Increased MIB-1 Labeling Index Is Associated with Abducens Nerve Morbidity in Primary Sporadic Petroclival Meningioma Surgery: Beyond Location and Approach
Abstract
:1. Introduction
2. Materials and Methods
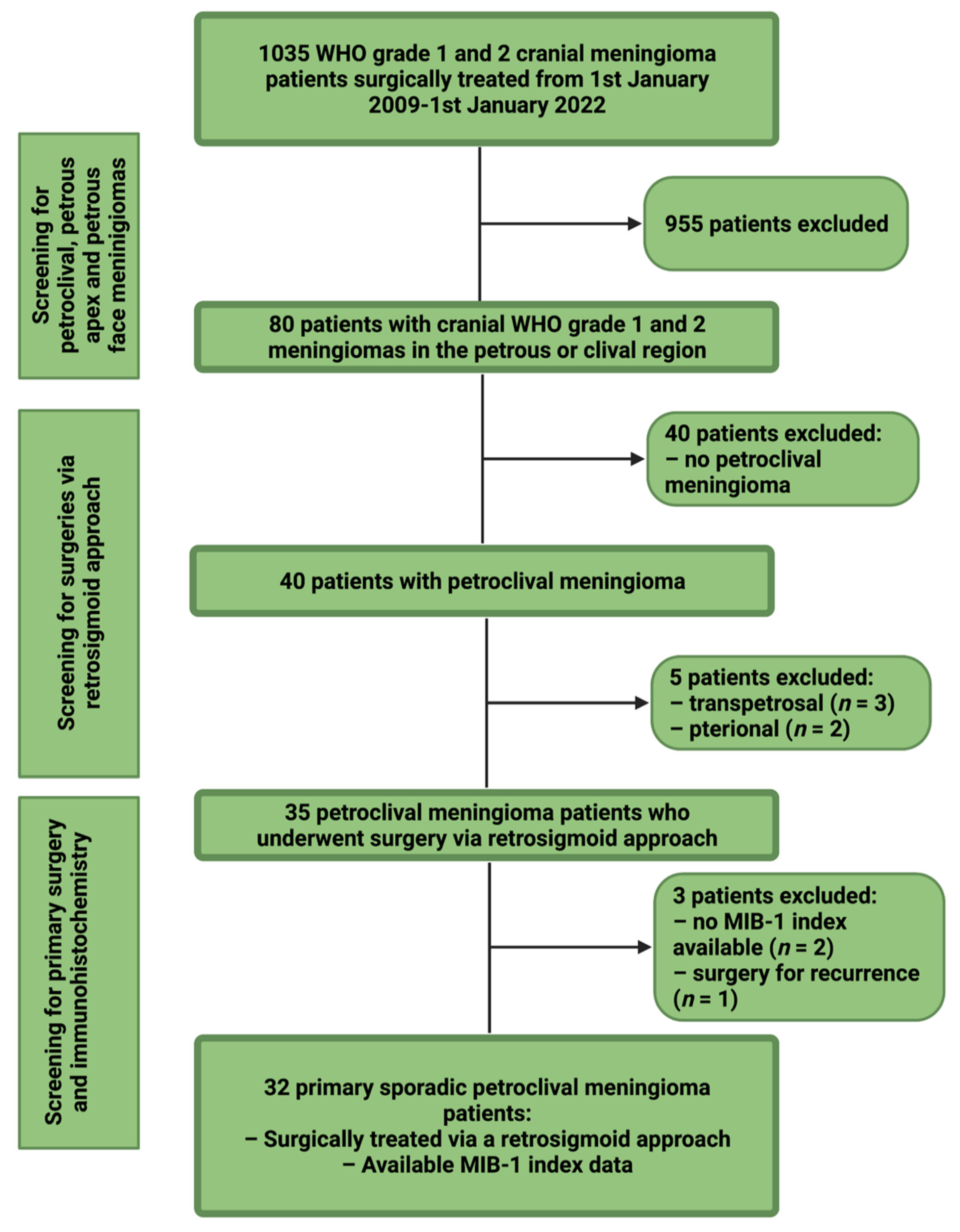
2.1. Study Design and Patient Characteristics
2.2. Data Recording
2.3. Institutional Treatment Strategy for Petroclival Meningiomas
2.4. Surgical Workflow
2.5. Neuropathology
2.6. Statistical Analysis
3. Results
3.1. Baseline Patient Characteristics
3.2. Neuropathological Grading, Extent of Resection, and Postoperative Functioning
3.3. Diagnostic Performance of the MIB-1 Index in the Association with Postoperative Abducens Nerve Palsy
3.4. Association between New-Onset Abducens Nerve Palsy and Clinical, Tumor Morphology, and Neuropathological Characteristics
3.5. Perioperative Development of Preoperatively Existing Abducens Nerve Palsy after PC MNG Surgery
3.6. MIB-1 Index and Other New-Onset Cranial Nerve Palsies
3.7. MIB-1 Index and Probability of Progression-Free Survival after Petroclival Meningioma Surgery via Retrosigmoid Approach
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ostrom, Q.T.; Gittleman, H.; Fulop, J.; Liu, M.; Blanda, R.; Kromer, C.; Wolinsky, Y.; Kruchko, C.; Barnholtz-Sloan, J.S. CBTRUS Statistical Report: Primary Brain and Central Nervous System Tumors Diagnosed in the United States in 2008–2012. Neuro Oncol. 2015, 17 (Suppl. S4), iv1–iv62. [Google Scholar] [CrossRef] [PubMed]
- Domingues, P.H.; Sousa, P.; Otero, Á.; Gonçalves, J.M.; Ruiz, L.; de Oliveira, C.; Lopes, M.C.; Orfao, A.; Tabernero, M.D. Proposal for a new risk stratification classification for meningioma based on patient age, WHO tumor grade, size, localization, and karyotype. Neuro Oncol. 2014, 16, 735–747. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Louis, D.N.; Perry, A.; Wesseling, P.; Brat, D.J.; Cree, I.A.; Figarella-Branger, D.; Hawkings, C.; Ng, H.K.; Pfister, S.M.; Reifenberger, G.; et al. The 2021 WHO Classification of Tumors of the Central Nervous System: A summary. Neuro Oncol. 2021, 23, 1231–1251. [Google Scholar] [CrossRef] [PubMed]
- Alexiou, G.A.; Gogou, P.; Markoula, S.; Kyritsis, A.P. Management of meningiomas. Clin. Neurol Neurosurg. 2010, 112, 177–182. [Google Scholar] [CrossRef]
- Castellano, F.; Ruggiero, G. Meningiomas of the posterior fossa. Acta Radiol. Suppl. 1953, 104, 1–177. [Google Scholar]
- Martínez, R.; Vaquero, J.; Areitio, E.; Bravo, G. Meningiomas of the posterior fossa. Surg. Neurol. 1983, 19, 237–243. [Google Scholar] [CrossRef]
