Striving to Fill in Gaps between Clinical Practice and Standards: The Evolution of a Pan-Canadian Approach to Patient-Reported Outcomes Use
Abstract
1. Introduction
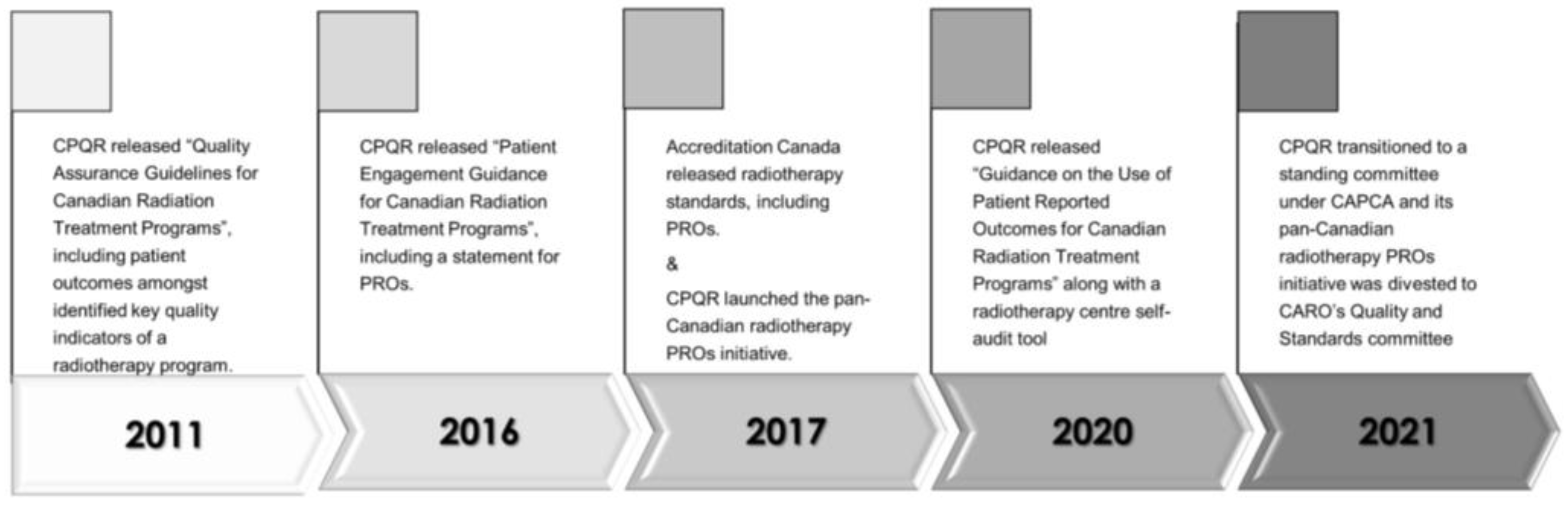
2. Development of the Canadian Partnership for Quality Radiotherapy (CPQR)’s PROs Initiative
3. CPQR’s PRO Guidance Developed
4. The Patient Voice in PROs
5. Expansion of PROs across Canadian Radiotherapy Centres
6. PROs Collection and Use in the Era of COVID-19
7. The Future of the Pan-Canadian PROs Initiative
8. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Greenhalgh, J. The Application of PROs in Clinical Practice: What are they, Do they Work, and Why? Qual. Life Res. 2009, 18, 115–123. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.L.; Manhas, D.; Howard, F.; Olson, R. Patient-Reported Outcome use in Oncology: A Systematic Review of the Impact on Patient-Clinician Communication. Support. Care Cancer 2017, 26, 41–60. [Google Scholar] [CrossRef] [PubMed]
- Siddiqui, F.; Liu, A.K.; Watkins-Bruner, D.; Movsas, B. Patient-Reported Outcomes and Survivorship in Radiation Oncology: Overcoming the Cons. J. Clin. Oncol. 2014, 32, 2920–2927. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Basch, E.; Deal, A.M.; Kris, M.G.; Scher, H.I.; Hudis, C.A.; Sabbatini, P.; Rogak, L.; Bennett, A.V.; Dueck, A.C.; Atkinson, T.M.; et al. Symptom Monitoring with Patient-Reported Outcomes During Routine Cancer Treatment: A Randomized Controled Trial. J. Clin. Oncol. 2016, 34, 557–565. [Google Scholar] [CrossRef]
- Lalani, N.; Cummings, B.; Halperin, R.; Rakovitch, E.; Brundage, M.; Vigneault, E.; Milosevic, M. The Practice of Radiation Oncology in Canada. Int. J. Radiat. Oncol. Biol. Phys. 2017, 97, 876–880. [Google Scholar] [CrossRef]
- Brown, E.; Milosevic, M. Quality in Cancer Care—Lessons from the Canadian Partnership for Quality Radiotherapy. Healthc. Manag. Forum 2017, 31, 18–21. [Google Scholar] [CrossRef]
- Caissie, A.; Brown, E.; Olson, R.; Barbera, L.; Davis, C.; Brundage, M.; Milosevic, M. Improving Patient Outcomes and Radiotherapy Systems: A Pan-Canadian Approach to Patient-Reported Outcome Use. Med. Phys. 2018, 45, e841–e844. [Google Scholar] [CrossRef]
- The Quality Assurance Guidelines for Canadian Radiation Treatment Program. 2019. Available online: http://www.cpqr.ca/wp-content/uploads/2020/03QRT2019-12-04.pdf (accessed on 7 March 2022).
