Comprehensive Review of Chronic Stress Pathways and the Efficacy of Behavioral Stress Reduction Programs (BSRPs) in Managing Diseases
Abstract
1. Introduction
2. Summary
- Re-education involves transforming potential threats into beneficial opportunities through knowledge and understanding;
- Refocusing: shifting focus to stimuli already perceived as beneficial;
- Recoping: transitioning from harmful to healthy coping mechanisms.
3. How Stress Influences Health
3.1. Immune Response
3.2. Cancer
3.3. Gastrointestinal Illnesses
3.4. Diabetes
3.5. Epilepsy
3.6. Parkinson’s Disease
3.7. Depression and Anxiety
3.8. PTSD
3.9. Accelerated Aging, Early Mortality
3.10. Unhealthy Coping Responses to Stress
3.10.1. Smoking and Alcohol Consumption
3.10.2. Drugs and Hypersexual Behavior
3.10.3. Gambling
3.10.4. Compulsive Buying–Shopping Disorder (CBSD)
3.10.5. Overeating
3.10.6. Media and Games
3.10.7. Violence
3.10.8. Suicide
3.11. Conclusions
4. Sources of Chronic Stress
4.1. Work and Education
4.2. Old Age
4.3. Prenatal Stress
4.4. Traumatic Events
4.5. Parenting, Caring, and Nursing
4.6. Media
4.7. Conclusions
5. The Influence of BSRPs on Health
5.1. Perception: The Central Pillar in Stress
5.2. Perception Is a Learnable Skill
5.3. Over 200 BSRP Studies
5.4. Conclusions
- Re-education;
- Refocusing;
- Recoping.
6. Behavioral Stress Reduction Programs (BSRPs)
6.1. PsychoEducation, Paced Respiration, and Relaxation (PEPRR)
6.2. Animal-Assisted Therapy
6.3. Music Therapy
6.4. Singing
6.5. Distraction
6.6. Transcendental Meditation
6.7. Mindfulness-Based Stress Reduction and Cognitive Therapy (MBSR and MBCT)
6.8. The Teutsch IDEAL Method
- Resentment and irritation;
- Suppression;
- Increased resentment and irritation;
- Indirect expression, depression, alcoholism, overeating, drug abuse, gambling, hypersexuality, compulsive buying, illness, and scapegoating.
- The first pillar, behavioral psychogenetics, explores the inheritance of behavior, the formation of reactions during the prenatal period and childhood, and how these can be leveraged for permanent behavioral change through re-education. This re-education aims to alter responses to previously stressful situations, impacting gene expression and inducing epigenetic changes.
- The second pillar, human physics, applies the principles of physics to human behavior. This approach provides a scientific framework for understanding and predicting behavior in response to various stimuli by applying strict physical laws, thereby offering a robust foundation for behavior modification.
- The third pillar is akin to the Mindfulness-Based Stress Reduction Program, Transcendental Meditation, and other practices rooted in Buddhism or Hinduism that employ religion-neutral, scientific methodologies derived from these religious principles to achieve consistent results. However, in the case of the IDEAL method, it religion-neutrally incorporates spiritual laws and moral principles from the Bible, interpreting them through a scientific lens.
6.9. Eye Movement Desensitization and Reprocessing (EMDR)
6.10. Tai Chi
6.11. Loving-Kindness and Compassion Meditation
6.12. Inquiry-Based Stress Reduction (IBSR, the Work)
6.13. Comprehensive Lifestyle Modification Programs (CLMPs)
6.14. Ngoma
6.15. Stress Management Education
7. Conclusions
8. Future Directions
- Implementing more controlled randomized studies;
- Developing standardized methodologies;
- Increasing sample sizes;
- Extending the duration of studies to capture long-term effects;
- Utilizing established biomarkers for stress diagnostics;
- Gathering comprehensive data on biochemical changes associated with stress and disease resolution;
- Investigating long-term epigenetic and genetic changes influenced by BSRPs.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gałecki, P.; Talarowska, M. Inflammatory Theory of Depression. Psychiatr. Polska 2018, 52, 437–447. [Google Scholar] [CrossRef]
- Quintana, M.; Rivera, O. Mindfulness Training Online for Stress Reduction, A Global Measure. In Annual Review of Cybertherapy and Telemedicine 2012; IOS Press: Amsterdam, The Netherlands, 2012; pp. 143–148. [Google Scholar]
- Zannas, A.S.; Wiechmann, T.; Gassen, N.C.; Binder, E.B. Gene-Stress-Epigenetic Regulation of FKBP5: Clinical and Translational Implications. Neuropsychopharmacology 2016, 41, 261–274. [Google Scholar] [CrossRef]
- Domínguez-Gerpe, L.; Rey-Méndez, M. Alterations Induced by Chronic Stress in Lymphocyte Subsets of Blood and Primary and Secondary Immune Organs of Mice. BMC Immunol. 2001, 2, 7. [Google Scholar] [CrossRef] [PubMed]
- Hölzel, B.K.; Carmody, J.; Evans, K.C.; Hoge, E.A.; Dusek, J.A.; Morgan, L.; Pitman, R.K.; Lazar, S.W. Stress Reduction Correlates with Structural Changes in the Amygdala. Soc. Cogn. Affect. Neurosci. 2010, 5, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Yang, T.; Qiao, Y.; Xiang, S.; Li, W.; Gan, Y.; Chen, Y. Work Stress and the Risk of Cancer: A Meta-Analysis of Observational Studies. Int. J. Cancer 2019, 144, 2390–2400. [Google Scholar] [CrossRef]
- Esch, T.; Stefano, G.B. Endogenous Reward Mechanisms and Their Importance in Stress Reduction, Exercise and the Brain. Arch. Med. Sci. 2010, 6, 447–455. [Google Scholar] [CrossRef]
- Galla, B.M.; O’Reilly, G.A.; Kitil, M.J.; Smalley, S.L.; Black, D.S. Community-Based Mindfulness Program for Disease Prevention and Health Promotion: Targeting Stress Reduction. Am. J. Heal. Promot. 2015, 30, 36–41. [Google Scholar] [CrossRef]
- Marin, M.-F.; Lord, C.; Andrews, J.; Juster, R.-P.; Sindi, S.; Arsenault-Lapierre, G.; Fiocco, A.J.; Lupien, S.J. Chronic Stress, Cognitive Functioning and Mental Health. Neurobiol. Learn. Mem. 2011, 96, 583–595. [Google Scholar] [CrossRef]
- Rosenzweig, S.; Greeson, J.M.; Reibel, D.K.; Green, J.S.; Jasser, S.A.; Beasley, D. Mindfulness-Based Stress Reduction for Chronic Pain Conditions: Variation in Treatment Outcomes and Role of Home Meditation Practice. J. Psychosom. Res. 2010, 68, 29–36. [Google Scholar] [CrossRef]
- Eckerling, A.; Ricon-Becker, I.; Sorski, L.; Sandbank, E.; Ben-Eliyahu, S. Stress and Cancer: Mechanisms, Significance and Future Directions. Nat. Rev. Cancer 2021, 21, 767–785. [Google Scholar] [CrossRef]
- Brummett, B.H.; Kuhn, C.M.; Boyle, S.H.; Babyak, M.A.; Siegler, I.C.; Williams, R.B. Cortisol Responses to Emotional Stress in Men: Association with a Functional Polymorphism in the 5HTR2C Gene. Biol. Psychol. 2012, 89, 94–98. [Google Scholar] [CrossRef][Green Version]
- Wiley, J.W.; Higgins, G.A.; Hong, S. Chronic Psychological Stress Alters Gene Expression in Rat Colon Epithelial Cells Promoting Chromatin Remodeling, Barrier Dysfunction and Inflammation. PeerJ 2022, 10, e13287. [Google Scholar] [CrossRef] [PubMed]
- Lin, T.; Simchovitz, A.; Shenhar-Tsarfaty, S.; Vaisvaser, S.; Admon, R.; Hanin, G.; Hanan, M.; Kliper, E.; Bar-Haim, Y.; Shomron, N.; et al. Intensified vmPFC Surveillance over PTSS under Perturbed microRNA-608/AChE Interaction. Transl. Psychiatry 2016, 6, e801. [Google Scholar] [CrossRef] [PubMed]
- Cui, B.; Peng, F.; Lu, J.; He, B.; Su, Q.; Luo, H.; Deng, Z.; Jiang, T.; Su, K.; Huang, Y.; et al. Cancer and Stress: NextGen Strategies. Brain Behav. Immun. 2021, 93, 368–383. [Google Scholar] [CrossRef]
- Rentscher, K.E.; Carroll, J.E.; Polsky, L.R.; Lamkin, D.M. Chronic Stress Increases Transcriptomic Indicators of Biological Aging in Mouse Bone Marrow Leukocytes. Brain Behav. Immun.-Health 2022, 22, 100461. [Google Scholar] [CrossRef]
- Kawai, T.; Morita, K.; Masuda, K.; Nishida, K.; Shikishima, M.; Ohta, M.; Saito, T.; Rokutan, K. Gene Expression Signature in Peripheral Blood Cells from Medical Students Exposed to Chronic Psychological Stress. Biol. Psychol. 2007, 76, 147–155. [Google Scholar] [CrossRef]
- Antonenko, S.V.; Kravchuk, I.V.; Telegeev, G.D. Interaction of Bcl-Abl Oncoprotein with the Glg1 Protein in K562 Cells: Its Role in the Pathogenesis of Chronic Myeloid Leukemia. Cytol. Genet. 2020, 54, 48–54. [Google Scholar] [CrossRef]
- Yuan, H.; Wang, Z.; Li, L.; Zhang, H.; Modi, H.; Horne, D.; Bhatia, R.; Chen, W. Activation of Stress Response Gene SIRT1 by BCR-ABL Promotes Leukemogenesis. Blood 2012, 119, 1904–1914. [Google Scholar] [CrossRef]
- Trifa, A.P.; Bănescu, C.; Dima, D.; Bojan, A.S.; Tevet, M.; Moldovan, V.G.; Vesa, C.; Murat, M.; Pop, I.V.; Skrypnyk, C.; et al. Among a Panel of Polymorphisms in Genes Related to Oxidative Stress, CAT-262 C>T, GPX1 Pro198Leu and GSTP1 Ile105Val Influence the Risk of Developing BCR-ABL Negative Myeloproliferative Neoplasms. Hematol. Amst. Neth. 2016, 21, 520–525. [Google Scholar] [CrossRef]
- Li, X.; Jiang, T.; Sun, X.; Yong, X.; Ma, X.; Liu, J. The Relationship between Occupational Stress, Musculoskeletal Disorders and the Mental Health of Coal Miners: The Interaction between BDNF Gene, TPH2 Gene Polymorphism and the Environment. J. Psychiatr. Res. 2021, 135, 76–85. [Google Scholar] [CrossRef] [PubMed]
- Azadmarzabadi, E.; Haghighatfard, A.; Mohammadi, A. Low Resilience to Stress Is Associated with Candidate Gene Expression Alterations in the Dopaminergic Signalling Pathway. Psychogeriatr. Off. J. Jpn. Psychogeriatr. Soc. 2018, 18, 190–201. [Google Scholar] [CrossRef]
- St-Cyr, S.; McGowan, P.O. Programming of Stress-Related Behavior and Epigenetic Neural Gene Regulation in Mice Offspring through Maternal Exposure to Predator Odor. Front. Behav. Neurosci. 2015, 9, 145. [Google Scholar] [CrossRef] [PubMed]
- van Winkel, M.; Peeters, F.; van Winkel, R.; Kenis, G.; Collip, D.; Geschwind, N.; Jacobs, N.; Derom, C.; Thiery, E.; van Os, J.; et al. Impact of Variation in the BDNF Gene on Social Stress Sensitivity and the Buffering Impact of Positive Emotions: Replication and Extension of a Gene-Environment Interaction. Eur. Neuropsychopharmacol. 2014, 24, 930–938. [Google Scholar] [CrossRef]
- Cohen, S.; Frank, E.; Doyle, W.J.; Skoner, D.P.; Rabin, B.S.; Gwaltney, J.M., Jr. Types of Stressors That Increase Susceptibility to the Common Cold in Healthy Adults. Health Psychol. 1998, 17, 214–223. [Google Scholar] [CrossRef]
- Dong, K.; Zhang, F.; Zhu, W.; Wang, Z.; Wang, G. Partial Least Squares Based Gene Expression Analysis in Posttraumatic Stress Disorder. Eur. Rev. Med. Pharmacol. Sci. 2014, 18, 2306–2310. [Google Scholar] [PubMed]
- Zhang, B.; Zhong, W.; Yang, B.; Li, Y.; Duan, S.; Huang, J.; Mao, Y. Gene Expression Profiling Reveals Candidate Biomarkers and Probable Molecular Mechanisms in Chronic Stress. Bioengineered 2022, 13, 6048–6060. [Google Scholar] [CrossRef]
- Hatton-Jones, K.M.; du Toit, E.F.; Cox, A.J. Effect of Chronic Restraint Stress and Western-Diet Feeding on Colonic Regulatory Gene Expression in Mice. Neurogastroenterol. Motil. 2022, 34, e14300. [Google Scholar] [CrossRef]
- Laudenslager, M.L.; Simoneau, T.L.; Philips, S.; Benitez, P.; Natvig, C.; Cole, S. A Randomized Controlled Pilot Study of Inflammatory Gene Expression in Response to a Stress Management Intervention for Stem Cell Transplant Caregivers. J. Behav. Med. 2016, 39, 346–354. [Google Scholar] [CrossRef] [PubMed]
- Verstraeten, B.S.E.; McCreary, J.K.; Weyers, S.; Metz, G.A.S.; Olson, D.M. Prenatal Two-Hit Stress Affects Maternal and Offspring Pregnancy Outcomes and Uterine Gene Expression in Rats: Match or Mismatch? Biol. Reprod. 2019, 100, 195–207. [Google Scholar] [CrossRef]
- Xiao, Y.; Liu, D.; Liu, K.; Wu, C.; Zhang, H.; Niu, Y.; Jiang, X. Association of DRD2, 5-HTTLPR, and 5-HTTVNTR Gene Polymorphisms with Posttraumatic Stress Disorder in Tibetan Adolescents: A Case-Control Study. Biol. Res. Nurs. 2019, 21, 286–295. [Google Scholar] [CrossRef]
- Chang, S.-H.; Chang, Y.-M.; Chen, H.-Y.; Shaw, F.-Z.; Shyu, B.-C. Time-Course Analysis of Frontal Gene Expression Profiles in the Rat Model of Posttraumatic Stress Disorder and a Comparison with the Conditioned Fear Model. Neurobiol. Stress 2023, 27, 100569. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.W.; Ching, S.M.; Ramachandran, V.; Tusimin, M.; Mohd Nordin, N.; Chong, S.C.; Hoo, F.K. Association Analysis of 14 Candidate Gene Polymorphism with Depression and Stress among Gestational Diabetes Mellitus. Genes 2019, 10, 988. [Google Scholar] [CrossRef]
- Mihaljevic, M.; Zeljic, K.; Soldatovic, I.; Andric, S.; Mirjanic, T.; Richards, A.; Mantripragada, K.; Pekmezovic, T.; Novakovic, I.; Maric, N.P. The Emerging Role of the FKBP5 Gene Polymorphisms in Vulnerability-Stress Model of Schizophrenia: Further Evidence from a Serbian Population. Eur. Arch. Psychiatry Clin. Neurosci. 2017, 267, 527–539. [Google Scholar] [CrossRef]
- Haxhibeqiri, S.; Haxhibeqiri, V.; Agani, F.; Goci Uka, A.; Hoxha, B.; Dzubur Kulenovic, A.; Kučukalić, A.; Avdibegović, E.; Sinanović, O.; Babic, D.; et al. Association of Neuropeptide S Receptor 1 and Glutamate Decarboxylase 1 Gene Polymorphisms with Posttraumatic Stress Disorder. Psychiatr. Danub. 2019, 31, 249–255. [Google Scholar] [CrossRef]
- Mitra, S.; Sameer Kumar, G.S.; Jyothi Lakshmi, B.; Thakur, S.; Kumar, S. Absence of Wdr13 Gene Predisposes Mice to Mild Social Isolation—Chronic Stress, Leading to Depression-Like Phenotype Associated with Differential Expression of Synaptic Proteins. Front. Mol. Neurosci. 2018, 11, 133. [Google Scholar] [CrossRef]
- Smart, C.; Strathdee, G.; Watson, S.; Murgatroyd, C.; McAllister-Williams, R.H. Early life trauma, depression and the glucocorticoid receptor gene—An epigenetic perspective. Psychol. Med. 2015, 45, 3393–3410. [Google Scholar] [CrossRef]
- Barnthouse, M.; Jones, B.L. The Impact of Environmental Chronic and Toxic Stress on Asthma. Clin. Rev. Allergy Immunol. 2019, 57, 427–438. [Google Scholar] [CrossRef] [PubMed]
- Chalfun, G.; Reis, M.M.; de Oliveira, M.B.G.; de Araújo Brasil, A.; Dos Santos Salú, M.; da Cunha, A.J.L.A.; Prata-Barbosa, A.; de Magalhães-Barbosa, M.C. Perinatal Stress and Methylation of the NR3C1 Gene in Newborns: Systematic Review. Epigenetics 2022, 17, 1003–1019. [Google Scholar] [CrossRef] [PubMed]
- Oeckinghaus, A.; Hayden, M.S.; Ghosh, S. Crosstalk in NF-κB Signaling Pathways. Nat. Immunol. 2011, 12, 695–708. [Google Scholar] [CrossRef]
- Peter, H.L.; Giglberger, M.; Frank, J.; Streit, F.; Zänkert, S.; Kreuzpointner, L.; Rietschel, M.; Kudielka, B.M.; Wüst, S. The Association between Genetic Variability in the NPS/NPSR1 System and Chronic Stress Responses: A Gene-Environment-(Quasi-) Experiment. Psychoneuroendocrinology 2022, 144, 105883. [Google Scholar] [CrossRef]
- Chigr, F.; Rachidi, F.; Tardivel, C.; Najimi, M.; Moyse, E. Modulation of Orexigenic and Anorexigenic Peptides Gene Expression in the Rat DVC and Hypothalamus by Acute Immobilization Stress. Front. Cell. Neurosci. 2014, 8, 198. [Google Scholar] [CrossRef][Green Version]
- Olsen, M.B.; Sannes, A.-C.; Yang, K.; Nielsen, M.B.; Einarsen, S.V.; Christensen, J.O.; Pallesen, S.; Bjørås, M.; Gjerstad, J. Mapping of Pituitary Stress-Induced Gene Regulation Connects Nrcam to Negative Emotions. iScience 2022, 25, 104953. [Google Scholar] [CrossRef]
- Freire-Cobo, C.; Wang, J. Dietary Phytochemicals Modulate Experience-Dependent Changes in Neurexin Gene Expression and Alternative Splicing in Mice after Chronic Variable Stress Exposure. Eur. J. Pharmacol. 2020, 883, 173362. [Google Scholar] [CrossRef]
- Wingo, A.P.; Velasco, E.R.; Florido, A.; Lori, A.; Choi, D.C.; Jovanovic, T.; Ressler, K.J.; Andero, R. Expression of the PPM1F Gene Is Regulated by Stress and Associated with Anxiety and Depression. Biol. Psychiatry 2018, 83, 284–295. [Google Scholar] [CrossRef] [PubMed]
- Caspi, A.; Sugden, K.; Moffitt, T.E.; Taylor, A.; Craig, I.W.; Harrington, H.; McClay, J.; Mill, J.; Martin, J.; Braithwaite, A.; et al. Influence of Life Stress on Depression: Moderation by a Polymorphism in the 5-HTT Gene. Science 2003, 301, 386–389. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.-J.; Bang, M.; Park, C.I.; Lee, S.-H. Altered DNA Methylation of the Serotonin Transporter Gene Associated with Early Life Stress and White Matter Microalterations in Korean Patients with Panic Disorder. Neuropsychobiology 2023, 82, 210–219. [Google Scholar] [CrossRef] [PubMed]
- Ford, B.Q.; Mauss, I.B.; Troy, A.S.; Smolen, A.; Hankin, B. Emotion Regulation Moderates the Risk Associated with the 5-HTT Gene and Stress in Children. Emotion 2014, 14, 930–939. [Google Scholar] [CrossRef]
- Tsuboi, H.; Sakakibara, H.; Yamakawa-Kobayashi, K.; Tatsumi, A.; Inamori, T.; Hamamoto, R.; Suzuki, A.; Shimoi, K. Val1483Ile Polymorphism in the Fatty Acid Synthase Gene Was Associated with Depressive Symptoms under the Influence of Psychological Stress. J. Affect. Disord. 2011, 134, 448–452. [Google Scholar] [CrossRef]
- Wu, M.; Lin, L.; Wu, Y.; Zheng, Y.; Chen, H. Correlation between 5-HTTLPR Gene Polymorphism and Cognitive Function of Traumatic Stress in Chinese Han Children. Transl. Pediatr. 2022, 11, 1251–1260. [Google Scholar] [CrossRef]
- Jensen, C.G.; Lansner, J.; Petersen, A.; Vangkilde, S.A.; Ringkøbing, S.P.; Frokjaer, V.G.; Adamsen, D.; Knudsen, G.M.; Denninger, J.W.; Hasselbalch, S.G. Open and Calm--a Randomized Controlled Trial Evaluating a Public Stress Reduction Program in Denmark. BMC Public Health 2015, 15, 1245. [Google Scholar] [CrossRef]
- Wang, L.; Hu, T.; Shen, Z.; Zheng, Y.; Geng, Q.; Li, L.; Sha, B.; Li, M.; Sun, Y.; Guo, Y.; et al. Inhibition of USP1 Activates ER Stress through Ubi-Protein Aggregation to Induce Autophagy and Apoptosis in HCC. Cell Death Dis. 2022, 13, 951. [Google Scholar] [CrossRef] [PubMed]
- Antonenko, S.V.; Telegeev, G.D. Inhibition of USP1, a New Partner of Bcr-Abl, Results in Decrease of Bcr-Abl Level in K562 Cells. Exp. Oncol. 2020, 42, 109–114. [Google Scholar] [CrossRef]
- Coleman, K.E.; Yin, Y.; Lui, S.K.L.; Keegan, S.; Fenyo, D.; Smith, D.J.; Rothenberg, E.; Huang, T.T. USP1-Trapping Lesions as a Source of DNA Replication Stress and Genomic Instability. Nat. Commun. 2022, 13, 1740. [Google Scholar] [CrossRef] [PubMed]
- Antonenko, S.V.; Gurianov, D.S.; Тelegeev, G.D. Colocalization of USP1 and РН Domain of BcrAbl Oncoprotein in Terms of Cronic Myeloid Leukemia Cell Rearrangements. Tsitol. Genet. 2016, 50, 11–15. [Google Scholar]
