Can Mindfulness-Based Stress Reduction Influence the Quality of Life, Anxiety, and Depression of Women Diagnosed with Breast Cancer? —A Review
Abstract
:1. Introduction
Aim
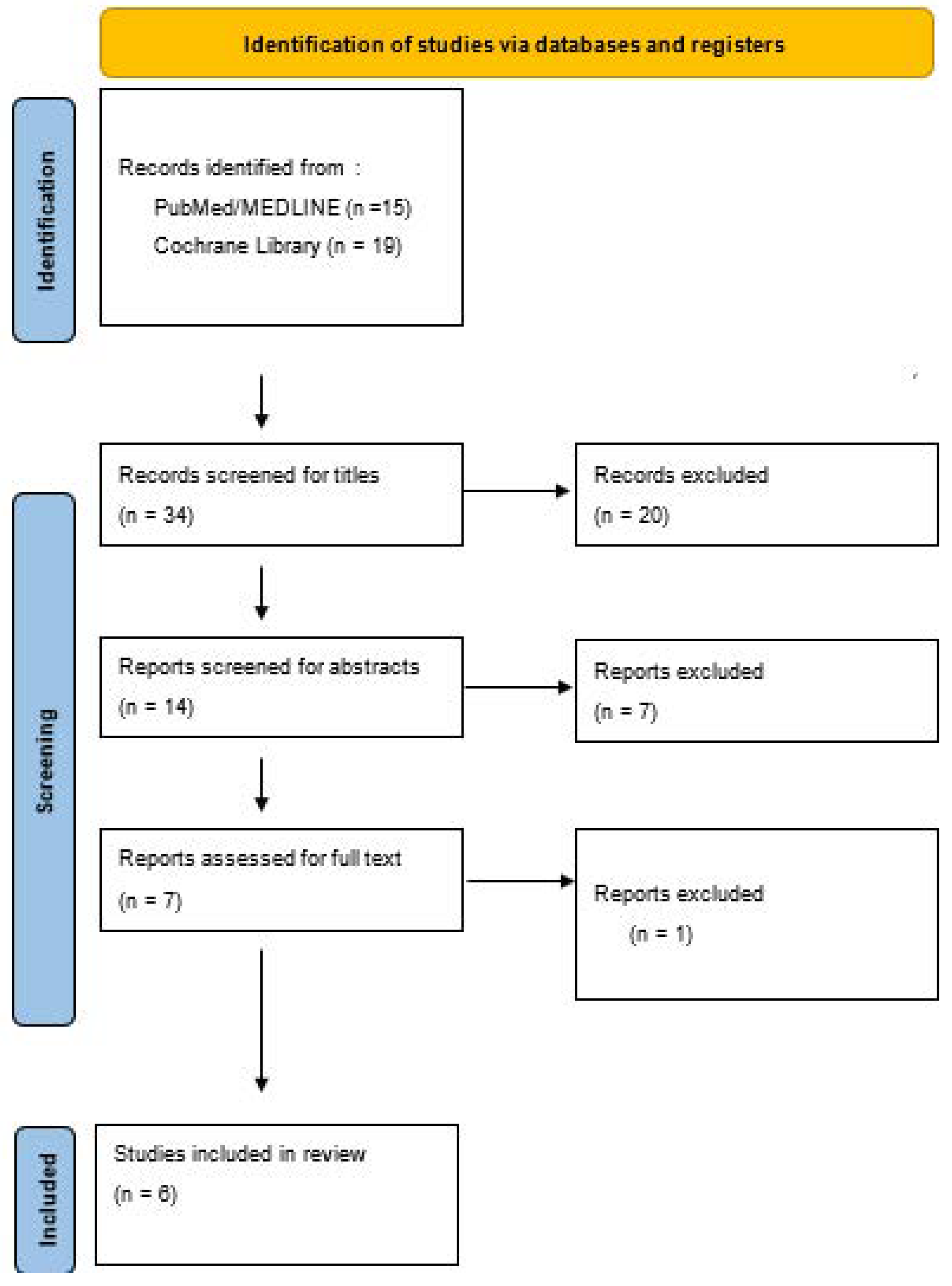
2. Materials and Methods
2.1. Risk of Bias Assessment
2.2. Ethical Consideration
2.3. Definition of Measurement Tools
3. Results
3.1. Primary Outcome: Quality of Life
3.2. Secondary Outcomes: Anxiety and Depression
4. Discussion
5. Conclusions
- (1)
- The duration of the intervention varied between the studies included and did not always last the mandatory eight-week time period of MBSR training, which may have had an adverse impact on the effectiveness of the interventions.