- People Powered Health. Available online: https://accreditation.ca (accessed on 7 March 2022).
- Canadian Partnership for Quality Radiotherapy. Guidance on the Use of Patient Reported Outcomes for Canadian Radiation Treatment Programs. Available online: http://www.cpqr.ca/wp-content/uploads/2020/09/PRO.2020.09.01.pdf (accessed on 7 March 2022).
- Patient Reported Outcomes. Canadian Partnership for Quality Radiotherapy. Available online: http://www.cpqr.ca/programs/patient-reported-outcomes/ (accessed on 7 March 2022).
- Canadian Partnership for Quality Radiotherapy. Patient Engagement Guidance for Canadian Radiation Treatment Programs. Available online: https://www.cpqr.ca/wp-content/uploads/2020/04/PEG.2016.06.01-1.pdf (accessed on 7 March 2022).
- Montgomery, N.; Howell, D.; Ismail, Z.; Bartlett, S.J.; Brundage, M.; Bryant-Lukosius, D.; Krzyzanowska, M.; Moody, L.; Snyder, C.; Barbera, L.; et al. Selecting, Implementing and Evaluating Patient-Reported Outcome Measures for Routine Clinical Use in Cancer: The Cancer Care Ontario Approach. Journal of Patient-Reported Outcomes. J. Oncol. Pract. 2020, 4, 101. [Google Scholar]
- Pereira, J.; Green, E.; Molloy, S.; Dudgeon, D.; Howell, D.; Krzyzanowska, M.K.; Mahase, W.; Tabing, R.; Urowitz, S.; Macdougall, L. Population-Based Standardized Symptom Screening: Cancer Care Ontario’s Edmonton Symptom Assessment System and Performance Status Initiatives. J. Oncol. Pract. 2014, 10, 212–214. [Google Scholar] [CrossRef]
- Barbera, L.; Sutradhar, R.; Seow, H.; Mittmann, N.; Howell, D.; Earle, C.C.; Li, Q.; Thiruchelvam, D. The Impact of Routine Edmonton Symptom Assessment System (ESAS) Use on Overall Survival in Cancer Patients: Results of a Population-Based Retrospective Matched Cohort Analysis. Cancer Med. 2020, 9, 7107–7115. [Google Scholar] [CrossRef]
- Barbera, L.; Sutradhar, R.; Earle, C.C.; Howell, D.; Mittman, N.; Li, Q.; Thiruchelvam, D.; Seow, H. The Impact of Routine Edmonton Symptom Assessment System Use on Receiving Palliative Care Services: Results of a Population-Based Retrospective-Matched Cohort Analysis. BMJ Support. Palliat. Care 2020, 17. [Google Scholar] [CrossRef] [PubMed]
- Gascon, B.; Leung, Y.; Espin-Garcia, O.; Rodin, G.; Chu, D.; Li, M. Suicide Risk Screening and Suicide Prevention in Patients with Cancer. JNCI Cancer Spectr. 2021, 5, pkab057. [Google Scholar] [CrossRef] [PubMed]
- Barbera, L.; Sutradhar, R.; Seow, H.; Earle, C.C.; Howell, D.; Mittmann, N.; Li, Q.; Thiruchelvam, D. Impact of Standardized Edmonton Symptom Assessment System Use on Emergency Department Visits and Hospitalization: Results of a Population-Based Retrospective Matched Cohort Analysis. JCO Oncol. Pract. 2020, 16, e958–e965. [Google Scholar] [CrossRef] [PubMed]
- Howell, D.; Rosberger, Z.; Mayer, C.; Faria, R.; Hamel, M.; Snider, A.; Lukosius, D.B.; Montgomery, N.; Mozuraitis, M.; Li, M.; et al. Personalized Symptom Management: A Quality Improvement Collaborative for Implementation of Patient Reported Outcomes (PROs) in ‘Real-World’ Oncology Multisite Practices. J. Patient-Rep. Outcomes 2020, 4, 1–13. [Google Scholar] [CrossRef]
