Liver-Directed Locoregional Therapies for Neuroendocrine Liver Metastases: Recent Advances and Management
Abstract
:1. Introduction
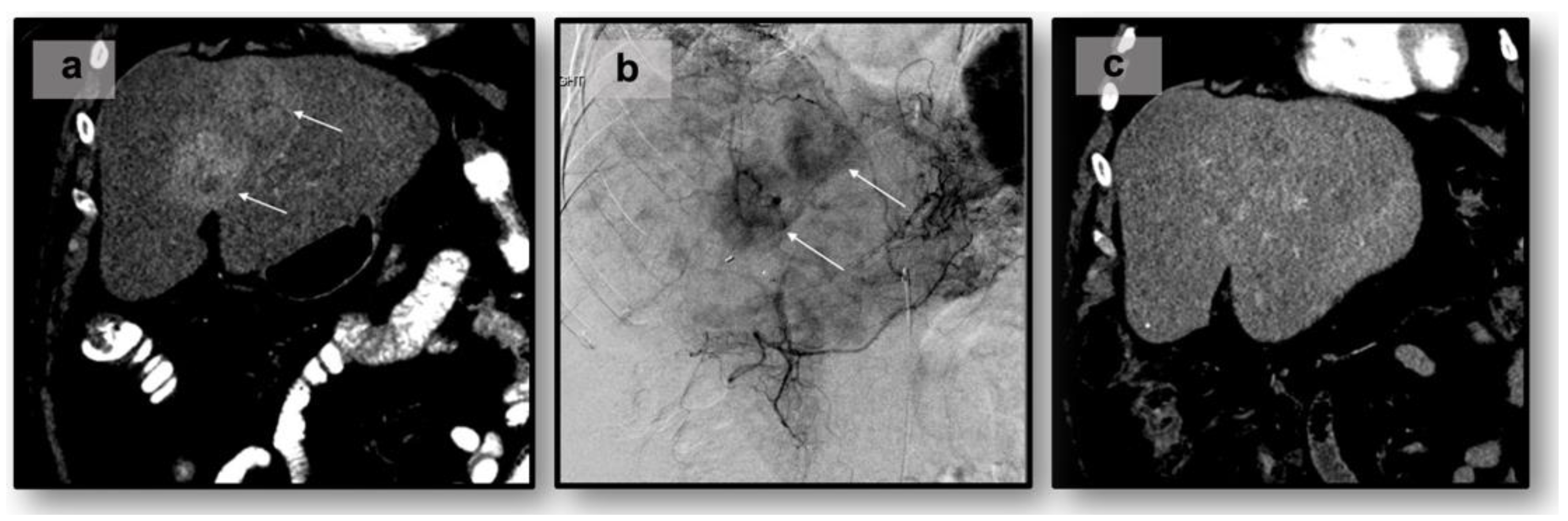
2. Tumor Characterization and Guidelines for Locoregional Therapy
2.1. Diagnostic Imaging and NET Classification
2.2. General Overview of Treatment Approaches
2.3. Alternatives to Surgery
3. Locoregional Therapies
3.1. Transarterial “Bland” Embolization
3.2. Transarterial Chemoembolization
3.3. Important Considerations with Transarterial Approaches
| Locoregional Therapy | Approach | Highlights and Outcomes |
|---|---|---|
| Transarterial “bland” Embolization (TAE) | Selective catheterization using embolic agents (e.g., microspheres or gelatin sponge particles) of the hepatic artery and embolization of vessels supplying the tumor | |
| Transarterial Chemoembolization (TACE) | Selective catheterization using chemotherapeutic agents (e.g., doxorubicin or cisplatin) injected into the hepatic artery supplying the tumor |
|
| ||
| Transarterial Radioembolization (TARE) | Microspheres are loaded with a radioactive isotope (e.g., yttrium-90) resulting in localized radiation therapy to the tumor |
|
| Ablation (e.g., microwave or radiofrequency) | Intra-operative or percutaneous probe(s) employing microwave energy or high-frequency alternativity currents to induce coagulative necrosis of the tumor |
3.4. Transarterial Radioembolization
3.5. Transarterial Radioembolization vs. Chemoembolization
4. Ablative Therapies
5. Multimodal Strategies and Future Directions
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Dasari, A.; Shen, C.; Halperin, D.; Zhao, B.; Zhou, S.; Xu, Y.; Shih, T.; Yao, J.C. Trends in the Incidence, Prevalence, and Survival Outcomes in Patients With Neuroendocrine Tumors in the United States. JAMA Oncol. 2017, 3, 1335–1342. [Google Scholar] [CrossRef] [PubMed]
- Das, S.; Dasari, A. Epidemiology, Incidence, and Prevalence of Neuroendocrine Neoplasms: Are There Global Differences? Curr. Oncol. Rep. 2021, 23, 43. [Google Scholar] [CrossRef] [PubMed]
- Muttillo, E.M.; Mazzarella, G.; Picardi, B.; Rossi, S.; Cinelli, L.; Diana, M.; Baiocchini, A.; Felli, E.; Pessaux, P.; Felli, E.; et al. Treatment Strategies for Neuroendocrine Liver Metastases: A Systematic Review. HPB 2022, 24, 1832–1843. [Google Scholar] [CrossRef]
- Davis, Z.; Moertel, C.G.; McIlrath, D.C. The Malignant Carcinoid Syndrome. Surg. Gynecol. Obs. 1973, 137, 637–644. [Google Scholar]
- Ito, T.; Lee, L.; Jensen, R.T. Carcinoid-Syndrome: Recent Advances, Current Status and Controversies. Curr. Opin. Endocrinol. Diabetes Obes. 2018, 25, 22–35. [Google Scholar] [CrossRef] [PubMed]
- de Celis Ferrari, A.C.R.; Glasberg, J.; Riechelmann, R.P. Carcinoid Syndrome: Update on the Pathophysiology and Treatment. Clinics 2018, 73, e490s. [Google Scholar] [CrossRef] [PubMed]
- Ihse, I.; Lindell, G.; Tibblin, S. Neuroendocrine Tumors Metastatic to the Liver. In Surgical Treatment: Evidence-Based and Problem-Oriented; Zuckschwerdt: Munich, Germany, 2001. [Google Scholar]
- Ihse, I.; Persson, B.; Tibblin, S. Neuroendocrine Metastases of the Liver. World J. Surg. 1995, 19, 76–82. [Google Scholar] [CrossRef]
- Harrelson, A.; Wang, R.; Stewart, A.; Ingram, C.; Gillis, A.; Rose, J.B.; El-Rayes, B.; Azmi, A.; Chen, H. Management of Neuroendocrine Tumor Liver Metastases. Am. J. Surg. 2023, 226, 623–630. [Google Scholar] [CrossRef]
- Riihimäki, M.; Hemminki, A.; Sundquist, K.; Sundquist, J.; Hemminki, K. The Epidemiology of Metastases in Neuroendocrine Tumors. Int. J. Cancer 2016, 139, 2679–2686. [Google Scholar] [CrossRef]
- Xu, Z.; Wang, L.; Dai, S.; Chen, M.; Li, F.; Sun, J.; Luo, F. Epidemiologic Trends of and Factors Associated With Overall Survival for Patients With Gastroenteropancreatic Neuroendocrine Tumors in the United States. JAMA Netw. Open 2021, 4, e2124750. [Google Scholar] [CrossRef]
- Pavel, M.; Baudin, E.; Couvelard, A.; Krenning, E.; Öberg, K.; Steinmüller, T.; Anlauf, M.; Wiedenmann, B.; Salazar, R. ENETS Consensus Guidelines for the Management of Patients with Liver and Other Distant Metastases from Neuroendocrine Neoplasms of Foregut, Midgut, Hindgut, and Unknown Primary. Neuroendocrinology 2012, 95, 157–176. [Google Scholar] [CrossRef] [PubMed]
- Colquhoun, S.D. Neuroendocrine Tumors with Hepatic Metastases: A Review of Evolving Treatment Options. Liver Res. 2018, 2, 92–99. [Google Scholar] [CrossRef]
- Machairas, N.; Daskalakis, K.; Felekouras, E.; Alexandraki, K.I.; Kaltsas, G.; Sotiropoulos, G.C. Currently Available Treatment Options for Neuroendocrine Liver Metastases. Ann. Gastroenterol. 2021, 34, 130–141. [Google Scholar] [CrossRef]
- Wild, D.; Bomanji, J.B.; Benkert, P.; Maecke, H.; Ell, P.J.; Reubi, J.C.; Caplin, M.E. Comparison of 68Ga-DOTANOC and 68Ga-DOTATATE PET/CT within Patients with Gastroenteropancreatic Neuroendocrine Tumors. J. Nucl. Med. 2013, 54, 364–372. [Google Scholar] [CrossRef] [PubMed]
