | b) | c) | a) | 5 |
| Yang S., 2020 [175] | longitudinal | c) | a) | a) | a) | a)b) | c) | b) | 6 |
| Zalech M., 2021 [176] | longitudinal | b) | a) | a) | b) | a)b) | c) | a) | 8 |
| Zheng C., 2020 [177] | longitudinal | c) | a) | a) | b) | c) | a) | 5 | |
| Zhu Q., 2021 [178] | cross-sectional | c) | b) | c) | b) | c) | a) | 3 | |
References
- WHO. WHO—Emergency Situation Reports. 2021. Available online: https://www.who.int/emergencies/situation-reports (accessed on 1 January 2023).
- Perra, N. Non-pharmaceutical interventions during the COVID-19 pandemic: A review. Phys. Rep. 2021, 913, 1–52. [Google Scholar] [CrossRef] [PubMed]
- Kupcova, I.; Danisovic, L.; Klein, M.; Harsanyi, S. Effects of the COVID-19 pandemic on mental health, anxiety, and depression. BMC Psychol. 2023, 11, 108. [Google Scholar] [CrossRef]
- Baquerizo-Sedano, L.; Chaquila, J.A.; Aguilar, L.; Ordovás, J.M.; González-Muniesa, P.; Garaulet, M. Anti-COVID-19 measures threaten our healthy body weight: Changes in sleep and external synchronizers of circadian clocks during confinement. Clin. Nutr. 2022, 41, 2988–2995. [Google Scholar] [CrossRef]
- Kalmbach, D.A.; Anderson, J.R.; Drake, C.L. The impact of stress on sleep: Pathogenic sleep reactivity as a vulnerability to insomnia and circadian disorders. J. Sleep Res. 2018, 27, e12710. [Google Scholar] [CrossRef] [PubMed]
- Alimoradi, Z.; Gozal, D.; Tsang, H.W.H.; Lin, C.Y.; Broström, A.; Ohayon, M.M.; Pakpour, A.H. Gender-specific estimates of sleep problems during the COVID-19 pandemic: Systematic review and meta-analysis. J. Sleep Res. 2022, 31, e13432. [Google Scholar] [CrossRef] [PubMed]
- Nochaiwong, S.; Ruengorn, C.; Thavorn, K.; Hutton, B.; Awiphan, R.; Phosuya, C.; Ruanta, Y.; Wongpakaran, N.; Wongpakaran, T. Global prevalence of mental health issues among the general population during the coronavirus disease-2019 pandemic: A systematic review and meta-analysis. Sci. Rep. 2021, 11, 10173. [Google Scholar] [CrossRef] [PubMed]
- Scarpelli, S.; Zagaria, A.; Ratti, P.L.; Albano, A.; Fazio, V.; Musetti, A.; Varallo, G.; Castelnuovo, G.; Plazzi, G.; Franceschini, C. Subjective sleep alterations in healthy subjects worldwide during COVID-19 pandemic: A systematic review, meta-analysis and meta-regression. Sleep Med. 2022, 100, 89–102. [Google Scholar] [CrossRef]
- Jahrami, H.; BaHammam, A.S.; Bragazzi, N.L.; Saif, Z.; Faris, M.; Vitiello, M.V. Sleep problems during the COVID-19 pandemic by population: A systematic review and meta-analysis. J. Clin. Sleep Med. 2021, 17, 299–313. [Google Scholar] [CrossRef]
- AlRasheed, M.M.; Fekih-Romdhane, F.; Jahrami, H.; Pires, G.N.; Saif, Z.; Alenezi, A.F.; Humood, A.; Chen, W.; Dai, H.; Bragazzi, N.; et al. The prevalence and severity of insomnia symptoms during COVID-19: A global systematic review and individual participant data meta-analysis. Sleep Med. 2022, 100, 7–23. [Google Scholar] [CrossRef]
- Limongi, F.; Siviero, P.; Trevisan, C.; Noale, M.; Catalani, F.; Ceolin, C.; Conti, S.; di Rosa, E.; Perdixi, E.; Remelli, F.; et al. Changes in sleep quality and sleep disturbances in the general population from before to during the COVID-19 lockdown: A systematic review and meta-analysis. Front. Psychiatry 2023, 14, 1166815. [Google Scholar] [CrossRef]
- Yuan, R.K.; Zitting, K.M.; Maskati, L.; Huang, J. Increased sleep duration and delayed sleep timing during the COVID-19 pandemic. Sci. Rep. 2022, 12, 10937. [Google Scholar] [CrossRef] [PubMed]
- Robbins, R.; Affouf, M.; Weaver, M.D.; Czeisler, M.É.; Barger, L.K.; Quan, S.F.; Czeisler, C.A. Estimated Sleep Duration Before and during the COVID-19 Pandemic in Major Metropolitan Areas on Different Continents: Observational Study of Smartphone App Data. J. Med. Internet Res. 2021, 23, e20546. [Google Scholar] [CrossRef] [PubMed]
- Rezaei, N.; Grandner, M.A. Changes in sleep duration, timing, and variability during the COVID-19 pandemic: Large-scale Fitbit data from 6 major US cities. Sleep Health 2021, 7, 303–313. [Google Scholar] [CrossRef] [PubMed]
- Al-Ajlouni, Y.A.; Al Ta’ani, O.; Shamaileh, G.; Mushasha, R.; Makarem, N.; Duncan, D.T. Effects of the COVID-19 pandemic on sleep health among Middle Eastern and North African (MENA) populations: A systematic review of the literature. BMJ Open 2022, 12, e066964. [Google Scholar] [CrossRef] [PubMed]
- Cui, D.; Zhang, X.; Guo, J. The impact of the COVID-19 pandemic on physical activity and sleep among healthy adults: A systematic review and meta-analysis. Front. Psychol. 2023, 14, 1149215. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Wells, G.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V. The Newcastle-Ottawa Scale (NOS) for assessing the quality of case-control studies in meta-analyses. Eur. J. Epidemiol. 2011, 25, 603–605. [Google Scholar]
- Modesti, P.A.; Reboldi, G.; Cappuccio, F.P.; Agyemang, C.; Remuzzi, G.; Rapi, S.; Perruolo, E.; Parati, G.; ESH Working Group on CV Risk in Low Resource Settings. Panethnic Differences in Blood Pressure in Europe: A Systematic Review and Meta-Analysis. PLoS ONE 2016, 11, e0147601. [Google Scholar] [CrossRef] [PubMed]
- Luchini, C.; Stubbs, B.; Solmi, M.; Veronese, N. Assessing the quality of studies in meta-analyses: Advantages and limitations of the Newcastle Ottawa Scale. World J. Meta-Anal. 2017, 5, 80. [Google Scholar] [CrossRef]
- MedCalc Software Ltd, Ostend, Belgium. 2022. Available online: https://www.medcalc.org (accessed on 1 January 2023).
