Feasibility, Acceptability, and Clinical Significance of a Dyadic, Web-Based, Psychosocial and Physical Activity Self-Management Program (TEMPO) Tailored to the Needs of Men with Prostate Cancer and Their Caregivers: A Multi-Center Randomized Pilot Trial
Abstract
:1. Introduction
TEMPO
- Self-Efficacy Theory [35] whereby strategies to enhance self-efficacy were built into TEMPO such as behavioral goals, behavior modeling from others, and verbal persuasion.
2. Materials and Methods
2.1. Design
2.2. Participants
2.3. Recruitment Procedures
2.4. Randomization and Blinding
2.5. TEMPO Intervention Group
2.6. Wait-List Control Group
2.7. Data Collection
2.7.1. Baseline Questionnaire (T1)
2.7.2. Follow-Up (T2) Questionnaires
2.7.3. Dyadic Exit Interviews
2.7.4. Study Logs
2.7.5. User Tracking Information
2.8. Data Analysis
2.8.1. Feasibility and Acceptability Data
2.8.2. Clinical Significance
2.8.3. Analysis of Exit Interviews
3. Results
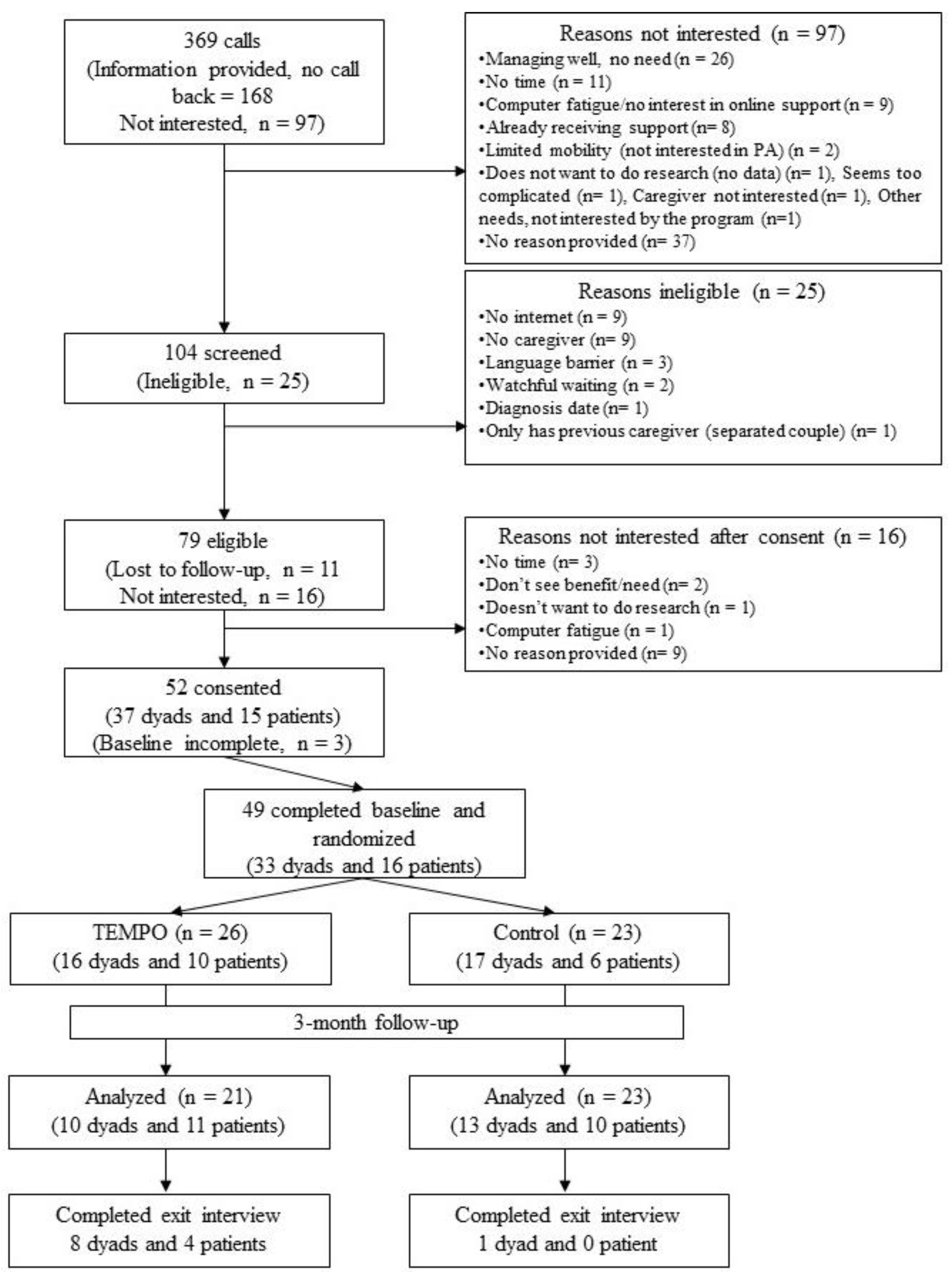
3.1. Study Participants
3.2. Feasibility
Feasibility of Cost-Utility Data Collection Methods
3.3. Acceptability
I liked that the sessions were set up in such a way that it was thought-provoking and engaging. I think sometimes when you gothrough these—like I’ve done 360 processes in business and things like that and you know, your brain starts to drift, but I felt quite engaged throughout the entire session. I thought it wasvery relevant(man, 11072–12072)
3.3.1. TEMPO Feedback Survey
Different people get on TEMPO at different stages (…) and different people fork in different ways. (…) A person could argue you need 10 different TEMPOs and that just wouldn’t be realistic. But the major branches for me would be first step diagnosis but the person has not yet made a decision about treatment. (…) And then once you’ve made a decision about treatment (…) these are all major branches where people stop having things in common(man, 81006–82006)
Going through that section (mood-monitoring tool) about how you’re feeling (…) certainly gave me some insight into how (patient) was experiencingthings. I think we have a very good relationship and we assume we’re on the same wavelength, but that’s not always the case(caregiver, 11057–12057)
3.3.2. Adherence
3.4. Primary Outcomes
3.5. Secondary Outcomes
4. Discussion
4.1. Strengths and Limitations
4.2. Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Canadian Cancer Society’s Advisory Committee on Cancer Statistics. Canadian Cancer Statistics 2016; Canadian Cancer Society: Toronto, ON, Canada, 2016. [Google Scholar]
- Msaouel, P.; Gralla, R.J.; Jones, R.A.; Hollen, P.J. Key issues affecting quality of life and patient-reported outcomes in prostate cancer: An analysis conducted in 2128 patients with initial psychometric assessment of the prostate cancer symptom scale (PCSS). BMJ Support. Palliat. Care 2017, 7, 308–315. [Google Scholar] [CrossRef]
- Regan, T.W.; Lambert, S.D.; Kelly, B.; McElduff, P.; Girgis, A.; Kayser, K.; Turner, J. Cross-sectional relationships between dyadic coping and anxiety, depression, and relationship satisfaction for patients with prostate cancer and their spouses. Patient Educ. Couns. 2014, 96, 120–127. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Isbarn, H.; Boccon-Gibod, L.; Carroll, P.R.; Montorsi, F.; Schulman, C.; Smith, M.R.; Sternberg, C.N.; Studer, U.E. Androgen Deprivation Therapy for the Treatment of Prostate Cancer: Consider Both Benefits and Risks. Eur. Urol. 2009, 55, 62–75. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hsiao, C.-P.; Loescher, L.J.; Moore, I.M.K. Symptoms and Symptom Distress in Localized Prostate Cancer. Cancer Nurs. 2007, 30, E19–E32. [Google Scholar] [CrossRef] [PubMed]
- Casey, R.G.; Corcoran, N.M.; Goldenberg, S.L. Quality of life issues in men undergoing androgen deprivation therapy: A review. Asian J. Androl. 2012, 14, 226–231. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chipperfield, K.; Fletcher, J.; Millar, J.; Brooker, J.; Smith, R.; Frydenberg, M.; Burney, S. Predictors of depression, anxiety and quality of life in patients with prostate cancer receiving androgen deprivation therapy. Psycho-Oncology 2013, 22, 2169–2176. [Google Scholar] [CrossRef] [PubMed]
- Donovan, K.A.; Walker, L.M.; Wassersug, R.J.; Thompson, L.M.A.; Robinson, J.W. Psychological effects of androgen-deprivation therapy on men with prostate cancer and their partners. Cancer 2015, 121, 4286–4299. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mazariego, C.G.; Egger, S.; King, M.T.; Juraskova, I.; Woo, H.; Berry, M.; Armstrong, B.K.; Smith, D.P. Fifteen year quality of life outcomes in men with localised prostate cancer: Population based Australian prospective study. BMJ 2020, 371, m3503. [Google Scholar] [CrossRef] [PubMed]
- Northouse, L.L.; McCorkle, R. Spouse Caregivers of Cancer Patients. In Psycho-Oncology; Oxford University Press: New York, NY, USA, 2015. [Google Scholar]