- Galgano, S.J.; Iravani, A.; Bodei, L.; El-Haddad, G.; Hofman, M.S.; Kong, G. Imaging of Neuroendocrine Neoplasms: Monitoring Treatment Response—AJR Expert Panel Narrative Review. Am. J. Roentgenol. 2022, 218, 767–780. [Google Scholar] [CrossRef] [PubMed]
- Carideo, L.; Prosperi, D.; Panzuto, F.; Magi, L.; Pratesi, M.S.; Rinzivillo, M.; Annibale, B.; Signore, A. Role of Combined [68Ga]Ga-DOTA-SST Analogues and [18F]FDG PET/CT in the Management of GEP-NENs: A Systematic Review. J. Clin. Med. 2019, 8, 1032. [Google Scholar] [CrossRef] [PubMed]
- Balogova, S.; Talbot, J.-N.; Nataf, V.; Michaud, L.; Huchet, V.; Kerrou, K.; Montravers, F. 18F-Fluorodihydroxyphenylalanine vs Other Radiopharmaceuticals for Imaging Neuroendocrine Tumours According to Their Type. Eur. J. Nucl. Med. Mol. Imaging 2013, 40, 943–966. [Google Scholar] [CrossRef] [PubMed]
- Gowdra Halappa, V.; Corona-Villalobos, C.P.; Bonekamp, S.; Li, Z.; Reyes, D.; Cosgrove, D.; Pawlik, T.M.; Diaz, L.A.; Bhagat, N.; Eng, J.; et al. Neuroendocrine Liver Metastasis Treated by Using Intraarterial Therapy: Volumetric Functional Imaging Biomarkers of Early Tumor Response and Survival. Radiology 2013, 266, 502–513. [Google Scholar] [CrossRef]
- Mete, O.; Wenig, B.M. Update from the 5th Edition of the World Health Organization Classification of Head and Neck Tumors: Overview of the 2022 WHO Classification of Head and Neck Neuroendocrine Neoplasms. Head Neck Pathol. 2022, 16, 123–142. [Google Scholar] [CrossRef]
- Grawe, F.; Rosenberger, N.; Ingenerf, M.; Beyer, L.; Eschbach, R.; Todica, A.; Seidensticker, R.; Schmid-Tannwald, C.; Cyran, C.C.; Ricke, J.; et al. Diagnostic Performance of PET/CT in the Detection of Liver Metastases in Well-Differentiated NETs. Cancer Imaging 2023, 23, 41. [Google Scholar] [CrossRef]
- Frilling, A.; Li, J.; Malamutmann, E.; Schmid, K.-W.; Bockisch, A.; Broelsch, C.E. Treatment of Liver Metastases from Neuroendocrine Tumours in Relation to the Extent of Hepatic Disease. Br. J. Surg. 2009, 96, 175–184. [Google Scholar] [CrossRef]
- Sarmiento, J.M.; Heywood, G.; Rubin, J.; Ilstrup, D.M.; Nagorney, D.M.; Que, F.G. Surgical Treatment of Neuroendocrine Metastases to the Liver: A Plea for Resection to Increase Survival. J. Am. Coll. Surg. 2003, 197, 29–37. [Google Scholar] [CrossRef] [PubMed]
- Mayo, S.C.; de Jong, M.C.; Pulitano, C.; Clary, B.M.; Reddy, S.K.; Gamblin, T.C.; Celinksi, S.A.; Kooby, D.A.; Staley, C.A.; Stokes, J.B.; et al. Surgical Management of Hepatic Neuroendocrine Tumor Metastasis: Results from an International Multi-Institutional Analysis. Ann. Surg. Oncol. 2010, 17, 3129–3136. [Google Scholar] [CrossRef]
- Mahuron, K.M.; Singh, G. Defining a New Classification System for the Surgical Management of Neuroendocrine Tumor Liver Metastases. J. Clin. Med. 2023, 12, 2456. [Google Scholar] [CrossRef] [PubMed]
- Zane, K.E.; Cloyd, J.M.; Mumtaz, K.S.; Wadhwa, V.; Makary, M.S. Metastatic Disease to the Liver: Locoregional Therapy Strategies and Outcomes. World J. Clin. Oncol. 2021, 12, 725–745. [Google Scholar] [CrossRef] [PubMed]
- Citterio, D.; Coppa, J.; Sposito, C.; Busset, M.D.D.; Virdis, M.; Pezzoli, I.; Mazzaferro, V. The Role of Liver Transplantation in the Treatment of Liver Metastases from Neuroendocrine Tumors. Curr. Treat. Options Oncol. 2023, 24, 1651–1665. [Google Scholar] [CrossRef]
- Cloyd, J.M.; Ejaz, A.; Konda, B.; Makary, M.S.; Pawlik, T.M. Neuroendocrine Liver Metastases: A Contemporary Review of Treatment Strategies. Hepatobiliary Surg. Nutr. 2020, 9, 440–451. [Google Scholar] [CrossRef] [PubMed]
- Herrera-Martínez, A.D.; Hofland, J.; Hofland, L.J.; Brabander, T.; Eskens, F.A.L.M.; Gálvez Moreno, M.A.; Luque, R.M.; Castaño, J.P.; de Herder, W.W.; Feelders, R.A. Targeted Systemic Treatment of Neuroendocrine Tumors: Current Options and Future Perspectives. Drugs 2019, 79, 21–42. [Google Scholar] [CrossRef]
- Costa, F.; Gumz, B. Octreotide—A Review of Its Use in Treating Neuroendocrine Tumours. Eur. Endocrinol. 2014, 10, 70–74. [Google Scholar] [CrossRef]
- Milewska-Kranc, A.; Ćwikła, J.B.; Kolasinska-Ćwikła, A. The Role of Receptor–Ligand Interaction in Somatostatin Signaling Pathways: Implications for Neuroendocrine Tumors. Cancers 2023, 16, 116. [Google Scholar] [CrossRef]
- Stueven, A.K.; Kayser, A.; Wetz, C.; Amthauer, H.; Wree, A.; Tacke, F.; Wiedenmann, B.; Roderburg, C.; Jann, H. Somatostatin Analogues in the Treatment of Neuroendocrine Tumors: Past, Present and Future. Int. J. Mol. Sci. 2019, 20, 3049. [Google Scholar] [CrossRef] [PubMed]
- Caplin, M.E.; Pavel, M.; Ćwikła, J.B.; Phan, A.T.; Raderer, M.; Sedláčková, E.; Cadiot, G.; Wolin, E.M.; Capdevila, J.; Wall, L.; et al. Lanreotide in Metastatic Enteropancreatic Neuroendocrine Tumors. N. Engl. J. Med. 2014, 371, 224–233. [Google Scholar] [CrossRef] [PubMed]
- Rinke, A.; Müller, H.-H.; Schade-Brittinger, C.; Klose, K.-J.; Barth, P.; Wied, M.; Mayer, C.; Aminossadati, B.; Pape, U.-F.; Bläker, M.; et al. Placebo-Controlled, Double-Blind, Prospective, Randomized Study on the Effect of Octreotide LAR in the Control of Tumor Growth in Patients with Metastatic Neuroendocrine Midgut Tumors: A Report from the PROMID Study Group. J. Clin. Oncol. 2009, 27, 4656–4663. [Google Scholar] [CrossRef] [PubMed]
