HPV Vaccination: An Underused Strategy for the Prevention of Cancer
Abstract
:1. The Burden of HPV
2. Vaccination as a Tool to Prevent Cancer
3. The Underuse of HPV Vaccination
4. Drivers for Achieving High Global HPV Vaccine Coverage
4.1. Practical Issues
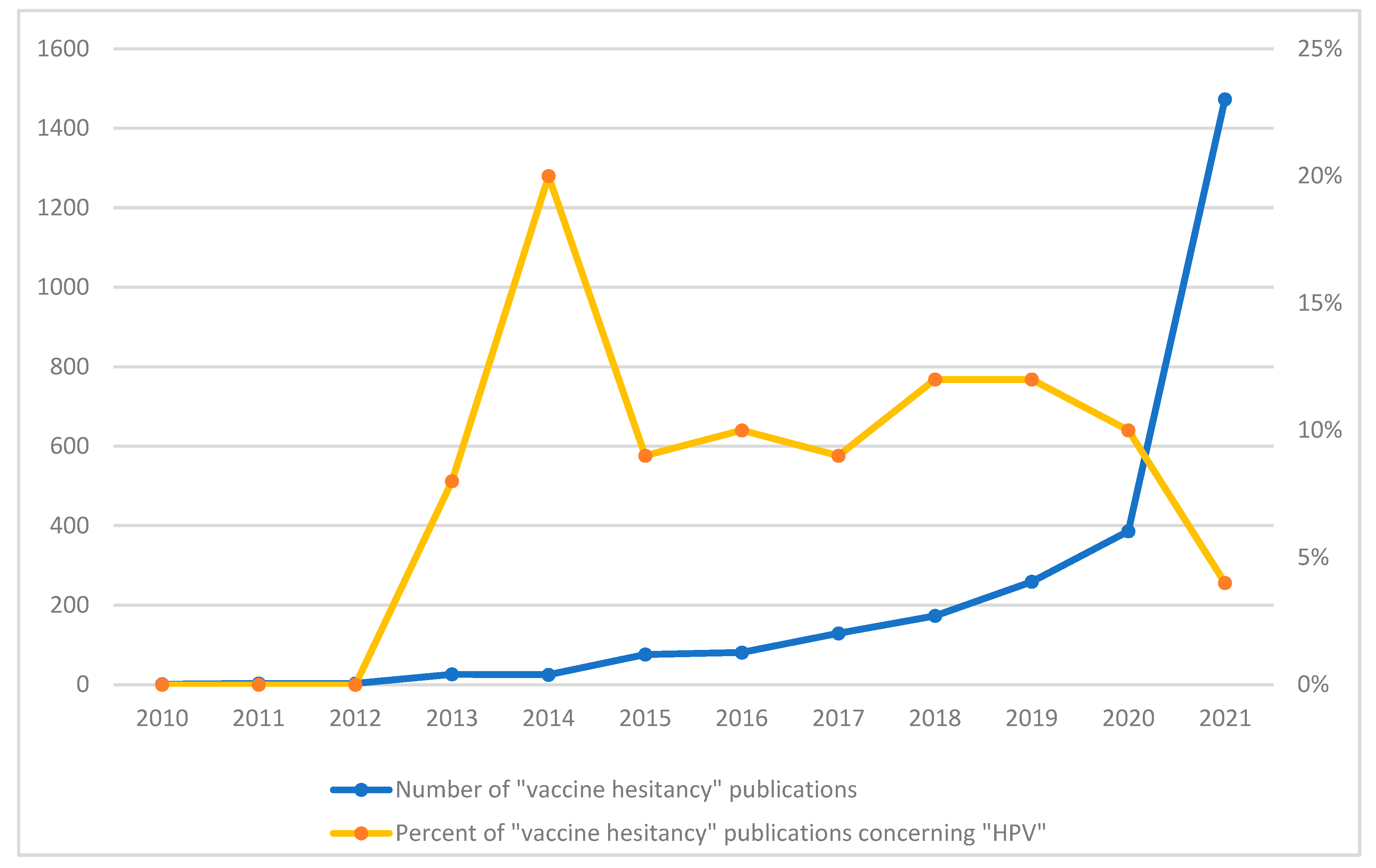
4.2. Motivation
4.3. Social Processes
4.4. Thinking and Feeling
5. Conclusions
Funding
Data Availability Statement
Conflicts of Interest
References
- De Martel, C.; Georges, D.; Bray, F.; Ferlay, J.; Clifford, G.M. Global burden of cancer attributable to infections in 2018: A worldwide incidence analysis. Lancet Glob. Health 2020, 8, e180–e190. [Google Scholar] [CrossRef] [Green Version]
- Nobel Media. Harald zur Hausen—Nobel Lecture: The Search for Infectious Causes of Human Cancers: Where and Why. 2014. Available online: http://www.nobelprize.org/nobel_prizes/medicine/laureates/2008/hausen-lecture.html (accessed on 22 April 2018).
