Institutional Violence Perpetrated against Transgender Individuals in Health Services: A Systematic Review of Qualitative Studies
Abstract
1. Introduction
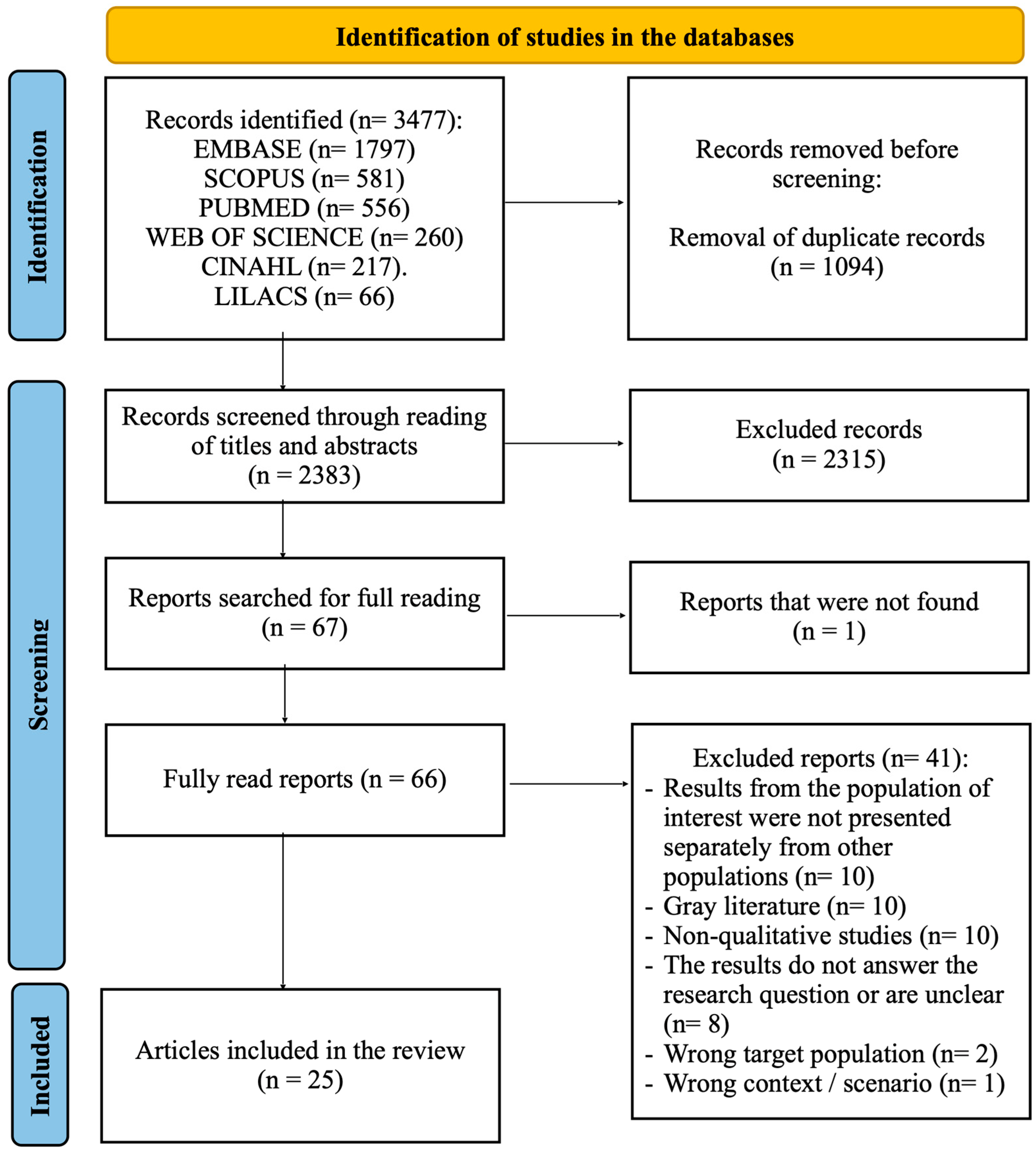
2. Materials and Methods
3. Results
4. Discussion
4.1. Refusal of Care
4.2. Resistance to the Use of Social Names and Pronouns
4.3. Barriers to Accessing Health Services
4.4. Discrimination and Stigma
4.5. Insensitivity of Healthcare Workers
4.6. Lack of Confidence in Healthcare Services
4.7. Technological Limitations Relating to the Binary-Focused System
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hernandez-Valles, J.; Arredondo-Lopez, A. Barreras de acceso a los servicios de salud en la comunidad transgénero y transexual. Horiz. Sanit. 2020, 19, 19–25. [Google Scholar] [CrossRef]
- Silva, N.L.; Lopes, R.O.P.; Bitencourt, G.R.; Bossato, H.R.; Brandão, M.A.G.; Ferreira, M.A. Identidade social da pessoa transgěnero: Análise do conceito e proposição do diagnόstico de enfermagem. Rev. Bras. Enferm. 2020, 73, e20200070. [Google Scholar] [CrossRef]
- Silva, L.K.M.; Silva, A.L.M.A.; Coelho, A.A.; Martiniano, C.S. Uso do nome social no Sistema Único de Saúde: Elementos para o debate sobre a assistência prestada a travestis e transexuais. Physis 2017, 27, 835–846. [Google Scholar] [CrossRef]
- Winter, S.; Diamond, M.; Green, J.; Karmic, D.; Reed, T.; Whittle, S.; Wylie, K. Transgender people: Health at the margins of society. Lancet 2016, 388, 390–400. [Google Scholar] [CrossRef]
- Silva, G.W.S.; Meira, C.K.; Azevedo, D.M.; Sena, R.C.F.; Lins, S.L.F.; Dantas, E.S.O.; Miranda, F.A.N. Fatores associados à ideação suicida em travestis e transexuais assistidas por organizações não governamentais. Cien Saude Colet. 2021, 26, 4955–4966. [Google Scholar] [CrossRef]
- Schuster, M.A.; Reisner, S.L.; Onorato, S.E. Beyond Bathrooms--Meeting the Health Needs of Transgender People. N. Engl. J. Med. 2016, 375, 101–103. [Google Scholar] [CrossRef]
- Silva, G.W.S.; Souza, E.F.L.; Sena, R.C.F.; Moura, I.B.L.; Sobreira, M.V.S.; Miranda, F.A.N. Situações de violência contra travestis e transexuais em um município do nordeste brasileiro. Rev. Gaúcha Enferm. 2016, 37, e56407. [Google Scholar] [CrossRef]
- Moreira, G.A.R. Manifestações de violência institucional no contexto da atenção em saúde às mulheres em situação de violência sexual. Saúde Soc. 2020, 29, e80895. [Google Scholar] [CrossRef]
- Trindade, M. Violência Institucional e Transexualidade: Desafios para o Serviço Social. Rev. Praia Vermelha 2015, 25, 209–233. [Google Scholar]
- Azevedo, Y.N.; Schraiber, L.B. Violência institucional e humanização em saúde: Apontamentos para o debate. Ciênc Saúde Colet. 2017, 22, 3013–3022. [Google Scholar] [CrossRef]
- Mkhize, S.P.; Maharaj, P. Structural violence on the margins of society: LGBT student access to health services. Agenda 2020, 34, 104–114. [Google Scholar] [CrossRef]
- Mulavu, M.; Menon, J.A.; Mulubwa, C.; Matenga, T.F.L.; Nguyen, H.; MacDonell, K.; Wang, B.; Mweemba, O. Psychosocial challenges and coping strategies among people with minority gender and sexual identities in Zambia: Health promotion and human rights implications. Health Psychol. Behav. Med. 2021, 11, 2173201. [Google Scholar] [CrossRef]
- Kenagy, G.P. Transgender health: Findings from two needs assessment studies in Philadelphia. Health Social. Work. 2005, 30, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Miskolci, R.; Signorelli, M.C.; Canavese, D.; Teixeira, F.B.; Polidoro, M.; Moretti-Pires, R.O.; Souza, M.H.T.; Pereira, P.P.G. Health challenges in the LGBTI+ population in Brazil: A scenario analysis through the triangulation of methods. Cien Saude Colet. 2022, 27, 3815–3824. [Google Scholar] [CrossRef]