- Strosberg, J.; El-Haddad, G.; Wolin, E.; Hendifar, A.; Yao, J.; Chasen, B.; Mittra, E.; Kunz, P.L.; Kulke, M.H.; Jacene, H.; et al. Phase 3 Trial of 177Lu-Dotatate for Midgut Neuroendocrine Tumors. N. Engl. J. Med. 2017, 376, 125–135. [Google Scholar] [CrossRef]
- Camus, B.; Cottereau, A.-S.; Palmieri, L.-J.; Dermine, S.; Tenenbaum, F.; Brezault, C.; Coriat, R. Indications of Peptide Receptor Radionuclide Therapy (PRRT) in Gastroenteropancreatic and Pulmonary Neuroendocrine Tumors: An Updated Review. J. Clin. Med. 2021, 10, 1267. [Google Scholar] [CrossRef] [PubMed]
- Strosberg, J.R.; Caplin, M.E.; Kunz, P.L.; Ruszniewski, P.B.; Bodei, L.; Hendifar, A.; Mittra, E.; Wolin, E.M.; Yao, J.C.; Pavel, M.E.; et al. 177Lu-Dotatate plus Long-Acting Octreotide versus High-dose Long-Acting Octreotide in Patients with Midgut Neuroendocrine Tumours (NETTER-1): Final Overall Survival and Long-Term Safety Results from an Open-Label, Randomised, Controlled, Phase 3 Trial. Lancet Oncol. 2021, 22, 1752–1763. [Google Scholar] [CrossRef] [PubMed]
- Kulke, M.H.; Anthony, L.B.; Bushnell, D.L.; de Herder, W.W.; Goldsmith, S.J.; Klimstra, D.S.; Marx, S.J.; Pasieka, J.L.; Pommier, R.F.; Yao, J.C.; et al. NANETS Treatment Guidelines. Pancreas 2010, 39, 735–752. [Google Scholar] [CrossRef]
- Hicks, R.J.; Kwekkeboom, D.J.; Krenning, E.; Bodei, L.; Grozinsky-Glasberg, S.; Arnold, R.; Borbath, I.; Cwikla, J.; Toumpanakis, C.; Kaltsas, G.; et al. ENETS Consensus Guidelines for the Standards of Care in Neuroendocrine Neoplasms: Peptide Receptor Radionuclide Therapy with Radiolabelled Somatostatin Analogues. Neuroendocrinology 2017, 105, 295–309. [Google Scholar] [CrossRef]
- Halfdanarson, T.R.; Strosberg, J.R.; Tang, L.; Bellizzi, A.M.; Bergsland, E.K.; O’Dorisio, T.M.; Halperin, D.M.; Fishbein, L.; Eads, J.; Hope, T.A.; et al. The North American Neuroendocrine Tumor Society Consensus Guidelines for Surveillance and Medical Management of Pancreatic Neuroendocrine Tumors. Pancreas 2020, 49, 863–881. [Google Scholar] [CrossRef]
- North American Neuroendocrine Tumor Society Consensus Guidelines; NANETS: Albany, NY, USA, 2023.
- Harris, P.E.; Zhernosekov, K. The Evolution of PRRT for the Treatment of Neuroendocrine Tumors; What Comes Next? Front. Endocrinol. 2022, 13, 941832. [Google Scholar] [CrossRef]
- Pavel, M.E.; Rinke, A.; Baum, R.P. COMPETE Trial: Peptide Receptor Radionuclide Therapy (PRRT) with 177Lu-Edotreotide vs. Everolimus in Progressive GEP-NET. Ann. Oncol. 2018, 29, viii478. [Google Scholar] [CrossRef]
- di Santo, G.; Santo, G.; Sviridenko, A.; Virgolini, I. Peptide Receptor Radionuclide Therapy Combinations for Neuroendocrine Tumours in Ongoing Clinical Trials: Status 2023. Theranostics 2024, 14, 940–953. [Google Scholar] [CrossRef] [PubMed]
- Schreckenbach, T.; Hübert, H.; Koch, C.; Bojunga, J.; Schnitzbauer, A.A.; Bechstein, W.O.; Holzer, K. Surgical Resection of Neuroendocrine Tumor Liver Metastases as Part of Multimodal Treatment Strategies: A Propensity Score Matching Analysis. Eur. J. Surg. Oncol. 2019, 45, 808–815. [Google Scholar] [CrossRef] [PubMed]
- Labib, P.L.; Davidson, B.R.; Sharma, R.A.; Pereira, S.P. Locoregional Therapies in Cholangiocarcinoma. Hepat. Oncol. 2017, 4, 99–109. [Google Scholar] [CrossRef] [PubMed]
- Makary, M.S.; Khandpur, U.; Cloyd, J.M.; Mumtaz, K.; Dowell, J.D. Locoregional Therapy Approaches for Hepatocellular Carcinoma: Recent Advances and Management Strategies. Cancers 2020, 12, 1914. [Google Scholar] [CrossRef] [PubMed]
- Llovet, J.M.; De Baere, T.; Kulik, L.; Haber, P.K.; Greten, T.F.; Meyer, T.; Lencioni, R. Locoregional Therapies in the Era of Molecular and Immune Treatments for Hepatocellular Carcinoma. Nat. Rev. Gastroenterol. Hepatol. 2021, 18, 293–313. [Google Scholar] [CrossRef] [PubMed]
- Guiu, B.; Garin, E.; Allimant, C.; Edeline, J.; Salem, R. TARE in Hepatocellular Carcinoma: From the Right to the Left of BCLC. Cardiovasc. Interv. Radiol. 2022, 45, 1599–1607. [Google Scholar] [CrossRef]
- Reig, M.; Forner, A.; Rimola, J.; Ferrer-Fàbrega, J.; Burrel, M.; Garcia-Criado, Á.; Kelley, R.K.; Galle, P.R.; Mazzaferro, V.; Salem, R.; et al. BCLC Strategy for Prognosis Prediction and Treatment Recommendation: The 2022 Update. J. Hepatol. 2022, 76, 681–693. [Google Scholar] [CrossRef]
- Pavel, M.; Öberg, K.; Falconi, M.; Krenning, E.P.; Sundin, A.; Perren, A.; Berruti, A. Gastroenteropancreatic Neuroendocrine Neoplasms: ESMO Clinical Practice Guidelines for Diagnosis, Treatment and Follow-Up†. Ann. Oncol. 2020, 31, 844–860. [Google Scholar] [CrossRef]
- Strosberg, J.R.; Halfdanarson, T.R.; Bellizzi, A.M.; Chan, J.A.; Dillon, J.; Heaney, A.P.; Kunz, P.L.; O’Dorisio, T.M.; Salem, R.; Segelov, E.; et al. The North American Neuroendocrine Society (NANETS) Consensus Guidelines for Surveillance and Medical Management of Midgut Neuroendocrine Tumors. Pancreas 2017, 46, 707–714. [Google Scholar] [CrossRef]
