The Economic Burden of Cancer in Canada from a Societal Perspective
Abstract
1. Introduction
2. Materials and Methods
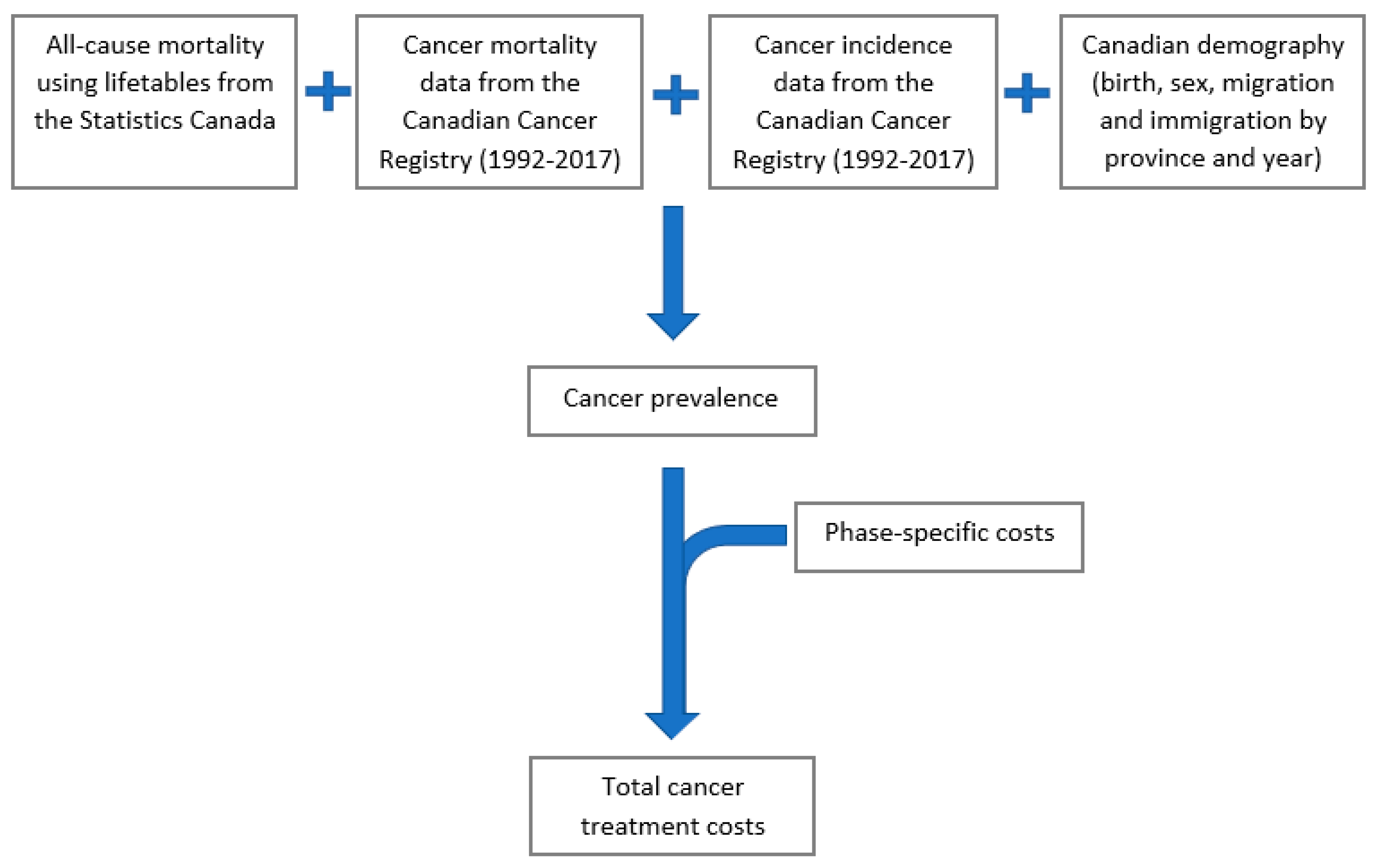
2.1. OncoSim Model Overview
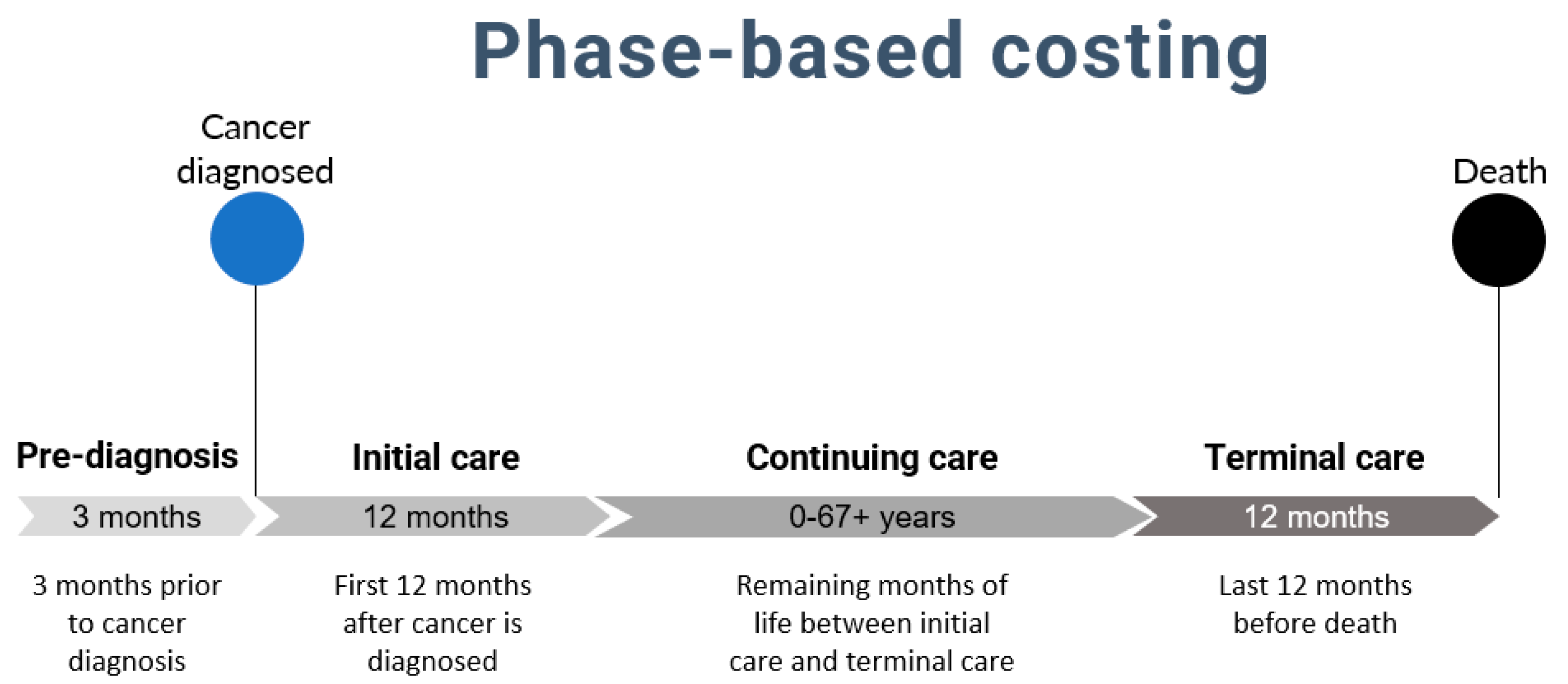
2.2. Conceptual Framework
2.3. Data Sources
2.4. Assumptions
2.5. Base Case Analysis
2.6. Sensitivity Analyses
3. Results
Cancer Costs by Sex and Cancer Site
4. Discussion
4.1. Strengths and Limitations
4.2. Future Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- The Public Health Agency of Canada. Release notice—Canadian Cancer Statistics 2021. Health Promot. Chronic Dis. Prev. Can. 2021, 41, 399. [Google Scholar] [CrossRef]
- de Oliveira, C.; Bremner, K.E.; Pataky, R.; Gunraj, N.; Haq, M.; Chan, K.; Cheung, W.Y.; Hoch, J.S.; Peacock, S.; Krahn, M.D. Trends in use and cost of initial cancer treatment in Ontario: A population-based descriptive study. Can. Med. Assoc. J. 2013, 1, 151–158. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Landwehr, M.S.; Watson, S.E.; Macpherson, C.F.; Novak, K.A.; Johnson, R.H. The cost of cancer: A retrospective analysis of the financial impact of cancer on young adults. Cancer Med. 2016, 5, 863–870. [Google Scholar] [CrossRef] [PubMed]
- Mahon, K. The Financial Impact of Cancer in Canadian Young Adults. Master’s Thesis, Memorial University of Newfoundland, St. John’s, NL, Canada, 2020. [Google Scholar]