- Nishimura, S.; Hakuba, A.; Jang, B.J.; Inoue, Y. Clivus and apicopetroclivus meningiomas—Report of 24 cases. Neurol. Med. Chir. 1989, 29, 1004–1011. [Google Scholar] [CrossRef] [Green Version]
- Diluna, M.L.; Bulsara, K.R. Surgery for petroclival meningiomas: A comprehensive review of outcomes in the skull base surgery era. Skull Base 2010, 20, 337–342. [Google Scholar] [CrossRef] [Green Version]
- Meling, T.R.; Da Broi, M.; Scheie, D.; Helseth, E.; Smoll, N.R. Meningioma Surgery-Are We Making Progress? World Neurosurg. 2019, 125, e205–e213. [Google Scholar] [CrossRef]
- Samii, M.; Ammirati, M.; Mahran, A.; Bini, W.; Sepehrnia, A. Surgery of petroclival meningiomas: Report of 24 cases. Neurosurgery 1989, 24, 12–17. [Google Scholar] [CrossRef]
- Couldwell, W.T.; Fukushima, T.; Giannotta, S.L.; Weiss, M.H. Petroclival meningiomas: Surgical experience in 109 cases. J. Neurosurg. 1996, 84, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Zhang, Q.; Weng, J.C.; Chen, L.P.; Li, D.; Jia, G.J.; Zhang, L.W.; Wu, Z.; Jia, W.; Zhang, J.T. A clinical study of ocular motor nerve functions after petroclival meningioma resection. Acta Neurochir. 2020, 162, 1249–1257. [Google Scholar] [CrossRef] [PubMed]
- Seifert, V. Clinical management of petroclival meningiomas and the eternal quest for preservation of quality of life: Personal experiences over a period of 20 years. Acta Neurochir. 2010, 152, 1099–1116. [Google Scholar] [CrossRef] [PubMed]
- Spetzler, R.F.; Daspit, C.P.; Pappas, C.T. The combined supra- and infratentorial approach for lesions of the petrous and clival regions: Experience with 46 cases. J. Neurosurg. 1992, 76, 588–599. [Google Scholar] [CrossRef] [PubMed]
- Gerdes, J.; Schwab, U.; Lemke, H.; Stein, H. Production of a mouse monoclonal antibody reactive with a human nuclear antigen associated with cell proliferation. Int. J. Cancer 1983, 31, 13–20. [Google Scholar] [CrossRef]
- Scholzen, T.; Gerdes, J. The Ki-67 protein: From the known and the unknown. J. Cell. Physiol. 2000, 182, 311–322. [Google Scholar] [CrossRef]
- Wach, J.; Lampmann, T.; Güresir, Á.; Schuss, P.; Vatter, H.; Herrlinger, U.; Becker, A.; Hölzel, M.; Toma, M.; Güresir, E. FORGE: A Novel Scoring System to Predict the MIB-1 Labeling Index in Intracranial Meningiomas. Cancers 2021, 13, 3643. [Google Scholar] [CrossRef]
- Liu, N.; Song, S.Y.; Jiang, J.B.; Wang, T.J.; Yan, C.X. The prognostic role of Ki-67/MIB-1 in meningioma: A systematic review with meta-analysis. Medicine 2020, 99, e18644. [Google Scholar] [CrossRef]
- Mirian, C.; Skyrman, S.; Bartek, J., Jr.; Jensen, L.R.; Kihlström, L.; Förander, P.; Orrego, A.; Mathiesen, T. The Ki-67 Proliferation Index as a Marker of Time to Recurrence in Intracranial Meningioma. Neurosurgery 2020, 87, 1289–1298. [Google Scholar] [CrossRef]
