The Effect of Manual Therapy on Psychological Factors and Quality of Life in Lumbar Disc Herniation Patients: A Single Blinded Randomized Clinical Trial
Abstract
1. Background
2. Methods
2.1. Participants
2.2. Procedure
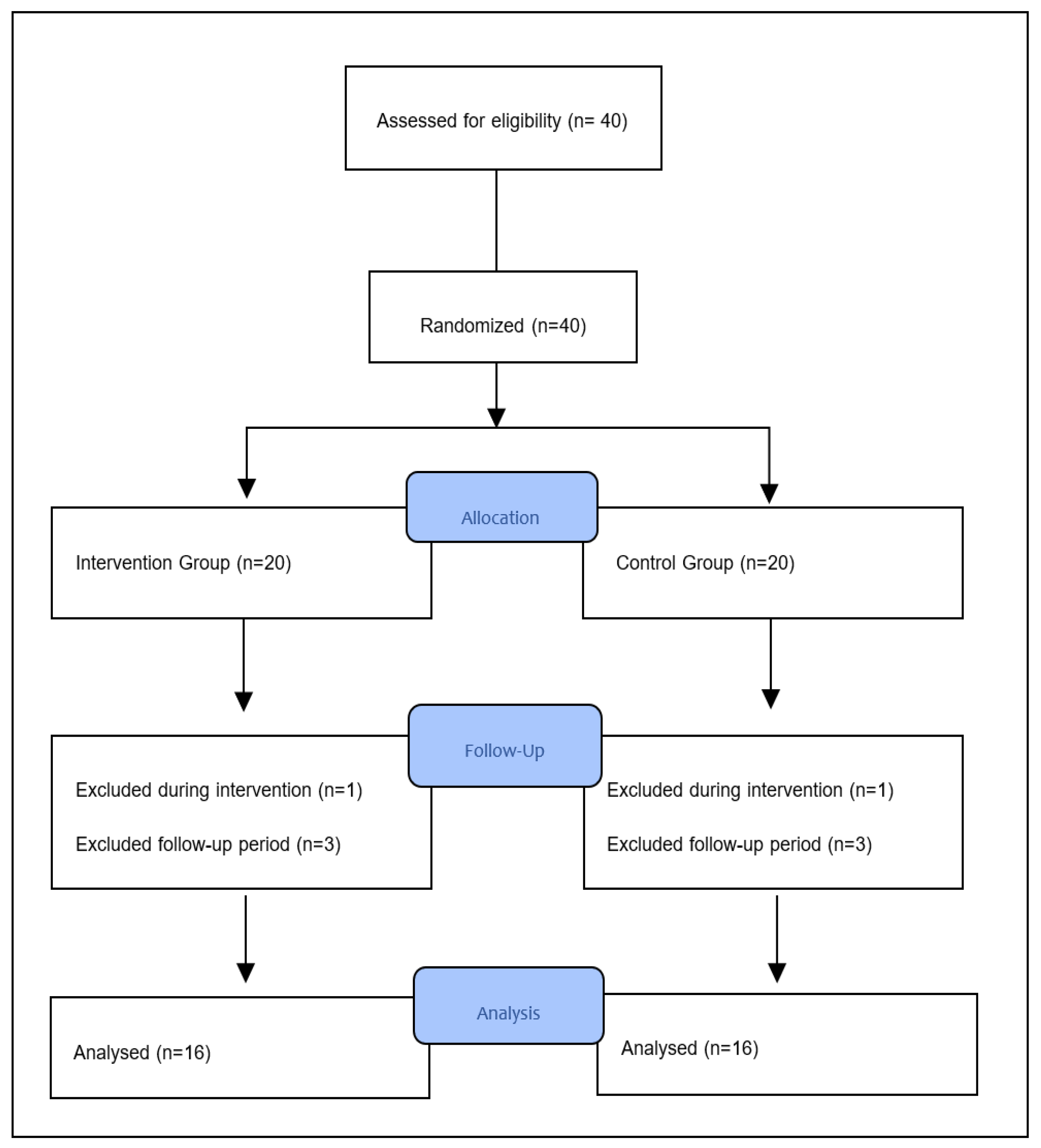
2.3. Randomization and Blinding
2.4. Measurements
2.5. Demographic Information
2.6. Pain Assessment
2.7. Psychological Factors Assessment
2.8. Assessment of the Quality of Life
2.9. Intervention
2.10. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| LDH | Lumbar Disc Herniation |
| MMPQ | McGill–Melzack Pain Questionnaire |
| HADS | Hospital Anxiety and Depression Scale |
| TKS | Tampa Kinesiophobia Scale |
| PCS | Pain Catastrophizing Scale |
| NSP | Nottingham Health Profile |
| MTG | Manual therapy group |
| EG | Exercise group |
References
- Xu, J.; Ding, X.; Wu, J.; Zhou, X.; Jin, K.; Yan, M.; Junming, M.; Xuequn, W.; Jie, Y.; Wen, M. A randomized controlled study for the treatment of middle-aged and old-aged lumbar disc herniation by Shis spine balance manipulation combined with bone and muscle guidance. Medicine 2020, 99, e23812. [Google Scholar] [CrossRef] [PubMed]
- Bletzer, J.; Gantz, S.; Voigt, T.; Neubauer, E.; Schiltenwolf, M. Chronic low back pain and psychological comorbidity: A review. Schmerz 2017, 31, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Dworkin, R.H.; Gitlin, M.J. Clinical aspects of depression in chronic pain patients. Clin. J. Pain 1991, 7, 79–94. [Google Scholar] [CrossRef] [PubMed]
- Kayhan, F.; Albayrak, G.İ.; Kayhan, A.; Kitiş, S.; Gölen, M. Mood and anxiety disorders in patients with chronic low back and neck pain caused by disc herniation. Int. J. Psychiatry Clin. Pract. 2016, 20, 19–23. [Google Scholar] [CrossRef] [PubMed]
- De Freitas, C.D.; Costa, D.A.; Junior, N.C.; Civile, V.T. Effects of the pilates method on kinesiophobia associated with chronic non-specific low back pain: Systematic review and meta-analysis. Bodyw. Mov. Ther. 2020, 24, 300–306. [Google Scholar] [CrossRef] [PubMed]
- Turk, D.C.; Fillingim, R.B.; Ohrbach, R.; Patel, K.V. Assessment of psychosocial and functional impact of chronic pain. J. Pain 2016, 17, T21–T49. [Google Scholar] [CrossRef]
- Polat, Ö.; Uçkun, A. Lomber disk hastalığında konservatif tedavi yöntemleri. Türk Nöroşirürji Derg. 2018, 28, 185–189. [Google Scholar]
- Kisner, C.; Colby, L.A.; Borstad, J. Therapeutic Exercise: Foundations and Techniques, 5th ed.; F.A. Davis Company: Philadelphia, PA, USA, 2007; pp. 109–147. ISBN 978-0-8036-1584-7. [Google Scholar]
- Kao, Y.C.; Chen, J.Y.; Chen, H.H.; Liao, K.W.; Huang, S.S. The association between depression and chronic lower back pain from disc degeneration and herniation of the lumbar spine. Int. J. Psychiatry 2022, 57, 165–177. [Google Scholar] [CrossRef]
