Daily Temperatures and Child Hospital Admissions in Aotearoa New Zealand: Case Time Series Analysis
Abstract
1. Introduction
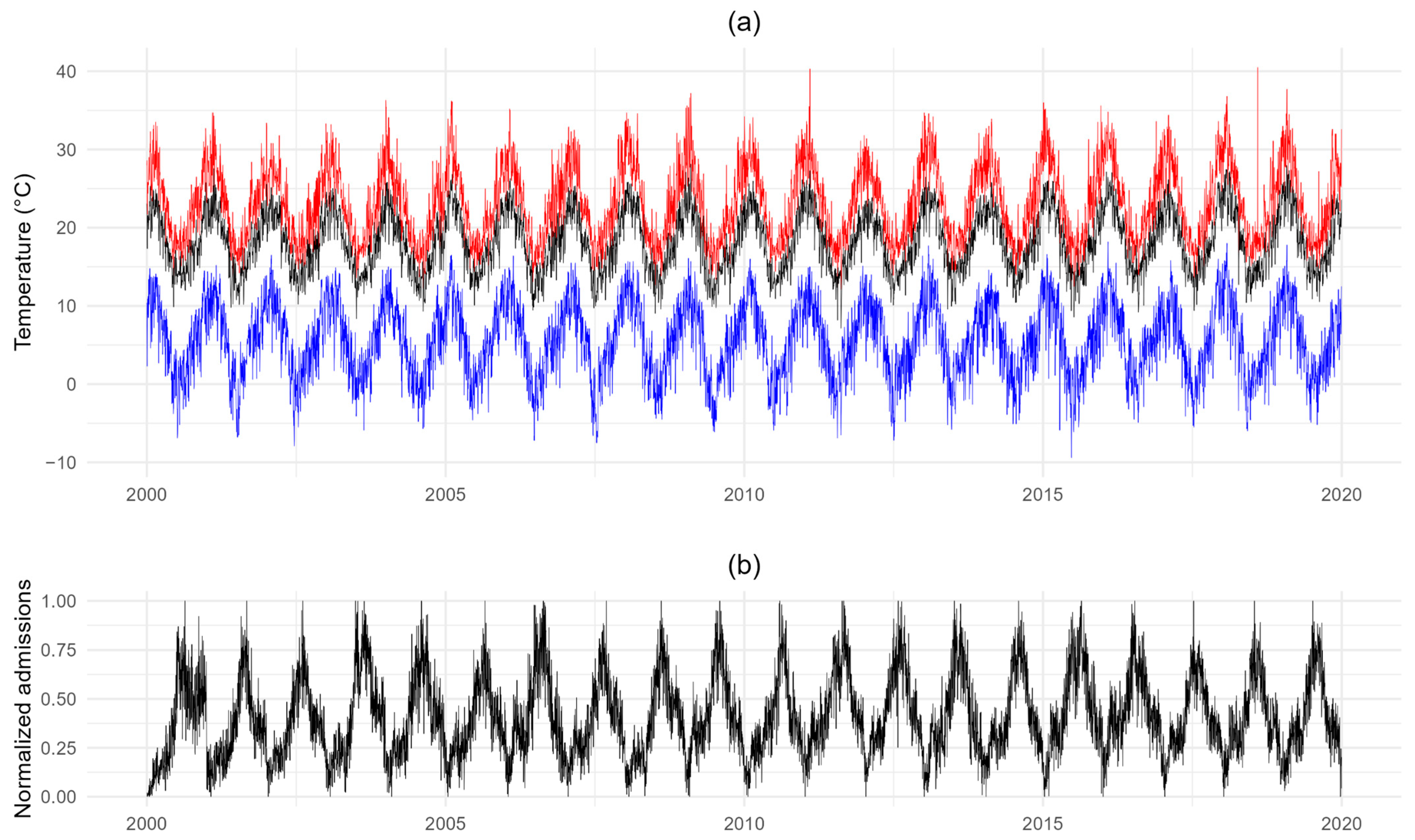
2. Materials and Methods
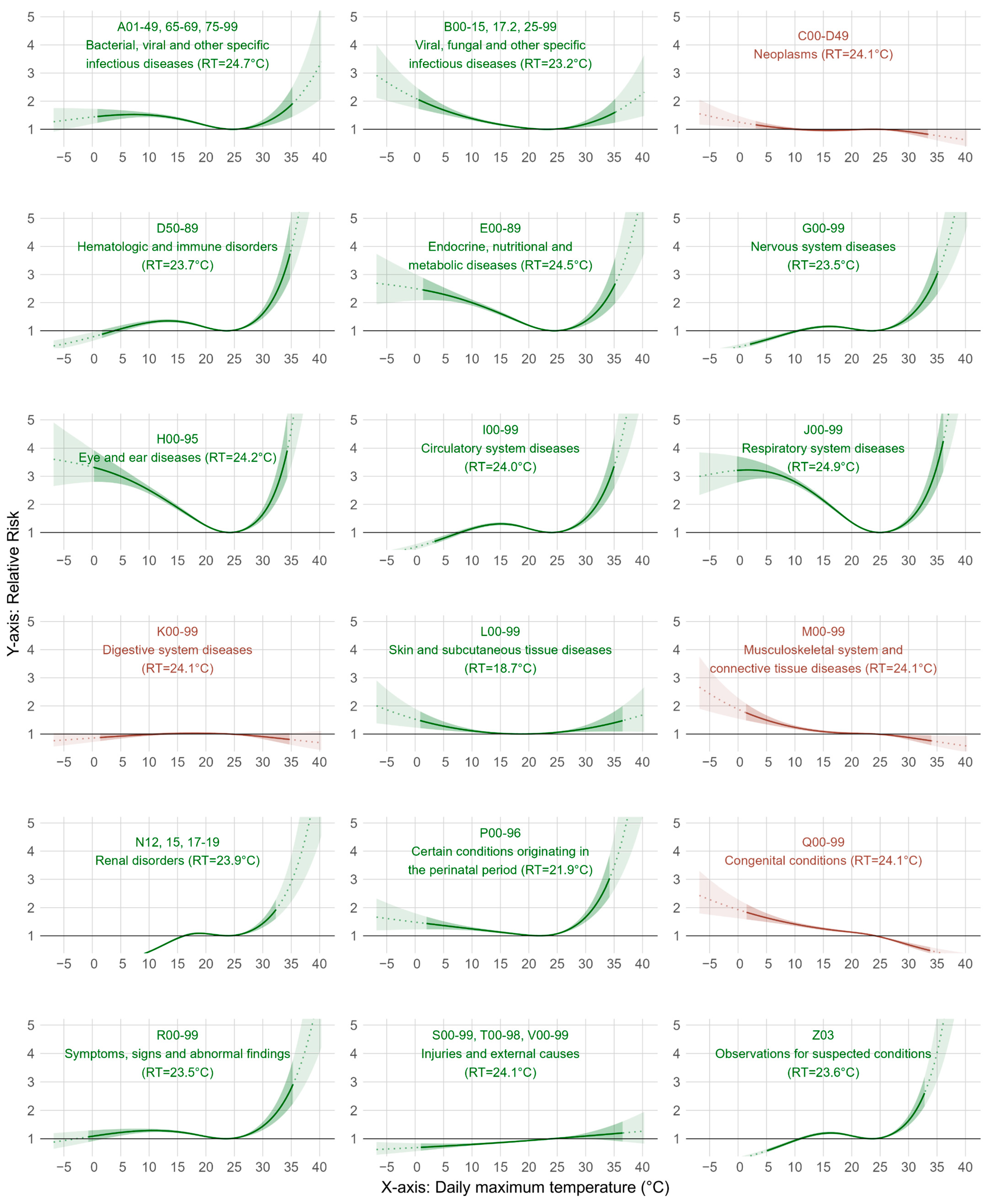
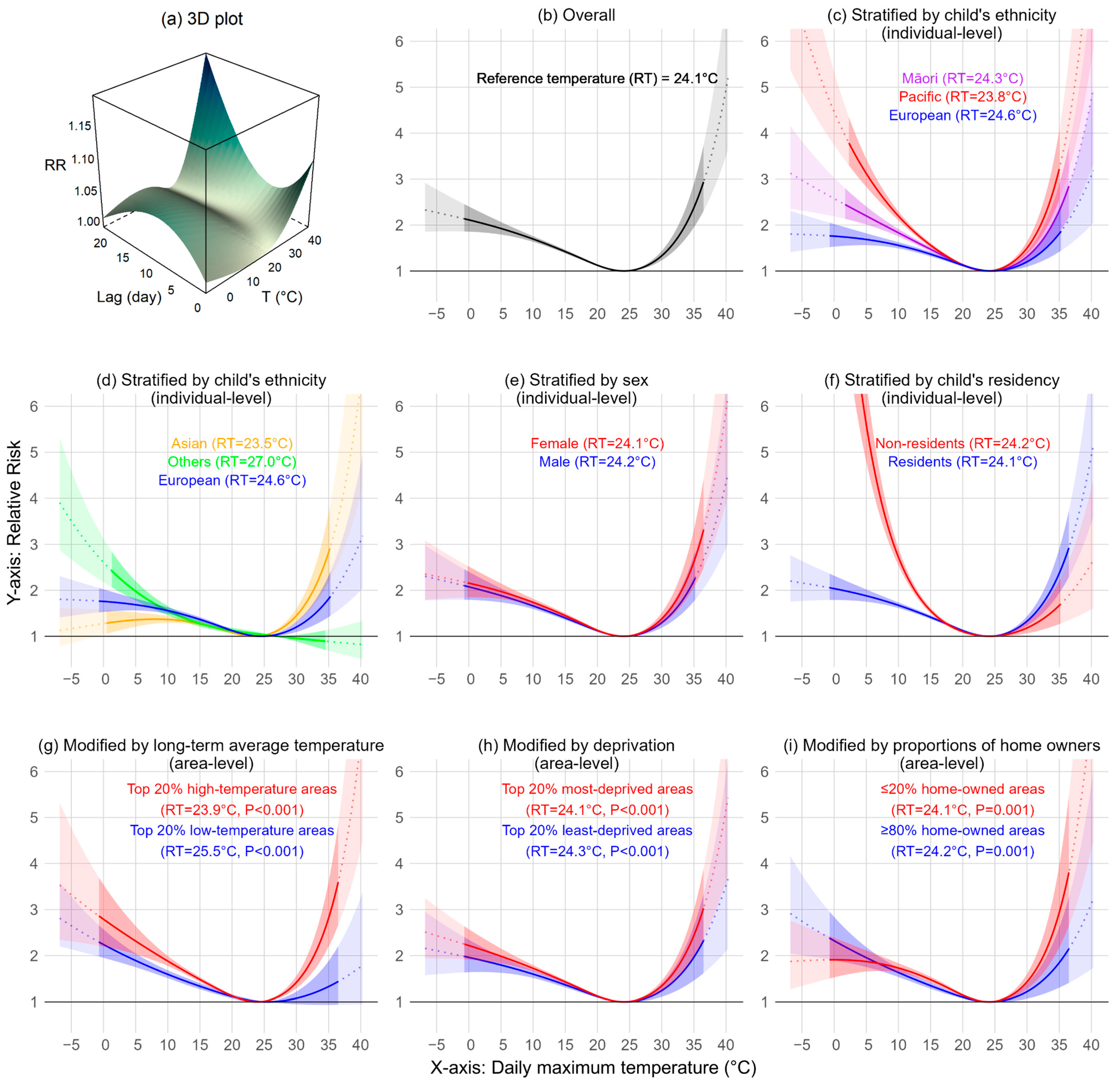
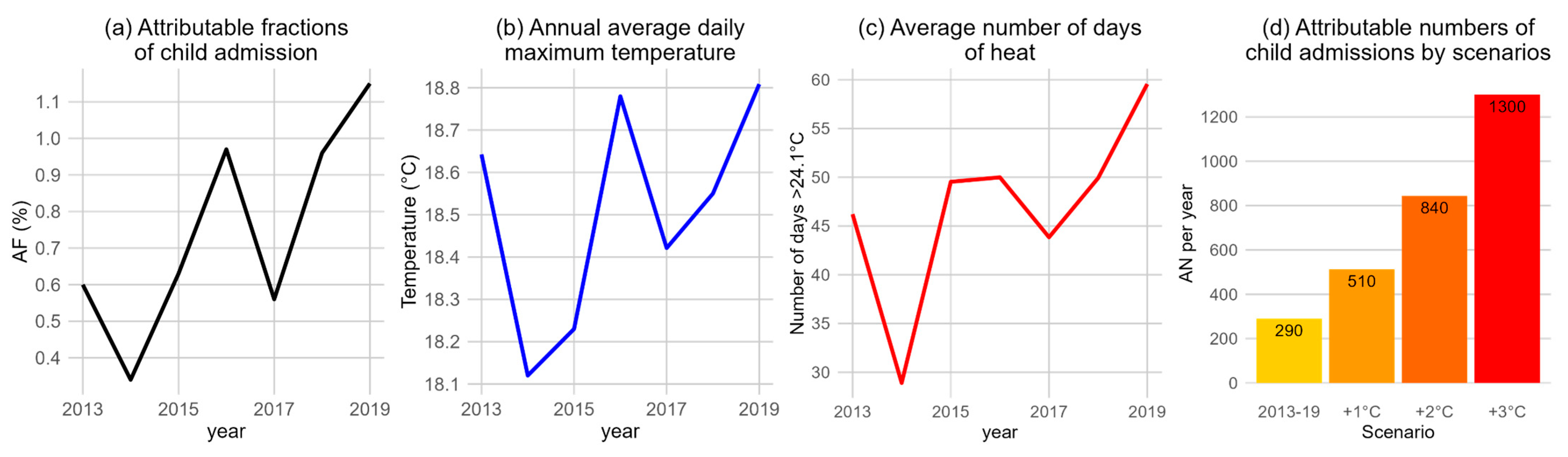
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Costello, A.; Abbas, M.; Allen, A.; Ball, S.; Bell, S.; Bellamy, R.; Friel, S.; Groce, N.; Johnson, A.; Kett, M.; et al. Managing the health effects of climate change: Lancet and University College London Institute for Global Health Commission. Lancet 2009, 373, 1693–1733. [Google Scholar] [CrossRef] [PubMed]
- Romanello, M.; Napoli, C.D.; Green, C.; Kennard, H.; Lampard, P.; Scamman, D.; Walawender, M.; Ali, Z.; Ameli, N.; Ayeb-Karlsson, S.; et al. The 2023 report of the Lancet Countdown on health and climate change: The imperative for a health-centred response in a world facing irreversible harms. Lancet 2023, 402, 2346–2394. [Google Scholar] [CrossRef] [PubMed]
- Rogelj, J.; Fransen, T.; den Elzen, M.G.J.; Lamboll, R.D.; Schumer, C.; Kuramochi, T.; Hans, F.; Mooldijk, S.; Portugal-Pereira, J. Credibility gap in net-zero climate targets leaves world at high risk. Science 2023, 380, 1014–1016. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Sheffield, P.E.; Su, H.; Wang, X.; Bi, Y.; Tong, S. The impact of heat waves on children’s health: A systematic review. Int. J. Biometeorol. 2014, 58, 239–247. [Google Scholar] [CrossRef]
- Philipsborn, R.P.; Chan, K. Climate Change and Global Child Health. Pediatrics 2018, 141, e20173774. [Google Scholar] [CrossRef]
- Sheffield, P.E.; Landrigan, P.J. Global Climate Change and Children’s Health: Threats and Strategies for Prevention. Environ. Health Perspect. 2011, 119, 291–298. [Google Scholar] [CrossRef]