- Shihadeh, N.A.; Pessoa, E.M.; Silva, F.F. A (in)visibilidade do acolhimento no âmbito da saúde: Em pauta as experiências de integrantes da comunidade LGBTQIA+. Barbarói 2021, 58, 172–194. [Google Scholar] [CrossRef]
- Rocon, P.C.; Wandekoken, K.D.; Barros, M.E.B.; Duarte, M.J.O.; Sodré, F. Acesso à saúde pela população trans no Brasil: Nas entrelinhas da revisão integrativa. Trab. Educ. Saúde 2020, 18, e0023469. [Google Scholar] [CrossRef]
- Bristowe, K.; Hodson, M.; Wee, B.; Almack, K.; Johnson, K.; Daveson, B.A.; Koffman, J.; McEnhill, L.; Harding, R. Recommendations to reduce inequalities for LGBT people facing advanced illness: ACCESSCare national qualitative interview study. Palliat. Med. 2018, 32, 23–35. [Google Scholar] [CrossRef]
- Beattie, T.S.H.; Bhattacharjee, P.; Suresh, M.; Isac, S.; Ramesh, B.M.; Moses, S. Personal, interpersonal and structural challenges to accessing HIV testing, treatment and care services among female sex workers, men who have sex with men and transgenders in Karnataka state, South India. J. Epidemiol. Community Health 2012, 66, ii42–ii48. [Google Scholar] [CrossRef]
- Jones, S.; Patel, T. Inaccessible and stigmatizing: LGBTQ+ youth perspectives of services and sexual violence. LGBT Youth 2022, 20, 632–657. [Google Scholar] [CrossRef]
- Evens, E.; Lanham, M.; Santi, K.; Cooke, J.; Ridgeway, K.; Morales, G.; Parker, C.; Brennan, C.; Bruin, M.; Desrosiers, P.C.; et al. Experiences of gender-based violence among female sex workers, men who have sex with men, and transgender women in Latin America and the Caribbean: A qualitative study to inform HIV programming. BMC Int. 2019, 19, 9. [Google Scholar] [CrossRef]
- Azucar, D.; Slay, L.; Valerio, D.G.; Kipke, M.D. Barriers to COVID-19 Vaccine Uptake in the LGBTQIA Community. Am. J. Public. Health 2022, 112, 405–407. [Google Scholar] [CrossRef] [PubMed]
- Gomes, R.; Murta, D.; Facchini, R.; Meneghel, S.N. Gênero, direitos sexuais e suas implicações na saúde. Saúde Colet. 2018, 23, 1997–2005. [Google Scholar] [CrossRef]
- Shires, D.A.; Jaffee, K. Factors associated with health care discrimination experiences among a national sample of female-to-male transgender individuals. Health Soc. Work 2015, 40, 134–141. [Google Scholar] [CrossRef] [PubMed]
- Logie, C.; James, L.; Tharao, W.; Loutfy, M.R. “We don’t exist”: A qualitative study of marginalization experienced by HIV-positive lesbian, bisexual, queer and transgender women in Toronto, Canada. J. Int. AIDS Soc. 2012, 15, 1–11. [Google Scholar] [CrossRef]
- Doan, P.; Johnston, L. Rethinking Transgender Identities: Reflections from Around the Globe; Routledge: London, UK, 2022. [Google Scholar]
- Jesus, J.G. Transfobia e crimes de ódio: Assassinatos de pessoas transgênero como genocídio. (In)visibilidade Trans 2. História Agora 2013, 16, 101–123. [Google Scholar]
- Joanna Briggs Institute. JBI Manuals. Available online: https://jbi.global/ebp#jbi-manuals (accessed on 3 March 2024).
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, 71. [Google Scholar] [CrossRef]
- Lopes, A.L.M.; Fracolli, L.A. Revisão sistemática de literatura e metassíntese qualitativa: Considerações sobre sua aplicação na pesquisa em enfermagem. Texto Contexto Enferm. 2008, 17, 771–778. [Google Scholar] [CrossRef]
- Deslandes, S.F.; Gomes, R.; Minayo, M.C.S. Pesquisa Social: Teoria, Método e Criatividade, 29th ed.; Vozes: Petrópolis, Brazil, 2010. [Google Scholar]
- Marsiglia, R.M.G. Perfil dos trabalhadores da atenção básica em saúde no município de São Paulo: Região norte e central da cidade. Saúde Soc. 2011, 20, 900–911. [Google Scholar] [CrossRef]
- Aromataris, E.; Lockwood, C.; Porritt, K.; Pilla, B.; Jordan, Z. JBI Manual for Evidence Synthesis. JBI; 2024. Available online: https://synthesismanual.jbi.global (accessed on 25 March 2024).