- Eads, J.R.; Halfdanarson, T.R.; Asmis, T.; Bellizzi, A.M.; Bergsland, E.K.; Dasari, A.; El-Haddad, G.; Frumovitz, M.; Meyer, J.; Mittra, E.; et al. Expert Consensus Practice Recommendations of the North American Neuroendocrine Tumor Society for the Management of High Grade Gastroenteropancreatic and Gynecologic Neuroendocrine Neoplasms. Endocr. Relat. Cancer 2023, 30, e220206. [Google Scholar] [CrossRef] [PubMed]
- Rabei, R.; Fidelman, N. Liver-Directed Therapy for Neuroendocrine Tumor Metastases in the Era of Peptide Receptor Radionuclide Therapy. Curr. Treat. Options Oncol. 2023, 24, 1994–2004. [Google Scholar] [CrossRef] [PubMed]
- Vinik, A.I.; Woltering, E.A.; Warner, R.R.P.; Caplin, M.; O’Dorisio, T.M.; Wiseman, G.A.; Coppola, D.; Go, V.L.W.; North American Neuroendocrine Tumor Society (NANETS). NANETS Consensus Guidelines for the Diagnosis of Neuroendocrine Tumor. Pancreas 2010, 39, 713–734. [Google Scholar] [CrossRef] [PubMed]
- Ronot, M.; Clift, A.K.; Baum, R.P.; Singh, A.; Kulkarni, H.R.; Frilling, A.; Vilgrain, V. Morphological and Functional Imaging for Detecting and Assessing the Resectability of Neuroendocrine Liver Metastases. Neuroendocrinology 2017, 106, 74–88. [Google Scholar] [CrossRef] [PubMed]
- Dörffel, Y.; Wermke, W. Neuroendocrine Tumors: Characterization with Contrast-Enhanced Ultrasonography. Ultraschall Med. 2008, 29, 506–514. [Google Scholar] [CrossRef]
- Miyayama, S. Treatment Strategy of Transarterial Chemoembolization for Hepatocellular Carcinoma. Appl. Sci. 2020, 10, 7337. [Google Scholar] [CrossRef]
- Ngongoni, R.; Visser, B. Surgery, Liver Directed Therapy and Peptide Receptor Radionuclide Therapy for Pancreatic Neuroendocrine Tumor Liver Metastases. Cancers 2022, 14, 5103. [Google Scholar] [CrossRef] [PubMed]
- Ghanaati, H.; Mohammadifard, M.; Mohammadifard, M. A Review of Applying Transarterial Chemoembolization (TACE) Method for Management of Hepatocellular Carcinoma. J. Fam. Med. Prim. Care 2021, 10, 3553–3560. [Google Scholar] [CrossRef]
- Melchiorre, F.; Patella, F.; Pescatori, L.; Pesapane, F.; Fumarola, E.; Biondetti, P.; Brambillasca, P.; Monaco, C.; Ierardi, A.M.; Franceschelli, G.; et al. DEB-TACE: A Standard Review. Future Oncol. 2018, 14, 2969–2984. [Google Scholar] [CrossRef]
- Makary, M.S.; Kapke, J.; Yildiz, V.; Pan, X.; Dowell, J.D. Conventional versus Drug-Eluting Bead Transarterial Chemoembolization for Neuroendocrine Tumor Liver Metastases. J. Vasc. Interv. Radiol. 2016, 27, 1298–1304. [Google Scholar] [CrossRef]
- Tu, J.; Jia, Z.; Ying, X.; Zhang, D.; Li, S.; Tian, F.; Jiang, G. The Incidence and Outcome of Major Complication Following Conventional TAE/TACE for Hepatocellular Carcinoma. Medicine 2016, 95, e5606. [Google Scholar] [CrossRef]
- Egger, M.E.; Armstrong, E.; Martin, R.C.; Scoggins, C.R.; Philips, P.; Shah, M.; Konda, B.; Dillhoff, M.; Pawlik, T.M.; Cloyd, J.M. Transarterial Chemoembolization vs. Radioembolization for Neuroendocrine Liver Metastases: A Multi-Institutional Analysis. J. Am. Coll. Surg. 2020, 230, 363–370. [Google Scholar] [CrossRef]
- Touloupas, C.; Faron, M.; Hadoux, J.; Deschamps, F.; Roux, C.; Ronot, M.; Yevich, S.; Joskin, J.; Gelli, M.; Barbé, R.; et al. Long Term Efficacy and Assessment of Tumor Response of Transarterial Chemoembolization in Neuroendocrine Liver Metastases: A 15-Year Monocentric Experience. Cancers 2021, 13, 5366. [Google Scholar] [CrossRef]
- Dong, X.D.; Carr, B.I. Hepatic Artery Chemoembolization for the Treatment of Liver Metastases from Neuroendocrine Tumors: A Long-Term Follow-up in 123 Patients. Med. Oncol. 2011, 28 (Suppl. 1), S286–S290. [Google Scholar] [CrossRef] [PubMed]
- Arrese, D.; McNally, M.E.; Chokshi, R.; Feria-Arias, E.; Schmidt, C.; Klemanski, D.; Gregory, G.; Khabiri, H.; Shah, M.; Bloomston, M. Extrahepatic Disease Should Not Preclude Transarterial Chemoembolization for Metastatic Neuroendocrine Carcinoma. Ann. Surg. Oncol. 2013, 20, 1114–1120. [Google Scholar] [CrossRef]
- Dhir, M.; Shrestha, R.; Steel, J.L.; Marsh, J.W.; Tsung, A.; Tublin, M.E.; Amesur, N.B.; Orons, P.D.; Santos, E.; Geller, D.A. Initial Treatment of Unresectable Neuroendocrine Tumor Liver Metastases with Transarterial Chemoembolization Using Streptozotocin: A 20-Year Experience. Ann. Surg. Oncol. 2017, 24, 450–459. [Google Scholar] [CrossRef] [PubMed]
- McDermott, S.M.; Saunders, N.D.; Schneider, E.B.; Strosberg, D.; Onesti, J.; Dillhoff, M.; Schmidt, C.R.; Shirley, L.A. Neutrophil Lymphocyte Ratio and Transarterial Chemoembolization in Neuroendocrine Tumor Metastases. J. Surg. Res. 2018, 232, 369–375. [Google Scholar] [CrossRef]
- Minh, D.D.; Chapiro, J.; Gorodetski, B.; Huang, Q.; Liu, C.; Smolka, S.; Savic, L.J.; Wainstejn, D.; Lin, M.; Schlachter, T.; et al. Intra-Arterial Therapy of Neuroendocrine Tumor Liver Metastases: Comparing Conventional TACE, Drug-Eluting Beads TACE and 90Yttrium Radioembolization as Treatment Options Using a Propensity Score Analysis Model. Eur. Radiol. 2017, 27, 4995–5005. [Google Scholar] [CrossRef] [PubMed]
