Prognostic Value of Performance Status, Albumin, and CRP in Last-Line Chemotherapy for Pancreatic vs. Other Gastrointestinal Cancers—Simple Tools Matter
Abstract
:1. Introduction
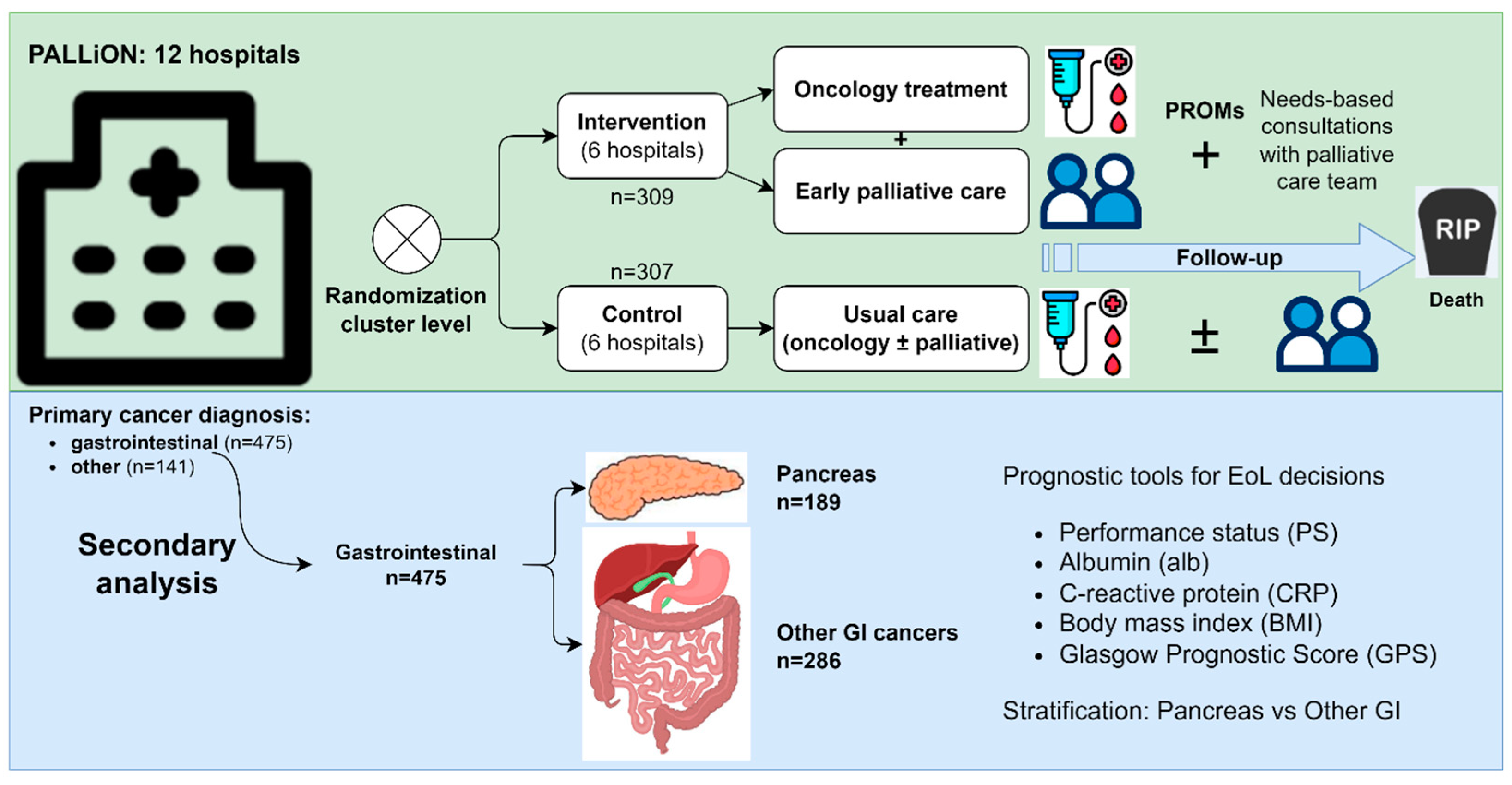
2. Materials and Methods
2.1. Study Design
2.2. Prognostic Factors
2.3. Statistical Analyses
2.4. Ethical Approval and Consent
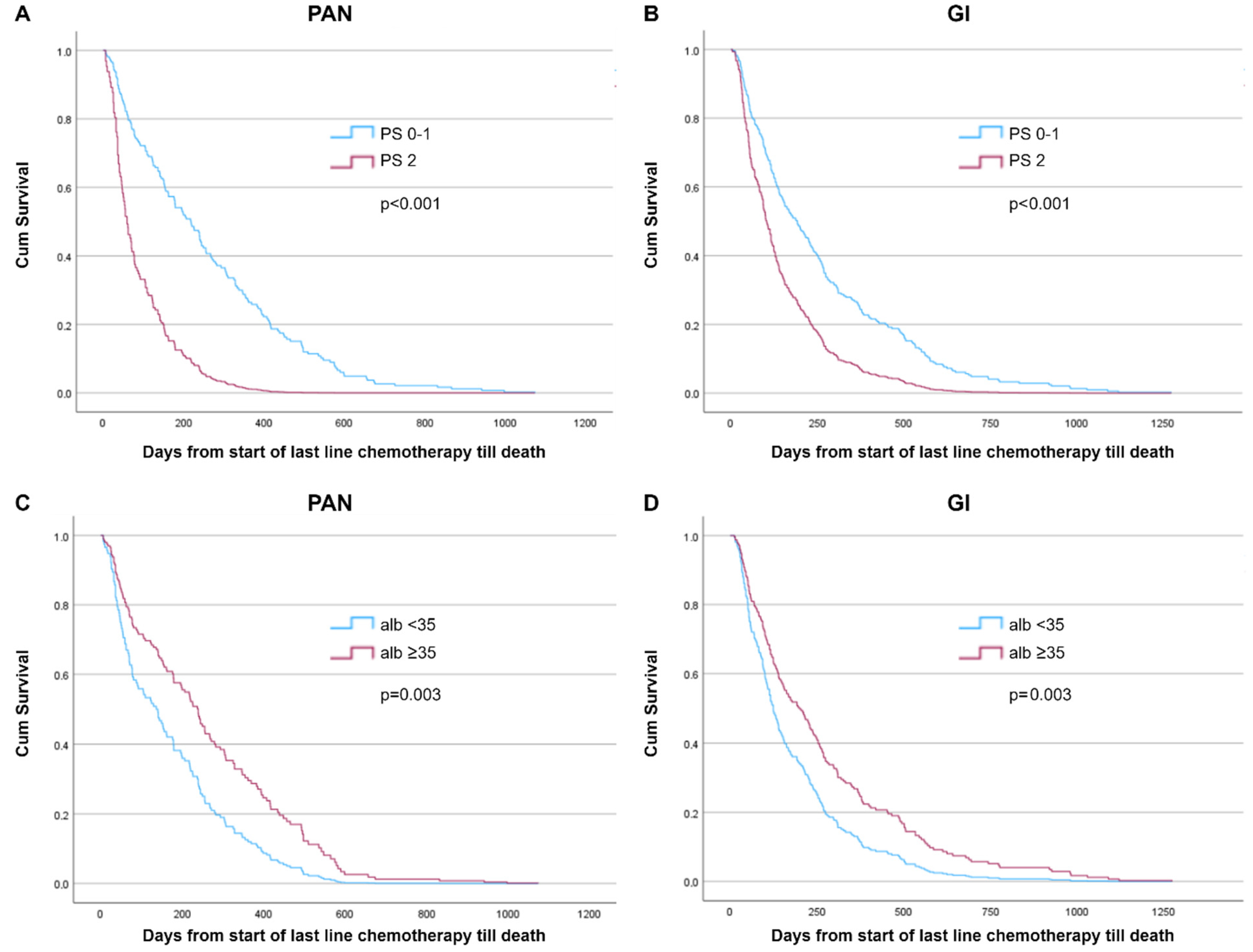
3. Results
4. Discussion
4.1. Comparison with Previous Studies
4.2. Future Directions
4.3. Strengths and Limitations
4.4. Clinical Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Crawford, G.B.; Dzierżanowski, T.; Hauser, K.; Larkin, P.; Luque-Blanco, A.I.; Murphy, I.; Puchalski, C.M.; Ripamonti, C.I.; ESMO Guidelines Committee. Care of the adult cancer patient at the end of life: ESMO Clinical Practice Guidelines. ESMO Open. 2021, 6, 100225. [Google Scholar] [CrossRef] [PubMed]
- These Countries Have the Most Well-Developed Public Health Systems: U.S. News. Available online: https://www.usnews.com/news/best-countries/rankings/well-developed-public-health-system (accessed on 11 September 2024).