- Xavier, J.; Bradford, J.; Hendricks, M.; Safford, L.; McKee, R.; Martin, E.; Honnold, J.A. Transgender health care access in Virginia: A qualitative study. Int. J. Transgenderism 2013, 14, 3–17. [Google Scholar] [CrossRef]
- Kosenko, K.; Rintamaki, L.; Raneym, S.; Maness, K. Transgender Patient Perceptions of Stigma in Health Care Contexts. Med. Care 2013, 51, 819–822. [Google Scholar] [CrossRef] [PubMed]
- Lyons, T.; Shannon, K.; Pierre, L.; Small, W.; Krüsi, A.; Kerr, T. A qualitative study of transgender individuals’ experiences in residential addiction treatment settings: Stigma and inclusivity. Subst. Abus. Treat. Prev. Policy 2015, 10, 17. [Google Scholar] [CrossRef]
- Souza, M.H.T.; Malvasi, P.; Signorelli, M.C.; Pereira, P.P.G. Violência e sofrimento social no itinerário de travestis de Santa Maria, Rio Grande do Sul, Brasil. Cad. Saúde Pública 2015, 31, 676–776. [Google Scholar] [CrossRef]
- Lyons, T.; Krusi, A.; Pierre, L.; Smith, A.; Small, W.; Shannon, K. Experiences of Trans Women and Two-Spirit Persons Accessing Women-Specific Health and Housing Services in a Downtown Neighborhood of Vancouver, Canada. LGBT Health 2016, 3, 373–378. [Google Scholar] [CrossRef]
- Ritterbusch, A.E.; Salazar, C.C.; Correa, A. Stigma-related access barriers and violence against trans women in the Colombian healthcare system. Glob. Public Health 2018, 13, 1831–1845. [Google Scholar] [CrossRef] [PubMed]
- Samuels, E.A.; Tape, C.; Garber, N.; Bowman, S.; Choo, E.K. “Sometimes You Feel Like the Freak Show”: A qualitative assessment of emergency care experiences among transgender and gender-nonconforming patients. Ann. Emerg. Med. 2018, 71, 170–182. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, S.; Brigeiro, M. Experiences of transgender women/transvestites with access to health services: Progress, limits, and tensions. Cad. Saúde Pública 2019, 35, e00111318. [Google Scholar] [CrossRef]
- King, R.; Nanteza, J.; Sebyala, Z.; Bbaale, J.; Sande, E.; Poteat, T.; Kiyingi, H.; Hladik, W. HIV and transgender women in Kampala, Uganda—Double Jeopardy. Double Jeopardy Cult. Health Sex. 2019, 21, 727–740. [Google Scholar] [CrossRef] [PubMed]
- Goldenberg, A.E.; Kuvalanka, K.A.; Budge, S.L.; Benz, M.B.; Smith, J.Z. Health Care Experiences of Transgender Binary and Nonbinary University Students. Couns. Psychol. 2019, 47, 59–97. [Google Scholar] [CrossRef]
- Dutta, S.; Khan, S.; Lorway, R. Following the divine: An ethnographic study of structural violence among transgender in South India. Cult. Health Sex. 2019, 21, 1240–1256. [Google Scholar] [CrossRef]
- Calderón-Jaramillo, M.; Mendoza, Á.; Acevedo, N.; Forero-Martínez, L.J.; Sánchez, S.M.; Rivillas-García, J.C. How to adapt sexual and reproductive health services to the needs and circumstances of trans people— a qualitative study in Colombia. Int. J. Equity Health 2020, 19, 148. [Google Scholar] [CrossRef]
- Silva, R.G.; Abreu, P.D.; Araújo, E.C.; Santana, A.D.S.; Sousa, J.C.; Lyra, J.; Santos, C.B. Vulnerability in the health of young transgender women living with HIV/AIDS. Rev. Bras. Enferm. 2020, 73, e20190046. [Google Scholar] [CrossRef]
- Lacombe-Duncan, A.; Olawale, R. Context, Types, and Consequences of Violence Across the Life Course: A Qualitative Study of the Lived Experiences of Transgender Women Living with HIV. J. Interpers. Violence 2020, 37, 2242–2266. [Google Scholar] [CrossRef]
- Reisner, S.L.; Silva-Santisteban, A.; Salazar, X.; Vilela, J.; D’Amico, L.; Perez-Brumer, A. “Existimos”: Health and social needs of transgender men in Lima, Peru. PLoS ONE 2021, 16, e0254494. [Google Scholar] [CrossRef]
- Oliveira, G.S.; Salimena, A.M.O.; Penna, L.H.G.; Paraíso, A.F.; Ramos, C.M.; Alves, M.S.; Pacheco, Z.M.L. O vivido de mulheres trans ou travestis no acesso aos serviços públicos de saúde. Rev. Bras. Enferm. 2022, 75, e20210713. [Google Scholar] [CrossRef]
- Santander-Morillas, K.; Leyva-Moral, J.M.; Villar-Salgueiro, M.; Aguayo-González, M.; Téllez-Velasco, D.; Granel-Giménez, N.; Gómez-Ibáñez, R. TRANSALUD: A qualitative study of the healthcare experiences of transgender people in Barcelona (Spain). PLoS ONE 2022, 17, e0271484. [Google Scholar] [CrossRef]
- Tun, W.; Pulerwitz, J.; Shoyemi, E.; Fernandez, A.; Adeniran, A.; Ejiogu, F.; Sangowawa, O.; Granger, K.; Dirisu, O.; Adedimeji, A.A. A qualitative study of how stigma influences HIV services for transgender men and women in Nigeria. J. Int. AIDS Soc. 2022, 25, e25933. [Google Scholar] [CrossRef] [PubMed]
- Ssekamatte, T.; Nalugya, A.; Isunju, J.B.; Naume, M.; Oputan, P.; Kiguli, J.; Wafula, S.T.; Kibira, S.P.S.; Ssekamatte, D.; Orza, L.; et al. Help-seeking and challenges faced by transwomen following exposure to gender-based violence; a qualitative study in the Greater Kampala Metropolitan Area, Uganda. Int. J. Equity Health 2022, 21, 171. [Google Scholar] [CrossRef]
- Sherman, A.D.F.; Bhaltazar, M.S.; Daniel, G.; Johnson, K.B.; Klepper, M.; Clark, K.D.; Baguso, G.N.; Cicero, E.; Allure, K.; Wharton, W.; et al. Barriers to accessing and engaging in healthcare as potential modifiers in the association between polyvictimization and mental health among Black transgender women. PLoS ONE 2022, 17, e0269776. [Google Scholar] [CrossRef]
- Lobo, B.H.S.C.; Santos, G.S.; Porcino, C.; Mota, T.N.; Machuca-Contreras, F.A.; Oliveira, J.F.; Carvalho, E.S.S.; Sousa, A.R. Transphobia as a social disease: Discourses of vulnerabilities in trans men and transmasculine people. Rev. Bras. Enferm. 2023, 76, e20220183. [Google Scholar] [CrossRef]
- Jesus, M.K.M.R.; Moré, I.A.A.; Querino, R.A.; Oliveira, V.H. Transgender women’s experiences in the healthcare system: Visibility towards equity. Interface 2023, 27, e220369. [Google Scholar] [CrossRef]
- Muyanga, N.; Isunju, J.B.; Ssekamatte, T.; Nalugya, A.; Oputan, P.; Kiguli, J.; Kibira, S.P.S.; Wafula, S.T.; Ssekamatte, D.; Mugambe, R.K.; et al. Understanding the effect of gender-based violence on uptake and utilisation of HIV prevention, treatment, and care services among transgender women: A qualitative study in the greater Kampala metropolitan area, Uganda. BMC Women’s Health 2023, 23, 250. [Google Scholar] [CrossRef]
- Burchell, D.; Coleman, T.; Travers, R.; Aversa, I.; Schmid, E.; Coulombe, S.; Wilson, C.; Woodford, M.R.; Davis, C. ‘I don’t want to have to teach every medical provider’: Barriers to care among non-binary people in the Canadian healthcare system. Cult. Health Sex. 2023, 26, 61–76. [Google Scholar] [CrossRef] [PubMed]
- Atuk, T. “If I knew you were a travesti, I wouldn’t have touched you”: Iatrogenic violence and trans necropolitics in Turkey. Social. Sci. Med. 2024, 345, 116693. [Google Scholar] [CrossRef]
- Mello, L.; Perilo, M.; Braz, C.A.; Pedrosa, C. Políticas de saúde para lésbicas, gays, bissexuais, travestis e transexuais no Brasil: Em busca de universalidade, integralidade e equidade. Sex. Salud Soc. 2011, 9, 7–28. [Google Scholar] [CrossRef]
- Teixeira, F.B. Histórias que não têm era uma vez: As (in)certezas da transexualidade. Estud. Fem. 2014, 20, 501–521. [Google Scholar] [CrossRef]
- Rosa, D.F.; Carvalho, M.V.F.; Pereira, N.R.; Rocha, N.T.; Neves, V.R.; Rosa, A.S. Nursing Care for the transgender population: Genders from the perspective of professional practice. Rev. Bras. Enferm. 2019, 72, 311–319. [Google Scholar] [CrossRef]
- Rocon, P.C.; Sodré, F.; Zamboni, J.; Rodrigues, A.; Roseiro, M.C.F. What trans people expect of the Brazilian National Health System? Interface 2018, 22, 43–53. [Google Scholar] [CrossRef]
- Almeida, G.; Murta, D. Reflexões sobre a possibilidade da despatologização da transexualidade e a necessidade da assistência integral à saúde de transexuais no Brasil. Sex. Salud Soc. 2013, 14, 380–407. [Google Scholar] [CrossRef]
