Technological Advances in the Diagnosis of Cardiovascular Disease: A Public Health Strategy
Abstract
1. Introduction
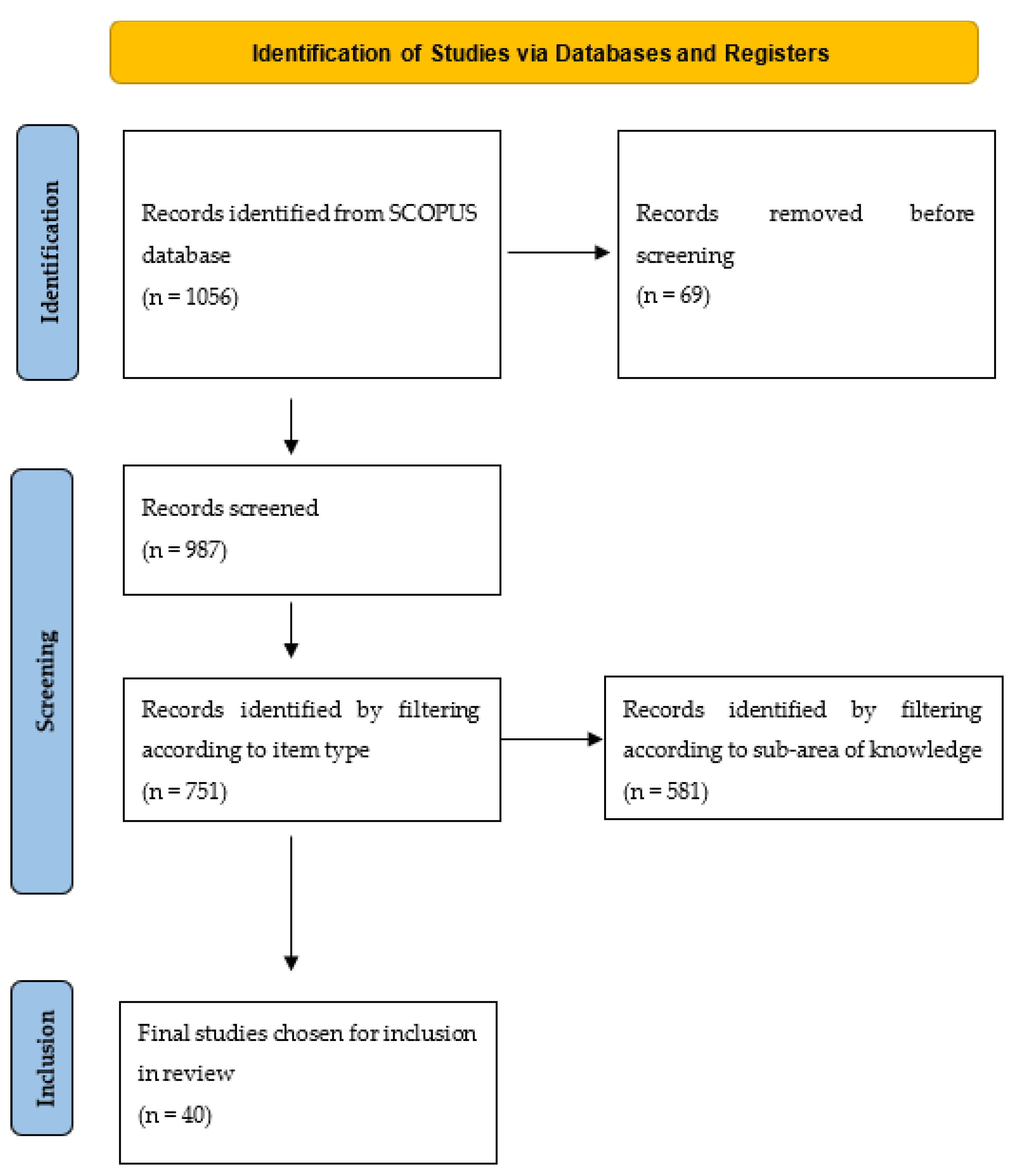
2. Methods
2.1. Search Strategy
2.1.1. Search Source
2.1.2. Search Terms and Criteria
- -
- Publications within the last 13 years;
- -
- Articles and reviews published in popular science journals.