- Thau, L.; Gandhi, J.; Sharma, S. Physiology, Cortisol. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Mychasiuk, R.; Gibb, R.; Kolb, B. Prenatal Stress Produces Sexually Dimorphic and Regionally Specific Changes in Gene Expression in Hippocampus and Frontal Cortex of Developing Rat Offspring. Dev. Neurosci. 2011, 33, 531–538. [Google Scholar] [CrossRef]
- Pulopulos, M.M.; Baeken, C.; De Raedt, R. Cortisol Response to Stress: The Role of Expectancy and Anticipatory Stress Regulation. Horm. Behav. 2020, 117, 104587. [Google Scholar] [CrossRef] [PubMed]
- Rahman, M.F.; McGowan, P.O. Cell-Type-Specific Epigenetic Effects of Early Life Stress on the Brain. Transl. Psychiatry 2022, 12, 326. [Google Scholar] [CrossRef]
- Bhasin, M.K.; Dusek, J.A.; Chang, B.-H.; Joseph, M.G.; Denninger, J.W.; Fricchione, G.L.; Benson, H.; Libermann, T.A. Relaxation Response Induces Temporal Transcriptome Changes in Energy Metabolism, Insulin Secretion and Inflammatory Pathways. PLoS ONE 2013, 8, e62817. [Google Scholar] [CrossRef]
- Jacobs, G.D. Clinical Applications of the Relaxation Response and Mind-Body Interventions. J. Altern. Complement. Med. 2001, 7 (Suppl. S1), S93–S101. [Google Scholar] [CrossRef]
- Xiang, L.; Rehm, K.E.; Sunesara, I.; Griswold, M.; Marshall, G.D. Gene Polymorphisms of Stress Hormone and Cytokine Receptors Associate with Immunomodulatory Profile and Psychological Measurement. J. Psychosom. Res. 2015, 78, 438–444. [Google Scholar] [CrossRef]
- Silberman, D.M.; Wald, M.R.; Genaro, A.M. Acute and Chronic Stress Exert Opposing Effects on Antibody Responses Associated with Changes in Stress Hormone Regulation of T-Lymphocyte Reactivity. J. Neuroimmunol. 2003, 144, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Dai, S.; Mo, Y.; Wang, Y.; Xiang, B.; Liao, Q.; Zhou, M.; Li, X.; Li, Y.; Xiong, W.; Li, G.; et al. Chronic Stress Promotes Cancer Development. Front. Oncol. 2020, 10, 1492. [Google Scholar] [CrossRef] [PubMed]
- Lei, Y.; Liao, F.; Tian, Y.; Wang, Y.; Xia, F.; Wang, J. Investigating the Crosstalk between Chronic Stress and Immune Cells: Implications for Enhanced Cancer Therapy. Front. Neurosci. 2023, 17, 1321176. [Google Scholar] [CrossRef] [PubMed]
- Tsigos, C.; Kyrou, I.; Kassi, E.; Chrousos, G.P. Stress: Endocrine Physiology and Pathophysiology. In Endotext; Feingold, K.R., Anawalt, B., Blackman, M.R., Boyce, A., Chrousos, G., Corpas, E., de Herder, W.W., Dhatariya, K., Dungan, K., Hofland, J., et al., Eds.; MDText.com, Inc.: South Dartmouth, MA, USA, 2000. [Google Scholar]
- Brown, G.W.; Harris, T.O. Life Events and Illness; Guilford Press: New York City, NY, USA, 1989; ISBN 978-0-89862-723-7. [Google Scholar]
- Gulyaeva, N.V. Stress-Associated Molecular and Cellular Hippocampal Mechanisms Common for Epilepsy and Comorbid Depressive Disorders. Biochem. Biokhimiia 2021, 86, 641–656. [Google Scholar] [CrossRef] [PubMed]
- de Pablos, R.M.; Herrera, A.J.; Espinosa-Oliva, A.M.; Sarmiento, M.; Muñoz, M.F.; Machado, A.; Venero, J.L. Chronic Stress Enhances Microglia Activation and Exacerbates Death of Nigral Dopaminergic Neurons under Conditions of Inflammation. J. Neuroinflamm. 2014, 11, 34. [Google Scholar] [CrossRef] [PubMed]
- Zargar, F.; Rahafrouz, L.; Tarrahi, M.J. Effect of Mindfulness-Based Stress Reduction Program on Psychological Symptoms, Quality of Life, and Symptom Severity in Patients with Somatic Symptom Disorder. Adv. Biomed. Res. 2021, 10, 9. [Google Scholar] [CrossRef]
- Zhang, J.-Y.; Liu, T.-H.; He, Y.; Pan, H.-Q.; Zhang, W.-H.; Yin, X.-P.; Tian, X.-L.; Li, B.-M.; Wang, X.-D.; Holmes, A.; et al. Chronic Stress Remodels Synapses in an Amygdala Circuit-Specific Manner. Biol. Psychiatry 2019, 85, 189–201. [Google Scholar] [CrossRef] [PubMed]
- Kohrt, B.A.; Worthman, C.M.; Adhikari, R.P.; Luitel, N.P.; Arevalo, J.M.G.; Ma, J.; McCreath, H.; Seeman, T.E.; Crimmins, E.M.; Cole, S.W. Psychological Resilience and the Gene Regulatory Impact of Posttraumatic Stress in Nepali Child Soldiers. Proc. Natl. Acad. Sci. USA 2016, 113, 8156–8161. [Google Scholar] [CrossRef] [PubMed]
- Rossi, E.L. Stress-Induced Alternative Gene Splicing in Mind-Body Medicine. Adv. Mind Body Med. 2004, 20, 12–19. [Google Scholar]
- Yegorov, Y.E.; Poznyak, A.V.; Nikiforov, N.G.; Sobenin, I.A.; Orekhov, A.N. The Link between Chronic Stress and Accelerated Aging. Biomedicines 2020, 8, 198. [Google Scholar] [CrossRef]
- Lengacher, C.A.; Reich, R.R.; Kip, K.E.; Barta, M.; Ramesar, S.; Paterson, C.L.; Moscoso, M.S.; Carranza, I.; Budhrani, P.H.; Kim, S.J.; et al. Influence of Mindfulness-Based Stress Reduction (MBSR) on Telomerase Activity in Women with Breast Cancer (BC). Biol. Res. Nurs. 2014, 16, 438–447. [Google Scholar] [CrossRef]
- Biegler, K.A.; Anderson, A.K.L.; Wenzel, L.B.; Osann, K.; Nelson, E.L. Longitudinal Change in Telomere Length and the Chronic Stress Response in a Randomized Pilot Biobehavioral Clinical Study: Implications for Cancer Prevention. Cancer Prev. Res. Phila. Pa 2012, 5, 1173–1182. [Google Scholar] [CrossRef]
- Creswell, J.D.; Irwin, M.R.; Burklund, L.J.; Lieberman, M.D.; Arevalo, J.M.G.; Ma, J.; Breen, E.C.; Cole, S.W. Mindfulness-Based Stress Reduction Training Reduces Loneliness and pro-Inflammatory Gene Expression in Older Adults: A Small Randomized Controlled Trial. Brain Behav. Immun. 2012, 26, 1095–1101. [Google Scholar] [CrossRef]
- Algorani, E.B.; Gupta, V. Coping Mechanisms. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar]
- Buhelt, L.P.; Pisinger, C.; Andreasen, A.H. Smoking and Stress in the General Population in Denmark. Tob. Prev. Cessat. 2021, 7, 27. [Google Scholar] [CrossRef]
- Cohen, S.; Gianaros, P.J.; Manuck, S.B. A Stage Model of Stress and Disease. Perspect. Psychol. Sci. 2016, 11, 456–463. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Janicki-Deverts, D.; Miller, G.E. Psychological Stress and Disease. JAMA 2007, 298, 1685–1687. [Google Scholar] [CrossRef]
- Wynd, C.A. Relaxation Imagery Used for Stress Reduction in the Prevention of Smoking Relapse. J. Adv. Nurs. 1992, 17, 294–302. [Google Scholar] [CrossRef]
- Burke, A.R.; Miczek, K.A. Stress in Adolescence and Drugs of Abuse in Rodent Models: Role of Dopamine, CRF, and HPA Axis. Psychopharmacology 2014, 231, 1557–1580. [Google Scholar] [CrossRef]
- Lemieux, A.; al’Absi, M. Stress Psychobiology in the Context of Addiction Medicine: From Drugs of Abuse to Behavioral Addictions. Prog. Brain Res. 2016, 223, 43–62. [Google Scholar] [CrossRef] [PubMed]
- Williams, J.K.; Glover, D.A.; Wyatt, G.E.; Kisler, K.; Liu, H.; Zhang, M. A Sexual Risk and Stress Reduction Intervention Designed for HIV-Positive Bisexual African American Men with Childhood Sexual Abuse Histories. Am. J. Public Health 2013, 103, 1476–1484. [Google Scholar] [CrossRef]
- al’Absi, M.; Allen, A.M. Impact of Acute and Chronic Cannabis Use on Stress Response Regulation: Challenging the Belief That Cannabis Is an Effective Method for Coping. Front. Psychol. 2021, 12, 687106. [Google Scholar] [CrossRef]
- Frank, M.G.; Watkins, L.R.; Maier, S.F. Stress- and Glucocorticoid-Induced Priming of Neuroinflammatory Responses: Potential Mechanisms of Stress-Induced Vulnerability to Drugs of Abuse. Brain Behav. Immun. 2011, 25 (Suppl. S1), S21–S28. [Google Scholar] [CrossRef]
- Hellberg, S.N.; Russell, T.I.; Robinson, M.J.F. Cued for Risk: Evidence for an Incentive Sensitization Framework to Explain the Interplay between Stress and Anxiety, Substance Abuse, and Reward Uncertainty in Disordered Gambling Behavior. Cogn. Affect. Behav. Neurosci. 2019, 19, 737–758. [Google Scholar] [CrossRef]
- Grubbs, J.B.; Chapman, H.; Shepherd, K.A. Post-Traumatic Stress and Gambling Related Cognitions: Analyses in Inpatient and Online Samples. Addict. Behav. 2019, 89, 128–135. [Google Scholar] [CrossRef]
- Ronzitti, S.; Kraus, S.W.; Hoff, R.A.; Potenza, M.N. Stress Moderates the Relationships between Problem-Gambling Severity and Specific Psychopathologies. Psychiatry Res. 2018, 259, 254–261. [Google Scholar] [CrossRef]
- Li, H.; Ma, X.; Fang, J.; Liang, G.; Lin, R.; Liao, W.; Yang, X. Student Stress and Online Shopping Addiction Tendency among College Students in Guangdong Province, China: The Mediating Effect of the Social Support. Int. J. Environ. Res. Public. Health 2022, 20, 176. [Google Scholar] [CrossRef]
- Thomas, T.A.; Schmid, A.M.; Kessling, A.; Wolf, O.T.; Brand, M.; Steins-Loeber, S.; Müller, A. Stress and Compulsive Buying-Shopping Disorder: A Scoping Review. Compr. Psychiatry 2024, 132, 152482. [Google Scholar] [CrossRef]
- Smith, B.W.; Shelley, B.M.; Dalen, J.; Wiggins, K.; Tooley, E.; Bernard, J. A Pilot Study Comparing the Effects of Mindfulness-Based and Cognitive-Behavioral Stress Reduction. J. Altern. Complement. Med. 2008, 14, 251–258. [Google Scholar] [CrossRef]
- Pickett, S.; McCoy, T.P.; Odetola, L. The Influence of Chronic Stress and Emotions on Eating Behavior Patterns and Weight among Young African American Women. West. J. Nurs. Res. 2020, 42, 894–902. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Ye, B.; Wang, P.; Tang, C.; Yang, Q. Coronavirus Stress and Overeating: The Role of Anxiety and COVID-19 Burnout. J. Eat. Disord. 2022, 10, 59. [Google Scholar] [CrossRef] [PubMed]
- Razzoli, M.; Pearson, C.; Crow, S.; Bartolomucci, A. Stress, Overeating, and Obesity: Insights from Human Studies and Preclinical Models. Neurosci. Biobehav. Rev. 2017, 76, 154–162. [Google Scholar] [CrossRef]
- Arora, M.; Singh, A.; Singh, A.K.; Sharma, V.; Kotwal, A. Coping Strategies and Perception toward Drugs, Electronic Gadgets, and Media in Relation to Stress: A Cross-Sectional Study among Residents of a Suburban Area. Indian J. Community Med. 2021, 46, 137–140. [Google Scholar] [CrossRef]
- Pahayahay, A.; Khalili-Mahani, N. What Media Helps, What Media Hurts: A Mixed Methods Survey Study of Coping with COVID-19 Using the Media Repertoire Framework and the Appraisal Theory of Stress. J. Med. Internet Res. 2020, 22, e20186. [Google Scholar] [CrossRef]
- Eden, A.L.; Johnson, B.K.; Reinecke, L.; Grady, S.M. Media for Coping During COVID-19 Social Distancing: Stress, Anxiety, and Psychological Well-Being. Front. Psychol. 2020, 11, 577639. [Google Scholar] [CrossRef]
- Kirchebner, J.; Sonnweber, M.; Nater, U.M.; Günther, M.; Lau, S. Stress, Schizophrenia, and Violence: A Machine Learning Approach. J. Interpers. Violence 2022, 37, 602–622. [Google Scholar] [CrossRef]
- Botha, E.; Gwin, T.; Purpora, C. The Effectiveness of Mindfulness Based Programs in Reducing Stress Experienced by Nurses in Adult Hospital Settings: A Systematic Review of Quantitative Evidence Protocol. JBI Database Syst. Rev. Implement. Rep. 2015, 13, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Street, A.E.; Jiang, T.; Horváth-Puhó, E.; Rosellini, A.J.; Lash, T.L.; Sørensen, H.T.; Gradus, J.L. Stress Disorders and the Risk of Nonfatal Suicide Attempts in the Danish Population. J. Trauma. Stress 2021, 34, 1108–1117. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, D.B.; Gartland, N.; O’Connor, R.C. Stress, Cortisol and Suicide Risk. Int. Rev. Neurobiol. 2020, 152, 101–130. [Google Scholar] [CrossRef]
- dos Santos, A.T.; Soares, F.C.; Lima, R.A.; dos Santos, S.J.; Silva, C.R.d.M.; Bezerra, J.; de Barros, M.V.G. Violence and Psychosocial Stress: A 10-Year Time Trend Analysis. J. Affect. Disord. 2021, 295, 116–122. [Google Scholar] [CrossRef]
- Aboumrad, M.; Shiner, B.; Mucci, L.; Neupane, N.; Schroeck, F.R.; Klaassen, Z.; Freedland, S.J.; Young-Xu, Y. Posttraumatic Stress Disorder and Suicide among Veterans with Prostate Cancer. Psychooncology 2021, 30, 581–590. [Google Scholar] [CrossRef]
- Wu, R.; Zhu, H.; Wu, M.-Y.; Wang, G.-H.; Jiang, C.-L. Childhood Trauma and Suicide: The Mediating Effect of Stress and Sleep. Int. J. Environ. Res. Public. Health 2022, 19, 8493. [Google Scholar] [CrossRef] [PubMed]
- Glaser, R.; Kennedy, S.; Lafuse, W.P.; Bonneau, R.H.; Speicher, C.; Hillhouse, J.; Kiecolt-Glaser, J.K. Psychological Stress-Induced Modulation of Interleukin 2 Receptor Gene Expression and Interleukin 2 Production in Peripheral Blood Leukocytes. Arch. Gen. Psychiatry 1990, 47, 707–712. [Google Scholar] [CrossRef] [PubMed]
- Haghighinejad, H.; Ghazipoor, H.; Jafari, P.; Taghipour, K.; Rezaie, M.; Liaghat, L.; Ramzi, M. Investigating the Impact of Modified Mindfulness-Based Stress Reduction (MBSR) Program on Occupational Burnout and Other Mental Health Status among Nonmedical Staff in a Hospital: A Randomized Controlled Trial. Int. Arch. Occup. Environ. Health 2022, 95, 2005–2016. [Google Scholar] [CrossRef] [PubMed]
- Kurumaji, A.; Umino, M.; Nishikawa, T. Effects of Novelty Stress on Hippocampal Gene Expression, Corticosterone and Motor Activity in Mice. Neurosci. Res. 2011, 71, 161–167. [Google Scholar] [CrossRef]
- Chiang, J.J.; Cole, S.W.; Bower, J.E.; Irwin, M.R.; Taylor, S.E.; Arevalo, J.; Fuligni, A.J. Daily Interpersonal Stress, Sleep Duration, and Gene Regulation during Late Adolescence. Psychoneuroendocrinology 2019, 103, 147–155. [Google Scholar] [CrossRef] [PubMed]
- Olsson, G.; Rehnqvist, N. Sudden Death Precipitated by Psychological Stress. A Case Report. Acta Med. Scand. 1982, 212, 437–441. [Google Scholar] [CrossRef]
- Llorente, E.; Brito, M.L.; Machado, P.; González, M.C. Effect of Prenatal Stress on the Hormonal Response to Acute and Chronic Stress and on Immune Parameters in the Offspring. J. Physiol. Biochem. 2002, 58, 143–149. [Google Scholar] [CrossRef] [PubMed]
- Andersen, E.; Geiger, P.; Schiller, C.; Bluth, K.; Watkins, L.; Zhang, Y.; Xia, K.; Tauseef, H.; Leserman, J.; Girdler, S.; et al. Effects of Mindfulness-Based Stress Reduction on Experimental Pain Sensitivity and Cortisol Responses in Women with Early Life Abuse: A Randomized Controlled Trial. Psychosom. Med. 2021, 83, 515–527. [Google Scholar] [CrossRef] [PubMed]
- Boyd, J.E.; Lanius, R.A.; McKinnon, M.C. Mindfulness-Based Treatments for Posttraumatic Stress Disorder: A Review of the Treatment Literature and Neurobiological Evidence. J. Psychiatry Neurosci. JPN 2018, 43, 7–25. [Google Scholar] [CrossRef]
- Bowling, A. Mortality after Bereavement: A Review of the Literature on Survival Periods and Factors Affecting Survival. Soc. Sci. Med. 1982 1987, 24, 117–124. [Google Scholar] [CrossRef]
- Gallegos, A.M.; Lytle, M.C.; Moynihan, J.A.; Talbot, N.L. Mindfulness-Based Stress Reduction to Enhance Psychological Functioning and Improve Inflammatory Biomarkers in Trauma-Exposed Women: A Pilot Study. Psychol. Trauma Theory Res. Pract. Policy 2015, 7, 525–532. [Google Scholar] [CrossRef] [PubMed]
- Lallukka, T.; Lahelma, E.; Rahkonen, O. Changes in Economic Difficulties and Subsequent Sickness Absence: A Prospective Register-Linkage Study. BMJ Open 2013, 3, e002212. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ranjit, N.; Diez-Roux, A.V.; Shea, S.; Cushman, M.; Ni, H.; Seeman, T. Socioeconomic Position, Race/Ethnicity, and Inflammation in the Multi-Ethnic Study of Atherosclerosis. Circulation 2007, 116, 2383–2390. [Google Scholar] [CrossRef] [PubMed]
- Eitam, H.; Vaya, J.; Brosh, A.; Orlov, A.; Khatib, S.; Izhaki, I.; Shabtay, A. Differential Stress Responses among Newly Received Calves: Variations in Reductant Capacity and Hsp Gene Expression. Cell Stress Chaperones 2010, 15, 865–876. [Google Scholar] [CrossRef] [PubMed]
- Grelet, C.; Vanden Dries, V.; Leblois, J.; Wavreille, J.; Mirabito, L.; Soyeurt, H.; Franceschini, S.; Gengler, N.; Brostaux, Y.; Consortium, H.; et al. Identification of Chronic Stress Biomarkers in Dairy Cows. Anim. Int. J. Anim. Biosci. 2022, 16, 100502. [Google Scholar] [CrossRef] [PubMed]
- Karailiev, P.; Hlavacova, N.; Chomanic, P.; Riecansky, I.; Jezova, D. Dopamine Concentrations and Dopamine Receptor Gene Expression in Emotion-Related Brain Structures of Female Adult Rats Exposed to Stress of Chronic Isolation from Weaning. Gen. Physiol. Biophys. 2020, 39, 393–398. [Google Scholar] [CrossRef] [PubMed]
- Reuveni, E.; Getselter, D.; Oron, O.; Elliott, E. Differential Contribution of Cis and Trans Gene Transcription Regulatory Mechanisms in Amygdala and Prefrontal Cortex and Modulation by Social Stress. Sci. Rep. 2018, 8, 6339. [Google Scholar] [CrossRef] [PubMed]
- Nanda, S.A.; Qi, C.; Roseboom, P.H.; Kalin, N.H. Predator Stress Induces Behavioral Inhibition and Amygdala Somatostatin Receptor 2 Gene Expression. Genes Brain Behav. 2008, 7, 639–648. [Google Scholar] [CrossRef]
- Giotakos, O. Neurobiology of Emotional Trauma. Psychiatr. Psychiatr. 2020, 31, 162–171. [Google Scholar] [CrossRef]
- Li, J.; Cowden, L.G.; King, J.D.; Briles, D.A.; Schroeder, H.W.; Stevens, A.B.; Perry, R.T.; Chen, Z.; Simmons, M.S.; Wiener, H.W.; et al. Effects of Chronic Stress and Interleukin-10 Gene Polymorphisms on Antibody Response to Tetanus Vaccine in Family Caregivers of Patients with Alzheimer’s Disease. Psychosom. Med. 2007, 69, 551–559. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Tang, S.; Zhou, W. Effect of Mindfulness-Based Stress Reduction Therapy on Work Stress and Mental Health of Psychiatric Nurses. Psychiatr. Danub. 2018, 30, 189–196. [Google Scholar] [CrossRef]
- Tajnia, S.; Iranmanesh, S.; Asadi, N.; McDermott, M. Investigating the Effect of Inquiry-Based Stress Reduction on Mortality Awareness and Interpersonal Problems among Intensive Care Unit Nurses. BMC Psychiatry 2022, 22, 106. [Google Scholar] [CrossRef]
- Peng, P.; Liao, Y. Six Addiction Components of Problematic Social Media Use in Relation to Depression, Anxiety, and Stress Symptoms: A Latent Profile Analysis and Network Analysis. BMC Psychiatry 2023, 23, 321. [Google Scholar] [CrossRef]
- Akca, A.; Ayaz-Alkaya, S. Media Use, Positive and Negative Emotions, and Stress Levels of Adults during COVID-19 Pandemic in Turkey: A Cross-Sectional Study. Int. J. Nurs. Pract. 2022, 28, e13035. [Google Scholar] [CrossRef]
- Wolfers, L.N.; Utz, S. Social Media Use, Stress, and Coping. Curr. Opin. Psychol. 2022, 45, 101305. [Google Scholar] [CrossRef] [PubMed]
- Binford, J.; Dolan, M.; Elhai, J.D.; Contractor, A.A. Examining Relationships between Posttraumatic Stress Disorder Severity and Types of Media/Technology Usage. Psychol. Trauma Theory Res. Pract. Policy 2024, 16, 92–97. [Google Scholar] [CrossRef]
- Pfefferbaum, B.; Palka, J.; North, C.S. Media Contact and Posttraumatic Stress in Employees of New York City Area Businesses after the September 11 Attacks. Disaster Med. Public Health Prep. 2022, 16, 163–169. [Google Scholar] [CrossRef] [PubMed]