- Mu, W.; Shang, Y.; Zhang, C.; Tang, S. Analysis of the depression and anxiety status and related risk factors in patients with lumbar disc herniation. Pak. J. Med. Sci. 2019, 35, 658. [Google Scholar] [CrossRef]
- Roiha, M.; Marjamaa, J.; Siironen, J.; Koskinen, S.; Koski-Palkén, A. Favorable long-term health-related quality of life after surgery for lumbar disc herniation in young adult patients. Acta Neurochir. 2023, 165, 797–805. [Google Scholar] [CrossRef]
- Cao, B.; Zhou, X.; Zhang, S.P.; Zhu, Q.G.; Kong, L.J.; Fang, M. Effect of traditional Chinese manual therapy on alleviating pain and dysfunction of lumbar disc herniation: A randomized controlled pilot study. Am. J. Transl. Res. 2022, 14, 6941. [Google Scholar] [PubMed]
- Danazumi, M.S.; Bello, B.; Yakasai, A.M.; Kaka, B. Two manual therapy techniques for management of lumbar radiculopathy: A randomized clinical trial. J. Osteopath. Med. 2021, 121, 391–400. [Google Scholar] [CrossRef] [PubMed]
- Yadav, S.; Nijhawan, M.A.; Panda, P. Effectiveness of spinal mobilization with leg movement (SMWLM) in patients with lumbar radiculopathy (L5/S1 nerve root) in lumbar disc herniation. Int. J. Physiother. Res. 2014, 2, 712–718. [Google Scholar]
- Danazumi, M.S.; Nuhu, J.M.; Ibrahim, S.U.; Falke, M.A.; Rufai, S.A.; Abdu, U.G.; Adamu, I.A.; Usman, M.H.; Frederic, A.D.; Yakasai, A.M.G. Effects of spinal manipulation or mobilization as an adjunct to neurodynamic mobilization for lumbar disc herniation with radiculopathy: A randomized clinical trial. J. Man. Manip. Ther. 2023, 31, 408–420. [Google Scholar] [CrossRef]
- Bello, B.; Danazumi, M.S.; Kaka, B. Comparative effectiveness of 2 manual therapy techniques in the management of lumbar radiculopathy: A randomized clinical trial. J. Chiropr. Med. 2019, 18, 253–260. [Google Scholar] [CrossRef]
- Gong, C.; Dai, S.; Jin, B.; Xie, Y. Comparison of Feng spinal mobilization with Maitland mobilization in management of chronic nonspecific low back pain: A cohort study. Medicine 2023, 102, e32984. [Google Scholar] [CrossRef]
- Kuguoglu, S.; Eti-Aslan, F.; Olgun, N. McGill Melzack Ağrı Soru Formu (MASF) nun Türkçe’ye uyarlanması [Turkish adaptation of the McGill Melzack Pain Questionnaire (MPQ)]. Agrı 2003, 15, 47–52. [Google Scholar]
- Julian, L.J. Measures of anxiety. Arthritis Care Res. 2011, 63, 11. [Google Scholar] [CrossRef] [PubMed]
- Aydemir, Ö.; Kirpinar, I.; Tülay, S.A.T.I.; Uykur, B.; Cengisiz, C. Reliability and Validity of the Turkish version of Hospital Anxiety and Depression Scale. Turk. J. Psychiatry 1997, 8, 280–287. [Google Scholar] [CrossRef]
- Weermeijer, J.D.; Meulders, A. Clinimetrics: Tampa scale for kinesiophobia. J. Physiother. 2018, 64, 126. [Google Scholar] [CrossRef]