- de Oliveira, C.; Bremner, K.E.; Pataky, R.; Gunraj, N.; Haq, M.; Chan, K.; Cheung, W.Y.; Hoch, J.S.; Peacock, S.; Krahn, M.D. The economic burden of cancer care in Canada: A population-based cost study. Can. Med. Assoc. J. 2018, 6, E1–E10. [Google Scholar] [CrossRef]
- Iragorri, N.; de Oliveira, C.; Fitzgerald, N.; Essue, B.M. The indirect cost burden of cancer care in Canada: A systematic literature review. Appl. Health Econ. Health Policy 2021, 19, 325–341. [Google Scholar] [CrossRef]
- Iragorri, N.; de Oliveira, C.; Fitzgerald, N.; Essue, B.M. The out-of-pocket cost burden of cancer care—A systematic literature review. Curr. Oncol. 2021, 28, 1216–1248. [Google Scholar] [CrossRef]
- Essue, B.M.; Iragorri, N.; Fitzgerald, N.; de Oliveira, C. The psychosocial cost burden of cancer: A systematic literature review. Psycho-oncology 2020, 29, 1746–1760. [Google Scholar] [CrossRef]
- Longo, C.J.; Fitch, M.I.; Loree, J.M.; Carlson, L.E.; Turner, D.; Cheung, W.Y.; Gopaul, D.; Ellis, J.; Ringash, J.; Mathews, M.; et al. Patient and family financial burden associated with cancer treatment in Canada: A national study. Support Care Cancer 2021, 29, 3377–3386. [Google Scholar] [CrossRef]
- de Oliveira, C.; Pataky, R.; Bremner, K.E.; Rangrej, J.; Chan, K.K.W.; Cheung, W.Y.; Hoch, J.S.; Peacock, S.; Krahn, M.D. Phase-specific and lifetime costs of cancer care in Ontario, Canada. BMC Cancer 2016, 16, 809. [Google Scholar] [CrossRef]
- Yabroff, K.R.; Lamont, E.B.; Mariotto, A.; Warren, J.L.; Topor, M.; Meekins, A.; Brown, M.L. Cost of care for elderly cancer patients in the United States. J. Natl. Cancer Inst. 2008, 100, 630–641. [Google Scholar] [CrossRef]