- Robert, M.; Stene, L.E.; Garfin, D.R.; Vandentorren, S.; Motreff, Y.; du Roscoat, E.; Pirard, P. Media Exposure and Post-Traumatic Stress Symptoms in the Wake of the November 2015 Paris Terrorist Attacks: A Population-Based Study in France. Front. Psychiatry 2021, 12, 509457. [Google Scholar] [CrossRef]
- Luo, Y.; He, X.; Wang, S.; Li, J.; Zhang, Y. Media Exposure Predicts Acute Stress and Probable Acute Stress Disorder during the Early COVID-19 Outbreak in China. PeerJ 2021, 9, e11407. [Google Scholar] [CrossRef]
- Hall, B.J.; Xiong, Y.X.; Yip, P.S.Y.; Lao, C.K.; Shi, W.; Sou, E.K.L.; Chang, K.; Wang, L.; Lam, A.I.F. The Association between Disaster Exposure and Media Use on Post-Traumatic Stress Disorder Following Typhoon Hato in Macao, China. Eur. J. Psychotraumatology 2019, 10, 1558709. [Google Scholar] [CrossRef] [PubMed]
- Lau, J.T.F.; Lau, M.; Kim, J.H.; Tsui, H.Y. Impacts of Media Coverage on the Community Stress Level in Hong Kong after the Tsunami on 26 December 2004. J. Epidemiol. Community Health 2006, 60, 675–682. [Google Scholar] [CrossRef] [PubMed]
- Brailovskaia, J.; Cosci, F.; Mansueto, G.; Margraf, J. The Relationship between Social Media Use, Stress Symptoms and Burden Caused by Coronavirus (COVID-19) in Germany and Italy: A Cross-Sectional and Longitudinal Investigation. J. Affect. Disord. Rep. 2021, 3, 100067. [Google Scholar] [CrossRef] [PubMed]
- Abdalla, S.M.; Cohen, G.H.; Tamrakar, S.; Koya, S.F.; Galea, S. Media Exposure and the Risk of Post-Traumatic Stress Disorder Following a Mass Traumatic Event: An In-Silico Experiment. Front. Psychiatry 2021, 12, 674263. [Google Scholar] [CrossRef]
- Daimer, S.; Mihatsch, L.L.; Neufeld, S.A.S.; Murray, G.K.; Knolle, F. Investigating the Relationship of COVID-19 Related Stress and Media Consumption with Schizotypy, Depression, and Anxiety in Cross-Sectional Surveys Repeated throughout the Pandemic in Germany and the UK. eLife 2022, 11, e75893. [Google Scholar] [CrossRef]
- Teutsch, J.M.; Teutsch, C.K.; Julian, J. From Here to Greater Happiness or How to Change Your Life for Good! 1st ed.; Price/Stern/Sloan: Los Angeles, CA, USA, 1975; ISBN 978-0-8431-0398-4. [Google Scholar]
- Dam, V.A.T.; Dao, N.G.; Nguyen, D.C.; Vu, T.M.T.; Boyer, L.; Auquier, P.; Fond, G.; Ho, R.C.M.; Ho, C.S.H.; Zhang, M.W.B. Quality of Life and Mental Health of Adolescents: Relationships with Social Media Addiction, Fear of Missing out, and Stress Associated with Neglect and Negative Reactions by Online Peers. PLoS ONE 2023, 18, e0286766. [Google Scholar] [CrossRef]
- Maftei, A.; Pătrăușanu, A.-M. Digital Reflections: Narcissism, Stress, Social Media Addiction, and Nomophobia. J. Psychol. 2024, 158, 147–160. [Google Scholar] [CrossRef]
- An, H.; Gu, X.; Obrenovic, B.; Godinic, D. The Role of Job Insecurity, Social Media Exposure, and Job Stress in Predicting Anxiety Among White-Collar Employees. Psychol. Res. Behav. Manag. 2023, 16, 3303–3318. [Google Scholar] [CrossRef] [PubMed]
- Taskin, S.; Yildirim Kurtulus, H.; Satici, S.A.; Deniz, M.E. Doomscrolling and Mental Well-Being in Social Media Users: A Serial Mediation through Mindfulness and Secondary Traumatic Stress. J. Community Psychol. 2024, 52, 512–524. [Google Scholar] [CrossRef]
- McCauley, S.M.; Hestvik, A.; Vogel, I. Perception and Bias in the Processing of Compound versus Phrasal Stress: Evidence from Event-Related Brain Potentials. Lang. Speech 2013, 56, 23–44. [Google Scholar] [CrossRef]
- McEwen, B.S. Neurobiological and Systemic Effects of Chronic Stress. Chronic Stress Thousand Oaks Calif 2017, 1, 2470547017692328. [Google Scholar] [CrossRef]
- Khosrowabadi, R. Stress and Perception of Emotional Stimuli: Long-Term Stress Rewiring the Brain. Basic Clin. Neurosci. 2018, 9, 107–120. [Google Scholar] [CrossRef]
- Gotink, R.A.; Meijboom, R.; Vernooij, M.W.; Smits, M.; Hunink, M.G.M. 8-Week Mindfulness Based Stress Reduction Induces Brain Changes Similar to Traditional Long-Term Meditation Practice—A Systematic Review. Brain Cogn. 2016, 108, 32–41. [Google Scholar] [CrossRef] [PubMed]
- Harp, N.R.; Freeman, J.B.; Neta, M. Mindfulness-Based Stress Reduction Triggers a Long-Term Shift toward More Positive Appraisals of Emotional Ambiguity. J. Exp. Psychol. Gen. 2022, 151, 2160–2172. [Google Scholar] [CrossRef]
- Yan, C.; Cheung, R.S.-Y.; Wong, C.L.; Cheng, H.Y.; Liu, F.; Huang, H.; Ewig, C.L.-Y.; Li, C.-K.; Zhang, H.; Cheung, Y.T. Stress and Perception of Procedural Pain Management in Chinese Parents of Children with Cancer. J. Pain Symptom Manag. 2021, 61, 90–102.e5. [Google Scholar] [CrossRef]
- Moss, A.S.; Reibel, D.K.; Greeson, J.M.; Thapar, A.; Bubb, R.; Salmon, J.; Newberg, A.B. An Adapted Mindfulness-Based Stress Reduction Program for Elders in a Continuing Care Retirement Community: Quantitative and Qualitative Results from a Pilot Randomized Controlled Trial. J. Appl. Gerontol. 2015, 34, 518–538. [Google Scholar] [CrossRef]
- Shoda, H.; Tabei, K.-I.; Abe, M.; Nakahara, J.; Yasuda, S.; Williamon, A.; Isaka, T. Effects of Choir Singing on Physiological Stress in Japanese Older Adults: Its Relationship with Cognitive Functioning and Subjective Well-Being. Arts Health 2023, 1–13. [Google Scholar] [CrossRef]
- Higgins, E.T.; Davidson, R.J.; Busse, W.W.; Klaus, D.R.; Bednarek, G.T.; Goldman, R.I.; Sachs, J.; Rosenkranz, M.A. Clinically Relevant Effects of Mindfulness-Based Stress Reduction in Individuals with Asthma. Brain Behav. Immun.-Health 2022, 25, 100509. [Google Scholar] [CrossRef] [PubMed]
- Pokladnikova, J.; Selke-Krulichova, I. Effectiveness of a Comprehensive Lifestyle Modification Program for Asthma Patients: A Randomized Controlled Pilot Trial. J. Asthma Off. J. Assoc. Care Asthma 2013, 50, 318–326. [Google Scholar] [CrossRef]
- Alrabadi, L.S.; Dutton, A.; Rabiee, A.; Roberts, S.J.; Deng, Y.; Cusack, L.; Silveira, M.G.; Ciarleglio, M.; Bucala, R.; Sinha, R.; et al. Mindfulness-Based Stress Reduction May Decrease Stress, Disease Activity, and Inflammatory Cytokine Levels in Patients with Autoimmune Hepatitis. JHEP Rep. Innov. Hepatol. 2022, 4, 100450. [Google Scholar] [CrossRef]
- Jones, B.J.; Kaur, S.; Miller, M.; Spencer, R.M.C. Mindfulness-Based Stress Reduction Benefits Psychological Well-Being, Sleep Quality, and Athletic Performance in Female Collegiate Rowers. Front. Psychol. 2020, 11, 572980. [Google Scholar] [CrossRef]
- Liu, L.; Tian, L.; Jiang, J.; Zhang, Y.; Chi, X.; Liu, W.; Zhao, Y.-H.; Sun, P. Effect of an Online Mindfulness-Based Stress Reduction Intervention on Postpandemic Era Nurses’ Subjective Well-Being, Job Burnout, and Psychological Adaptation. Holist. Nurs. Pract. 2023, 37, 244–252. [Google Scholar] [CrossRef]
- dos Santos, T.M.; Kozasa, E.H.; Carmagnani, I.S.; Tanaka, L.H.; Lacerda, S.S.; Nogueira-Martins, L.A. Positive Effects of a Stress Reduction Program Based on Mindfulness Meditation in Brazilian Nursing Professionals: Qualitative and Quantitative Evaluation. Explore 2016, 12, 90–99. [Google Scholar] [CrossRef]
- Lamothe, M.; Rondeau, É.; Duval, M.; McDuff, P.; Pastore, Y.D.; Sultan, S. Changes in Hair Cortisol and Self-Reported Stress Measures Following Mindfulness-Based Stress Reduction (MBSR): A Proof-of-Concept Study in Pediatric Hematology-Oncology Professionals. Complement. Ther. Clin. Pract. 2020, 41, 101249. [Google Scholar] [CrossRef]
- Stier-Jarmer, M.; Frisch, D.; Oberhauser, C.; Berberich, G.; Schuh, A. The Effectiveness of a Stress Reduction and Burnout Prevention Program. Dtsch. Arzteblatt Int. 2016, 113, 781–788. [Google Scholar] [CrossRef]
- Schnaider-Levi, L.; Ganz, A.B.; Zafrani, K.; Goldman, Z.; Mitnik, I.; Rolnik, B.; Lev-Ari, S. The Effect of Inquiry-Based Stress Reduction on Teacher Burnout: A Controlled Trial. Brain Sci. 2020, 10, 468. [Google Scholar] [CrossRef]
- Lengacher, C.A.; Kip, K.E.; Barta, M.; Post-White, J.; Jacobsen, P.B.; Groer, M.; Lehman, B.; Moscoso, M.S.; Kadel, R.; Le, N.; et al. A Pilot Study Evaluating the Effect of Mindfulness-Based Stress Reduction on Psychological Status, Physical Status, Salivary Cortisol, and Interleukin-6 among Advanced-Stage Cancer Patients and Their Caregivers. J. Holist. Nurs. Off. J. Am. Holist. Nurses Assoc. 2012, 30, 170–185. [Google Scholar] [CrossRef]
- Bränström, R.; Kvillemo, P.; Brandberg, Y.; Moskowitz, J.T. Self-Report Mindfulness as a Mediator of Psychological Well-Being in a Stress Reduction Intervention for Cancer Patients—A Randomized Study. Ann. Behav. Med. 2010, 39, 151–161. [Google Scholar] [CrossRef]
- Yildirim, D.; Çiriş Yildiz, C.; Ozdemir, F.A.; Harman Özdoğan, M.; Can, G. Effects of a Mindfulness-Based Stress Reduction Program on Stress, Depression, and Psychological Well-Being in Patients with Cancer: A Single-Blinded Randomized Controlled Trial. Cancer Nurs. 2024, 47, E84–E92. [Google Scholar] [CrossRef]
- Birnie, K.; Garland, S.N.; Carlson, L.E. Psychological Benefits for Cancer Patients and Their Partners Participating in Mindfulness-Based Stress Reduction (MBSR). Psychooncology 2010, 19, 1004–1009. [Google Scholar] [CrossRef]
- Garland, S.N.; Tamagawa, R.; Todd, S.C.; Speca, M.; Carlson, L.E. Increased Mindfulness Is Related to Improved Stress and Mood Following Participation in a Mindfulness-Based Stress Reduction Program in Individuals with Cancer. Integr. Cancer Ther. 2013, 12, 31–40. [Google Scholar] [CrossRef]
- Carlson, L.E.; Speca, M.; Faris, P.; Patel, K.D. One Year Pre-Post Intervention Follow-up of Psychological, Immune, Endocrine and Blood Pressure Outcomes of Mindfulness-Based Stress Reduction (MBSR) in Breast and Prostate Cancer Outpatients. Brain Behav. Immun. 2007, 21, 1038–1049. [Google Scholar] [CrossRef]
- Fancourt, D.; Williamon, A.; Carvalho, L.A.; Steptoe, A.; Dow, R.; Lewis, I. Singing Modulates Mood, Stress, Cortisol, Cytokine and Neuropeptide Activity in Cancer Patients and Carers. Ecancermedicalscience 2016, 10, 631. [Google Scholar] [CrossRef] [PubMed]
- Telke, S.; Leininger, B.; Hanson, L.; Kreitzer, M.J. A Randomized Trial of 21 Days of Loving Kindness Meditation for Stress Reduction and Emotional Well-Being Within an Online Health Community for Patients, Family, and Friends Experiencing a Cancer Health Journey. J. Integr. Complement. Med. 2022, 28, 158–167. [Google Scholar] [CrossRef]
- Würtzen, H.; Dalton, S.O.; Christensen, J.; Andersen, K.K.; Elsass, P.; Flyger, H.L.; Pedersen, A.E.; Sumbundu, A.; Steding-Jensen, M.; Johansen, C. Effect of Mindfulness-Based Stress Reduction on Somatic Symptoms, Distress, Mindfulness and Spiritual Wellbeing in Women with Breast Cancer: Results of a Randomized Controlled Trial. Acta Oncol. Stockh. Swed. 2015, 54, 712–719. [Google Scholar] [CrossRef]
- Lengacher, C.A.; Reich, R.R.; Paterson, C.L.; Shelton, M.; Shivers, S.; Ramesar, S.; Pleasant, M.L.; Budhrani-Shani, P.; Groer, M.; Post-White, J.; et al. A Large Randomized Trial: Effects of Mindfulness-Based Stress Reduction (MBSR) for Breast Cancer (BC) Survivors on Salivary Cortisol and IL-6. Biol. Res. Nurs. 2019, 21, 39–49. [Google Scholar] [CrossRef] [PubMed]
- Lengacher, C.A.; Reich, R.R.; Paterson, C.L.; Ramesar, S.; Park, J.Y.; Alinat, C.; Johnson-Mallard, V.; Moscoso, M.; Budhrani-Shani, P.; Miladinovic, B.; et al. Examination of Broad Symptom Improvement Resulting from Mindfulness-Based Stress Reduction in Breast Cancer Survivors: A Randomized Controlled Trial. J. Clin. Oncol. 2016, 34, 2827–2834. [Google Scholar] [CrossRef]
- Matchim, Y.; Armer, J.M.; Stewart, B.R. Effects of Mindfulness-Based Stress Reduction (MBSR) on Health among Breast Cancer Survivors. West. J. Nurs. Res. 2011, 33, 996–1016. [Google Scholar] [CrossRef]
- Rahmani, S.; Talepasand, S. The Effect of Group Mindfulness—Based Stress Reduction Program and Conscious Yoga on the Fatigue Severity and Global and Specific Life Quality in Women with Breast Cancer. Med. J. Islam. Repub. Iran 2015, 29, 175. [Google Scholar]
- Wang, H.; Yang, Y.; Zhang, X.; Shu, Z.; Tong, F.; Zhang, Q.; Yi, J. Research on Mindfulness-Based Stress Reduction in Breast Cancer Patients Undergoing Chemotherapy: An Observational Pilot Study. Altern. Ther. Health Med. 2023, 29, 228–232. [Google Scholar]
- Mirmahmoodi, M.; Mangalian, P.; Ahmadi, A.; Dehghan, M. The Effect of Mindfulness-Based Stress Reduction Group Counseling on Psychological and Inflammatory Responses of the Women with Breast Cancer. Integr. Cancer Ther. 2020, 19, 1534735420946819. [Google Scholar] [CrossRef]
- Witek Janusek, L.; Tell, D.; Mathews, H.L. Mindfulness Based Stress Reduction Provides Psychological Benefit and Restores Immune Function of Women Newly Diagnosed with Breast Cancer: A Randomized Trial with Active Control. Brain Behav. Immun. 2019, 80, 358–373. [Google Scholar] [CrossRef]
- Lee, C.E.; Kim, S.; Kim, S.; Joo, H.M.; Lee, S. Effects of a Mindfulness-Based Stress Reduction Program on the Physical and Psychological Status and Quality of Life in Patients with Metastatic Breast Cancer. Holist. Nurs. Pract. 2017, 31, 260. [Google Scholar] [CrossRef]
- Lengacher, C.A.; Shelton, M.M.; Reich, R.R.; Barta, M.K.; Johnson-Mallard, V.; Moscoso, M.S.; Paterson, C.; Ramesar, S.; Budhrani, P.; Carranza, I.; et al. Mindfulness Based Stress Reduction (MBSR(BC)) in Breast Cancer: Evaluating Fear of Recurrence (FOR) as a Mediator of Psychological and Physical Symptoms in a Randomized Control Trial (RCT). J. Behav. Med. 2014, 37, 185–195. [Google Scholar] [CrossRef]
- Zhu, P.; Wu, Q.; Liu, X.; Chen, C.; Ji, Q.; Shang, X. Effects of Mindfulness-Based Stress Reduction Therapy on Posttraumatic Growth and Quality of Life in Patients with Breast Cancer Under Early Chemotherapy: A Randomized Controlled Trial. Holist. Nurs. Pract. 2022. [Google Scholar] [CrossRef]
- Lengacher, C.A.; Reich, R.R.; Ramesar, S.; Alinat, C.B.; Moscoso, M.; Cousin, L.; Marino, V.R.; Elias, M.N.; Paterson, C.L.; Pleasant, M.L.; et al. Feasibility of the Mobile Mindfulness-Based Stress Reduction for Breast Cancer (mMBSR(BC)) Program for Symptom Improvement among Breast Cancer Survivors. Psychooncology 2018, 27, 524–531. [Google Scholar] [CrossRef]
- Sun, L.; Zhang, X.; Gong, P.; Zhang, L.; Zhao, Y. Clinical Efficacy of Bevacizumab Plus XELOX Chemotherapy in Colorectal Cancer and Application Value of Mindfulness-Based Stress Reduction Intervention. Altern. Ther. Health Med. 2022, 28, 65–71. [Google Scholar]
- Pollard, A.; Burchell, J.L.; Castle, D.; Neilson, K.; Ftanou, M.; Corry, J.; Rischin, D.; Kissane, D.W.; Krishnasamy, M.; Carlson, L.E.; et al. Individualised Mindfulness-Based Stress Reduction for Head and Neck Cancer Patients Undergoing Radiotherapy of Curative Intent: A Descriptive Pilot Study. Eur. J. Cancer Care 2017, 26, e12474. [Google Scholar] [CrossRef]
- Aminnasab, A.; Hatami, M.; Ahadi, H. Effectiveness of Mindfulness-Based Stress Reduction Therapy on the Quality of Life of Patients with Lung Cancer. Tanaffos 2022, 21, 503–511. [Google Scholar]
- Schellekens, M.P.J.; van den Hurk, D.G.M.; Prins, J.B.; Donders, A.R.T.; Molema, J.; Dekhuijzen, R.; van der Drift, M.A.; Speckens, A.E.M. Mindfulness-Based Stress Reduction Added to Care as Usual for Lung Cancer Patients and/or Their Partners: A Multicentre Randomized Controlled Trial. Psychooncology 2017, 26, 2118–2126. [Google Scholar] [CrossRef]
- Saban, K.L.; Motley, D.; Shawahin, L.; Mathews, H.L.; Tell, D.; De La Pena, P.; Janusek, L.W. Preliminary Evidence for a Race-Based Stress Reduction Intervention for Black Women at Risk for Cardiovascular Disease. Complement. Ther. Med. 2021, 58, 102710. [Google Scholar] [CrossRef]
- Momeni, J.; Omidi, A.; Raygan, F.; Akbari, H. The Effects of Mindfulness-Based Stress Reduction on Cardiac Patients’ Blood Pressure, Perceived Stress, and Anger: A Single-Blind Randomized Controlled Trial. J. Am. Soc. Hypertens. 2016, 10, 763–771. [Google Scholar] [CrossRef]
- Osama, H.; Rabea, H.M.; Abdelrahman, M.A. The Impact of Mindfulness-Based Stress Reduction on Psychological Health among Patients with Chronic Diseases during COVID-19 Outbreak Lockdown. Beni-Suef Univ. J. Basic Appl. Sci. 2023, 12, 50. [Google Scholar] [CrossRef]
- Mccubbin, T.; Dimidjian, S.; Kempe, K.; Glassey, M.S.; Ross, C.; Beck, A. Mindfulness-Based Stress Reduction in an Integrated Care Delivery System: One-Year Impacts on Patient-Centered Outcomes and Health Care Utilization. Perm. J. 2014, 18, 4–9. [Google Scholar] [CrossRef] [PubMed]
- Simpson, J.; Mapel, T. An Investigation into the Health Benefits of Mindfulness-Based Stress Reduction (MBSR) for People Living with a Range of Chronic Physical Illnesses in New Zealand. N. Z. Med. J. 2011, 124, 68–75. [Google Scholar]
- Vinesett, A.L.; Price, M.; Wilson, K.H. Therapeutic Potential of a Drum and Dance Ceremony Based on the African Ngoma Tradition. J. Altern. Complement. Med. 2015, 21, 460–465. [Google Scholar] [CrossRef] [PubMed]
- Beaulac, J.; Bailly, M. Mindfulness-Based Stress Reduction: Pilot Study of a Treatment Group for Patients with Chronic Pain in a Primary Care Setting. Prim. Health Care Res. Dev. 2015, 16, 424–428. [Google Scholar] [CrossRef]
- Braden, B.B.; Pipe, T.B.; Smith, R.; Glaspy, T.K.; Deatherage, B.R.; Baxter, L.C. Brain and Behavior Changes Associated with an Abbreviated 4-Week Mindfulness-Based Stress Reduction Course in Back Pain Patients. Brain Behav. 2016, 6, e00443. [Google Scholar] [CrossRef]
- Schmidt, S.; Gmeiner, S.; Schultz, C.; Löwer, M.; Kuhn, K.; Naranjo, J.R.; Brenneisen, C.; Hinterberger, T. Mindfulness-Based Stress Reduction (MBSR) as Treatment for Chronic Back Pain—An Observational Study with Assessment of Thalamocortical Dysrhythmia. Forsch. Komplementärmedizin/Res. Complement. Med. 2015, 22, 298–303. [Google Scholar] [CrossRef]
- Smith, A.M.; Leeming, A.; Fang, Z.; Hatchard, T.; Mioduszewski, O.; Schneider, M.A.; Ferdossifard, A.; Shergill, Y.; Khoo, E.-L.; Poulin, P. Mindfulness-Based Stress Reduction Alters Brain Activity for Breast Cancer Survivors with Chronic Neuropathic Pain: Preliminary Evidence from Resting-State fMRI. J. Cancer Surviv. Res. Pract. 2021, 15, 518–525. [Google Scholar] [CrossRef]