- American Cancer Society. What Causes Cancer? American Cancer Society: Atlanta, GA, USA, 2018. [Google Scholar]
- Tota, J.E.; Chevarie-Davis, M.; Richardson, L.A.; Devries, M.; Franco, E.L. Epidemiology and burden of HPV infection and related diseases: Implications for prevention strategies. Prev. Med. 2011, 53 (Suppl. 1), S12–S21. [Google Scholar] [CrossRef] [PubMed]
- Plummer, M.; de Martel, C.; Vignat, J.; Ferlay, J.; Bray, F.; Franceschi, S. Global burden of cancers attributable to infections in 2012: A synthetic analysis. Lancet Glob. Health 2016, 4, e609–e616. [Google Scholar] [CrossRef] [Green Version]
- Forman, D.; de Martel, C.; Lacey, C.J.; Soerjomataram, I.; Lortet-Tieulent, J.; Bruni, L.; Vignat, J.; Ferlay, J.; Bray, F.; Plummer, M.; et al. Global burden of human papillomavirus and related diseases. Vaccine 2012, 30 (Suppl. 5), F12–F23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- National Advisory Committee on Immunization (NACI). Update On Human Papillomavirus Vaccines; An Advisory Committee Statement (ACS); Canada Communicable Disease Report; Public Health Agency of Canada: Ottawa, ON, Canada, 2012; Volume 38, ACS-1:1-62. [Google Scholar]
- You, E.L.; Henry, M.; Zeitouni, A.G. Human papillomavirus-associated oropharyngeal cancer: Review of current evidence and management. Curr. Oncol. 2019, 26, 119–123. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aral, S.O.; Holmes, K.K. Social and behavioral determinants of epidemiology of STDs: Industrialized and developing countries. In Sexually Transmitted Diseases; Holmes, K.K., Sparling, P.F., Mardh, P.A., Lemon, S.M., Stamm, W.E., Piot, P., Wasserheit, J.N., Eds.; McGraw-Hill: New York, NY, USA, 1999; pp. 39–76. [Google Scholar]
- Steben, M.; Duarte-Franco, E. Human papillomavirus infection: Epidemiology and pathophysiology. Gynecol Oncol. 2007, 107, S2–S5. [Google Scholar] [CrossRef]
- Serrano, B.; Brotons, M.; Bosch, F.X.; Bruni, L. Epidemiology and burden of HPV-related disease. Best Pract. Res. Clin. Obstet. Gynaecol. 2018, 47, 14–26. [Google Scholar] [CrossRef]
- Canadian Cancer Society. Canadian Cancer Statistics 2016; Canadian Cancer Society: Toronto, ON, Canada, 2016. [Google Scholar]
- Canadian Cancer Society. Canadian Cancer Statistics 2017; Canadian Cancer Society: Toronto, ON, Canada, 2017. [Google Scholar]
- Zhao, R.W.; Guo, Z.Q.; Zhang, R.X. Human papillomavirus infection and the malignant transformation of sinonasal inverted papilloma: A meta-analysis. J. Clin. Virol. 2016, 79, 36–43. [Google Scholar] [CrossRef]
- Knör, M.; Tziridis, K.; Agaimy, A.; Zenk, J.; Wendler, O. Human Papillomavirus (HPV) Prevalence in Nasal and Antrochoanal Polyps and Association with Clinical Data. PLoS ONE 2015, 10, e0141722. [Google Scholar] [CrossRef] [Green Version]
- Afrogheh, A.H.; Jakobiec, F.A.; Hammon, R.; Grossniklaus, H.E.; Rocco, J.; Lindeman, N.I.; Sadow, P.M.; Faquin, W.C. Evaluation for High-risk HPV in Squamous Cell Carcinomas and Precursor Lesions Arising in the Conjunctiva and Lacrimal Sac. Am. J. Surg. Pathol. 2016, 40, 519–528. [Google Scholar] [CrossRef]
- Welschmeyer, A.; Berke, G.S. An updated review of the epidemiological factors associated with recurrent respiratory papillomatosis. Laryngoscope Investig. Otolaryngol. 2021, 6, 226–233. [Google Scholar] [CrossRef] [PubMed]
- Houlihan, C.F.; Larke, N.L.; Watson-Jones, D.; Smith-McCune, K.K.; Shiboski, S.; Gravitt, P.E.; Smith, J.S.; Kuhn, L.; Wang, C.; Hayes, R. Human papillomavirus infection and increased risk of HIV acquisition. A systematic review and meta-analysis. AIDS 2012, 26, 2211–2222. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Koning, M.N.; ter Schegget, J.; Eekhof, J.A.; Kamp, M.; Kleter, B.; Gussekloo, J.; Feltkamp, M.C.; Bouwes Bavinck, J.N.; Purdie, K.J.; Bunker, C.B.; et al. Evaluation of a novel broad-spectrum PCR-multiplex genotyping assay for identification of cutaneous wart-associated human papillomavirus types. J. Clin. Microbiol. 2010, 48, 1706–1711. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coles, V.A.; Chapman, R.; Lanitis, T.; Carroll, S.M. The costs of managing genital warts in the UK by devolved nation: England, Scotland, Wales and Northern Ireland. Int. J. STD AIDS 2016, 27, 51–57. [Google Scholar] [CrossRef] [PubMed]
- De Martel, C.; Plummer, M.; Vignat, J.; Franceschi, S. Worldwide burden of cancer attributable to HPV by site, country and HPV type. Int. J. Cancer 2017, 141, 664–670. [Google Scholar] [CrossRef] [Green Version]
