Predictive Factors for Bilateral Disease in Papillary Microcarcinoma: A Retrospective Cohort Study
Abstract
:1. Introduction
2. Material and Methods
3. Results
3.1. Overall Collective
3.2. Bilateral Tumor Manifestation with One Solo Tumor in One Thyroid Lobe
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ross, D.S.; Litofsky, D.; Ain, K.; Bigos, T.; Brierley, J.D.; Cooper, D.S.; Haugen, B.R.; Jonklaas, J.; Ladenson, P.W.; Magner, J.; et al. Recurrence After Treatment of Micropapillary Thyroid Cancer. Thyroid 2009, 19, 1043–1048. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.K.; Park, I.; Woo, J.-W.; Lee, J.H.; Choe, J.-H.; Kim, J.-H.; Kim, J.S. Total thyroidectomy versus lobectomy in conventional papillary thyroid microcarcinoma: Analysis of 8,676 patients at a single institution. Surgery 2017, 161, 485–492. [Google Scholar] [CrossRef] [PubMed]
- Haugen, B.R.; Alexander, E.K.; Bible, K.C.; Doherty, G.M.; Mandel, S.J.; Nikiforov, Y.E.; Pacini, F.; Randolph, G.W.; Sawka, A.M.; Schlumberger, M.; et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 2016, 26, 1–133. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sugitani, I.; Ito, Y.; Takeuchi, D.; Nakayama, H.; Masaki, C.; Shindo, H.; Teshima, M.; Horiguchi, K.; Yoshida, Y.; Kanai, T.; et al. Indications and Strategy for Active Surveillance of Adult Low-Risk Papillary Thyroid Microcarcinoma: Consensus Statements from the Japan Association of Endocrine Surgery Task Force on Management for Papillary Thyroid Microcarcinoma. Thyroid 2021, 31, 183–192. [Google Scholar] [CrossRef]
- Noguchi, S.; Yamashita, H.; Uchino, S.; Watanabe, S. Papillary Microcarcinoma. World J. Surg. 2008, 32, 747–753. [Google Scholar] [CrossRef] [Green Version]
- Mercante, G.; Frasoldati, A.; Pedroni, C.; Formisano, D.; Renna, L.; Piana, S.; Gardini, G.; Valcavi, R.; Barbieri, V. Prognostic Factors Affecting Neck Lymph Node Recurrence and Distant Metastasis in Papillary Microcarcinoma of the Thyroid: Results of a Study in 445 Patients. Thyroid 2009, 19, 707–716. [Google Scholar] [CrossRef]
- Brito, J.P.; Ito, Y.; Miyauchi, A.; Tuttle, R.M. A Clinical Framework to Facilitate Risk Stratification When Considering an Active Surveillance Alternative to Immediate Biopsy and Surgery in Papillary Microcarcinoma. Thyroid 2016, 26, 144–149. [Google Scholar] [CrossRef] [Green Version]
- Miyauchi, A.; Kudo, T.; Ito, Y.; Oda, H.; Sasai, H.; Higashiyama, T.; Fukushima, M.; Masuoka, H.; Kihara, M.; Miya, A. Estimation of the lifetime probability of disease progression of papillary microcarcinoma of the thyroid during active surveillance. Surgery 2018, 163, 48–52. [Google Scholar] [CrossRef] [Green Version]
