The Prediction of Survival after Surgical Management of Bone Metastases of the Extremities—A Comparison of Prognostic Models
Abstract
:1. Introduction
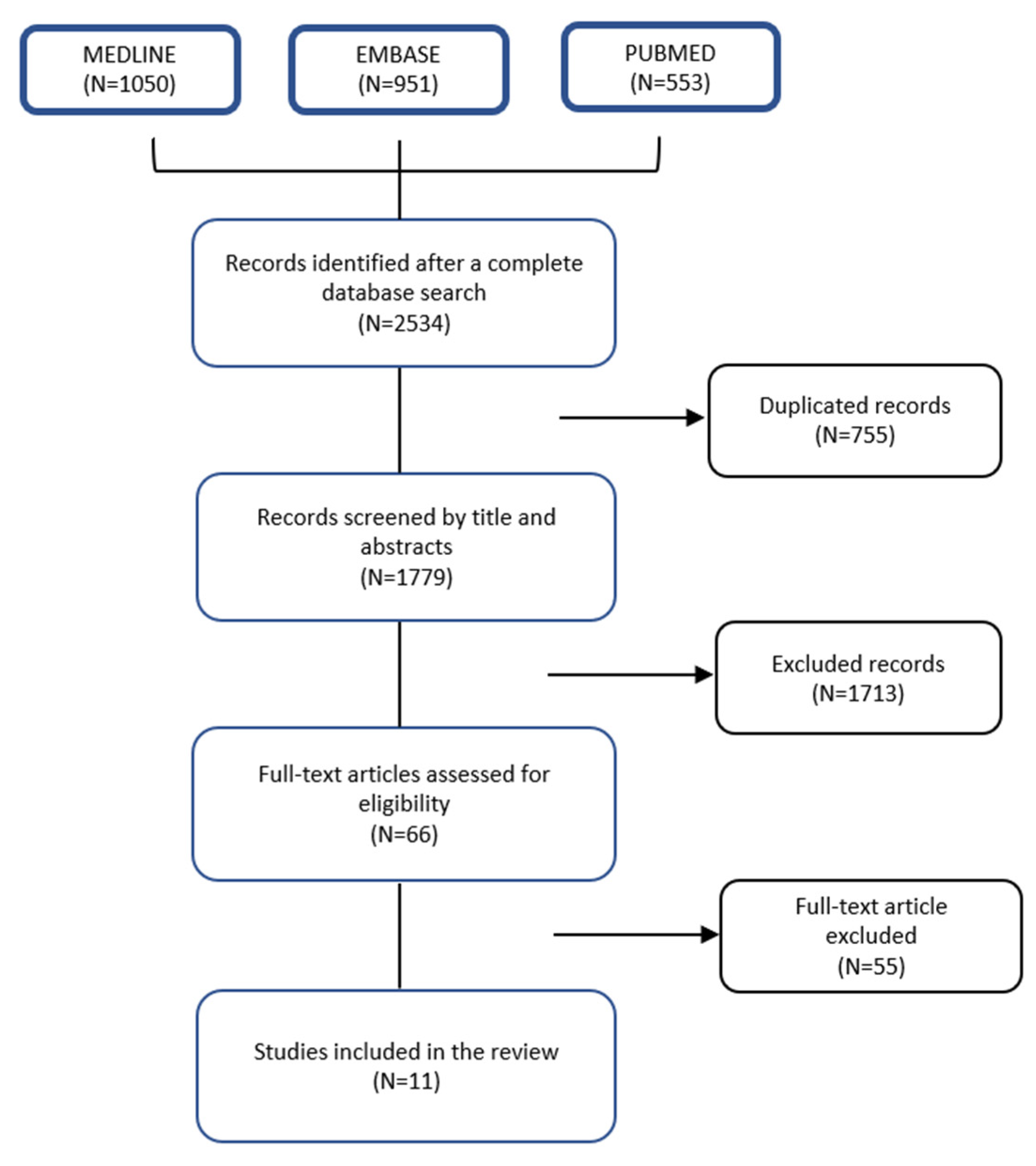
2. Materials and Methods
2.1. Data Source and Searches
2.2. Data Selection
2.3. Data Synthesis and Analysis
3. Results
3.1. Discrimination Accuracy and Calibration Score
3.2. Summary of the Models
3.2.1. SPRING 2013 Nomogram
3.2.2. 7 SSG Score
3.2.3. Janssen Score, Nomogram, Model
3.2.4. OptiModel
3.2.5. SORG Model
3.2.6. PATHfx Model
3.2.7. IOR (Instituto Orthopedico Rizzoli) Score
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Errani, C.; Mavrogenis, A.F.; Cevolani, L.; Spinelli, S.; Piccioli, A.; Maccauro, G.; Baldini, N.; Donati, D.M. Treatment for long bone metastases based on a systematic literature review. Eur. J. Orthop. Surg. Traumatol. 2017, 27, 205–211. [Google Scholar] [CrossRef] [PubMed]
- Abbott, A.; Kendal, J.K.; Hewison, C.; Puloski, S.; Monument, M. Longitudinal survival trends of patients with cancer with surgically managed appendicular metastatic bone disease: Systematic review. Can. J. Surg. 2021, 64, E550–E560. [Google Scholar] [CrossRef] [PubMed]
- Forsberg, J.A.; Eberhardt, J.; Boland, P.J.; Wedin, R.; Healey, J. Estimating Survival in Patients with Operable Skeletal Metastases: An Application of a Bayesian Belief Network. PLoS ONE 2011, 6, e19956. [Google Scholar] [CrossRef] [Green Version]
- Harvey, N.; Ahlmann, E.R.; Allison, D.C.; Wang, L.; Menendez, L.R. Endoprostheses Last Longer Than Intramedullary Devices in Proximal Femur Metastases. Clin. Orthop. Relat. Res. 2012, 470, 684–691. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ratasvuori, M.; Wedin, R.; Keller, J.; Nottrott, M.; Zaikova, O.; Bergh, P.; Kalen, A.; Nilsson, J.; Jonsson, H.; Laitinen, M. Insight opinion to surgically treated metastatic bone disease: Scandinavian Sarcoma Group Skeletal Metastasis Registry report of 1195 operated skeletal metastasis. Surg. Oncol. 2013, 22, 132–138. [Google Scholar] [CrossRef] [PubMed]
- Nathan, S.S.; Healey, J.H.; Mellano, D.; Hoang, B.; Lewis, I.; Morris, C.D.; Athanasian, E.A.; Boland, P.J. Survival in Patients Operated on for Pathologic Fracture: Implications for End-of-Life Orthopedic Care. J. Clin. Oncol. 2005, 23, 6072–6082. [Google Scholar] [CrossRef] [PubMed]
- Hartsell, W.F.; Desilvio, M.; Bruner, D.W.; Scarantino, C.; Ivker, R.; Roach, M., 3rd; Suh, J.; Demas, W.F.; Movsas, B.; Petersen, I.A.; et al. Can physicians accurately predict survival time in patients with metastatic cancer? Analysis of RTOG 97-14. J. Palliat. Med. 2008, 11, 723–728. [Google Scholar] [CrossRef]