- Burchell, A.N.; Richardson, H.; Mahmud, S.M.; Trottier, H.; Tellier, P.P.; Hanley, J.; Coutlee, F.; Franco, E.L. Modeling the sexual transmissibility of human papillomavirus infection using stochastic computer simulation and empirical data from a cohort study of young women in Montreal, Canada. Am. J. Epidemiol. 2006, 163, 534–543. [Google Scholar] [CrossRef] [Green Version]
- Gowda, C.; Dempsey, A.F. The rise (and fall?) of parental vaccine hesitancy. Hum. Vaccines Immunother. 2013, 9, 1755–1762. [Google Scholar] [CrossRef] [Green Version]
- Ma, X.; Wang, Q.; Ong, J.J.; Fairley, C.K.; Su, S.; Peng, P.; Jing, J.; Wang, L.; Soe, N.N.; Cheng, F.; et al. Prevalence of human papillomavirus by geographical regions, sexual orientation and HIV status in China: A systematic review and meta-analysis. Sex Transm. Infect. 2018, 94, 434–442. [Google Scholar] [CrossRef]
- Batista Ferrer, H.; Audrey, S.; Trotter, C.; Hickman, M. An appraisal of theoretical approaches to examining behaviours in relation to Human Papillomavirus (HPV) vaccination of young women. Prev. Med. 2015, 81, 122–131. [Google Scholar] [CrossRef] [Green Version]
- Nielsen, K.J.; Jakobsen, K.K.; Jensen, J.S.; Grønhøj, C.; Von Buchwald, C. The Effect of Prophylactic HPV Vaccines on Oral and Oropharyngeal HPV Infection-A Systematic Review. Viruses 2021, 13, 1339. [Google Scholar] [CrossRef]
- Kobayashi, K.; Hisamatsu, K.; Suzui, N.; Hara, A.; Tomita, H.; Miyazaki, T. A Review of HPV-Related Head and Neck Cancer. J. Clin. Med. 2018, 7, 241. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guichon, J.; Shapiro, G.K. Opinion: Give HPV vaccine to prevent mouth and throat cancers. Vancouver Sun. 28 October 2016. Available online: https://vancouversun.com/opinion/opinion-give-hpv-vaccine-to-prevent-mouth-and-throat-cancers (accessed on 29 March 2022).
- Timbang, M.R.; Sim, M.W.; Bewley, A.F.; Farwell, D.G.; Mantravadi, A.; Moore, M.G. HPV-related oropharyngeal cancer: A review on burden of the disease and opportunities for prevention and early detection. Hum. Vaccines Immunother. 2019, 15, 1920–1928. [Google Scholar] [CrossRef] [PubMed]
- Lechner, M.; Liu, J.; Masterson, L.; Fenton, T.R. HPV-associated oropharyngeal cancer: Epidemiology, molecular biology and clinical management. Nat. Rev. Clin. Oncol. 2022, 19, 306–327. [Google Scholar] [CrossRef] [PubMed]
- St Laurent, J.; Luckett, R.; Feldman, S. HPV vaccination and the effects on rates of HPV-related cancers. Curr. Probl. Cancer 2018, 42, 493–506. [Google Scholar] [CrossRef]
- Gold, D. The psychosocial care needs of patients with HPV-related head and neck cancer. Otolaryngol. Clin. North Am. 2012, 45, 879–897. [Google Scholar] [CrossRef]
- Milbury, K.; Rosenthal, D.I.; El-Naggar, A.; Badr, H. An exploratory study of the informational and psychosocial needs of patients with human papillomavirus-associated oropharyngeal cancer. Oral Oncol. 2013, 49, 1067–1071. [Google Scholar] [CrossRef] [Green Version]
- Reich, M.; Licitra, L.; Vermorken, J.B.; Bernier, J.; Parmar, S.; Golusinski, W.; Castellsagué, X.; Leemans, C.R. Best practice guidelines in the psychosocial management of HPV-related head and neck cancer: Recommendations from the European Head and Neck Cancer Society’s Make Sense Campaign. Ann. Oncol. 2016, 27, 1848–1854. [Google Scholar] [CrossRef]
- Crosignani, P.; De Stefani, A.; Fara, G.M.; Isidori, A.M.; Lenzi, A.; Liverani, C.A.; Lombardi, A.; Mennini, F.S.; Palu, G.; Pecorelli, S.; et al. Towards the eradication of HPV infection through universal specific vaccination. BMC Public Health 2013, 13, 642. [Google Scholar] [CrossRef] [Green Version]
- De Felice, F.; Polimeni, A.; Tombolini, V. Human papillomavirus (HPV) vaccine and HPV-related head and neck cancer: What’s next? Oral. Oncol. 2019, 93, 125–126. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control. Introduction of HPV Vaccines in European Union Countries—An Update; European Centre for Disease Prevention and Control: Stockholm, Sweden, 2012. [Google Scholar]
- Centers for Disease Control and Prevention. FDA Licensure of Quadrivalent Human Papillomavirus Vaccine (HPV4, Gardasil) for Use in Males and Guidance from the Advisory Committee on Immunization Practices (ACIP). Available online: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5920a5.htm (accessed on 25 May 2021).