- Hur, S.; Chung, J.W.; Kim, H.-C.; Oh, D.-Y.; Lee, S.-H.; Bang, Y.-J.; Kim, W.H. Survival Outcomes and Prognostic Factors of Transcatheter Arterial Chemoembolization for Hepatic Neuroendocrine Metastases. J. Vasc. Interv. Radiol. 2013, 24, 947–956. [Google Scholar] [CrossRef]
- Merola, E.; Michielan, A.; Rozzanigo, U.; Erini, M.; Sferrazza, S.; Marcucci, S.; Sartori, C.; Trentin, C.; de Pretis, G.; Chierichetti, F. Therapeutic Strategies for Gastroenteropancreatic Neuroendocrine Neoplasms: State-of-the-Art and Future Perspectives. World J. Gastrointest. Surg. 2022, 14, 78–106. [Google Scholar] [CrossRef]
- de Baere, T.; Deschamps, F.; Tselikas, L.; Ducreux, M.; Planchard, D.; Pearson, E.; Berdelou, A.; Leboulleux, S.; Elias, D.; Baudin, E. GEP-NETS Update: Interventional Radiology: Role in the Treatment of Liver Metastases from GEP-NETs. Eur. J. Endocrinol. 2015, 172, R151–R166. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.X.; Wileyto, E.P.; Soulen, M.C. Randomized Embolization Trial for NeuroEndocrine Tumor Metastases to the Liver (RETNET): Study Protocol for a Randomized Controlled Trial. Trials 2018, 19, 390. [Google Scholar] [CrossRef]
- Makary, M.S.; Regalado, L.E.; Alexander, J.; Sukrithan, V.; Konda, B.; Cloyd, J.M. Clinical Outcomes of DEB-TACE in Hepatic Metastatic Neuroendocrine Tumors: A 5-Year Single-Institutional Experience. Acad. Radiol. 2023, 30 (Suppl. 1), S117–S123. [Google Scholar] [CrossRef] [PubMed]
- Barat, M.; Cottereau, A.-S.; Kedra, A.; Dermine, S.; Palmieri, L.-J.; Coriat, R.; Dautry, R.; Tselikas, L.; Soyer, P.; Dohan, A. The Role of Interventional Radiology for the Treatment of Hepatic Metastases from Neuroendocrine Tumor: An Updated Review. J. Clin. Med. 2020, 9, 2302. [Google Scholar] [CrossRef] [PubMed]
- Fiore, F.; Del Prete, M.; Franco, R.; Marotta, V.; Ramundo, V.; Marciello, F.; Di Sarno, A.; Carratù, A.C.; de Luca di Roseto, C.; Colao, A.; et al. Transarterial Embolization (TAE) Is Equally Effective and Slightly Safer than Transarterial Chemoembolization (TACE) to Manage Liver Metastases in Neuroendocrine Tumors. Endocrine 2014, 47, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Tai, E.; Kennedy, S.; Farrell, A.; Jaberi, A.; Kachura, J.; Beecroft, R. Comparison of Transarterial Bland and Chemoembolization for Neuroendocrine Tumours: A Systematic Review and Meta-Analysis. Curr. Oncol. 2020, 27, e537–e546. [Google Scholar] [CrossRef]
- Pericleous, M.; Caplin, M.E.; Tsochatzis, E.; Yu, D.; Morgan-Rowe, L.; Toumpanakis, C. Hepatic Artery Embolization in Advanced Neuroendocrine Tumors: Efficacy and Long-Term Outcomes. Asia Pac. J. Clin. Oncol. 2016, 12, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Wigmore, S.J.; Redhead, D.N.; Thomson, B.N.J.; Currie, E.J.; Parks, R.W.; Madhavan, K.K.; Garden, O.J. Postchemoembolisation Syndrome--Tumour Necrosis or Hepatocyte Injury? Br. J. Cancer 2003, 89, 1423–1427. [Google Scholar] [CrossRef] [PubMed]
- Blackburn, H.; West, S. Management of Postembolization Syndrome Following Hepatic Transarterial Chemoembolization for Primary or Metastatic Liver Cancer. Cancer Nurs. 2016, 39, E1. [Google Scholar] [CrossRef]
- Sakamoto, I.; Aso, N.; Nagaoki, K.; Matsuoka, Y.; Uetani, M.; Ashizawa, K.; Iwanaga, S.; Mori, M.; Morikawa, M.; Fukuda, T.; et al. Complications Associated with Transcatheter Arterial Embolization for Hepatic Tumors. RadioGraphics 1998, 18, 605–619. [Google Scholar] [CrossRef]
- Del Prete, M.; Fiore, F.; Modica, R.; Marotta, V.; Marciello, F.; Ramundo, V.; Di Sarno, A.; Carratù, A.; di Roseto, C.d.L.; Tafuto, S.; et al. Hepatic Arterial Embolization in Patients with Neuroendocrine Tumors. J. Exp. Clin. Cancer Res. 2014, 33, 43. [Google Scholar] [CrossRef] [PubMed]
- Yao, K.A.; Talamonti, M.S.; Nemcek, A.; Angelos, P.; Chrisman, H.; Skarda, J.; Benson, A.B.; Rao, S.; Joehl, R.J. Indications and Results of Liver Resection and Hepatic Chemoembolization for Metastatic Gastrointestinal Neuroendocrine Tumors. Surgery 2001, 130, 677–685. [Google Scholar] [CrossRef] [PubMed]
- Piscaglia, F.; Ogasawara, S. Patient Selection for Transarterial Chemoembolization in Hepatocellular Carcinoma: Importance of Benefit/Risk Assessment. Liver Cancer 2018, 7, 104–119. [Google Scholar] [CrossRef] [PubMed]
- De Jong, M.C.; Farnell, M.B.; Sclabas, G.; Cunningham, S.C.; Cameron, J.L.; Geschwind, J.-F.; Wolfgang, C.L.; Herman, J.M.; Edil, B.H.; Choti, M.A.; et al. Liver-Directed Therapy for Hepatic Metastases in Patients Undergoing Pancreaticoduodenectomy: A Dual-Center Analysis. Ann. Surg. 2010, 252, 142–148. [Google Scholar] [CrossRef] [PubMed]
- Farid, K.; Elalfy, H.; El-Bendary, M.; Besheer, T.; El-Eraky, A.; Abdelbadie, M.; Elmokadem, A.; Moawad, A.; El-khair, S.A.; Sakr, S.; et al. Cardiopulmonary Assessment of Patients with Unresectable Hepatocellular Carcinoma Treated by Transarterial Chemoembolization. J. Liver Transplant. 2022, 5, 100063. [Google Scholar] [CrossRef]
- Xu, A.; Suz, P.; Reljic, T.; Are, A.C.; Kumar, A.; Powers, B.; Strosberg, J.; Denbo, J.W.; Fleming, J.B.; Anaya, D.A. Perioperative Carcinoid Crisis: A Systematic Review and Meta-Analysis. Cancers 2022, 14, 2966. [Google Scholar] [CrossRef]