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 1988. [Google Scholar]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef]
- Egger, M.; Davey Smith, G.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef] [PubMed]
- Abouzid, M.; El-Sherif, D.M.; Eltewacy, N.K.; Dahman, N.B.H.; Okasha, S.A.; Ghozy, S.; Islam, S.M.S.; EARG Collaborators. Influence of COVID-19 on lifestyle behaviors in the Middle East and North Africa Region: A survey of 5896 individuals. J. Transl. Med. 2021, 19, 129. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.; Akter, R.; Islam, M.J.; Muthalib, A.A.; Sadia, A.A. Impact of lockdown on musculoskeletal health due to COVID-19 outbreak in Bangladesh: A cross sectional survey study. Heliyon 2021, 7, e07335. [Google Scholar] [CrossRef] [PubMed]
- Aishworiya, R.; Lim, M.T.C.; Ramamurthy, M.B.; Tran, A.P.; Rajgor, D.D.; Goh, D.Y.T. Impact of work routines on parents’ and children’s sleep during the COVID-19 pandemic lockdown. Sleep Med. 2021, 88, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Akbari, H.A.; Pourabbas, M.; Yoosefi, M.; Briki, W.; Attaran, S.; Mansoor, H.; Moalla, W.; Damak, M.; Dergaa, I.; Teixeira, A.L.; et al. How physical activity behavior affected well-being, anxiety and sleep quality during COVID-19 restrictions in Iran. Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 7847–7857. [Google Scholar] [CrossRef] [PubMed]
- Aldhwayan, M.; Alabdulkader, B. The impact of precautionary lockdown measures during COVID-19 on eating behaviour and lifestyle. Prog. Nutr. 2022, 24, e2022055. [Google Scholar] [CrossRef]
- Alhusseini, N.; Alammari, D.; Ramadan, M.; Ziadeh, N.; Zyadeh, Z.; Alshamrani, J.; Qasim, H.; Alamri, N.; Alqahtani, S.A. The impact of COVID-19 pandemic on lifestyle among the Saudi population. J. Public Health Res. 2022, 11, 22799036221123156. [Google Scholar] [CrossRef] [PubMed]
- Ali, A.; Siddiqui, A.A.; Arshad, M.S.; Iqbal, F.; Arif, T.B. Effects of COVID-19 pandemic and lockdown on lifestyle and mental health of students: A retrospective study from Karachi, Pakistan. Ann. Med. Psychol. 2022, 180, S29–S37. [Google Scholar] [CrossRef] [PubMed]
- Al-Musharaf, S.; Aljuraiban, G.; Bogis, R.; Alnafisah, R.; Aldhwayan, M.; Tahrani, A. Lifestyle changes associated with COVID-19 quarantine among young Saudi women: A prospective study. PLoS ONE 2021, 16, e0250625. [Google Scholar] [CrossRef]
- Alomari, M.A.; Alzoubi, K.H.; Khabour, O.F.; Darabseh, M.Z. Sleeping habits during COVID-19 induced confinement: A study from Jordan. Heliyon 2021, 7, e08545. [Google Scholar] [CrossRef]
- Alrubaysh, M.A.; Alkahtani, A.A.; Alluwaymi, Z.S.; Alanazi, S.M.; Alanazi, A.M.; Al Harbi, K.M. Lifestyle changes that can increase the risk of cardiovascular disease during the COVID-19 pandemic: A cross-sectional study. Middle East J. Fam. Med. 2021, 19, 44–53. [Google Scholar]
- Amerio, A.; Lugo, A.; Stival, C.; Fanucchi, T.; Gorini, G.; Pacifici, R.; Odone, A.; Serafini, G.; Gallus, S. COVID-19 lockdown impact on mental health in a large representative sample of Italian adults. J. Affect. Disord. 2021, 292, 398–404. [Google Scholar] [CrossRef] [PubMed]
- AMHSI Research Team; Milken Research Team; Roitblat, Y.; Burger, J.; Vaiman, M.; Nehuliaieva, L.; Buchris, N.; Shterenshis, M. Owls and larks do not exist: COVID-19 quarantine sleep habits. Sleep Med. 2021, 77, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Anastasiou, E.; Duquenne, M.N. What about the “Social Aspect of COVID”? Exploring the Determinants of Social Isolation on the Greek Population during the COVID-19 Lockdown. Soc. Sci. 2021, 10, 27. [Google Scholar] [CrossRef]
- Antunes, R.; Frontini, R.; Amaro, N.; Salvador, R.; Matos, R.; Morouço, P.; Rebelo-Gonçalves, R. Exploring Lifestyle Habits, Physical Activity, Anxiety and Basic Psychological Needs in a Sample of Portuguese Adults during COVID-19. Int. J. Environ. Res. Public. Health 2020, 17, 4360. [Google Scholar] [CrossRef] [PubMed]
- Arrona-Palacios, A.; Rebolledo-Mendez, G.; Escamilla, J.; Hosseini, S.; Duffy, J. Effects of COVID-19 lockdown on sleep duration, sleep quality and burnout in faculty members of higher education in Mexico. Ciência Saúde Coletiva 2022, 27, 2985–2993. [Google Scholar] [CrossRef] [PubMed]
- Asensio-Cuesta, S.; Blanes-Selva, V.; Portolés, M.; Conejero, J.A.; García-Gómez, J.M. How the Wakamola chatbot studied a university community’s lifestyle during the COVID-19 confinement. Health Inform. J. 2021, 27, 14604582211017944. [Google Scholar] [CrossRef]
- Aymerich-Franch, L. COVID-19 lockdown: Impact on psychological well-being and relationship to habit and routine modifications. psyarxiv 2020. [Google Scholar] [CrossRef]
- Azizi, A.; Achak, D.; Aboudi, K.; Saad, E.; Nejjari, C.; Nouira, Y.; Hilali, A.; Youlyouz-Marfak, I.; Marfak, A. Health-related quality of life and behavior-related lifestyle changes due to the COVID-19 home confinement: Dataset from a Moroccan sample. Data Brief 2020, 32, 106239. [Google Scholar] [CrossRef]
- Azuma, K.; Nojiri, T.; Kawashima, M.; Hanai, A.; Ayaki, M.; Tsubota, K.; TRF-Japan Study Group. Possible favorable lifestyle changes owing to the coronavirus disease 2019 (COVID-19) pandemic among middle-aged Japanese women: An ancillary survey of the TRF-Japan study using the original “Taberhythm” smartphone app. PLoS ONE 2021, 16, e0248935. [Google Scholar] [CrossRef]
- Bann, D.; Villadsen, A.; Maddock, J.; Hughes, A.; Ploubidis, G.B.; Silverwood, R.; Patalay, P. Changes in the behavioural determinants of health during the COVID-19 pandemic: Gender, socioeconomic and ethnic inequalities in five British cohort studies. J. Epidemiol. Community Health 2021, 75, 1136–1142. [Google Scholar] [CrossRef]
- Barbouzas, A.E.; Malli, F.; Daniil, Z.; Gourgoulianis, K. Long-Term Impact of COVID-19 Pandemic in Sleep Quality and Lifestyle in Young Adults. Int. J. Environ. Res. Public. Health 2022, 19, 12333. [Google Scholar] [CrossRef]
- Bertrand, L.; Schröder, C.; Bourgin, P.; Maruani, J.; Atoui, Y.; d’Ortho, M.P.; Lejoyeux, M.; Geoffroy, P.A. Sleep and circadian rhythm characteristics in individuals from the general population during the French COVID-19 full lockdown. J. Sleep Res. 2022, 31, e13480. [Google Scholar] [CrossRef]
- Bigalke, J.A.; Greenlund, I.M.; Carter, J.R. Sex differences in self-report anxiety and sleep quality during COVID-19 stay-at-home orders. Biol. Sex Differ. 2020, 11, 56. [Google Scholar] [CrossRef]
- Blume, C.; Schmidt, M.H.; Cajochen, C. Effects of the COVID-19 lockdown on human sleep and rest-activity rhythms. Curr. Biol. 2020, 30, R795–R797. [Google Scholar] [CrossRef] [PubMed]
- Borisenkov, M.F.; Popov, S.V.; Smirnov, V.V.; Gubin, D.G.; Petrov, I.M.; Vasilkova, T.N.; Solovieva, S.V.; Martinson, E.A.; Pecherkina, A.A.; Dorogina, O.I.; et al. Associations among sleep-wake rhythm characteristics, time perspective and psycho-emotional state during COVID-19 isolation. Biol. Rhythm. Res. 2022, 53, 1770–1781. [Google Scholar] [CrossRef]