- Yilmaz, Ö.T.; Yakut, Y.; Uygur, F.; Uluğ, N. Tampa Kinezyofobi Ölçeği’nin Türkçe versiyonu ve test-tekrar test güvenirliği. Fiz. Rehabil. 2011, 22, 44–49. [Google Scholar]
- Kapoor, S.; Thorn, B.E.; Bandy, O.; Clements, K.L. Pain referents used to respond to the Pain Catastrophizing Scale. Eur. J. Pain 2015, 19, 400–407. [Google Scholar] [CrossRef] [PubMed]
- Ugurlu, M.; Karakas, U.G.; Erten, S.; Caykoylu, A. Validity of Turkish form of Pain Catastrophizing Scale and modeling of the relationship between pain-related disability with pain intensity, cognitive, and emotional factors. Psychiatry Clin. Psychopharmacol. 2017, 27, 189–196. [Google Scholar] [CrossRef]
- Wiklund, I. The Nottingham Health Profile—A measure of health-related quality of life. Scand. J. Prim. 1990, 1, 15–18. [Google Scholar]
- Miyamoto, N.; Hirata, K.; Kimura, N.; Miyamoto-Mikami, E. Contributions of hamstring stiffness to straight-leg-raise and sit-and-reach test scores. Int. J. Sports Med. 2018, 39, 110–114. [Google Scholar] [CrossRef]
- Akuthota, V.; Nadler, S.F. Core strengthening. Arch. Phys. Med. Rehabil. 2004, 85, 86–92. [Google Scholar] [CrossRef]
- Powers, C.M.; Beneck, G.J.; Kulig, K.; Landel, R.F.; Fredericson, M. Effects of a single session of posterior-to-anterior spinal mobilization and press-up exercise on pain response and lumbar spine extension in people with nonspecific low back pain. Phys. Ther. 2008, 88, 485–493. [Google Scholar] [CrossRef]
- Tsung, B.Y.; Evans, J.; Tong, P.; Lee, R.Y. Measurement of lumbar spine loads and motions during rotational mobilization. J. Manip. Physiol. Ther. 2005, 28, 238–244. [Google Scholar] [CrossRef]
- Büyüköztürk, Ş. Sosyal Bilimler Için Veri Analizi el Kitabı [Data Analysis Handbook for Social Sciences], 28th ed.; Pegem Akademi Yayıncılık: Ankara, Türkiye, 2023; pp. 1–214. ISBN 9789756802748. [Google Scholar]
- Melzack, R.; Wall, P.D. Pain Mechanisms: A New Theory: A gate control system modulates sensory input from the skin before it evokes pain perception and response. Science 1965, 150, 971–979. [Google Scholar] [CrossRef]
- Rampazo, É.P.; Telles, J.D.; Schiavon, M.A.G.; Liebano, R.E. Hypoalgesic effects of specific vs non-specific cervical manipulation in healthy subjects: A randomized crossover trial. Bodyw. Mov. Ther. 2021, 28, 311–316. [Google Scholar] [CrossRef]
- Wright, A. Hypoalgesia post-manipulative therapy: A review of a potential neurophysiological mechanism. Man. Ther. 1995, 1, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Satpute, K.; Hall, T.; Bisen, R.; Lokhande, P. The effect of spinal mobilization with leg movement in patients with lumbar radiculopathy—A double-blind randomized controlled trial. Arch. Phys. Med. Rehabil. 2019, 100, 828–836. [Google Scholar] [CrossRef] [PubMed]