- Shah, H.B.U.; Rashid, F.; Atif, I.; Hydrie, M.Z.; Fawad, M.W.B.; Muzaffar, H.Z.; Rehman, A.; Anjum, S.; Mehroz, M.B.; Haider, A.; et al. Challenges faced by marginalized communities such as transgenders in Pakistan. Pan Afr. Med. J. 2018, 30, 1–7. [Google Scholar] [CrossRef]
- Lo, S.; Horton, R. Transgender health: An opportunity for global health equity. Lancet 2016, 388, 316–318. [Google Scholar] [CrossRef]
| Acronym Application | Descriptors Found | |
|---|---|---|
| P | Transgender persons | “transgender persons”, “transgender person”, transgender, transvestisme, “sexual and gender minorities”, transvestism, “gender dysphoria”, transfeminine, “trans-Feminine”, transmasculine, “trans-Masculine”, transexual *, transsexual *, “trans people”, “trans person”, “transgender individuals”, trans |
| I | Violence | violence, “gender violence”, “gender-based violence”, “interpersonal violence”, “interpersonal violences”, “physical attack” |
| Co | Health services | “health services”, “health care services”, “healthcare services”, “health facilities”, “health care facilities”, “healthcare facilities”, “primary health care”, “primary Care”, “primary healthcare”, “secondary care”, “secondary cares”, “tertiary healthcare”, “tertiary care”, “care center”, “health services for transgender persons”, “health services accessibility”, “transgender care”, “transinclusive care”, “sexual health”, hospital * |
| Base | Adapted Search Strategy |
|---|---|
| MEDLINE | (“transgender persons” [All Fields] OR “transgender person” [All Fields] OR (“transgender persons” [MeSH Terms] OR (“transgender” [All Fields] AND “persons” [All Fields]) OR “transgender persons” [All Fields] OR “transgender” [All Fields] OR “transgendered” [All Fields] OR “transgenders” [All Fields]) OR “transvestisme” [All Fields] OR “sexual and gender minorities” [All Fields] OR (“transvestic” [All Fields] OR “transvestism” [MeSH Terms] OR “transvestism” [All Fields]) OR “gender dysphoria” [All Fields] OR “transfeminine” [All Fields] OR “trans-Feminine” [All Fields] OR “transmasculine” [All Fields] OR “trans-Masculine” [All Fields] OR “transexual *” [All Fields] OR “transsexual *” [All Fields] OR “trans people” [All Fields] OR “trans person” [All Fields] OR “transgender individuals” [All Fields] OR “trans” [All Fields]) AND (“violence” [MeSH Terms] OR “violence” [All Fields] OR “violence s” [All Fields] OR “violences” [All Fields] OR “gender violence” [All Fields] OR “gender-based violence” [All Fields] OR “interpersonal violence” [All Fields] OR (“violence” [MeSH Terms] OR “violence” [All Fields] OR (“interpersonal” [All Fields] AND “violences” [All Fields])) OR “physical attack” [All Fields]) AND (“health services” [All Fields] OR “health care services” [All Fields] OR “healthcare services” [All Fields] OR “health facilities” [All Fields] OR “health care facilities” [All Fields] OR “healthcare facilities” [All Fields] OR “primary health care” [All Fields] OR “primary Care” [All Fields] OR “primary healthcare” [All Fields] OR “secondary care” [All Fields] OR “secondary cares” [All Fields] OR “tertiary healthcare” [All Fields] OR “tertiary care” [All Fields] OR “care center” [All Fields] OR “health services for transgender persons” [All Fields] OR “health services accessibility” [All Fields] OR “transgender care” [All Fields] OR “transinclusive care” [All Fields] OR “sexual health” [All Fields] OR “hospital*” [All Fields]) |
| Scopus | TITLE-ABS-KEY (“transgender persons” OR “transgender person” OR transgender OR transvestisme OR “sexual and gender minorities” OR transvestism OR “gender dysphoria” OR transfeminine OR “trans-Feminine” OR transmasculine OR “trans-Masculine” OR transexual * OR transsexual * OR “trans people” OR “trans person” OR “transgender individuals” OR trans) AND TITLE-ABS-KEY (violence OR “gender violence” OR “gender-based violence” OR “interpersonal violence” OR “interpersonal violences” OR “physical attack”) AND TITLE-ABS-KEY (“health services” OR “health care services” OR “healthcare services” OR “health facilities” OR “health care facilities” OR “healthcare facilities” OR “primary health care” OR “primary Care” OR “primary healthcare” OR “secondary care” OR “secondary cares” OR “tertiary healthcare” OR “tertiary care” OR “care center” OR “health services for transgender persons” OR “health services accessibility” OR “transgender care” OR “transinclusive care” OR “sexual health” OR hospital *) |
| EMBASE | #1 ‘transgender persons’/exp OR ‘transgender persons’ OR ‘transgender person’/exp OR ‘transgender person’ OR ‘transgender’/exp OR transgender OR transvestisme OR ‘sexual and gender minorities’/exp OR ‘sexual and gender minorities’ OR ‘transvestism’/exp OR transvestism OR ‘gender dysphoria’/exp OR ‘gender dysphoria’ OR transfeminine OR ‘trans-feminine’ OR transmasculine OR ‘trans-masculine’ OR transexual * OR transsexual * OR ‘trans people’/exp OR ‘trans people’ OR ‘trans person’/exp OR ‘trans person’ OR ‘transgender individuals’ OR trans #2 ‘violence’/exp OR violence OR ‘gender violence’/exp OR ‘gender violence’ OR ‘gender-based violence’/exp OR ‘gender-based violence’ OR ‘interpersonal violence’/exp OR ‘interpersonal violence’ OR ‘interpersonal violences’ OR ‘physical attack’ #3 ‘health services’/exp OR ‘health services’ OR ‘health care services’ OR ‘healthcare services’ OR ‘health facilities’/exp OR ‘health facilities’ OR ‘health care facilities’ OR ‘healthcare facilities’ OR ‘primary health care’/exp OR ‘primary health care’ OR ‘primary care’/exp OR ‘primary care’ OR ‘primary healthcare’/exp OR ‘primary healthcare’OR ‘secondary care’/exp OR ‘secondary care’ OR ‘secondary cares’ OR ‘tertiary healthcare’/exp OR ‘tertiary healthcare’ OR ‘tertiary care’/exp OR ‘tertiary care’ OR ‘care center’ OR ‘health services for transgender persons’/exp OR ‘health services for transgender persons’ OR ‘health services accessibility’/exp OR ‘health services accessibility’ OR ‘transgender care’ OR ‘transinclusive care’ OR ‘sexual health’/exp OR ‘sexual health’ OR hospital* #4 #1AND #2 AND #3 #5 #4AND [embase]/lim |
| Web of Science | “transgender persons” OR “transgender person” OR transgender OR transvestisme OR “sexual and gender minorities” OR transvestism OR “gender dysphoria” OR transfeminine OR “trans-Feminine” OR transmasculine OR “trans-Masculine” OR transexual * OR transsexual* OR “trans people” OR “trans person” OR “transgender individuals” OR trans (Topic) and violence OR “gender violence” OR “gender-based violence” OR “interpersonal violence” OR “interpersonal violences” OR “physical attack” (Topic) and “health services” OR “health care services” OR “healthcare services” OR “health facilities” OR “health care facilities” OR “healthcare facilities” OR “primary health care” OR “primary Care” OR “primary healthcare” OR “secondary care” OR “secondary cares” OR “tertiary healthcare” OR “tertiary care” OR “care center” OR “health services for transgender persons” OR “health services accessibility” OR “transgender care” OR “transinclusive care” OR “sexual health” OR hospital* (Topic) |