- Sheffield, P.E.; Weinberger, K.R.; Kinney, P.L. Climate change, aeroallergens, and pediatric allergic disease. Mt. Sinai J. Med. 2011, 78, 78–84. [Google Scholar] [CrossRef]
- Clarke, B.; Otto, F.; Stuart-Smith, R.; Harrington, L. Extreme weather impacts of climate change: An attribution perspective. Environ. Res. Clim. 2022, 1, 012001. [Google Scholar] [CrossRef]
- Vicedo-Cabrera, A.M.; Scovronick, N.; Sera, F.; Royé, D.; Schneider, R.; Tobias, A.; Astrom, C.; Guo, Y.; Honda, Y.; Hondula, D.M.; et al. The burden of heat-related mortality attributable to recent human-induced climate change. Nat. Clim. Chang. 2021, 11, 492–500. [Google Scholar] [CrossRef]
- Ebi, K.L. Managing climate change risks is imperative for human health. Nat. Rev. Nephrol. 2022, 18, 74–75. [Google Scholar] [CrossRef]
- Lakhoo, D.P.; Blake, H.A.; Chersich, M.F.; Nakstad, B.; Kovats, S. The Effect of High and Low Ambient Temperature on Infant Health: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 9109. [Google Scholar] [CrossRef] [PubMed]
- Chersich, M.F.; Pham, M.D.; Areal, A.; Haghighi, M.M.; Manyuchi, A.; Swift, C.P.; Wernecke, B.; Robinson, M.; Hetem, R.; Boeckmann, M.; et al. Associations between high temperatures in pregnancy and risk of preterm birth, low birth weight, and stillbirths: Systematic review and meta-analysis. BMJ (Clin. Res. Ed.) 2020, 371, m3811. [Google Scholar] [CrossRef] [PubMed]
- Iñiguez, C.; Schifano, P.; Asta, F.; Michelozzi, P.; Vicedo-Cabrera, A.; Ballester, F. Temperature in summer and children’s hospitalizations in two Mediterranean cities. Environ. Res. 2016, 150, 236–244. [Google Scholar] [CrossRef] [PubMed]
- Oh, J.; Kim, E.; Kwag, Y.; An, H.; Kim, H.S.; Shah, S.; Lee, J.H.; Ha, E. Heat wave exposure and increased heat-related hospitalizations in young children in South Korea: A time-series study. Environ. Res. 2024, 241, 117561. [Google Scholar] [CrossRef] [PubMed]