- Kaltsas, G.; Caplin, M.; Davies, P.; Ferone, D.; Garcia-Carbonero, R.; Grozinsky-Glasberg, S.; Hörsch, D.; Tiensuu Janson, E.; Kianmanesh, R.; Kos-Kudla, B.; et al. ENETS Consensus Guidelines for the Standards of Care in Neuroendocrine Tumors: Pre- and Perioperative Therapy in Patients with Neuroendocrine Tumors. Neuroendocrinology 2017, 105, 245–254. [Google Scholar] [CrossRef] [PubMed]
- Howe, J.R.; Merchant, N.B.; Conrad, C.; Keutgen, X.M.; Hallet, J.; Drebin, J.A.; Minter, R.M.; Lairmore, T.C.; Tseng, J.F.; Zeh, H.J.; et al. The North American Neuroendocrine Tumor Society Consensus Paper on the Surgical Management of Pancreatic Neuroendocrine Tumors. Pancreas 2020, 49, 1–33. [Google Scholar] [CrossRef] [PubMed]
- Wong, T.Y.; Zhang, K.S.; Gandhi, R.T.; Collins, Z.S.; O’Hara, R.; Wang, E.A.; Vaheesan, K.; Matsuoka, L.; Sze, D.Y.; Kennedy, A.S.; et al. Long-Term Outcomes Following 90Y Radioembolization of Neuroendocrine Liver Metastases: Evaluation of the Radiation-Emitting SIR-Spheres in Non-Resectable Liver Tumor (RESiN) Registry. BMC Cancer 2022, 22, 224. [Google Scholar] [CrossRef]
- Currie, B.M.; Nadolski, G.; Mondschein, J.; Dagli, M.; Sudheendra, D.; Stavropoulos, S.W.; Soulen, M.C. Chronic Hepatotoxicity in Patients with Metastatic Neuroendocrine Tumor: Transarterial Chemoembolization versus Transarterial Radioembolization. J. Vasc. Interv. Radiol. 2020, 31, 1627–1635. [Google Scholar] [CrossRef]
- Currie, B.M.; Hoteit, M.A.; Ben-Josef, E.; Nadolski, G.J.; Soulen, M.C. Radioembolization-Induced Chronic Hepatotoxicity: A Single-Center Cohort Analysis. J. Vasc. Interv. Radiol. 2019, 30, 1915–1923. [Google Scholar] [CrossRef] [PubMed]
- Braat, A.J.A.T.; Bruijnen, R.C.G.; van Rooij, R.; Braat, M.N.G.J.A.; Wessels, F.J.; van Leeuwaarde, R.S.; van Treijen, M.J.C.; de Herder, W.W.; Hofland, J.; Tesselaar, M.E.T.; et al. Additional Holmium-166 Radioembolisation after Lutetium-177-Dotatate in Patients with Neuroendocrine Tumour Liver Metastases (HEPAR PLuS): A Single-Centre, Single-Arm, Open-Label, Phase 2 Study. Lancet Oncol. 2020, 21, 561–570. [Google Scholar] [CrossRef] [PubMed]
- Ramdhani, K.; Braat, A.J.A.T. The Evolving Role of Radioembolization in the Treatment of Neuroendocrine Liver Metastases. Cancers 2022, 14, 3415. [Google Scholar] [CrossRef] [PubMed]
- Taner, T.; Atwell, T.D.; Zhang, L.; Oberg, T.N.; Harmsen, W.S.; Slettedahl, S.W.; Kendrick, M.L.; Nagorney, D.M.; Que, F.G. Adjunctive Radiofrequency Ablation of Metastatic Neuroendocrine Cancer to the Liver Complements Surgical Resection. HPB 2013, 15, 190–195. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.W.; Kim, H.-C. Radioembolization for Hepatocellular Carcinoma: What Clinicians Need to Know. J. Liver Cancer 2022, 22, 4–13. [Google Scholar] [CrossRef] [PubMed]
- d’Abadie, P.; Hesse, M.; Louppe, A.; Lhommel, R.; Walrand, S.; Jamar, F. Microspheres Used in Liver Radioembolization: From Conception to Clinical Effects. Molecules 2021, 26, 3966. [Google Scholar] [CrossRef] [PubMed]
- Alrfooh, A.; Patel, A.; Laroia, S. Transarterial Radioembolization Agents: A Review of the Radionuclide Agents and the Carriers. Nucl. Med. Mol. Imaging 2021, 55, 162–172. [Google Scholar] [CrossRef] [PubMed]
- Sivananthan, G.; Tabori, N.E. Principles of Radioembolization. Semin. Interv. Radiol. 2021, 38, 393–396. [Google Scholar] [CrossRef]
- Sundram, F.X.; Buscombe, J.R. Selective Internal Radiation Therapy for Liver Tumours. Clin. Med. 2017, 17, 449–453. [Google Scholar] [CrossRef]
- Spreafico, C.; Maccauro, M.; Mazzaferro, V.; Chiesa, C. The Dosimetric Importance of the Number of 90Y Microspheres in Liver Transarterial Radioembolization (TARE). Eur. J. Nucl. Med. Mol. Imaging 2014, 41, 634–638. [Google Scholar] [CrossRef]
- Helmberger, T.; Golfieri, R.; Pech, M.; Pfammatter, T.; Arnold, D.; Cianni, R.; Maleux, G.; Munneke, G.; Pellerin, O.; Peynircioglu, B.; et al. Clinical Application of Trans-Arterial Radioembolization in Hepatic Malignancies in Europe: First Results from the Prospective Multicentre Observational Study CIRSE Registry for SIR-Spheres Therapy (CIRT). Cardiovasc. Interv. Radiol. 2021, 44, 21–35. [Google Scholar] [CrossRef] [PubMed]
- Frilling, A.; Clift, A.K.; Braat, A.J.A.T.; Alsafi, A.; Wasan, H.S.; Al-Nahhas, A.; Thomas, R.; Drymousis, P.; Habib, N.; Tait, P.N. Radioembolisation with 90Y Microspheres for Neuroendocrine Liver Metastases: An Institutional Case Series, Systematic Review and Meta-Analysis. HPB 2019, 21, 773–783. [Google Scholar] [CrossRef] [PubMed]
- Jia, Z.; Wang, W. Yttrium-90 Radioembolization for Unresectable Metastatic Neuroendocrine Liver Tumor: A Systematic Review. Eur. J. Radiol. 2018, 100, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Ngo, L.; Elnahla, A.; Attia, A.S.; Hussein, M.; Toraih, E.A.; Kandil, E.; Killackey, M. Chemoembolization Versus Radioembolization for Neuroendocrine Liver Metastases: A Meta-Analysis Comparing Clinical Outcomes. Ann. Surg. Oncol. 2021, 28, 1950–1958. [Google Scholar] [CrossRef] [PubMed]