- Feng, J.; Gan, X.; Shen, F.; Cai, W.; Xu, B. The role of two tumor foci for predicting central lymph node metastasis in papillary thyroid carcinoma: A meta-analysis. Int. J. Surg. 2018, 52, 166–170. [Google Scholar] [CrossRef]
- Xue, S.; Wang, P.; Liu, J.; Chen, G. Total thyroidectomy may be more reasonable as initial surgery in unilateral multifocal papillary thyroid microcarcinoma: A single-center experience. World J. Surg. Oncol. 2017, 15, 62. [Google Scholar] [CrossRef] [Green Version]
- Goran, M.; Markovic, I.; Buta, M.; Gavrilovic, D.; Cvetkovic, A.; Santrac, N.; Rakovic, M.; Milijic, N.M.; Dzodic, R. The influence of papillary thyroid microcarcinomas size on the occurrence of lymph node metastases. J BUON 2019, 24, 2120–2126. [Google Scholar] [PubMed]
- Sugitani, I.; Ito, Y.; Miyauchi, A.; Imai, T.; Suzuki, S. Active Surveillance Versus Immediate Surgery: Questionnaire Survey on the Current Treatment Strategy for Adult Patients with Low-Risk Papillary Thyroid Microcarcinoma in Japan. Thyroid 2019, 29, 1563–1571. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhou, B.; Wei, L.; Qin, J. Does Multifocal Papillary Thyroid Microcarcinoma With a Total Tumor Diameter >1 cm Indicate Poor Biological Behavior? The Evidence is Insufficient. Endocr. Pract. 2021, 27, 131–136. [Google Scholar] [CrossRef] [PubMed]
- Tam, A.A.; Ozdemir, D.; Ogmen, B.E.; Fakı, S.; Dumlu, E.G.; Yazgan, A.K.; Ersoy, R.; Cakır, B. Should multifocal papillary thyroid carcinomas classified as T1a with a tumor diameter sumit if 1 to 2 cm be reclassified as T1b? Endocr. Pract. 2017, 23, 526–535. [Google Scholar] [CrossRef] [PubMed]
- So, Y.K.; Kim, M.W.; Son, Y.-I. Multifocality and Bilaterality of Papillary Thyroid Microcarcinoma. Clin. Exp. Otorhinolaryngol. 2015, 8, 174–178. [Google Scholar] [CrossRef]
- Qu, N.; Zhang, L.; Ji, Q.-H.; Zhu, Y.-X.; Wang, Z.-Y.; Shen, Q.; Wang, Y.; Li, D.-S. Number of tumor foci predicts prognosis in papillary thyroid cancer. BMC Cancer 2014, 4, 914. [Google Scholar] [CrossRef] [Green Version]
- Lee, K.J.; Cho, Y.J.; Kim, J.G.; Lee, D.H. How Many Contralateral Papillary Thyroid Carcinomas Can Be Missed? World J. Surg. 2013, 37, 780–785. [Google Scholar] [CrossRef]
- Kaliszewski, K.; Diakowska, D.; Wojtczak, B.; Migoń, J.; Kasprzyk, A.; Rudnicki, J. The occurrence of and predictive factors for multifocality and bilaterality in patients with papillary thyroid microcarcinoma. Medicine 2019, 98, e15609. [Google Scholar] [CrossRef]
- Karatzas, T.; Vasileiadis, I.; Charitoudis, G.; Karakostas, E.; Tseleni-Balafouta, S.; Kouraklis, G. Bilateral versus unilateral papillary thyroid microcarcinoma: Predictive factors and associated histopathological findings following total thyroidectomy. Hormones 2013, 12, 529–536. [Google Scholar] [CrossRef] [Green Version]