- Shum, G.L.; Tsung, B.Y.; Lee, R.Y. The immediate effect of posteroanterior mobilization on reducing back pain and the stiffness of the lumbar spine. Arch. Phys. Med. Rehabil. 2013, 94, 673–679. [Google Scholar] [CrossRef]
- Groeneweg, R.; Haanstra, T.; Bolman, C.A.; Oostendorp, R.A.; van Tulder, M.W.; Ostelo, R.W. Treatment success in neck pain: The added predictive value of psychosocial variables in addition to clinical variables. Scand. J. Pain 2017, 14, 44–52. [Google Scholar] [CrossRef]
- Ailliet, L.; Rubinstein, S.M.; Knol, D.; Van Tulder, M.W.; de Vet, H.C. Somatization is associated with worse outcome in a chiropractic patient population with neck pain and low back pain. Man. Ther. 2016, 21, 170–176. [Google Scholar] [CrossRef]
- Martí-Salvador, M.; Hidalgo-Moreno, L.; Doménech-Fernández, J.; Lisón, J.F.; Arguisuelas, M.D. Osteopathic manipulative treatment including specific diaphragm techniques improves pain and disability in chronic nonspecific low back pain: A randomized trial. Arch. Phys. Med. Rehabil. 2018, 99, 1720–1729. [Google Scholar] [CrossRef]
- De Oliveira Meirelles, F.; de Oliveira Muniz Cunha, J.C.; da Silva, E.B. Osteopathic manipulation treatment versus therapeutic exercises in patients with chronic nonspecific low back pain: A randomized, controlled and double-blind study. J. Back Musculoskelet. Rehabil. 2020, 33, 367–377. [Google Scholar] [CrossRef]
- Arguisuelas, M.D.; Lisón, J.F.; Sánchez-Zuriaga, D.; Martínez-Hurtado, I.; Doménech-Fernández, J. Effects of myofascial release in nonspecific chronic low back pain: A randomized clinical trial. Spine 2017, 42, 627–634. [Google Scholar] [CrossRef] [PubMed]
- Quartana, P.J.; Campbell, C.M.; Edwards, R.R. Pain catastrophizing: A critical review. Expert Rev. Neurother. 2009, 9, 745–758. [Google Scholar] [CrossRef]
- Sobhani, V.; Shamsoddini, A.; Khatibi-Aghda, A.; Mazloum, V.; Kia, H.H.; Meybodi, M.E. Effectiveness of Dry Needling, Manual Therapy, and Kinesio Taping (R) for Patients with Chronic Myofascial Neck Pain: A Single-Blind Clinical Trial. Trauma Mon. 2017, 22, 8. [Google Scholar] [CrossRef]
- Kamonseki, D.H.; Christenson, P.; Rezvanifar, S.C.; Calixtre, L.B. Effects of manual therapy on fear avoidance, kinesiophobia and pain catastrophizing in individuals with chronic musculoskeletal pain: Systematic review and meta-analysis. Musculoskelet. Sci. Pract. 2021, 51, 102311. [Google Scholar] [CrossRef] [PubMed]
- Kagaya, H.; Takahashi, H.; Sugawara, K.; Kuroda, T.; Takahama, M. Quality of life assessment before and after lumbar disc surgery. J. Orthop. Sci. 2005, 10, 486–489. [Google Scholar] [CrossRef] [PubMed]
- Levy, H.I.; Hanscom, B.; Boden, S.D. Three-question depression screener used for lumbar disc herniations and spinal stenosis. Spine 2002, 27, 1232–1236. [Google Scholar] [CrossRef] [PubMed]