- OECD/European Observatory on Health Systems and Policies. Norway: Country Health Profile 2023: State of Health in the EU; OECD Publishing: Paris, France, 2023. [Google Scholar] [CrossRef]
- Norwegian Quality Registry for Pancreatic Cancer, Yearly Report 2023. Available online: https://www.kreftregisteret.no/en/The-Registries/clinical-registries/Quality-registry-for-pancreatic-cancer/ (accessed on 11 September 2024).
- Simmons, C.P.L.; McMillan, D.C.; McWilliams, K.; Sande, T.A.; Fearon, K.C.; Tuck, S.; Fallon, M.T.; Laird, B.J. Prognostic Tools in Patients with Advanced Cancer: A Systematic Review. J. Pain Symptom. Manag. 2017, 53, 962–970.e10. [Google Scholar] [CrossRef] [PubMed]
- Proctor, M.J.; Morrison, D.S.; Talwar, D.; Balmer, S.M.; O’Reilly, D.S.; Foulis, A.K.; Horgan, P.G.; McMillan, D.C. An inflammation-based prognostic score (mGPS) predicts cancer survival independent of tumour site: A Glasgow Inflammation Outcome Study. Br. J. Cancer 2011, 104, 726–734. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Ren, D.; Jin, X.; Wu, H. The prognostic value of modified Glasgow Prognostic Score in pancreatic cancer: A meta-analysis. Cancer Cell. Int. 2020, 20, 462. [Google Scholar] [CrossRef] [PubMed]
- Halbrook, C.J.; Lyssiotis, C.A.; Pasca di Magliano, M.; Maitra, A. Pancreatic cancer: Advances and challenges. Cell 2023, 186, 1729–1754. [Google Scholar] [CrossRef] [PubMed]
- Hjermstad, M.J.; Pirnat, A.; Aass, N.; Andersen, S.; Astrup, G.L.; Dajani, O.; Garresori, H.; Guldhav, K.V.; Hamre, H.; Haukland, E.C.; et al. PALLiative care in ONcology (PALLiON): A cluster-randomised trial investigating the effect of palliative care on the use of anticancer treatment at the end of life. Palliat. Med. 2024, 38, 229–239. [Google Scholar] [CrossRef] [PubMed]
- Hjermstad, M.J.; Aass, N.; Andersen, S.; Brunelli, C.; Dajani, O.; Garresori, H.; Hamre, H.; Haukland, E.C.; Holmberg, M.; Jordal, F.; et al. PALLiON—PALLiative care Integrated in ONcology: Study protocol for a Norwegian national cluster-randomized control trial with a complex intervention of early integration of palliative care. Trials 2020, 21, 303. [Google Scholar] [CrossRef] [PubMed]
- Oken, M.M.; Creech, R.H.; Tormey, D.C.; Horton, J.; Davis, T.E.; McFadden, E.T.; Carbone, P.P. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am. J. Clin. Oncol. 1982, 5, 649–655. [Google Scholar] [CrossRef] [PubMed]
- Buccheri, G.; Ferrigno, D.; Tamburini, M. Karnofsky and ECOG performance status scoring in lung cancer: A prospective, longitudinal study of 536 patients from a single institution. Eur. J. Cancer 1996, 32, 1135–1141. [Google Scholar] [CrossRef]
- Spruance, S.L.; Reid, J.E.; Grace, M.; Samore, M. Hazard ratio in clinical trials. Antimicrob. Agents Chemother. 2004, 48, 2787–2792. [Google Scholar] [CrossRef] [PubMed]
- Heikkilä, R.; Kaasa, S. Chemotherapy in end-of-life care. Ann. Oncol. 2017, 28, 684–685. [Google Scholar] [CrossRef] [PubMed]