- Yabroff, K.R.; Warren, J.L.; Knopf, K.; Davis, W.W.; Brown, M.L. Estimating patient time costs associated with colorectal cancer care. Med. Care 2005, 43, 640–648. [Google Scholar] [CrossRef] [PubMed]
- Yabroff, K.R.; Mariotto, A.; Tangka, F.; Zhao, J.; Islami, F.; Sung, H.; Sherman, R.L.; Henley, S.J.; Jemal, A.; Ward, E.M. Annual report to the nation on the status of cancer, part 2: Patient economic burden associated with cancer care. J. Natl. Cancer Inst. 2021, 113, 1670–1682. [Google Scholar] [CrossRef] [PubMed]
- Pisu, M.; Azuero, A.; McNees, P.; Burkhardt, J.; Benz, R.; Meneses, K. The out of pocket cost of breast cancer survivors: A review. J. Cancer Surviv. 2010, 4, 202–209. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira, C.; Bremner, K.E.; Ni, A.; Alibhai, S.M.H.; Laporte, A.; Krahn, M.D. Patient time and out-of-pocket costs for long-term prostate cancer survivors in Ontario, Canada. J. Cancer Surviv. 2014, 8, 9–20. [Google Scholar] [CrossRef] [PubMed]
- Dumont, S.; Jacobs, P.; Turcotte, V.; Turcotte, S.; Johnston, G. Palliative care costs in Canada: A descriptive comparison of studies of urban and rural patients near end of life. Palliat. Med. 2015, 29, 908–917. [Google Scholar] [CrossRef] [PubMed]
- Statistics Canada. Table 14-10-0134-01. Average Weekly Earnings, Average Hourly Wage Rate and Average Usual Weekly Hours by Union Status, Annual. Available online: https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1410013401 (accessed on 12 January 2022).