- Danazumi, M.S.; Ibrahim, S.U.; Abubakar, M.F.; Yakasai, A.M.; Zakari, U.U. Effect of spinal manipulation compared with spinal mobilization for lumbar disc herniation with radiculopathy: Design of a randomized clinical trial with 1 year follow-up. Middle East J. Rehabil. Health Stud. 2019, 6, e92770. [Google Scholar] [CrossRef]
- Ulger, O.; Demirel, A.; Oz, M.; Tamer, S. The effect of manual therapy and exercise in patients with chronic low back pain: Double blind randomized controlled trial. J. Back Musculoskelet. Rehabil. 2017, 30, 1303–1309. [Google Scholar] [CrossRef]
- Bryans, R.; Decina, P.; Descarreaux, M.; Duranleau, M.; Marcoux, H.; Potter, B.; Ruegg, R.P.; Shaw, L.; Watkin, R.; White, E. Evidence-based guidelines for the chiropractic treatment of adults with neck pain. J. Manip. Physiol. Ther. 2014, 37, 42–63. [Google Scholar] [CrossRef]
- Reiman, M.P.; Harris, J.Y.; Cleland, J.A. Manual therapy interventions for patients with lumbar spinal stenosis: A systematic review. In Database of Abstracts of Reviews of Effects (DARE): Quality-Assessed Reviews [Internet]; University of York: York, UK, 2009; Available online: https://www.highbeam.com/doc/1G1-207945598.html (accessed on 24 March 2010).
- Bryans, R.; Decina, P.; Descarreaux, M.; Duranleau, M.; Marcoux, H.; Potter, B.; Ruegg, R.P.; Shaw, L.; Watkin, R.; White, E. Evidence-based guidelines for the chiropractic treatment of adults with headache. J. Manip. Physiol. Ther. 2011, 34, 274–289. [Google Scholar] [CrossRef]
- Hoeksma, H.L.; Dekker, J.; Ronday, H.K.; Heering, A.; Van Der Lubbe, N.; Vel, C.; Breedveld, F.C.; Van Den Ende, C.H. Comparison of manual therapy and exercise therapy in osteoarthritis of the hip: A randomized clinical trial. Arthritis Care Res. Off. J. Am. Coll. Rheumatol. 2004, 51, 722–729. [Google Scholar] [CrossRef]
| Continuous Variables | MTG (n = 16) (X ± SD) | EG (n = 16) (X ± SD) | t | p * |
|---|---|---|---|---|
| Age (years) | 39.81 ± 9.45 | 38.31 ± 9.21 | 0.455 | 0.653 |
| Weight (kg) | 89.62 ± 12.96 | 80.75 ± 11.55 | 2.044 | 0.050 |
| Height (cm) | 175.94 ± 9.45 | 170.50 ± 7.00 | 1.848 | 0.074 |
| BMI (kg/m2) | 28.96 ± 4.27 | 27.69 ± 2.82 | 0.989 | 0.330 |
| Variables | MTG (16) | EG (16) | Test Ve p-Value * |
|---|---|---|---|
| McGill–Melzack Pain | |||
| Questionnaire | 58.56 ± 11.17 | 40.62 ± 9.85 | t: 4.814 p: 0.000 |
| T1 | 28.62 ± 10.72 | 23.43 ± 11.51 | t: 1.318 p: 0.197 |
| T2 | 32 ± 15.69 | 21.31 ± 11.71 | t: 2.182 p: 0.037 |
| T3 | Mauchly’s W: 0.735 + | Mauchly’s W: 0.686+ | |
| Test and p-value | F: 45.816 p: 0.000 | F: 21.459 p: 0.000 | |
| Post hoc | T1 > T2,T3 | T1 > T2,T3 | |
| Effect size | 0.753 | 0.589 | |
| Hospital Anxiety and Depression | |||
| Scale | 12.93 ± 6.22 | 10.68 ± 6.74 | t: 0.981 p: 0.334 |
| T1 | 6.62 ± 5 | 9.43 ± 5.76 | t: −1.474 p: 0.151 |
| T2 | 9.06 ± 5.35 | 9.18 ± 6.03 | t: −0.062 p: 0.951 |