- Pérez-Aranda, A.; Feliu-Soler, A.; Montero-Marín, J.; García-Campayo, J.; Andrés-Rodríguez, L.; Borràs, X.; Rozadilla-Sacanell, A.; Peñarrubia-Maria, M.T.; Angarita-Osorio, N.; McCracken, L.M.; et al. A Randomized Controlled Efficacy Trial of Mindfulness-Based Stress Reduction Compared with an Active Control Group and Usual Care for Fibromyalgia: The EUDAIMON Study. Pain 2019, 160, 2508–2523. [Google Scholar] [CrossRef]
- Andrés-Rodríguez, L.; Borràs, X.; Feliu-Soler, A.; Pérez-Aranda, A.; Rozadilla-Sacanell, A.; Montero-Marin, J.; Maes, M.; Luciano, J.V. Immune-Inflammatory Pathways and Clinical Changes in Fibromyalgia Patients Treated with Mindfulness-Based Stress Reduction (MBSR): A Randomized, Controlled Clinical Trial. Brain Behav. Immun. 2019, 80, 109–119. [Google Scholar] [CrossRef] [PubMed]
- Simshäuser, K.; Lüking, M.; Kaube, H.; Schultz, C.; Schmidt, S. Is Mindfulness-Based Stress Reduction a Promising and Feasible Intervention for Patients Suffering from Migraine? A Randomized Controlled Pilot Trial. Complement. Med. Res. 2020, 27, 19–30. [Google Scholar] [CrossRef]
- Sampalli, T.; Berlasso, E.; Fox, R.; Petter, M. A Controlled Study of the Effect of a Mindfulness-Based Stress Reduction Technique in Women with Multiple Chemical Sensitivity, Chronic Fatigue Syndrome, and Fibromyalgia. J. Multidiscip. Healthc. 2009, 2, 53–59. [Google Scholar] [CrossRef]
- Zhu, X.; Hu, P.; Fan, Z.; Zhan, W.; Wang, H.; Yang, Y.; Zhou, Z.; Ma, L.; Gao, H. Effects of Mindfulness-Based Stress Reduction on Depression, Anxiety, and Pain in Patients with Postherpetic Neuralgia. J. Nerv. Ment. Dis. 2019, 207, 482–486. [Google Scholar] [CrossRef]
- Hou, Y.; Zhao, X.; Lu, M.; Lei, X.; Wu, Q.; Wang, X. Brief, One-on-One, Telephone-Adapted Mindfulness-Based Stress Reduction for Patients Undergoing Percutaneous Coronary Intervention: A Randomized Controlled Trial. Transl. Behav. Med. 2019, 9, 1216–1223. [Google Scholar] [CrossRef]
- Lundgren, O.; Garvin, P.; Nilsson, L.; Tornerefelt, V.; Andersson, G.; Kristenson, M.; Jonasson, L. Mindfulness-Based Stress Reduction for Coronary Artery Disease Patients: Potential Improvements in Mastery and Depressive Symptoms. J. Clin. Psychol. Med. Settings 2022, 29, 489–497. [Google Scholar] [CrossRef]
- Michalsen, A.; Grossman, P.; Lehmann, N.; Knoblauch, N.T.M.; Paul, A.; Moebus, S.; Budde, T.; Dobos, G.J. Psychological and Quality-of-Life Outcomes from a Comprehensive Stress Reduction and Lifestyle Program in Patients with Coronary Artery Disease: Results of a Randomized Trial. Psychother. Psychosom. 2005, 74, 344–352. [Google Scholar] [CrossRef]
- Rydén, M.; Hedbäck, B.; Jonasson, L. Does Stress Reduction Change the Levels of Cortisol Secretion in Patients with Coronary Artery Disease? J. Cardiopulm. Rehabil. Prev. 2009, 29, 314–317. [Google Scholar] [CrossRef]
- Blumenthal, J.A.; Sherwood, A.; Smith, P.J.; Watkins, L.; Mabe, S.; Kraus, W.E.; Ingle, K.; Miller, P.; Hinderliter, A. Enhancing Cardiac Rehabilitation with Stress Management Training: A Randomized, Clinical Efficacy Trial. Circulation 2016, 133, 1341–1350. [Google Scholar] [CrossRef]
- Parswani, M.J.; Sharma, M.P.; Iyengar, S. Mindfulness-Based Stress Reduction Program in Coronary Heart Disease: A Randomized Control Trial. Int. J. Yoga 2013, 6, 111–117. [Google Scholar] [CrossRef]
- Bokhari, S.; Schneider, R.H.; Salerno, J.W.; Rainforth, M.V.; Gaylord-King, C.; Nidich, S.I. Effects of Cardiac Rehabilitation with and without Meditation on Myocardial Blood Flow Using Quantitative Positron Emission Tomography: A Pilot Study. J. Nucl. Cardiol. Off. Publ. Am. Soc. Nucl. Cardiol. 2021, 28, 1596–1607. [Google Scholar] [CrossRef]
- Li, H.; Chen, H.; Ye, Z.; Li, X.; Yang, L.; Wang, S.; Yang, S.; Liu, S.; Chen, S.; Li, R.; et al. Effect of the Online Mindfulness-Based Stress Reduction on Anxiety and Depression Status of COVID-19 Patients Treated in Fangcang Hospitals: A Randomized Controlled Trial. Psychol. Res. Behav. Manag. 2023, 16, 2735–2745. [Google Scholar] [CrossRef]
- Güney, E.; Cengizhan, S.Ö.; Karataş Okyay, E.; Bal, Z.; Uçar, T. Effect of the Mindfulness-Based Stress Reduction Program on Stress, Anxiety, and Childbirth Fear in Pregnant Women Diagnosed with COVID-19. Complement. Ther. Clin. Pract. 2022, 47, 101566. [Google Scholar] [CrossRef]
- Sadooghiasl, A.; Ghalenow, H.R.; Mahinfar, K.; Hashemi, S.S. Effectiveness of Mindfulness-Based Stress Reduction Program in Improving Mental Well-Being of Patients with COVID-19: A Randomized Controlled Trial. Indian J. Crit. Care Med. Peer-Rev. Off. Publ. Indian Soc. Crit. Care Med. 2022, 26, 439–445. [Google Scholar] [CrossRef]
- Goren, G.; Schwartz, D.; Friger, M.; Banai, H.; Sergienko, R.; Regev, S.; Abu-Kaf, H.; Greenberg, D.; Nemirovsky, A.; Ilan, K.; et al. Randomized Controlled Trial of Cognitive-Behavioral and Mindfulness-Based Stress Reduction on the Quality of Life of Patients with Crohn Disease. Inflamm. Bowel Dis. 2022, 28, 393–408. [Google Scholar] [CrossRef]
- Bauer, N.; Löffler, C.; Oeznur, O.; Uecker, C.; Schlee, C.; Adamczyk, A.; Elsenbruch, S.S.; Pfuhlmann, K.; Reissmann, R.; Westendorf, A.; et al. Evaluation of a Multimodal Stress Management and Comprehensive Lifestyle Modification Program on Quality-of-Life and Gastrointestinal Symptoms in Patients with Crohn’s Disease—A Randomized Controlled Pilot Trial with Nine-Month Follow-Up. Digestion 2024, 105, 201–212. [Google Scholar] [CrossRef]
- Sanprakhon, P.; Chaimongkol, N.; Hengudomsub, P.; Lach, H.W. An Integrative Stress Reduction Program for Family Caregivers of Persons with Advanced Dementia: A Pilot Study. J. Gerontol. Nurs. 2022, 48, 26–32. [Google Scholar] [CrossRef]
- Berk, L.; Hotterbeekx, R.; van Os, J.; van Boxtel, M. Mindfulness-Based Stress Reduction in Middle-Aged and Older Adults with Memory Complaints: A Mixed-Methods Study. Aging Ment. Health 2018, 22, 1107–1114. [Google Scholar] [CrossRef]
- Chen, H.; Wang, Y.; Zhang, M.; Wang, N.; Li, Y.; Liu, Y. Effects of Animal-Assisted Therapy on Patients with Dementia: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Psychiatry Res. 2022, 314, 114619. [Google Scholar] [CrossRef]
- Poos, J.M.; van den Berg, E.; Papma, J.M.; van der Tholen, F.C.; Seelaar, H.; Donker Kaat, L.; Kievit, J.A.; Tibben, A.; van Swieten, J.C.; Jiskoot, L.C. Mindfulness-Based Stress Reduction in Pre-Symptomatic Genetic Frontotemporal Dementia: A Pilot Study. Front. Psychiatry 2022, 13, 864391. [Google Scholar] [CrossRef]
- Hazlett-Stevens, H.; Oren, Y. Effectiveness of Mindfulness-Based Stress Reduction Bibliotherapy: A Preliminary Randomized Controlled Trial. J. Clin. Psychol. 2017, 73, 626–637. [Google Scholar] [CrossRef]
- Shapiro, S.L.; Schwartz, G.E.; Bonner, G. Effects of Mindfulness-Based Stress Reduction on Medical and Premedical Students. J. Behav. Med. 1998, 21, 581–599. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Adiga, K.R.; George, A. Impact of Mindfulness-Based Stress Reduction (MBSR) on Depression among Elderly Residing in Residential Homes. Nurs. J. India 2014, 105, 248–251. [Google Scholar] [CrossRef] [PubMed]
- Javadzade, N.; Esmaeili, S.V.; Omranifard, V.; Zargar, F. Effect of Mindfulness-Based Stress Reduction (MBSR) Program on Depression, Emotion Regulation, and Sleep Problems: A Randomized Controlled Trial Study on Depressed Elderly. BMC Public Health 2024, 24, 271. [Google Scholar] [CrossRef]
- Charry-Sánchez, J.D.; Pradilla, I.; Talero-Gutiérrez, C. Animal-Assisted Therapy in Adults: A Systematic Review. Complement. Ther. Clin. Pract. 2018, 32, 169–180. [Google Scholar] [CrossRef]
- Kornfield, S.L.; Nicol, G.E.; Lenze, E.J.; Yingling, M.; Loebach Wetherell, J. Mindfulness-Based Stress Reduction in Older Individuals: Who Benefits the Most? Adv. Mind Body Med. 2022, 36, 4–12. [Google Scholar] [PubMed]
- Takagi, S.; Ohira, H. Effects of Expression and Inhibition of Negative Emotions on Health, Mood States, and Salivary Secretory Immunoglobulin A in Japanese Mildly Depressed Undergraduates. Percept. Mot. Skills 2004, 98, 1187–1198. [Google Scholar] [CrossRef]
- Smernoff, E.; Mitnik, I.; Lev-Ari, S. The Effects of Inquiry-Based Stress Reduction (IBSR) on Mental Health and Well-Being among a Non-Clinical Sample. Complement. Ther. Clin. Pract. 2019, 34, 30–34. [Google Scholar] [CrossRef]
- Chan, E.S.; Koh, D.; Teo, Y.C.; Hj Tamin, R.; Lim, A.; Fredericks, S. Biochemical and Psychometric Evaluation of Self-Healing Qigong as a Stress Reduction Tool among First Year Nursing and Midwifery Students. Complement. Ther. Clin. Pract. 2013, 19, 179–183. [Google Scholar] [CrossRef]
- Pereira, M.G.; Pedras, S.; Louro, A.; Lopes, A.; Vilaça, M. Stress Reduction Interventions for Patients with Chronic Diabetic Foot Ulcers: A Qualitative Study into Patients and Caregivers’ Perceptions. J. Foot Ankle Res. 2023, 16, 3. [Google Scholar] [CrossRef]
- Zeinabeh, M.Z.; Atefeh, A.; Masumeh, G.H.P.; Tania, D.; Mojgan, S.; Katayoun, A. The Effect of Mindfulness-Based Stress Reduction Counseling on Blood Glucose and Perceived Stress in Women with Gestational Diabetes. Rev. Bras. Ginecol. E Obs. /RBGO Gynecol. Obstet. 2023, 45, e517–e523. [Google Scholar] [CrossRef] [PubMed]
- Xia, T.; Lopes, S.; Chen, L.; Roth, R.; Zinzow, H.; Jones, K.; Zhang, L.; Shi, L.; Jindal, M. A Feasibility Study on Low-Dose Mindfulness-Based Stress Reduction Intervention among Prediabetes and Diabetes Patients. Complement. Ther. Med. 2022, 65, 102810. [Google Scholar] [CrossRef]
- Rosenzweig, S.; Reibel, D.K.; Greeson, J.M.; Edman, J.S.; Jasser, S.A.; McMearty, K.D.; Goldstein, B.J. Mindfulness-Based Stress Reduction Is Associated with Improved Glycemic Control in Type 2 Diabetes Mellitus: A Pilot Study. Altern. Ther. Health Med. 2007, 13, 36–38. [Google Scholar]
- Jung, H.Y.; Lee, H.; Park, J. Comparison of the Effects of Korean Mindfulness-Based Stress Reduction, Walking, and Patient Education in Diabetes Mellitus. Nurs. Health Sci. 2015, 17, 516–525. [Google Scholar] [CrossRef]
- Yoo, J.-S.; Lee, S.-J.; Lee, H.-C.; Kim, M.-J. The Effect of a Comprehensive Lifestyle Modification Program on Glycemic Control and Body Composition in Patients with Type 2 Diabetes. Asian Nurs. Res. 2007, 1, 106–115. [Google Scholar] [CrossRef]
- Hecht, F.M.; Moskowitz, J.T.; Moran, P.; Epel, E.S.; Bacchetti, P.; Acree, M.; Kemeny, M.E.; Mendes, W.B.; Duncan, L.G.; Weng, H.; et al. A Randomized, Controlled Trial of Mindfulness-Based Stress Reduction in HIV Infection. Brain Behav. Immun. 2018, 73, 331–339. [Google Scholar] [CrossRef] [PubMed]
- Robinson, F.P.; Mathews, H.L.; Witek-Janusek, L. Psycho-Endocrine-Immune Response to Mindfulness-Based Stress Reduction in Individuals Infected with the Human Immunodeficiency Virus: A Quasiexperimental Study. J. Altern. Complement. Med. 2003, 9, 683–694. [Google Scholar] [CrossRef]
- SeyedAlinaghi, S.; Jam, S.; Foroughi, M.; Imani, A.; Mohraz, M.; Djavid, G.E.; Black, D.S. RCT of Mindfulness-Based Stress Reduction Delivered to HIV+ Patients in Iran: Effects on CD4+ T Lymphocyte Count and Medical and Psychological Symptoms. Psychosom. Med. 2012, 74, 620–627. [Google Scholar] [CrossRef] [PubMed]
- Moskowitz, J.T.; Sharma, B.; Javandel, S.; Moran, P.; Paul, R.; De Gruttola, V.; Tomov, D.; Azmy, H.; Sandoval, R.; Hillis, M.; et al. Mindfulness-Based Stress Reduction for Symptom Management in Older Individuals with HIV-Associated Neurocognitive Disorder. AIDS Behav. 2024, 28, 1811–1821. [Google Scholar] [CrossRef]
- Chhatre, S.; Metzger, D.S.; Frank, I.; Boyer, J.; Thompson, E.; Nidich, S.; Montaner, L.J.; Jayadevappa, R. Effects of Behavioral Stress Reduction Transcendental Meditation Intervention in Persons with HIV. AIDS Care 2013, 25, 1291–1297. [Google Scholar] [CrossRef]
- Jam, S.; Imani, A.H.; Foroughi, M.; SeyedAlinaghi, S.; Koochak, H.E.; Mohraz, M. The Effects of Mindfulness-Based Stress Reduction (MBSR) Program in Iranian HIV/AIDS Patients: A Pilot Study. Acta Med. Iran. 2010, 48, 101–106. [Google Scholar] [PubMed]
- Duncan, L.G.; Moskowitz, J.T.; Neilands, T.B.; Dilworth, S.E.; Hecht, F.M.; Johnson, M.O. Mindfulness-Based Stress Reduction for HIV Treatment Side Effects: A Randomized, Wait-List Controlled Trial. J. Pain Symptom Manag. 2012, 43, 161–171. [Google Scholar] [CrossRef] [PubMed]
- McCraty, R.; Atkinson, M.; Tomasino, D. Impact of a Workplace Stress Reduction Program on Blood Pressure and Emotional Health in Hypertensive Employees. Altern. Complement. Med. 2003, 9, 355–369. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.K.P.; Yeung, N.C.Y.; Xu, Z.; Zhang, D.; Yu, C.-P.; Wong, S.Y.S. Effect and Acceptability of Mindfulness-Based Stress Reduction Program on Patients with Elevated Blood Pressure or Hypertension: A Meta-Analysis of Randomized Controlled Trials. Hypertension 2020, 76, 1992–2001. [Google Scholar] [CrossRef] [PubMed]
- Schneider, R.H.; Myers, H.F.; Marwaha, K.; Rainforth, M.A.; Salerno, J.W.; Nidich, S.I.; Gaylord-King, C.; Alexander, C.N.; Norris, K.C. Stress Reduction in the Prevention of Left Ventricular Hypertrophy: A Randomized Controlled Trial of Transcendental Meditation and Health Education in Hypertensive African Americans. Ethn. Dis. 2019, 29, 577–586. [Google Scholar] [CrossRef] [PubMed]
- Katsarou, A.L.; Vryonis, M.M.; Protogerou, A.D.; Alexopoulos, E.C.; Achimastos, A.; Papadogiannis, D.; Chrousos, G.P.; Darviri, C. Stress Management and Dietary Counseling in Hypertensive Patients: A Pilot Study of Additional Effect. Prim. Health Care Res. Dev. 2014, 15, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Arefnasab, Z.; Babamahmoodi, A.; Babamahmoodi, F.; Noorbala, A.A.; Alipour, A.; Panahi, Y.; Shams, J.; Riazi Rad, F.; Khaze, V.; Ghanei, M. Mindfulness-Based Stress Reduction (MBSR) and Its Effects on Psychoimmunological Factors of Chemically Pulmonary Injured Veterans. Iran. J. Allergy Asthma Immunol. 2016, 15, 476–486. [Google Scholar] [PubMed]
- Arefnasab, Z.; Ghanei, M.; Noorbala, A.A.; Alipour, A.; Babamahmoodi, F.; Babamahmoodi, A.; Salehi, M. Effect of Mindfulness Based Stress Reduction on Quality of Life (SF-36) and Spirometry Parameters, in Chemically Pulmonary Injured Veterans. Iran. J. Public Health 2013, 42, 1026–1033. [Google Scholar] [PubMed]
- Mohammed, W.A.; Pappous, A.; Sharma, D. Effect of Mindfulness Based Stress Reduction (MBSR) in Increasing Pain Tolerance and Improving the Mental Health of Injured Athletes. Front. Psychol. 2018, 9, 722. [Google Scholar] [CrossRef]
- Meesters, A.; den Bosch-Meevissen, Y.M.C.I.; Weijzen, C.A.H.; Buurman, W.A.; Losen, M.; Schepers, J.; Thissen, M.R.T.M.; Alberts, H.J.E.M.; Schalkwijk, C.G.; Peters, M.L. The Effect of Mindfulness-Based Stress Reduction on Wound Healing: A Preliminary Study. J. Behav. Med. 2018, 41, 385–397. [Google Scholar] [CrossRef]
- Garland, S.N.; Carlson, L.E.; Stephens, A.J.; Antle, M.C.; Samuels, C.; Campbell, T.S. Mindfulness-Based Stress Reduction Compared with Cognitive Behavioral Therapy for the Treatment of Insomnia Comorbid with Cancer: A Randomized, Partially Blinded, Noninferiority Trial. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2014, 32, 449–457. [Google Scholar] [CrossRef] [PubMed]
- Sgalla, G.; Cerri, S.; Ferrari, R.; Ricchieri, M.P.; Poletti, S.; Ori, M.; Garuti, M.; Montanari, G.; Luppi, F.; Petropulacos, K.; et al. Mindfulness-Based Stress Reduction in Patients with Interstitial Lung Diseases: A Pilot, Single-Centre Observational Study on Safety and Efficacy. BMJ Open Respir. Res. 2015, 2, e000065. [Google Scholar] [CrossRef] [PubMed]
- Ghandi, F.; Sadeghi, A.; Bakhtyari, M.; Imani, S.; Abdi, S.; Banihashem, S.S. Comparing the Efficacy of Mindfulness-Based Stress Reduction Therapy with Emotion Regulation Treatment on Quality of Life and Symptoms of Irritable Bowel Syndrome. Iran. J. Psychiatry 2018, 13, 175–183. [Google Scholar] [PubMed]
- Peerani, F.; Watt, M.; Ismond, K.P.; Whitlock, R.; Ambrosio, L.; Hotte, N.; Mitchell, N.; Bailey, R.J.; Kroeker, K.; Dieleman, L.A.; et al. A Randomized Controlled Trial of a Multicomponent Online Stress Reduction Intervention in Inflammatory Bowel Disease. Ther. Adv. Gastroenterol. 2022, 15, 17562848221127238. [Google Scholar] [CrossRef] [PubMed]
- Yazdani Aliabadi, M.; Javadnoori, M.; Saki Malehi, A.; Aslani, K. A Study of Mindfulness-Based Stress-Reduction Training Effects on Menopause-Specific Quality of Life in Postmenopausal Women: A Randomized Controlled Trial. Complement. Ther. Clin. Pract. 2021, 44, 101398. [Google Scholar] [CrossRef] [PubMed]
- Şener, N.; Timur Taşhan, S. The Effects of Mindfulness Stress Reduction Program on Postmenopausal Women’s Menopausal Complaints and Their Life Quality. Complement. Ther. Clin. Pract. 2021, 45, 101478. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.; Yip, B.H.-K.; Gao, T.; Lam, K.Y.Y.; Woo, D.M.S.; Yip, A.L.K.; Chin, C.Y.; Tang, W.P.Y.; Choy, M.M.T.; Tsang, K.W.K.; et al. Mindfulness-Based Stress Reduction (MBSR) or Psychoeducation for the Reduction of Menopausal Symptoms: A Randomized, Controlled Clinical Trial. Sci. Rep. 2018, 8, 6609. [Google Scholar] [CrossRef] [PubMed]
- Monin, J.K.; Sperduto, C.M.; Manigault, A.W.; Dutton, A.; Ali, A.; Clark, M.S.; Jastreboff, A.M. Mindfulnes-Based Stress Reduction for Older Couples with Metabolic Syndrome: A Pilot Randomized Controlled Trial. Mindfulness 2020, 11, 917–927. [Google Scholar] [CrossRef]
- Kolahkaj, B.; Zargar, F.; Majdinasab, N. The Effect of Mindfulness-Based Stress Reduction (MBSR) Therapy on Quality of Life in Women with Multiple Sclerosis, Ahvaz, Iran. J. Caring Sci. 2019, 8, 213–217. [Google Scholar] [CrossRef][Green Version]
- Blankespoor, R.J.; Schellekens, M.P.J.; Vos, S.H.; Speckens, A.E.M.; de Jong, B.A. The Effectiveness of Mindfulness-Based Stress Reduction on Psychological Distress and Cognitive Functioning in Patients with Multiple Sclerosis: A Pilot Study. Mindfulness 2017, 8, 1251–1258. [Google Scholar] [CrossRef]
- Kolahkaj, B.; Zargar, F. Effect of Mindfulness-Based Stress Reduction on Anxiety, Depression and Stress in Women with Multiple Sclerosis. Nurs. Midwifery Stud. 2015, 4, e29655. [Google Scholar] [CrossRef] [PubMed]
- Salajegheh, Z.; Ahmadi, A.; Shahrahmani, H.; Jahani, Y.; Alidousti, K.; Nasiri Amiri, F.; Salari, Z. Mindfulness-Based Stress Reduction (MBSR) Effects on the Worries of Women with Poly Cystic Ovary Syndrome (PCOS). BMC Psychiatry 2023, 23, 185. [Google Scholar] [CrossRef] [PubMed]