- Bottary, R.; Fields, E.C.; Kensinger, E.A.; Cunningham, T.J. Age and chronotype influenced sleep timing changes during the first wave of the COVID-19 pandemic. J. Sleep Res. 2022, 31, e13495. [Google Scholar] [CrossRef] [PubMed]
- Bourdas, D.I.; Zacharakis, E.D.; Travlos, A.K.; Souglis, A.; Georgali, T.I.; Gofas, D.C.; Ktistakis, I.E.; Deltsidou, A. Impact of lockdown on smoking and sleeping in the early COVID-19 presence: Datasets of Greek Adults sample. Data Brief 2021, 39, 107480. [Google Scholar] [CrossRef]
- Buoite Stella, A.; AjČeviĆ, M.; Furlanis, G.; Cillotto, T.; Menichelli, A.; Accardo, A.; Manganotti, P. Smart technology for physical activity and health assessment during COVID-19 lockdown. J. Sports Med. Phys. Fit. 2021, 61, 452–460. [Google Scholar] [CrossRef]
- Bushnaq, T.; Algheshairy, R.M.; Almujaydil, M.S.; Malki, A.A.; Alharbi, H.F.; Barakat, H. Dietary Habits and Lifestyle Behaviors of Saudi Residents during the COVID-19 Pandemic: A Cross-Sectional Study. Int. J. Environ. Res. Public. Health 2022, 19, 7659. [Google Scholar] [CrossRef]
- Cancello, R.; Soranna, D.; Zambra, G.; Zambon, A.; Invitti, C. Determinants of the Lifestyle Changes during COVID-19 Pandemic in the Residents of Northern Italy. Int. J. Environ. Res. Public. Health 2020, 17, 6287. [Google Scholar] [CrossRef]
- Casas, R.; Raidó-Quintana, B.; Ruiz-León, A.M.; Castro-Barquero, S.; Bertomeu, I.; Gonzalez-Juste, J.; Campolier, M.; Estruch, R. Changes in Spanish lifestyle and dietary habits during the COVID-19 lockdown. Eur. J. Nutr. 2022, 61, 2417–2434. [Google Scholar] [CrossRef]
- Cellini, N.; Canale, N.; Mioni, G.; Costa, S. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J. Sleep Res. 2020, 29, e13074. [Google Scholar] [CrossRef]
- Cellini, N.; Conte, F.; De Rosa, O.; Giganti, F.; Malloggi, S.; Reyt, M.; Guillemin, C.; Schmidt, C.; Muto, V.; Ficca, G. Changes in sleep timing and subjective sleep quality during the COVID-19 lockdown in Italy and Belgium: Age, gender and working status as modulating factors. Sleep Med. 2021, 77, 112–119. [Google Scholar] [CrossRef]
- Celorio-Sardà, R.; Comas-Basté, O.; Latorre-Moratalla, M.L.; Zerón-Rugerio, M.F.; Urpi-Sarda, M.; Illán-Villanueva, M.; Farran-Codina, A.; Izquierdo-Pulido, M.; Vidal-Carou, M.D.C. Effect of COVID-19 Lockdown on Dietary Habits and Lifestyle of Food Science Students and Professionals from Spain. Nutrients 2021, 13, 1494. [Google Scholar] [CrossRef]
- Cheikh Ismail, L.; Hashim, M.; Mohamad, M.N.; Hassan, H.; Ajab, A.; Stojanovska, L.; Jarrar, A.H.; Hasan, H.; Abu Jamous, D.O.; Saleh, S.T.; et al. Dietary Habits and Lifestyle During Coronavirus Pandemic Lockdown: Experience From Lebanon. Front. Nutr. 2021, 8, 730425. [Google Scholar] [CrossRef]
- Cheikh Ismail, L.; Osaili, T.M.; Mohamad, M.N.; Al Marzouqi, A.; Jarrar, A.H.; Abu Jamous, D.O.; Magriplis, E.; Ali, H.I.; Al Sabbah, H.; Hasan, H.; et al. Eating Habits and Lifestyle during COVID-19 Lockdown in the United Arab Emirates: A Cross-Sectional Study. Nutrients 2020, 12, 3314. [Google Scholar] [CrossRef]
- Cheikh Ismail, L.; Osaili, T.M.; Mohamad, M.N.; Al Marzouqi, A.; Jarrar, A.H.; Zampelas, A.; Habib-Mourad, C.; Omar Abu Jamous, D.; Ali, H.I.; Al Sabbah, H.; et al. Assessment of eating habits and lifestyle during the coronavirus 2019 pandemic in the Middle East and North Africa region: A cross-sectional study. Br. J. Nutr. 2021, 126, 757–766. [Google Scholar] [CrossRef]
- Chopra, S.; Ranjan, P.; Singh, V.; Kumar, S.; Arora, M.; Hasan, M.S.; Kasiraj, R.; Suryansh; Kaur, D.; Vikram, N.K.; et al. Impact of COVID-19 on lifestyle-related behaviours- a cross-sectional audit of responses from nine hundred and ninety-five participants from India. Diabetes Metab. Syndr. 2020, 14, 2021–2030. [Google Scholar] [CrossRef]
- Chouchou, F.; Augustini, M.; Caderby, T.; Caron, N.; Turpin, N.A.; Dalleau, G. The importance of sleep and physical activity on well-being during COVID-19 lockdown: Reunion island as a case study. Sleep Med. 2021, 77, 297–301. [Google Scholar] [CrossRef]
- Conte, F.; Cellini, N.; De Rosa, O.; Rescott, M.L.; Malloggi, S.; Giganti, F.; Ficca, G. Dissociated profiles of sleep timing and sleep quality changes across the first and second wave of the COVID-19 pandemic. J. Psychiatr. Res. 2021, 143, 222–229. [Google Scholar] [CrossRef] [PubMed]
- Cooper, J.A.; vanDellen, M.; Bhutani, S. Self-weighing Practices and Associated Health Behaviors during COVID-19. Am. J. Health Behav. 2021, 45, 17–30. [Google Scholar] [CrossRef] [PubMed]
- Csépe, P.; Dinya, E.; Balázs, P.; Hosseini, S.M.; Küzdy, G.; Rosivall, L. Impact of the first wave of COVID-19 pandemic on the Hungarian university students’ social and health behaviour. J. Public Health 2021, 31, 999–1005. [Google Scholar] [CrossRef] [PubMed]
- Curtis, R.G.; Olds, T.; Ferguson, T.; Fraysse, F.; Dumuid, D.; Esterman, A.; Hendrie, G.A.; Brown, W.J.; Lagiseti, R.; Maher, C.A. Changes in diet, activity, weight, and wellbeing of parents during COVID-19 lockdown. PLoS ONE 2021, 16, e0248008. [Google Scholar] [CrossRef]
- Czeisler, M.É.; Capodilupo, E.R.; Weaver, M.D.; Czeisler, C.A.; Howard, M.E.; Rajaratnam, S.M.W. Prior sleep-wake behaviors are associated with mental health outcomes during the COVID-19 pandemic among adult users of a wearable device in the United States. Sleep Health 2022, 8, 311–321. [Google Scholar] [CrossRef] [PubMed]
- Czeisler, M.É.; Wiley, J.F.; Facer-Childs, E.R.; Robbins, R.; Weaver, M.D.; Barger, L.K.; Czeisler, C.A.; Howard, M.E.; Rajaratnam, S.M.W. Mental health, substance use, and suicidal ideation during a prolonged COVID-19-related lockdown in a region with low SARS-CoV-2 prevalence. J. Psychiatr. Res. 2021, 140, 533–544. [Google Scholar] [CrossRef]
- Davy, J.P.; Scheuermaier, K.; Roden, L.C.; Christie, C.J.; Bentley, A.; Gomez-Olive, F.X.; Iacovides, S.; Lewis, R.; Lipinska, G.; Roche, J.; et al. The COVID-19 Lockdown and Changes in Routine-Oriented Lifestyle Behaviors and Symptoms of Depression, Anxiety, and Insomnia in South Africa. J. Phys. Act. Health 2021, 18, 1046–1057. [Google Scholar] [CrossRef] [PubMed]
- Delgado-Ortiz, L.; Carsin, A.E.; Merino, J.; Cobo, I.; Koch, S.; Goldberg, X.; Chevance, G.; Bosch de Basea, M.; Castaño-Vinyals, G.; Espinosa, A.; et al. Changes in Population Health-Related Behaviors During a COVID-19 Surge: A Natural Experiment. Ann. Behav. Med. 2023, 57, 216–226. [Google Scholar] [CrossRef]
- Di Renzo, L.; Gualtieri, P.; Pivari, F.; Soldati, L.; Attinà, A.; Cinelli, G.; Leggeri, C.; Caparello, G.; Barrea, L.; Scerbo, F.; et al. Eating habits and lifestyle changes during COVID-19 lockdown: An Italian survey. J. Transl. Med. 2020, 18, 229. [Google Scholar] [CrossRef]
