Mixed Reality in Clinical Settings for Pediatric Patients and Their Families: A Literature Review
Abstract
1. Introduction
1.1. Importance of New Technologies in Health and Education
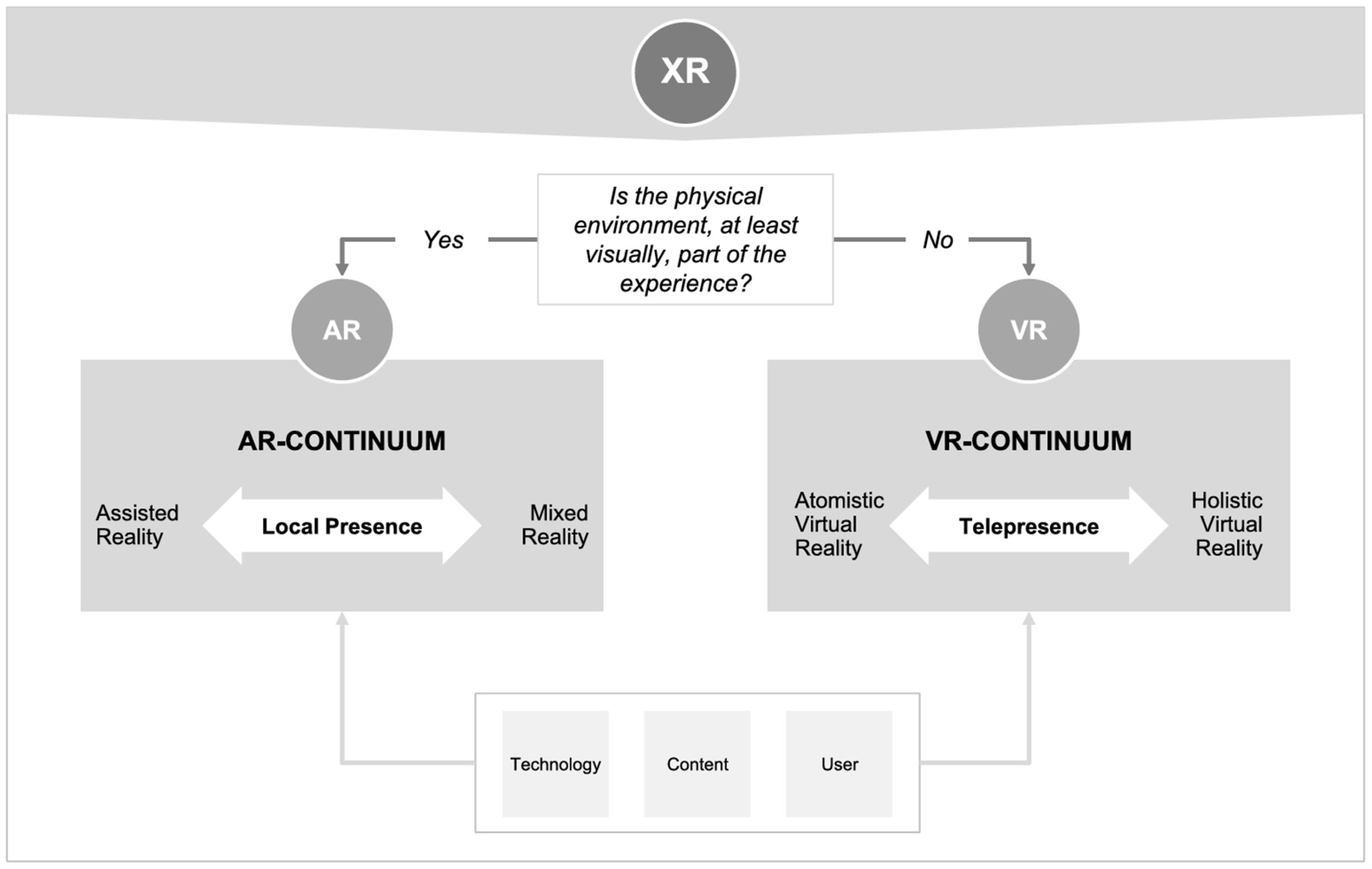
1.2. Definitions and Distinctions between AR, VR, and MR
1.3. Conceptual Challenges and Frameworks
1.4. Technological Advancements and Applications
1.5. The Role of AR and MR in Modern Healthcare and Education
1.6. Psychological and Physical Risks of AR and VR
1.7. Gaps in Research and the Need for Focused MR Interventions
2. Materials and Methods
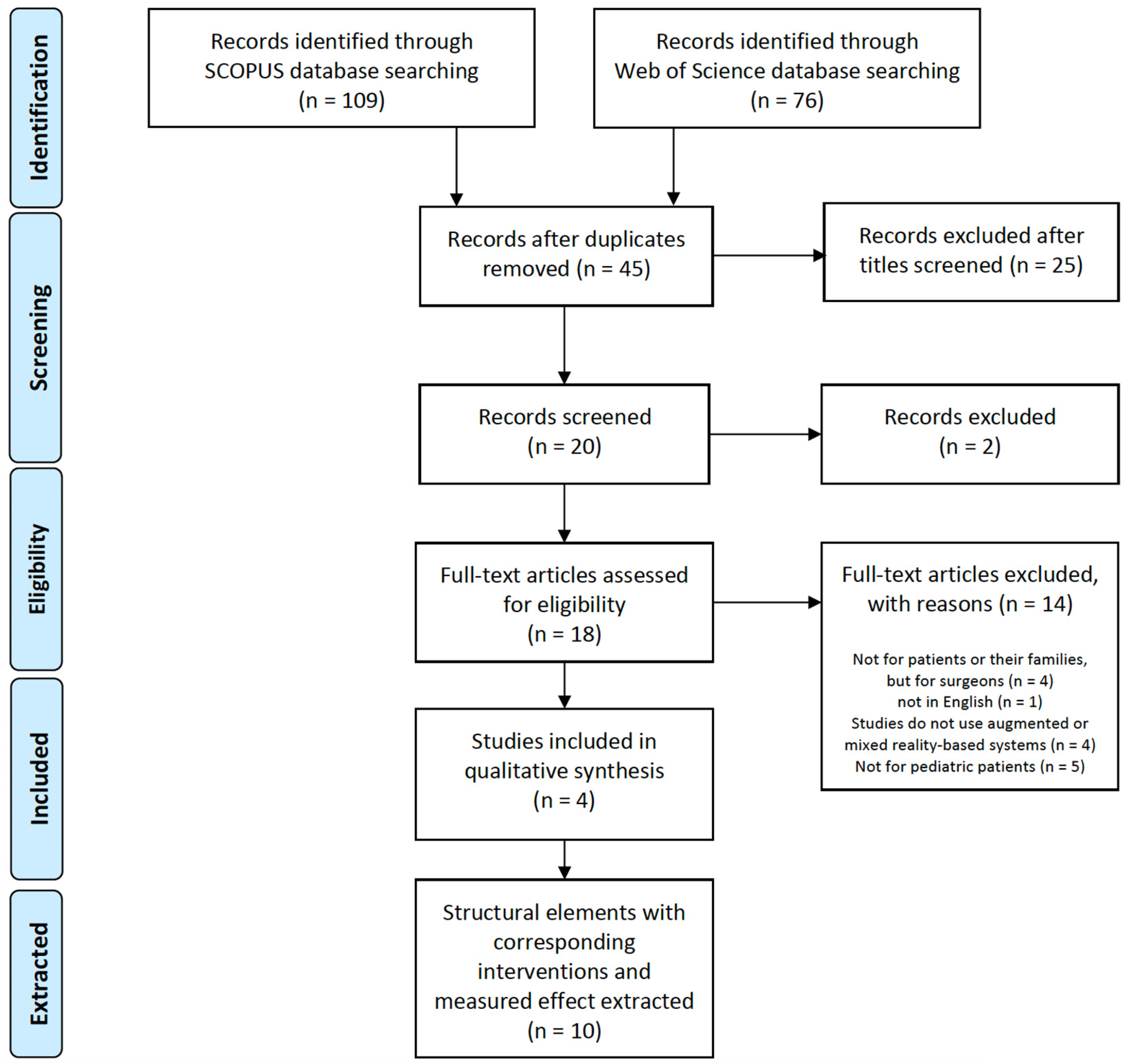
2.1. Identification
2.2. Screening and Eligibility
2.3. Included Articles
3. Results
3.1. Overview of Included Studies
3.1.1. Search Results
3.1.2. Study Characteristics
3.2. General Characteristics of the Studies
3.2.1. Methods
3.2.2. Study Population
3.3. Description of the Interventions
3.3.1. Clinical Settings of the MR Application
3.3.2. MR Devices and Software
3.3.3. MR-Based Interventions
- (1)
- Overview of MR-Based Interventions
- (2)
- MR Interventions in Hospital Settings
- Early Adoption in Pain Management: Mott et al. [43], in 2008, represented the early adoption of MR in pediatric care. A child could visualize a 3D animation character from multiple angles in an MR system with audio narration, which made the child perform tasks. This highlights MR’s application in pain management and its ability to improve patient experiences in medical settings.
- Developmental and Educational Tools: By 2015, Bai et al. [38] established a setting for patients playing with augmented toys in a mirror MR display to improve and learn how to pretend to play, a crucial skill for autistic children. This showed the application of AR as a tool for social and cognitive development in children with ASD, promoting interaction and engagement. Similarly, a study by Calle-Bustos et al. [36] revealed MR’s role in interactive education for chronic health conditions, such as diabetes mellitus. An Android device overlaying MR food on a real dish was used in an AR game to support therapeutic education for children with diabetes mellitus, significantly contributing to self-management education in pediatric diabetes.