- Fordham, B.; Griffiths, C.E.M.; Bundy, C. Can Stress Reduction Interventions Improve Psoriasis? A Review. Psychol. Health Med. 2013, 18, 501–514. [Google Scholar] [CrossRef] [PubMed]
- Woldemariam, S.; Ashman, D.; Carvalho, E.; Wong, S.-L.; Hoersting, R. AIP-Based Professional Intervention Program for Adversity for Trauma and Stress Reduction in Groups: A Pilot Study in Ethiopia. Front. Psychiatry 2024, 15, 1351713. [Google Scholar] [CrossRef] [PubMed]
- Karadag, M.; Gokcen, C.; Sarp, A.S. EMDR Therapy in Children and Adolescents Who Have Post-Traumatic Stress Disorder: A Six-Week Follow-up Study. Int. J. Psychiatry Clin. Pract. 2020, 24, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Kearney, D.J.; Malte, C.A.; Storms, M.; Simpson, T.L. Loving-Kindness Meditation vs Cognitive Processing Therapy for Posttraumatic Stress Disorder Among Veterans: A Randomized Clinical Trial. JAMA Netw. Open 2021, 4, e216604. [Google Scholar] [CrossRef] [PubMed]
- Pradhan, E.K.; Baumgarten, M.; Langenberg, P.; Handwerger, B.; Gilpin, A.K.; Magyari, T.; Hochberg, M.C.; Berman, B.M. Effect of Mindfulness-Based Stress Reduction in Rheumatoid Arthritis Patients. Arthritis Rheum. 2007, 57, 1134–1142. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.-T.; Hsieh, T.-L.; Chen, M.-L.; Tseng, W.-T.; Hung, C.-F.; Chen, C.-R. Animal-Assisted Therapy in Middle-Aged and Older Patients with Schizophrenia: A Randomized Controlled Trial. Front. Psychiatry 2021, 12, 713623. [Google Scholar] [CrossRef] [PubMed]
- Özdemir, A.A.; Kavak Budak, F. The Effects of Mindfulness-Based Stress Reduction Training on Hope, Psychological Well-Being, and Functional Recovery in Patients with Schizophrenia. Clin. Nurs. Res. 2022, 31, 183–193. [Google Scholar] [CrossRef] [PubMed]
- Kim, A.S.; Jang, M.H.; Sun, M.J. Effects of Mindfulness-Based Stress Reduction (MBSR) on Stress, Heart Rate Variability, Affect, and Wellbeing among People with Schizophrenia. Int. J. Environ. Res. Public. Health 2021, 18, 11871. [Google Scholar] [CrossRef]
- Feldman, O.; Goldstien, E.; Rolnik, B.; Ganz, A.B.; Lev-Ari, S. Inquiry Based Stress Reduction (IBSR) Improves Overall Stuttering Experience among Adults Who Stutter: A Randomized Controlled Trial. J. Clin. Med. 2021, 10, 2187. [Google Scholar] [CrossRef] [PubMed]
- Ardi, Z.; Golland, Y.; Shafir, R.; Sheppes, G.; Levit-Binnun, N. The Effects of Mindfulness-Based Stress Reduction on the Association between Autonomic Interoceptive Signals and Emotion Regulation Selection. Psychosom. Med. 2021, 83, 852–862. [Google Scholar] [CrossRef] [PubMed]
- Gura, N. Parental families as a source forming adult women’s conditional reactions and behavioral patterns. Psychol. J. 2020, 6, 114–126. [Google Scholar] [CrossRef]
- Kilpatrick, L.A.; Suyenobu, B.Y.; Smith, S.R.; Bueller, J.A.; Goodman, T.; Creswell, J.D.; Tillisch, K.; Mayer, E.A.; Naliboff, B.D. Impact of Mindfulness-Based Stress Reduction Training on Intrinsic Brain Connectivity. NeuroImage 2011, 56, 290–298. [Google Scholar] [CrossRef] [PubMed]
- Fancourt, D.; Aufegger, L.; Williamon, A. Low-Stress and High-Stress Singing Have Contrasting Effects on Glucocorticoid Response. Front. Psychol. 2015, 6, 1242. [Google Scholar] [CrossRef] [PubMed]
- Vaughn, D.A.; Maggiora, M.B.; Vaughn, K.J.; Maggiora, C.J.; Tavakoli, A.-V.; Liang, W.; Zava, D.; Cohen, M.S.; Lenartowicz, A. Modulation of Attention and Stress with Arousal: The Mental and Physical Effects of Riding a Motorcycle. Brain Res. 2021, 1752, 147203. [Google Scholar] [CrossRef] [PubMed]
- Snippe, E.; Nyklíček, I.; Schroevers, M.J.; Bos, E.H. The Temporal Order of Change in Daily Mindfulness and Affect during Mindfulness-Based Stress Reduction. J. Couns. Psychol. 2015, 62, 106–114. [Google Scholar] [CrossRef] [PubMed]
- Aziraj-Smajić, V.; de la Fosse, C. EMDR Techniques and Behavioral Therapy in Group Training Dealing with Stress. Psychiatr. Danub. 2021, 33, 24–28. [Google Scholar] [PubMed]
- Esch, T.; Duckstein, J.; Welke, J.; Braun, V. Mind/Body Techniques for Physiological and Psychological Stress Reduction: Stress Management via Tai Chi Training—A Pilot Study. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2007, 13, CR488–CR497. [Google Scholar]
- Wong, G.; Sun, R.; Adler, J.; Yeung, K.W.; Yu, S.; Gao, J. Loving-Kindness Meditation (LKM) Modulates Brain-Heart Connection: An EEG Case Study. Front. Hum. Neurosci. 2022, 16, 891377. [Google Scholar] [CrossRef]
- Martín-Asuero, A.; García-Banda, G. The Mindfulness-Based Stress Reduction Program (MBSR) Reduces Stress-Related Psychological Distress in Healthcare Professionals. Span. J. Psychol. 2010, 13, 897–905. [Google Scholar] [CrossRef] [PubMed]
- Weitlauf, A.S.; Broderick, N.; Stainbrook, J.A.; Taylor, J.L.; Herrington, C.G.; Nicholson, A.G.; Santulli, M.; Dykens, E.M.; Juárez, A.P.; Warren, Z.E. Mindfulness-Based Stress Reduction for Parents Implementing Early Intervention for Autism: An RCT. Pediatrics 2020, 145, S81–S92. [Google Scholar] [CrossRef]
- Roberts, L.R.; Boostrom, G.G.; Dehom, S.O.; Neece, C.L. Self-Reported Parenting Stress and Cortisol Awakening Response Following Mindfulness-Based Stress Reduction Intervention for Parents of Children with Developmental Delays: A Pilot Study. Biol. Res. Nurs. 2020, 22, 217–225. [Google Scholar] [CrossRef]
- Shahidi, S.; Zargar, F.; Aghaee Khajelangi, H.; Tarrahi, M.J. The Effect of Internet-Delivered Mindfulness Stress Reduction Combined with Acceptance and Commitment Therapy on Health Anxiety and Quality of Life of Caregiver of Patients Infected by COVID-19: A Randomized Clinical Trial. Int. J. Community Based Nurs. Midwifery 2023, 11, 110–121. [Google Scholar] [CrossRef]
- Sui, Y.; Kor, P.P.K.; Li, M.; Wang, J. Effects of a Social Media-Based Mind-Body Intervention Embedded with Acupressure and Mindfulness for Stress Reduction Among Family Caregivers of Frail Older Adults: Pilot Randomized Controlled Trial. JMIR Form. Res. 2023, 7, e42861. [Google Scholar] [CrossRef] [PubMed]
- Laudenslager, M.L.; Simoneau, T.L.; Mikulich-Gilbertson, S.K.; Natvig, C.; Brewer, B.W.; Sannes, T.S.; Kilbourn, K.; Gutman, J.; McSweeney, P. A Randomized Control Trial of Stress Management for Caregivers of Stem Cell Transplant Patients: Effect on Patient Quality of Life and Caregiver Distress. Psychooncology 2019, 28, 1614–1623. [Google Scholar] [CrossRef]
- Ouseph, R.; Croy, C.; Natvig, C.; Simoneau, T.; Laudenslager, M.L. Decreased Mental Health Care Utilization Following a Psychosocial Intervention in Caregivers of Hematopoietic Stem Cell Transplant Patients. Ment. Illn. 2014, 6, 5120. [Google Scholar] [CrossRef]
- Cheung, D.S.K.; Kor, P.P.K.; Jones, C.; Davies, N.; Moyle, W.; Chien, W.T.; Yip, A.L.K.; Chambers, S.; Yu, C.T.K.; Lai, C.K.Y. The Use of Modified Mindfulness-Based Stress Reduction and Mindfulness-Based Cognitive Therapy Program for Family Caregivers of People Living with Dementia: A Feasibility Study. Asian Nurs. Res. 2020, 14, 221–230. [Google Scholar] [CrossRef] [PubMed]
- Amiri, P.; Mirghafourvand, M.; Esmaeilpour, K.; Kamalifard, M.; Ivanbagha, R. The Effect of Distraction Techniques on Pain and Stress during Labor: A Randomized Controlled Clinical Trial. BMC Pregnancy Childbirth 2019, 19, 534. [Google Scholar] [CrossRef]
- Azizi, E.; Maleki, A.; Mazloomzadeh, S.; Pirzeh, R. Effect of Stress Management Counseling on Self-Efficacy and Continuity of Exclusive Breastfeeding. Breastfeed. Med. Off. J. Acad. Breastfeed. Med. 2020, 15, 501–508. [Google Scholar] [CrossRef]
- Shamsdanesh, S.; Nourizadeh, R.; Hakimi, S.; Ranjbar, F.; Mehrabi, E. The Effect of Counseling with Stress Management Approach on Postpartum Anxiety and Distress and Breastfeeding Self-Efficacy during COVID-19 Pandemic: A Ramdomized Controlled Trial. BMC Pregnancy Childbirth 2023, 23, 26. [Google Scholar] [CrossRef] [PubMed]
- Delgado, C.; Toukonen, M.; Wheeler, C. Effect of Canine Play Interventions as a Stress Reduction Strategy in College Students. Nurse Educ. 2018, 43, 149–153. [Google Scholar] [CrossRef]
- Bergen-Cico, D.; Possemato, K.; Cheon, S. Examining the Efficacy of a Brief Mindfulness-Based Stress Reduction (Brief MBSR) Program on Psychological Health. J. Am. Coll. Health 2013, 61, 348–360. [Google Scholar] [CrossRef]
- Gouda, S.; Luong, M.T.; Schmidt, S.; Bauer, J. Students and Teachers Benefit from Mindfulness-Based Stress Reduction in a School-Embedded Pilot Study. Front. Psychol. 2016, 7, 590. [Google Scholar] [CrossRef]
- Deshpande, A.G.; Johnson, J.R.; Casta, A.M.; Marien, M.S.; Reiff, M. The Impact of a Mindfulness-Based Stress Reduction Program on University Students’ Mental Health: A Mixed-Methods Evaluation. J. Am. Coll. Health 2023, 1–11. [Google Scholar] [CrossRef]
- Rosenzweig, S.; Reibel, D.K.; Greeson, J.M.; Brainard, G.C.; Hojat, M. Mindfulness-Based Stress Reduction Lowers Psychological Distress in Medical Students. Teach. Learn. Med. 2003, 15, 88–92. [Google Scholar] [CrossRef]
- Gebhart, V.; Buchberger, W.; Klotz, I.; Neururer, S.; Rungg, C.; Tucek, G.; Zenzmaier, C.; Perkhofer, S. Distraction-Focused Interventions on Examination Stress in Nursing Students: Effects on Psychological Stress and Biomarker Levels. A Randomized Controlled Trial. Int. J. Nurs. Pract. 2020, 26, e12788. [Google Scholar] [CrossRef]
- An, A.; Hoang, H.; Trang, L.; Vo, Q.; Tran, L.; Le, T.; Le, A.; McCormick, A.; Du Old, K.; Williams, N.S.; et al. Investigating the Effect of Mindfulness-Based Stress Reduction on Stress Level and Brain Activity of College Students. IBRO Neurosci. Rep. 2022, 12, 399–410. [Google Scholar] [CrossRef]
- Accoto, A.; Chiarella, S.G.; Raffone, A.; Montano, A.; de Marco, A.; Mainiero, F.; Rubbino, R.; Valzania, A.; Conversi, D. Beneficial Effects of Mindfulness-Based Stress Reduction Training on the Well-Being of a Female Sample during the First Total Lockdown Due to COVID-19 Pandemic in Italy. Int. J. Environ. Res. Public. Health 2021, 18, 5512. [Google Scholar] [CrossRef] [PubMed]
- Gawrysiak, M.J.; Grassetti, S.N.; Greeson, J.M.; Shorey, R.C.; Pohlig, R.; Baime, M.J. The Many Facets of Mindfulness and the Prediction of Change Following Mindfulness-Based Stress Reduction (MBSR). J. Clin. Psychol. 2018, 74, 523–535. [Google Scholar] [CrossRef]
- Kotwal, M.R.; Rinchhen, C.Z.; Ringe, V.V. Stress Reduction through Listening to Indian Classical Music during Gastroscopy. Diagn. Ther. Endosc. 1998, 4, 191–197. [Google Scholar] [CrossRef]
- Schneider, N.; Schedlowski, M.; Schürmeyer, T.H.; Becker, H. Stress Reduction through Music in Patients Undergoing Cerebral Angiography. Neuroradiology 2001, 43, 472–476. [Google Scholar] [CrossRef] [PubMed]
- Cheung, C.W.C.; Yee, A.W.W.; Chan, P.S.; Saravelos, S.H.; Chung, J.P.W.; Cheung, L.P.; Kong, G.W.S.; Li, T.-C. The Impact of Music Therapy on Pain and Stress Reduction during Oocyte Retrieval—A Randomized Controlled Trial. Reprod. Biomed. Online 2018, 37, 145–152. [Google Scholar] [CrossRef]
- Corah, N.L.; Gale, E.N.; Illig, S.J. Psychological Stress Reduction during Dental Procedures. J. Dent. Res. 1979, 58, 1347–1351. [Google Scholar] [CrossRef] [PubMed]
- Landau, C.; Novak, A.M.; Ganz, A.B.; Rolnik, B.; Friedman, E.; Lev-Ari, S. Effect of Inquiry-Based Stress Reduction on Well-Being and Views on Risk-Reducing Surgery Among Women with BRCA Variants in Israel: A Randomized Clinical Trial. JAMA Netw. Open 2021, 4, e2139670. [Google Scholar] [CrossRef]
- Guo, D.; Sun, L.; Yu, X.; Liu, T.; Wu, L.; Sun, Z.; Zhang, F.; Zhou, Y.; Shen, M.; Liu, W. Mindfulness-Based Stress Reduction Improves the General Health and Stress of Chinese Military Recruits: A Pilot Study. Psychiatry Res. 2019, 281, 112571. [Google Scholar] [CrossRef] [PubMed]
- Kang, H.; Seo, J.-B.; Hwang, I.-Y. Mindfulness-Based Stress Reduction for Stress, Anxiety, and Psychological Well-Being: Effects in a Republic of Korea Navy Fleet Crew. J. Psychosoc. Nurs. Ment. Health Serv. 2020, 58, 48–55. [Google Scholar] [CrossRef]
- Kluepfel, L.; Ward, T.; Yehuda, R.; Dimoulas, E.; Smith, A.; Daly, K. The Evaluation of Mindfulness-Based Stress Reduction for Veterans with Mental Health Conditions. J. Holist. Nurs. Off. J. Am. Holist. Nurses Assoc. 2013, 31, 248–255. [Google Scholar] [CrossRef] [PubMed]
- Khodabandeh Shahraki, S.; Adelian, H.; Miri, S.; Farokhzadian, J. Using Mindfulness-Based Stress Reduction Group Therapy to Reduce Perceived Stress of Vulnerable Women in South of Iran. Psychol. Health Med. 2023, 28, 582–594. [Google Scholar] [CrossRef]
- Jabson Tree, J.M.; Patterson, J.G. A Test of Feasibility and Acceptability of Online Mindfulness-Based Stress Reduction for Lesbian, Gay, and Bisexual Women and Men at Risk for High Stress: Pilot Study. JMIR Ment. Health 2019, 6, e15048. [Google Scholar] [CrossRef]
- Khatib, L.; Riegner, G.; Dean, J.G.; Oliva, V.; Cruanes, G.; Mulligan, B.A.; Zeidan, F. The Effects of Mindfulness-Based Stress Reduction on Trauma in Victims of Gun Violence: A Pilot Study. Mindfulness 2022, 13, 1032–1041. [Google Scholar] [CrossRef] [PubMed]
- Klatt, M.D.; Buckworth, J.; Malarkey, W.B. Effects of Low-Dose Mindfulness-Based Stress Reduction (MBSR-Ld) on Working Adults. Health Educ. Behav. Off. Publ. Soc. Public Health Educ. 2009, 36, 601–614. [Google Scholar] [CrossRef] [PubMed]
- Bravo-Mehmedbasic, A.; Salcic, D.; Kucukalic, A.; Fadilpasic, S.; Cakovic, L.; Mehmedika-Suljic, E.; Masic, I. Impact of Psychoeducation on Professional Stress Reduction among Prison Guards. Mater. Socio-Medica 2009, 21, 24–26. [Google Scholar] [CrossRef]
- Pignata, S.; Winefield, A.H. Stress-Reduction Interventions in an Australian University: A Case Study. Stress Health J. Int. Soc. Investig. Stress 2015, 31, 24–34. [Google Scholar] [CrossRef] [PubMed]
- Żołnierczyk-Zreda, D.; Sanderson, M.; Bedyńska, S. Mindfulness-Based Stress Reduction for Managers: A Randomized Controlled Study. Occup. Med. Oxf. Engl. 2016, 66, 630–635. [Google Scholar] [CrossRef]
- Hwang, H.; Kim, S.M.; Netterstrøm, B.; Han, D.H. The Efficacy of a Smartphone-Based App on Stress Reduction: Randomized Controlled Trial. J. Med. Internet Res. 2022, 24, e28703. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Martínez, M.D.C.; De la Plana Maestre, A.; Armenta-Peinado, J.A.; Barbancho, M.Á.; García-Casares, N. Evidence of Animal-Assisted Therapy in Neurological Diseases in Adults: A Systematic Review. Int. J. Environ. Res. Public. Health 2021, 18, 12882. [Google Scholar] [CrossRef] [PubMed]
- Taub, R.; Horesh, D.; Rubin, N.; Glick, I.; Reem, O.; Shriqui, G.; Agmon-Levin, N. Mindfulness-Based Stress Reduction for Systemic Lupus Erythematosus: A Mixed-Methods Pilot Randomized Controlled Trial of an Adapted Protocol. J. Clin. Med. 2021, 10, 4450. [Google Scholar] [CrossRef]
- Greco, C.M.; Rudy, T.E.; Manzi, S. Effects of a Stress-Reduction Program on Psychological Function, Pain, and Physical Function of Systemic Lupus Erythematosus Patients: A Randomized Controlled Trial. Arthritis Rheum. 2004, 51, 625–634. [Google Scholar] [CrossRef]
- El Aoufy, K.; Pezzutto, A.; Pollina, A.; Rasero, L.; Bambi, S.; Bellando-Randone, S.; Guiducci, S.; Maddali-Bongi, S.; Matucci Cerinic, M. Systemic Sclerosis Patients Experiencing Mindfulness-Based Stress Reduction Program: The Beneficial Effect on Their Psychological Status and Quality of Life. Int. J. Environ. Res. Public. Health 2023, 20, 2512. [Google Scholar] [CrossRef]
- Omidi, A.; Zargar, F. Effects of Mindfulness-Based Stress Reduction on Perceived Stress and Psychological Health in Patients with Tension Headache. J. Res. Med. Sci. Off. J. Isfahan Univ. Med. Sci. 2015, 20, 1058–1063. [Google Scholar] [CrossRef]
- Ghonchehpour, A.; Forouzi, M.A.; Dehghan, M.; Ahmadi, A.; Okou, G.; Tirgari, B. The Effect of Mindfulness-Based Stress Reduction on Rejection Sensitivity and Resilience in Patients with Thalassemia: A Randomized Controlled Trial. BMC Psychiatry 2023, 23, 281. [Google Scholar] [CrossRef]
- Schlee, C.; Uecker, C.; Bauer, N.; Koch, A.K.; Langhorst, J. Multimodal Stress Reduction and Lifestyle Modification Program for Patients with Ulcerative Colitis: A Qualitative Study. BMC Complement. Med. Ther. 2022, 22, 60. [Google Scholar] [CrossRef]
- Jedel, S.; Hoffman, A.; Merriman, P.; Swanson, B.; Voigt, R.; Rajan, K.B.; Shaikh, M.; Li, H.; Keshavarzian, A. A Randomized Controlled Trial of Mindfulness-Based Stress Reduction to Prevent Flare-up in Patients with Inactive Ulcerative Colitis. Digestion 2014, 89, 142–155. [Google Scholar] [CrossRef]
- Langhorst, J.; Mueller, T.; Luedtke, R.; Franken, U.; Paul, A.; Michalsen, A.; Schedlowski, M.; Dobos, G.J.; Elsenbruch, S. Effects of a Comprehensive Lifestyle Modification Program on Quality-of-Life in Patients with Ulcerative Colitis: A Twelve-Month Follow-Up. Scand. J. Gastroenterol. 2007, 42, 734–745. [Google Scholar] [CrossRef]
- Oikonomou, M.T.; Arvanitis, M.; Sokolove, R.L. Mindfulness Training for Smoking Cessation: A Meta-Analysis of Randomized-Controlled Trials. J. Health Psychol. 2017, 22, 1841–1850. [Google Scholar] [CrossRef] [PubMed]
- Marcus, D.A. The Science behind Animal-Assisted Therapy. Curr. Pain Headache Rep. 2013, 17, 322. [Google Scholar] [CrossRef] [PubMed]
- Yinger, O.S.; Gooding, L. Music Therapy and Music Medicine for Children and Adolescents. Child Adolesc. Psychiatr. Clin. N. Am. 2014, 23, 535–553. [Google Scholar] [CrossRef]
- Bullack, A.; Gass, C.; Nater, U.M.; Kreutz, G. Psychobiological Effects of Choral Singing on Affective State, Social Connectedness, and Stress: Influences of Singing Activity and Time Course. Front. Behav. Neurosci. 2018, 12, 223. [Google Scholar] [CrossRef] [PubMed]
- Crino, O.L.; Larkin, I.; Phelps, S.M. Stress Coping Styles and Singing Behavior in the Short-Tailed Singing Mouse (Scotinomys Teguina). Horm. Behav. 2010, 58, 334–340. [Google Scholar] [CrossRef]
- Ooi, S.L.; Giovino, M.; Pak, S.C. Transcendental Meditation for Lowering Blood Pressure: An Overview of Systematic Reviews and Meta-Analyses. Complement. Ther. Med. 2017, 34, 26–34. [Google Scholar] [CrossRef]
- Tikhonova, V. The Problems of Typology of Transcendental Meditation Movement (TM). St Tikhons Univ. Rev. 2018, 75, 111–127. [Google Scholar] [CrossRef]
- Hinduism and the 1960s. Available online: http://www.bloomsburycollections.com/collections/monograph (accessed on 26 May 2024).