- Garland, S.M. The Australian experience with the human papillomavirus vaccine. Clin. Ther. 2014, 36, 17–23. [Google Scholar] [CrossRef]
- Brotherton, J.M.L.; Zuber, P.L.F.; Bloem, P.J.N. Primary Prevention of HPV through Vaccination: Update on the Current Global Status. Curr. Obstet. Gynecol. 2016, 5, 210–224. [Google Scholar] [CrossRef]
- Markowitz, L.E.; Schiller, J.T. Human Papillomavirus Vaccines. J. Infect. Dis. 2021, 224, S367–s378. [Google Scholar] [CrossRef] [PubMed]
- Schneider, K.; Grønhøj, C.; Hahn, C.H.; von Buchwald, C. Therapeutic human papillomavirus vaccines in head and neck cancer: A systematic review of current clinical trials. Vaccine 2018, 36, 6594–6605. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. One-Dose Human Papillomavirus (HPV) Vaccine Offers Solid Protection against Cervical Cancer. Available online: https://www.who.int/news/item/11-04-2022-one-dose-human-papillomavirus-(hpv)-vaccine-offers-solid-protection-against-cervical-cancer (accessed on 20 April 2022).
- Shapiro, G.K.; Perez, S.; Rosberger, Z. Including males in Canadian human papillomavirus vaccination programs: A policy analysis. Can. Med. Assoc. J. = J. Assoc. Med. Can. 2016, 188, 881–886. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bergman, H.; Buckley, B.S.; Villanueva, G.; Petkovic, J.; Garritty, C.; Lutje, V.; Riveros-Balta, A.X.; Low, N.; Henschke, N. Comparison of different human papillomavirus (HPV) vaccine types and dose schedules for prevention of HPV-related disease in females and males. Cochrane Database Syst. Rev. 2019, 11, CD013479. [Google Scholar] [CrossRef]
- Shapiro, G.K.; Guichon, J.; Prue, G.; Perez, S.; Rosberger, Z. A Multiple Streams analysis of the decisions to fund gender-neutral HPV vaccination in Canada. Prev. Med. 2017, 100, 123–131. [Google Scholar] [CrossRef] [Green Version]
- Markowitz, L.E.; Dunne, E.F.; Saraiya, M.; Chesson, H.W.; Curtis, C.R.; Gee, J.; Bocchini, J.A., Jr.; Unger, E.R.; Centers for Disease, C.; Prevention. Human papillomavirus vaccination: Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm. Rep. 2014, 63, 1–30. [Google Scholar]
- Ferris, D.; Samakoses, R.; Block, S.L.; Lazcano-Ponce, E.; Restrepo, J.A.; Reisinger, K.S.; Mehlsen, J.; Chatterjee, A.; Iversen, O.E.; Sings, H.L.; et al. Long-term study of a quadrivalent human papillomavirus vaccine. Pediatrics 2014, 134, e657–e665. [Google Scholar] [CrossRef] [Green Version]
- Goldstone, S.E.; Giuliano, A.R.; Palefsky, J.M.; Lazcano-Ponce, E.; Penny, M.E.; Cabello, R.E.; Moreira, E.D., Jr.; Baraldi, E.; Jessen, H.; Ferenczy, A.; et al. Efficacy, immunogenicity, and safety of a quadrivalent HPV vaccine in men: Results of an open-label, long-term extension of a randomised, placebo-controlled, phase 3 trial. Lancet Infect. Dis. 2022, 22, 413–425. [Google Scholar] [CrossRef]
- Drolet, M.; Benard, E.; Boily, M.C.; Ali, H.; Baandrup, L.; Bauer, H.; Beddows, S.; Brisson, J.; Brotherton, J.M.; Cummings, T.; et al. Population-level impact and herd effects following human papillomavirus vaccination programmes: A systematic review and meta-analysis. Lancet Infect. Dis. 2015, 15, 565–580. [Google Scholar] [CrossRef] [Green Version]
- Villa, A.; Patton, L.L.; Giuliano, A.R.; Estrich, C.G.; Pahlke, S.C.; O’Brien, K.K.; Lipman, R.D.; Araujo, M.W.B. Summary of the evidence on the safety, efficacy, and effectiveness of human papillomavirus vaccines: Umbrella review of systematic reviews. J. Am Dent. Assoc. 2020, 151, 245–254.e24. [Google Scholar] [CrossRef] [PubMed]
- Arbyn, M.; Xu, L.; Simoens, C.; Martin-Hirsch, P.P. Prophylactic vaccination against human papillomaviruses to prevent cervical cancer and its precursors. Cochrane Database Syst. Rev. 2018, 5, CD009069. [Google Scholar] [CrossRef] [PubMed]
- Markowitz, L.E.; Meites, E.; Unger, E.R. Two vs Three Doses of Human Papillomavirus Vaccine: New Policy for the Second Decade of the Vaccination Program. JAMA 2016, 316, 2370–2372. [Google Scholar] [CrossRef] [PubMed]