| CINAHL | (“transgender persons” OR “transgender person” OR transgender OR transvestisme OR “sexual and gender minorities” OR transvestism OR “gender dysphoria” OR transfeminine OR “trans-Feminine” OR transmasculine OR “trans-Masculine” OR transexual* OR transsexual* OR “trans people” OR “trans person” OR “transgender individuals” OR trans) AND (violence OR “gender violence” OR “gender-based violence” OR “interpersonal violence” OR “interpersonal violences” OR “physical attack”) AND (“health services” OR “health care services” OR “healthcare services” OR “health facilities” OR “health care facilities” OR “healthcare facilities” OR “primary health care” OR “primary Care” OR “primary healthcare” OR “secondary care” OR “secondary cares” OR “tertiary healthcare” OR “tertiary care” OR “care center” OR “health services for transgender persons” OR “health services accessibility” OR “transgender care” OR “transinclusive care” OR “sexual health” OR hospital*) |
| LILACS | (“transgender persons” OR “transgender person” OR transgender OR transvestisme OR “sexual and gender minorities” OR transvestism OR “gender dysphoria” OR transfeminine OR “trans-Feminine” OR transmasculine OR “trans-Masculine” OR transexual* OR transsexual* OR “trans people” OR “trans person” OR “transgender individuals” OR trans OR “pessoas transgênero” OR “pessoa transgênero” OR transgênero OR travestismo OR “minorias sexuais e de gênero” OR “disforia de gênero” OR transfeminino OR “trans-Feminino” OR transmasculino OR “trans-Masculino” OR transexual* OR “pessoas trans” OR “pessoa trans” OR “indivíduos trans” OR “personas transgénero” OR “persona transgénero” OR transgénero OR travestismo OR “minorías sexuales y de género” OR “disforia de género” OR transfemenino OR “persona trans” OR “individuos transgénero”) AND (violence OR “gender violence” OR “gender-based violence” OR “interpersonal violence” OR “interpersonal violences” OR “physical attack” OR violência OR “violência de gênero” OR “violência interpessoal” OR “violências interpessoais” OR “ataque físico” OR violencia OR “violencia de género” OR “violencia interpersonal” OR “violencias interpersonales”) AND (“health services” OR “health care services” OR “healthcare services” OR “health facilities” OR “health care facilities” OR “healthcare facilities” OR “primary health care” OR “primary Care” OR “primary healthcare” OR “secondary care” OR “secondary cares” OR “tertiary healthcare” OR “tertiary care” OR “care center” OR “health services for transgender persons” OR “health services accessibility” OR “transgender care” OR “transinclusive care” OR “sexual health” OR hospital* OR “serviços de saúde” OR “estabelecimentos de saúde” OR “cuidados de saúde primários” OR “cuidados secundários”or “cuidados de saúde terciários” OR “cuidados terciários” OR “centro de cuidados” OR “serviços de saúde para pessoas trans” OR “acessibilidade aos serviços de saúde” OR “atendimento a transgêneros” OR “atendimento transinclusivo” OR “atendimento sexual saúde” OR “servicios de salud” OR “servicios de atención médica” OR “centros de salud” OR “centros de atención médica” OR “atención primaria de salud” OR “atención primaria” OR “ atención secundaria” OR “atención médica terciaria” OR “atención terciaria” OR “centro de atención” OR “servicios de salud para personas transgénero” OR “accesibilidad a servicios de salud” OR “atención a personas transgénero” OR “atención transinclusiva” OR “atención sexual salud”) AND (db:(“LILACS”)) |
| ID | Author/Year of Publication/Journal/Country | Study Objective | Place of Study/Participants | Data Collection/Data Analysis | Main Findings |
|---|---|---|---|---|---|
| A1 [33] | Xavier et al./2013/International Journal of Transgenderism/USA | Identify the factors associated with greater risk of HIV infection and the principal social determinants of health status among transgender people in Virginia. | Virginia, USA/32 trans women and 15 trans men participated of the study | Seven focus groups and one individual interview were conducted/Initial descriptive coding was performed separately on the transcriptions line by line using NVivo 2.0 software | Victimization associated with social stigmatization played a dominant role in participants’ lives, manifested by discrimination; violence; and health care provider insensitivity, hostility, and ignorance of transgender health. Access to transgender-related medical services that would allow for participants to pass in their chosen genders was their highest medical priority. Faced with barriers to access, hormonal self-medication was common, and silicone injections were reported by both MtF and FtM participants. Due to economic vulnerability, sex work was reported as a source of income by both MtFs and FtMs. MtFs expressed concern over confidentiality of HIV testing and additional discrimination if testing positive. FtMs expressed difficulty accessing gynecological care due to their masculine gender identities and expressions. |
| A2 [34] | Kosenko et al./2013/Medical Care/USA | To explore the negative experiences of transgender individuals in health care settings. | USA/152 self-identified transgender adults from 40 different states and 2 foreign countries participated. | Data collected in 2010 as part of an IRB-approved needs assessment of transgender adults. Questionnaire completed online and through mailings to LGBTQ organizations/Data were collected and analyzed according to Morse and Field’s conventional qualitative content analytic approach. | Participants reported mistreatment in health care contexts due to gender identity or presentation. Problematic provider behaviors included gender insensitivity, displays of discomfort, denial of services, substandard care, verbal abuse, and forced care. |
| A3 [35] | Lyons et al./2015/Substance Abuse Treatment, Prevention and Policy/Canada | Qualitatively investigate the treatment experiences of transgender individuals using illicit drugs in a residential dependency setting in a Canadian environment. | Vancouver, Canada/34 transgender people participated. | In-depth semi-structured interviews were conducted/The interviews were transcribed verbatim and imported into Atlas.ti software (version 8.3.0.)/Theoretical thematic analysis and a participatory analysis approach were applied | Three themes emerged from the data characterizing individuals’ experiences in treatment settings: (1) stigma enacted through social rejection and violence, (2) felt transphobia and stigma, and (3) “trans-friendly” and inclusive treatment. Participants who reported feeling and experiencing stigma, including violence, prematurely left the treatment after experiencing isolation and conflicts. In contrast, participants who felt included and respected in the treatment settings reported positive treatment experiences. |
| A4 [36] | Souza et al./2015/Cadernos de Saúde Pública/Brazil | The article discusses the violence experienced by transvestites (in the family, school, police precincts, and health services), specifically seeking to understand how such violence relates to their experiences with health services and how the latter respond. | Rio Grande do Sul, Brazil/49 transvestites participated | The authors conducted an ethnographic research with transgender persons in Santa Maria, Rio Grande do Sul State, Brazil, in 2012, using participant observation, semi-structured interviews, and following their everyday lives/The observations and narratives that emerged from the field were transcribed, coded, thematically categorized, and compared with theoretical concepts from gender studies, violence studies, and the field of public health. | The various forms of violence experienced by transgender women throughout their lives directly interfere with their health conditions. Besides distancing them from their nuclear families and kinship relations, thereby removing material support and emotional connections, it also pushes them away from schools and health services, which, as we have seen, replicate violence, contributing to their suffering. The physical and symbolic violence and the resulting suffering were constants that participants had to deal with in their daily practices and routines. |