- Sawyer, D.; Humes, C. The Transcendental Meditation Movement; Elements in New Religious Movements; Cambridge University Press: Cambridge, UK, 2023; ISBN 978-1-00-936549-9. [Google Scholar]
- Marchand, W.R. Mindfulness-Based Stress Reduction, Mindfulness-Based Cognitive Therapy, and Zen Meditation for Depression, Anxiety, Pain, and Psychological Distress. J. Psychiatr. Pract. 2012, 18, 233–252. [Google Scholar] [CrossRef] [PubMed]
- Wiltink, J.; Glaesmer, H.; Canterino, M.; Wölfling, K.; Knebel, A.; Kessler, H.; Brähler, E.; Beutel, M.E. Regulation of Emotions in the Community: Suppression and Reappraisal Strategies and Its Psychometric Properties. Psycho-Soc. Med. 2011, 8, Doc09. [Google Scholar] [CrossRef]
- Greenberg, L.S.; Safran, J.D. Emotion in Psychotherapy: Affect, Cognition, and the Process of Change; Guilford Press: New York, NY, USA, 1987; pp. xiii, 338. ISBN 978-0-89862-010-8. [Google Scholar]
- Heyman, R.E.; Baucom, K.J.W.; Giresi, J.; Isaac, L.J.; Slep, A.M.S. Patient Experience and Expression of Unpleasant Emotions During Health Care Encounters. J. Patient Exp. 2020, 7, 969–972. [Google Scholar] [CrossRef]
- Görlach, M.G.; Kohlmann, S.; Shedden-Mora, M.; Rief, W.; Westermann, S. Expressive Suppression of Emotions and Overeating in Individuals with Overweight and Obesity. Eur. Eat. Disord. Rev. J. Eat. Disord. Assoc. 2016, 24, 377–382. [Google Scholar] [CrossRef] [PubMed]
- Chung, M.C.; Shakra, M.; AlQarni, N.; AlMazrouei, M.; Al Mazrouei, S.; Al Hashimi, S. Posttraumatic Stress Among Syrian Refugees: Trauma Exposure Characteristics, Trauma Centrality, and Emotional Suppression. Psychiatry 2018, 81, 54–70. [Google Scholar] [CrossRef]
- Tyra, A.T.; Fergus, T.A.; Ginty, A.T. Emotion Suppression and Acute Physiological Responses to Stress in Healthy Populations: A Quantitative Review of Experimental and Correlational Investigations. Health Psychol. Rev. 2023, 18, 396–420. [Google Scholar] [CrossRef]
- Joseph, J. Separated Twins and the Genetics of Personality Differences: A Critique. Am. J. Psychol. 2001, 114, 1–30. [Google Scholar] [CrossRef] [PubMed]
- Gura, N. Development of the doctrine of conditioned reflexes in world science: Contribution of c.-к. Teutsch. Habitus 2022, 40, 51–57. [Google Scholar] [CrossRef]
- Teutsch, C.K. Depression: A New Approach. Genetic Factor. Lawyer 1982, 9. [Google Scholar]
- Teutsch, J.M.; Teutsch, C.K. Victimology: An Effect of Consciousness, Interpersonal Dynamics and Human Physics. Int. J. Criminol. Penol. 1974, 2, 249–274. [Google Scholar]
- Novo Navarro, P.; Landin-Romero, R.; Guardiola-Wanden-Berghe, R.; Moreno-Alcázar, A.; Valiente-Gómez, A.; Lupo, W.; García, F.; Fernández, I.; Pérez, V.; Amann, B.L. 25 Years of Eye Movement Desensitization and Reprocessing (EMDR): The EMDR Therapy Protocol, Hypotheses of Its Mechanism of Action and a Systematic Review of Its Efficacy in the Treatment of Post-Traumatic Stress Disorder. Rev. Psiquiatr. Salud Ment. 2018, 11, 101–114. [Google Scholar] [CrossRef] [PubMed]
- Huston, P.; McFarlane, B. Health Benefits of Tai Chi. Can. Fam. Physician 2016, 62, 881–890. [Google Scholar] [PubMed]
- Hofmann, S.G.; Grossman, P.; Hinton, D.E. Loving-Kindness and Compassion Meditation: Potential for Psychological Interventions. Clin. Psychol. Rev. 2011, 31, 1126–1132. [Google Scholar] [CrossRef] [PubMed]
- Hao, J.; Liu, C.; Feng, S.; Luo, J. Imagination-Based Loving-Kindness and Compassion Meditation: A New Meditation Method Developed from Chinese Buddhism. J. Relig. Health 2022, 61, 2753–2769. [Google Scholar] [CrossRef] [PubMed]
- Vinesett, A.L.; Whaley, R.R.; Woods-Giscombe, C.; Dennis, P.; Johnson, M.; Li, Y.; Mounzeo, P.; Baegne, M.; Wilson, K.H. Modified African Ngoma Healing Ceremony for Stress Reduction: A Pilot Study. J. Altern. Complement. Med. 2017, 23, 800–804. [Google Scholar] [CrossRef] [PubMed]
- Arif, S.A.; Moran, K.; Quiñones-Boex, A.; El-Ibiary, S.Y. Student Stress Management and Wellness Programs among Colleges of Pharmacy. Innov. Pharm. 2021, 12. [Google Scholar] [CrossRef] [PubMed]
- Chakr, V.C.B.G. Stress Management in Medicine. Rev. Assoc. Medica Bras. 2021, 67, 349–352. [Google Scholar] [CrossRef]
- Kriener, C.; Schwertfeger, A.; Deimel, D.; Köhler, T. [Psychosocial Stress, Stress Perception and Stress Management of Students of Social Work: A Quantitative Study]. Das Gesundheitswesen 2018, 80, S37–S43. [Google Scholar] [CrossRef]
- Kim, H.; Lee, K.-S. Association of Stress Management with Success of Smoking Cessation in Korean Female Emotional Labor Workers for Service and Sales. Int. J. Environ. Res. Public. Health 2021, 18, 3023. [Google Scholar] [CrossRef] [PubMed]

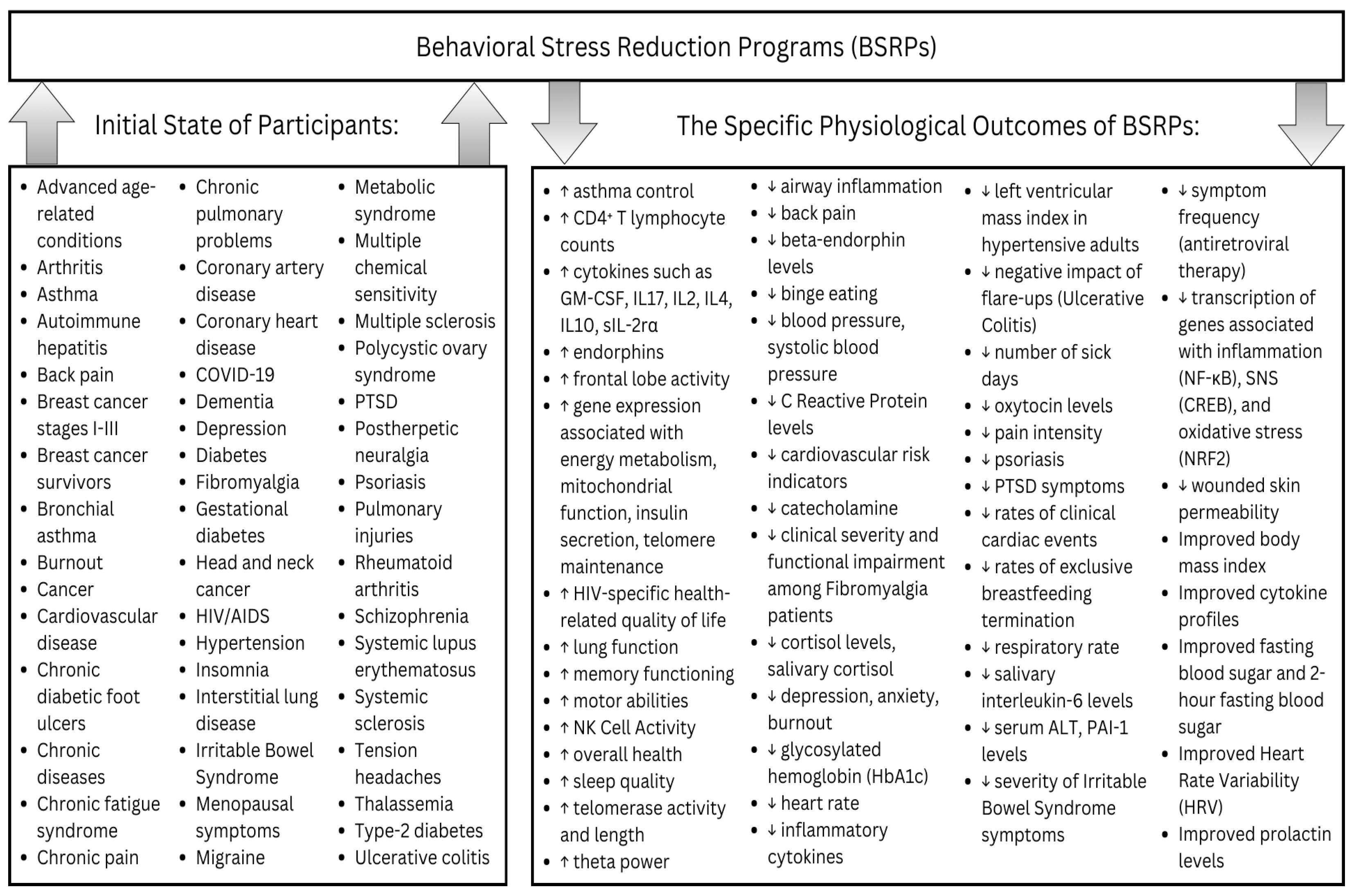
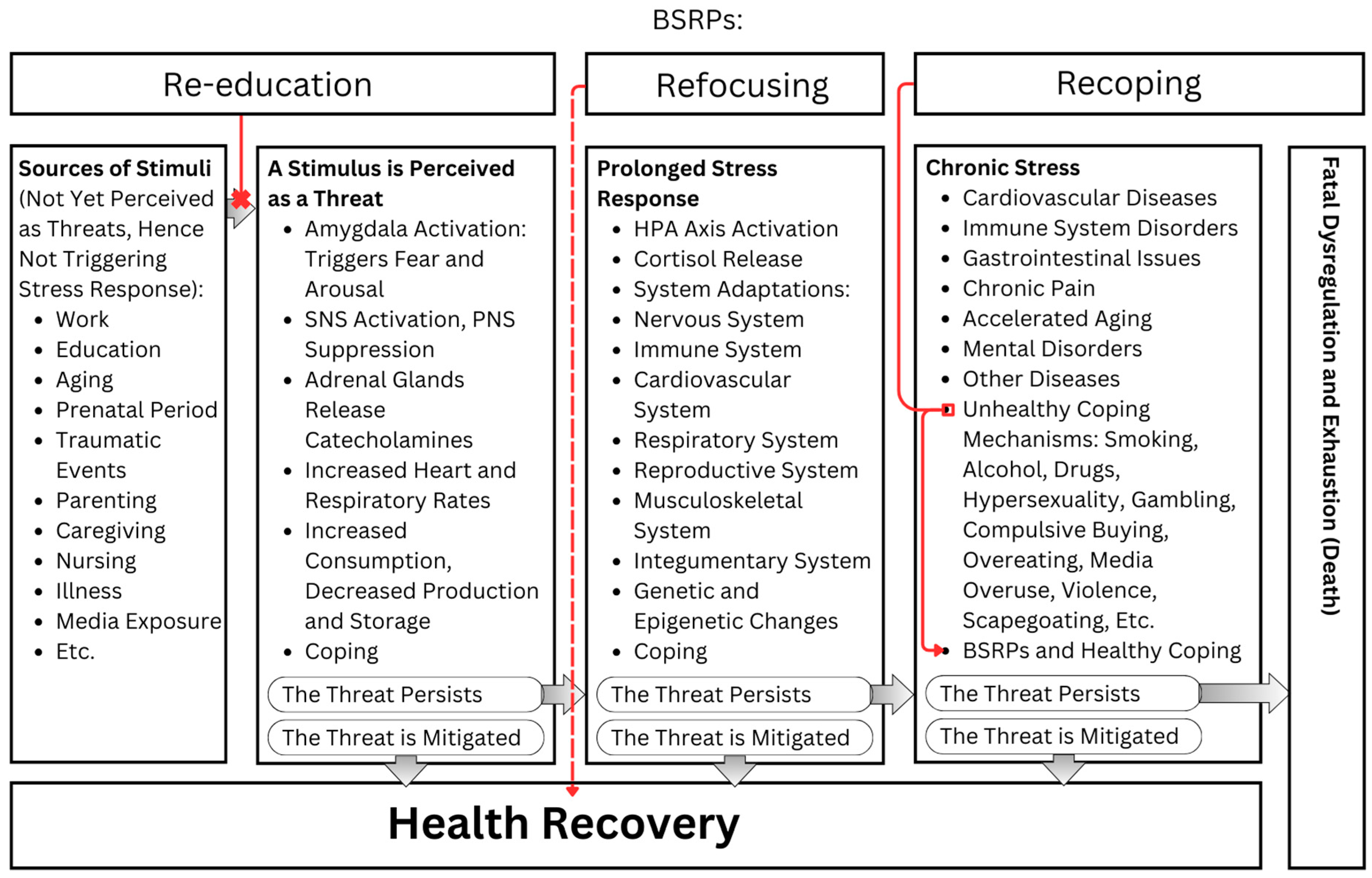
| Gene Name | Associated with | Studies |
|---|---|---|
| 5HTR2C | cardiovascular disease, depression, type-2 diabetes | [12] |
| ABAT | immune system | [13] |
| ACHE | PTSD | [14] |
| ADRB | tumor | [15] |
| AP-1 | restraint stress, inflammation | [16] |
| ARHGEF1 | anxiety | [17] |
| ATG16L1 | immune system | [13] |
| BCR-ABL | leukemogenesis | [18,19,20] |
| BDNF | mental disorders, MSDs | [21,22,23,24] |
| BRCA1 | breast cancer | [25] |
| CALM1 | PTSD | [26] |
| CCNI | anxiety | [17] |
| CD247 | depression | [27] |
| CD28 | ||
| CD3e | ||
| Cited2 | immune system | [13] |
| CLDN2 | restraint stress, metabolism | [28] |
| COMT | neuroticism, depression | [9] |
| Coq10b | immune system | [13] |
| CREB | immune system | [16,29] |
| CRHR1 | anxiety | [22,23,30] |
| CSF3R | anxiety | [17] |
| CTNNB1 | ||
| DPYD | ||
| DAT | anxiety | [22] |
| DBH | ||
| DRD1 | anxiety | [22,31] |
| DRD2 | ||
| DRD3 | ||
| DRD4 | ||
| EIF2 | PTSD | [32] |
| EP300 | PTSD | [26] |
| EPHX2 | depression | [33] |
| FKBP5 | neuroticism, schizophrenia | [3,34] |
| GAD1 | PTSD | [35] |
| GATA1 | depression | [36] |
| GPX1 | leukemogenesis | [20] |
| GSTP1 | ||
| GR/NR3C1 | depression, asthma, early life and perinatal stress | [3,37,38,39] |
| IRF3 | anxiety | [17] |
| NFKB1/NF-kB | immune system | [40] |
| NPS | PTSD, anxiety | [35,41] |
| NPSR1 | ||
| NPY | appetite | [42] |
| NR1H4 | restraint stress | [28] |
| NRCAM | social defeat, abusive supervision | [43] |
| NRF2 | oxidative stress | [16,32] |
| NRG1 | depression | [33] |
| OXTR | ||
| NRXN1 | synaptic strength, depression, PTSD | [44] |
| NRXN2 | ||
| NRXN3 | ||
| PLCB2 | anxiety | [17] |
| POLM | ||
| PPP3CA | ||
| PPM1F | PTSD, depression | [45] |
| PRKCA | PTSD | [26] |
| SASP | restraint stress | [16] |
| SIRT1 | leukemogenesis | [19] |
| SLC6A4/5-HTT/5-HTTLPR | PTSD, neuroticism, anxiety, depression, early life stress, panic disorder | [31,46,47,48,49,50,51] |
| TP53 | anxiety, PTSD | [17,26] |
| TPH2 | mental disorders | [21] |
| USP1 | ER, DNA stress | [52,53,54,55] |
| WDR13 | social isolation, anhedonia, anxiety | [36] |
| State | Participants | The Specific Psychological and Physiological Outcomes of BSRPs | Critique | Study |
|---|---|---|---|---|
| Advanced age-related conditions | 39 elderly, mean age 82 years | Improved acceptance, psychological flexibility, role limitations due to physical health; increased awareness, reduced judgment, greater self-compassion | Small sample size, no long-term follow-up, qualitative data may introduce bias | [151] |
| Advanced age-related conditions | 40 older adults, age 55–85 years | Reduced loneliness, downregulated pro-inflammatory NF-κB gene expression, a trend towards reduced C Reactive Protein | Small sample size, no active control group, short duration of experiment | [77] |
| Advanced age-related conditions | 36 Japanese older adults | Decreased salivary cortisol; correlation between decreased cortisol, negative affect, and cognitive impairment | Small sample size | [152] |
| Asthma | 73 adults | Improved asthma control by 32%, significant reduction in exhaled nitric oxide | Small sample size, no active control group | [153] |
| Asthma | 29 patients | Improvements in quality of life, asthma control, lung function; reduction of rescue medication, stress, enhanced psychosocial and spiritual well-being | Small sample size | [154] |
| Autoimmune hepatitis | 17 adults, mean age 53 years | Perceived stress scores decreased by 28.6%, ALT levels decreased by 37.8%, prednisone doses reduced by 42.5%, significant decrease in IL-6, IL-8, IL-10, IL-17, IL-23 | Small sample size, single-arm, non-randomized, no control group | [155] |
| Burnout | 50 nonmedical hospital staff | Significant reductions in burnout, anxiety, and stress scores immediately after BSRP | Small sample size, no long-term follow-up, no active control group | [108] |
| Burnout | 27 female collegiate rowers | Improved psychological well-being, decreased depression and anxiety, enhanced sleep quality, improved athletic coping skills, reduced ergometer test completion time | Small sample size, quasi-randomized design, no active control group, short follow-up duration, potential non-specific intervention effects | [156] |
| Burnout | 90 post-pandemic era nurses | Positive emotions increased, life satisfaction improved, psychological adaptation significantly higher, negative emotions decreased, low personal accomplishment reduced, job burnout significantly lower | Small sample size, no control group, short intervention duration | [157] |
| Burnout | 13 nursing professionals | Reduction in perceived stress, burnout, depression, and anxiety; significant increase in physical and psychological domains of quality of life | Small sample size, lack of a control group, short duration of the intervention | [158] |
| Burnout | 37 pediatric professionals | Improvement in psychological distress, anxiety, depression, and burnout; effects maintained over 3 months | Change in hair cortisol, small sample size, retreat attendance influenced results | [159] |
| Burnout | 88 adults, mean age 51 | Immediate improvement in perceived stress, burnout, well-being, health status, back pain, and number of sick days; large effect sizes (Cohen’s d for PSQ: 1.09–1.72) | Small sample size, short duration of intervention | [160] |
| Burnout | 53 teachers | Improvements in emotional exhaustion by 15.4% and personal accomplishment by 12.8% | Small sample size | [161] |
| Cancer | 26 patient–caregiver dyads | Reduced cortisol and interleukin-6 levels, decreased stress and anxiety in patients | Small sample size, no control group, short intervention period | [162] |
| Cancer | 71 patients | Significant decrease in perceived stress and post-traumatic avoidance symptoms, increase in positive states of mind and FFMQ scores | Small sample size, no long-term follow-up, no active control condition | [163] |
| Cancer | 120 adult patients | Decreased stress and depression, increased psychological well-being | Short duration, self-reported measures | [164] |
| Cancer | 21 couples | Significant reductions in mood disturbance, muscle tension, neurological/GI symptoms, and upper respiratory symptoms | No control group, small sample size | [165] |
| Cancer | 268 patients, 84% women | 55% reduction in mood disturbance, 29% reduction in stress symptoms, mindfulness increased significantly | No control group, improvements in some mindfulness aspects may need more time | [166] |
| Cancer | 59 patients | Decreased cortisol levels, reduced Th1 cytokines, and lower systolic blood pressure; significant improvements in stress symptoms, quality of life, and mood | Small sample size, lack of a control group | [167] |
| Cancer | 193 participants | Increased cytokines: GM-CSF, IL17, IL2, IL4, sIL-2rα; decreased cortisol, beta-endorphin, and oxytocin levels | No control group, results based on a single 70 min singing session | [168] |
| Cancer | 979 adults | Medium improvements in stress, self-compassion, and social connectedness; participants practicing 5 or more days/week had greater reductions in perceived stress and increases in self-compassion | Differential study retention rates by treatment arm and self-reported engagement introduce selection bias | [169] |
| Cancer/Breast cancer | 336 women | Reduced somatic symptoms and distress post-intervention and at 6 months; increased mindfulness at 6 months; no significant effect at 12 months | No long-term effect on somatic symptoms at 12 months, small sample size, non-active control, varied time since diagnosis | [170] |
| Cancer/Breast cancer | 322 women | Reduced cortisol and IL-6 levels | Short-term study, no long-term data, small effect sizes, no significant group differences over 6 weeks | [171] |
| Cancer/Breast cancer | 322 women | Significant improvement in anxiety, fear of recurrence, fatigue severity, and fatigue interference; largest effect sizes in fear of recurrence problems and fatigue severity | Small to moderate effect sizes, greater benefits observed in participants with higher baseline stress levels | [172] |
| Cancer/Breast cancer | 36 women | Reduced blood pressure, heart rate, respiratory rate, morning cortisol, increased mindfulness state | Small sample size, no control group, short follow-up period | [173] |
| Cancer/Breast cancer | 24 women | Significant improvement in role, cognitive, emotion, social functions, pain, fatigue, body image, future functions, therapy side effects | Small sample size, self-report tools | [174] |
| Cancer/Breast cancer | 225 women undergoing postoperative chemotherapy | Significant improvement in physiological, social, family, emotional, and functional statuses; significant reductions in anxiety and depression | Small sample size, unclear underlying mechanisms, and lack of long-term follow-up | [175] |
| Cancer/Breast cancer | 44 women | Anxiety decreased by 7.68, no significant changes in depression, stress, cortisol, and CRP | Small sample size, limited effect on depression, stress, and inflammatory markers | [176] |
| Cancer/Breast cancer | 192 women newly diagnosed | Decreased stress, fatigue, sleep disturbance; increased NKCA and IFN-gamma, decreased TNF-alpha | Inconsistent practice logging | [177] |
| Cancer/Breast cancer | 18 patients with metastasis | Mild improvements in average pain, general activity, sleep, and enjoyment of life; distress significantly reduced by 27% | Small sample size, some participants dropped out due to disease progression | [178] |
| Cancer/Breast cancer | 82 post-treatment patients | Reduced fear of recurrence, improved physical functioning, and mediated significant reductions in perceived stress and anxiety | Small sample size, short intervention duration | [179] |
| Cancer/Breast cancer | 101 patients (early chemotherapy) | Significant increases in post-traumatic growth, perceived social support, and quality of life | Small sample size, potential biases, and the short duration of the intervention | [180] |
| Cancer/Breast cancer | 142 breast cancer survivors | Increased telomerase activity by 17% over 12 weeks, no significant change in telomere length | No effect on telomere length, small sample size, short study duration | [75] |
| Cancer/Breast cancer | 15 female breast cancer survivors | Improvements in depression, state anxiety, stress, fear of recurrence, sleep quality, fatigue, and quality of life | Single-group pre–post-test design, small sample size, no control group | [181] |
| Cancer/Cervical cancer | 22 cervical cancer survivors | Improved quality of life and modulated stress-associated biomarkers; significant increase in telomere length in CD14(+) cells and a trend in CD14(-) cells; increases in naive T-cell population correlated with telomere length in CD14(-) cells | Small sample size, no control group, short duration | [76] |
| Cancer/Colorectal cancer | 88 patients | Higher disease control rate by 7.67%, improved functional status by 18.53%, lower depression/anxiety scores, better treatment compliance by 18.53%, improved QoL | Small sample size, no long-term follow-up, non-blinded design | [182] |
| Cancer/head/neck | 19 patients, Australia | Reduced psychological distress and improved QoL, reductions in tension–anxiety | Small sample size, no control group, limited generalizability, no significant changes in depression–dejection | [183] |
| Cancer/Lung cancer | 30 patients | Significant improvement in quality of life | Small sample size, short follow-up period | [184] |
| Cancer/Lung cancer | 107 patients and partners | Patients: significant reduction in psychological distress, anxiety, depression, rumination, improved quality of life | Small sample size, high dropout, missing data, no significant effects for partners | [185] |
| Cardiovascular disease | 74 black women | Reduced avoidance coping, slight decrease in TNF-alpha and hsCRP levels | Small sample size, no active control group, low baseline levels of psychological distress | [186] |
| Cardiovascular disease | 60 cardiac patients | Systolic blood pressure decreased by 12%, perceived stress decreased by 45%, anger decreased by 48% | No significant effect on diastolic blood pressure, short intervention duration, no follow-up, self-reported measures | [187] |
| Chronic diseases | 149 patients | Significant reduction in psychological distress (mean IES-R score decreased by 7.75 points), depression, and stress; improvements in psychological health sustained over 8 weeks | Small sample size, no long-term follow-up, no active control group, reliance on self-reported measures, limited gender representation | [188] |
| Chronic diseases | 38 participants (74% white, 79% female, average age 52.6 years) | Improved mental and physical function, reduced pain, self-efficacy; decreased primary care visits by 50%, specialty care by 38%, emergency department visits by 50%, and hospital admissions by 80% at 1 year | Single-cohort design, small sample size, no control group | [189] |
| Chronic diseases | 29 individuals | Statistically significant improvements in physical, psychological health, well-being | Small sample size, no control group | [190] |
| Chronic diseases | 17 participants | 94% found the BSRP positive, reporting increased exercise tolerance, group support, stress reduction, and beneficial spiritual experiences; none found it uncomfortable | Small sample size, no control group, short duration of the experiment, self-reported data may introduce bias | [191] |
| Chronic pain/Arthritis, migraine, and fibromyalgia | 133 patients | Significant improvements in pain intensity, HRQoL, and psychological distress, particularly in patients with arthritis; smallest improvements in patients with chronic headache/migraine and fibromyalgia | Small sample size, no control group, varied compliance with home practice | [10] |
| Chronic pain/Arthritis, lower back pain, fibromyalgia | 26 patients | Pain disability (22.2% improvement), psychological distress (31.1% improvement), and subjective pain rating (24.9% improvement) | Small sample size, no control group, short program length, reliance on self-reported measures, lack of follow-up data | [192] |
| Chronic pain/Back pain | 23 patients | Improved back pain, somatic–affective depression symptoms, and frontal lobe activity | Small sample size | [193] |
| Chronic pain/Back pain/Low back pain | 22 patients | Medium effect on health-related quality of life, psychological functioning, health-related life satisfaction, depression, and affective pain perception; pain severity improved | Small sample size, no control group, no differences in EEG power spectral density | [194] |
| Chronic pain/Chronic neuropathic pain | 23 female breast cancer survivors | Increased posterior cingulate connectivity with medial prefrontal regions, correlated with a reduction in pain severity | Small sample size, no long-term follow-up | [195] |
| Chronic pain/Fibromyalgia | 225 adults with fibromyalgia | BSRP superior to TAU post-treatment and at 12-month follow-up, superior to FibroQoL post-treatment, modestly better long-term in pain catastrophizing and fibromyalgianess | Small sample size, need for larger long-term studies, potential biases due to self-report measures | [196] |