- Lambert, S.D.; Levesque, J.V.; Girgis, A. The Impact of Cancer and Chronic Conditions on Caregivers and Family Members. In Cancer and Chronic Conditions: Addressing the Problem of Multimorbidity in Cancer Patients and Survivors; Koczwara, B., Ed.; Springer: Singapore, 2016; pp. 159–202. [Google Scholar]
- Sinha, M. Spotlight on Canadians: Results from the General Social Survey. Portrait of Caregivers, 2012; Minister of Industry Canada: Ottawa, ON, Canada, 2013; pp. 1–21. Available online: https://www150.statcan.gc.ca/n1/en/pub/89-652-x/89-652-x2013001-eng.pdf?st=Fn_g-Lbt (accessed on 15 December 2014).
- McMullen, C.K.; Schneider, J.; Altschuler, A.; Grant, M.; Hornbrook, M.C.; Liljestrand, P.; Krouse, R.S. Caregivers as healthcare managers: Health management activities, needs, and caregiving relationships for colorectal cancer survivors with ostomies. Support. Care Cancer 2014, 22, 2401–2408. [Google Scholar] [CrossRef] [Green Version]
- Ellis, J.; Wagland, R.; Tishelman, C.; Williams, M.L.; Bailey, C.D.; Haines, J.; Caress, A.; Lorigan, P.; Smith, J.A.; Booton, R.; et al. Considerations in Developing and Delivering a Nonpharmacological Intervention for Symptom Management in Lung Cancer: The Views of Patients and Informal Caregivers. J. Pain Symptom Manag. 2012, 44, 831–842. [Google Scholar] [CrossRef]
- Lambert, S.D.; Girgis, A.; Lecathelinais, C.; Stacey, F. Walking a mile in their shoes: Anxiety and depression among partners and caregivers of cancer survivors at 6 and 12 months post-diagnosis. Support. Care Cancer 2013, 21, 75–85. [Google Scholar] [CrossRef] [PubMed]
- Girgis, A.; Lambert, S. Caregivers of cancer survivors: The state of the field. Cancer Forum 2009, 33, 167–171. [Google Scholar]
- Stenberg, U.; Ruland, C.M.; Miaskowski, C. Review of the literature on the effects of caring for a patient with cancer. Psycho-Oncology 2009, 19, 1013–1025. [Google Scholar] [CrossRef] [PubMed]
- Lambert, S.D.; Girgis, A.; Descallar, J.; Levesque, J.V.; Jones, B.L. Partners’ and Caregivers’ Psychological and Physical Adjustment to Cancer within the First Five Years Post Survivor Diagnosis. Psycho-Oncology 2014, 23, 77. [Google Scholar]
- Reinhard, S.C.; Given, B.; Petlick, N.H.; Bemis, A.; Hughes, R.G. Supporting Family Caregivers in Providing Care. In Patient Safety and Quality: An Evidence-Based Handbook for Nurses; Hughes, R.G., Ed.; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2008. [Google Scholar]
- Regan, T.W.; Lambert, S.D.; Girgis, A.; Kelly, B.; Kayser, K.; Turner, J. Do Couple-Based Interventions Make a Difference for Couples Affected by Cancer?: A Systematic Review. BMC Cancer 2012, 12, 279. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jones, M.C.; MacGillivray, S.; Kroll, T.; Zohoor, A.R.; Connaghan, J. A thematic analysis of the conceptualisation of self-care, self-management and self-management support in the long-term conditions management literature. J. Nurs. Health Chronic Illn. 2011, 3, 174–185. [Google Scholar] [CrossRef]
- Institute of Medicine; Board on Health Care Services; Committee on the Crossing the Quality Chasm: Next Steps Toward a New Health Care System; Adams, K.; Greiner, A.C.; Corrigan, J.M. (Eds.) The 1st Annual Crossing the Quality Chasm Summit: A Focus on Communities: Report of a Summit; The National Academies Press: Washington, DC, USA, 2004. [Google Scholar]
- Boekaerts, M.; Pintrich, P.R.; Zeider, M. Handbook of Self-Regulation; Academic Press: San Diego, CA, USA, 2000. [Google Scholar]
- McCorkle, R.; Ercolano, E.; Lazenby, M.; Schulman-Green, D.; Schilling, L.S.; Lorig, K.; Wagner, E.H. Self-management: Enabling and empowering patients living with cancer as a chronic illness. CA: A Cancer J. Clin. 2011, 61, 50–62. [Google Scholar] [CrossRef]
- Haase, K.R.; Sattar, S.; Hall, S.; McLean, B.; Wills, A.; Gray, M.; Kenis, C.; Donison, V.; Howell, D.; Puts, M. Systematic review of self-management interventions for older adults with cancer. Psycho-Oncology 2021, 30, 989–1008. [Google Scholar] [CrossRef]
- Howell, D.; Harth, T.; Brown, J.; Bennett, C.; Boyko, S. Self-management education interventions for patients with cancer: A systematic review. Support. Care Cancer 2017, 25, 1323–1355. [Google Scholar] [CrossRef]
- Northouse, L.; Williams, A.-L.; Given, B.; McCorkle, R. Psychosocial Care for Family Caregivers of Patients with Cancer. J. Clin. Oncol. 2012, 30, 1227–1234. [Google Scholar] [CrossRef]
- Beatty, L.; Lambert, S. A systematic review of internet-based self-help therapeutic interventions to improve distress and disease-control among adults with chronic health conditions. Clin. Psychol. Rev. 2013, 33, 609–622. [Google Scholar] [CrossRef]