- Ding, X.; Brazel, D.M.; Mills, M.C. Gender differences in sleep disruption during COVID-19: Cross-sectional analyses from two UK nationally representative surveys. BMJ Open 2022, 12, e055792. [Google Scholar] [CrossRef]
- Diz-Ferreira, E.; Díaz-Vidal, P.; Da Cunha Soares Nicolau, M.L.; Criado-Santos, M.P.; Ayán, C.; Diz, J.C. Effect of confinement during COVID-19 outbreak on sleep quality in Galicia. Rev. Española Salud Pública 2021, 95, e202101001. [Google Scholar]
- Dragun, R.; Veček, N.N.; Marendić, M.; Pribisalić, A.; Đivić, G.; Cena, H.; Polašek, O.; Kolčić, I. Have Lifestyle Habits and Psychological Well-Being Changed among Adolescents and Medical Students Due to COVID-19 Lockdown in Croatia? Nutrients 2020, 13, 97. [Google Scholar] [CrossRef] [PubMed]
- Elhadi, M.; Alsoufi, A.; Msherghi, A.; Alshareea, E.; Ashini, A.; Nagib, T.; Abuzid, N.; Abodabos, S.; Alrifai, H.; Gresea, E.; et al. Psychological Health, Sleep Quality, Behavior, and Internet Use Among People During the COVID-19 Pandemic: A Cross-Sectional Study. Front. Psychiatry 2021, 12, 632496. [Google Scholar] [CrossRef] [PubMed]
- Abd ElHafeez, S.; E Cruz, M.M.; Gouda, S.; Nofal, M.; Fayed, A.; Ghazy, R.M.; Mekky, J. Sleep quality and anxiety among Egyptian population during COVID-19 pandemic. Sleep Sci. 2022, 15, 8–16. [Google Scholar] [CrossRef] [PubMed]
- Enriquez-Martinez, O.G.; Martins, M.C.T.; Pereira, T.S.S.; Pacheco, S.O.S.; Pacheco, F.J.; Lopez, K.V.; Huancahuire-Vega, S.; Silva, D.A.; Mora-Urda, A.I.; Rodriguez-Vásquez, M.; et al. Diet and Lifestyle Changes During the COVID-19 Pandemic in Ibero-American Countries: Argentina, Brazil, Mexico, Peru, and Spain. Front. Nutr. 2021, 8, 671004. [Google Scholar] [CrossRef] [PubMed]
- Esht, V.; Quraishi, S.; Ghosalkar, H.R.; Sharma, S.; Atri, G. A Web-Based Survey of COVID-19 Pandemic and its Impact on Physical, Recreational, Mental Health and Socio-Economic Factors of General Population of India. Biosci. Biotechnol. Res. Commun. 2021, 14, 227–235. [Google Scholar] [CrossRef]
- Falkingham, J.C.; Evandrou, M.; Qin, M.; Vlachantoni, A. Prospective longitudinal study of ‘Sleepless in Lockdown’: Unpacking differences in sleep loss during the coronavirus pandemic in the UK. BMJ Open 2022, 12, e053094. [Google Scholar] [CrossRef]
- Felician, J.; Galvao, F.; Lefebvre, M.; Nourredine, M.; Peter-Derex, L. Association of Delayed Sleep/Wake Rhythm with Depression During the First COVID-19 Lockdown in France. Nat. Sci. Sleep 2022, 14, 1545–1557. [Google Scholar] [CrossRef]
- Flanagan, E.W.; Beyl, R.A.; Fearnbach, S.N.; Altazan, A.D.; Martin, C.K.; Redman, L.M. The Impact of COVID-19 Stay-at-Home Orders on Health Behaviors in Adults. Obesity 2021, 29, 438–445. [Google Scholar] [CrossRef]
- Flores, L.E.; Elgart, J.F.; Abraham, A.G.; Garrote, G.L.; Torrieri, R.; Cepeda, A.; Cardelle-Cobas, A.; Gagliardino, J.J. Changes in lifestyle behaviors during COVID-19 isolation in Argentina: A cross-sectional study. Nutr. Health 2022, 12, 2601060221127115. [Google Scholar] [CrossRef]
- Franceschini, C.; Musetti, A.; Zenesini, C.; Palagini, L.; Scarpelli, S.; Quattropani, M.C.; Lenzo, V.; Freda, M.F.; Lemmo, D.; Vegni, E.; et al. Poor Sleep Quality and Its Consequences on Mental Health During the COVID-19 Lockdown in Italy. Front. Psychol. 2020, 11, 574475. [Google Scholar] [CrossRef]
- Gao, C.; Scullin, M.K. Sleep health early in the coronavirus disease 2019 (COVID-19) outbreak in the United States: Integrating longitudinal, cross-sectional, and retrospective recall data. Sleep Med 2020, 73, 1–10. [Google Scholar] [CrossRef]
- García-Esquinas, E.; Ortolá, R.; Gine-Vázquez, I.; Carnicero, J.A.; Mañas, A.; Lara, E.; Alvarez-Bustos, A.; Vicente-Rodriguez, G.; Sotos-Prieto, M.; Olaya, B.; et al. Changes in Health Behaviors, Mental and Physical Health among Older Adults under Severe Lockdown Restrictions during the COVID-19 Pandemic in Spain. Int. J. Environ. Res. Public. Health 2021, 18, 7067. [Google Scholar] [CrossRef]
- García-Garro, P.A.; Aibar-Almazán, A.; Rivas-Campo, Y.; Vega-Ávila, G.C.; Afanador-Restrepo, D.F.; Hita-Contreras, F. Influence of the COVID-19 Pandemic on Quality of Life, Mental Health, and Level of Physical Activity in Colombian University Workers: A Longitudinal Study. J. Clin. Med. 2022, 11, 4104. [Google Scholar] [CrossRef]
- Gibson, R.; Shetty, H.; Carter, M.; Münch, M. Sleeping in a bubble: Factors affecting sleep during New Zealand’s COVID-19 lockdown. Sleep Adv. 2022, 3, zpac017. [Google Scholar] [CrossRef]
- González-Calderón, M.J.; Baile, J.I.; Izquierdo-Sotorrío, E. A Comparative Cross-Sectional Study of the Consequences of the COVID-19 Lockdown on Women’s Health Behaviors in Spain. Nutrients 2022, 14, 846. [Google Scholar] [CrossRef]
- Górnicka, M.; Drywień, M.E.; Zielinska, M.A.; Hamułka, J. Dietary and Lifestyle Changes During COVID-19 and the Subsequent Lockdowns among Polish Adults: A Cross-Sectional Online Survey PLifeCOVID-19 Study. Nutrients 2020, 12, 2324. [Google Scholar] [CrossRef]
- Gupta, R.; Grover, S.; Basu, A.; Krishnan, V.; Tripathi, A.; Subramanyam, A.; Nischal, A.; Hussain, A.; Mehra, A.; Ambekar, A.; et al. Changes in sleep pattern and sleep quality during COVID-19 lockdown. Indian J. Psychiatry 2020, 62, 370–378. [Google Scholar] [CrossRef]
- Hernández-Nava, R.G.; de la Luz Sánchez-Mundo, M.; García-Barrientos, R.; Espinosa-Solis, V.; Villalobos-Aguayo, P.; Salmerón-Muñiz, N.N.; Anaya-Tacuba, J.D. Lifestyle Changes among Mexican People during the COVID-19 Lockdown in 2020: A Cross-Sectional Study. Healthcare 2022, 10, 2537. [Google Scholar] [CrossRef]
- Hisler, G.C.; Twenge, J.M. Sleep characteristics of U.S. adults before and during the COVID-19 pandemic. Soc. Sci. Med. 2021, 276, 113849. [Google Scholar] [CrossRef]
- Huancahuire-Vega, S.; Newball-Noriega, E.E.; Rojas-Humpire, R.; Saintila, J.; Rodriguez-Vásquez, M.; Ruiz-Mamani, P.G.; Morales-García, W.C.; White, M. Changes in Eating Habits and Lifestyles in a Peruvian Population during Social Isolation for the COVID-19 Pandemic. J. Nutr. Metab. 2021, 2021, 4119620. [Google Scholar] [CrossRef]
- Husain, W.; Ashkanani, F. Does COVID-19 change dietary habits and lifestyle behaviours in Kuwait: A community-based cross-sectional study. Environ. Health Prev. Med. 2020, 25, 61. [Google Scholar] [CrossRef] [PubMed]
- Islam, M.A.; Nahar, M.T.; Ibn Anik, S.M.F.; Barna, S.D.; Hossain, M.T. Changes in dietary patterns among Bangladeshi adult population during the COVID-19 pandemic: A web-based cross-sectional study. Heliyon 2022, 8, e10349. [Google Scholar] [CrossRef] [PubMed]
- Janssen, X.; Fleming, L.; Kirk, A.; Rollins, L.; Young, D.; Grealy, M.; MacDonald, B.; Flowers, P.; Williams, L. Changes in Physical Activity, Sitting and Sleep across the COVID-19 National Lockdown Period in Scotland. Int. J. Environ. Res. Public. Health 2020, 17, 9362. [Google Scholar] [CrossRef] [PubMed]