- Herweijer, E.; Sundström, K.; Ploner, A.; Uhnoo, I.; Sparén, P.; Arnheim-Dahlström, L. Quadrivalent HPV vaccine effectiveness against high-grade cervical lesions by age at vaccination: A population-based study. Int. J. Cancer 2016, 138, 2867–2874. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Drolet, M.; Bénard, É.; Pérez, N.; Brisson, M. Population-level impact and herd effects following the introduction of human papillomavirus vaccination programmes: Updated systematic review and meta-analysis. Lancet 2019, 394, 497–509. [Google Scholar] [CrossRef] [Green Version]
- Falcaro, M.; Castañon, A.; Ndlela, B.; Checchi, M.; Soldan, K.; Lopez-Bernal, J.; Elliss-Brookes, L.; Sasieni, P. The effects of the national HPV vaccination programme in England, UK, on cervical cancer and grade 3 cervical intraepithelial neoplasia incidence: A register-based observational study. Lancet 2021, 398, 2084–2092. [Google Scholar] [CrossRef]
- Lei, J.; Ploner, A.; Elfström, K.M.; Wang, J.; Roth, A.; Fang, F.; Sundström, K.; Dillner, J.; Sparén, P. HPV Vaccination and the Risk of Invasive Cervical Cancer. N. Engl. J. Med. 2020, 383, 1340–1348. [Google Scholar] [CrossRef]
- Kaczmarczyk, K.H.; Yusuf, H. The impact of HPV vaccination on the prevention of oropharyngeal cancer: A scoping review. Community Dent. Health 2022, 39, 14–21. [Google Scholar]
- Tsentemeidou, A.; Fyrmpas, G.; Stavrakas, M.; Vlachtsis, K.; Sotiriou, E.; Poutoglidis, A.; Tsetsos, N. Human Papillomavirus Vaccine to End Oropharyngeal Cancer. A Systematic Review and Meta-Analysis. Sex Transm. Dis. 2021, 48, 700–707. [Google Scholar] [CrossRef]
- Shearer, B.D. HPV Vaccination: Understanding the Impact on HPV Disease. Available online: http://www.nccid.ca/files/Purple_Paper_Note_mauve/PP_34_EN.pdf (accessed on 15 March 2015).
- Phillips, A.; Patel, C.; Pillsbury, A.; Brotherton, J.; Macartney, K. Safety of Human Papillomavirus Vaccines: An Updated Review. Drug Saf. 2018, 41, 329–346. [Google Scholar] [CrossRef]
- WHO Report. Human papillomavirus vaccines: WHO position paper, October 2014-Recommendations. Vaccine 2015, 33, 4383–4384. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Centers for Disease Control and Prevention. HPV Vaccines: Vaccinating Your Preteen or Teen. Available online: http://www.cdc.gov/hpv/parents/vaccine.html (accessed on 7 January 2015).
- National Advisory Committee on Immunization. Update on the Recommended Human Papillomavirus Vaccine Immunization Schedule; National Advisory Committee on Immunization: Ottawa, ON, Canada, 2015. [Google Scholar]
- Ng, S.S.; Hutubessy, R.; Chaiyakunapruk, N. Systematic review of cost-effectiveness studies of human papillomavirus (HPV) vaccination: 9-Valent vaccine, gender-neutral and multiple age cohort vaccination. Vaccine 2018, 36, 2529–2544. [Google Scholar] [CrossRef] [PubMed]
- Datta, S.; Pink, J.; Medley, G.F.; Petrou, S.; Staniszewska, S.; Underwood, M.; Sonnenberg, P.; Keeling, M.J. Assessing the cost-effectiveness of HPV vaccination strategies for adolescent girls and boys in the UK. BMC Infect. Dis. 2019, 19, 552. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suijkerbuijk, A.W.; Donken, R.; Lugnér, A.K.; de Wit, G.A.; Meijer, C.J.; de Melker, H.E.; Bogaards, J.A. The whole story: A systematic review of economic evaluations of HPV vaccination including non-cervical HPV-associated diseases. Expert Rev. Vaccines 2017, 16, 361–375. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Report EB146/9. Accelerating the Elimination of Cervical Cancer as a Global Public Health Problem. Available online: https://apps.who.int/gb/ebwha/pdf_files/EB146/B146_9-en.pdf (accessed on 17 March 2022).
- World Health Organization. WHO Immunization Data Portal. Available online: https://app.powerbi.com/view?r=eyJrIjoiNDIxZTFkZGUtMDQ1Ny00MDZkLThiZDktYWFlYTdkOGU2NDcwIiwidCI6ImY2MTBjMGI3LWJkMjQtNGIzOS04MTBiLTNkYzI4MGFmYjU5MCIsImMiOjh9 (accessed on 29 March 2022).