| A5 [37] | Lyons et al./2016/LGBT Health/Canada | Investigate the experiences of trans women and Two-Spirit people in accessing women-specific services in the Downtown Eastside of Vancouver. | Vancouver, Canada/32 trans women and two-spirit individuals participated. | In-depth semi-structured interviews were conducted/The interview data were analyzed using a participatory and inductive analysis approach. | Participants generally managed to access women-specific services in the neighborhood. However, there were reports of discrimination related to gender identity, discrimination based on gender expression (e.g., the requirement for a feminine gender expression), and lack of staff intervention in the harassment by other service users. |
| A6 [38] | Ritterbusch; Salazar; Correa/2018/Global Public Health/Colombia | Present the stigma-related barriers to healthcare experienced by trans women and their experiences of multi-level violence within the healthcare system. | Colombia/28 transgender women participated | Semi-structured interviews were conducted within a participatory action research framework/The interviews were coded using a grounded theory approach. | Trans women experience violence at various levels, from intimate bodily violence to the formulation of high-level public health policies. |
| A7 [39] | Samuels et al./2018/Annals of Emergency Medicine/USA | To understand the experiences of transgender adults with at least one emergency department visit in the past 5 years and identify barriers and suggestions for improving emergency care for this population. | Oregon, USA/32 transgender adults participated in 4 focus groups, with most participants being white, preferring male pronouns, and identifying as female to male, transgender, or male. | Focus group discussions facilitated by the study principal investigator and another research team member, lasting approximately 2 h and recorded digitally/Transcripts were professionally transcribed, identified, and analyzed using qualitative data management software (NVivo). | Experiences of harassment and assault were common among participants, with the majority experiencing verbal harassment, physical assault, and sexual assault. While most had a primary care provider and insurance, only a small percentage had insurance plans covering sex affirmation or reassignment health services. Nearly half reported avoiding the emergency department when in need of acute care. |
| A8 [40] | Monteiro; Brigeiro/2019/Cadernos de Saúde Pública/Brazil | Analyzing the access experience of trans/transvestite women to the healthcare service. | Baixada Fluminense, Rio de Janeiro, Brazil/9 trans/transvestite women participated. | Individual and semi-structured interviews were conducted with trans women/transvestites from lower-income backgrounds in Baixada Fluminense, Rio de Janeiro. | Comparing to past experiences of aggression, narratives from trans women/transvestites highlight social advancements. They report that professionals generally do not discriminate based on their condition, though there is resistance to using their preferred name. |
| A9 [41] | King et al./2019/Culture, Health & Sexuality/Uganda | Exploring HIV and gender-related contexts among transgender women. | Kampala, Uganda/45 trans/transvestite women participated | Computer-assisted self-interviews, in-person qualitative interviews, and HIV and CD4 blood tests were conducted. Recruitment occurred through snowball sampling/Quantitative interviews utilized Questionnaire Design Studio (QDS v2.5). Trained qualitative social scientists coded and analyzed transcripts using NVivo Version 11 for data management, employing content analysis. | Nearly all interviewees reported frequently engaging in sex work, primarily due to lack of employment. HIV-related themes included limited access to non-stigmatizing health services, inconsistent condom use, inaccurate perceptions of risk for themselves and their partners, alcohol use, receptive anal sex with men, multiple sexual partners, frequent self-stigma, and enacted violence. |
| A10 [42] | Goldenberg et al./2019/The Counseling Psychologist/USA | Understanding the mental health experiences and healthcare of participants, including factors related to gender misalignment and less affirmative treatment by providers. | USA/506 transgender undergraduate and graduate students participated in the study. | It is a mixed methods study involving an online questionnaire with both open-ended and closed-ended questions. Thematic analysis was employed in the qualitative phase. | The prominent characteristics of negative interactions included invalidation, avoidance, or excessive focus on participants’ non-binary identities. Non-binary students reported more gender misidentifications by therapists and healthcare professionals, and less trans-affirmative care from healthcare providers, compared to binary students. |
| A11 [43] | Dutta; Khan; Lorway/2019/Culture, Health & Sexuality/India | Describing the effects of overlapping forms of structural violence around education, livelihood, family life, and attempts to access social and healthcare services. | Karnataka, India/3 transgender people participated. | Ethnographic research was conducted using thematic interpretative analysis and inductive reasoning. | The findings indicate how social inequalities contribute to the development of transgender identities along the journey to becoming a “jogappa”. They emphasize the evolving needs of transgender individuals in India, which are rooted in moral narratives of religiosity, urging policymakers to take these diverse needs into account. |
| A12 [44] | Calderón-Jaramillo et al./2020/International Journal for Equality in Health/Colombia | Identifying the primary sexual and reproductive health needs of individuals living a trans life; generating new evidence to guide the adaptation of sexual and reproductive health services centered on the needs, identities, and circumstances of trans people. | Barranquilla, Bogota, Cali and Medellín, Colombia/13 transgender people participated. | Focus group discussions and in-depth interviews were conducted for a qualitative study from a constructivist perspective. NVivo software was utilized for data coding and analysis. | Among the main barriers encountered were healthcare costs, lack of insurance, stigma, discrimination, and abuse by healthcare professionals. Some of the most notable sexual and reproductive health needs included trans-specific services, such as sensitive assistance for the transition process, endocrinology consultations, and sexual affirmation surgeries. |
| A13 [45] | Silva et al./2020/Revista Brasileira de Enfermagem/Brazil | Analyzing the health vulnerability of young transgender women living with HIV/AIDS. | Recife, Pernambuco, Brazil/6 transgender women participated. | Semi-structured interviews were conducted for a qualitative, descriptive, and exploratory study grounded in the theoretical framework of Social Representation and vulnerability concept. Individual interviews were analyzed, recorded, and fully transcribed using IRaMuTeQ software (version 0.7) for Similarity Analysis. | Young transgender women living with HIV/AIDS experience health vulnerability associated with lack of knowledge and difficulties in practicing self-care. There were representations of social abjection and unpreparedness among primary healthcare teams in providing qualified assistance for effective and humane care. |