- Akhlaghi, E.; Lehto, R.H.; Torabikhah, M.; Sharif Nia, H.; Taheri, A.; Zaboli, E.; Yaghoobzadeh, A. Chemotherapy use and quality of life in cancer patients at the end of life: An integrative review. Health Qual. Life Outcomes 2020, 18, 332. [Google Scholar] [CrossRef] [PubMed]
- Dolan, R.D.; McSorley, S.T.; Horgan, P.G.; Laird, B.; McMillan, D.C. The role of the systemic inflammatory response in predicting outcomes in patients with advanced inoperable cancer: Systematic review and meta-analysis. Crit. Rev. Oncol. Hematol. 2017, 116, 134–146. [Google Scholar] [CrossRef] [PubMed]
- Rocha, B.M.M.; Dolan, R.D.; Paiva, C.E.; McGovern, J.; Paiva, B.S.R.; Preto, D.D.; McMillan, D.C.; Maia, Y.C.P.; Laird, B.J. Inflammation and Performance Status: The Cornerstones of Prognosis in Advanced Cancer. J. Pain Symptom. Manag. 2023, 65, 348–357. [Google Scholar] [CrossRef]
- Jatoi, A.; Kaasa, S.; Strijbos, M. ESMO Handbook of Nutrition and Cancer, 2nd ed.; ESMO Press: Lugano, Switzerland, 2023. [Google Scholar]
- Canavan, M.E.; Wang, X.; Ascha, M.S.; Miksad, R.A.; Showalter, T.N.; Calip, G.S.; Gross, C.P.; Adelson, K.B. Systemic Anticancer Therapy and Overall Survival in Patients with Very Advanced Solid Tumors. JAMA Oncol. 2024, 10, 887–895. [Google Scholar] [CrossRef] [PubMed]
- Oettle, H.; Reiss, H.; Stieler, J.M.; Heil, G.; Schwaner, I.; Seraphin, J.; Görner, M.; Mölle, M.; Greten, T.F.; Lakner, V.; et al. Second-Line Oxaliplatin, Folinic Acid, and Fluorouracil Versus Folinic Acid and Fluorouracil Alone for Gemcitabine-Refractory Pancreatic Cancer: Outcomes From the CONKO-003. Trial. J. Clin. Oncol. 2014, 32, 2423–2429. [Google Scholar] [CrossRef]
- Gill, S.; Ko, Y.-J.; Cripps, C.; Beaudoin, A.; Dhesy-Thind, S.; Zulfigar, M.; Zalewski, P.; Do, T.; Cano, P.; Lam, W.Y.H.; et al. PANCREOX: A Randomized Phase III Study of Fluorouracil/Leucovorin with or without Oxaliplatin for Second-Line Advanced Pancreatic Cancer in Patients Who Have Received Gemcitabine-Based Chemotherapy. J. Clin. Oncol. 2016, 34, 3914–3920. [Google Scholar] [CrossRef] [PubMed]
- MyPath—The Digital Solution to Patient-Centred Cancer Care. Available online: https://mypath-cancercare.eu/ (accessed on 11 September 2024).

| Characteristics | PAN (N = 189) | GI (N = 286) | p | |
|---|---|---|---|---|
| Age | Mean (±SD) | 67.7 (8.76) | 67.2 (10.24) | 0.54 |
| Sex (%) | Male | 124 (65.6) | 177 (61.9) | 0.44 |
| Female | 65 (34.4) | 109 (38.1) | ||
| PS (%) | 0–1 | 178 (94.2) | 265 (92.7) | |
| 2 | 11 (5.8) | 19 (6.6) | 0.85 | |
| 3 | 0 | 2 (0.7) | ||
| BMI 1 (%) | <18.5 | 8 (4.2) | 14 (4.9) | 0.73 |
| ≥18.5 | 181 (95.8) | 271 (94.8) | ||
| Main cancer diagnosis (%) | Pancreas | 189 (100.0) | - | NA |
| Colorectal | - | 131 (45.8) | ||
| Cholangiocarcinoma | - | 57 (19.9) | ||
| Gastric | - | 41 (14.3) | ||
| Oesophagus | - | 35 (12.2) | ||
| Rectum | - | 21 (7.3) | ||
| Liver | - | 1 (0.3) | ||
| mGPS 2 (%) | 0 | 29 (15.3) | 30 (10.4) | 0.47 |
| 1 | 56 (29.6) | 96 (33.6) | ||