- Neff, J.M.; Clifton, H.; Park, K.J.; Goldenberg, C.; Popalisky, J.; Stout, J.W.; Danielson, B.S. Identifying children with lifelong chronic conditions for care coordination by using hospital discharge data. Acad. Pediatr. 2010, 10, 417–423. [Google Scholar] [CrossRef]
- McMichael, A.J.; Wilkinson, P.; Kovats, R.S.; Pattenden, S.; Hajat, S.; Armstrong, B.; Vajanapoom, N.; Niciu, E.M.; Mahomed, H.; Kingkeow, C.; et al. International study of temperature, heat and urban mortality: The ‘ISOTHURM’ project. Int. J. Epidemiol. 2008, 37, 1121–1131. [Google Scholar] [CrossRef]
- Zhao, Q.; Guo, Y.; Ye, T.; Gasparrini, A.; Tong, S.; Overcenco, A.; Urban, A.; Schneider, A.; Entezari, A.; Vicedo-Cabrera, A.M.; et al. Global, regional, and national burden of mortality associated with non-optimal ambient temperatures from 2000 to 2019: A three-stage modelling study. Lancet Planet Health 2021, 5, e415–e425. [Google Scholar] [CrossRef]
- Gasparrini, A.; Guo, Y.; Hashizume, M.; Lavigne, E.; Zanobetti, A.; Schwartz, J.; Tobias, A.; Tong, S.; Rocklov, J.; Forsberg, B.; et al. Mortality risk attributable to high and low ambient temperature: A multicountry observational study. Lancet 2015, 386, 369–375. [Google Scholar] [CrossRef]
- Cure Kids; New Zealand Child & Youth Epidemiology Service; Paediatric Society of New Zealand; Royal Australasian College of Physicians. State of child health in Aotearoa New Zealand 2022; Cure Kids: Auckland, New Zealand, 2023. [Google Scholar]
- MoH. Reducing Inequalities in Health; Ministry of Health: Wellington, New Zealand, 2002. [Google Scholar]
- Young, P.C.; Korgenski, K.; Buchi, K.F. Early readmission of newborns in a large health care system. Pediatrics 2013, 131, e1538–e1544. [Google Scholar] [CrossRef]
- NIWA. Climate Data—NIWA Maintains the National Climate Database for New Zealand, and Can Supply Climate Data in a Variety of Ways. Available online: https://niwa.co.nz/climate-and-weather/climate-data (accessed on 1 December 2022).