- Northouse, L.; Schafenacker, A.; Barr, K.L.C.; Katapodi, M.; Yoon, H.; Brittain, K.; Song, L.; Ronis, D.L.; An, L. A Tailored Web-Based Psychoeducational Intervention for Cancer Patients and Their Family Caregivers. Cancer Nurs. 2014, 37, 321–330. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Badr, H.; Lipnick, D.; Diefenbach, M.A.; Posner, M.R.; Kotz, T.; Miles, B.A.; Genden, E.M. Development and usability testing of a web-based self-management intervention for oral cancer survivors and their family caregivers. Eur. J. Cancer Care 2015, 25, 806–821. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal, and Coping; Springer: New York, NY, USA, 1984. [Google Scholar]
- Stanton, A.L.; Danoff-Burg, S.; Huggins, M.E. The first year after breast cancer diagnosis: Hope and coping strategies as predictors of adjustment. Psycho-Oncology 2002, 11, 93–102. [Google Scholar] [CrossRef] [PubMed]
- Bodenmann, G. A systemic-transactional conceptualization of stress and coping in couples. Swiss J. Psychol. 1995, 54, 34–49. [Google Scholar]
- Regan, T.W.; Lambert, S.; Kelly, B.; Falconier, M.; Kissane, D.; Levesque, J.V. Couples coping with cancer: Exploration of theoretical frameworks from dyadic studies. Psycho-Oncology 2015, 24, 1605–1617. [Google Scholar] [CrossRef]
- Bandura, A. Social Foundations of Thought and Action: A Social Cognitive Theory; Prentice-Hall Inc.: Englewood Cliffs, NJ, USA, 1986; Volume xiii, p. 617. [Google Scholar]
- Hoffmann, T.C.; Glasziou, P.P.; Boutron, I.; Milne, R.; Perera, R.; Moher, D.; Altman, D.G.; Barbour, V.; Macdonald, H.; Johnston, M.; et al. Better reporting of interventions: Template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014, 348, g1687. [Google Scholar] [CrossRef] [Green Version]
- Lambert, S.D.; Duncan, L.R.; Ellis, J.; Schaffler, J.L.; Loban, E.; Robinson, J.W.; Culos-Reed, N.; Matthew, A.; Clayberg, K.; Mina, D.S.; et al. Acceptability and Usefulness of a Dyadic, Tailored, Web-Based, Psychosocial and Physical Activity Self-Management Program (TEMPO): A Qualitative Study. J. Clin. Med. 2020, 9, 3284. [Google Scholar] [CrossRef]
- Hallward, L.; Chemtob, K.; Lambert, S.D.; Duncan, L.R. Prostate Cancer Survivors’ and Caregivers’ Experiences Using Behavior Change Techniques during a Web-Based Self-Management and Physical Activity Program: A Qualitative Study. J. Clin. Med. 2020, 9, 3244. [Google Scholar] [CrossRef]
- Lambert, S.D.; Duncan, L.R.; Ellis, J.; Robinson, J.W.; Sears, C.; Culos-Reed, N.; Matthew, A.; De Raad, M.; Schaffler, J.L.; Mina, D.S.; et al. A study protocol for a multicenter randomized pilot trial of a dyadic, tailored, web-based, psychosocial, and physical activity self-management program (TEMPO) for men with prostate cancer and their caregivers. Pilot Feasibility Stud. 2021, 7, 78. [Google Scholar] [CrossRef]
- Moher, D.; Hopewell, S.; Schulz, K.F.; Montori, V.; Gøtzsche, P.C.; Devereaux, P.J.; Elbourne, D.; Egger, M.; Altman, D.G. CONSORT 2010 Explanation and Elaboration: Updated guidelines for reporting parallel group randomised trials. BMJ 2010, 340, c869. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thabane, L.; Hopewell, S.; Lancaster, G.; Bond, C.M.; Coleman, C.L.; Campbell, M.J.; Eldridge, S. Methods and processes for development of a CONSORT extension for reporting pilot randomized controlled trials. Pilot Feasibility Stud. 2016, 2, 25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [Green Version]
- Bjelland, I.; Dahl, A.A.; Haug, T.T.; Neckelmann, D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J. Psychosom. Res. 2002, 52, 69–77. [Google Scholar] [CrossRef]
- Roberge, P.; Dore, I.; Menear, M.; Chartrand, E.; Ciampi, A.; Duhoux, A.; Fournier, L. A psychometric evaluation of the French Canadian version of the Hospital Anxiety and Depression Scale in a large primary care population. J. Affect. Disord. 2013, 147, 171–179. [Google Scholar] [CrossRef] [PubMed]
- Kosinski, M.; Ware, J.E.; Turner-Bowker, D.M.; Gandek, B. User’s Manual for the SF-12v2 Health Survey: With a Supplement Documenting the SF-12® Health Survey; QualityMetric Incorporated: Lincoln, RI, USA, 2007. [Google Scholar]
- Gandek, B.; Ware, J.E.; Aaronson, N.K.; Apolone, G.; Bjorner, J.B.; Brazier, J.E.; Bullinger, M.; Kaasa, S.; Leplege, A.; Prieto, L.; et al. Cross-Validation of Item Selection and Scoring for the SF-12 Health Survey in Nine Countries: Results from the IQOLA Project. International Quality of Life Assessment. J. Clin. Epidemiol. 1998, 51, 1171–1178. [Google Scholar] [CrossRef]
- Busija, L.; Pausenberger, E.; Haines, T.; Haymes, S.; Buchbinder, R.; Osborne, R. Adult measures of general health and health-related quality of life: Medical Outcomes Study Short Form 36-Item (SF-36) and Short Form 12-Item (SF-12) Health Surveys, Nottingham Health Profile (NHP), Sickness Impact Profile (SIP), Medical Outcomes Study Sh. Arthritis Care Res. 2011, 63, S383–S412. [Google Scholar] [CrossRef] [Green Version]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A Global Measure of Perceived Stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef]
- Lee, E.-H. Review of the Psychometric Evidence of the Perceived Stress Scale. Asian Nurs. Res. 2012, 6, 121–127. [Google Scholar] [CrossRef] [Green Version]