| A14 [46] | Lacombe-Duncan; Olawale/2020/Journal of Interpersonal Violence/Canada | Understanding the context, types, and consequences of violence experienced by transgender women living with HIV across their lives, from intersectional and social–ecological perspectives. | Canada/Eleven transgender women living with HIV participated in the study. | Semi-structured individual interviews were conducted. Structural analysis was used to identify key themes, patterns within themes across participants, and patterns across themes among participants. | The findings revealed that transgender women living with HIV experience specific contexts of violence shaped at the intersection of stigma based on gender identity, gender expression, HIV status, and other identities/experiences. Once living with HIV, transgender women were subjected to discursive violence from healthcare professionals. These multiple forms of violence have serious consequences for the social, mental, and physical well-being of transgender women living with HIV. |
| A15 [47] | Reisner et al./2021/PLoS ONE/Peru | The user aims to increase visibility, document, and understand the health needs and contexts shaping the health and well-being of transgender men in Lima, Peru, to inform responsive public health efforts. | Lima, Peru/46 transgender men participated | User conducted 4 focus groups and 10 individual interviews. Analysis was conducted using an immersion crystallization approach to identify themes. | Transgender men reported lack of awareness and information among medical providers, avoidance of healthcare due to discrimination and mistreatment, absence of public services for medical gender affirmation (hormones, surgeries), and unmet mental health needs. They described health as multidimensional and influenced by social, economic, and legal contexts, including family, school, employment, legal identity recognition, discrimination in public spaces, and peer support. Violence, stigma, and intersecting forms of oppression were described as limiting social and legal recognition of transgender identity, a central dimension of health. Peer support, often in online spaces, was described as important for resilience and well-being. |
| A16 [48] | Oliveira et al./2022/Revista Brasileira de Enfermagem/Brazil | Understanding the meanings of being a transgender woman or transvestite in the healthcare provided by professionals of the Unified Health System. | Minas Gerais, Brazil/10 transgender women or transvestites residents and users of the Unified Health System (Sistema Único de Saúde) participated. | Interviews were conducted/Heideggerian Phenomenology was used as the theoretical, methodological, and philosophical foundation | Transgender women and transvestites often conform to socially constructed and accepted feminine patterns, frequently seeking hormone therapy. They sometimes resort to self-medication when facing difficulties obtaining prescriptions. Acceptance and use of their chosen name by healthcare professionals promote their recognition. These individuals experience daily prejudice, not only from professionals but also from assumptions made by other service users. |
| A17 [49] | Santander-Morillas et al./2022/PLoS ONE/Spain | Describing the experiences of transgender individuals regarding the healthcare they received in primary and hospital services in Barcelona from 2017 to 2019. | Barcelona, Espanha/16 transgender people participated | Semi-structured interviews were conducted based on a descriptive phenomenological approach. Data were analyzed descriptively and thematically following the method proposed by Colaizzi, aided by Atlas.ti 8 software. | The experiences of transgender care were divided into three categories: overcoming obstacles, training consultations, and coping strategies. Participants identified negative experiences and challenges with the healthcare system due to the lack of competence among healthcare professionals. Discriminatory, authoritarian, and paternalistic behaviors continue to exist, hindering therapeutic relationships, care, and access to health services. |
| A18 [50] | Tun et al./2022/J Internacional AIDS Society/Nigeria | Evaluate how stigma influences HIV services for transgender individuals in Lagos, Nigeria. | Lagos, Nigeria/25 transgender women and 13 transgender men participated. | In-depth interviews and focus group discussions were conducted. Thematic content analysis was used to analyze the data, utilizing NVivo 12 software. | The disclosure of gender identity is challenging due to anticipated stigma experienced by transgender individuals and fear of legal repercussions. Fear of being reported to authorities was a major barrier to disclosing to providers in non-affiliated transgender-inclusive clinic facilities. Participants reported a lack of sensitivity among providers regarding gender identity, with instances of confusion between transgender men and lesbian women, and transgender women with gay men or men who have sex with men, the latter being more common. Transgender participants also expressed feeling disrespected when providers were not sensitive to their preferred pronouns. HIV services that are not transgender-inclusive and affirming can reinforce stigma. |
| A19 [51] | Ssekamatte et al./2022/International Journal for Equity in Health/Uganda | Exploring sources of gender-based violence support services and the challenges faced by transgender women in seeking help. | Kampala, Uganda/60 transgender women and 10 key informants participated. | Deep interviews and a focus group discussion guide were utilized. Recruitment was through snowball sampling. Data were transcribed verbatim and analyzed following a thematic structure informed by the socioecological model. | Lack of recognition of transgender identity; long distances to health facilities; discrimination by healthcare professionals and civil society organization staff; inadequate questioning of transgender identity by police and healthcare providers; and the lack of transgender-competent healthcare professionals and legal personnel hindered seeking help after exposure to gender-based violence. |
| A20 [52] | Sherman et al./2022/PLoS ONE/EUA | To explore the help-seeking process post-exposure to violence among Black transgender women and the association between polyvictimization, barriers to healthcare, and mental health outcomes. | Baltimore e Washington, United States of America/Nineteen transgender women participated in the qualitative stage of the study. | Semi-structured interviews were conducted. Analyses included thematic content analysis, bivariate analysis, joint display, and multivariate linear regression analysis examining mediation and moderation. | The study found that barriers to accessing and engaging in healthcare, polyvictimization, and mental health symptom severity were interconnected among Black transgender women. The research highlighted the importance of addressing these barriers to improve overall well-being in this population. |
| A21 [53] | Lobo et al./2023/Revista Brasileira de Enfermagem/Brazil | Analyzing the repercussions of transphobia on the health of transgender men and transmasculine individuals. | Bahia, Brazil/Thirty-eight individuals participated, including 35 transgender men and three transmasculine individuals. | In-depth interviews were conducted. The Collective Subject Discourse technique was employed, and interpretation was based on the theoretical concept of transphobia. | Transphobia has brought intra and interpersonal repercussions in the lives and health of transgender men and transmasculine individuals who access healthcare services. Experiences of violence in private spaces, strained family ties, discrimination in educational settings, limitations in professional opportunities/employment, barriers in self-care and access to healthcare services, development of strategies to protect transgender identity, and consequences of transphobia on psychosocial health were found. |