- (2)
- The number of participants in every study was less than 100, which makes it difficult to draw general conclusions about the general population.
- (3)
- Hardly any long-term data were collected in the studies included, which rules out the projection of long-term trends.
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Johannsen, M.; O’Connor, M.; O’Toole, M.S.; Jensen, A.B.; Hojris, I.; Zachariae, R. Efficacy of Mindfulness-Based Cognitive Therapy on Late Post-Treatment Pain in Women Treated for Primary Breast Cancer: A Randomized Controlled Trial. J. Clin. Oncol. 2016, 34, 3390–3399. [Google Scholar] [CrossRef] [PubMed]
- Kabat-Zinn, J. Gesund Durch Meditation, Das Große Buch Der Selbstheilung MIT Mbsr; Kappen, H., Ed.; KNAUR Verlag: Munich, Germany, 2019. [Google Scholar]
- Schell, L.K.; Monsef, I.; Wöckel, A.; Skoetz, N. Mindfulness-based stress reduction for women diagnosed with breast cancer. Cochrane Database Syst. Rev. 2019, 3, Cd011518. [Google Scholar] [CrossRef] [PubMed]
- Elimimian, E.; Elson, L.; Bilani, N.; Farrag, S.E.; Dwivedi, A.K.; Pasillas, R.; Nahleh, Z.A. Long-Term Effect of a Nonrandomized Psychosocial Mindfulness-Based Intervention in Hispanic/Latina Breast Cancer Survivors. Integr. Cancer Ther. 2020, 19, 1534735419890682. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chang, Y.C.; Lin, G.M.; Yeh, T.L.; Chang, Y.M.; Yang, C.H.; Lo, C.; Yeh, C.Y.; Hu, W.Y. Impact of mindfulness-based stress reduction on female sexual function and mental health in patients with breast cancer. Support. Care Cancer 2022, 30, 4315–4325. [Google Scholar] [CrossRef] [PubMed]
- Lengacher, C.A.; Reich, R.R.; Paterson, C.L.; Shelton, M.; Shivers, S.; Ramesar, S.; Pleasant, M.L.; Budhrani-Shani, P.; Groer, M.; Post-White, J.; et al. A Large Randomized Trial: Effects of Mindfulness-Based Stress Reduction (MBSR) for Breast Cancer (BC) Survivors on Salivary Cortisol and IL-6. Biol. Res. Nurs. 2019, 21, 39–49. [Google Scholar] [CrossRef] [PubMed]
- Mirmahmoodi, M.; Mangalian, P.; Ahmadi, A.; Dehghan, M. The Effect of Mindfulness-Based Stress Reduction Group Counseling on Psychological and Inflammatory Responses of the Women With Breast Cancer. Integr. Cancer Ther. 2020, 19, 1534735420946819. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.C.; Yeh, T.L.; Chang, Y.M.; Hu, W.Y. Short-term Effects of Randomized Mindfulness-Based Intervention in Female Breast Cancer Survivors: A Systematic Review and Meta-analysis. Cancer Nurs. 2021, 44, E703–E714. [Google Scholar] [CrossRef]
- Zhang, Q.; Zhao, H.; Zheng, Y. Effectiveness of mindfulness-based stress reduction (MBSR) on symptom variables and health-related quality of life in breast cancer patients-a systematic review and meta-analysis. Support. Care Cancer 2019, 27, 771–781. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomized studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhou, T.; Guan, H.; Wang, L.; Zhang, Y.; Rui, M.; Ma, A. Health-Related Quality of Life in Patients With Different Diseases Measured With the EQ-5D-5L: A Systematic Review. Front. Public Health 2021, 9, 675523. [Google Scholar] [CrossRef] [PubMed]
- Patel, A.A.; Donegan, D.; Albert, T. The 36-item short form. J. Am. Acad. Orthop. Surg. 2007, 15, 126–134. [Google Scholar] [CrossRef] [PubMed]
- Castaldelli-Maia, J.M.; Marziali, M.E.; Lu, Z.; Martins, S.S. Investigating the effect of national government physical distancing measures on depression and anxiety during the COVID-19 pandemic through meta-analysis and meta-regression. Psychol. Med. 2021, 51, 881–893. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.T.; Epstein, N.; Brown, G.; Steer, R.A. An inventory for measuring clinical anxiety: Psychometric properties. J. Consult. Clin. Psychol. 1988, 56, 893–897. [Google Scholar] [CrossRef] [PubMed]