- Brundage, M.; Barbera, L.; McCallum, F.; Howell, D. A pilot Evaluation of the Expanded Prostate Cancer Index Composite for Clinical Practice (EPIC-CP) tool in Ontario. Qual. Life Res. 2019, 28, 771–782. [Google Scholar] [CrossRef]
- Atallah, S.; Barbera, L.; Folwell, M.; Howell, D.; Liu, Z.; Croke, J. Feasibility of Implementing a Cervix Cancer–Specific Patient-Reported Outcome Measure in Routine Ambulatory Clinics. Support. Care Cancer 2021, 29, 499–507. [Google Scholar] [CrossRef]
- Kildea, J.; Battista, J.; Cabral, B.; Hendren, L.; Herrera, D.; Hijal, T.; Joseph, A. Design and Development of a Person-Centered Patient Portal Using Participatory Stakeholder Co-Design. J. Med. Internet Res. 2019, 21, e11371. [Google Scholar] [CrossRef]
- Olson, R.A.; Howard, F.; Lapointe, V.; Schellenberg, D.; Nichol, A.; Bowering, G.; Curtis, S.; Walter, A.; Brown, S.; Thompson, C.; et al. Provincial Development of a Patient-Reported Outcome Initiative to Guide Patient Care, Quality Improvement and Research. Healthc. Manag. Forum 2018, 31, 13–17. [Google Scholar] [CrossRef]
- Howard, A.; Medhurst, K.; Manhas, D.; Manhas, D.S.; Yang, L.Y.; Brown, S.; Brown, E.; Olson, R.A. The Usefulness of Patient-Reported Outcomes and the Influence on Palliative Oncology Patients and Health Services: A qualitative Study of the Prospective Outcomes and Support Initiative. Cancer Nurs. 2020, 44, 388–397. [Google Scholar] [CrossRef]
- Hamilton, S.N.; Tran, E.; Ho, C.; Berthelet, E.; Wu, J.; DeVries, K.; LaPointe, V.; Bowman, A.; Lagman, M.; Olson, R. Patient-Reported Outcome Measures in Patients Undergoing Radiotherapy for Head and Neck Cancer. Support. Care Cancer 2021, 29, 2537–2547. [Google Scholar] [CrossRef]
- Conway, J.L.; Yurkowski, E.; Glazier, J.; Gentles, Q.; Walter, A.; Bowering, G.; Curtis, S.; Schellenberg, D.; Halperin, R.; Lapointe, V.; et al. Comparison of Patient-Reported Outcomes with Single Versus Multiple Fraction Palliative Radiotherapy for Bone Metastasis in a Population-Based Cohort. Radiother. Oncol. 2016, 119, 202–207. [Google Scholar] [CrossRef] [PubMed]
- Sit, D.; Zhao, B.; Chen, K.T.; Lohrisch, C.; Olson, R.; Nichol, A.; Hsu, F. The Effect of Breast Cancer Subtype on Symptom Improvement Following Palliative Radiotherapy for Bone Metastases. Clin. Oncol. 2021, 34, 267–273. [Google Scholar] [CrossRef] [PubMed]
- Olson, R.A.; LaPointe, V.; Benny, A.; Chan, M.; Lefresne, S.; McKenzie, M. Evaluation of Patient-Reported Outcome Differences by Radiotherapy Techniques for Bone Metastases in A Population-Based Healthcare System. Curr. Oncol. 2022, 29, 2073–2080. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Grimshaw, J.M.; Nielsen, C.; Judd, M.; Coyte, P.C.; Graham, I.D. Evolution of Wenger’s Concept of Community of Practice. Implement. Sci. 2009, 4, 11. [Google Scholar] [CrossRef] [PubMed]
- Berlin, A.; Lovas, M.; Truong, T.; Melwani, S.; Liu, J.; Liu, Z.A.; Badzynski, A.; Carpenter, M.B.; Virtanen, C.; Morley, L.; et al. Implementation and Outcomes of Virtual Care Across a Tertiary Cancer Center During COVID-19. JAMA Oncol. 2021, 7, 597–602. [Google Scholar] [CrossRef] [PubMed]
- Ontario, C.C. Managing Symptoms, Side Effects & Well-Being. Available online: https://www.cancercareontario.ca/en/symptom-management (accessed on 5 October 2021).