| A22 [54] | Jesus et al./2023/Interface (Botucatu)/Brazil | Understanding how transgender women have been treated in institutions of the Unified Health System (Sistema Único de Saúde). | Minas Gerais, Brazil/Four transgender women participated. | Focus group interviews were conducted, and thematic content analysis was performed. | The participants mentioned not having ties with Primary Care and seeking care at the outpatient clinic linked to the teaching hospital and emergency services. Instances of institutional violence, negligence, and prejudice permeate their experiences. |
| A23 [55] | Muyanga et al./2023/BMC Women’s Health/Uganda | Exploring how gender-based violence affects the uptake and utilization of HIV prevention, treatment, and care services among transgender women in the greater Kampala metropolitan area, Uganda. | Kampala, Uganda/60 transgender women participated. | Twenty in-depth interviews, six focus group discussions, and ten interviews with key informants were conducted. Data were analyzed using a thematic content analysis framework. Verbatim transcription of data was performed, and NVivo 12 was used for coding. | Physical and emotional violence at the community level has led to fear among transgender women traveling to healthcare facilities. Emotional violence experienced by transgender women in healthcare settings has resulted in limited use of pre-exposure prophylaxis and HIV testing services, denial of healthcare services, and delays in receiving appropriate care. Fear of emotional violence has also made it difficult for transgender women to approach healthcare professionals. Fear of physical violence, such as being assaulted while in healthcare settings, has caused transgender women to avoid healthcare facilities. |
| A24 [56] | Burchell et al./2023/Culture, Health & Sexuality/Canada | Understanding the barriers to healthcare among non-binary individuals living in a medium-sized urban/rural region of Canada. | Waterloo, Ontario, Canada/12 non-binary individuals participated. | Semi-structured interviews were conducted. The theoretical framework of this study was based on interpretative phenomenology. Transcribed interviews were thematically analyzed using NVivo. | Three overarching themes were developed: erasure, barriers to accessing healthcare, and assessing whether (or not) to seek care. Subthemes included institutional erasure, informational erasure, general health barriers, medical transition barriers to healthcare, anticipated discrimination, and safety assessment. |
| A25 [57] | Atuk/2024/Social Science & Medicine /Turkey | Examining the medical experiences of HIV-positive trans women who engage in sex work and the harmful violence they encounter at the hands of healthcare professionals. | Turkey/10 women participated | As part of a broader research initiative, this article integrates multiple data sources, including public archives, medical records, newspaper articles, official government reports, and 45 in-depth interviews with healthcare providers/When it came to the inclusion of the study, it focused on in-dept interviews carried out with trans woman/thematic analysis was applied using ethnographically informed interpretive frameworks. | Trans women are treated by healthcare professionals as if they were always infectious. Trans communities are slowly weakened by the denial of healthcare services. |
| ID | Is There Congruence between the Stated Philosophical Perspective and the Research Methodology? | Is There Congruence between the Research Methodology and the Research Question or Objectives? | Is There Congruence between the Research Methodology and the Methods Used to Collect the Data? | Is There Congruence between the Research Methodology and the Representation and Analysis of Data? | Is There Congruence between the Research Methodology and the Interpretation of Results? | Is There a Statement Locating the Researcher Culturally or Theoretically? | Is the Researcher’s Influence on Research and Vice Versa Addressed? | Are Participants and Their Voices Adequately Represented? | Is the Research Ethical According to Current Criteria or, Recent Studies, for Is There Evidence of Ethical Approval by an Appropriate Body? | Do the Conclusions Drawn in the Research Report Stem from Data Analysis or Interpretation? |
|---|---|---|---|---|---|---|---|---|---|---|
| A1 [33] | Y | Y | Y | Y | Y | Y | U | Y | Y | Y |
| A2 [34] | U | Y | Y | Y | Y | U | U | Y | Y | Y |
| A3 [35] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| A4 [36] | U | Y | Y | Y | Y | U | U | Y | Y | Y |
| A5 [37] | Y | Y | Y | Y | Y | N | U | Y | Y | Y |
| A6 [38] | Y | Y | Y | Y | Y | Y | U | Y | Y | Y |
| A7 [39] | Y | Y | Y | Y | Y | U | U | Y | Y | Y |
| A8 [40] | U | Y | Y | Y | Y | Y | U | Y | Y | Y |
| A9 [41] | U | Y | Y | Y | Y | Y | U | Y | Y | Y |
| A10 [42] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| A11 [43] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| A12 [44] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| A13 [45] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| A14 [46] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| A15 [47] | U | Y | Y | Y | Y | U | U | Y | Y | Y |
| A16 [48] | U | Y | Y | Y | Y | U | U | Y | Y | Y |
| A17 [49] | U | Y | Y | Y | Y | Y | U | Y | Y | Y |
| A18 [50] | Y | Y | Y | Y | Y | Y | U | Y | Y | Y |
| A19 [51] | Y | Y | Y | Y | Y | U | U | Y | Y | Y |
| A20 [52] | Y | Y | Y | Y | Y | Y | U | Y | Y | Y |
| A21 [53] | Y | Y | Y | Y | Y | Y | U | Y | Y | Y |
| A22 [54] | Y | Y | Y | Y | Y | U | U | Y | Y | Y |
| A23 [55] | U | Y | Y | Y | Y | U | U | Y | Y | Y |
| A24 [56] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| A25 [57] | U | Y | Y | Y | Y | Y | Y | Y | U | Y |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leal, G.d.C.; Júnior, J.N.d.B.S.; Ferreira, Q.R.; Ballestero, J.G.d.A.; Palha, P.F. Institutional Violence Perpetrated against Transgender Individuals in Health Services: A Systematic Review of Qualitative Studies. Int. J. Environ. Res. Public Health 2024, 21, 1106. https://doi.org/10.3390/ijerph21081106
Leal GdC, Júnior JNdBS, Ferreira QR, Ballestero JGdA, Palha PF. Institutional Violence Perpetrated against Transgender Individuals in Health Services: A Systematic Review of Qualitative Studies. International Journal of Environmental Research and Public Health. 2024; 21(8):1106. https://doi.org/10.3390/ijerph21081106
Chicago/Turabian StyleLeal, Gilberto da Cruz, José Nildo de Barros Silva Júnior, Quezia Rosa Ferreira, Jaqueline Garcia de Almeida Ballestero, and Pedro Fredemir Palha. 2024. "Institutional Violence Perpetrated against Transgender Individuals in Health Services: A Systematic Review of Qualitative Studies" International Journal of Environmental Research and Public Health 21, no. 8: 1106. https://doi.org/10.3390/ijerph21081106
APA StyleLeal, G. d. C., Júnior, J. N. d. B. S., Ferreira, Q. R., Ballestero, J. G. d. A., & Palha, P. F. (2024). Institutional Violence Perpetrated against Transgender Individuals in Health Services: A Systematic Review of Qualitative Studies. International Journal of Environmental Research and Public Health, 21(8), 1106. https://doi.org/10.3390/ijerph21081106