- Lesage, F.-X.; Berjot, S.; Deschamps, F. Psychometric properties of the French versions of the Perceived Stress Scale. Int. J. Occup. Med. Environ. Health 2012, 25, 178–184. [Google Scholar] [CrossRef]
- Osborne, R.H.; Elsworth, G.R.; Whitfield, K. The Health Education Impact Questionnaire (heiQ): An outcomes and evaluation measure for patient education and self-management interventions for people with chronic conditions. Patient Educ. Couns. 2007, 66, 192–201. [Google Scholar] [CrossRef] [PubMed]
- Maunsell, E.; Lauzier, S.; Brunet, J.; Pelletier, S.; Osborne, R.H.; Campbell, H.S. Health-Related Empowerment in Cancer: Validity of Scales from the Health Education Impact Questionnaire. Cancer 2014, 120, 3228–3236. [Google Scholar] [CrossRef] [PubMed]
- Bélanger, A.; Hudon, C.; Fortin, M.; Amirall, J.; Bouhali, T.; Chouinard, M.-C. Validation of a French-language version of the health education impact Questionnaire (heiQ) among chronic disease patients seen in primary care: A cross-sectional study. Health Qual. Life Outcomes 2015, 13, 64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Osborne, R.H.; Batterham, R.W.; Elsworth, G.R.; Hawkins, M.; Buchbinder, R. The grounded psychometric development and initial validation of the Health Literacy Questionnaire (HLQ). BMC Public Health 2013, 13, 658. [Google Scholar] [CrossRef] [Green Version]
- Debussche, X.; Lenclume, V.; Balcou-Debussche, M.; Alakian, D.; Sokolowsky, C.; Ballet, D.; Elsworth, G.R.; Osborne, R.; Huiart, L. Characterisation of health literacy strengths and weaknesses among people at metabolic and cardiovascular risk: Validity testing of the Health Literacy Questionnaire. SAGE Open Med. 2018, 6, 2050312118801250. [Google Scholar] [CrossRef] [Green Version]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International Physical Activity Questionnaire: 12-Country Reliability and Validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [Green Version]
- Ajzen, I. Constructing a TpB Questionnaire: Conceptual and Methodological Considerations. 2002. Available online: https://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.601.956&rep=rep1&type=pdf (accessed on 17 March 2019).
- Rodgers, W.M.; Wilson, P.M.; Hall, C.R.; Fraser, S.N.; Murray, T.C. Evidence for a multidimensional self-efficacy for exercise scale. Res. Q. Exerc. Sport 2008, 79, 222–234. [Google Scholar] [CrossRef]
- Bodenmann, G. Dyadisches Coping Inventar: Test Manual [Dyadic Coping Inventory: Test Manual]; Huber: Bern, Switzerland, 2008. [Google Scholar]
- Feldman, B.; Broussard, C.A. The Influence of relational factors on men’s adjustment to their partners’ newly-diagnosed breast cancer. J. Psychosoc. Oncol. 2005, 23, 23–43. [Google Scholar] [CrossRef]
- Bodenmann, G.; Arista, L.J.; Walsh, K.J.; Randall, A.K. Dyadic Coping Inventory. In Encyclopedia of Couple and Family Therapy; Lebow, J., Chambers, A., Breunlin, D., Eds.; Springer: Cham, Switzerland, 2018; Available online: https://doi.org/10.1007/978-3-319-15877-8_678-1 (accessed on 26 November 2021). [CrossRef]
- Spanier, G.B. Measuring Dyadic Adjustment: New Scales for Assessing the Quality of Marriage and Similar Dyads. J. Marriage Fam. 1976, 38, 15. [Google Scholar] [CrossRef]
- Manne, S.L.; Norton, T.R.; Ostroff, J.S.; Winkel, G.; Fox, K.; Grana, G. Protective buffering and psychological distress among couples coping with breast cancer: The moderating role of relationship satisfaction. J. Fam. Psychol. 2007, 21, 380–388. [Google Scholar] [CrossRef]
- Lambert, S.D.; Girgis, A.; McElduff, P.; Turner, J.; Levesque, J.V.; Kayser, K.; Mihalopoulos, C.; Shih, S.T.F.; Barker, D. A parallel-group, randomised controlled trial of a multimedia, self-directed, coping skills training intervention for patients with cancer and their partners: Design and rationale. BMJ Open 2013, 3, e003337. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brooke, J. SUS: A ’Quick and Dirty’ Usability Scale. Usability Eval. Ind. 1996, 189, 4–7. [Google Scholar]
- Davis, F.D.; Bagozzi, R.P.; Warshaw, P.R. User Acceptance of Computer Technology: A Comparison of Two Theoretical Models. Manag. Sci. 1989, 35, 982–1003. [Google Scholar] [CrossRef] [Green Version]
- Davis, F.D. Perceived Usefulness, Perceived Ease of Use, and User Acceptance of Information Technology. MIS Q. 1989, 13, 319–340. [Google Scholar] [CrossRef] [Green Version]
- Venkatesh, V.; Morris, M.G.; Davis, G.B.; Davis, F.D. User Acceptance of Information Technology: Toward a Unified View. MIS Q. 2003, 27, 425–478. [Google Scholar] [CrossRef] [Green Version]
- SAS Institute Inc. SAS (R) University Edition; SAS Institute Inc.: Cary, NC, USA, 2015. [Google Scholar]
- StataCorp. Stata Statistical Software: Release 15; StataCorp LLC.: College Station, TX, USA, 2017. [Google Scholar]
- R Core Team. R: A Language and Environment for Statistical Computing; R Core Team: Vienna, Austria, 2020. [Google Scholar]