- Singla, S.; LeVea, C.M.; Pokuri, V.K.; Attwood, K.M.; Wach, M.M.; Tomaszewski, G.M.; Kuvshinoff, B.; Iyer, R. Ki67 Score as a Potential Predictor in the Selection of Liver-Directed Therapies for Metastatic Neuroendocrine Tumors: A Single Institutional Experience. J. Gastrointest. Oncol. 2016, 7, 441–448. [Google Scholar] [CrossRef] [PubMed]
- Nadler, A.; Cukier, M.; Rowsell, C.; Kamali, S.; Feinberg, Y.; Singh, S.; Law, C.H.L. Ki-67 Is a Reliable Pathological Grading Marker for Neuroendocrine Tumors. Virchows Arch. 2013, 462, 501–505. [Google Scholar] [CrossRef]
- Schaarschmidt, B.M.; Wildgruber, M.; Kloeckner, R.; Nie, J.; Steinle, V.; Braat, A.J.A.T.; Lohoefer, F.; Kim, H.S.; Lahner, H.; Weber, M.; et al. 90Y Radioembolization in the Treatment of Neuroendocrine Neoplasms: Results of an International Multicenter Retrospective Study. J. Nucl. Med. 2022, 63, 679–685. [Google Scholar] [CrossRef] [PubMed]
- Cholapranee, A.; van Houten, D.; Deitrick, G.; Dagli, M.; Sudheendra, D.; Mondschein, J.I.; Soulen, M.C. Risk of Liver Abscess Formation in Patients with Prior Biliary Intervention Following Yttrium-90 Radioembolization. Cardiovasc. Interv. Radiol. 2015, 38, 397–400. [Google Scholar] [CrossRef] [PubMed]
- Gala, K.B.; Shetty, N.S.; Patel, P.; Kulkarni, S.S. Microwave Ablation: How We Do It? Indian. J. Radiol. Imaging 2020, 30, 206–213. [Google Scholar] [CrossRef]
- Lim, H.K. Radiofrequency Thermal Ablation of Hepatocellular Carcinomas. Korean J. Radiol. 2000, 1, 175–184. [Google Scholar] [CrossRef]
- Izzo, F.; Granata, V.; Grassi, R.; Fusco, R.; Palaia, R.; Delrio, P.; Carrafiello, G.; Azoulay, D.; Petrillo, A.; Curley, S.A. Radiofrequency Ablation and Microwave Ablation in Liver Tumors: An Update. Oncologist 2019, 24, e990–e1005. [Google Scholar] [CrossRef] [PubMed]
- Hong, K.; Georgiades, C. Radiofrequency Ablation: Mechanism of Action and Devices. J. Vasc. Interv. Radiol. 2010, 21, S179–S186. [Google Scholar] [CrossRef] [PubMed]
- Mazzaferro, V.; Battiston, C.; Perrone, S.; Pulvirenti, A.; Regalia, E.; Romito, R.; Sarli, D.; Schiavo, M.; Garbagnati, F.; Marchianò, A.; et al. Radiofrequency Ablation of Small Hepatocellular Carcinoma in Cirrhotic Patients Awaiting Liver Transplantation. Ann. Surg. 2004, 240, 900–909. [Google Scholar] [CrossRef] [PubMed]
- Lubner, M.G.; Brace, C.L.; Hinshaw, J.L.; Lee, F.T. Microwave Tumor Ablation: Mechanism of Action, Clinical Results and Devices. J. Vasc. Interv. Radiol. 2010, 21, S192–S203. [Google Scholar] [CrossRef] [PubMed]
- Simon, C.J.; Dupuy, D.E.; Mayo-Smith, W.W. Microwave Ablation: Principles and Applications. Radiographics 2005, 25 (Suppl. 1), S69–S83. [Google Scholar] [CrossRef] [PubMed]
- Poulou, L.S.; Botsa, E.; Thanou, I.; Ziakas, P.D.; Thanos, L. Percutaneous Microwave Ablation vs Radiofrequency Ablation in the Treatment of Hepatocellular Carcinoma. World J. Hepatol. 2015, 7, 1054–1063. [Google Scholar] [CrossRef] [PubMed]
- Pillai, K.; Akhter, J.; Chua, T.C.; Shehata, M.; Alzahrani, N.; Al-Alem, I.; Morris, D.L. Heat Sink Effect on Tumor Ablation Characteristics as Observed in Monopolar Radiofrequency, Bipolar Radiofrequency, and Microwave, Using Ex Vivo Calf Liver Model. Medicine 2015, 94, e580. [Google Scholar] [CrossRef] [PubMed]
- Niu, L.-Z.; Li, J.-L.; Xu, K.-C. Percutaneous Cryoablation for Liver Cancer. J. Clin. Transl. Hepatol. 2014, 2, 182–188. [Google Scholar] [CrossRef]
- Livraghi, T.; Vettori, C.; Lazzaroni, S. Liver Metastases: Results of Percutaneous Ethanol Injection in 14 Patients. Radiology 1991, 179, 709–712. [Google Scholar] [CrossRef]
- Seifert, J.K.; Cozzi, P.J.; Morris, D.L. Cryotherapy for Neuroendocrine Liver Metastases. Semin. Surg. Oncol. 1998, 14, 175–183. [Google Scholar] [CrossRef]
- Perrodin, S.F.; Renzulli, M.M.; Maurer, M.H.; Kim-Fuchs, C.; Candinas, D.; Beldi, G.; Lachenmayer, A. Can Microwave Ablation Be an Alternative to Resection for the Treatment of Neuroendocrine Liver Metastases? Endocr. Pract. 2020, 26, 378–387. [Google Scholar] [CrossRef] [PubMed]
- Mazzaglia, P.J.; Berber, E.; Milas, M.; Siperstein, A.E. Laparoscopic Radiofrequency Ablation of Neuroendocrine Liver Metastases: A 10-Year Experience Evaluating Predictors of Survival. Surgery 2007, 142, 10–19. [Google Scholar] [CrossRef] [PubMed]
- Maxwell, J.E.; Sherman, S.K.; O’Dorisio, T.M.; Bellizzi, A.M.; Howe, J.R. Liver-Directed Surgery of Neuroendocrine Metastases: What Is the Optimal Strategy? Surgery 2016, 159, 320–335. [Google Scholar] [CrossRef] [PubMed]
- Mohan, H.; Nicholson, P.; Winter, D.C.; O’Shea, D.; O’Toole, D.; Geoghegan, J.; Maguire, D.; Hoti, E.; Traynor, O.; Cantwell, C.P. Radiofrequency Ablation for Neuroendocrine Liver Metastases: A Systematic Review. J. Vasc. Interv. Radiol. 2015, 26, 935–942.e1. [Google Scholar] [CrossRef] [PubMed]
- Pickens, R.C.; Sulzer, J.K.; Passeri, M.J.; Murphy, K.; Vrochides, D.; Martinie, J.B.; Baker, E.H.; Ocuin, L.M.; McKillop, I.H.; Iannitti, D.A. Operative Microwave Ablation for the Multimodal Treatment of Neuroendocrine Liver Metastases. J. Laparoendosc. Adv. Surg. Tech. A 2021, 31, 917–925. [Google Scholar] [CrossRef] [PubMed]