- -
- Publications prior to 2010;
- -
- Books, book chapters, conferences, and other types of publications that are not published in indexed popular science journals;
- -
- Research outside the field of health sciences and health technology.
3. Results
3.1. Scientific Production
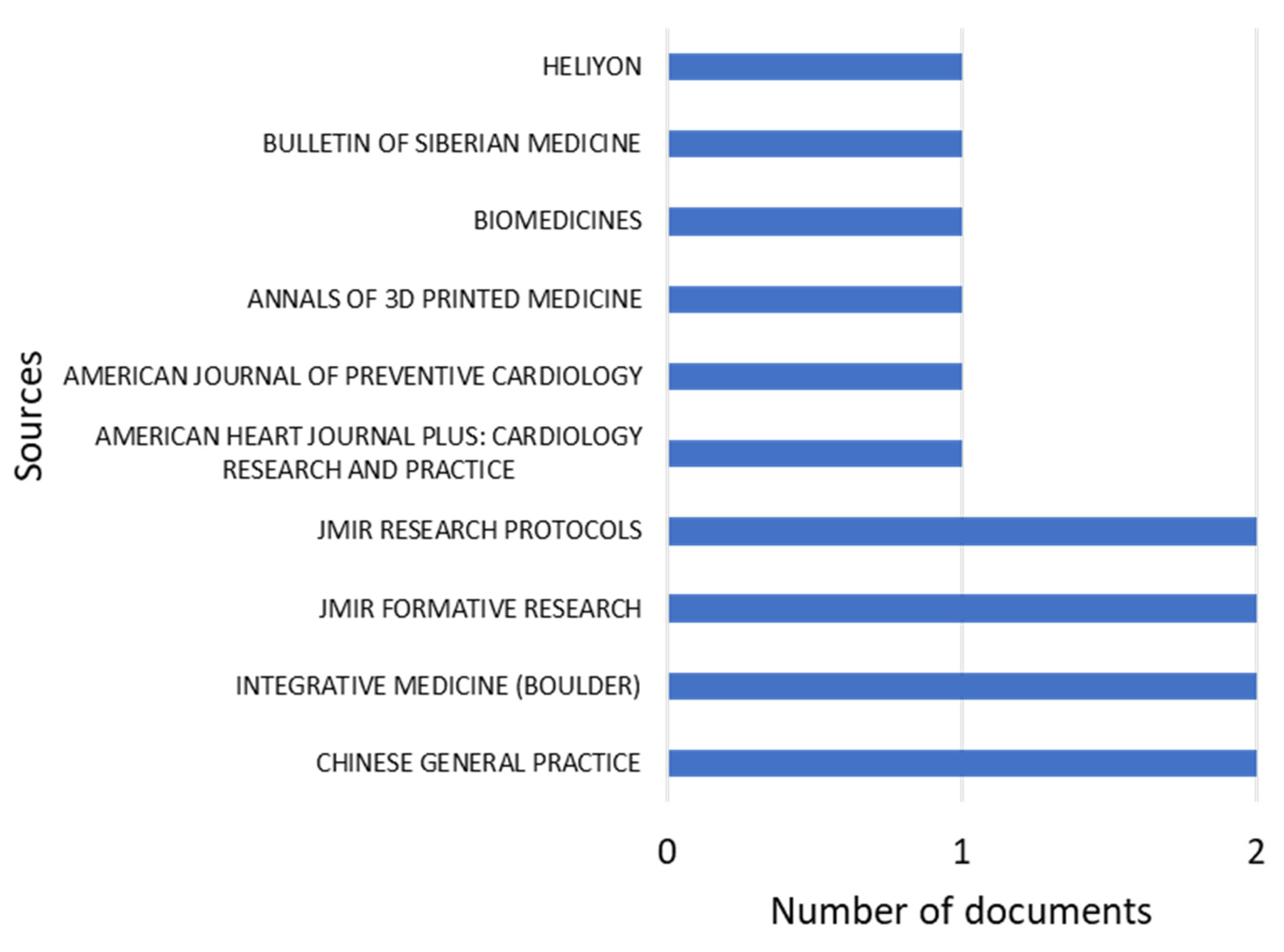
3.2. Most Relevant Journals
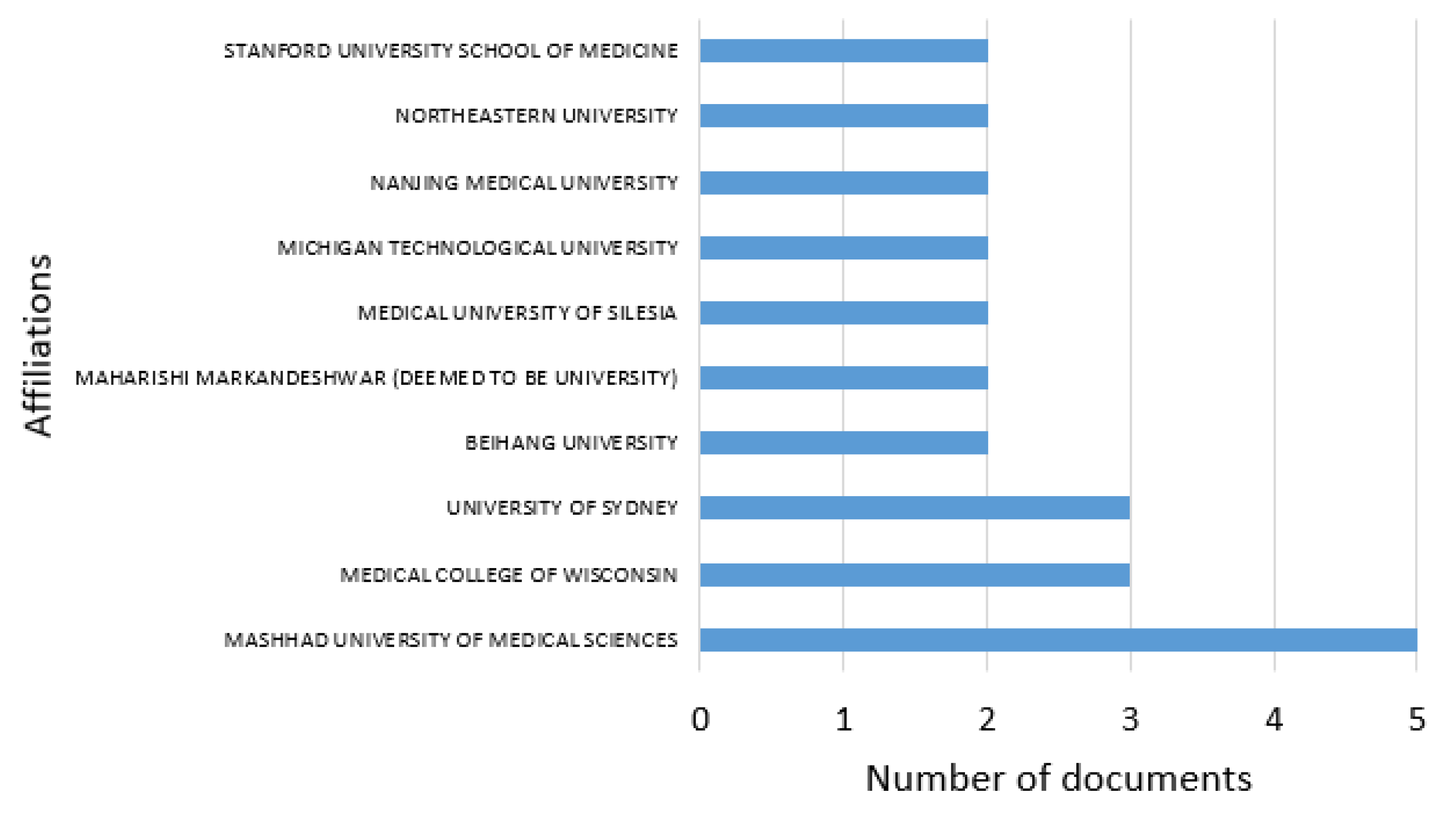
3.3. Most Relevant Institutions