- Toledano-Toledano, F.; Moral de la Rubia, J.; Domínguez-Guedea, M.T.; Nabors, L.A.; Barcelata-Eguiarte, B.E.; Rocha-Pérez, E.; Luna, D.; Leyva-López, A.; Rivera-Rivera, L. Validity and Reliability of the Beck Anxiety Inventory (BAI) for Family Caregivers of Children with Cancer. Int. J. Environ. Res. Public Health 2020, 17, 7765. [Google Scholar] [CrossRef] [PubMed]
- Park, K.; Jaekal, E.; Yoon, S.; Lee, S.H.; Choi, K.H. Diagnostic Utility and Psychometric Properties of the Beck Depression Inventory-II Among Korean Adults. Front. Psychol. 2019, 10, 2934. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blodgett, J.M.; Lachance, C.C.; Stubbs, B.; Co, M.; Wu, Y.T.; Prina, M.; Tsang, V.W.L.; Cosco, T.D. A systematic review of the latent structure of the Center for Epidemiologic Studies Depression Scale (CES-D) amongst adolescents. BMC Psychiatry 2021, 21, 197. [Google Scholar] [CrossRef] [PubMed]
| Category | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Population | Women over the age of 18, who have been diagnosed with breast cancer, who have no initial psychological co-morbidity and who undergo MBSR | Women younger than 18; women with any psychological illness diagnosed before their breast cancer diagnosis |
| Intervention | Any form of mindfulness-based stress reduction or mindfulness-based cognitive therapy | Any other form of psychological therapy |
| Control | Women suffering from breast cancer that did not receive any form of psychological therapy | Any other forms of therapy beside MBSR |
| Outcomes |
| Other outcomes that cannot be allocated to the intervention |
| Study design |
| Any other study design |
| Publication date | After 2018 | Before 2018 |
| Language | German or English | Any other language |
| Duration | Any duration | No limitations |
| Search | Query | Results |
|---|---|---|
| #1 | breast cancer [Title/Abstract] | 307,817 |
| #2 | breast neoplasm [Title/Abstract] | 1013 |
| #3 | “Breast Neoplasms”[Mesh] Sort by: Most Recent | 321,610 |
| #4 | #1 OR #2 OR #3 | 410,079 |
| #5 | mindfulness based stress reduction [Title/Abstract] | 1189 |
| #6 | #5 OR #6 OR #7 | 1796 |
| #7 | #4 AND #8 | 114 |
| #8 | (“german”[Language]) OR (“english”[Language]) | 29,884,822 |
| #9 | #9 AND #10 | 112 |
| #10 | (“2018/01/01”[Date-Publication]: “3000”[Date-Publication]) | 5,816,422 |
| #11 | quality of life | 473,503 |
| #12 | #10 AND #11 AND #12 | 15 |
| Type of Study | Number of Participants (n) | Primary Outcome | Secondary Outcome | Duration of the Intervention | Number of Included Studies | (Mean) Age | Stage of Disease | Treatment | MBSR Intervention Time Period | |
|---|---|---|---|---|---|---|---|---|---|---|
| Elimimian (2020) [4] | nRCT | n = 94 | Quality of life | Anxiety, Depression | Eight weeks | / | 54.4 (SD = 8.71) | 1–3 | Surgery, chemotherapy and/or radiation therapy | After treatment |
| Chang (2022) [5] | nRCT | n = 51 | Female sexual function, Depression | Quality of life, Anxiety | Six weeks | / | 47.77 (SD = 9.29) | 0–4 | Mainly hormone therapy | During treatment |
| Lengacher (2019) [6] | RCT | n = 322 | Cortisol-levels, IL-6-levels | Depression, Anxiety, Quality of life, Stress | Six weeks | / | 56.6 (SD = 9.7) | 0–3 | Lumpectomy and/or mastectomy Adjuvant radiation and/or chemotherapy | After treatment |
| Mirmahmoodi (2020) [7] | RCT | n = 44 | Depression, Anxiety, Perceived Stress | / | Eight weeks | / | 44.14 (SD = 11.19) | Nonmetastatic stage | Mainly chemotherapy and radiotherapy and surgery | During treatment |