- Cohen, J. A power primer. Psychol. Bull. 1992, 112, 155–159. [Google Scholar] [CrossRef]
- Fitzmaurice, G.M.; Laird, N.M.; Ware, J.H. Applied Longitudinal Analysis; John Wiley & Sons Inc.: Hoboken, NJ, USA, 2014. [Google Scholar]
- Hedges, L.V. Effect sizes in nested designs. In The Handbook of Research Synthesis and Meta-Analysis; Cooper, H., Hedges, L.V., Valentine, J.C., Eds.; Russell Sage Foundation: New York, NY, USA, 2009; pp. 337–356. [Google Scholar]
- Borenstein, M.; Hedges, L.V.; Higgins, J.P.T.; Rothstein, H.R. Introduction to Meta-Analysis, 1st ed.; John Wiley & Sons Ltd.: Hoboken, NJ, USA, 2009. [Google Scholar]
- Puhan, M.A.; Frey, M.; Büchi, S.; Schünemann, H.J. The minimal important difference of the hospital anxiety and depression scale in patients with chronic obstructive pulmonary disease. Health Qual. Life Outcomes 2008, 6, 46. [Google Scholar] [CrossRef] [Green Version]
- Díaz-Arribas, M.J.; Fernández-Serrano, M.; Royuela, A.; Kovacs, F.M.; Gallego-Izquierdo, T.; San, M.-P.O.; Llorca-Palomera, R.; Pardo-Hervás, P.; Martín-Pariente, O.S. Minimal Clinically Important Difference in Quality of Life for Patients with Low Back Pain. Spine 2017, 42, 1908–1916. [Google Scholar] [CrossRef]
- QSR International Pty Ltd. NVivo (Version 12). 2018. Available online: https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home (accessed on 26 November 2021).
- Northouse, L.L.; Katapodi, M.C.; Song, L.; Zhang, L.; Mood, D.W. Interventions with Family Caregivers of Cancer Patients: Meta-Analysis of Randomized Trials. CA A Cancer J. Clin. 2010, 60, 317–339. [Google Scholar] [CrossRef] [Green Version]
- Fitch, M. Supportive care framework. Can. Oncol. Nurs. J. 2015, 18, 9. [Google Scholar] [CrossRef]
- Lambert, S.D.; Brahim, L.O.; Morrison, M.; Girgis, A.; Yaffe, M.; Belzile, E.; Clayberg, K.; Robinson, J.; Thorne, S.; Bottorff, J.L.; et al. Priorities for caregiver research in cancer care: An international Delphi survey of caregivers, clinicians, managers, and researchers. Support. Care Cancer 2018, 27, 805–817. [Google Scholar] [CrossRef]
- Thompson, T.; Ketcher, D.; Gray, T.F.; Kent, E.E. The Dyadic Cancer Outcomes Framework: A general framework of the effects of cancer on patients and informal caregivers. Soc. Sci. Med. 2021, 287, 114357. [Google Scholar] [CrossRef] [PubMed]
- Beatty, L.; Kemp, E.; Coll, J.R.; Turner, J.; Butow, P.; Milne, D.; Yates, P.; Lambert, S.; Wootten, A.; Yip, D.; et al. Finding My Way: Results of a multicentre RCT evaluating a web-based self-guided psychosocial intervention for newly diagnosed cancer survivors. Support. Care Cancer 2018, 27, 2533–2544. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Girgis, A.; Lambert, S.D.; McElduff, P.; Bonevski, B.; Lecathelinais, C.; Boyes, A.; Stacey, F. Some things change, some things stay the same: A longitudinal analysis of cancer caregivers’ unmet supportive care needs. Psycho-Oncology 2013, 22, 1557–1564. [Google Scholar] [CrossRef] [PubMed]
- Lambert, S.D.; Girgis, A. Unmet supportive care needs among informal caregivers of patients with cancer: Opportunities and challenges in informing the development of interventions. Asia-Pacific J. Oncol. Nurs. 2017, 4, 136–139. [Google Scholar] [CrossRef]
- Lambert, S.D.; Hulbert-Williams, N.; Belzile, E.; Ciampi, A.; Girgis, A. Beyond using composite measures to analyze the effect of unmet supportive care needs on caregivers’ anxiety and depression. Psycho-Oncology 2018, 27, 1572–1579. [Google Scholar] [CrossRef]
- Harrison, J.D.; Young, J.M.; Price, M.A.; Butow, P.N.; Solomon, M. What are the unmet supportive care needs of people with cancer? A systematic review. Support. Care Cancer 2009, 17, 1117–1128. [Google Scholar] [CrossRef]
- Jacobsen, P.B.; Phillips, K.M.; Jim, H.S.L.; Small, B.; Faul, L.A.; Meade, C.D.; Thompson, L.; Williams, C.C., Jr.; Loftus, L.S.; Fishman, M.; et al. Effects of self-directed stress management training and home-based exercise on quality of life in cancer patients receiving chemotherapy: A randomized controlled trial. Psycho-Oncology 2012, 22, 1229–1235. [Google Scholar] [CrossRef]
- Lambert, S.D.; Duncan, L.R.; Kapellas, S.; Bruson, A.-M.; Myrand, M.; Santa Mina, D.; Culos-Reed, N.; Lambrou, A. A descriptive systematic review of physical activity interventions for caregivers: Effects on caregivers’ and care recipients’ psychosocial outcomes, physical activity levels, and physical health. Ann. Behav. Med. 2016, 50, 907–919. [Google Scholar] [CrossRef]
- Park, C.L.; Gaffey, A.E. Relationships between psychosocial factors and health behavior change in cancer survivors: An integrative review. Ann. Behav. Med. 2007, 34, 115–134. [Google Scholar] [CrossRef]
- Pisu, M.; Demark-Wahnefried, W.; Kenzik, K.M.; Oster, R.; Lin, C.P.; Manne, S.; Alvarez, R.; Martin, M.Y. A dance intervention for cancer survivors and their partners (RHYTHM). J. Cancer Surviv. 2017, 11, 350–359. [Google Scholar] [CrossRef]