3.4. Cooperation between Countries
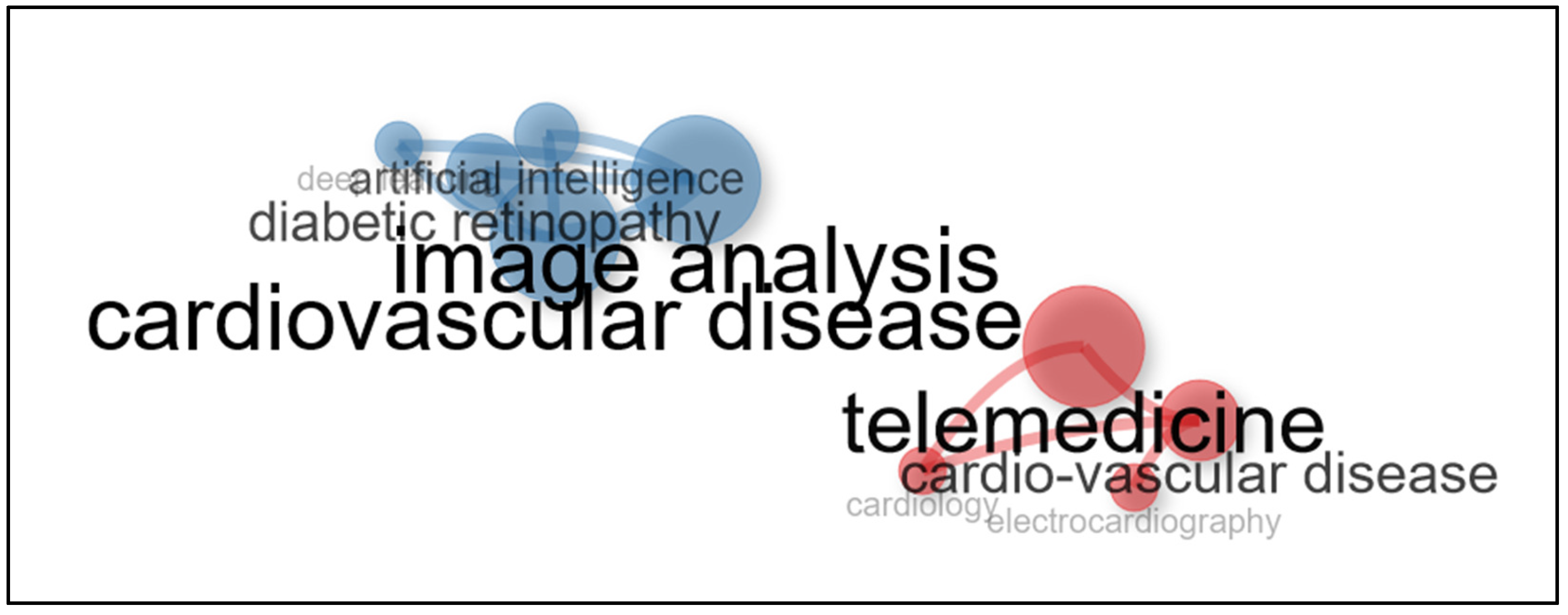
3.5. Keyword Analysis
3.6. Medical Technology
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Gerc, V.; Masic, I.; Salihefendic, N.; Zildzic, M. Cardiovascular Diseases (CVDs) in COVID-19 Pandemic Era. Mater. Socio-Medica 2020, 32, 158. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7428924/ (accessed on 26 June 2024). [CrossRef]
- Rubiés-Prat, J. Factores de riesgo cardiovascular. Med. -Programa de Form. Médica Contin. Acreditado 2005, 9, 2506–2513. [Google Scholar] [CrossRef]
- Padua, G.R.; Jacobo, W.; Piñera, D.; Gladys, M.; Padua, R. Enfermedades no transmisibles. Tendencias actuales. Revista Cubana de Salud y Trabajo 2012, 13, 50. Available online: https://revsaludtrabajo.sld.cu/index.php/revsyt/article/view/609 (accessed on 26 June 2024).