- Gasparrini, A.; Masselot, P.; Scortichini, M.; Schneider, R.; Mistry, M.N.; Sera, F.; Macintyre, H.L.; Phalkey, R.; Vicedo-Cabrera, A.M. Small-area assessment of temperature-related mortality risks in England and Wales: A case time series analysis. Lancet Planet Health 2022, 6, e557–e564. [Google Scholar] [CrossRef]
- Xu, Z.; Hu, W.; Su, H.; Turner, L.R.; Ye, X.; Wang, J.; Tong, S. Extreme temperatures and paediatric emergency department admissions. J. Epidemiol. Community Health 2014, 68, 304–311. [Google Scholar] [CrossRef] [PubMed]
- Gasparrini, A.; Leone, M. Attributable risk from distributed lag models. BMC Med. Res. Methodol. 2014, 14, 55. [Google Scholar] [CrossRef] [PubMed]
- Bernstein, A.S.; Sun, S.; Weinberger, K.R.; Spangler, K.R.; Sheffield, P.E.; Wellenius, G.A. Warm Season and Emergency Department Visits to U.S. Children’s Hospitals. Environ. Health Perspect. 2022, 130, 17001. [Google Scholar] [CrossRef] [PubMed]
- Uibel, D.; Sharma, R.; Piontkowski, D.; Sheffield, P.E.; Clougherty, J.E. Association of ambient extreme heat with pediatric morbidity: A scoping review. Int. J. Biometeorol. 2022, 66, 1683–1698. [Google Scholar] [CrossRef] [PubMed]
- Czumbel, I.; Quinten, C.; Lopalco, P.; Semenza, J.C.; Tozzi, A.E.; Weil-Oliver, C.; Nichols, G.; Nøkleby, H.; Brumboiu, I.; Verheijen, J.; et al. Management and control of communicable diseases in schools and other child care settings: Systematic review on the incubation period and period of infectiousness. BMC Infect. Dis. 2018, 18, 199. [Google Scholar] [CrossRef]
- Huang, N.N.; Zheng, H.; Li, B.; Fei, G.Q.; Ding, Z.; Wang, J.J.; Li, X.B. The Short-term Effects of Temperature on Infectious Diarrhea among Children under 5 Years Old in Jiangsu, China: A Time-series Study (2015–2019). Curr. Med. Sci. 2021, 41, 211–218. [Google Scholar] [CrossRef]