- Jeon, S.H. The long-term effects of cancer on employment and earnings. J. Health Econ. 2017, 26, 671–684. [Google Scholar] [CrossRef]
- Ferrell, B.R.; Temel, J.S.; Temin, S.; Alesi, E.R.; Balboni, T.A.; Basch, E.M.; Firn, J.I.; Paice, J.A.; Peppercorn, J.M.; Phillips, T.; et al. Integration of palliative care into standard oncology care: American society of clinical oncology clinical practice guideline update. J. Clin. Oncol. 2017, 35, 96–112. [Google Scholar] [CrossRef]
- Temel, J.S.; Greer, J.A.; Muzikansky, A.; Gallagher, E.R.; Admane, S.; Jackson, V.A.; Dahlin, C.M.; Blinderman, C.D.; Jacobsen, J.; Pirl, W.F.; et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N. Engl. J. Med. 2010, 363, 733–742. [Google Scholar] [CrossRef]
- Statistics Canada. Table 18-10-0004-13 Consumer Price Index by Product Group, Monthly, Percentage Change, Not Seasonally Adjusted, Canada, Provinces, Whitehorse, Yellowknife, and Iqaluit. Available online: https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1810000413&pickMembers%5B0%5D=1.2&cubeTimeFrame.startMonth=10&cubeTimeFrame.startYear=2021&referencePeriods=20211001%2C20211001 (accessed on 12 January 2022).
- Statistics Canada. Table 14-10-0060-01. Retirement Age by Class of Worker, Annual. Available online: https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1410006001 (accessed on 12 January 2022).
- Bradley, C.J.; Neumark, D.; Luo, Z.; Bednarek, H.; Schenk, M. Employment outcomes of men treated for prostate cancer. J. Natl. Cancer Inst. 2005, 97, 958–965. [Google Scholar] [CrossRef]
- Nieuwenhuijsen, K.; Bos-Ransdorp, B.; Uitterhoeve, L.L.J.; Sprangers, M.A.G.; Verbeek, J.H.A.M. Enhanced provider communication and patient education regarding return to work in cancer survivors following curative treatment: A pilot study. J. Occup. Rehabil. 2006, 16, 647–657. [Google Scholar] [CrossRef]
- Baker, M.S.; Kessler, L.G.; Urban, N.; Smucker, R.C. Estimating the treatment costs of breast and lung cancer. Med. Care 1991, 29, 40–49. [Google Scholar] [CrossRef] [PubMed]
- Yu, M.; Guerriere, D.N.; Coyte, P.C. Societal costs of home and hospital end-of-life care for palliative care patients in Ontario, Canada. Health Soc. Care Community 2015, 23, 605–618. [Google Scholar] [CrossRef] [PubMed]
- Public Health Agency of Canada. Economic Burden of Illness in Canada, 2005–2008; Public Health Agency of Canada: Ottawa, ON, Canada, 2014.
- Jung, Y.L.; Tompa, E.; Longo, C.; Kalcevich, C.; Kim, J.; Song, C.; Demers, P. The economic burden of bladder cancer due to occupational exposure. J. Occup. Environ. Med. 2018, 60, 217–225. [Google Scholar] [CrossRef] [PubMed]
- Canadian Partnership Against Cancer. The Economic Burden of Skin Cancer in Canada: Current and Projected Final Report; Canadian Partnership Against Cancer: Toronto, ON, Canada, 2010. [Google Scholar]
- Ontario Lung Association. Life and Economic Burden of Lung Disease in Ontario: 2011 to 2041. 2011. Available online: https://books.google.ca/books/about/Life_and_Economic_Burden_of_Lung_Disease.html?id=nppcAQAACAAJ&redir_esc=y (accessed on 17 January 2022).