- Steyerberg, E.W.; Vergouwe, Y. Towards better clinical prediction models: Seven steps for development and an ABCD for validation. Eur. Heart J. 2014, 35, 1925–1931. [Google Scholar] [CrossRef] [Green Version]
- Wood, T.J.; Racano, A.; Yeung, H.; Farrokhyar, F.; Ghert, M.; Deheshi, B.M. Surgical management of bone metastases: Quality of evidence and systematic review. Ann Surg Oncol. 2014, 21, 4081–4089. [Google Scholar] [CrossRef]
- Bauer, H.C.F.; Wedin, R. Survival after surgery for spinal and extremity metastases. Prognostication in 241 patients. Acta Orthop. Scand. 1995, 66, 143–146. [Google Scholar] [CrossRef]
- Steensma, M.; Healey, J.H. Trends in the Surgical Treatment of Pathologic Proximal Femur Fractures among Musculoskeletal Tumor Society Members. Clin. Orthop. Relat. Res. 2013, 471, 2000–2006. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Owari, T.; Miyake, M.; Nakai, Y.; Tanaka, N.; Itami, Y.; Hirao, S.; Momose, H.; Nakagawa, Y.; Iida, K.; Maesaka, F.; et al. External validation of a genitourinary cancer-specific prognostic scoring system to predict survival for patients with bone metastasis (modified B-FOM scoring model): Comparison with other scoring models in terms of accuracy. J. Bone Oncol. 2020, 26, 100344. [Google Scholar] [CrossRef] [PubMed]
- Deng, J.; Zhang, D.; Zhang, W.; Li, J. Construction and Validation of New Nomograms to Predict Risk and Prognostic Factors of Breast Cancer Bone Metastasis in Asian Females: A Population-Based Retrospective Study. Int. J. Gen. Med. 2021, 14, 8881–8902. [Google Scholar] [CrossRef] [PubMed]
- Takeshita, S.; Todo, Y.; Matsumiya, H.; Okamoto, K.; Yamashiro, K.; Kato, H. A prediction model of survival for patients with bone metastasis from uterine corpus cancer. Jpn. J. Clin. Oncol. 2016, 46, 973–978. [Google Scholar] [CrossRef]
- Tokuhashi, Y.; Matsuzaki, H.; Toriyama, S.; Kawano, H.; Ohsaka, S. Scoring System for the Preoperative Evaluation of Metastatic Spine Tumor Prognosis. Spine 1990, 15, 1110–1113. [Google Scholar] [CrossRef]
- Meares, C.; Badran, A.; Dewar, D. Prediction of survival after surgical management of femoral metastatic bone disease—A comparison of prognostic models. J. Bone Oncol. 2019, 15, 100225. [Google Scholar] [CrossRef]
- Alfaro, P.A.; Delgado, J.; Dumas, A.; Mesa, C.; Wevar, O.; Herrera, C.; Padilla, F.; Botello, E. Comparison between different prognostic models to be used for metastatic bone disease on appendicular skeleton in a Chilean population. Eur. J. Orthop. Surg. Traumatol. 2021, 31, 1657–1662. [Google Scholar] [CrossRef]