- Pajuelo, M.J.; Anticona Huaynate, C.; Correa, M.; Mayta Malpartida, H.; Ramal Asayag, C.; Seminario, J.R.; Gilman, R.H.; Murphy, L.; Oberhelman, R.A.; Paz-Soldan, V.A. Delays in seeking and receiving health care services for pneumonia in children under five in the Peruvian Amazon: A mixed-methods study on caregivers’ perceptions. BMC Health Serv. Res. 2018, 18, 149. [Google Scholar] [CrossRef]
- Liska, D.; Mah, E.; Brisbois, T.; Barrios, P.L.; Baker, L.B.; Spriet, L.L. Narrative Review of Hydration and Selected Health Outcomes in the General Population. Nutrients 2019, 11, 70. [Google Scholar] [CrossRef]
- Duncanson, M.; Roy, M.; van Asten, H.; Oben, G.; Wicken, A.; Tustin, K.; McAnally, H.; Adams, J. Child Poverty Monitor 2022 Technical Report; NZ Child and Youth Epidemiology Service, University of Otago: Dunedin, New Zealand, 2022. [Google Scholar]
- Sinclair, O.; Lyndon, M. Pathways towards Health Equity for Tamariki MĀORI; Child Poverty Action Group: Auckland, New Zealand, 2023. [Google Scholar]
- Liu, L.S.; Jia, X.; Zhu, A.; Ran, G.J.; Siegert, R.; French, N.; Johnston, D. Stigmatising and Racialising COVID-19: Asian People’s Experience in New Zealand. J. Racial Ethn. Health Disparities 2023, 10, 2704–2717. [Google Scholar] [CrossRef]
- Hansen, A.; Bi, L.; Saniotis, A.; Nitschke, M. Vulnerability to extreme heat and climate change: Is ethnicity a factor? Glob. Health Action 2013, 6, 21364. [Google Scholar] [CrossRef]
- Exeter, D.J.; Zhao, J.; Crengle, S.; Lee, A.; Browne, M. The New Zealand Indices of Multiple Deprivation (IMD): A new suite of indicators for social and health research in Aotearoa, New Zealand. PLoS ONE 2017, 12, e0181260. [Google Scholar] [CrossRef] [PubMed]
- George, M.; Richards, R.; Watson, B.; Lucas, A.; Fitzgerald, R.; Taylor, R.; Galland, B. Pacific families navigating responsiveness and children’s sleep in Aotearoa New Zealand. Sleep Med. X 2021, 3, 100039. [Google Scholar] [CrossRef] [PubMed]