| Chang (2020) [8] | Meta- analysis | n = 36–322 | Depression, Anxiety | Quality of life, Fatigue, Pain | Six–eight weeks | n = 11 | 43–58 * | 0–4 | Mastectomy, lumpectomy, chemotherapy, radiation therapy and hormonal therapy | During, and after treatment |
| Zhang (2018) [9] | Meta- analysis | n = 1505 | Quality of life, Physical function, Pain, Fatigue | Anxiety, Depression, Sleep quality | Four–eight weeks | n = 14 | 40–57 * | 0–3 | No information | During, and after treatment |
| Lengacher (2019) [6] | Mirmahmoodi (2020) [7] | ||
|---|---|---|---|
| Domain 1: Randomisation process | 1.1. Was the allocation sequence random? | Y | Y |
| 1.2. Was the allocation sequence concealed until participants were enrolled and assigned to interventions? | Y | Y | |
| 1.3. Did baseline differences between intervention groups suggest a problem with the randomisation process? | N | N | |
| Risk of bias judgement | Low | Low | |
| Domain 2: Deviations from the intended interventions (effect of assignment to intervention) | 2.1. Were participants aware of their assigned intervention during the trial? | N | N |
| 2.2. Were carers and people delivering the interventions aware of participants assigned intervention during the trial? | Y | Y | |
| 2.3. If Y/PY/NI to 2.1 or 2.2: Were there deviations from the intended intervention that arose because of the trial context? | N | N | |
| 2.4. If Y/PY to 2.3: Were these deviations likely to have affected the outcome? | / | / | |
| 2.5. If Y/PY/NI to 2.4: Were these deviations from intended intervention balanced between groups? | / | / | |
| 2.6. Was an appropriate analysis used to estimate the effect of assignment to intervention? | Y | Y | |
| 2.7. If N/PN/NI to 2.6: Was there potential for a substantial impact (on the result) of the failure to analyse participants in the group to which they were randomised? | / | / | |
| Risk of bias judgement | Low | Low | |
| Domain 3: Risk of bias due to missing outcome data | 3.1. Were data for this outcome available for all, or nearly all, participants randomised? | Y | Y |
| 3.2 If N/PN/NI to 3.1: Is there evidence that the result was not biased by missing outcome data? | / | / | |
| 3.3. If N/PN to 3.2: Could missingness in the outcome depend on its true value? | / | / | |
| 3.4 If Y/PY/NI to 3.3: Is it likely that missingness in the outcome depended on its true value? | / | / | |
| Risk of bias judgement | Low | Low | |
| Domain 4: Risk of bias in measurement of the outcome | 4.1. Was the method of measuring the outcome inappropriate? | N | N |
| 4.2. Could measurement or ascertainment of the outcome have differed between intervention groups? | N | N | |
| 4.3. If N/PN/NI to 4.1 and 4.2: Were outcome assessors aware of the intervention received by study participants? | Y | N | |
| 4.4. If Y/PY/NI to 4.3: Could assessment of the outcome have been influenced by knowledge of intervention received? | Y | N | |
| 4.5. If Y/PY/NI to 4.4: Is it likely that assessment of the outcome was influenced by knowledge of intervention received? | N | / | |
| Risk of bias judgement | Some concerns | Low | |
| Domain 5: Selection of the reported result | 5.1. Were the data that produced this result analysed in accordance with a pre-specified analysis plan that was finalised before unblinded outcome data were available for analysis? | Y | Y |
| Is the numerical result being assessed likely to have been selected on the basis of the results from … | |||
| 5.2. multiple eligible outcome measurements (e.g., scales, definitions, timepoints) within the outcome domain? | N | N | |
| 5.3. multiple eligible analyses of the data? | N | N | |
| Risk of bias judgement | Low | Low | |
| Overall Risk of Bias | Some concerns | Low | |
| Elimimian (2020) [4] | Chang (2022) [5] | ||