- Mofidi, A.; Tompa, E.; Spencer, J.; Kalcevich, C.; Peters, C.E.; Kim, J.; Song, C.; Mortazavi, S.B.; Demers, P.A. The economic burden of occupational non-melanoma skin cancer due to solar radiation. J. Occup. Environ. Hyg. 2018, 15, 481–491. [Google Scholar] [CrossRef]
- Longo, C.J.; Fitch, M.; Deber, R.B.; Williams, A.P. Financial and family burden associated with cancer treatment in Ontario, Canada. Support Care Cancer 2006, 14, 1077–1085. [Google Scholar] [CrossRef]
- Athas, W.F.; Adams-Cameron, M.; Hunt, W.C.; Amir-Fazli, A.; Key, C.R. Travel distance to radiation therapy and receipt of radiotherapy following breast-conserving surgery. J. Natl. Cancer Inst. 2000, 92, 269–271. [Google Scholar] [CrossRef]
- Brown, M.L.; Lipscomb, J.; Snyder, C. The burden of illness in cancer: Economic cost and quality of life. Ann. Rev. Public Health 2001, 22, 91–113. [Google Scholar] [CrossRef]


| Cancer Treatment Care Phase | |||||
|---|---|---|---|---|---|
| Pre-Diagnosis (3 Months) | Initial Care (12 Months) | Continuing Care (Annual/12 Months) | Terminal Care (12 Months) | Total | |
| Direct Health System Costs | 1612 a | 28,891 a | 6070 a | 52,861 a | 89,434 |
| Direct Out-of-Pocket Costs | 0 | 10,649 b | 264 c | 2868 d | 13,781 |
| Direct Time Costs | 0 | 5774 e | 375 e | 3504 e | 9653 |
| Indirect Costs | 0 | 5923 f | 664 f | 5923 f | 12,510 |
| Total | 1612 | 51,237 | 7373 | 65,156 | 125,378 |
| Pre-Diagnosis | Initial Care | Continuing Care | Terminal Care | ||
|---|---|---|---|---|---|
| Best-case | Direct Health System Costs | Base case estimates | Base case estimates | Base case estimates | Base case estimates |
| Direct Out-of-Pocket Costs | Base case estimates | Estimates were decreased by 40%. | Base case estimates | Estimates were decreased by 40%. | |
| Direct Time Costs | Base case estimates | Hourly wage decreased to CAD 15.00 | Hourly wage decreased to CAD 15.00 | Hourly wage decreased to CAD 15.00 | |
| Indirect Costs | Base case estimates | Base case estimates | Costs were extended for a maximum of two years. For cancer sites where average life expectancies were greater than 60 years, costs were set to zero for individuals over 60. | Base case estimates | |
| Worst-case | Direct Health System Costs | Base case estimates | Base case estimates | No time limit on receiving additional medical care (base-case limit is 10 years). | Base case estimates |
| Direct Out-of-Pocket Costs | Base case estimates | Estimates were increased by 40%. | Base case estimates | Estimates were increased by 40%. | |
| Direct Time Costs | Base case estimates | Hourly wage increased to CAD 31.14. | Hourly wage increased to CAD 31.14. | Hourly wage increased to CAD 31.14. | |
| Indirect Costs | Base case estimates | Estimates were increased by 20%. | Costs were extended for a maximum of four years. For cancer sites where average life expectancies were greater than 70 years, costs were set to zero for individuals over 70. | Estimates were increased by 20%. |
| Pre-Diagnosis | Initial Care | Continuing Care | Terminal Care | Total | ||
|---|---|---|---|---|---|---|
| Worst-Case | Direct Health System Costs | 321 M | 5599 M | 12,575 M | 4359 M | 22,854 M |
| Direct Out-of-Pocket Costs | 0 | 3273 M | 491 M | 354 M | 4118 M | |