- Jones, C.; Kaizi-Lutu, M.; Cordoza, M.; Mange, A.; Dinges, D. 226 Changes in sleep amount and sleep quality due to the COVID-19 pandemic confinement associate with ratings of health and stress. Sleep 2021, 44 (Suppl. S2), A90. [Google Scholar] [CrossRef]
- Joshi, D.R.; Neupane, U.; Singh, J.K.; Khanal, B.; Belbase, S. Impact of COVID-19 Pandemic on Academic Activities of Academicians in Nepal. J. Educ. 2023, 204, 439–454. [Google Scholar] [CrossRef]
- Kaizi-Lutu, M.; Dinges, D.; Cordoza, M.; Jones, C.; Mange, A. 215 Sleep duration, quality and timing during confinement amid the COVID-19 Pandemic. Sleep 2021, 44 (Suppl. S2), A86. [Google Scholar] [CrossRef]
- Karahan Yılmaz, S.; Eskici, G. Evaluation of emotional (depression) and behavioural (nutritional, physical activity and sleep) status of Turkish adults during the COVID-19 pandemic period. Public. Health Nutr. 2021, 24, 942–949. [Google Scholar] [CrossRef] [PubMed]
- Khojasteh, M.R.; Khadem-Rezaiyan, M. Evaluation of Sleep Quality before and During COVID-19 Quarantine and Its Relationship with Family Social Support: A Web-based Survey among University Students. Iran. J. Psychiatry Behav. Sci. 2022, 16, e123447. [Google Scholar] [CrossRef]
- Kholghi, M.; Ellender, C.M.; Zhang, Q.; Gao, Y.; Higgins, L.; Karunanithi, M. Home-Based Sleep Sensor Measurements in an Older Australian Population: Before and during a Pandemic. Sensors 2021, 21, 5993. [Google Scholar] [CrossRef]
- Kim, A.C.H.; Du, J.; Andrew, D.P.S. Changes in Physical Activity and Depressive Symptoms During COVID-19 Lockdown: United States Adult Age Groups. Front. Psychol. 2022, 13, 769930. [Google Scholar] [CrossRef]
- Kolokotroni, O.; Mosquera, M.C.; Quattrocchi, A.; Heraclides, A.; Demetriou, C.; Philippou, E. Lifestyle habits of adults during the COVID-19 pandemic lockdown in Cyprus: Evidence from a cross-sectional study. BMC Public. Health 2021, 21, 786. [Google Scholar] [CrossRef]
- Kontsevaya, A.V.; Mukaneeva, D.K.; Myrzamatova, A.O.; Okely, A.D.; Drapkina, O.M. Changes in physical activity and sleep habits among adults in Russian Federation during COVID-19: A cross-sectional study. BMC Public. Health 2021, 21, 893. [Google Scholar] [CrossRef] [PubMed]
- Leone, M.J.; Sigman, M.; Golombek, D.A. Effects of lockdown on human sleep and chronotype during the COVID-19 pandemic. Curr. Biol. 2020, 30, R930–R931. [Google Scholar] [CrossRef]
- Li, J.W.; Guo, Y.T.; Di Tanna, G.L.; Neal, B.; Chen, Y.D.; Schutte, A.E. Vital Signs During the COVID-19 Outbreak: A Retrospective Analysis of 19,960 Participants in Wuhan and Four Nearby Capital Cities in China. Glob. Heart 2021, 16, 47. [Google Scholar] [CrossRef]
- Liboredo, J.C.; Anastácio, L.R.; Ferreira, L.G.; Oliveira, L.A.; Della Lucia, C.M. Quarantine During COVID-19 Outbreak: Eating Behavior, Perceived Stress, and Their Independently Associated Factors in a Brazilian Sample. Front. Nutr. 2021, 8, 704619. [Google Scholar] [CrossRef] [PubMed]
- López-Bueno, R.; Calatayud, J.; Casaña, J.; Casajús, J.A.; Smith, L.; Tully, M.A.; Andersen, L.L.; López-Sánchez, G.F. COVID-19 Confinement and Health Risk Behaviors in Spain. Front. Psychol. 2020, 11, 1426. [Google Scholar] [CrossRef] [PubMed]
- López-Moreno, M.; López, M.T.I.; Miguel, M.; Garcés-Rimón, M. Physical and Psychological Effects Related to Food Habits and Lifestyle Changes Derived from COVID-19 Home Confinement in the Spanish Population. Nutrients 2020, 12, 3445. [Google Scholar] [CrossRef]
- Luciano, F.; Cenacchi, V.; Vegro, V.; Pavei, G. COVID-19 lockdown: Physical activity, sedentary behaviour and sleep in Italian medicine students. Eur. J. Sport Sci. 2021, 21, 1459–1468. [Google Scholar] [CrossRef]
- Majumdar, P.; Biswas, A.; Sahu, S. COVID-19 pandemic and lockdown: Cause of sleep disruption, depression, somatic pain, and increased screen exposure of office workers and students of India. Chronobiol. Int. 2020, 37, 1191–1200. [Google Scholar] [CrossRef]
- Mandelkorn, U.; Genzer, S.; Choshen-Hillel, S.; Reiter, J.; Meira E Cruz, M.; Hochner, H.; Kheirandish-Gozal, L.; Gozal, D.; Gileles-Hillel, A. Escalation of sleep disturbances amid the COVID-19 pandemic: A cross-sectional international study. J. Clin. Sleep Med. 2021, 17, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Marelli, S.; Castelnuovo, A.; Somma, A.; Castronovo, V.; Mombelli, S.; Bottoni, D.; Leitner, C.; Fossati, A.; Ferini-Strambi, L. Impact of COVID-19 lockdown on sleep quality in university students and administration staff. J. Neurol. 2021, 268, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Vázquez, S.E.; Ceballos-Rasgado, M.; Posada-Velázquez, R.; Hunot-Alexander, C.; Nava-González, E.J.; Ramírez-Silva, I.; Aguilar-López, D.K.; Quiroz-Olguín, G.; López-Jara, B.; Delgado-de-la-Cruz, C.; et al. Perceived Diet Quality, Eating Behaviour, and Lifestyle Changes in a Mexican Population with Internet Access during Confinement for the COVID-19 Pandemic: ESCAN-COVID19Mx Survey. Nutrients 2021, 13, 4256. [Google Scholar] [CrossRef]
- Mititelu, M.; Stanciu, T.I.; Udeanu, D.I.; Popa, D.E.; Drăgănescu, D.; Cobelschi, C.; Grigore, N.D.; Pop, A.L.; Ghica, M. The impact of COVID-19 lockdown on the lifestyle and dietary patterns among Romanian population. Farmacia 2021, 69, 1–11. [Google Scholar] [CrossRef]
- Mohsin, A.; Riaz, J.; Ahmad, S.A. Potential Physical Health Changes during the Covid-19 Confinement in Pakistan. Pak. J. Med. Health Sci. 2021, 15, 1365–1367. [Google Scholar] [CrossRef]
- Mónaco, E.; Zaragozá, M.; Montoya-Castilla, I. Sleep and emotions: How much are they affected by confinement due to COVID-19? A longitudinal study. Int. J. Psychiatry Clin. Pr. 2023, 27, 8–17. [Google Scholar] [CrossRef]
- Morin, C.M.; Vézina-Im, L.A.; Ivers, H.; Micoulaud-Franchi, J.A.; Philip, P.; Lamy, M.; Savard, J. Prevalent, incident, and persistent insomnia in a population-based cohort tested before (2018) and during the first-wave of COVID-19 pandemic (2020). Sleep 2022, 45, zsab258. [Google Scholar] [CrossRef]
- Nishijima, C.; Miyagawa, N.; Tsuboyama-Kasaoka, N.; Chiba, T.; Miyachi, M. Association between Lifestyle Changes and at-Home Hours during and after the State of Emergency Due to the COVID-19 Pandemic in Japan. Nutrients 2021, 13, 2698. [Google Scholar] [CrossRef] [PubMed]
- Ong, J.L.; Lau, T.; Massar, S.A.A.; Chong, Z.T.; Ng, B.K.L.; Koek, D.; Zhao, W.; Yeo, B.T.T.; Cheong, K.; Chee, M.W.L. COVID-19-related mobility reduction: Heterogenous effects on sleep and physical activity rhythms. Sleep 2021, 44, zsaa179. [Google Scholar] [CrossRef]
- Pachocka, L.; El-Helou, B.; Wojda, B.; Mękus, M. Impact of lockdown on changes in lifestyle, including changes in consumtion of selected groups of food products among the inhabitatns in the Mazowieckie Region. Prz. Epidemiol. 2022, 76, 79–96. [Google Scholar] [CrossRef]
- Panarese, P.; Azzarita, V. The Impact of the COVID-19 Pandemic on Lifestyle: How Young people have Adapted Their Leisure and Routine during Lockdown in Italy. Young 2021, 29 (Suppl. S4), S35–S64. [Google Scholar] [CrossRef]