- Ragel, B.T.; Mendez, G.A.; Reddington, J.; Ferachi, D.; Kubicky, C.D.; Philipp, T.C.; Zusman, N.L.; Klimo, P.; Hart, R.; Yoo, J.; et al. Life Expectancy and Metastatic Spine Scoring Systems: An Academic Institutional Experience. Clin. Spine Surg. 2017, 30, 335–342. [Google Scholar] [CrossRef]
- Katagiri, H.; Okada, R.; Takagi, T.; Takahashi, M.; Murata, H.; Harada, H.; Nishimura, T.; Asakura, H.; Ogawa, H. New prognostic factors and scoring system for patients with skeletal metastasis. Cancer Med. 2014, 3, 1359–1367. [Google Scholar] [CrossRef]
- Chen, J.H.; Alagappan, M.; Goldstein, M.K.; Asch, S.M.; Altman, R. Decaying relevance of clinical data towards future decisions in data-driven inpatient clinical order sets. Int. J. Med Inform. 2017, 102, 71–79. [Google Scholar] [CrossRef]
- Steyerberg, E.W.; Vickers, A.J.; Cook, N.R.; Gerds, T.; Gonen, M.; Obuchowski, N.; Pencina, M.J.; Kattan, M.W. Assessing the performance of prediction models: A framework for traditional and novel measures. Epidemiology 2010, 21, 128–138. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hastie, T.; Tibshirani, R.; Friedman, J. The Elements of Statistical Learning: Data Mining, Inference, and Prediction; Springer: New York, NY, USA, 2009. [Google Scholar]
- Ratasvuori, M.; Wedin, R.; Hansen, B.H.; Keller, J.; Trovik, C.; Zaikova, O.; Bergh, P.; Kalen, A.; Laitinen, M. Prognostic role of en-bloc resection and late onset of bone metastasis in patients with bone-seeking carcinomas of the kidney, breast, lung, and prostate: SSG study on 672 operated skeletal metastases. J. Surg. Oncol. 2014, 110, 360–365. [Google Scholar] [CrossRef] [PubMed]
- Sørensen, M.S.; Gerds, T.A.; Hindsø, K.; Petersen, M.M. Prediction of survival after surgery due to skeletal metastases in the extremities. Bone Jt. J. 2016, 98-B, 271–277. [Google Scholar] [CrossRef] [PubMed]
- Sørensen, M.S.; Gerds, T.A.; Hindsø, K.; Petersen, M.M. External Validation and Optimization of the SPRING Model for Prediction of Survival after Surgical Treatment of Bone Metastases of the Extremities. Clin. Orthop. Relat. Res. 2018, 476, 1591–1599. [Google Scholar] [CrossRef]
- Willeumier, J.J.; van der Linden, Y.M.; van der Wal, C.W.P.G.; Jutte, P.C.; van der Velden, J.M.; Smolle, M.A.; van der Zwaal, P.; Koper, P.; Bakri, L.; de Pree, I.; et al. An Easy-to-Use Prognostic Model for Survival Estimation for Patients with Symptomatic Long Bone Metastases. J. Bone Jt. Surg. 2018, 100, 196–204. [Google Scholar] [CrossRef]
- Thio, Q.C.B.S.; Karhade, A.V.; Bindels, B.J.J.; Ogink, P.T.; Bramer, J.A.M.; Ferrone, M.L.; Calderón, S.L.; Raskin, K.A.; Schwab, J.H. Development and Internal Validation of Machine Learning Algorithms for Preoperative Survival Prediction of Extremity Metastatic Disease. Clin. Orthop. Relat. Res. 2020, 478, 322–333. [Google Scholar] [CrossRef]