- Anxiety Reduction and Advanced MR Applications: In 2020, studies by Tait et al. [34] and Bray et al. [35] exemplified the maturity of MR technologies. Tait et al. used a printed storybook and an MR-enabled iPad program overlaying MR graphics, animations, and a chatbot with embedded interactive quizzes for information evaluation. Bray et al. employed the preloaded iPad Xploro®, a digital therapeutic (DTx) platform that adopts AR, gameplay, and artificial intelligence, providing information on health environments, key health staff, and hospital equipment. Another study by Libaw et al. [37] in 2020 furthered the application of MR in clinical settings by applying the AR “Jenny the Robot” distraction technique during mask induction to encourage patients to take deep breaths.
- (3)
- MR Interventions in Non-Hospital Settings
- Social and Communication Skills Enhancement: Extracted from the primary study of Karami et al. [32], five individual studies on ASD conducted between 2015 and 2018 applied MR interventions for various social and communication skill-enhancing purposes. In a study by Chen et al. [39], AR-based Video-Modeling with Storybook (ARVMS)—comprising seven sessions—was devised to learn the facial expressions and emotions of others in social situations.
- Integration with Therapeutic Methods: Other studies targeting children with ASD, such as those by Kurniawan [40] and Nubia et al. [41], showed a continued trend toward using MR for enhancing communication and social skills. Kurniawan developed the Picture Exchange Communication System with AR-based multimedia using visual aids in a more interactive format to improve the communication abilities of children with ASD. In contrast, Nubia et al. introduced the process and simulation of an MR-based pictogram recognition task to improve the attention process and the appearance of verbal language in participants with ASD.
- Innovative Smart Glasses Applications: Vahabzadeh et al. [42] illustrated the innovative use of smart glasses-based interventions. Specifically, they reported that Empowered Brain, a smart glasses-based social communication and behavioral intervention, was used to improve the duration of gaze at faces and reduce ADHD symptoms in children, adolescents, and young adults with ASD.
3.4. Outcomes
3.4.1. Variables
3.4.2. Main Effect
4. Discussion
4.1. Study Design and Methodological Considerations
4.2. Intervention Characteristics and Technological Implementation
4.3. Population Characteristics and Clinical Settings
4.4. Functional Outcomes and Practical Implications
4.5. Intervention Settings, Technological Implementation, and Functional Outcomes
4.6. Interrelationships between Functional Outcomes
4.7. Family Involvement, Care Continuity, and Future Research Directions
4.8. Limitations and Future Research Directions
5. Conclusions
Funding
Conflicts of Interest
References
- Barteit, S.; Lanfermann, L.; Bärnighausen, T.; Neuhann, F.; Beiersmann, C. Augmented, Mixed, and Virtual Reality-Based Head-Mounted Devices for Medical Education: Systematic Review. JMIR Serious Games 2021, 9, e29080. [Google Scholar] [CrossRef]
- Nesenbergs, K.; Abolins, V.; Ormanis, J.; Mednis, A. Use of Augmented and Virtual Reality in Remote Higher Education: A Systematic Umbrella Review. Educ. Sci. 2021, 11, 8. [Google Scholar] [CrossRef]
- Kaplan, A.D.; Cruit, J.; Endsley, M.; Beers, S.M.; Sawyer, B.D.; Hancock, P.A. The Effects of Virtual Reality, Augmented Reality, and Mixed Reality as Training Enhancement Methods: A Meta-Analysis. Hum. Factors 2021, 63, 706–726. [Google Scholar] [CrossRef]
- Sala, N. Virtual Reality, Augmented Reality, and Mixed Reality in Education: A Brief Overview. In Current and Prospective Applications of Virtual Reality in Higher Education; Choi, D., Dailey-Hebert, A., Estes, J., Eds.; IGI Global: Hershey, PA, USA, 2021; pp. 48–73. [Google Scholar] [CrossRef]
- Gaol, F.L.; Prasolova-Førland, E. Special Section Editorial: The Frontiers of Augmented and Mixed Reality in All Levels of Education. Educ. Inf. Technol. 2022, 27, 611–623. [Google Scholar] [CrossRef] [PubMed]
- Rokhsaritalemi, S.; Sadeghi-Niaraki, A.; Choi, S.M. A Review on Mixed Reality: Current Trends, Challenges and Prospects. Appl. Sci. 2020, 10, 636. [Google Scholar] [CrossRef]