- Pecotić, R.; Pavlinac Dodig, I.; Lušić Kalcina, L.; Demirović, S.; Madirazza, K.; Valić, M.; Đogaš, Z. The COVID-19 lockdown promotes changes in sleep habits in the Croatian general population. Croat. Med. J. 2022, 63, 352–361. [Google Scholar] [CrossRef] [PubMed]
- Pépin, J.L.; Bailly, S.; Mordret, E.; Gaucher, J.; Tamisier, R.; Ben Messaoud, R.; Arnal, P.J.; Mignot, E. Greatest changes in objective sleep architecture during COVID-19 lockdown in night owls with increased REM sleep. Sleep 2021, 44, zsab075. [Google Scholar] [CrossRef]
- Pérez-Carbonell, L.; Meurling, I.J.; Wassermann, D.; Gnoni, V.; Leschziner, G.; Weighall, A.; Ellis, J.; Durrant, S.; Hare, A.; Steier, J. Impact of the novel coronavirus (COVID-19) pandemic on sleep. J. Thorac. Dis. 2020, 12 (Suppl. S2), S163–S175. [Google Scholar] [CrossRef] [PubMed]
- Peterson, M.; Lundholm, K.; Skeiky, L.; Van Dongen, H.; Hansen, D. 727 Impact of Washington State COVID-19 Lockdown on Sleep. Sleep 2021, 44 (Suppl. S2), A283–A284. [Google Scholar] [CrossRef]
- Petrov, M.E.; Pituch, K.A.; Kasraeian, K.; Jiao, N.; Mattingly, J.; Hasanaj, K.; Youngstedt, S.D.; Buman, M.P.; Epstein, D.R. Impact of the COVID-19 pandemic on change in sleep patterns in an exploratory, cross-sectional online sample of 79 countries. Sleep Health 2021, 7, 451–458. [Google Scholar] [CrossRef] [PubMed]
- Pišot, S.; Milovanović, I.; Šimunič, B.; Gentile, A.; Bosnar, K.; Prot, F.; Bianco, A.; Lo Coco, G.; Bartoluci, S.; Katović, D.; et al. Maintaining everyday life praxis in the time of COVID-19 pandemic measures (ELP-COVID-19 survey). Eur. J. Public. Health 2020, 30, 1181–1186. [Google Scholar] [CrossRef] [PubMed]
- Pitol, M.N.S.; Sapir, A.S.M. COVID-19: Introduction of a new lifestyle and diet among the Malaysians. Bull. Natl. Res. Cent. 2023, 47, 3. [Google Scholar] [CrossRef]
- Pouget, M.; Clinchamps, M.; Lambert, C.; Pereira, B.; Farigon, N.; Gentes, E.; Miolanne, M.; Picard, M.; Tyrode, A.; Alligier, M.; et al. Impact of COVID-19 Lockdown on Food Consumption and Behavior in France (COVISTRESS Study). Nutrients 2022, 14, 3739. [Google Scholar] [CrossRef]
- Priego-Parra, B.A.; Triana-Romero, A.; Mayanin Pinto-Gálvez, S.; Durán Ramos, C.; Salas-Nolasco, O.; Manriquez Reyes, M.; Ramos-de-la-Medina, A.; María Remes-Troche, J. Anxiety, depression, attitudes, and internet addiction during the initial phase of the 2019 coronavirus disease (COVID-19) epidemic: A cross-sectional study in México. medRxiv 2020. [Google Scholar] [CrossRef]
- Rababah, T.; Al-U’datt, M.; Angor, M.M.; Gammoh, S.; Rababah, R.; Magableh, G.; Almajwal, A.; Al-Rayyan, Y.; Al-Rayyan, N. Impact of COVID-19 pandemic on obesity among adults in Jordan. Front. Nutr. 2023, 10, 1114076. [Google Scholar] [CrossRef] [PubMed]
- Radwan, H.; Al Kitbi, M.; Hasan, H.; Al Hilali, M.; Abbas, N.; Hamadeh, R.; Saif, E.R.; Naja, F. Indirect Health Effects of COVID-19: Unhealthy Lifestyle Behaviors during the Lockdown in the United Arab Emirates. Int. J. Environ. Res. Public. Health 2021, 18, 1964. [Google Scholar] [CrossRef] [PubMed]
- Ramírez, C.; García, A.; Santos, I.; Borrani, J.; Valdez, P. Changes in sleep habits during the lockdown for the COVID-19 pandemic in the population and people attending a morning or an afternoon shift in Monterrey, Mexico. Chronobiol. Int. 2022, 39, 918–935. [Google Scholar] [CrossRef] [PubMed]
- Ramos Socarras, L.; Potvin, J.; Forest, G. COVID-19 and sleep patterns in adolescents and young adults. Sleep Med. 2021, 83, 26–33. [Google Scholar] [CrossRef] [PubMed]
- Reynaud, E.; Pottelette, J.; Rabot, J.; Rolling, J.; Royant-Parola, S.; Hartley, S.; Coutelle, R.; Schröder, C.M. Differential effects of COVID-related lockdown on sleep-wake rhythms in adults with autism spectrum disorder compared to the general population. Autism Res. 2022, 15, 945–956. [Google Scholar] [CrossRef] [PubMed]
- Robinson, E.; Gillespie, S.; Jones, A. Weight-related lifestyle behaviours and the COVID-19 crisis: An online survey study of UK adults during social lockdown. Obes. Sci. Pr. 2020, 6, 735–740. [Google Scholar] [CrossRef] [PubMed]
- Rotvold, A.; Parker, K.; Honrath, K.; Rhee, Y. Sleep and diet patterns of college students during the COVID-19 pandemic lockdowns. J. Am. Coll. Health 2022, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Zaldibar, C.; García-Garcés, L.; Vicario-Merino, Á.; Mayoral-Gonzalo, N.; Lluesma-Vidal, M.; Ruiz-López, M.; Pérez-Manchón, D. The Impact of COVID-19 on the Lifestyles of University Students: A Spanish Online Survey. Healthcare 2022, 10, 309. [Google Scholar] [CrossRef] [PubMed]
- Saalwirth, C.; Leipold, B. Well-being and sleep in stressful times of the COVID-19 pandemic: Relations to worrying and different coping strategies. Stress Health 2021, 37, 973–985. [Google Scholar] [CrossRef]
- Salehinejad, M.A.; Majidinezhad, M.; Ghanavati, E.; Kouestanian, S.; Vicario, C.M.; Nitsche, M.A.; Nejati, V. Negative impact of COVID-19 pandemic on sleep quantitative parameters, quality, and circadian alignment: Implications for health and psychological well-being. EXCLI J. 2020, 19, 1297–1308. [Google Scholar] [CrossRef]
- Salfi, F.; Lauriola, M.; D’Atri, A.; Amicucci, G.; Viselli, L.; Tempesta, D.; Ferrara, M. Demographic, psychological, chronobiological, and work-related predictors of sleep disturbances during the COVID-19 lockdown in Italy. Sci. Rep. 2021, 11, 11416. [Google Scholar] [CrossRef] [PubMed]
- Santos-Miranda, E.; Rico-Díaz, J.; Carballo-Fazanes, A.; Abelairas-Gómez, C. Changes in healthy habits regarding physical activity and sedentary lifestyle during a national lockdown due to COVID-19. Retos 2022, 43, 415–421. [Google Scholar] [CrossRef]
- Sañudo, B.; Fennell, C.; Sánchez-Oliver, A.J. Objectively-assessed physical activity, sedentary behavior, smartphone use, and sleep patterns preand during-COVID-19 quarantine in young adults from Spain. Sustainability 2020, 12, 5890. [Google Scholar] [CrossRef]
- Scarpelli, S.; Alfonsi, V.; Mangiaruga, A.; Musetti, A.; Quattropani, M.C.; Lenzo, V.; Freda, M.F.; Lemmo, D.; Vegni, E.; Borghi, L.; et al. Pandemic nightmares: Effects on dream activity of the COVID-19 lockdown in Italy. J. Sleep Res. 2021, 30, e13300. [Google Scholar] [CrossRef] [PubMed]
- Shahzadi, K.; Liaqat, B.; Shahbaz, A.; Farooq, H.U. Covid-19 lockdown Impact on the Adult Pakistani Population. Pak. J. Med. Health Sci. 2021, 15, 1180–1184. [Google Scholar] [CrossRef]
- Sheehan, C.; Li, L.; Petrov, M.E. How did trends in sleep duration in 2020 compare to previous years and how did they vary by sex, race/ethnicity, and educational attainment? Sleep Med. 2023, 101, 570–577. [Google Scholar] [CrossRef] [PubMed]
- Singh, B.; Jain, S.; Rastogi, A. Effects of nationwide COVID-19 lockdown on lifestyle and diet: An Indian survey. J. Fam. Med. Prim. Care 2021, 10, 1246–1250. [Google Scholar] [CrossRef] [PubMed]