| Direct Time Costs | 0 | 2062 M | 1133 M | 502 M | 3698 M | |
| Indirect Costs | 0 | 2097 M | 2809 M | 850 M | 5755 M | |
| Total | 321 M | 12,096 M | 17,008 M | 5964 M | 35,389 M | |
| Base Case | Direct Health System Costs | 321 M | 5599 M | 8137 M | 4359 M | 18,415 M |
| Direct Out-of-Pocket Costs | 0 | 2338 M | 491 M | 253 M | 3082 M | |
| Direct Time Costs | 0 | 1267 M | 439 M | 309 M | 2016 M | |
| Indirect Costs | 0 | 1216 M | 1002 M | 465 M | 2684 M | |
| Total | 321 M | 10,420 M | 10,069 M | 5386 M | 26,196 M | |
| Best-Case | Direct Health System Costs | 321 M | 5599 M | 8137 M | 4359 M | 18,415 M |
| Direct Out-of-Pocket Costs | 0 | 1403 M | 491 M | 152 M | 2045 M | |
| Direct Time Costs | 0 | 993 M | 344 M | 242 M | 1579 M | |
| Indirect Costs | 0 | 442 M | 320 M | 174 M | 937 M | |
| Total | 321 M | 9372 M | 9292 M | 5028 M | 24,013 M |
| Direct Health System Costs | Direct Out-of-Pocket Costs | Direct Time Costs | Indirect Costs | |
|---|---|---|---|---|
| Oral cavity | 211 M | 33 M | 22 M | 40 M |
| Oropharynx | 96 M | 16 M | 10 M | 20 M |
| Hypopharynx | 22 M | 3 M | 2 M | 1 M |
| Other oral | 124 M | 18 M | 12 M | 23 M |
| Esophagus | 293 M | 32 M | 22 M | 28 M |
| Stomach | 377 M | 50 M | 36 M | 47 M |
| Colorectal | 2468 M | 364 M | 251 M | 107 M |
| Liver | 278 M | 40 M | 27 M | 116 M |
| Pancreas | 651 M | 78 M | 53 M | 53 M |
| Larynx | 116 M | 17 M | 12 M | 5 M |
| Lung | 2713 M | 419 M | 291 M | 243 M |
| Melanoma | 363 M | 116 M | 70 M | 121 M |
| Breast | 2141 M | 393 M | 235 M | 417 M |
| Cervix | 81 M | 24 M | 13 M | 29 M |
| Body of uterus | 353 M | 99 M | 61 M | 105 M |
| Ovary | 264 M | 40 M | 29 M | 166 M |
| Prostate | 1514 M | 356 M | 226 M | 99 M |
| Testis | 49 M | 19 M | 9 M | 21 M |
| Bladder | 720 M | 161 M | 108 M | 38 M |
| Kidney | 500 M | 98 M | 64 M | 115 M |
| Brain/CNS | 498 M | 42 M | 30 M | 190 M |
| Thyroid | 248 M | 95 M | 49 M | 96 M |
| Hodgkin lymphoma | 101 M | 19 M | 9 M | 20 M |
| Non-Hodgkin lymphoma | 968 M | 134 M | 90 M | 108 M |
| Multiple myeloma | 510 M | 44 M | 31 M | 38 M |
| Leukemias | 879 M | 91 M | 62 M | 330 M |
| Vulva | 64 M | 10 M | 7 M | 3 M |
| Vagina | 19 M | 3 M | 2 M | 1 M |
| Anal | 68 M | 10 M | 7 M | 13 M |
| Penile | 24 M | 3 M | 2 M | 1 M |
| Other cancer | 1701 M | 256 M | 175 M | 75 M |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Garaszczuk, R.; Yong, J.H.E.; Sun, Z.; de Oliveira, C. The Economic Burden of Cancer in Canada from a Societal Perspective. Curr. Oncol. 2022, 29, 2735-2748. https://doi.org/10.3390/curroncol29040223
Garaszczuk R, Yong JHE, Sun Z, de Oliveira C. The Economic Burden of Cancer in Canada from a Societal Perspective. Current Oncology. 2022; 29(4):2735-2748. https://doi.org/10.3390/curroncol29040223
Chicago/Turabian StyleGaraszczuk, Roxanne, Jean H. E. Yong, Zhuolu Sun, and Claire de Oliveira. 2022. "The Economic Burden of Cancer in Canada from a Societal Perspective" Current Oncology 29, no. 4: 2735-2748. https://doi.org/10.3390/curroncol29040223
APA StyleGaraszczuk, R., Yong, J. H. E., Sun, Z., & de Oliveira, C. (2022). The Economic Burden of Cancer in Canada from a Societal Perspective. Current Oncology, 29(4), 2735-2748. https://doi.org/10.3390/curroncol29040223