- Brotherton, J.M.; Bloem, P.N. Population-based HPV vaccination programmes are safe and effective: 2017 update and the impetus for achieving better global coverage. Best Practice & Research. Clin. Obstet. Gynaecol. 2018, 47, 42–58. [Google Scholar]
- Gallagher, K.E.; LaMontagne, D.S.; Watson-Jones, D. Status of HPV vaccine introduction and barriers to country uptake. Vaccine 2018, 36, 4761–4767. [Google Scholar] [CrossRef]
- Lefèvre, H.; Moro, M.R.; Lachal, J. The New HPV Vaccination Policy in France. N. Engl. J. Med. 2018, 378, 1160. [Google Scholar] [CrossRef] [Green Version]
- Bruni, L.; Saura-Lázaro, A.; Montoliu, A.; Brotons, M.; Alemany, L.; Diallo, M.S.; Afsar, O.Z.; LaMontagne, D.S.; Mosina, L.; Contreras, M.; et al. HPV vaccination introduction worldwide and WHO and UNICEF estimates of national HPV immunization coverage 2010–2019. Prev. Med. 2021, 144, 106399. [Google Scholar] [CrossRef]
- Shapiro, G.K.; Guichon, J.; Kelaher, M. Canadian school-based HPV vaccine programs and policy considerations. Vaccine 2017, 35, 5700–5707. [Google Scholar] [CrossRef] [Green Version]
- Bird, Y.; Obidiya, O.; Mahmood, R.; Nwankwo, C.; Moraros, J. Human Papillomavirus Vaccination Uptake in Canada: A Systematic Review and Meta-analysis. Int. J. Prev. Med. 2017, 8, 71. [Google Scholar] [CrossRef]
- Kuehn, B.M. HPV Vaccination Coverage Has Increased Among Adolescents. JAMA 2021, 326, 1366. [Google Scholar] [CrossRef] [PubMed]
- Hanley, S.J.; Yoshioka, E.; Ito, Y.; Kishi, R. HPV vaccination crisis in Japan. Lancet 2015, 385, 2571. [Google Scholar] [CrossRef] [Green Version]
- Australian Government Department of Health. National HPV Vaccination Program Register; Australian Government Department of Health: Canberra, Australia, 2018. [Google Scholar]
- Shapiro, G.K.; Head, K.J.; Rosberger, Z.; Zimet, G. Making the Decision to Give Adolescents the HPV Vaccine: Why Are Some Parents so Hesitant? Available online: https://www.hpvworld.com/media/29/media_section/8/2/982/Shapirohead.pdf (accessed on 25 March 2022).
- Vorsters, A.; Muñoz, N.; Murillo, R.; Van Damme, P.; Karafillakis, E.; de SanJosé, S.; Bruni, L.; Larson, H. Colombia: Decreasing HPV vaccination coverage: Mapping roles of different stakeholders and societal-historical factors. In Proceedings of the HPV Symposium: Building Trust, Managing Risk: Vaccine Confidence and Human Papillomavirus Vaccination, London, UK, 7–8 June 2017. [Google Scholar]
- Health Protection Surveillance Centre. HPV Vaccine Uptake in Ireland: 2016/2017; Health Protection Surveillance Centre: Dublin, Ireland, 2018. [Google Scholar]
- Hansen, P.R.; Schmidtblaicher, M.; Brewer, N.T. Resilience of HPV vaccine uptake in Denmark: Decline and recovery. Vaccine 2020, 38, 1842–1848. [Google Scholar] [CrossRef] [PubMed]
- Shapiro, G.K.; Kaufman, J.; Brewer, N.T.; Wiley, K.; Menning, L.; Leask, J. A critical review of measures of childhood vaccine confidence. Curr. Opin. Immunol. 2021, 71, 34–45. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Improving Vaccination Demand and Addressing Hesitancy. Available online: https://www.who.int/teams/immunization-vaccines-and-biologicals/essential-programme-on-immunization/demand (accessed on 29 March 2022).
- World Health Organization. Data for Action: Achieving High Uptake of COVID-19 Vaccines. Available online: https://www.who.int/publications/i/item/WHO-2019-nCoV-vaccination-demand-planning-2021.1 (accessed on 29 March 2022).
- World Health Organization. Strategic Advisory Group of Experts on Immunization (SAGE)—October 2021. Available online: https://www.who.int/news-room/events/detail/2021/10/04/default-calendar/sage_meeting_october_2021 (accessed on 20 March 2022).
- World Health Organization. Global Market Study: HPV Vaccines (December 2019). Available online: https://www.who.int/immunization/programmes_systems/procurement/mi4a/platform/module2/WHO_HPV_market_study_public_summary_Dec2019.pdf (accessed on 17 March 2022).
- Gavi The Vaccine Alliance. About our Alliance. Available online: https://www.gavi.org/our-alliance/about (accessed on 20 March 2022).
- Shapiro, G.K.; Gottfredson, N.; Leask, J.; Wiley, K.; Ganter-Restrepo, F.E.; Jones, S.P.; Menning, L.; Brewer, N.T. COVID-19 and missed or delayed vaccination in 26 middle- and high-income countries: An observational survey. Vaccine 2022, 40, 945–952. [Google Scholar] [CrossRef] [PubMed]
- UK Health Security Agency. Human Papillomavirus (HPV) Vaccination Coverage in Adolescent Females and Males in England: 2020 to 2021. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1040436/hpr2021_hpv-vc.pdf (accessed on 25 March 2022).