- Forsberg, J.A.; Wedin, R.; Bauer, H.C.; Hansen, B.H.; Laitinen, M.; Trovik, C.S.; Keller, J.; Boland, P.J.; Healey, J.H. External validation of the Bayesian Estimated Tools for Survival (BETS) models in patients with surgically treated skeletal metastases. BMC Cancer 2012, 12, 493. [Google Scholar] [CrossRef] [Green Version]
- Anderson, A.B.; Wedin, R.; Fabbri, N.; Boland, P.; Healey, J.; Forsberg, J.A. External Validation of PATHFx Version 3.0 in Patients Treated Surgically and Nonsurgically for Symptomatic Skeletal Metastases. Clin. Orthop. Relat. Res. 2020, 478, 808–818. [Google Scholar] [CrossRef]
- Janssen, S.J.; Van Der Heijden, A.S.; Van Dijke, M.; Ready, J.E.; Raskin, K.A.; Ferrone, M.L.; Hornicek, F.J.; Schwab, J.H. 2015 Marshall Urist Young Investigator Award: Prognostication in Patients With Long Bone Metastases: Does a Boosting Algorithm Improve Survival Estimates? Clin. Orthop. Relat. Res. 2015, 473, 3112–3121. [Google Scholar] [CrossRef] [Green Version]
- Errani, C.; Cosentino, M.; Ciani, G.; Ferra, L.; Alfaro, P.A.; Bordini, B.; Donati, D.M. C-reactive protein and tumour diagnosis predict survival in patients treated surgically for long bone metastases. Int. Orthop. 2021, 45, 1337–1346. [Google Scholar] [CrossRef]
- Katagiri, H.; Takahashi, M.; Wakai, K.; Sugiura, H.; Kataoka, T.; Nakanishi, K. Prognostic factors and a scoring system for patients with skeletal metastasis. J. Bone Jt. Surgery. Br. 2005, 87, 698–703. [Google Scholar] [CrossRef] [PubMed]
- Quan, H.; Li, B.; Couris, C.M.; Fushimi, K.; Graham, P.; Hider, P.; Januel, J.-M.; Sundararajan, V. Updating and Validating the Charlson Comorbidity Index and Score for Risk Adjustment in Hospital Discharge Abstracts Using Data From 6 Countries. Am. J. Epidemiol. 2011, 173, 676–682. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jung, S.-H.; Yang, D.-H.; Ahn, J.-S.; Lee, S.-S.; Ahn, S.-Y.; Kim, Y.-K.; Kim, H.; Lee, J.-J. Decreased body mass index is associated with poor prognosis in patients with multiple myeloma. Ann Hematol. 2014, 93, 835–840. [Google Scholar] [CrossRef]
- Bollen, L.; Van Der Linden, Y.M.; Pondaag, W.; Fiocco, M.; Pattynama, B.P.M.; Marijnen, C.; Nelissen, R.; Peul, W.C.; Dijkstra, P.S. Prognostic factors associated with survival in patients with symptomatic spinal bone metastases: A retrospective cohort study of 1 043 patients. Neuro-Oncology 2014, 16, 991–998. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bongers, M.E.R.; Thio, Q.C.B.S.; Karhade, A.V.; Stor, M.L.; Raskin, K.A.; Calderon, S.A.L.; DeLaney, T.F.; Ferrone, M.L.; Schwab, J.H. Does the SORG Algorithm Predict 5-year Survival in Patients with Chondrosarcoma? An External Validation. Clin. Orthop. Relat. Res. 2019, 477, 2296–2303. [Google Scholar] [CrossRef] [PubMed]