- Oya, S.; Kawai, K.; Nakatomi, H.; Saito, N. Significance of Simpson grading system in modern meningioma surgery: Integration of the grade with MIB-1 labeling index as a key to predict the recurrence of WHO Grade I meningiomas. J. Neurosurg. 2012, 117, 121–128. [Google Scholar] [CrossRef] [Green Version]
- Wach, J.; Lampmann, T.; Güresir, A.; Vatter, H.; Herrlinger, U.; Becker, A.; Cases-Cunillera, S.; Hölzel, M.; Toma, M.; Güresir, E. Proliferative Potential, and Inflammatory Tumor Microenvironment in Meningioma Correlate with Neurological Function at Presentation and Anatomical Location-From Convexity to Skull Base and Spine. Cancers 2022, 14, 1033. [Google Scholar] [CrossRef] [PubMed]
- Antinheimo, J.; Haapasalo, H.; Haltia, M.; Tatagiba, M.; Thomas, S.; Brandis, A.; Sainio, M.; Carpen, O.; Samii, M.; Jääskeläinen, J. Proliferation potential and histological features in neurofibromatosis 2-associated and sporadic meningiomas. J. Neurosurg. 1997, 87, 610–614. [Google Scholar] [CrossRef] [PubMed]
- Goldbrunner, R.; Minniti, G.; Preusser, M.; Jenkinson, M.D.; Sallabanda, K.; Houdart, E.; von Deimling, A.; Stavrinou, P.; Lefranc, F.; Lund-Johansen, M.; et al. EANO guidelines for the diagnosis and treatment of meningiomas. Lancet Oncol. 2016, 17, e383–e391. [Google Scholar] [CrossRef] [Green Version]
- Scott, A.B.; Kraft, S.P. Botulinium toxin injection in the management of lateral rectus paresis. Ophtalmology 1985, 92, 676–683. [Google Scholar] [CrossRef]
- Wach, J.; Apallas, S.; Schneider, M.; Güresir, A.; Schuss, P.; Herrlinger, U.; Vatter, H.; Güresir, E. Baseline Serum C-Reactive Protein and Plasma Fibrinogen-Based Score in the Prediction of Survival in Glioblastoma. Front. Oncol. 2021, 11, 653614. [Google Scholar] [CrossRef]
- Kim, B.W.; Kim, M.S.; Kim, S.W.; Chang, C.H.; Kim, O.L. Peritumoral brain edema in meningiomas: Correlation of radiologic and pathologic features. J. Korean Neurosurg. Soc. 2011, 49, 26–30. [Google Scholar] [CrossRef]
- Zhao, Z.; Yuan, X.; Yuan, J.; Cai, L.; Jiang, W.; Xie, Y.; Wanggou, S.; Zhang, C.; Tang, G.; Peng, Z.; et al. Treatment Strategy for Petroclival Meninigomas Based on a Proposed Classification in a Study of 168 Cases. Sci. Rep. 2020, 10, 4655. [Google Scholar] [CrossRef]
- Goldbrunner, R.; Stavrinou, P.; Jenkinson, M.D.; Sahm, F.; Mawrin, C.; Weber, D.C.; Preusser, M.; Minniti, G.; Lund-Johansen, M.; Lefranc, F.; et al. EANO guideline on the diagnosis and management of meninigiomas. Neuro Oncol. 2021, 23, 1821–1834. [Google Scholar] [CrossRef]