- Matrood, S.; Gress, T.M.; Rinke, A.; Mahnken, A.H. Radiofrequency and Microwave Ablation Controls Hepatic Oligoprogression of Advanced Gastroenteropancreatic Neuroendocrine Tumors. J. Neuroendocrinol. 2023, 35, e13289. [Google Scholar] [CrossRef]
- Cazzato, R.L.; Hubelé, F.; De Marini, P.; Ouvrard, E.; Salvadori, J.; Addeo, P.; Garnon, J.; Kurtz, J.-E.; Greget, M.; Mertz, L.; et al. Liver-Directed Therapy for Neuroendocrine Metastases: From Interventional Radiology to Nuclear Medicine Procedures. Cancers 2021, 13, 6368. [Google Scholar] [CrossRef]
- Yordanova, A.; Ahmadzadehfar, H. Combination Therapies with PRRT. Pharmaceuticals 2021, 14, 1005. [Google Scholar] [CrossRef]
- Kim, H.S.; Shaib, W.L.; Zhang, C.; Nagaraju, G.P.; Wu, C.; Alese, O.B.; Chen, Z.; Brutcher, E.; Renfroe, M.; El-Rayes, B.F. Phase 1b Study of Pasireotide, Everolimus, and Selective Internal Radioembolization Therapy for Unresectable Neuroendocrine Tumors with Hepatic Metastases. Cancer 2018, 124, 1992–2000. [Google Scholar] [CrossRef]
- Filippi, L.; Ciorra, A.; Sardella, B.; Schillaci, O.; Bagni, O. Sequential Use of 90Y Microspheres Radioembolization and 177Lu-Dotatate in Pluri-Metastatic Neuroendocrine Tumors: A Case Report. Nucl. Med. Mol. Imaging 2014, 48, 321–325. [Google Scholar] [CrossRef]
- Geisler, J.; Auernhammer, C.; Zech, C.; Bartenstein, P.; Hacker, M.; Haug, A. Toxicity of Sequential Treatment with Radioembolization and PRRT in Hepatic Metastasized Neuroendocrine Tumors. J. Nucl. Med. 2012, 53, 1189. [Google Scholar]
- Braat, A.J.A.T.; Ahmadzadehfar, H.; Kappadath, S.C.; Stothers, C.L.; Frilling, A.; Deroose, C.M.; Flamen, P.; Brown, D.B.; Sze, D.Y.; Mahvash, A.; et al. Radioembolization with 90Y Resin Microspheres of Neuroendocrine Liver Metastases After Initial Peptide Receptor Radionuclide Therapy. Cardiovasc. Interv. Radiol. 2020, 43, 246–253. [Google Scholar] [CrossRef]
- Strosberg, J.; Kunz, P.L.; Hendifar, A.; Yao, J.; Bushnell, D.; Kulke, M.H.; Baum, R.P.; Caplin, M.; Ruszniewski, P.; Delpassand, E.; et al. Impact of Liver Tumour Burden, Alkaline Phosphatase Elevation, and Target Lesion Size on Treatment Outcomes with 177Lu-Dotatate: An Analysis of the NETTER-1 Study. Eur. J. Nucl. Med. Mol. Imaging 2020, 47, 2372–2382. [Google Scholar] [CrossRef] [PubMed]
- Yilmaz, N.; Yilmaz, U.E.; Suer, K.; Goral, V.; Cakir, N. Screening for Hepatocellular Carcinoma: Summary of Current Guidelines up to 2018. Hepatoma Res. 2018, 4, 46. [Google Scholar] [CrossRef]
- Ezziddin, S.; Meyer, C.; Kahancova, S.; Haslerud, T.; Willinek, W.; Wilhelm, K.; Biersack, H.-J.; Ahmadzadehfar, H. 90Y Radioembolization after Radiation Exposure from Peptide Receptor Radionuclide Therapy. J. Nucl. Med. 2012, 53, 1663–1669. [Google Scholar] [CrossRef]
- Strosberg, J.; Hendifar, A.; Yao, J.C.; Kulke, M.; O’Dorisio, T.; Caplin, M.; Baum, R.P.; Kunz, P.; Hobday, T.; Wolin, E.; et al. Impact of Liver Tumor Burden on Therapeutic Effect of 177Lu-Dotatate Treatment in NETTER-1 Study. Ann. Oncol. 2018, 29, viii471. [Google Scholar] [CrossRef]
- Ebbers, S.C.; Braat, A.J.A.T.; Moelker, A.; Stokkel, M.P.M.; Lam, M.G.E.H.; Barentsz, M.W. Intra-Arterial versus Standard Intravenous Administration of Lutetium-177-DOTA-Octreotate in Patients with NET Liver Metastases: Study Protocol for a Multicenter, Randomized Controlled Trial (LUTIA Trial). Trials 2020, 21, 141. [Google Scholar] [CrossRef] [PubMed]
- Ebbers, S.C.; Barentsz, M.W.; de Vries-Huizing, D.M.V.; Versleijen, M.W.J.; Klompenhouwer, E.G.; Tesselaar, M.E.T.; Stokkel, M.P.M.; Brabander, T.; Hofland, J.; Moelker, A.; et al. Intra-Arterial Peptide-Receptor Radionuclide Therapy for Neuro-Endocrine Tumour Liver Metastases: An in-Patient Randomised Controlled Trial (LUTIA). Eur. J. Nucl. Med. Mol. Imaging 2024, 51, 1121–1132. [Google Scholar] [CrossRef]
- Deroose, C.M. The LUTIA Trial: A Small Step for PRRT, a Giant Leap for Intra-Arterial Radionuclide Therapy Trial Methodology. Eur. J. Nucl. Med. Mol. Imaging 2024, 51, 1133–1135. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Criss, C.R.; Makary, M.S. Liver-Directed Locoregional Therapies for Neuroendocrine Liver Metastases: Recent Advances and Management. Curr. Oncol. 2024, 31, 2076-2091. https://doi.org/10.3390/curroncol31040154
Criss CR, Makary MS. Liver-Directed Locoregional Therapies for Neuroendocrine Liver Metastases: Recent Advances and Management. Current Oncology. 2024; 31(4):2076-2091. https://doi.org/10.3390/curroncol31040154
Chicago/Turabian StyleCriss, Cody R., and Mina S. Makary. 2024. "Liver-Directed Locoregional Therapies for Neuroendocrine Liver Metastases: Recent Advances and Management" Current Oncology 31, no. 4: 2076-2091. https://doi.org/10.3390/curroncol31040154
APA StyleCriss, C. R., & Makary, M. S. (2024). Liver-Directed Locoregional Therapies for Neuroendocrine Liver Metastases: Recent Advances and Management. Current Oncology, 31(4), 2076-2091. https://doi.org/10.3390/curroncol31040154