- Forsberg, J.A.; Sjoberg, D.; Chen, Q.-R.; Vickers, A.; Healey, J.H. Treating Metastatic Disease: Which Survival Model Is Best Suited for the Clinic? Clin. Orthop. Relat. Res. 2013, 471, 843–850. [Google Scholar] [CrossRef] [Green Version]
- Piccioli, A.; Spinelli, M.S.; Forsberg, J.A.; Wedin, R.; Healey, J.H.; Ippolito, V.; Daolio, P.A.; Ruggieri, P.; Maccauro, G.; Gasbarrini, A.; et al. How do we estimate survival? External validation of a tool for survival estimation in patients with metastatic bone disease—decision analysis and comparison of three international patient populations. BMC Cancer 2015, 15, 424. [Google Scholar] [CrossRef]
- Ogura, K.; Gokita, T.; Shinoda, Y.; Kawano, H.; Takagi, T.; Ae, K.; Kawai, A.; Wedin, R.; Forsberg, J.A. Can A Multivariate Model for Survival Estimation in Skeletal Metastases (PATHFx) Be Externally Validated Using Japanese Patients? Clin. Orthop. Relat. Res. 2017, 475, 2263–2270. [Google Scholar] [CrossRef] [Green Version]
- Forsberg, J.A.; Wedin, R.; Boland, P.J.; Healey, J. Can We Estimate Short- and Intermediate-term Survival in Patients Undergoing Surgery for Metastatic Bone Disease? Clin. Orthop. Relat. Res. 2017, 475, 1252–1261. [Google Scholar] [CrossRef] [Green Version]
- Overmann, A.L.; Clark, D.M.; Tsagkozis, P.; Wedin, R.; Forsberg, J.A. Validation of PATHFx 2.0: An open-source tool for estimating survival in patients undergoing pathologic fracture fixation. J. Orthop. Res. 2020, 38, 2149–2156. [Google Scholar] [CrossRef]
- Alba, A.C.; Agoritsas, T.; Walsh, M.; Hanna, S.; Iorio, A.; Devereaux, P.J.; McGinn, T.; Guyatt, G. Discrimination and Calibration of Clinical Prediction Models: Users’ Guides to the Medical Literature. JAMA 2017, 318, 1377–1384. [Google Scholar] [CrossRef] [PubMed]
- Siontis, G.C.; Tzoulaki, I.; Castaldi, P.J.; Ioannidis, J.P. External validation of new risk prediction models is infrequent and reveals worse prognostic discrimination. J. Clin. Epidemiol. 2015, 68, 25–34. [Google Scholar] [CrossRef] [PubMed]


| Study ID—Ref | Type (y) | Patients (n) | Prognostic Factors (Number of Categories) | Intervention | Survival (m) | External Validation (n) |
|---|---|---|---|---|---|---|