- Singh, V.; Raghav, P.; Singh, G.; Pritish Baskaran, T.B.; Bishnoi, A.; Gautam, V.; Chaudhary, A.K.; Kumar, A.; Kumar, S.; Sahu, S. Lifestyle and behavioral changes during nationwide lockdown in India-A cross-sectional analysis. J. Fam. Med. Prim. Care 2021, 10, 2661–2667. [Google Scholar] [CrossRef]
- Sinha, M.; Pande, B.; Sinha, R. Association of mid sleep time and social jetlag with psychosocial behaviour of Indian population during COVID-19 lockdown. J. Public. Health Res. 2020, 9, 1870. [Google Scholar] [CrossRef]
- Sinha, M.; Pande, B.; Sinha, R. Impact of COVID-19 lockdown on sleep-wake schedule and associated lifestyle related behavior: A national survey. J. Public. Health Res. 2020, 9, 1826. [Google Scholar] [CrossRef]
- Sinisterra Loaiza, L.I.; Vázquez Belda, B.; Miranda López, J.M.; Cepeda, A.; Cardelle Cobas, A. Food habits in the Galician population during confinement byCOVID-19. Nutr. Hosp. 2020, 37, 1190–1196. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.L.; Herbert, A.; Hughes, A.; Northstone, K.; Howe, L.D. Socioeconomic position and adverse childhood experiences as risk factors for health-related behaviour change and employment adversity during the COVID-19 pandemic: Insights from a prospective cohort study in the UK. BMC Public. Health 2022, 22, 1820. [Google Scholar] [CrossRef]
- Souza, T.C.; Oliveira, L.A.; Daniel, M.M.; Ferreira, L.G.; Della Lucia, C.M.; Liboredo, J.C.; Anastácio, L.R. Lifestyle and eating habits before and during COVID-19 quarantine in Brazil. Public. Health Nutr. 2022, 25, 65–75. [Google Scholar] [CrossRef]
- Storari, M.; Orrù, G.; Manconi, M.; Caruso, L.; Viscuso, D. Sleep/wake rhythm modifications in the Italian population during SARS-CoV-2 pandemic: A web-based cross-sectional survey. Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 5047–5056. [Google Scholar] [CrossRef] [PubMed]
- Szczepańska, E.; Janota, B. Lifestyle of Families with Children Aged 4-8 Years before and during Lockdown Due to COVID-19 Pandemic in Poland. Int. J. Environ. Res. Public. Health 2022, 19, 15064. [Google Scholar] [CrossRef]
- Tang, N.K.Y.; McEnery, K.A.M.; Chandler, L.; Toro, C.; Walasek, L.; Friend, H.; Gu, S.; Singh, S.P.; Meyer, C. Pandemic and student mental health: Mental health symptoms among university students and young adults after the first cycle of lockdown in the UK. BJPsych Open 2022, 8, e138. [Google Scholar] [CrossRef] [PubMed]
- Taporoski, T.P.; Beijamini, F.; Gómez, L.M.; Ruiz, F.S.; Ahmed, S.S.; von Schantz, M.; Pereira, A.C.; Knutson, K.L. Subjective sleep quality before and during the COVID-19 pandemic in a Brazilian rural population. Sleep Health 2022, 8, 167–174. [Google Scholar] [CrossRef] [PubMed]
- Trabelsi, K.; Ammar, A.; Masmoudi, L.; Boukhris, O.; Chtourou, H.; Bouaziz, B.; Brach, M.; Bentlage, E.; How, D.; Ahmed, M.; et al. Globally altered sleep patterns and physical activity levels by confinement in 5056 individuals: ECLB COVID-19 international online survey. Biol. Sport 2021, 38, 495–506. [Google Scholar] [CrossRef]
- Trakada, A.; Nikolaidis, P.T.; Andrade, M.D.S.; Puccinelli, P.J.; Economou, N.T.; Steiropoulos, P.; Knechtle, B.; Trakada, G. Sleep During “Lockdown” in the COVID-19 Pandemic. Int. J. Environ. Res. Public. Health 2020, 17, 9094. [Google Scholar] [CrossRef]
- Tsigkas, G.; Koufou, E.E.; Katsanos, K.; Patrinos, P.; Moulias, A.; Miliordos, I.; Almpanis, G.; Christodoulou, I.; Papanikolaou, F.; Dimitroula, T.; et al. Potential Relationship Between Lifestyle Changes and Incidence of Hospital Admissions for Acute Coronary Syndrome During the COVID-19 Lockdown. Front. Cardiovasc. Med. 2021, 8, 604374. [Google Scholar] [CrossRef]
- Urquía, Y.J.M.; Pereira, T.S.S.; Martinez, O.G.E.; Silva, D.A.; Martins, M.C.T.; Molina, M.d.C.B. Food, lifestyle and social distancing: A study in the Brazilian southeast during the COVID-19 pandemic. Población Salud Mesoamérica 2022, 20, 165–188. [Google Scholar] [CrossRef]
- Valiensi, S.M.; Folgueira, A.L.; Garay, A. Early impact on sleep and mental health during the mandatory social isolation of COVID-19 outbreak: An observational cross-sectional study carried out in Argentina. Sleep Sci. 2022, 15 (Suppl. S1), 41–48. [Google Scholar] [CrossRef] [PubMed]
- van der Werf, E.T.; Busch, M.; Jong, M.C.; Hoenders, H.J.R. Lifestyle changes during the first wave of the COVID-19 pandemic: A cross-sectional survey in the Netherlands. BMC Public. Health 2021, 21, 1226. [Google Scholar] [CrossRef]
- Villadsen, A.; Patalay, P.; Bann, D. Mental health in relation to changes in sleep, exercise, alcohol and diet during the COVID-19 pandemic: Examination of four UK cohort studies. Psychol. Med. 2023, 53, 2748–2757. [Google Scholar] [CrossRef] [PubMed]
- Villaseñor Lopez, K.; Jimenez Garduño, A.M.; Ortega Regules, A.E.; Islas Romero, L.M.; Gonzalez Martinez, O.A.; Silva Pereira, T.S. Cambios en el estilo de vida y nutrición durante el confinamiento por SARS-CoV-2 (COVID-19) en México: Un estudio observacional. Rev. Española Nutr. Humana Dietética 2021, 25 (Suppl. S2), e1099. [Google Scholar] [CrossRef]
- Vinogrado, O.O.; Guzhva, O.I. The impact of restrictive measures to prevent the spread of COVID-19 on students’ lifestyle. Med. Perspect. 2022, 3, 2786–4804. [Google Scholar] [CrossRef]
- Viselli, L.; Salfi, F.; D’Atri, A.; Amicucci, G.; Ferrara, M. Sleep Quality, Insomnia Symptoms, and Depressive Symptomatology among Italian University Students before and during the Covid-19 Lockdown. Int. J. Environ. Res. Public. Health 2021, 18, 13346. [Google Scholar] [CrossRef] [PubMed]
- Vollmer, C.; Jankowski, K.S. COVID-19-lockdown delayed sleep timing in Tyrolean teachers. Chronobiol. Int. 2022, 39, 1601–1610. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Lei, S.M.; Le, S.; Yang, Y.; Zhang, B.; Yao, W.; Gao, Z.; Cheng, S. Bidirectional Influence of the COVID-19 Pandemic Lockdowns on Health Behaviors and Quality of Life among Chinese Adults. Int. J. Environ. Res. Public. Health 2020, 17, 5575. [Google Scholar] [CrossRef]
- Wright, K.P., Jr.; Linton, S.K.; Withrow, D.; Casiraghi, L.; Lanza, S.M.; Iglesia, H.; Vetter, C.; Depner, C.M. Sleep in university students prior to and during COVID-19 Stay-at-Home orders. Curr. Biol. 2020, 30, R797–R798. [Google Scholar] [CrossRef]
- Yang, G.Y.; Lin, X.L.; Fang, A.P.; Zhu, H.L. Eating Habits and Lifestyles during the Initial Stage of the COVID-19 Lockdown in China: A Cross-Sectional Study. Nutrients 2021, 13, 970. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; Guo, B.; Ao, L.; Yang, C.; Zhang, L.; Zhou, J.; Jia, P. Obesity and activity patterns before and during COVID-19 lockdown among youths in China. Clin. Obes. 2020, 10, e12416. [Google Scholar] [CrossRef] [PubMed]