- Milbury, K.; Liao, Z.; Shannon, V.; Mallaiah, S.; Nagarathna, R.; Li, Y.; Yang, C.; Carmack, C.; Bruera, E.; Cohen, L. Dyadic yoga program for patients undergoing thoracic radiotherapy and their family caregivers: Results of a pilot randomized controlled trial. Psycho-Oncology 2019, 28, 615–621. [Google Scholar] [CrossRef] [PubMed]
- Winters-Stone, K.M.; Lyons, K.; Dobek, J.C.; Dieckmann, N.; Bennett, J.A.; Nail, L.M.; Beer, T.M. Benefits of partnered strength training for prostate cancer survivors and spouses: Results from a randomized controlled trial of the Exercising Together project. J. Cancer Surviv. 2015, 10, 633–644. [Google Scholar] [CrossRef]
- Beatty, L.; Binnion, C. A Systematic Review of Predictors of, and Reasons for, Adherence to Online Psychological Interventions. Int. J. Behav. Med. 2016, 23, 776–794. [Google Scholar] [CrossRef]
- Kenter, R.M.F.; Cuijpers, P.; Beekman, A.; Van Straten, A.; Al-Asadi, A.; Crisp, D. Effectiveness of a Web-Based Guided Self-help Intervention for Outpatients with a Depressive Disorder: Short-term Results From a Randomized Controlled Trial. J. Med. Internet Res. 2016, 18, e80. [Google Scholar] [CrossRef]
- Kleiboer, A.; Donker, T.; Seekles, W.; van Straten, A.; Riper, H.; Cuijpers, P. A randomized controlled trial on the role of support in Internet-based problem solving therapy for depression and anxiety. Behav. Res. Ther. 2015, 72, 63–71. [Google Scholar] [CrossRef]
- Day, V.; McGrath, P.; Wojtowicz, M. Internet-based guided self-help for university students with anxiety, depression and stress: A randomized controlled clinical trial. Behav. Res. Ther. 2013, 51, 344–351. [Google Scholar] [CrossRef]
- Twomey, C.; Reilly, G.O.; Byrne, M.; Bury, M.; White, A.; Kissane, S.; McMahon, A.; Clancy, N. A randomized controlled trial of the computerized CBT programme, MoodGYM, for public mental health service users waiting for interventions. Br. J. Clin. Psychol. 2014, 53, 433–450. [Google Scholar] [CrossRef] [PubMed]
- Boß, L.; Lehr, D.; Schaub, M.P.; Castro, R.P.; Riper, H.; Berking, M.; Ebert, D.D. Efficacy of a web-based intervention with and without guidance for employees with risky drinking: Results of a three-arm randomized controlled trial. Addiction 2018, 113, 635–646. [Google Scholar] [CrossRef] [Green Version]
- Lintvedt, O.K.; Griffiths, K.M.; Sørensen, K.; Østvik, A.R.; Wang, C.E.A.; Eisemann, M.; Waterloo, K. Evaluating the effectiveness and efficacy of unguided internet-based self-help intervention for the prevention of depression: A randomized controlled trial. Clin. Psychol. Psychother. 2011, 20, 10–27. [Google Scholar] [CrossRef] [PubMed]
- Northouse, L.L.; Mood, D.W.; Schafenacker, A.; Montie, J.E.; Sandler, H.M.; Forman, J.D.; Hussain, M.; Pienta, K.; Smith, D.; Kershaw, T. Randomized clinical trial of a family intervention for prostate cancer patients and their spouses. Cancer 2007, 110, 2809–2818. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Items | Description |
|---|---|
| Brief Name | Tailored, wEb-based, psychosocial and physical activity self-Management PrOgram (TEMPO) |
| Why | TEMPO aims to increase dyads’ confidence in using self-management strategies demonstrated to be effective in addressing key psychosocial issues (e.g., dealing with stress) and assist dyads in developing the self-regulatory skills necessary to meet the physical activity guidelines. |
| What (materials and procedures) | Dyads complete five modules: (a) identification of needs and priorities, (b) setting goals, (c) tracking progress and developing a coping plan, (d) strengthening support systems, and (e) maintaining behavior change beyond TEMPO. Modules focus on specific aspects of the behavior change process and integrate key persuasive technology techniques (e.g., primary task support). Each module specifies online (e.g., worksheets to set goals) and offline (e.g., practicing chosen skills) activities. In addition to modules, TEMPO includes a health library, incorporating 49 factsheets based on the most up-to-date evidence on self-management and physical activity. The health library includes eight sections: (a) communicating with your health care team, (b) treatment decision-making, (c) dealing with stress and worry, (d) supporting each other, (e) getting the support you need, (f) wanting to feel more fit and healthy, (g) getting on top of symptoms, and (h) caregiving. TEMPO is available in French and in English. |
| Who provided | TEMPO is a self-directed intervention, whereby no external guidance is provided. All the support to navigate the intervention is included in its design. |
| How | Participants randomized to TEMPO are sent an email with a brief, illustrated instructional guide on creating a TEMPO account, and on accessing the modules. They are also invited to schedule a phone call with a RA to review the registration instructions, receive support with account creation, and/or receive assistance with module access as required. Once dyads use Module 1 to identify their needs, they can use the appropriate factsheets to get ideas for self-management strategies to address these and set their goals accordingly. |