- Turcu, A.M.; Ilie, A.C.; Ștefăniu, R.; Țăranu, S.M.; Sandu, I.A.; Alexa-Stratulat, T.; Pîslaru, A.I.; Alexa, I.D. The impact of heart rate variability monitoring on preventing severe cardiovascular events. Diagnostics 2023, 13, 2384. [Google Scholar] [CrossRef]
- Blanco-Colio, L.M.; Méndez-Barbero, N.; Pello Lázaro, A.M.; Aceña, Á.; Tarín, N.; Cristóbal, C.; Martínez-Milla, J.; González-Lorenzo, Ó.; Martín-Ventura, J.L.; Huelmos, A.; et al. MCP-1 predicts recurrent cardiovascular events in patients with persistent inflammation. J. Clin. Med. 2021, 10, 1137. [Google Scholar] [CrossRef]
- Freak-Poli, R.; Hu, J.; Phyo, A.Z.Z.; Barker, S.F. Social isolation and social support influence health service utilisation and survival after a cardiovascular disease event: A systematic review. Int. J. Environ. Res. Public Health 2023, 20, 4853. [Google Scholar] [CrossRef]
- Zheng, Z.; Zhang, P.; Yuan, F.; Bo, Y. Scientometric analysis of the relationship between a built environment and cardiovascular disease. Int. J. Environ. Res. Public Health 2022, 19, 5625. [Google Scholar] [CrossRef]
- Attaran, M. Blockchain technology in healthcare: Challenges and opportunities. Int. J. Healthc. Manag. 2022, 15, 70–83. [Google Scholar] [CrossRef]
- Sandeep, B.; Liu, X.; Huang, X.; Wang, X.; Mao, L.; Xiao, Z. Feasibility of artificial intelligence its current status, clinical applications, and future direction in cardiovascular disease. Curr. Probl. Cardiol. 2024, 49, 102349. [Google Scholar] [CrossRef]
- Morcillo Serra, C.; González Romero, J.L. New digital healthcare technologies. Med. Clin. 2020, 154, 257–259. [Google Scholar] [CrossRef]
- Yin, A.L.; Hachuel, D.; Pollak, J.P.; Scherl, E.J.; Estrin, D. Digital health apps in the clinical care of inflammatory bowel disease: Scoping review. J. Med. Internet Res. 2019, 21, e14630. [Google Scholar] [CrossRef] [PubMed]
- Baladrón, C.; de Diego, J.J.G.; Amat-Santos, I.J. Big data and new information technology: What cardiologists need to know. Rev. Española Cardiol. (Engl.Ed.) 2021, 74, 81–89. [Google Scholar] [CrossRef]
- Gomez-Garcia, C.A.; Askar-Rodriguez, M.; Velasco-Medina, J. Platform for Healthcare Promotion and Cardiovascular Disease Prevention. IEEE J. Biomed. Health Inform. 2021, 25, 2758–2767. [Google Scholar] [CrossRef] [PubMed]
- Mohsen, F.; Al-Saadi, B.; Abdi, N.; Khan, S.; Shah, Z. Artificial Intelligence-Based Methods for Precision Cardiovascular Medicine. J. Pers. Med. 2023, 13, 1268. [Google Scholar] [CrossRef] [PubMed]
- Yeung, A.W.K.; Kulnik, S.T.; Parvanov, E.D.; Fassl, A.; Eibensteiner, F.; Völkl-Kernstock, S.; Kletecka-Pulker, M.; Crutzen, R.; Gutenberg, J.; Höppchen, I.; et al. Research on Digital Technology Use in Cardiology: Bibliometric Analysis. J. Med. Internet Res. 2022, 24, e36086. [Google Scholar] [CrossRef] [PubMed]
- Chou, H.-Y.; Tsai, Y.-W.; Ma, S.-C.; Ma, S.-M.; Shih, C.-L.; Yeh, C.-T. Efficacy and cost over 12 hospitalization weeks of postacute care for stroke. Int. J. Environ. Res. Public Health 2023, 20, 1419. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Antes, G.; Atkins, D.; Barbour, V.; Barrowman, N.; Berlin, J.A.; Clark, J.; et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, 336–341. [Google Scholar] [CrossRef] [PubMed]