- Rauschnabel, P.A.; Felix, R.; Hinsch, C.; Shahab, H.; Alt, F. What Is XR? Towards a Framework for Augmented and Virtual Reality. Comput. Hum. Behav. 2022, 133, 107289. [Google Scholar] [CrossRef]
- Xi, N.; Chen, J.; Gama, F.; Riar, M.; Hamari, J. The Challenges of Entering the Metaverse: An Experiment on the Effect of Extended Reality on Workload. Inf. Syst. Front. 2023, 25, 659–680. [Google Scholar] [CrossRef]
- Speicher, M.; Hall, B.D.; Nebeling, M. What Is Mixed Reality? In Proceedings of the CHI Conference on Human Factors in Computing Systems, Glasgow, UK, 4–9 May 2019; ACM: New York, NY, USA, 2019; pp. 1–15. [Google Scholar] [CrossRef]
- Solbiati, L.; Gennaro, N.; Muglia, R. Augmented Reality: From Video Games to Medical Clinical Practice. Cardiovasc. Interv. Radiol. 2020, 43, 1427–1429. [Google Scholar] [CrossRef] [PubMed]
- Gupta, R.; He, J.; Ranjan, R.; Gan, W.-S.; Klein, F.; Schneiderwind, C.; Neidhardt, A.; Brandenburg, K.; Valimaki, V. Augmented/Mixed Reality Audio for Hearables: Sensing, Control, and Rendering. IEEE Signal Process. Mag. 2022, 39, 63–89. [Google Scholar] [CrossRef]
- Nasr, R.S.; El-Deeb, S. Exploring Mixed Reality: Enhancing Consumer Interaction. In Advances in Marketing, Customer Relationship Management, and E-Services; Pires, P.B., Santos, J.D., Pereira, I.V., Torres, A.I., Eds.; IGI Global: Hershey, PA, USA, 2023; pp. 234–251. [Google Scholar] [CrossRef]
- Tene, T.; Vique López, D.F.; Valverde Aguirre, P.E.; Orna Puente, L.M.; Vacacela Gomez, C. Virtual Reality and Augmented Reality in Medical Education: An Umbrella Review. Front. Digit. Health 2024, 6, 1365345. [Google Scholar] [CrossRef]
- Xu, X.; Mangina, E.; Campbell, A.G. HMD-Based Virtual and Augmented Reality in Medical Education: A Systematic Review. Front. Virtual Real. 2021, 2, 69210. [Google Scholar] [CrossRef]
- Wu, Y.; Hu, K.; Chen, D.Z.; Wu, J. AI-Enhanced Virtual Reality in Medicine: A Comprehensive Survey. In Proceedings of the International Joint Conference on Artificial Intelligence, Jeju, Republic of Korea, 3–9 August 2024; p. 920. [Google Scholar] [CrossRef]
- Mergen, M.; Graf, N.; Meyerheim, M. Reviewing the Current State of Virtual Reality Integration in Medical Education—A Scoping Review. BMC Med. Educ. 2024, 24, 788. [Google Scholar] [CrossRef] [PubMed]
- Ro, J.; Hong, C.W. Technology Trends of Virtual Augmented Reality and Application to Military Education and Training. Inst. Inf. Technol. 2022, 20, 151–164. [Google Scholar] [CrossRef]
- Syahry, A.; Basuki, D.K.; Sukaridhoto, S.; Budiarti, R.P.N.; Hanifati, K.; Muntahir, I. Implementation of Augmented Reality in Medical Education. In Proceedings of the 2022 International Electronics Symposium (IES), Surabaya, Indonesia, 9–11 August 2022; IEEE: Piscataway, NJ, USA, 2022; pp. 684–690. [Google Scholar] [CrossRef]
- Kim, M.; Choi, S.H.; Park, K.B.; Lee, J.Y. User Interactions for Augmented Reality Smart Glasses: A Comparative Evaluation of Visual Contexts and Interaction Gestures. Appl. Sci. 2019, 9, 3171. [Google Scholar] [CrossRef]
- Chengoden, R.; Victor, N.; Huynh-The, T.; Yenduri, G.; Jhaveri, R.H.; Alazab, M.; Bhattacharya, S.; Hegde, P.; Maddikunta, P.K.R.; Gadekallu, T.R. Metaverse for Healthcare: A Survey on Potential Applications, Challenges, and Future Directions. IEEE Access 2023, 11, 12765–12795. [Google Scholar] [CrossRef]
- Moro, C.; Phelps, C.; Redmond, P.; Stromberga, Z. HoloLens and Mobile Augmented Reality in Medical and Health Science Education: A Randomised Controlled Trial. Br. J. Educ. Technol. 2021, 52, 680–694. [Google Scholar] [CrossRef]
- Han, S.; Lim, C. Research Trends on Augmented Reality Education in Korea from 2008 to 2019. J. Educ. Technol. 2020, 36, 505–528. [Google Scholar] [CrossRef]
- Nam, S.H.; Lee, J.M. Augmented Reality in Education: A Meta-Analysis. J. Educ. Media 2020, 26, 129–156. [Google Scholar] [CrossRef]
- Yoo, M.; Kim, J.; Koo, Y.; Song, J.H. A Meta-Analysis on Effects of VR, AR, MR-Based Learning in Korea. J. Educ. Media 2018, 24, 459–488. [Google Scholar] [CrossRef]
- Dhar, P.; Rocks, T.; Samarasinghe, R.M.; Stephenson, G.; Smith, C. Augmented Reality in Medical Education: Students’ Experiences and Learning Outcomes. Med. Educ. Online 2021, 26, 1953953. [Google Scholar] [CrossRef]
- O’Shiel, D. Disappearing Boundaries? Reality, Virtuality, and the Possibility of “Pure” Mixed Reality (MR). Indo-Pac. J. Phenomenol. 2020, 20, e1887570. [Google Scholar] [CrossRef]