| Where | Each module becomes immediately available upon completion of the preceding module. If participants are not completing the modules at the expected pace (2 weeks per module), a maximum of two e-mail reminders are sent. |
| When and How much | As a self-directed intervention, TEMPO can be completed where participants prefer, as long as they have an internet connection. |
| Tailoring | Dyads complete a needs assessment in Module 1 and based on their answers, they can prioritize issues and set goals to work on throughout TEMPO. |
| Modifications | Following our initial acceptability study: (a) new health library content was added to help participants engage in physical activity during COVID-19-related confinement, (b) streamlining the content of the modules, and (c) instead of releasing modules every two weeks, having them available as soon as the previous one is completed. |
| Criteria | Benchmarks | Results |
|---|---|---|
| Feasibility | ||
| Recruitment rate | 8 dyads/month across sites | 6.1 dyads (or patients)/month |
| Refusal rate | <45% | 34% |
| Missing data | <10% | <10% |
| Protocol infringement | Amenable to change | None |
| Acceptability | ||
| Attrition | <25% across groups | 19% |
| Adherence | 75% of dyads adhere to modules | 45% |
| System usability (satisfaction) | High system usability reported | Above average |
| Clinical Significance | ||
| Effect size | 0.2 on the primary outcomes | Anxiety = 0.24 Quality of life—mental = 0.38 Quality of life—physical = 0.30 |
| Minimal clinically important difference improvement | 25% of participants improve on the primary outcomes by at least the minimal clinically important difference | Anxiety = yes Quality of life—mental = yes Quality of life—physical = patient no, caregiver yes |
| Characteristics | Men with Prostate Cancer | Caregivers | ||
|---|---|---|---|---|
| TEMPO (n = 26) | Control (n = 23) | TEMPO (n = 16) | Control (n = 17) | |
| n (%) | n (%) | n (%) | n (%) | |
| Age | ||||
| ≤60 | 6 (23.1) | 6 (26.1) | 4 (25.0) | 6 (35.3) |
| ≥61 | 20 (76.9) | 17 (73.9) | 12 (75.0) | 11 (64.7) |
| Sex | ||||
| Male | 26 (100) | 26 (100) | 1 (6.2) | 1 (6.2) |
| Female | 15 (93.8) | 15 (93.8) | ||
| Language | ||||
| English | 23 (88.5) | 21(91.3) | 15 (93.7) | 15 (88.2) |
| French | 0 | 1 (4.3) | 0 | 0 |
| Other | 3 (11.5) | 1 (4.3) | 1 (6.3) | 2 (11.8) |
| Country of Birth | ||||
| Canada | 20 (76.9) | 17 (73.9) | 13 (81.3) | 12 (70.6) |
| Other | 6 (23.1) | 6 (26.1) | 3 (18.7) | 5 (29.4) |
| Education | ||||
| High school or below | 0 | 2 (8.7) | 1(6.3) | 4 (23.5) |
| Post-secondary diploma | 10 (38.5) | 10 (43.5) | 4 (25.0) | 3 (17.6) |
| Undergraduate university | 6 (23.0) | 5 (21.7) | 6 (37.5) | 5 (29.4) |
| Graduate diploma | 10 (38.5) | 6 (26.1) | 5 (31.2) | 5 (29.4) |
| Employment | ||||
| Full time | 5 (19.2) | 7 (30.4) | 1 (12.5) | 2 (16.7) |
| Part time | 2 (7.7) | 1 (4.3) | 5 (62.5) | 2 (16.7) |
| Retired | 15 (57.7) | 14 (60.9) | 2 (25.0) | 7 (58.3) |
| Other | 4 (15.4) | 1 (4.3) | 0 (0.0) | 1 (8.3) |
| (Missing) | (8) | (5) | ||
| Patient-Caregiver Relationship | ||||
| Spouse/Partner | 23 (88.5) | 20 (87.0) | 16 (100) | 16 (94.1) |
| Other (friend, relative, etc.) | 3 (11.5) | 3 (13.0) | 0 | 1 (5.9) |
| Living Together | 22 (84.6) | 20 (87.0) | 15 (93.8) | 16 (94.1) |
| Marital Status | ||||
| Married/common law | 22 (84.6) | 22 (95.7) | 15 (93.8) | 17 (100.0) |
| Other | 4 (15.4) | 1 (4.3) | 1 (6.2) | 0 |
| Time Since Diagnosis | ||||
| <6 months | 1 (3.8) | 1 (4.3) | ||
| 6–12 months | 5 (19.2) | 2 (8.7) | ||
| 12–24 months | 16 (61.5) | 10 (43.5) | ||
| >24 months | 4 (15.4) | 10 (43.5) | ||
| Stages | ||||
| Early | 16 (61.5) | 14 (60.9) | ||
| Advanced | 8 (30.8) | 9 (39.1) | ||
| Don’t know | 2 (7.7) | 0 (0.0) | ||
| Treatment (can have more than one) | ||||
| Surgery | 17 (65.4) | 16 (69.6) | ||
| Chemo | 2 (7.7) | 1 (4.3) | ||
| Radio | 13 (50.0) | 5 (21.7) | ||
| Hormonal | 13 (50.0) | 9 (39.1) | ||
| Brachytherapy | 5 (19.2) | 3 (13.0) | ||
| Other | 5 (19.2) | 3 (13.0) | ||
| Outcomes | Men with Prostate Cancer | Caregivers | Combined Effect Size * | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Follow-Up | Effect Size | Baseline | Follow-Up | Effect Size | ||||||
| TEMPO (n = 26) | Control (n = 23) | TEMPO (n = 21) | Control (n = 23) | TEMPO (n = 16) | Control (n = 17) | TEMPO (n = 10) | Control (n = 13) | ||||
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ||||
| Primary Outcomes | |||||||||||
| Quality of Life | |||||||||||
| Mental | 48.0 (8.5) | 46.1 (9.2) | 49.3 (10.3) | 46.8 (10.8) | 0.23 | 52.5 (7.1) | 50.4 (9.3) | 54.7 (5.3) | 47.6 (9.6) | 0.87 | 0.38 |