- Zalech, M. Effects of social isolation caused by the COVID-19 pandemic on changes in daily activity: A case study of physical education students. Balt. J. Health Phys. Act. 2021, 13, 63–74. [Google Scholar] [CrossRef]
- Zheng, C.; Huang, W.Y.; Sheridan, S.; Sit, C.H.; Chen, X.K.; Wong, S.H. COVID-19 Pandemic Brings a Sedentary Lifestyle in Young Adults: A Cross-Sectional and Longitudinal Study. Int. J. Environ. Res. Public. Health 2021, 17, 6035. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Q.; Li, M.; Ji, Y.; Shi, Y.; Zhou, J.; Li, Q.; Qin, R.; Zhuang, X. “Stay-at-Home” Lifestyle Effect on Weight Gain during the COVID-19 Outbreak Confinement in China. Int. J. Environ. Res. Public. Health 2021, 18, 1813. [Google Scholar] [CrossRef] [PubMed]
- Kantermann, T. Behavior: How a Global Social Lockdown Unlocks Time for Sleep. Curr. Biol. 2020, 30, R822–R823. [Google Scholar] [CrossRef] [PubMed]
- Bird, K.A.; Castleman, B.L.; Lohner, G. Negative Impacts from the Shift to Online Learning during the COVID-19 Crisis: Evidence from a Statewide Community College System; EdWorkingPaper: 20-299; Annenberg Institute at Brown University: Providence, RI, USA, 2020. [Google Scholar] [CrossRef]
- Chattu, V.K.; Manzar, M.D.; Kumary, S.; Burman, D.; Spence, D.W.; Pandi-Perumal, S.R. The Global Problem of Insufficient Sleep and Its Serious Public Health Implications. Healthcare 2018, 7, 1. [Google Scholar] [CrossRef] [PubMed]
- Roland, A.; Colomb, C.; Noël, S.; Putilov, A.; Oginska, H.; Delwiche, B.; Benkirane, O.; Windal, M.; Vanlaer, N.; Briganti, G.; et al. Prevalence of Insomnia and Sleep Habits during the First and Second Wave of COVID-19 in Belgium. Psychol. Belg. 2023, 63, 18–29. [Google Scholar] [CrossRef] [PubMed]
- Salfi, F.; D’Atri, A.; Tempesta, D.; Ferrara, M. Sleeping under the waves: A longitudinal study across the contagion peaks of the COVID-19 pandemic in Italy. J. Sleep Res. 2021, 30, e13313. [Google Scholar] [CrossRef]
- Watson, N.F.; Badr, M.S.; Belenky, G.; Bliwise, D.L.; Buxton, O.M.; Buysse, D.; Dinges, D.F.; Gangwisch, J.; Grandner, M.A.; Kushida, C.; et al. Recommended Amount of Sleep for a Healthy Adult: A Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep 2015, 38, 843–844. [Google Scholar] [CrossRef]
- Benedict, C.; Cedernaes, J. Could a good night’s sleep improve COVID-19 vaccine efficacy? Lancet Respir. Med. 2021, 9, 447–448. [Google Scholar]
- Patel, S.R.; Malhotra, A.; Gao, X.; Hu, F.B.; Neuman, M.I.; Fawzi, W.W. A prospective study of sleep duration and pneumonia risk in women. Sleep 2012, 35, 97–101. [Google Scholar] [CrossRef] [PubMed]
- Athanasiou, N.; Baou, K.; Papandreou, E.; Varsou, G.; Amfilochiou, A.; Kontou, E.; Pataka, A.; Porpodis, K.; Tsiouprou, I.; Kaimakamis, E.; et al. Association of sleep duration and quality with immunological response after vaccination against severe acute respiratory syndrome coronavirus-2 infection. J. Sleep Res. 2023, 32, e13656. [Google Scholar] [CrossRef] [PubMed]
- Izuhara, M.; Matsui, K.; Yoshiike, T.; Kawamura, A.; Utsumi, T.; Nagao, K.; Tsuru, A.; Otsuki, R.; Kitamura, S.; Kuriyama, K. Association between sleep duration and antibody acquisition after mRNA vaccination against SARS-CoV-2. Front. Immunol. 2023, 14, 1242302. [Google Scholar] [CrossRef]
- Chaput, J.P.; Dutil, C.; Featherstone, R.; Ross, R.; Giangregorio, L.; Saunders, T.J.; Janssen, I.; Poitras, V.J.; Kho, M.E.; Ross-White, A.; et al. Sleep timing, sleep consistency, and health in adults: A systematic review. Appl. Physiol. Nutr. Metab. 2020, 45 (Suppl. S2), S232–S247. [Google Scholar] [CrossRef] [PubMed]
- Zatońska, K.; Basiak-Rasała, A.; Połtyn-Zaradna, K.; Kinastowski, K.; Szuba, A. Sleep Duration and Bedtime in the PURE Poland Cohort Study and the Link with Noncommunicable Diseases. Int. J. Environ. Res. Public. Health 2021, 19, 403. [Google Scholar] [CrossRef] [PubMed]
- Itani, O.; Jike, M.; Watanabe, N.; Kaneita, Y. Short sleep duration and health outcomes: A systematic review, meta-analysis, and meta-regression. Sleep Med. 2017, 32, 246–256. [Google Scholar] [CrossRef]
- Jike, M.; Itani, O.; Watanabe, N.; Buysse, D.J.; Kaneita, Y. Long sleep duration and health outcomes: A systematic review, meta-analysis and meta-regression. Sleep Med. Rev. 2018, 39, 25–36. [Google Scholar] [CrossRef]
- Stenholm, S.; Kronholm, E.; Bandinelli, S.; Guralnik, J.M.; Ferrucci, L. Self-reported sleep duration and time in bed as predictors of physical function decline: Results from the InCHIANTI study. Sleep 2011, 34, 1583–1593. [Google Scholar] [CrossRef]
- Leong, R.L.F.; Lo, J.C.; Chee, M.W.L. Systematic review and meta-analyses on the effects of afternoon napping on cognition. Sleep Med. Rev. 2022, 65, 101666. [Google Scholar] [CrossRef]
- Li, J.; McPhillips, M.V.; Deng, Z.; Fan, F.; Spira, A. Daytime Napping and Cognitive Health in Older Adults: A Systematic Review. The journals of gerontology. Ser. A Biol. Sci. Med. Sci. 2023, 78, 1853–1860. [Google Scholar] [CrossRef] [PubMed]
- Xie, B.; Wang, J.; Li, X.; Zhang, J.; Chen, M. Association between daytime napping duration and depression in middle-aged and elderly Chinese: Evidence from the China Health and Retirement Longitudinal Study (CHARLS): A cross-sectional study in China. Medicine 2020, 99, e22686. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.; Ma, C.; Zhao, M.; Magnussen, C.G.; Xi, B. Daytime napping and cardiovascular risk factors, cardiovascular disease, and mortality: A systematic review. Sleep Med. Rev. 2022, 65, 101682. [Google Scholar] [CrossRef] [PubMed]
- Ferreira-Souza, L.F.; Julianelli-Peçanha, M.; Coelho-Oliveira, A.C.; da Silva Bahia, C.M.C.; Paineiras-Domingos, L.L.; Reis-Silva, A.; Moura-Fernandes, M.C.; Trindade-Gusmão, L.C.; Taiar, R.; da Cunha Sá-Caputo, D.; et al. Impacts of COVID-19 Pandemic on Sleep Quality Evaluated by Wrist Actigraphy: A Systematic Review. J. Clin. Med. 2023, 12, 1182. [Google Scholar] [CrossRef] [PubMed]
- Korman, M.; Tkachev, V.; Reis, C.; Komada, Y.; Kitamura, S.; Gubin, D.; Kumar, V.; Roenneberg, T. TCOVID-19-mandated social restrictions unveil the impact of social time pressure on sleep and body clock. Sci. Rep. 2020, 10, 22225. [Google Scholar] [CrossRef] [PubMed]
- Tull, M.T.; Edmonds, K.A.; Scamaldo, K.M.; Richmond, J.R.; Rose, J.P.; Gratz, K.L. Psychological Outcomes Associated with Stay-at-Home Orders and the Perceived Impact of COVID-19 on Daily Life. Psychiatry Res. 2020, 289, 113098. [Google Scholar] [CrossRef] [PubMed]
- Trott, M.; Driscoll, R.; Irlado, E.; Pardhan, S. Changes and correlates of screen time in adults and children during the COVID-19 pandemic: A systematic review and meta-analysis. eClinicalMedicine 2022, 48, 101452. [Google Scholar] [CrossRef]
- Drumheller, K.; Fan, C.W. Unprecedented times and uncertain connections: A systematic review examining sleep problems and screentime during the COVID-19 pandemic. Sleep Epidemiol. 2022, 2, 100029. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).