|---|---|---|---|
| Bias due to confounding | Potential for confounding? | N | N |
| Appropriate analysis method to control for all the important confounding domains? | Y | Y | |
| Risk of Bias | Low | Low | |
| Bias in selection of participants into the study | Selection based on participants characteristic observed after the start of the intervention? | N | N |
| Most participants followed from the start of the intervention? | Y | Y | |
| Risk of Bias | Low | Low | |
| Bias in classification of interventions | Intervention groups clearly defined? | Y | Y |
| Risk of Bias | Low | Low | |
| Bias due to deviation from intended interventions | Deviations from intended interventions (e.g., High drop-out rate)? | N | N |
| Deviation unbalanced between groups? | N | N | |
| Risk of bias | Low | Low | |
| Bias due to missing data | Outcome data available for nearly all participants? | Y | Y |
| Participants excluded due to missing data? | N | N | |
| Risk of Bias | Low | Low | |
| Bias in measurement of outcomes | Could the outcome measure have been influenced by knowledge of the intervention received? | N | N |
| Were outcome assessors aware of the intervention received by study participants? | NI | N | |
| Were the methods of outcome assessment comparable across intervention groups? | Y | Y | |
| Risk of Bias | Moderate | Low | |
| Bias in selection of the reported result | Results likely to be selected from multiple measurements? | N | N |
| Risk of bias | Low | Low | |
| Randomisation | N | N | |
| Overall risk of bias | Moderate | Low | |
| Test Score | Result |
|---|---|
| 0–4 | Minimal Anxiety |
| 5–9 | Mild Anxiety |
| 10–14 | Moderate Anxiety |
| 15–21 | Severe Anxiety |
| Test Score | Result |
|---|---|
| 0–4 | Minimal Depressive Symptoms |
| 5–9 | Mild Depressive Symptoms |
| 10–14 | Moderate Depressive Symptoms |
| 15–27 | Severe Depressive Symptoms |
| Depression | Anxiety | Stress | |
|---|---|---|---|
| Normal | 0–4 | 0–3 | 0–7 |
| Mild | 5–6 | 4–5 | 8–9 |
| Moderate | 7–10 | 6–7 | 10–12 |
| Severe | 11–13 | 8–9 | 13–16 |
| Extremely Severe | >14 | >10 | >17 |
| Test Score | Result |
|---|---|
| 0–21 | Mild Anxiety |
| 22–35 | Moderate Anxiety |
| >36 | Severe Anxiety |
| Measured (via) | Significant Change | ||
|---|---|---|---|
| Elimimian et al. (2020) [4] | 36-SF | MCS-subscore | Yes |
| PCS-subscore | No | ||
| Lengacher et al. (2017) [6] | 36-SF | Cortisol | No |
| IL-6 | Yes | ||
| Chang et al. (2022) [5] | EQ-5D | No | |
| Zhang et al. (2018) [9] | Meta-analysis | No | |
| Chang et al. (2020) [8] | Meta-analysis | No | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ladenbauer, S.; Singer, J. Can Mindfulness-Based Stress Reduction Influence the Quality of Life, Anxiety, and Depression of Women Diagnosed with Breast Cancer? —A Review. Curr. Oncol. 2022, 29, 7779-7793. https://doi.org/10.3390/curroncol29100615
Ladenbauer S, Singer J. Can Mindfulness-Based Stress Reduction Influence the Quality of Life, Anxiety, and Depression of Women Diagnosed with Breast Cancer? —A Review. Current Oncology. 2022; 29(10):7779-7793. https://doi.org/10.3390/curroncol29100615
Chicago/Turabian StyleLadenbauer, Severin, and Josef Singer. 2022. "Can Mindfulness-Based Stress Reduction Influence the Quality of Life, Anxiety, and Depression of Women Diagnosed with Breast Cancer? —A Review" Current Oncology 29, no. 10: 7779-7793. https://doi.org/10.3390/curroncol29100615
APA StyleLadenbauer, S., & Singer, J. (2022). Can Mindfulness-Based Stress Reduction Influence the Quality of Life, Anxiety, and Depression of Women Diagnosed with Breast Cancer? —A Review. Current Oncology, 29(10), 7779-7793. https://doi.org/10.3390/curroncol29100615