- Masalha, W.; Heiland, D.H.; Steiert, C.; Krueger, M.T.; Schnell, D.; Scheiwe, C.; Grosu, A.L.; Schnell, O.; Beck, J.; Grauvogel, J. A Retrospective Evaluation of the Retrosigmoid Approach for Petroclival Meningioma Surgery and Prognostic Factors Affecting Clinical Outcome. Front. Oncol. 2022, 12, 786909. [Google Scholar] [CrossRef]
- Wach, J.; Brandecker, S.; Güresir, A.; Schuss, P.; Vatter, H.; Güresir, E. The impact of the MIB-1 index on facial nerve outcomes in vestibular schwannoma surgery. Acta Neurochir. 2020, 162, 1205–1213. [Google Scholar] [CrossRef] [Green Version]
- Majores, M.; Schick, V.; Engels, G.; Fassunke, J.; Elger, C.E.; Schramm, J.; Blumcke, I.; Becker, A.J. Mutational and immunohistochemical analysis of ezrin-, radixin-, moesin (ERM) molecules in epilepsy-associated glioneuronal lesions. Acta Neuropathol. 2005, 110, 537–546. [Google Scholar] [CrossRef] [PubMed]
- Majores, M.; von Lehe, M.; Fassunke, J.; Schramm, J.; Becker, A.J.; Simon, M. Tumor recurrence and malignant progression of gangliogliomas. Cancer 2008, 113, 3355–3363. [Google Scholar] [CrossRef] [PubMed]
- Wach, J.; Lampmann, T.; Güresir, A.; Vatter, H.; Herrlinger, U.; Becker, A.; Toma, M.; Hölzel, M.; Güresir, E. Inflammatory Tumor Microenvironment in Cranial Meningiomas: Clinical Implications and Intraindividual Reproducibility. Diagnostics 2022, 12, 853. [Google Scholar] [CrossRef] [PubMed]
- Kawase, T.; Shiobara, R.; Ohira, T.; Toya, S. Developmental patterns and characteristic symptoms of petroclival meningiomas. Neurol. Med. Chir. 1996, 36, 1–6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bernard, F.; Troude, L.; Isnard, S.; Lemee, J.M.; Terrier, L.M.; Francois, P.; Velut, S.; Gay, E.; Fournier, H.D.; Roche, P.H. Long term surgical results of 154 petroclival meningiomas: A retrospective multicenter study. Neurochirurgie 2019, 65, 55–62. [Google Scholar] [CrossRef]
- Borghei-Razavi, H.; Tomio, R.; Fereshtehnejad, S.M. Pathological location of cranial nerves in petroclival lesions: How to avoid their injury during anterior petrosal approach. J. Neurol. Surg. B Skull Base 2016, 77, 6–13. [Google Scholar] [PubMed] [Green Version]
- Yoo, J.; Lim, S.H.; Jung, I.H.; Park, H.H.; Han, J.; Hong, C.K. Factors Associated with Abducens Nerve Palsy in Patients Undergoing Surgery for Petroclival Meningiomas. J. Neuroophtalmol. 2022, 42, e209–e216. [Google Scholar] [CrossRef]