- Poland, M.; Paterson, J.; Carter, S.; Gao, W.; Perese, L.; Stillman, S. Pacific Islands Families Study: Factors associated with living in extended families one year on from the birth of a child. Kōtuitui N. Z. J. Soc. Sci. Online 2007, 2, 17–28. [Google Scholar] [CrossRef]
- Wickham, K.A.; Wallace, P.J.; Cheung, S.S. Sex differences in the physiological adaptations to heat acclimation: A state-of-the-art review. Eur. J. Appl. Physiol. 2021, 121, 353–367. [Google Scholar] [CrossRef] [PubMed]
- Statistics New Zealand. International Migration: January 2024. Available online: https://www.stats.govt.nz/information-releases/international-migration-january-2024 (accessed on 1 August 2024).
- Tochihara, Y.; Wakabayashi, H.; Lee, J.-Y.; Wijayanto, T.; Hashiguchi, N.; Saat, M. How humans adapt to hot climates learned from the recent research on tropical indigenes. J. Physiol. Anthropol. 2022, 41, 27. [Google Scholar] [CrossRef]
- Kenny, G.P.; Notley, S.R.; Flouris, A.D.; Grundstein, A. Climate Change and Heat Exposure: Impact on Health in Occupational and General Populations. In Exertional Heat Illness: A Clinical and Evidence-Based Guide; Adams, W.M., Jardine, J.F., Eds.; Springer International Publishing: Cham, Switzerland, 2020; pp. 225–261. [Google Scholar]
- Hu, M.; Lin, Z.; Liu, Y. Housing Disparity between Homeowners and Renters: Evidence from China. J. Real Estate Financ. Econ. 2024, 68, 28–51. [Google Scholar] [CrossRef]
- Ballester, J.; Quijal-Zamorano, M.; Méndez Turrubiates, R.F.; Pegenaute, F.; Herrmann, F.R.; Robine, J.M.; Basagaña, X.; Tonne, C.; Antó, J.M.; Achebak, H. Heat-related mortality in Europe during the summer of 2022. Nat. Med. 2023, 29, 1857–1866. [Google Scholar] [CrossRef]
- Statistics New Zealand. National Population Projections: 2020(base)–2073. December 2020. Available online: https://www.stats.govt.nz/information-releases/national-population-projections-2020base2073 (accessed on 1 August 2024).