- Kim, S.; Ryu, J.; Choi, Y.; Kang, Y.; Li, H.; Kim, K. Eye-Contact Game Using Mixed Reality for the Treatment of Children with Attention Deficit Hyperactivity Disorder. IEEE Access 2020, 8, 45996–46006. [Google Scholar] [CrossRef]
- Aromataris, E.; Fernandez, R.; Godfrey, C.M.; Holly, C.; Khalil, H.; Tungpunkom, P. Summarizing Systematic Reviews: Methodological Development, Conduct, and Reporting of an Umbrella Review Approach. Int. J. Evid. Based Healthc. 2015, 13, 132–340. [Google Scholar] [CrossRef]
- Page, M.J.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. PRISMA 2020 Explanation and Elaboration: Updated Guidance and Exemplars for Reporting Systematic Reviews. BMJ 2021, 372, n160. [Google Scholar] [CrossRef]
- Urlings, J.; Sezer, S.; Ter Laan, M.; Bartels, R.; Maal, T.; Boogaarts, J.; Henssen, D. The Role and Effectiveness of Augmented Reality in Patient Education: A Systematic Review of the Literature. Patient Educ. Couns. 2022, 105, 1917–1927. [Google Scholar] [CrossRef] [PubMed]
- Alqudimat, M.; Mesaroli, G.; Lalloo, C.; Stinson, J.; Matava, C. State of the Art: Immersive Technologies for Perioperative Anxiety, Acute, and Chronic Pain Management in Pediatric Patients. Curr. Anesthesiol. Rep. 2021, 11, 265–274. [Google Scholar] [CrossRef] [PubMed]
- Karami, B.; Koushki, R.; Arabgol, F.; Rahmani, M.; Vahabie, A.H. Effectiveness of Virtual/Augmented Reality–Based Therapeutic Interventions on Individuals with Autism Spectrum Disorder: A Comprehensive Meta-Analysis. Front. Psychiatry 2021, 12, 665326. [Google Scholar] [CrossRef]
- Gasteratos, K.; Papakonstantinou, M.; Man, A.; Babatsikos, E.; Tamalonis, A.; Goverman, J. Adjunctive Nonpharmacologic Interventions for the Management of Burn Pain: A Systematic Review. Plast. Reconstr. Surg. 2022, 149, 985e–994e. [Google Scholar] [CrossRef] [PubMed]
- Tait, A.R.; Connally, L.; Doshi, A.; Johnson, A.; Skrzpek, A.; Grimes, M.; Becher, A.; Choi, J.E.; Weber, M. Development and Evaluation of an Augmented Reality Education Program for Pediatric Research. J. Clin. Transl. Res. 2020, 5, 96–101. [Google Scholar]
- Bray, L.; Sharpe, A.; Gichuru, P.; Fortune, P.M.; Blake, L.; Appleton, V. The Acceptability and Impact of the Xploro Digital Therapeutic Platform to Inform and Prepare Children for Planned Procedures in a Hospital: Before and After Evaluation Study. J. Med. Internet Res. 2020, 22, e17367. [Google Scholar] [CrossRef]
- Calle-Bustos, A.M.; Juan, M.C.; García-García, I.; Abad, F. An Augmented Reality Game to Support Therapeutic Education for Children with Diabetes. PLoS ONE 2017, 12, e0184645. [Google Scholar] [CrossRef] [PubMed]
- Libaw, J.S.; Sinskey, J.L. Use of Augmented Reality During Inhaled Induction of General Anesthesia in 3 Pediatric Patients: A Case Report. A A Pract. 2020, 14, e01219. [Google Scholar] [CrossRef]
- Bai, Z.; Blackwell, A.F.; Coulouris, G. Using Augmented Reality to Elicit Pretend Play for Children with Autism. IEEE Trans. Vis. Comput. Graph. 2015, 21, 598–610. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.-H.; Lee, I.-J.; Lin, L.-Y. Augmented Reality-Based Video-Modeling Storybook of Non-Verbal Facial Cues for Children with Autism Spectrum Disorder to Improve Their Perceptions and Judgments of Facial Expressions and Emotions. Comput. Hum. Behav. 2016, 55, 477–485. [Google Scholar] [CrossRef]
- Taryadi; Kurniawan, I. The Improvement of Autism Spectrum Disorders on Children Communication Ability with PECS Method Multimedia Augmented Reality-Based. J. Phys. Conf. Ser. 2018, 2018, 12009. [Google Scholar] [CrossRef]
- Nubia, R.M.; Fabián, G.R.; Wilson, R.A.; Wilmer, P.B. Development of a Mobile Application in Augmented Reality to Improve the Communication Field of Autistic Children at a Neurorehabilitar Clinic. In Proceedings of the 2015 Workshop on Engineering Applications—International Congress on Engineering (WEA), Bogota, Colombia, 1–4 July 2015; pp. 1–6. [Google Scholar] [CrossRef]
- Vahabzadeh, A.; Keshav, N.U.; Salisbury, J.P.; Sahin, N.T. Improvement of Attention-Deficit/Hyperactivity Disorder Symptoms in School-Aged Children, Adolescents, and Young Adults with Autism via a Digital Smartglasses-Based Socioemotional Coaching Aid: Short-Term, Uncontrolled Pilot Study. JMIR Ment. Health 2018, 5, e25. [Google Scholar] [CrossRef]