- Zhou, Y.-L.; Gao, E.-L.; Zhang, W.; Yang, H.; Guo, G.-L.; Zhang, X.-H.; Wang, O.-C. Factors predictive of papillary thyroid micro-carcinoma with bilateral involvement and central lymph node metastasis: A retrospective study. World J. Surg. Oncol. 2012, 19, 67. [Google Scholar] [CrossRef] [Green Version]
- Liu, C.; Wang, S.; Zeng, W.; Guo, Y.; Liu, Z.; Huang, T. Total tumour diameter is superior to unifocal diameter as a predictor of papillary thyroid microcarcinoma prognosis. Sci. Rep. 2017, 12, 1846–1848. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feng, J.-W.; Pan, H.; Wang, L.; Ye, J.; Jiang, Y.; Qu, Z. Total tumor diameter: The neglected value in papillary thyroid microcarcinoma. J. Endocrinol. Investig. 2020, 43, 601–613. [Google Scholar] [CrossRef]
- Nagaoka, R.; Ebina, A.; Toda, K.; Jikuzono, T.; Saitou, M.; Sen, M.; Kazusaka, H.; Matsui, M.; Yamada, K.; Mitani, H.; et al. Multifocality and Progression of Papillary Thyroid Microcarcinoma During Active Surveillance. World J. Surg. 2021, 45, 2769–2776. [Google Scholar] [CrossRef] [PubMed]
- Molinaro, E.; Campopiano, M.C.; Elisei, R. MANAGEMENT OF ENDOCRINE DISEASE: Papillary thyroid microcarcinoma: Toward an active surveillance strategy. Eur. J. Endocrinol. 2021, 185, R23–R34. [Google Scholar] [CrossRef] [PubMed]
- Ito, Y.; Miyauchi, A.; Kihara, M.; Higashiyama, T.; Kobayashi, K.; Miya, A. Patient Age Is Significantly Related to the Progression of Papillary Microcarcinoma of the Thyroid Under Observation. Thyroid 2014, 24, 27–34. [Google Scholar] [CrossRef] [Green Version]
- Yan, T.; Qiu, W.; Song, J.; Ying, T.; Fan, Y.; Yang, Z. Bilateral multifocality, a marker for aggressive disease, is not an independent prognostic factor for papillary thyroid microcarcinoma: A propensity score matching analysis. Clin. Endocrinol. 2021, 95, 209–216. [Google Scholar] [CrossRef]
- Lacout, A.; Chamorey, E.; Thariat, J.; El Hajjam, M.; Chevenet, C.; Schiappa, R.; Marcy, P.Y. Insight into Differentiated Thyroid Cancer Gross Pathological Specimen Shrinkage and Its Influence on TNM Staging. Eur. Thyroid. J. 2017, 6, 315–320. [Google Scholar] [CrossRef] [Green Version]

| Overall Collective (n = 545) | Unilateral PTMC (n = 473) | Bilateral PTMC (n = 72) | p-Value | |
|---|---|---|---|---|
| Age | 51 (13–83) | 51 (13–80) | 53 (21–78) | 0.516 |
| Male | 114 (20.9%) | 92 (19.5%) | 22 (30.6%) | 0.026 |
| Lymphadenectomy (yes) | 139 (25.5%) | 119 (25.2%) | 20 (27.8%) | 0.365 |
| Completion TE (yes) | 105 (14.9%) | 78 (16.5%) | 25 (34.7%) | <0.001 |
| Tumor localization | <0.001 | |||
| Right | 262 (48.1%) | 262 (55.4%) | 0 | |