| PATHfx. 1.0 Foresberg et al. (2011) [3] | Retrospective (1999–2009) | 815 | Age (y), Sex (2), Diagnostic group (3), Visceral metastases (2), Surgeon’s estimate survival (4), Pathologic/Impending fx (2), Lymph node involvement (2), Skeletal metastases (2), Preoperative Hb (4) and lymphocyte count (4), ECOG performance score (3) | Surgery | 3,12 | Yes |
| PATHfx 3.0 Anderson et al. (2019) [29] | Retrospective (1999–2003) (2015–2018) | 397 | Age (y), Sex (2), Diagnostic group (3), Visceral metastases (2), Surgeon’s estimate survival (4), Pathologic/Impending fx (2), Lymph node involvement (2), Skeletal metastases (2), Preoperative Hb (4) and lymphocyte count (4), ECOG performance score (3) | Surgery | 3,6,12,18,24 | Yes |
| SPRING 2008 Sorensen et al. (2016) [24] | Retrospective (2003–2008) | 121 | Diagnostic group (3), Hemoglobin (c), Visceral metastases (2), Bone metastases (2), Fracture/impending fracture (2), ASA group (2) and KPS (2) | EPR | 3,6,12 | No |
| SPRING 2013. Sorensen et al. (2018) [25] | Retrospective (2003–2013) | 270 | Diagnostic group (3), Hemoglobin (continuous), Visceral metastases (2), Bone metastases (2), fracture/impending fracture (2), ASA group (2) and KPS (2) | EPR | 3,6,12 | Yes |
| 7SSG. Ratasvuori et al. (2013) [23] | Retrospective (1999–2009) | 833 | Single bone metastases (2), Absence of visceral metastases (2), Primary tumor location in breast, kidney, thyroid, myeloma or lymphoma (2), KPS (2) | Surgery | 6,12 | Yes |
| OPTIModel. Willeumier et al. (2018) [26] | Retrospective (2000–2013) | 1520 | Diagnostic group (3), KPS (2), Visceral metastases (2) | RT or Surgery | 3,6,12 | Yes |
| SORG. Thio et al. (2019) [27] | Retrospective (1999–2017) | 1090 Training + Validation Datasets | Albumin (c), Neutrophil-to-lymphocyte ratio (c), Diagnostic group (3), ALP (c), Hemoglobin (c), Calcium (c) Absolute neutrophil count (c), WBC (C), Age, Platelet count (c), Visceral metastases (2), Sodium (c), Platelet-to-lymphocyte ratio | Surgery | 1,12 | No |
| Janssen et al. (2015) [30] | Retrospective (2009–2013) | 927 Training + Validation Datasets | Age 65 or older (2), Additional comorbidity (2), BMI less than 18.5 kg/m2 (2), Tumor type other than breast, kidney, prostate, thyroid, myeloma or lymphoma (2), Bone metastases (2), Visceral metastases (2), Hemoglobin level 10 g/dL or less (2) | Surgery | 1,3,12 | Yes |
| IOR. Errani et al. (2021) [31] | Prospective (2015–2018) | 159 | Pathological C-reactive protein (2), Diagnostic group (2) | Surgery | 12 | Yes |
| Study Model | Study ID | Discrimination Accuracy (AUC) | Calibration (Brier Score) | ||||
|---|---|---|---|---|---|---|---|
| 3 Months | 6 Months | 12 Months | 3 Months | 6 Months | 12 Months | ||
| PATHfx 1.0 | Alfaro et al. [17] | 0.62 (0.49, 0.73) | 0.66 (0.56, 0.75) | 0.54 (0.38, 0.68) | NA | NA | NA |