- Mott, J.; Bucolo, S.; Cuttle, L.; Mill, J.; Hilder, M.; Miller, K.; Kimble, R.M. The Efficacy of an Augmented Virtual Reality System to Alleviate Pain in Children Undergoing Burns Dressing Changes: A Randomised Controlled Trial. Burns 2008, 34, 803–808. [Google Scholar] [CrossRef]
- Cao, J.; Lam, K.Y.; Lee, L.H.; Liu, X.; Hui, P.; Su, X. Mobile Augmented Reality: User Interfaces, Frameworks, and Intelligence. ACM Comput. Surv. 2023, 55, 1–36. [Google Scholar] [CrossRef]
- Dargan, S.; Bansal, S.; Kumar, M.; Mittal, A.; Kumar, K. Augmented Reality: A Comprehensive Review. Arch. Comput. Methods Eng. 2023, 30, 1057–1080. [Google Scholar] [CrossRef]
- Wu, B.; Yu, X.; Gu, X. Effectiveness of Immersive Virtual Reality Using Head-Mounted Displays on Learning Performance: A Meta-Analysis. Br. J. Educ. Technol. 2020, 51, 1991–2005. [Google Scholar] [CrossRef]
- Xing, Y.; Liang, Z.; Fahy, C.; Shell, J.; Guan, K.; Liu, Y.; Zhang, Q. Virtual Reality Research: Design Virtual Education System for Epidemic (COVID-19) Knowledge to Public. Appl. Sci. 2021, 11, 10586. [Google Scholar] [CrossRef]
- Lovreglio, R.; Duan, X.; Rahouti, A.; Phipps, R.; Nilsson, D. Comparing the Effectiveness of Fire Extinguisher Virtual Reality and Video Training. Virtual Real. 2020, 25, 133–145. [Google Scholar] [CrossRef]
- Schmidli, H.; Häring, D.A.; Thomas, M.; Cassidy, A.; Weber, S.; Bretz, F. Beyond Randomized Clinical Trials: Use of External Controls. Clin. Pharmacol. Therap. 2020, 107, 806–816. [Google Scholar] [CrossRef] [PubMed]
- Levin, J.R.; Ferron, J.M.; Gafurov, B.S. Investigation of Single-Case Multiple-Baseline Randomization Tests of Trend and Variability. Educ. Psychol. Rev. 2021, 33, 713–737. [Google Scholar] [CrossRef]
- Beling, C.; Skinner, B.; Bluff, A. Xploro: Multi-User AR. In Proceedings of the ACM SIGGRAPH 2019 Appy Hour, Los Angeles, CA, USA, 28 July–1 August 2019; ACM: New York, NY, USA, 2019; pp. 1–2. [Google Scholar] [CrossRef]
- Sahin, N.T.; Keshav, N.U.; Salisbury, J.P.; Vahabzadeh, A. Safety and Lack of Negative Effects of Wearable Augmented-Reality Social Communication Aid for Children and Adults with Autism. J. Clin. Med. 2018, 7, 188. [Google Scholar] [CrossRef]
- Law, E.L.-C.; Heintz, M. Augmented Reality Applications for K-12 Education: A Systematic Review from the Usability and User Experience Perspective. Int. J. Child Comput. Interact. 2021, 30, 100321. [Google Scholar] [CrossRef]
- Ozdemir, M.; Sahin, C.; Arcagok, S.; Demir, M.K. The Effect of Augmented Reality Applications in the Learning Process: A Meta-Analysis Study. Eurasian J. Educ. Res. 2018, 18, 165–186. [Google Scholar] [CrossRef]
- Slater, M.; Gonzalez-Liencres, C.; Haggard, P.; Vinkers, C.; Gregory-Clarke, R.; Jelley, S.; Watson, Z.; Breen, G.; Schwarz, R.; Steptoe, W.; et al. The Ethics of Realism in Virtual and Augmented Reality. Front. Virtual Real. 2020, 1, 512449. [Google Scholar] [CrossRef]
- Csikszentmihalyi, M.; Csikszentmihalyi, M. Toward a Psychology of Optimal Experience. In Flow and the Foundations of Positive Psychology: The Collected Works of Mihaly Csikszentmihalyi; Csikszentmihalyi, M., Ed.; Springer: Dordrecht, The Netherlands, 2014; pp. 209–226. [Google Scholar] [CrossRef]
- Novak, T.P.; Hoffman, D.L.; Yung, Y.-F. Measuring the Customer Experience in Online Environments: A Structural Modeling Approach. Mark. Sci. 2000, 19, 22–42. [Google Scholar] [CrossRef]

| P | Patients/Families | Pediatric Patients and/or their Families in Hospitals, Medical Centers (Clinical Settings) |
| I | Intervention | Use of augmented reality and/or mixed reality technologies in clinical settings |
| C | Comparison | NA |
| O | Outcome | Impact on patient health and family-related outcomes |
| S | Study design | Systematic reviews |
| Database | Query | Results |
|---|---|---|
| Scopus | TITLE-ABS-KEY ((“Augmented reality” OR “Mixed reality”) AND (clinical OR medical OR hospital) AND (education OR program OR intervention OR trial) AND (patient OR family OR parent)) AND (LIMIT-TO (PUBYEAR, 2022) OR LIMIT-TO (PUBYEAR, 2021) OR LIMIT-TO (PUBYEAR, 2020) OR LIMIT-TO (PUBYEAR, 2019) OR LIMIT-TO (PUBYEAR, 2018) OR LIMIT-TO (PUBYEAR, >2012) AND (LIMIT-TO (DOCTYPE, “re”)) | 109 |
| Web of Science | (((TS = (“Augmented reality” OR “Mixed reality”)) AND TS = (clinical OR medical OR hospital)) AND TS = (education OR program OR intervention OR trial)) AND TS = (patient OR family OR parent) AND YEAR PUBLISHED: (>2012) AND DOCUMENT TYPE: Review Article | 76 |