- Aria, M.; Cuccurullo, C. bibliometrix: An R-tool for comprehensive science mapping analysis. J. Informetr. 2017, 11, 959–975. [Google Scholar] [CrossRef]
- Gauffriau, M.; Larsen, P.O.; Maye, I.; Roulin-Perriard, A.; von Ins, M. Publication, cooperation and productivity measures in scientific research. Scientometrics 2007, 73, 175–214. [Google Scholar] [CrossRef]
- Weismayer, C.; Pezenka, I. Identifying emerging research fields: A longitudinal latent semantic keyword analysis. Scientometrics 2017, 113, 1757–1785. [Google Scholar] [CrossRef]
- Leng, S.; Tan, R.S.; Chai, K.T.C.; Wang, C.; Ghista, D.; Zhong, L. The electronic stethoscope. Biomed. Eng. Online 2015, 14, 1–37. [Google Scholar] [CrossRef]
- Reed, T.R.; Reed, N.E.; Fritzson, P. Heart sound analysis for symptom detection and computer-aided diagnosis. Simul. Model. Pract. Theory 2004, 12, 129–146. [Google Scholar] [CrossRef]
- Wong, K.K.L.; Fortino, G.; Abbott, D. Deep learning-based cardiovascular image diagnosis: A promising challenge. Futur. Gener. Comput. Syst. 2020, 110, 802–811. [Google Scholar] [CrossRef]
- Briganti, G.; Le Moine, O. Artificial intelligence in medicine: Today and tomorrow. Front. Med. 2020, 7, 509744. Available online: https://www.frontiersin.org/articles/10.3389/fmed.2020.00027/full?trk=article-ssr-frontend-pulse_x-social-details_comments-action_comment-text (accessed on 26 June 2024). [CrossRef]
- Li, X.; Liu, X.; Deng, X.; Fan, Y. Interplay between artificial intelligence and biomechanics modeling in the cardiovascular disease prediction. Biomedicines 2022, 10, 2157. [Google Scholar] [CrossRef]
- Javaid, A.; Zghyer, F.; Kim, C.; Spaulding, E.M.; Isakadze, N.; Ding, J.; Kargillis, D.; Gao, Y.; Rahman, F.; Brown, D.E.; et al. Medicine 2032: The future of cardiovascular disease prevention with machine learning and digital health technology. Am. J. Prev. Cardiol. 2022, 12, 100379. [Google Scholar] [CrossRef] [PubMed]
- Tang, Z.; Chen, K.; Pan, M.; Wang, M.; Song, Z. An Augmentation Strategy for Medical Image Processing Based on Statistical Shape Model and 3D Thin Plate Spline for Deep Learning. IEEE Access 2019, 7, 133111–133121. [Google Scholar] [CrossRef]
- Lindquist, E.M.; Gosnell, J.M.; Khan, S.K.; Byl, J.L.; Zhou, W.; Jiang, J.; Vettukattil, J.J. 3D printing in cardiology: A review of applications and roles for advanced cardiac imaging. Ann. 3D Print. Med. 2021, 4, 100034. [Google Scholar] [CrossRef]
- Huang, Y.; Cheung, C.Y.; Li, D.; Tham, Y.C.; Sheng, B.; Cheng, C.Y.; Wang, Y.X.; Wong, T.Y. AI-integrated ocular imaging for predicting cardiovascular disease: Advancements and future outlook. Eye 2024, 38, 464–472. [Google Scholar] [CrossRef] [PubMed]
- Azmi, J.; Arif, M.; Nafis, M.T.; Alam, M.A.; Tanweer, S.; Wang, G. A systematic review on machine learning approaches for cardiovascular disease prediction using medical big data. Med. Eng. Phys. 2022, 105, 103825. [Google Scholar] [CrossRef]
- Tamura, Y.; Nomura, A.; Kagiyama, N.; Mizuno, A.; Node, K. Digitalomics, digital intervention, and designing future: The next frontier in cardiology. J. Cardiol. 2024, 83, 318–322. [Google Scholar] [CrossRef]