- Canadian Partnership for Quality Radiotherapy CPQR. Available online: https://www.proprofs.com/quiz-school/ugc/story.php?title=cpqr-patient-reported-outcomes-selfassessment-tool_3h8 (accessed on 7 March 2022).
- American Association of Physicists in Medicine (AAPM) Big Data Subcomittee (BDSC) of the Data Sciences Committee (DSC) Operational Ontology for Radiation Oncology (OORO). Available online: https://aapmbdsc.azurewebsites.net/Home/About?ReturnUrl=%2F (accessed on 7 March 2022).

| Disease Site | PRO Measure |
|---|---|
| All cancer (general) | Edmonton Symptom Assessment Screening (ESAS) |
| Bone metastasis | Brief Pain Inventory (BPI) |
| Prostate cancer | Expanded Prostate Cancer Index Composite (EPIC) |
| Head and neck cancer | MD Anderson Symptom Inventory for Head and Neck (MDASI-HN) |
| Gynecological cancer | Cervical cancer-specific quality of life module of the European Organization for Research and Treatment of Cancer (EORTC QLQ-CX24) |
| Publication | Publication Year | Publication Party/Society | Purpose | Relevance to PRO Promotion |
|---|---|---|---|---|
| Caissie et al. [7] | 2018 | CPQR | Develop a pan-Canadian approach to PRO integration in radiation oncology |
|
| Olson et al. [23] | 2018 | BCCA | Initiate prospective PRO collection to guide care, quality improvement and research |
|
| Brundage et al. [20] | 2019 | Multi-institutional-Ontario | Introduce a PRO (EPIC-CP) in routine ambulatory care of prostate cancer and assess acceptability by clinicians and patients |
|
| Barbera et al. [15] | 2020 | ICES | Examine the effect of generic PRO (ESAS) exposure on survival |
|
| Barbera et al. [18] | 2020 | ICES | Examine the effect of generic PRO (ESAS) exposure on emergency department visits and hospitalization |
|
| Montgomery et al. [13] | 2020 | CCO | Recommend an approach for PRO selection, implementation and evaluation for use in a clinical setting using an example from head and neck cancer |
|
| Atallah et al. [21] | 2021 | Multi-institutional-Ontario | Implement a cervix-cancer-specific PRO in gynecologic oncology clinics |
|
| Sit et al. [27] | 2021 | BCCA | Investigate potential relationships between tumour biology/histology and PROs |
|
| Olson et al. [28] | 2022 | BCCA | Assess advanced RT technique through PRO (BPI) in patients with bone metastasis |
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Caissie, A.; Olson, R.; Barbera, L.; O’Donnell, J.; Davis, C.-A.; Croke, J.; Bird, L.; Kildea, J.; Brown, E.; Brundage, M.; et al. Striving to Fill in Gaps between Clinical Practice and Standards: The Evolution of a Pan-Canadian Approach to Patient-Reported Outcomes Use. Curr. Oncol. 2022, 29, 3698-3707. https://doi.org/10.3390/curroncol29050296
Caissie A, Olson R, Barbera L, O’Donnell J, Davis C-A, Croke J, Bird L, Kildea J, Brown E, Brundage M, et al. Striving to Fill in Gaps between Clinical Practice and Standards: The Evolution of a Pan-Canadian Approach to Patient-Reported Outcomes Use. Current Oncology. 2022; 29(5):3698-3707. https://doi.org/10.3390/curroncol29050296
Chicago/Turabian StyleCaissie, Amanda, Robert Olson, Lisa Barbera, Jennifer O’Donnell, Carol-Anne Davis, Jennifer Croke, Louise Bird, John Kildea, Erika Brown, Michael Brundage, and et al. 2022. "Striving to Fill in Gaps between Clinical Practice and Standards: The Evolution of a Pan-Canadian Approach to Patient-Reported Outcomes Use" Current Oncology 29, no. 5: 3698-3707. https://doi.org/10.3390/curroncol29050296
APA StyleCaissie, A., Olson, R., Barbera, L., O’Donnell, J., Davis, C.-A., Croke, J., Bird, L., Kildea, J., Brown, E., Brundage, M., & Milosevic, M. (2022). Striving to Fill in Gaps between Clinical Practice and Standards: The Evolution of a Pan-Canadian Approach to Patient-Reported Outcomes Use. Current Oncology, 29(5), 3698-3707. https://doi.org/10.3390/curroncol29050296