| Author (Year) | Technologies Used for the Intervention | Main Users (Target Population) | No. of Papers per Review | Method of Analysis | Study Settings | Implications |
|---|---|---|---|---|---|---|
| Urlings et al. (2022) [30] | Augmented reality (AR) | Patients with chronic disease (e.g., prostate cancer, diabetes mellitus, multiple sclerosis, and epilepsy) | 10 | Qualitative meta- synthesis | Patient education | AR in patient education is limited; therefore, more high-quality studies are needed. |
| Alqudimat et al. (2021) [31] | Virtual (VR) and augmented reality (AR) | Pediatric patients (e.g., perioperative anxiety/acute/chronic pain) | 14 | Narrative synthesis | Perioperative settings (operating room and recovery area) | VR intervention is effective and safe. There is only one case report about AR for preoperative anxiety; therefore, more high-quality studies are needed. |
| Karami et al. (2021) [32] | Virtual (VR) and augmented reality (AR) | Patients with autism spectrum disorder | 33 | Quantitative synthesis | Clinical settings | The strongest effect was found for daily living skills. Five AR-based interventions showed efficacy. VR-based interventions in clinical settings are highly encouraged, while more high-quality trials are needed. |
| Gasteratos et al. (2022) [33] | Virtual (VR) and augmented reality (AR) | Burn survivors | 58 | Qualitative meta- synthesis | Outpatient department/clinical settings (e.g., burn care centers) | Six clinical trials based on VR or AR as nonpharmacologic interventions showed significant pain reduction during wound care and dressing procedures (e.g., rehabilitation, parental/provider satisfaction). |
| Country | Study Design | Population Characteristics | Sector (Primary Clinical Setting) | MR Device | Intervention | Variable | Significant Effect (Outcome Variables) | Primary Study | Reviewed Source |
|---|---|---|---|---|---|---|---|---|---|
| USA | Randomized Controlled Trial | Children (n = 91, mean age = 9.5, age range = 7–13 years) | Outpatient facilities | iPad | AR iPad program with a printed storybook (overlay of 3D graphics, Avatar “Remy” and sound) | (1) Patient knowledge (understanding of clinical research) (2) Perception of information delivery (easy to use) | (1) Increase (2-1) Easy to use in parents: 85.0% (2-2) Easy to use in children: 71.2% | [34] | [30] |
| UK | Mixed methods design | Children (n = 81, female n = 60, mean age = 10.4, age range = 8–14 years) | Outpatient and inpatient department | iPad | Xploro® (Corporation Pop, Manchester, UK) is a DTx platform including an avatar, chatbot, gameplay about health themes, information on a procedure, and coping strategies | (1) Perceived knowledge (2) Anxiety in children (3) Procedural involvement (4) Procedural satisfaction (5) Qualitative interviews about experiences | (1-1) Increased before the intervention (1-2) Significant group x time interaction in favor of the intervention group for the knowledge (2-1) Decreased before the procedure in children (2-2) Decreased before the procedure in parents (3) Increased (5) 80% more aware of how much they ate; 72.5% easy to use; enjoyed, fun, and easy to use; positive hospital experience | [35] | [31] |
| Spain | NA (there were pre- and post-tests) | Children with diabetes mellitus (n = 70, female n = 41, mean age = 9.2, age range = 5–14 years) | Children attended a conference for patients with diabetes and relatives in 2016 | Android device | AR games to support therapeutic education in diabetes (to learn the carbohydrate content of foods) | (1) Pre and post-knowledge (2) Satisfaction (3) Usability | (1) Significant (2) Very high (3) Very high | [36] | [30] |
| USA | Case report | Boys (n = 3, mean age = 8.7, age range = 8–10 years) | Operating room (during induction of general anesthesia) | Mira (Mira Labs, Inc., Los Angeles, CA, USA) AR headset and iPhone 7 | AR software was used as a distraction technique during induction by featuring Jenny the Robot to help patients take deep breaths | NA | Patients and parents described less preoperative anxiety than in previous inductions. | [37] | [31] |