| Chronic pain/Fibromyalgia | 70 females with fibromyalgia | Reduced clinical severity, prevented IL-10 decrease, higher IL-6/IL-10 and CXCL8/IL-10 ratios associated with less improvement in psychological inflexibility | Small sample size | [197] |
| Chronic pain/Migraine | 62 individuals, mean age 44 years | 27% reduction in migraine days, significant improvements in psychological symptoms, pain self-efficacy, and sensory pain perception | Small sample size | [198] |
| Chronic pain/Multiple chemical sensitivity, chronic fatigue syndrome, fibromyalgia | 76 women | Significant improvement in psychological distress, 5 of 9 SCL-90R subscales showed significant improvement, and 8 of 9 subscales showed significant improvement at 3-month follow-up | Control group scores unchanged, small sample size, larger sample and longer follow-up needed | [199] |
| Chronic pain/Postherpetic neuralgia | 50 patients | Significant reduction in depression, anxiety, and pain scores | Small sample size, short intervention duration | [200] |
| Coronary artery disease | 70 PCI patients | Decreased anxiety and depression, reduced perceived stress, increased mindfulness | Small sample size, short intervention, potential bias in telephone format | [201] |
| Coronary artery disease | 24 patients with depression | Depressive symptoms decreased by 33%, mastery scores increased by 8.7%, improvements sustained over 12 months | Small sample size, high dropout rate, no control group, limited generalizability | [202] |
| Coronary artery disease | 101 patients (59.4 ± 8.6 years) | Improved physical function and sum score, reduction in depression, anxiety, anger, and stress | No improvement in psychological outcomes for men, small sample size | [203] |
| Coronary artery disease | 24 male patients | Significant improvement in psychosocial well-being; no change in basal cortisol levels or diurnal rhythm of cortisol; no correlation between stress score and cortisol levels | Small sample size, no control group; raises questions about the utility of salivary cortisol as a stress marker | [204] |
| Coronary heart disease | 151 outpatients | Stress levels decreased significantly, anxiety decreased, distress decreased, perceived stress decreased, clinical events decreased | No significant difference in diastolic blood pressure, small sample size | [205] |
| Coronary heart disease | 30 male patients | Significant reduction in anxiety, depression, perceived stress, systolic BP, BMI; therapeutic gains maintained at 3-month follow-up | Small sample size, only male participants, changes in medication not controlled | [206] |
| Coronary heart disease | 56 African American patients | Myocardial flow reserve (MFR) increased by 14%, reductions in total cholesterol, LDL, triglycerides, smoking, depression, stress (GHQ) | Small sample size, limited follow-up period | [207] |
| COVID-19 | 58 asymptomatic/mild patients | Anxiety and depression scores decreased, severe anxiety and depression reduced to 0%, light anxiety and depression increased | Small sample size, no long-term effect measurement, limited technical assessment | [208] |
| COVID-19 | 84 pregnant women | Significant reductions in prenatal distress, anxiety, and childbirth fear scores | Small sample size, short-term follow-up | [209] |
| COVID-19 | 60 patients | Mental well-being scores increased by 42% in the intervention group; control group scores decreased by 6% | Small sample size, urban-only setting, short follow-up, self-reported data | [210] |
| Crohn’s disease | 116 adults | Decreased disease activity, increased quality of life by 22%, reduced psychological symptoms by 28%, reduced fatigue by 27% | Small sample size, short duration, only mild–moderate cases | [211] |
| Crohn’s disease | 37 patients, 18–75 years | Improved erythrocyte sedimentation rate, T-cell profiling, fecal lactoferrin, calprotectin, quality of life, emotional distress, and core self-evaluation | Small sample size | [212] |
| Dementia | 12 family caregivers of persons with dementia | Reduced behavioral and psychological symptoms of dementia in care recipients; decreased caregiver stress, improved sleep quality | Small sample size, no control group, short intervention period | [213] |
| Dementia | 13 middle-aged and older adults | Decreased worry and increased serenity, improved quality of life, reduced psychological distress, enhanced mindfulness and self-compassion | Small sample size, lack of control group, short follow-up period, potential bias in self-reported measures | [214] |
| Dementia | 825 patients (11 trials) | Significant reduction in behavioral and psychological symptoms of dementia, particularly depression | No significant improvement in cognitive function, activities of daily living, agitation, or quality of life | [215] |
| Dementia/Frontotemporal dementia | 13 individuals | Decline in anxiety (54% post-intervention, 62% at 2 months) and depression (23% at 2 months); improved coping, psychological distress, quality of life, and mindfulness skills | Small sample size, pilot study | [216] |
| Depression | 92 students | Increased mindfulness, decreased depression, anxiety, stress, perceived stress, and anxiety sensitivity, and improved quality of life in physical health, psychological, and environmental domains | No significant improvements in social relationships, quality of life, worry, and experiential avoidance, small sample size, and potential self-selection bias among participants | [217] |
| Depression | 78 premedical and medical students | Reduced self-reported state and trait anxiety, overall psychological distress, and depression, increased empathy | Small sample size, no long-term follow-up, potential bias, no active control group | [218] |
| Depression | 60 elderly | Significant reduction in depression and increase in mindfulness | Small sample size, non-random sampling, limited geographic scope | [219] |
| Depression | 60 elderly | Significant reduction in depression symptoms, improved emotion regulation and sleep quality | Small sample size; short study duration; no long-term follow-up; potential self-reporting bias | [220] |
| Depression | 50 adults | Improvement in perceived stress, depression, psychological well-being, neuroticism, binge eating, energy, pain, and mindfulness | Small sample size, no control group | [93] |
| Depression | Various sample sizes across 23 studies | Significant improvements in depression, dementia, agitation, PTSD symptoms, and motor functions in multiple sclerosis and stroke | Overall low quality of studies, inconsistent methodologies | [221] |
| Depression | 103 older adults | Clinical improvement, especially in younger, female participants with lower psychological symptom severity and those less likely to be diagnosed with depression or taking selective serotonin reuptake inhibitors | Small sample size | [222] |
| Depression | 32 Japanese females | Improved mood states, increased salivary s-IgA levels in the depressed group; emotional inhibition had harmful effects on subjective health in the depressed group | Small sample size, short follow-up period, lack of control group | [223] |
| Depression | 97 adults | Improvements in depression, overall psychological functioning, quality of life, anxiety, anger, and subjective happiness | Small sample size, no control group, short intervention duration | [224] |
| Depression | 34 first-year nursing and midwifery students | Improvements in depression, anxiety, and stress scores; increased salivary immunoglobulin-A secretion; decreased salivary cortisol concentrations | Small sample size, no long-term follow-up | [225] |
| Diabetes/Chronic diabetic foot ulcers | 8 patients, 6 family caregivers | Improved DFU healing and emotional well-being | Small sample size, qualitative study | [226] |
| Diabetes/Gestational diabetes | 78 women | Significant reduction in fasting blood sugar, 2 h blood sugar levels, significant reduction in perceived stress | Study design was quasi-experimental | [227] |
| Diabetes/Type-2 diabetes | 19 adults | Significant reduction in depression, lower HbA1c | Small sample size; of 15 participants, only 46.7% attended all sessions | [228] |
| Diabetes/Type-2 diabetes | 14 adults | Decreased HA1c, arterial pressure, anxiety, depression, and general psychological distress | Small sample size, no change in body weight | [229] |
| Diabetes/Type-2 diabetes | 56 adults | Significant reductions in serum cortisol and plasminogen activator inhibitor-1 (PAI-1) levels | Small sample size, no statistically significant differences in stress, glycemic control, vascular inflammation | [230] |
| Diabetes/Type-2 diabetes | 48 patients | Significant improvements in fasting blood sugar and HbA1c levels | Small sample size, no long-term follow-up | [231] |
| HIV/AIDS | 177 adults with HIV-1 | Depression decreased by 20.9%, positive affect increased by 1.4%, perceived stress decreased by 7.1%, mindfulness increased by 6.3%, no significant changes in CD4+ T-cell counts, HIV-1 viral load, IL-6, CRP, or D-dimer | Psychological benefits did not sustain long-term, no significant immunological outcomes, high control group interaction | [232] |
| HIV/AIDS | 34 adults, primarily gay | NK cell activity increased by 110%, NK cell number increased by 116%, no significant changes in psychological, endocrine, or functional health variables | Nonrandomized design, small sample size, high attrition rate, self-selected participants | [233] |
| HIV/AIDS | 173 HIV+ patients, mean age 35.1 years | CD4 count increased up to 9 months, SCL-90R scores improved up to 6 months, MSCL scores improved up to 12 months | Randomization failure for CD4 count, small sample size, non-blinded assessments, self-reporting bias | [234] |
| HIV/AIDS | 180 individuals aged 55+ | Improvement in depression at 8 weeks (not sustained at 16 weeks), improved quality of life (QOL) at 16 weeks, no change in cognitive performance | Short-term benefits in depression and QOL, no long-term sustainment, no cognitive improvement | [235] |
| HIV/AIDS | 22 individuals | Improved vitality, general health, physical well-being, HRQoL; reduced stress and depression; slightly lower cortisol and norepinephrine levels | No significant immune activation differences, small sample size, short follow-up | [236] |
| HIV/AIDS | 6 HIV-positive individuals | CD4 count increased significantly and remained up to 12 months; improved SCL-90-R, but not sustained at follow-ups; no significant changes in physical status (MSCL) | Small sample size, lack of sustained psychological improvement | [237] |
| HIV/AIDS | 76 individuals on ART | ART-related symptoms reduced by 39.1% at 3 months and 46.2% at 6 months, symptom-related distress decreased significantly | Small sample size, no significant effects on overall adherence or psychological functioning | [238] |
| Hypertension | 38 hypertensive employees | Systolic BP reduced by 10.6 mm Hg, diastolic BP reduced by 6.3 mm Hg, decreased stress, depression, psychological distress, increased peacefulness, positive outlook, workplace satisfaction, and value of contribution | Small sample size, no long-term follow-up, no active control group, potential self-selection bias | [239] |
| Hypertension | 872 patients (12 trials) | SBP decreased by 6.64 mmHg, DBP by 2.47 mmHg, DBP reduction sustained up to 3–6 months, no significant out-of-office BP reduction, reduced depression, anxiety, stress | Limited high-quality trials, few out-of-office BP reports, small sample sizes, lack of long-term data, inconsistent randomization | [240] |
| Hypertension | 85 African Americans (52.8 years) | Significantly lower LVMI, significant reductions in BP and in anger | Small sample size, high attrition rate, no record of compliance for home TM practice | [241] |
| Hypertension | 45 subjects | Systolic/diastolic blood pressure and perceived stress significantly reduced; adherence to the Mediterranean diet increased | Small sample size, no long-term follow-up | [242] |
| Injuries/Pulmonary | 40 male veterans | Improved mental health and health-related quality of life, increased lymphocyte proliferation (PHA) and IL-17 levels | Small sample size, no active control group | [243] |
| Injuries/Pulmonary | 40 male veterans | Improved SF-36 total score, role limitations due to physical problems, role limitations due to emotional problems, social functioning, mental health, vitality, and pain; no significant change in FEV1, FVC, or FEV1/FVC | Small sample size, no active control group | [244] |
| Injuries/Sport | 20 university athletes | Increased pain tolerance, improved mindful awareness, notable decrease in stress/anxiety scores | Small sample size, no active control group, diverse types of injuries | [245] |
| Injuries/Wound | 49 healthy adults | Greater mindfulness increase correlated with reduced skin permeability (days 3–4); lower IL-8 and placental growth factor levels at 22 h | Small sample size, no significant overall effect | [246] |
| Insomnia | 111 cancer patients with insomnia | Reduced sleep onset latency, wake after sleep onset, stress and mood disturbances; increased total sleep time; improved sleep quality and dysfunctional sleep beliefs | Small sample size, no control group, need for longer follow-up | [247] |
| Interstitial lung disease | 19 elderly patients | Improved mood and reduced stress (POMS, PSS scores); no significant changes in respiratory symptoms, lung function, or exercise tolerance | Small sample size, no control group, and unmonitored adherence to home exercises | [248] |
| Irritable Bowel Syndrome | 24 patients | Improved quality of life and reduced IBS severity | Small sample size | [249] |
| Irritable Bowel Syndrome | 101 patients | 22.4% decrease in perceived stress, improved mental health, resilience, and quality of life, no significant impact on IBD symptoms or inflammatory biomarkers | Small sample size, no control for IBD severity indices | [250] |
| Menopausal symptoms | 66 women, aged 47–62 | Significant improvements in menopause-specific quality of life, including physical, psychosocial, and sexual dimensions | Small sample size and short follow-up duration | [251] |
| Menopausal symptoms | 118 women | Significant improvement in menopausal symptoms, quality of life across vasomotor, psychosocial, sexual, and physical domains | Quasi-experimental design, no randomized control group | [252] |
| Menopausal symptoms | 197 women | Reduced total menopausal symptoms at 8 months, greater reduction in anxiety and depression | Both groups improved, BSRP had more psychological benefits | [253] |
| Metabolic syndrome | 22 individuals (11 couples) | Wives showed greater increases in physical functioning and relationship satisfaction; no significant intervention effects for husbands. | Small sample size, unequal prevalence of metabolic syndrome in couples | [254] |
| Multiple sclerosis | 48 female patients, Iran | Significant improvement in all subscales of quality of life (QOL) post-intervention and sustained at follow-up | Small sample size, single-gender study, limited to patients with low MS severity | [255] |
| Multiple sclerosis | 25 patients, Netherlands | Decreased depressive symptoms by 29%, increased physical QOL by 36%, increased mental QOL by 43%, reduced fatigue by 11%, enhanced visuospatial memory processing | Small sample size, high dropout rate, no control group, reliance on self-reported measures | [256] |
| Multiple sclerosis | 48 women, Iran | Depression reduced by 46.1%, anxiety reduced by 47.2%, stress reduced by 46.6% | Small sample size, short follow-up period | [257] |
| Polycystic ovary syndrome | 60 women | Significant reduction in mental complications, interpersonal problems, non-pregnancy physical complications, pregnancy complications, sexual complications, and religious issues | Small sample size, short follow-up, high proportion of educated participants | [258] |
| Psoriasis | 446 participants (10 studies) | Significant improvements in physical severity (3 studies), psychological outcomes (3 studies), and quality of life (1 study); mixed results across other studies with non-significant findings | Overall low quality of evidence, heterogeneity in study design, lack of validated outcome measures in some studies, and publication bias suspected | [259] |
| PTSD | 50 women | Decreased stress, depression, anxiety, emotion dysregulation, PTSD symptoms, increased mindfulness, lower IL-6 levels | Small sample size, no control group, short follow-up, potential selection bias | [116] |
| PTSD | 220 individuals (war trauma) | PTSD symptoms decreased (PCL-5 scores reduced from M = 38.58 to M = 20.59), SUDS scores significantly lowered | Small sample size, no long-term follow-up, lack of quantitative measures for all segments | [260] |
| PTSD | 30 children, adolescents | PTSD symptoms decreased by 60%, anxiety decreased by 30.5% | Small sample size, no control group, short follow-up period | [261] |
| PTSD | 184 veterans | PTSD symptom reduction, depression reduction; those attending ≥6 sessions saw a 39.3% improvement in depression scores | Small sample size, high noncompletion rates | [262] |
| Rheumatoid arthritis | 63 patients | At 6 months, significant improvement in psychological distress (35% reduction) and well-being, marginal improvement in depression and mindfulness | No significant changes at 2 months, small sample size, short follow-up period, no impact on RA disease activity | [263] |
| Schizophrenia | 40 middle-aged and older patients | Improved Positive and Negative Syndrome Scale (PANSS) scores and reduced stress (DASS-stress subscale), no significant change in happiness (CHI) | Small effect size, no significant difference in happiness, limited evidence for broader applicability | [264] |
| Schizophrenia | 137 patients | Significant increases in hope, psychological well-being, and functional recovery | Small sample size, no long-term follow-up | [265] |
| Schizophrenia | 26 individuals | Significant decrease in perceived stress and negative affect, significant improvement in heart rate variability | No significant change in positive affect or subjective well-being, small sample size | [266] |
| Somatic Symptom Disorder | 37 patients, mean age 37 years | Significant reductions in depression, anxiety, stress, and their severities; decreased number and severity of physical symptoms and overall SSD severity | Effective as complementary medicine, small sample size, no control group | [70] |
| Stuttering | 56 adults who stutter | Improvements in stuttering, awareness, reactions, daily communication, quality of life, reduced anxiety, and increased life satisfaction | Small sample size, short follow-up | [267] |
| Stress | 26 healthy individuals | Significant reduction in perceived stress; correlated with decreased gray matter density in the right basolateral amygdala | Small sample size, no control group, limited generalizability, short intervention duration | [5] |
| Stress | 127 community residents | Decreased perceived stress, increased mindfulness and self-compassion | No control group, potential demographic bias | [8] |
| Stress | 26 healthy practitioners and novices | Enhanced expression of genes related to energy metabolism, insulin secretion, and telomere maintenance; reduced expression of genes linked to inflammation and stress-related pathways | Small sample size, no control group, short-term study duration, need for further validation of molecular mechanisms | [60] |
| Stress | 58 participants | Increased positivity bias in response to emotionally ambiguous signals | No control group, small sample size, short-term effects not observed, reminder issues for completing tasks promptly | [149] |