| Physical | 50.2 (9.3) | 49.3 (12.2) | 52.6 (6.1) | 49.1 (12.5) | 0.35 | 52.7 (8.0) | 51.6 (7.9) | 51.1 (9.9) | 49.2 (8.6) | 0.21 | 0.30 |
| (missing) | (0) | (0) | (0) | (0) | (0) | (1) | (1) | (0) | |||
| Anxiety | 5.5 (3.4) | 6.3 (4.1) | 4.5 (4.2) | 5.3 (4.7) | 0.19 | 5.0 (4.1) | 4.6 (3.6) | 3.4 (2.8) | 4.8 (3.3) | 0.43 | 0.24 |
| (missing) | (0) | (0) | (0) | (0) | (0) | (0) | (1) | (0) | |||
| Secondary Outcomes | |||||||||||
| Depression | 3.6 (3.4) | 5.0 (4.2) | 3.7 (4.4) | 4.8 (4.3) | 0.26 | 2.3 (2.5) | 3.1 (2.2) | 1.2 (1.6) | 3.4 (3.0) | 0.88 | 0.31 |
| (missing) | (0) | (0) | (0) | (0) | (0) | (0) | (1) | (0) | |||
| Stress | 13.3 (6.2) | 13.4 (6.7) | 12.8 (7.1) | 12.4 (8.1) | 0.05 | 12.3 (7.7) | 14.7 (6.0) | 11.0 (5.5) | 12.1 (5.3) | 0.35 | 0.04 |
| (missing) | (1) | (1) | (1) | (1) | (1) | (2) | (1) | (1) | |||
| Self-Management | |||||||||||
| Positive engagement | 3.3 (0.5) | 3.1 (0.6) | 3.4 (0.6) | 3.2 (0.6) | 0.33 | 3.4 (0.4) | 3.1 (0.4) | 3.4 (0.5) | 3.1 (0.4) | 0.90 | 0.46 |
| Skill acquisition | 3.0 (0.4) | 3.1 (0.4) | 3.3 (0.4) | 3.1 (0.5) | 0.44 | 3.1 (0.5) | 2.5 (0.4) | 2.9 (0.4) | 2.6 (0.4) | 0.75 | 0.48 |
| Constructive attitudes | 3.4 (0.5) | 3.3 (0.7) | 3.4 (0.6) | 3.3 (0.7) | 0.15 | 3.3 (0.4) | 3.0 (0.4) | 3.3 (0.4) | 3.3 (0.4) | 0.00 | 0.14 |
| Self-monitoring | 3.3 (0.3) | 3.2 (0.4) | 3.4 (0.4) | 3.3 (0.4) | 0.25 | 3.3 (0.4) | 2.9 (0.5) | 3.2 (0.4) | 3 (0.5) | 0.43 | 0.29 |
| Health services navigation | 3.3 (0.4) | 3.4 (0.5) | 3.3 (0.5) | 3.4 (0.6) | −0.18 | 3.2 (0.4) | 2.7 (0.4) | 3.1 (0.1) | 2.6 (0.7) | 0.92 | 0.26 |
| Social integration and support | 3.1 (0.5) | 3.1 (0.6) | 3.2 (0.6) | 3.1 (0.6) | 0.17 | 3.1 (0.5) | 2.7 (0.6) | 3.1 (0.8) | 2.6 (0.6) | 0.73 | 0.34 |
| (missing) | (0) | (0) | (1) | (1) | (2) | (7) | (1) | (0) | |||
| Health Literacy | |||||||||||
| Sufficient information | 3.0 (0.5) | 3.0 (0.6) | 3.1 (0.5) | 3.1 (0.6) | 0.00 | 3.2 (0.5) | 3.2 (0.5) | 3.4 (0.5) | 3.1 (0.7) | 0.48 | 0.04 |
| Actively managing | 3.1 (0.6) | 3.1 (0.4) | 3.2 (0.5) | 3.1 (0.5) | 0.20 | 3.2 (0.5) | 3.1 (0.6) | 3.4 (0.6) | 3.0 (0.7) | 0.61 | 0.38 |
| (missing) | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) | |||
| Physical Activity (MET) | 1894 (1919) | 2365 (3313) | 2521 (1471) | 2253 (1969) | 0.17 | 1953 (2210) | 1410 (1082) | 2020 (1812) | 1713 (1870) | 0.17 | 0.15 |
| Physical Activity Plan | 4.2 (2.1) | 3.7 (2.2) | 4.7 (2.0) | 3.5 (1.8) | 0.63 | 4.8 (2.0) | 4.3 (1.9) | 5.0 (1.4) | 4.6 (1.9) | 0.24 | 0.48 |
| (missing) | (1) | (2) | (1) | (1) | (1) | (2) | (1) | (2) | |||
| Physical Activity Intention | 4.6 (2.0) | 3.9 (2.1) | 4.8 (1.7) | 4.1 (1.5) | 0.44 | 5.2 (1.8) | 4.8 (1.9) | 4.9 (1.2) | 4.4 (1.5) | 0.36 | 0.38 |
| (missing) | (3) | (3) | (1) | (1) | (3) | (4) | (3) | (4) | |||
| Physical Activity Self-Efficacy | 73.0 (21.5) | 66.2 (20.4) | 78.5 (16.5) | 61.6 (26.2) | 0.76 | 75.7 (20.1) | 70.9 (16.6) | 81.2 (13.9) | 68.1 (21.3) | 0.71 | 0.72 |
| (missing) | (4) | (2) | (1) | (1) | (1) | (2) | (1) | (1) | |||
| Dyadic Coping | 124.9 (24.7) | 128.0 (19.5) | 132.8 (14.8) | 121.5 (21.5) | 0.61 | 136 (22.1) | 121.5 (18.8) | 135.2 (19.3) | 126.1 (17.1) | 0.50 | 0.63 |
| (missing) | (4) | (2) | (1) | (1) | (1) | (2) | (1) | (2) | |||
| Dyadic Adjustment | 49.4 (12.2) | 47.9 (7.5) | 53.2 (6.4) | 51.0 (8.2) | 0.30 | 54.5 (9.2) | 48.5 (6.7) | 54.7 (7.6) | 51.3 (5.5) | 0.57 | 0.36 |
| (missing) | (7) | (6) | (9) | (11) | (6) | (6) | (7) | (4) | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lambert, S.D.; Duncan, L.R.; Culos-Reed, S.N.; Hallward, L.; Higano, C.S.; Loban, E.; Katz, A.; De Raad, M.; Ellis, J.; Korman, M.B.; et al. Feasibility, Acceptability, and Clinical Significance of a Dyadic, Web-Based, Psychosocial and Physical Activity Self-Management Program (TEMPO) Tailored to the Needs of Men with Prostate Cancer and Their Caregivers: A Multi-Center Randomized Pilot Trial. Curr. Oncol. 2022, 29, 785-804. https://doi.org/10.3390/curroncol29020067
Lambert SD, Duncan LR, Culos-Reed SN, Hallward L, Higano CS, Loban E, Katz A, De Raad M, Ellis J, Korman MB, et al. Feasibility, Acceptability, and Clinical Significance of a Dyadic, Web-Based, Psychosocial and Physical Activity Self-Management Program (TEMPO) Tailored to the Needs of Men with Prostate Cancer and Their Caregivers: A Multi-Center Randomized Pilot Trial. Current Oncology. 2022; 29(2):785-804. https://doi.org/10.3390/curroncol29020067
Chicago/Turabian StyleLambert, Sylvie D., Lindsay R. Duncan, S. Nicole Culos-Reed, Laura Hallward, Celestia S. Higano, Ekaterina Loban, Anne Katz, Manon De Raad, Janet Ellis, Melissa B. Korman, and et al. 2022. "Feasibility, Acceptability, and Clinical Significance of a Dyadic, Web-Based, Psychosocial and Physical Activity Self-Management Program (TEMPO) Tailored to the Needs of Men with Prostate Cancer and Their Caregivers: A Multi-Center Randomized Pilot Trial" Current Oncology 29, no. 2: 785-804. https://doi.org/10.3390/curroncol29020067