- Wan, K.; Lane, M.; Feng, Z. Heat-health governance in a cool nation: A case study of Scotland. Environ. Sci. Policy 2023, 147, 57–66. [Google Scholar] [CrossRef]
- Health New Zealand. Heat Health Plans: Guidelines and Key Information. September 2023. Available online: https://www.tewhatuora.govt.nz/publications/heat-health-plans-guidelines (accessed on 22 August 2024).
- Pourzand, F.; Bolton, A.; Salter, C.; Hales, S.; Woodward, A. Health and climate change: Adaptation policy in Aotearoa New Zealand. Lancet Reg. Health West. Pac. 2023, 40, 100954. [Google Scholar] [CrossRef]
- UNICEF. Protecting Children from Heat Stress—A Technical Note; Health Programme, Programme Group, United Nations Children’s Fund: New York, NY, USA, 2023. [Google Scholar]
- Zangerl, K.E.; Hoernke, K.; Andreas, M.; Dalglish, S.L.; Kelman, I.; Nilsson, M.; Rockloev, J.; Bärnighausen, T.; McMahon, S.A. Child health prioritisation in national adaptation policies on climate change: A policy document analysis across 160 countries. Lancet Child Adolesc. Health 2024, 8, 532–544. [Google Scholar] [CrossRef]
| Policy | Examples |
|---|---|
| |
| Advancing indigenous perspectives and solutions | (1) Collaboratively design solutions, and (2) jointly implement actions that specifically cater to the needs of Māori, Pacific, and Asian children, including indigenous solutions. |
| |
| All policy promotes equity and equitable solutions | (1) Respect and uphold the principles of absolute sovereignty and self-determination (tino rangatiratanga), and allocate funds to support kaupapa approaches. (2) The most vulnerable and at-risk children are prioritised. |
| |
| Knowledge transfer | (1) Share research findings and create opportunities to share knowledge on child-related health impacts, prevention, and adaptation to heat, (2) with a focus on pregnant women and infants and children. |
| Mainstreaming existing policies | (2) Craft policy briefs to effectively communicate research findings and facilitate their widespread distribution. (3) Incorporate temperature and health impacts into pertinent policy documents for comprehensive consideration. (4) Integrate and recognise synergies with existing climate adaptation plans, such as the Health National Adaptation Plan. (5) Develop national guidelines for educational initiatives addressing maximum temperatures to safeguard health and ensure safety. (6) Encompass climate mitigation and strategies for coping with extreme temperatures within Long-Term Plans. (7) Embrace a “Health in All Policies” approach, fostering a comprehensive consideration of health implications across all policy domains. |
| |
| Risk communication and surveillance | (1) Pregnant mothers, parents, carers, and those working with children have the knowledge to reduce the risk of heat-related impacts. |
| Enhancing governance in child heat health | (2) Foster cross-sectoral collaboration at both local and national levels, forging connections with established experts, such as the National Emergency Management Agency’s heat health group, MetService, the Ministry for the Environment, and the Ministry of Health. (3) Ensure adequate resourcing to effectively implement policy approaches. (4) Comply with and leverage existing legislation to strengthen the foundation of the initiatives and enhance their effectiveness. |
| |
| Review healthcare practices for pregnant women, infants, and children | (1) Enable diagnosis of heat-related illness in clinical settings. (2) Establish case management flows for diagnosing and treating heat-related illness in vulnerable populations. (3) Understand medications, complications, and comorbidities that relate to heat stress. (4) Understand comorbidities and the impact of health emergencies. |
| |
| Preparing child-specific and Early Childhood Education (ECE) centres | (1) Incorporate critical considerations into health and safety assessments and ensure compliance, including the provision of adequate shade, ventilation, water, and cooling/air conditioning. (2) Provide support for non-governmental organizations (NGOs) and independent groups, such as play centres, to enhance their capacity and effectiveness in implementing these considerations. |
| Preparing healthcare facilities | (3) Implement strategies for shade provision, cooling methods, emissions reduction, and adequate access to water resources. (4) Develop and enact Regional Heat Health Plans to address localized challenges and ensure comprehensive heat management strategies. |