| Stress | 84 participants | Increased likelihood of choosing reappraisal over distraction, improved sensitivity to interoceptive signals, enhanced well-being | Small sample size, lack of active control group, short duration of experiment | [268] |
| Stress | 90 participants aged 26–55 | Improved psychological well-being, hardiness, coping strategies, interpersonal interactions, and professional self-realization in adult women | Small sample size, no control group, reliance on self-reported data, potential bias in interpreting long-term parental influence | [269] |
| Stress | 32 healthy women | Increased functional connectivity within auditory and visual networks; improved attentional focus; enhanced sensory processing and reflective awareness of sensory experience | Small sample size, no control group, short duration of the experiment | [270] |
| Stress | 15 professional singers | Decrease in cortisol and cortisone | Increase across the high-stress condition, small sample size | [271] |
| Stress | 77 motorcyclists, 42 +/− 14 years | Decreased N1 amplitude, relative alpha power, cortisol; increased mismatch negativity, epinephrine, heart rate, DHEA-S | Small sample size, no control group | [272] |
| Stress | 83 individuals | Daily increases in mindfulness predicted subsequent decreases in negative affect and increases in positive affect | Magnitude of effects varied substantially between individuals, small sample size | [273] |
| Stress | 87 adults | 92% of participants strongly agreed the training was beneficial, 8% agreed | Small sample size, no control group, qualitative study | [274] |
| Stress | 21 young adults (beginners) | Reductions in saliva cortisol, perceived mental stress at follow-up; improvements in general health perception, social functioning, vitality, and mental health/psychological well-being | Small sample size, high dropout rate, no control group | [275] |
| Stress | 1 Buddhist monk | Significant increase in theta power, decrease in heart rate | Case study with a single participant limits generalizability | [276] |
| Stress/Care | 29 healthcare professionals | 35% reduction in distress, 30% reduction in rumination, 20% decrease in negative affect, benefits sustained over 3 months | Small sample size, no control group, short follow-up period | [277] |
| Stress/Care | Stress (61 parents of children with Autism) | Improvements in parental distress and parent–child dysfunctional interactions | Small sample size, no significant difference in depressive symptoms, anxiety, or life satisfaction | [278] |
| Stress/Care | Stress (47 parents of toddlers with developmental delays) | Decreased self-reported parenting stress and cortisol awakening response, greatest changes observed between baseline and follow-up | Small sample size, no control group | [279] |
| Stress/Care | Stress (100 psychiatric nurses) | Significant decreases in SCL-90, depression, anxiety, and Nursing Stress Scale scores | Short duration of study, no long-term follow-up, small sample size | [126] |
| Stress/Care | Stress (67 nurses in Iran) | Significant increases in mortality awareness and decreases in interpersonal problems | Quasi-experimental design, small sample size, short follow-up duration | [127] |
| Stress/Care | 72 caregivers (COVID-19) | Anxiety decreased by 20.7%, mental component summary increased by 22.9%, physical component summary increased by 18.2% | Small sample size, no long-term follow-up | [280] |
| Stress/Care | 64 family caregivers | Stress reduced by 8.3%, sleep quality improved by 9%, mindful awareness increased by 5.0%, no significant change in caregiver burden | Small sample size, short follow-up period, primarily self-reported outcomes | [281] |
| Stress/Care | 155 patients and caregivers | Reduced caregiver distress | No significant difference in patient QoL | [282] |
| Stress/Care | 148 caregivers | Reduced mental health service use | No significant differences in medical service or support group use | [283] |
| Stress/Care | 57 family caregivers | Significant improvements in perceived stress, depressive symptoms, and subjective caregiver burden | Small sample size, no control group | [284] |
| Stress/Childbirth | 68 pregnant women | Significantly lower perceived stress during labor and pain intensity | No significant difference in fear of childbirth, active phase of labor, second stage of delivery, total length of delivery, Apgar score, or oxytocin consumption | [285] |
| Stress/Childbirth | 46 pregnant women | Significant increase in breastfeeding self-efficacy at 1 and 4 months postpartum, higher continuation of exclusive breastfeeding | Small sample size | [286] |
| Stress/Childbirth | 64 breastfeeding mothers | Decreased anxiety, postpartum distress; increased breastfeeding self-efficacy | Small sample size | [287] |
| Stress/Education | 48 students | Significant reductions in perceived stress, anger, confusion, sadness, and salivary cortisol levels. | Small sample size, no control group, potential self-reporting bias, and short duration of the intervention. | [288] |
| Stress/Education | 119 students | Increased mindfulness, increased self-compassion | No significant reductions in trait anxiety, the quasi-experimental design and the short duration | [289] |
| Stress/Education | 58 students and teachers | Students: reduced stress, improved self-regulation, self-efficacy, and reduced interpersonal problems; teachers: increased mindfulness, reduced interpersonal problems | Small sample size, no active control, short-term follow-up | [290] |
| Stress/Education | 90 students | Significant improvements in mindfulness, psychological distress, perceived stress, and life satisfaction scores | Small sample size, no control group, short intervention duration, self-reported measures. | [291] |
| Stress/Education | 302 medical students | Decreased Total Mood Disturbance by 17.8%, significant improvements in tension–anxiety, confusion–bewilderment, fatigue–inertia, and vigor–activity subscales | Initial baseline differences between groups | [292] |
| Stress/Education | 72 nursing students | Significantly reduced stress biomarkers | Did not achieve statistically significant reductions in self-reported psychological stress during examinations | [293] |
| Stress/Education | 49 college students | A 33% reduction in perceived stress and nearly 40% reduction in depression, anxiety, stress; increased alpha band power in frontal and occipital lobes observed in EEG, particularly during stress-inducing tasks | Small sample size, short intervention period | [294] |
| Stress/Media | Stress (26 middle-aged women) | Increased self-acceptance, purpose in life, relations with others, mindfulness, psychological flexibility, and well-being | Small sample size, no control group, self-selection bias, online delivery limitations | [295] |
| Stress/Media | 131 participants | Decreased perceived stress, increased positive affect; individuals with lower baseline mindfulness exhibited greater overall improvement | Small sample size, no control group, short duration of the experiment, potential bias | [296] |
| Stress/Medical interventions | 104 patients undergoing GI endoscopy | Reduced blood pressure, heart rate, and respiratory rate; improved perception of the procedure | Small sample size, no control group for comparison, short duration of the intervention | [297] |
| Stress/Medical interventions | 30 patients undergoing cerebral angiography | Stable cortisol levels, reduced systolic blood pressure, decreased stress in patients with high fear levels | Small sample size, no control group, short duration of the intervention | [298] |
| Stress/Medical interventions | 209 women undergoing TUGOR | Lower vaginal pain, higher satisfaction with pain control | No significant differences in psychological scores or stress biomarkers | [299] |
| Stress/Medical interventions | 80 adults (dental procedures) | Significantly reduced discomfort | Small sample size, no control group, short duration | [300] |
| Stress/Medical interventions | 100 women with breast cancer (surgical procedures) | Increased autonomy (+17.6%), environmental control (+11.8%), personal growth (+11.2%), positive relationships (+9.4%), goals in life (+12.6%), self-acceptance (+21.6%); improved sleep quality (37.0%); favorable views on oophorectomy (+14%) and mastectomy (+17%). | Small sample size | [301] |
| Stress/Military | 49 Chinese military recruits | Improved general health, and reduced perceived stress at 12-week follow-up. | Small sample size and short follow-up duration. | [302] |
| Stress/Military | 39 ROK Navy crew | Decreased perceived stress by 15%, anxiety by 41%; improved psychological well-being by 23%; no change in depression | Small sample size, non-equivalent control group, limited generalizability | [303] |
| Stress/Military | 30 veterans | Reduction in perceived stress and depression; improved sleep quality; high satisfaction and compliance | Single-group design, no control group, small sample size | [304] |
| Stress/Trauma | 63 vulnerable women | Perceived stress decreased by 20.9% | Small sample size, quasi-experimental design, short follow-up period | [305] |
| Stress/Trauma | 24 LGB individuals | Perceived stress decreased by 23% in women and 40% in men, minority stress decreased by 12% in women | Small sample size, lack of control group, pilot study design, short follow-up period | [306] |
| Stress/Trauma | 24 victims of gun violence | Improvements in trauma, depression, sleep quality, and life satisfaction | Uncontrolled, non-randomized trial, small sample size | [307] |
| Stress/Trauma | 112 women with early life abuse | Increased temporal summation of heat pain intensity, reduced cortisol AUC, improved depression and emotion regulation abilities | Small sample size, no long-term follow-up, reliance on self-reported measures | [113] |
| Stress/Work | 42 healthy working adults | Decreased perceived stress, increased mindfulness, improved sleep quality | Small sample size, use of a wait-list control group | [308] |
| Stress/Work | 122 prison guards | Significant reduction in stress reactions, improved coping strategies, and better communication skills; in Kula prison, significant positive changes in attitudes toward detainees | Small sample size, variable significance across different prisons, no long-term follow-up, lack of control group, and potential bias in self-reported measures | [309] |
| Stress/Work | 247 university employees | Increased job satisfaction, affective organizational commitment, perceived procedural justice, and trust in senior management; no significant change in psychological strain | Small sample size, low awareness of interventions, cross-sectional data, lack of long-term follow-up, potential response bias | [310] |
| Stress/Work | 144 managers | Decreased perceived work-related stress (by 0.72), negative affect (by 0.93), somatic complaints intensity (by 0.69), sickness absence (by 0.69); increased self-esteem (by 1.25) and positive affect (by 0.43) | No effect on the frequency of somatic complaints, need for longer follow-up and consideration of individual differences in stress responses | [311] |
| Stress/Work | 75 nurses and midwives | Increased sexual satisfaction | No significant effect on occupational stress and marital satisfaction, small sample size | [225] |
| Stress/Work | 126 individuals | Improvements in perceived stress, work engagement, overall quality of life, physical health, psychological health, social relationships, and environmental | Depression and anxiety improved but did not survive Bonferroni correction; small sample size | [312] |
| Stroke, Dementia, Multiple Sclerosis, Spinal Cord Injury | 906 participants (17 trials) | Stroke: improved gait, balance, perception of recovery, and quality of life. Dementia: reduction in stress, anxiety, sadness, depression, improved balance and cognitive function. Multiple Sclerosis: reduced spasticity, fatigue, improved balance, general health perception, and quality of life. Spinal Cord Injury: reduced effort in upper limbs, improved spasticity and mental well-being | Stroke: variability in intervention protocols. Dementia: some studies showed stable depressive symptoms and agitation. Multiple Sclerosis: mixed results in depression and constipation. Spinal Cord Injury: short-term improvements only, small sample sizes | [313] |
| Systemic lupus erythematosus | 26 SLE patients | Improved quality of life, reduced psychological inflexibility in pain and SLE-related shame, reduced SLE symptoms, decreased depression | Small sample size, further research needed for long-term effects | [314] |
| Systemic lupus erythematosus | 92 SLE patients | Reductions in pain, psychological dysfunction; improved perceived physical function and psychological function at 9-month follow-up | Small sample size, limited long-term maintenance of benefits | [315] |
| Systemic sclerosis | 32 patients | Significant improvement in anger control and significant improvement in anger control and expression; no significant changes in physical functionality, anxiety, depression | Small sample size, non-random assignment, short duration, lack of significant quantitative improvements in most variables | [316] |
| Tension headaches | 60 patients | GSI decreased by 55.2% post-intervention and 43.2% at follow-up, perceived stress decreased by 25.1% post-intervention and 20.4% at follow-up | Small sample size, limited follow-up duration | [317] |
| Thalassemia | 66 patients | Rejection sensitivity decreased by 18.7%, resilience increased by 6.5% | Small sample size, short duration of experiment | [318] |
| Ulcerative colitis | 47 patients | Reduced psychosocial stress, decreased physical symptoms, and improved quality of life; enhanced disease acceptance, stress management, self-confidence, and social participation | Small sample size, no control group, short experiment duration, potential self-reporting bias, and limited long-term data | [319] |
| Ulcerative colitis | 55 adults | Reduced stress in flaring patients, prevented QOL drop during flares | Did not affect flare-up rate/severity, small sample size, short duration | [320] |
| Ulcerative colitis | 60 patients | At 3 months: improvement in SF-36 physical function, reduction in BSI anxiety | No significant long-term effects at 12 months, small sample size | [321] |
| Unhealthy coping/Hypersexuality | 88 bisexual men, with childhood sexual abuse | Unprotected anal insertive sex episodes reduced by 74%, depressive symptoms reduced by 43%, PTSD symptoms reduced by 56% | Small sample size, potential for bias due to self-reported measures | [85] |
| Unhealthy coping/Smoking | 76 adult ex-smokers | Reductions in perceived stress and higher rates of smoking abstinence, reduced relapse rates | Small sample size, lack of long-term follow-up, potential self-reporting bias | [82] |
| Unhealthy coping/Smoking | 474 individuals (4 trials) | 25.2% of BSRP participants remained abstinent for more than 4 months compared to 13.6% in the usual care therapy group | Limited number of trials, need for longer follow-up periods | [322] |
| BSRP Name | Short Description | BSRP Category |
|---|---|---|
| PsychoEducation, Paced Respiration, and Relaxation (PEPRR) | Integrates psychological training, regulated breathing techniques, and relaxation exercises to alleviate distress and its related health issues | Recoping, Refocusing, Re-education |
| Animal-Assisted Therapy | Utilizes interactions with specially trained animals, mainly dogs, to improve emotional well-being and reduce symptoms of stress and depression | Refocusing |
| Music Therapy | Employs structured music-based interventions delivered by certified professionals to achieve individualized therapeutic goals | Refocusing |
| Singing | Uses vocal expression as a means to manage emotional stress and promote psychological well-being | Recoping, Refocusing |
| Distraction | Shifts focus away from stressors to engaging activities such as games, creative pursuits, or physical exercise to mitigate stress responses | Refocusing |
| Transcendental Meditation (TM) | A mantra-based meditation technique rooted in religious-neutral Hindu traditions, involving initial guidance and independent practice for mental tranquility | Refocusing |
| Mindfulness-Based Stress Reduction (MBSR) | Combines mindfulness meditation, body scanning, and yoga, derived from religious-neutral Buddhist practices, to enhance present-moment awareness and reduce stress | Recoping, Refocusing, Re-education |
| Mindfulness-Based Cognitive Therapy (MBCT) | Blends mindfulness practices with cognitive–behavioral therapy elements, based on religious-neutral Buddhist principles, to prevent depressive relapse and manage stress | Recoping, Refocusing, Re-education |
| The Teutsch IDEAL Method | Encompasses behavioral psychogenetics, principles of human physics, and scientific interpretations of religious-neutral spiritual and moral teachings from the Bible | Recoping, Refocusing, Re-education |
| Eye Movement Desensitization and Reprocessing (EMDR) | Integrates elements of various psychological approaches, focusing on reprocessing traumatic memories and altering self-perceptions | Refocusing |
| Tai Chi | Involves gentle, mindful movements promoting structural alignment, flexibility, strength, and natural breathing, rooted in ancient Chinese martial arts | Refocusing |
| Loving-Kindness and Compassion Meditation | Focuses on cultivating unconditional kindness and empathy through the repetition of positive affirmations and compassionate thoughts, grounded in religious-neutral Buddhist traditions | Refocusing |
| Inquiry-Based Stress Reduction (IBSR, The Work) | Systematically challenges stressful thoughts by exploring them through a structured series of questions and cognitive reframing | Refocusing, Re-education |
| Comprehensive Lifestyle Modification Programs (CLMPs) | Incorporates yoga, stress management techniques, mindfulness, herbal remedies, communication skills, self-awareness, and culinary education to promote holistic well-being | Refocusing |
| Ngoma | Combines meditation, yoga, or prayer with rhythmic dance to traditional Congolese music, rooted in religious-neutral Central and South African cultural practices | Refocusing |
| Stress Management Education | Offers a wide array of strategies, including counseling, academic support, physical activity guidance, and relationship enhancement activities, to manage and reduce stress | Recoping, Refocusing |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shchaslyvyi, A.Y.; Antonenko, S.V.; Telegeev, G.D. Comprehensive Review of Chronic Stress Pathways and the Efficacy of Behavioral Stress Reduction Programs (BSRPs) in Managing Diseases. Int. J. Environ. Res. Public Health 2024, 21, 1077. https://doi.org/10.3390/ijerph21081077
Shchaslyvyi AY, Antonenko SV, Telegeev GD. Comprehensive Review of Chronic Stress Pathways and the Efficacy of Behavioral Stress Reduction Programs (BSRPs) in Managing Diseases. International Journal of Environmental Research and Public Health. 2024; 21(8):1077. https://doi.org/10.3390/ijerph21081077
Chicago/Turabian StyleShchaslyvyi, Aladdin Y., Svitlana V. Antonenko, and Gennadiy D. Telegeev. 2024. "Comprehensive Review of Chronic Stress Pathways and the Efficacy of Behavioral Stress Reduction Programs (BSRPs) in Managing Diseases" International Journal of Environmental Research and Public Health 21, no. 8: 1077. https://doi.org/10.3390/ijerph21081077
APA StyleShchaslyvyi, A. Y., Antonenko, S. V., & Telegeev, G. D. (2024). Comprehensive Review of Chronic Stress Pathways and the Efficacy of Behavioral Stress Reduction Programs (BSRPs) in Managing Diseases. International Journal of Environmental Research and Public Health, 21(8), 1077. https://doi.org/10.3390/ijerph21081077


_Garrett.png)