- Kato, Y.; Nishihara, H.; Mohri, H.; Kanno, H.; Kobayashi, H.; Kimura, T.; Tanino, M.; Terasaka, S.; Tanaka, S. Clinicopathological evaluation of cyclooxygenase-2 expression in meningioma immunohistochemical analysis of 76 cases of low and high-grade meningioma. Brain Tumor Pathol. 2014, 31, 23–30. [Google Scholar] [CrossRef] [Green Version]
- Wilgus, T.A.; Bergdall, V.K.; Tober, K.L.; Hill, K.J.; Mitra, S.; Flavahan, N.A.; Oberyszyn, T.M. The impact of cyclooxygenase-2 mediated inflammation on scarless fetal wound healing. Am. J. Pathol. 2004, 165, 753–761. [Google Scholar] [CrossRef] [Green Version]
- Ide, M.; Jimbo, M.; Yamamoto, M.; Umebara, Y.; Hagiwara, S.; Kubo, O. MIB-1 staining index and peritumoral brain edema of meninigomas. Cancer 1996, 78, 133–143. [Google Scholar] [CrossRef]
- Coons, S.W.; Johnson, P.C. Regional heterogeneity in the proliferative activity of human gliomas as measured by the Ki-67 labeling index. J. Neuropathol. Exp. Neurol. 1993, 120, 1278–1287. [Google Scholar] [CrossRef]
- Kirkegaard, L.J.; DeRose, P.B.; Yao, B.; Cohen, C. Image cytometric measurement of nuclear proliferation markers (MIB-1, PCNA) in astrocytomas. Prognostic significance. Am. J. Clin. Pathol. 1998, 109, 69–74. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cui, Y.; Li, J.; Zhu, Y.; Tang, H.; He, X.; Xu, Y. The neuroprotective effects of aspirin following crush injury to rat sciatic nerve. Int. J. Clin. Exp. Med. 2015, 8, 18185–18190. [Google Scholar] [PubMed]
- Moriya, J.; Tanino, M.A.; Takenami, T.; Endoh, T.; Urushido, M.; Kato, Y.; Wang, L.; Kimura, T.; Tsuda, M.; Nishihara, H.; et al. Rapid immunocytochemistry based on alternating electric field using squash smear preparation of central nervous system tumors. Brain Tumor Pathol. 2016, 33, 13–18. [Google Scholar] [CrossRef] [PubMed]
- Terata, K.; Saito, H.; Nanjo, H.; Hiroshima, Y.; Ito, S.; Narita, K.; Akagami, Y.; Nakamura, R.; Konno, H.; Ito, A.; et al. Novel rapid-immunohistochemistry using an alternating current electric field for intraoperative diagnosis of sentinel lymph nodes in breast cancer. Sci. Rep. 2017, 7, 2810. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oya, S.; Yoshida, S.; Tsuchiya, T.; Fujisawa, N.; Mukasa, A.; Nakatomi, H.; Saito, N.; Matsui, T. Intraoperative quantification of meningioma cell proliferation potential using rapid flow cytometry reveals intratumoral heterogeneity. Cancer Med. 2019, 8, 2793–2801. [Google Scholar] [CrossRef] [Green Version]




| Median Age (IQR) (in Y) | 56 (46–70) |
|---|---|
| Sex Female Male | 25 (78.1%) 7 (21.9%) |
| BMI, Mean ± SD | 26.5 ± 5.4 |
| Median preoperative KPS (IQR) | 90 (80–90) |
| Preoperative cranial nerve deficits CN II CN III CN IV CN V CN VI CN VII CN VIII Lower cranial nerve group | 26 (81.3%) 5 (15.6%) 4 (12.5%) 1 (3.1%) 12 (37.5%) 8 (25.0%) 6 (18.8%) 8 (25.0%) 7 (21.9%) |