- Musto, R.; Siever, J.E.; Johnston, J.C.; Seidel, J.; Rose, M.S.; McNeil, D.A. Social equity in Human Papillomavirus vaccination: A natural experiment in Calgary Canada. BMC Public Health 2013, 13, 640. [Google Scholar] [CrossRef] [Green Version]
- Shapiro, G.K.; Tatar, O.; Knäuper, B.; Griffin-Mathieu, G.; Rosberger, Z. The impact of publicly funded immunization programs on human papillomavirus vaccination in boys and girls: An observational study. Lancet Reg. Health Am. 2022, 8, 100128. [Google Scholar] [CrossRef]
- Tsu, V.D.; Cernuschi, T.; LaMontagne, D.S. Lessons learned from HPV vaccine delivery in low-resource settings and opportunities for HIV prevention, treatment, and care among adolescents. J. Acquir. Immune Defic. Syndr. 2014, 66 (Suppl. 2), S209–S216. [Google Scholar] [CrossRef]
- Poland, G.A.; Jacobson, R.M. The age-old struggle against the antivaccinationists. N. Engl. J. Med. 2011, 364, 97–99. [Google Scholar] [CrossRef] [Green Version]
- Offit, P.A. Deadly Choices: How the Anti-Vaccine Movement Threatens Us All; Basic Books: New York, NY, USA, 2011. [Google Scholar]
- Leask, J. Should we do battle with antivaccination activists? Public Health Res. Pract. 2015, 25, e2521515. [Google Scholar] [CrossRef] [Green Version]
- Callender, D. Vaccine hesitancy: More than a movement. Hum. Vaccines Immunother. 2016, 12, 2464–2468. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shapiro, G.K. Understanding Human Papillomavirus Vaccination and Vaccine Hesitancy among Canadian Parents; McGill University: Montreal, QC, Canada, 2018. [Google Scholar]
- Radisic, G.; Chapman, J.; Flight, I.; Wilson, C. Factors associated with parents’ attitudes to the HPV vaccination of their adolescent sons: A systematic review. Prev. Med. 2017, 95, 26–37. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, S.A.; Mullen, P.D.; Lopez, D.M.; Savas, L.S.; Fernández, M.E. Factors associated with adolescent HPV vaccination in the U.S.: A systematic review of reviews and multilevel framework to inform intervention development. Prev. Med. 2020, 131, 105968. [Google Scholar] [CrossRef] [PubMed]
- Reiter, P.L.; McRee, A.L.; Pepper, J.K.; Gilkey, M.B.; Galbraith, K.V.; Brewer, N.T. Longitudinal predictors of human papillomavirus vaccination among a national sample of adolescent males. Am. J. Public Health 2013, 103, 1419–1427. [Google Scholar] [CrossRef]
- Shapiro, G.K.; Tatar, O.; Amsel, R.; Prue, G.; Zimet, G.D.; Knauper, B.; Rosberger, Z. Using an integrated conceptual framework to investigate parents’ HPV vaccine decision for their daughters and sons. Prev. Med. 2018, 116, 203–210. [Google Scholar] [CrossRef] [Green Version]
- Niccolai, L.M.; Hansen, C.E. Practice- and Community-Based Interventions to Increase Human Papillomavirus Vaccine Coverage: A Systematic Review. JAMA Pediatrics 2015, 169, 686–692. [Google Scholar] [CrossRef] [Green Version]
- Oh, N.L.; Biddell, C.B.; Rhodes, B.E.; Brewer, N.T. Provider communication and HPV vaccine uptake: A meta-analysis and systematic review. Prev. Med. 2021, 148, 106554. [Google Scholar] [CrossRef]
- Fu, L.Y.; Zimet, G.D.; Latkin, C.A.; Joseph, J.G. Social Networks for Human Papillomavirus Vaccine Advice Among African American Parents. J. Adolesc. Health. 2019, 65, 124–129. [Google Scholar] [CrossRef]
- Lahijani, A.Y.; King, A.R.; Gullatte, M.M.; Hennink, M.; Bednarczyk, R.A. HPV Vaccine Promotion: The church as an agent of change. Soc. Sci. Med. 2021, 268, 113375. [Google Scholar] [CrossRef]
- Olagoke, A.A.; Floyd, B.; Caskey, R.; Hebert-Beirne, J.; Boyd, A.D.; Molina, Y. Disentangling the Role of Religiosity in Human Papillomavirus Vaccination Amidst COVID-19 Pandemic. J. Relig. Health 2022, 61, 1734–1749. [Google Scholar] [CrossRef]
- Chang, J.; Ipp, L.S.; de Roche, A.M.; Catallozzi, M.; Breitkopf, C.R.; Rosenthal, S.L. Adolescent-Parent Dyad Descriptions of the Decision to Start the HPV Vaccine Series. J. Pediatr. Adolesc. Gynecol. 2018, 31, 28–32. [Google Scholar] [CrossRef] [PubMed]
- Perez, S.; Restle, H.; Naz, A.; Tatar, O.; Shapiro, G.K.; Rosberger, Z. Parents’ involvement in the human papillomavirus vaccination decision for their sons. Sex Reprod. Healthc. 2017, 14, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Betsch, C.; Renkewitz, F.; Betsch, T.; Ulshofer, C. The influence of vaccine-critical websites on perceiving vaccination risks. J. Health Psychol. 2010, 15, 446–455. [Google Scholar] [CrossRef] [PubMed]