| Left | 211 (38.7%) | 211 (44.6%) | 0 | |
| On both sides | 72 (13.2%) | 0 | 73 (100%) | |
| n stage | 0.027 * | |||
| pN0 | 176 (32.3%) | 151 (31.9%) | 25 (34.7%) | |
| pN1 | 70 (12.8%) | 54 (11.4%) | 16 (22.2%) | |
| pNx | 299 (54.9%) | 268 (56.7%) | 31 (43.1%) | |
| Multifocal MPTC (yes) | 137 (25.1%) | 66 (14.0%) | 72 (100%) | <0.001 |
| Number of tumors | <0.001 | |||
| 1 | 407 (74.7%) | 407 (86.0%) | 0 | |
| 2 | 96 (17.6%) | 54 (11.4%) | 42 (58.3%) | |
| 3 | 18 (3.3%) | 9 (1.9%) | 9 (12.5%) | |
| 4 | 15 (2.8%) | 3 (0.6%) | 12 (16.7%) | |
| 5 | 8 (1.5%) | 0 | 8 (11.1%) | |
| 7 | 1 (0.2%) | 0 | 1 (1.4%) | |
| Number of tumors (median, range) | 0 (0–7) | 0 (0–4) | 2 (2–7) | <0.001 |
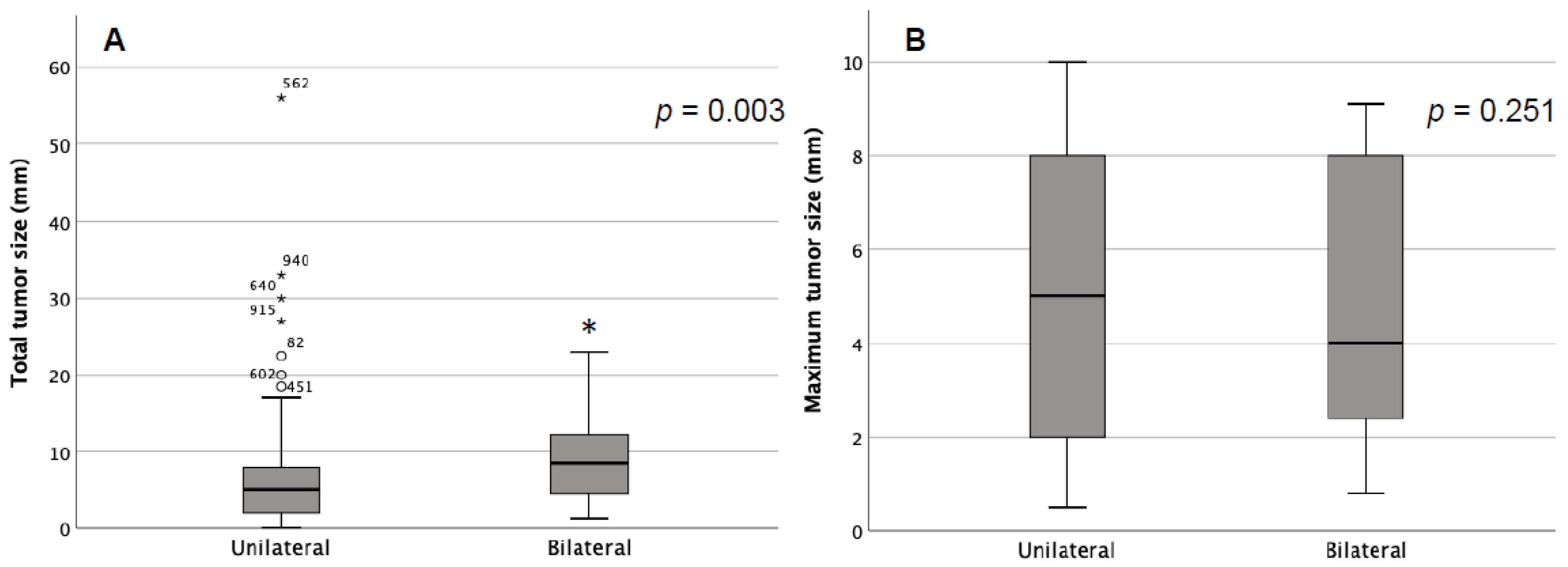
| Max tumor size (mm) | 5 (0.5–10) | 5 (0.5–10) | 4 (0.8–9.1) | 0.331 |
| Total tumor size (mm) | 5 (0.8–56) | 5 (0.8–56) | 7.1 (1–23) | <0.001 |
| Parameter | HR | 95%CI | p | |
|---|---|---|---|---|
| Lower | Upper | |||
| Sex | 0.443, 0.549 | 0.187, 0.316 | 1.052, 0.952 | 0.065, 0.074 |
| N stage | 1.000, 0.582 | 0.999, 0.888 | 1.001, 3.605 | 0.946, 0.103 |
| Tumor number | 2.282, 6.507 | 5.670, 4.354 | 19.922, 9.725 | <0.001 |
| Tumor size max | 1.284, 0.958 | 1.000, 0.878 | 1.647, 1.046 | 0.050, 0.341 |
| Total tumor size | 0.772, 1.113 | 0.654, 1.060 | 0.910, 1.169 | <0.001 |
| AUC | SE | p-Value | AUC 95% CI | ||
|---|---|---|---|---|---|
| Lower Limit | Upper Limit | ||||
| Total tumor size | 0.680 | 0.035 | <0.001 | 0.611 | 0.748 |
| Max tumor size | 0.460 | 0.036 | 0.296 | 0.388 | 0.531 |
| Tumor number | 0.897 | 0.014 | <0.001 | 0.870 | 0.924 |
| Cut-Off | TPR | TNR | YI | PPV | NPV | |
|---|---|---|---|---|---|---|
| Total tumor size (mm) | >10 | 0.292 | 0.947 | 0.239 | 0.292 | 0.964 |
| Max tumor size (mm) | >8 | 0.125 | 0.82 | 0.055 | 0.625 | 0.883 |
| Tumor number | >4 | 0.994 | 0.975 | 0.86 | 100 | 0.882 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lindner, K.; Iwen, K.A.; Kußmann, J.; Fendrich, V. Predictive Factors for Bilateral Disease in Papillary Microcarcinoma: A Retrospective Cohort Study. Curr. Oncol. 2022, 29, 6010-6017. https://doi.org/10.3390/curroncol29090473
Lindner K, Iwen KA, Kußmann J, Fendrich V. Predictive Factors for Bilateral Disease in Papillary Microcarcinoma: A Retrospective Cohort Study. Current Oncology. 2022; 29(9):6010-6017. https://doi.org/10.3390/curroncol29090473
Chicago/Turabian StyleLindner, Kirsten, K. Alexander Iwen, Jochen Kußmann, and Volker Fendrich. 2022. "Predictive Factors for Bilateral Disease in Papillary Microcarcinoma: A Retrospective Cohort Study" Current Oncology 29, no. 9: 6010-6017. https://doi.org/10.3390/curroncol29090473