| Tumor volume, cm3, median (IQR) | |
| Cavernous sinus infiltration | 19 (59.4%) |
| Internal auditory canal invasion | 12 (37.5%) |
| Peritumoral edema | 8 (25.0%) |
| Brainstem compression | 23 (71.9%) |
| Simpson grade Simpson grade I Simpson grade II Simpson grade III Simpson grade IV | 3 (9.4%) 9 (28.1%) 18 (56.35) 2 (6.3%) |
| New-onset of cranial deficits CN II CN III CN IV CN V CN VI CN VII CN VIII Lower cranial nerve group | 15 (46.9%) 0 (0%) 5 (15.6%) 2 (6.3%) 2 (6.3%) 7 (21.9%) 4 (12.5%) 2 (6.3%) 5 (15.6%) |
| WHO grade WHO grade 1 WHO grade 2 | 28 (87.5%) 4 (12.5%) |
| MIB-1 index, Median (IQR) | 4.0 (3.0-5.0) |
| Brain invasion | 0 (0%) |
| Mitotic figures | |
| CD68 staining Diffuse Focal none | 16 (50.0%) 11 (34.4%) 5 (15.6%) |
| Characteristics | MIB-1 Index < 4% (13/32; 40.6%) | MIB-1 Index ≥ 4% (19/32; 59.4%) | p-Value |
|---|---|---|---|
| Age (years), mean ± SD | 56.0 ± 14.2 | 58.6 ± 12.6 | 0.59 |
| Sex Female Male | 12 (92.3%) 1 (7.7%) | 13 (68.4%) 6 (31.6%) | 0.20 |
| Body mass index, mean ± SD | 26.2 ± 5.4 | 26.6 ± 5.6 | 0.84 |
| Preoperative KPS, mean ± SD | 86.2 ± 10.4 | 84.7 ± 9.6 | 0.70 |
| Tumor volume, cm3, mean ± SD | 14.2 cm3 ± 9.1 | 22.2 cm3 ± 14.1 | 0.09 |
| Serum c-reactive protein, mean ± SD | 5.3 ± 6.3 | 3.2 ± 4.3 | 0.22 |
| White blood cell count, mean ± SD | 6.5 ± 1.9 | 8.1 ± 2.7 | 0.07 |
| Cavernous sinus infiltration Present Absent | 6 (53.8%) 7 (46.2%) | 13 (68.4%) 6 (31.6%) | 0.28 |
| Internal auditory canal invasion Present Absent | 4 (30.8%) 9 (69.2%) | 8 (42.1%) 11 (57.9%) | 0.71 |
| Peritumoral edema Present Absent | 0 (0.0%) 13 (100.0%) | 8 (42.1%) 11 (57.9%) | 0.01 |
| Brainstem compression Present Absent | 8 (61.5%) 5 (38.5%) | 15 (78.9%) 4 (21.1%) | 0.43 |
| Simpson grade <III ≥III | 7 (53.8%) 6 (46.2%) | 5 (28.6%) 14 (71.4%) | 0.15 |
| WHO grade 1 2 | 12 (92.3%) 1 (7.7%) | 16 (84.2%) 3 (15.8%) | 0.63 |
| CD68 staining Diffuse Focal none | 4 (30.8%) 7 (53.8%) 2 (15.4%) | 12 (63.2%) 4 (21.1%) 3 (15.8%) | 0.14 |
| Characteristics | No CN VI Palsy (25/32; 78.12%) | New-Onset CN VI Palsy (7/32; 21.88%) | p-Value |
|---|---|---|---|
| Age (years), mean ± SD | 57.9 ± 14.1 | 56.4 ± 9.7 | 0.80 |
| Sex Female Male | 20 (80.0%) 5 (20.0%) | 5 (71.4%) 2 (28.6%) | 0.63 |
| Body mass index, mean ± SD | 26.6 ± 5.9 | 25.9 ± 3.9 | 0.75 |
| Preoperative KPS, mean ± SD | 84.4 ± 10.0 | 88.6 ± 9.0 | 0.33 |
| volume, cm3, mean ± SD | 17.8 cm3 ± 12.5 | 22.3 cm3 ± 17.6 | 0.87 |
| Cavernous sinus infiltration Present Absent | 14 (56.0%) 11 (44.0%) | 5 (71.4%) 2 (28.6%) | 0.33 |