| UK | Within-subject experiment | Children with autism spectrum disorder or Asperger’s syndrome (n = 12, female n = 2, mean age = 6.8, age range = 4–7 years) | NA | AR objects (three foam blocks and a cardboard box with markers attached), 24-inch monitor, a Logitech webcam Pro 9000, a mini-Bluetooth keyboard, a table, and play materials | Playing with AR toys in mirror AR display to improve and learn pretend to play and representation of pretense | Play observation scale by video analysis (1) Pretend play frequency (2) Pretend play duration (3) Constructive play frequency (4) Constructive play duration | (1) Increased (2) Increased | [38] | [32] |
| Taiwan | ABAB withdrawal design (withdrawal or reversal design) | Adolescents with autism spectrum disorder (n = 6, female n = 1, mean age = 11.5, age range = 11–13 years) | A 3 m by 6 m room inside a day-treatment room | Sony Vaio Duo Windows 8 tablet | ARVMS (Augmented Reality-based Video-Modeling with Storybook) with seven sessions to learn the facial expressions and emotions of others in social situations | (1) Correct facial expression recognition rate (2) Performance level improvement (assessed by instructor) | (1-1) Significantly improved in all children (1-2) Significant mean difference in performance level between the baseline and follow-up phases | [39] | [32] |
| Indonesia | Qualitative research (treatment–effect) | Children with autism (n = 12) | School in Pekalongan region | Android-based gadget | Picture Exchange Communication System) for communication training as a multimedia application built on AR technology | (1) Communication ability score (assessed by a teacher) | (1) Increased | [40] | [32] |
| Colombia | NA | Children with autism (n = 6, female n = 1, mean age = 6, age range = 5–9 years) | Neurorehabilitation clinic in Bogota | Android-based gadget | AR mobile application as a tool for semantical identification therapies | (1) Attention process (no. of children successfully finished the attention task) (2) Appearance of verbal language | (1) An increase of 14% (2) An increase of 9% | [41] | [32] |
| USA | NA | Children, adolescents, and young adults with autism spectrum disorder (n = 8, female n = 1, mean age = 15, age range = 11.7–20.5 years) - > high ADHD-related group (ABC-H ≥ 13) and low ADHD-related symptom group (ABC < 13) | NA | Google Glass | Empowered Brain, as a smart glasses-based social communication intervention (maintaining gaze toward faces by AR glasses to improve gaze duration to faces and reduce ADHD symptoms) | (1) ABC-H score (a measure of ADHD-related symptoms) | (1) Decrease in the high and low ADHD symptom groups | [42] | [32] |
| Australia | Prospective randomized controlled trial | Children with acute burns (n = 42, female n = 13, median age = 9, age range = 3–14) | Outpatient department (dressing changes) | AR device (with a 7-inch LCD screen (300 mm × 200 mm × 50 mm, weighing 1000 g, which was connected to an Intel Pentium Trademark 4 computer) | A child can visualize a 3D character called “Hospital Harry” from multiple angles | (1) Pain scores - Faces, Legs, Activity, Cry, and Consolability score for 3–4-years-old and non-verbalizing children - Faces Pain Scale-Revised for verbalizing 4–8-years-old children - Visual Analog Scale (VAS) for 8–14-years-old children (2) Pulse rates, respiratory rates, and oxygen saturation. | (1-1) Significantly lower mean pain scores in the AR group: for the long dressing time (>30 min), over time (1-2) Significantly lower parental VAS score in the AR group than in the control group | [43] | [33] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sin, J.E.; Kim, A.R. Mixed Reality in Clinical Settings for Pediatric Patients and Their Families: A Literature Review. Int. J. Environ. Res. Public Health 2024, 21, 1185. https://doi.org/10.3390/ijerph21091185
Sin JE, Kim AR. Mixed Reality in Clinical Settings for Pediatric Patients and Their Families: A Literature Review. International Journal of Environmental Research and Public Health. 2024; 21(9):1185. https://doi.org/10.3390/ijerph21091185
Chicago/Turabian StyleSin, Jae Eun, and Ah Rim Kim. 2024. "Mixed Reality in Clinical Settings for Pediatric Patients and Their Families: A Literature Review" International Journal of Environmental Research and Public Health 21, no. 9: 1185. https://doi.org/10.3390/ijerph21091185
APA StyleSin, J. E., & Kim, A. R. (2024). Mixed Reality in Clinical Settings for Pediatric Patients and Their Families: A Literature Review. International Journal of Environmental Research and Public Health, 21(9), 1185. https://doi.org/10.3390/ijerph21091185