- Nan, X.; Madden, K. HPV vaccine information in the blogosphere: How positive and negative blogs influence vaccine-related risk perceptions, attitudes, and behavioral intentions. Health Commun. 2012, 27, 829–836. [Google Scholar] [CrossRef]
- Dunn, A.G.; Surian, D.; Leask, J.; Dey, A.; Mandl, K.D.; Coiera, E. Mapping information exposure on social media to explain differences in HPV vaccine coverage in the United States. Vaccine 2017, 35, 3033–3040. [Google Scholar] [CrossRef]
- Netfa, F.; Tashani, M.; Booy, R.; King, C.; Rashid, H.; Skinner, S.R. Knowledge, Attitudes and Perceptions of Immigrant Parents Towards Human Papillomavirus (HPV) Vaccination: A Systematic Review. Trop. Med. Infect. Dis. 2020, 5, 58. [Google Scholar] [CrossRef] [Green Version]
- López, N.; Garcés-Sánchez, M.; Panizo, M.B.; de la Cueva, I.S.; Artés, M.T.; Ramos, B.; Cotarelo, M. HPV knowledge and vaccine acceptance among European adolescents and their parents: A systematic literature review. Public Health Rev. 2020, 41, 10. [Google Scholar] [CrossRef]
- Perez, S.; Tatar, O.; Gilca, V.; Shapiro, G.K.; Ogilvie, G.; Guichon, J.; Naz, A.; Rosberger, Z. Untangling the psychosocial predictors of HPV vaccination decision-making among parents of boys. Vaccine 2017, 35, 4713–4721. [Google Scholar] [CrossRef]
- Weinstein, N.D.; Sandman, P.M.; Blalock, S.J. The Precaution Adoption Process Model. In Health Behavior and Health Education: Theory, Research, and Practice, 4th ed.; Glanz, K., Rimer, B.K., Viswanath, K., Eds.; Jossey-Bass: San Francisco, CA, USA, 2008; pp. 123–148. [Google Scholar]
- Brewer, N.T.; Fazekas, K.I. Predictors of HPV vaccine acceptability: A theory-informed, systematic review. Prev. Med. 2007, 45, 107–114. [Google Scholar] [CrossRef]
- Cunningham, M.S.; Davison, C.; Aronson, K.J. HPV vaccine acceptability in Africa: A systematic review. Prev. Med. 2014, 69, 274–279. [Google Scholar] [CrossRef]
- Smith, L.E.; Amlot, R.; Weinman, J.; Yiend, J.; Rubin, G.J. A systematic review of factors affecting vaccine uptake in young children. Vaccine 2017, 35, 6059–6069. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferrer, H.B.; Trotter, C.; Hickman, M.; Audrey, S. Barriers and facilitators to HPV vaccination of young women in high-income countries: A qualitative systematic review and evidence synthesis. BMC Public Health 2014, 14, 700. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Whitworth, H.; Changalucha, J.; Baisley, K.; Watson-Jones, D. Adolescent Health Series: HPV infection and vaccination in sub-Saharan Africa: 10 years of research in Tanzanian female adolescents—Narrative review. Trop. Med. Int. Health 2021, 26, 1345–1355. [Google Scholar] [CrossRef] [PubMed]
- Kasting, M.L.; Shapiro, G.K.; Rosberger, Z.; Kahn, J.A.; Zimet, G.D. Tempest in a teapot: A systematic review of HPV vaccination and risk compensation research. Hum. Vaccines Immunother. 2016, 12, 1435–1450. [Google Scholar] [CrossRef] [Green Version]
- Lechuga, J.; Vera-Cala, L.; Martinez-Donate, A. HPV Vaccine Awareness, Barriers, Intentions, and Uptake in Latina Women. J. Immigr. Minor. Health 2016, 18, 173–178. [Google Scholar] [CrossRef]
| Brand Name | Gardasil® | Cervarix® | Gardasil®9 | Cecolin® |
| Developer | Merck | Glaxo SmithKline | Merck | Xiamen Innovax Biotech |
| Date licensed | 2006 | 2007 | 2014 | 2020 * |
| Type of vaccine | Quadrivalent | Bivalent | Nonavalent | Bivalent |
| HPV strains targeted | 6/11/16/18 | 16/18 | 6/11/16/18/31/33/45/52/58 | 16/18 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shapiro, G.K. HPV Vaccination: An Underused Strategy for the Prevention of Cancer. Curr. Oncol. 2022, 29, 3780-3792. https://doi.org/10.3390/curroncol29050303
Shapiro GK. HPV Vaccination: An Underused Strategy for the Prevention of Cancer. Current Oncology. 2022; 29(5):3780-3792. https://doi.org/10.3390/curroncol29050303
Chicago/Turabian StyleShapiro, Gilla K. 2022. "HPV Vaccination: An Underused Strategy for the Prevention of Cancer" Current Oncology 29, no. 5: 3780-3792. https://doi.org/10.3390/curroncol29050303
APA StyleShapiro, G. K. (2022). HPV Vaccination: An Underused Strategy for the Prevention of Cancer. Current Oncology, 29(5), 3780-3792. https://doi.org/10.3390/curroncol29050303