- Sun, Z. Clinical applications of patient-specific 3d printed models in cardiovascular disease: Current status and future directions. Biomolecules 2020, 10, 1577. [Google Scholar] [CrossRef]
- Al Knawy, B.; McKillop, M.M.; Abduljawad, J.; Tarkoma, S.; Adil, M.; Schaper, L.; Chee, A.; Bates, D.W.; Klag, M.; Lee, U.; et al. Successfully implementing digital health to ensure future global health security during pandemics: A consensus statement. JAMA Netw. Open 2022, 5, 220214. [Google Scholar] [CrossRef]
- Dhingra, D.; Dabas, A. Global Strategy on Digital Health. Indian Pediatr. 2020, 57, 356–358. [Google Scholar] [CrossRef]
- Garavand, A.; Aslani, N.; Nadri, H.; Abedini, S.; Dehghan, S. Acceptance of telemedicine technology among physicians: A systematic review. Inform. Med. Unlocked 2022, 30, 100943. [Google Scholar] [CrossRef]
- Gorshkov, Y. Visualization of power supply network interference in telemedicine systems of mobile electrocardiography. Sci. Vis. 2021, 13, 44–53. [Google Scholar] [CrossRef]
- France, K.; Jaya, A.; Tiliute, D. Machine and Deep Learning Algorithms for Healthcare Applications. In Handbook of Intelligent Healthcare Analytics: Knowledge Engineering with Big Data Analytics; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2022; pp. 233–253. [Google Scholar] [CrossRef]
- Jaen-Extremera, J.; Afanador-Restrepo, D.F.; Rivas-Campo, Y.; Gomez-Rodas, A.; Aibar-Almazan, A.; Hita-Contreras, F.; Carcelen-Fraile, M.d.C.; Castellote-Caballero, Y.; Ortiz-Quesada, R. Effectiveness of telemedicine for reducing cardiovascular risk: A systematic review and meta-analysis. J. Clin. Med. 2023, 12, 841. [Google Scholar] [CrossRef] [PubMed]
- Wongvibulsin, S.; Martin, S.S.; Steinhubl, S.R.; Muse, E.D. Connected health technology for cardiovascular disease prevention and management. Curr. Treat. Options Cardiovasc. Med. 2019, 21, 1–15. [Google Scholar] [CrossRef] [PubMed]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Restrepo Tique, M.; Araque, O.; Sanchez-Echeverri, L.A. Technological Advances in the Diagnosis of Cardiovascular Disease: A Public Health Strategy. Int. J. Environ. Res. Public Health 2024, 21, 1083. https://doi.org/10.3390/ijerph21081083
Restrepo Tique M, Araque O, Sanchez-Echeverri LA. Technological Advances in the Diagnosis of Cardiovascular Disease: A Public Health Strategy. International Journal of Environmental Research and Public Health. 2024; 21(8):1083. https://doi.org/10.3390/ijerph21081083
Chicago/Turabian StyleRestrepo Tique, Maria, Oscar Araque, and Luz Adriana Sanchez-Echeverri. 2024. "Technological Advances in the Diagnosis of Cardiovascular Disease: A Public Health Strategy" International Journal of Environmental Research and Public Health 21, no. 8: 1083. https://doi.org/10.3390/ijerph21081083
APA StyleRestrepo Tique, M., Araque, O., & Sanchez-Echeverri, L. A. (2024). Technological Advances in the Diagnosis of Cardiovascular Disease: A Public Health Strategy. International Journal of Environmental Research and Public Health, 21(8), 1083. https://doi.org/10.3390/ijerph21081083