| Planning and implementation of risk communication and outreach campaigns for educational or behavioural change | (5) Develop targeted public health messaging with tailored advice for parents and child caregivers. (6) Launch campaigns aimed at raising public awareness and delivering essential services for effective heat wave management. (7) Ensure consistent messaging that draws connections between addressing health impacts associated with both hot and cold temperatures, as well as air quality concerns. (8) Implement early warning systems that are integrated into healthcare planning and ECE settings for a proactive response. |
| |
| Advancing housing standards and guidelines | (1) Introduce new standards, codes, action plans, or infrastructural upgrades for buildings to enhance thermal comfort, keeping homes cool in summer and warm in winter. (2) Ensure rental houses adhere to guidelines for mitigating heat and cold, such as the Rental Warrant of Fitness and World Health Organization housing and health recommendations. |
| Addressing the interplay between housing and socioeconomic factors | (3) Provide support for vulnerable populations to prevent heating/cooling poverty, including initiatives like the Healthy Homes initiative, and (4) the expansion of grants from the Energy Efficiency and Conservation Authority or the Ministry for Business, Innovation and Employment. (5) Enhance safety in neighbourhoods and buildings through improved security features, facilitating natural ventilation. |
| |
| Navigating the intersection of housing and urban planning in local neighbourhoods | (1) Mitigate the urban heat island effect by incorporating strategic tree provision, recognising the necessary time for trees to mature, especially in new housing developments. (2) Enhance access to green and blue spaces, addressing disparities in tree canopy coverage. (3) Install drinking water fountains in schools, playgrounds, and other public areas. (4) Implement shading in parks and playgrounds to create comfortable outdoor spaces. (5) Strengthen the resilience of the water supply and critical infrastructure to manage increased demand during heat waves. (6) Provide shade and shelter in transportation settings. (7) Establish cooling centres, utilizing recreation facilities and other public spaces like shopping malls, and promote active health opportunities, such as swimming and indoor sports. |
| Promoting green and natural infrastructure | (8) Implement nature-based greening and water solutions to promote sustainable and environmentally friendly practices. |
| |
| Developing a Health National Adaptation Plan with a focus on children and other vulnerable populations | (1) Provide effective co-ordination mechanisms to protect human health from excess heat. (2) Provide effective polices for coping with excess heat. (3) Provide early warning and notification systems. (4) Ensure a primary healthcare approach to protecting children and other vulnerable populations from heat stress. (5) Adapt built environments for the long term (see g.1 to g.5 and h.1 to h.3). |
| Conducting comprehensive research and evaluation | (6) Draw insights from adaptation examples in countries with extensive experience in managing heat health, such as Australia. (7) Foster connections and effective communication channels for disseminating heat-related research to the appropriate end users. (8) Evaluate the return on investment of implemented policies to better understand their effectiveness and impact. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lai, H.; Lee, J.E.; Harrington, L.J.; Ahuriri-Driscoll, A.; Newport, C.; Bolton, A.; Salter, C.; Morton, S.; Woodward, A.; Hales, S. Daily Temperatures and Child Hospital Admissions in Aotearoa New Zealand: Case Time Series Analysis. Int. J. Environ. Res. Public Health 2024, 21, 1236. https://doi.org/10.3390/ijerph21091236
Lai H, Lee JE, Harrington LJ, Ahuriri-Driscoll A, Newport C, Bolton A, Salter C, Morton S, Woodward A, Hales S. Daily Temperatures and Child Hospital Admissions in Aotearoa New Zealand: Case Time Series Analysis. International Journal of Environmental Research and Public Health. 2024; 21(9):1236. https://doi.org/10.3390/ijerph21091236
Chicago/Turabian StyleLai, Hakkan, Jeong Eun Lee, Luke J. Harrington, Annabel Ahuriri-Driscoll, Christina Newport, Annette Bolton, Claire Salter, Susan Morton, Alistair Woodward, and Simon Hales. 2024. "Daily Temperatures and Child Hospital Admissions in Aotearoa New Zealand: Case Time Series Analysis" International Journal of Environmental Research and Public Health 21, no. 9: 1236. https://doi.org/10.3390/ijerph21091236
APA StyleLai, H., Lee, J. E., Harrington, L. J., Ahuriri-Driscoll, A., Newport, C., Bolton, A., Salter, C., Morton, S., Woodward, A., & Hales, S. (2024). Daily Temperatures and Child Hospital Admissions in Aotearoa New Zealand: Case Time Series Analysis. International Journal of Environmental Research and Public Health, 21(9), 1236. https://doi.org/10.3390/ijerph21091236