| T3 | Mauchly’s W: 0.523 ++ | Mauchly’s W: 0.967 + | |
| Test and p-value ** | F: 10.930 p: 0.000 | F: 1.966 p: 0.154 | |
| Post hoc | T1,T3 > T2 | - | |
| Effect size | 0.422 | 0.117 | |
| Tampa Kinesiophobia Scale | |||
| T1 | 40.62 ± 7.67 | 37.68 ± 7.21 | t: 1.115 p: 0.274 |
| T2 | 35.43 ± 6.41 | 31.81 ± 9.36 | t: 1.278 p: 0.211 |
| T3 | 35.93 ± 7.11 | 34.56 ± 6.02 | t: 0.590 p: 0.560 |
| Test and p-value ** | Mauchly’s W: 0.714 + | Mauchly’s W: 0.658 + | |
| F: 4.951 p: 0.014 | F: 2.510 p: 0.098 | ||
| Post hoc | T1 > T2,T3 | - | |
| Effect size | 0.248 | 0.143 | |
| Pain Catastrophizing Scale | |||
| T1 | 26.12 ± 10.84 | 14.43 ± 12.62 | t: 2.809 p: 0.009 |
| T2 | 12.93 ± 10.06 | 8.18 ± 9.68 | t: 1.360 p: 0.184 |
| T3 | 10.43 ± 8.45 | 8.18 ± 12.01 | t: 0.613 p: 0.545 |
| Test and p value | Mauchly’s W: 0.653 ++ | Mauchly’s W: 0.854 + | |
| F: 20.836 p: 0.000 | F: 5.444 p: 0.013 | ||
| Post hoc | T1 > T2,T3 | T1 > T2,T3 | |
| Effect size | 0.581 | 0.266 | |
| Nottingham Health Profile | |||
| T1 | 187.13 ± 116.55 | 143.27 ± 108.71 | t: 1.101 p: 0.280 |
| T2 | 67.79 ± 64.65 | 92.22 ± 83.66 | t: −0.924 p: 0.363 |
| T3 | 83.44 ± 89.41 | 65.13 ± 76.18 | t: 0.623 p: 0.538 |
| Test and p-value ** | Mauchly’s W: 0.605 ++ | Mauchly’s W: 0.778 + | |
| F: 10.096 p: 0.002 | F: 10.602 p: 0.000 | ||
| Post hoc | T1 > T2,T3 | T1 > T2,T3 | |
| Effect size | 0.402 | 0.414 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Taşkaya, B.; Taşkent, İ.; Çakıllı, M.; Yılmaz, Ö. The Effect of Manual Therapy on Psychological Factors and Quality of Life in Lumbar Disc Herniation Patients: A Single Blinded Randomized Clinical Trial. Int. J. Environ. Res. Public Health 2024, 21, 1234. https://doi.org/10.3390/ijerph21091234
Taşkaya B, Taşkent İ, Çakıllı M, Yılmaz Ö. The Effect of Manual Therapy on Psychological Factors and Quality of Life in Lumbar Disc Herniation Patients: A Single Blinded Randomized Clinical Trial. International Journal of Environmental Research and Public Health. 2024; 21(9):1234. https://doi.org/10.3390/ijerph21091234
Chicago/Turabian StyleTaşkaya, Burhan, İsmail Taşkent, Mahmut Çakıllı, and Öznur Yılmaz. 2024. "The Effect of Manual Therapy on Psychological Factors and Quality of Life in Lumbar Disc Herniation Patients: A Single Blinded Randomized Clinical Trial" International Journal of Environmental Research and Public Health 21, no. 9: 1234. https://doi.org/10.3390/ijerph21091234
APA StyleTaşkaya, B., Taşkent, İ., Çakıllı, M., & Yılmaz, Ö. (2024). The Effect of Manual Therapy on Psychological Factors and Quality of Life in Lumbar Disc Herniation Patients: A Single Blinded Randomized Clinical Trial. International Journal of Environmental Research and Public Health, 21(9), 1234. https://doi.org/10.3390/ijerph21091234