| Internal auditory canal invasion Present Absent | 9 (36.0%) 16 (64.0%) | 3 (42.9%) 4 (57.1%) | 0.99 |
| Peritumoral edema Present Absent | 4 (16.0%) 21 (84.0%) | 4 (57.1%) 3 (42.9%) | 0.047 |
| Brainstem compression Present Absent | 18 (72.0%) 7 (28.0%) | 5 (71.4%) 2 (28.6%) | 0.99 |
| Simpson grade <III ≥III | 10 (40.0%) 15 (60.0%) | 2 (28.6%) 5 (71.4%) | 0.68 |
| WHO grade 1 2 | 22 (88.0%) 3 (12.0%) | 6 (85.7%) 1 (14.3%) | 0.99 |
| MIB-1 Index <4% ≥4% | 13 (52.0%) 12 (48.0%) | 0 (0.0%) 7 (100.0%) | 0.025 |
| Mitotic figures, mean ± SD | 1.5 ± 2.3 | 1.1 ± 0.9 | 0.71 |
| CD68 staining Diffuse Focal/none | 12 (48.0%) 13 (52.0%) | 4 (57.1%) 3 (42.9%) | 0.99 |
| Cranial Nerves | Mean MIB-1 Index ± SD | p-Value | Peritumoral Edema | p-Value |
|---|---|---|---|---|
| CN III New-onset palsy (n = 5) Normal (n = 27) | 4.20 ± 1.1 4.15 ± 2.8 | 0.97 | 2 (40.0%) 6 (22.2%) | 0.58 |
| CN IV New-onset palsy (n = 2) Normal (n = 30) | 4.50 ± 0.7 4.13 ± 2.7 | 0.85 | 1 (50.0%) 7 (23.3%) | 0.44 |
| CN V New-onset palsy (n = 2) Normal (n = 30) | 5.00 ± 0.0 4.1 ± 2.7 | 0.64 | 2 (100.0%) 6 (20.0%) | 0.06 |
| CN VII New-onset palsy (n = 4) Normal (n = 28) | 4.00 ± 2.5 4.18 ± 2.7 | 0.90 | 2 (50.0%) 6 (21.4%) | 0.25 |
| CN VIII New-onset palsy (n = 2) Normal (n = 30) | 5.00 ± 0.00 4.10 ± 2.7 | 0.64 | 2 (100.0%) 6 (20.0%) | 0.06 |
| Lower cranial nerve group New-onset palsy (n = 5) Normal (n = 27) | 3.80 ± 1.3 4.22 ± 2.8 | 0.74 | 2 (40.0%) 6 (22.2%) | 0.58 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wach, J.; Lampmann, T.; Güresir, Á.; Vatter, H.; Herrlinger, U.; Becker, A.; Toma, M.; Hölzel, M.; Güresir, E. Increased MIB-1 Labeling Index Is Associated with Abducens Nerve Morbidity in Primary Sporadic Petroclival Meningioma Surgery: Beyond Location and Approach. Curr. Oncol. 2022, 29, 5026-5041. https://doi.org/10.3390/curroncol29070398
Wach J, Lampmann T, Güresir Á, Vatter H, Herrlinger U, Becker A, Toma M, Hölzel M, Güresir E. Increased MIB-1 Labeling Index Is Associated with Abducens Nerve Morbidity in Primary Sporadic Petroclival Meningioma Surgery: Beyond Location and Approach. Current Oncology. 2022; 29(7):5026-5041. https://doi.org/10.3390/curroncol29070398
Chicago/Turabian StyleWach, Johannes, Tim Lampmann, Ági Güresir, Hartmut Vatter, Ulrich Herrlinger, Albert Becker, Marieta Toma, Michael Hölzel, and Erdem Güresir. 2022. "Increased MIB-1 Labeling Index Is Associated with Abducens Nerve Morbidity in Primary Sporadic Petroclival Meningioma Surgery: Beyond Location and Approach" Current Oncology 29, no. 7: 5026-5041. https://doi.org/10.3390/curroncol29070398