| 2 | 33 (17.5) | 46 (16.1) | ||
| Albumin 3 (%) | <35 g/L | 48 (25.4) | 61 (21.3) | 0.42 |
| ≥35 g/L | 101 (53.4) | 158 (55.2) | ||
| CRP 4 (%) | ≤10 mg/L | 31 (16.4) | 30 (10.5) | 0.08 |
| >10 mg/L | 90 (47.6) | 142 (49.6) | ||
| Hospital size (%) | Large | 102 (53.9) | 149 (52.1) | 0.73 |
| Medium | 51 (2.6) | 89 (31.1) | ||
| Small | 36 (19.0) | 48 (16.8) | ||
| Pancreatic Cancer | Other Gastrointestinal Cancers | |||||
|---|---|---|---|---|---|---|
| N | HR (95% CI) | p | N | HR (95% CI) | p | |
| Performance status | ||||||
| PS 0–1 | 178 | 1.00 Reference | 265 | 1.0 Reference | ||
| PS ≥ 2 | 11 | 3.38 (1.75–6.53) | <0.001 | 21 | 1.90 (1.14–3.15) | 0.01 |
| Albumin (g/L) | ||||||
| <35 | 48 | 1.74 (1.21–2.50) | 0.003 | 61 | 1.55 (0.93–2.60) | 0.01 |
| ≥35 | 101 | 1.0 Reference | 158 | 1.0 Reference | ||
| CRP (mg/L) | ||||||
| ≤10 | 31 | 1.00 Reference | 30 | 1.0 Reference | ||
| >10 | 90 | 1.48 (0.95–2.90) | 0.81 | 142 | 2.09 (1.31–3.34) | 0.002 |
| mGPS | ||||||
| 0 | 29 | 1.00 Reference | 30 | 1.0 Reference | ||
| 1 | 56 | 1.21 (0.73–2.02) | 0.46 | 96 | 1.57 (0.94–2.62) | 0.08 |
| 2 | 33 | 2.20 (1.26–3.83) | 0.005 | 46 | 2.42 (1.40–4.19) | 0.002 |
| Model | Parameter | p | HR | Probability |
|---|---|---|---|---|
| Estimate | (95% CI) | |||
| Pancreatic cancer (N = 189) | ||||
| Basic model * + mGPS | ||||
| PS ≥ 2 | 1.29 | 0.002 | 3.63 (1.60–8.24) | 78.4% |
| mGPS 2 | 0.79 | 0.005 | 2.20 (1.26–3.83) | 68.7% |
| Other GI cancers (n = 286) | ||||
| Basic model * + mGPS | ||||
| PS ≥ 2 | 0.12 | 0.70 | 1.12 (0.62–2.03) | 52.8% |
| mGPS 2 | 0.88 | 0.002 | 2.42 (1.40–4.19) | 70.8% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Westgaard, A.; Pirnat, A.; Hjermstad, M.J.; Aass, N.; Kaasa, S.; Dajani, O.F. Prognostic Value of Performance Status, Albumin, and CRP in Last-Line Chemotherapy for Pancreatic vs. Other Gastrointestinal Cancers—Simple Tools Matter. Curr. Oncol. 2024, 31, 5462-5471. https://doi.org/10.3390/curroncol31090404
Westgaard A, Pirnat A, Hjermstad MJ, Aass N, Kaasa S, Dajani OF. Prognostic Value of Performance Status, Albumin, and CRP in Last-Line Chemotherapy for Pancreatic vs. Other Gastrointestinal Cancers—Simple Tools Matter. Current Oncology. 2024; 31(9):5462-5471. https://doi.org/10.3390/curroncol31090404
Chicago/Turabian StyleWestgaard, Arne, Aleksandra Pirnat, Marianne Jensen Hjermstad, Nina Aass, Stein Kaasa, and Olav Faisal Dajani. 2024. "Prognostic Value of Performance Status, Albumin, and CRP in Last-Line Chemotherapy for Pancreatic vs. Other Gastrointestinal Cancers—Simple Tools Matter" Current Oncology 31, no. 9: 5462-5471. https://doi.org/10.3390/curroncol31090404
APA StyleWestgaard, A., Pirnat, A., Hjermstad, M. J., Aass, N., Kaasa, S., & Dajani, O. F. (2024). Prognostic Value of Performance Status, Albumin, and CRP in Last-Line Chemotherapy for Pancreatic vs. Other Gastrointestinal Cancers—Simple Tools Matter. Current Oncology, 31(9), 5462-5471. https://doi.org/10.3390/curroncol31090404