| Meares et al. [16] | 0.70 (0.69, 0.7) | 0.70 (0.69, 0.70) | 0.71 (0.70, 0.71) | 0.23 (0.23, 0.23) | 0.23 (0.22, 0.23) | 0.19 (0.19, 0.19) | |
| Errani et al. [31] | 0.74 (NA) | ||||||
| PATHfx 3.0 | Anderson et al. [29] (IBMR) | 0.77 (0.70, 0.84) | 0.77 (0.70, 0.83) | 0.78 (0.71, 0.85) | 0.20 (0.16, 0.23) | 0.20 (0.17, 0.24) | 0.18 (0.15, 0.22) |
| Anderson et al. [29] (RT) | 0.83 (0.77, 0.90) | 0.79 (0.73, 0.86) | 0.79 (0.73, 0.86) | 0.14 (0.11, 0.17) | 0.20 (0.16, 0.24) | 0.20 (0.16, 0.24) | |
| SPRING 2013 | Sorensen et al. [25] | 0.82 (0.73, 0.91) | 0.85 (0.76, 0.93) | 0.86 (0.77, 0.95) | 0.16 (0.12, 0.19) | 0.16 (0.13, 0.20) | 0.15 (0.12, 0.19) |
| Meares et al. [16] | 0.66 (NA) | 0.68 (NA) | 0.76 (0.75, 0.76) | 0.25 (NA) | 0.26 (NA) | 0.19 (NA) | |
| OPTIModel | Alfaro et al. [17] | 0.57 (0.44, 0.69) | 0.64 (0.54, 0.73) | 0.55 (0.39, 0.70) | NA | NA | NA |
| Meares et al. [16] | 0.66 (NA) | 0.67 (NA) | 0.79 (0.78, 0.79) | 0.21 (NA) | 0.24 (NA) | 0.16 (0.16, 0.16) | |
| Errani et al. [31] | 0.751 (NA) | ||||||
| IOR | Alfaro et al. [17] | NA | NA | 0.65 (0.50, 0.79) | NA | NA | NA |
| Janssen | Meares et al. [16] | 0.68 (NA) | NA | 0.71 (0.70, 0.71) | 0.21 (NA) | NA | 0.22 (0.22, 0.22) |
| 7SSG | Meares et al. [16] | 0.63 (NA) | 0.64 (NA) | 0.62 (NA) | 0.22 (NA) | 0.24 (NA) | 0.21 (NA) |
| Errani et al. [31] | 0.72 (NA) | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ben Gal, O.; Soh, T.C.F.; Vaughan, S.; Jayasanker, V.; Mahendra, A.; Gupta, S. The Prediction of Survival after Surgical Management of Bone Metastases of the Extremities—A Comparison of Prognostic Models. Curr. Oncol. 2022, 29, 4703-4716. https://doi.org/10.3390/curroncol29070373
Ben Gal O, Soh TCF, Vaughan S, Jayasanker V, Mahendra A, Gupta S. The Prediction of Survival after Surgical Management of Bone Metastases of the Extremities—A Comparison of Prognostic Models. Current Oncology. 2022; 29(7):4703-4716. https://doi.org/10.3390/curroncol29070373
Chicago/Turabian StyleBen Gal, Ofir, Terrence Chi Fang Soh, Sarah Vaughan, Viswanath Jayasanker, Ashish Mahendra, and Sanjay Gupta. 2022. "The Prediction of Survival after Surgical Management of Bone Metastases of the Extremities—A Comparison of Prognostic Models" Current Oncology 29, no. 7: 4703-4716. https://doi.org/10.3390/curroncol29070373
APA StyleBen Gal, O., Soh, T. C. F., Vaughan, S., Jayasanker, V., Mahendra, A., & Gupta, S. (2022). The Prediction of Survival after Surgical Management of Bone Metastases of the Extremities—A Comparison of Prognostic Models. Current Oncology, 29(7), 4703-4716. https://doi.org/10.3390/curroncol29070373




