Laterally Positioned Flap Procedure with Augmented or Nonaugmented Palatal Connective Tissue Grafts in the Treatment of Multiple Adjacent Gingival Recessions: A Two-Year Follow-Up Study
Abstract
:1. Introduction
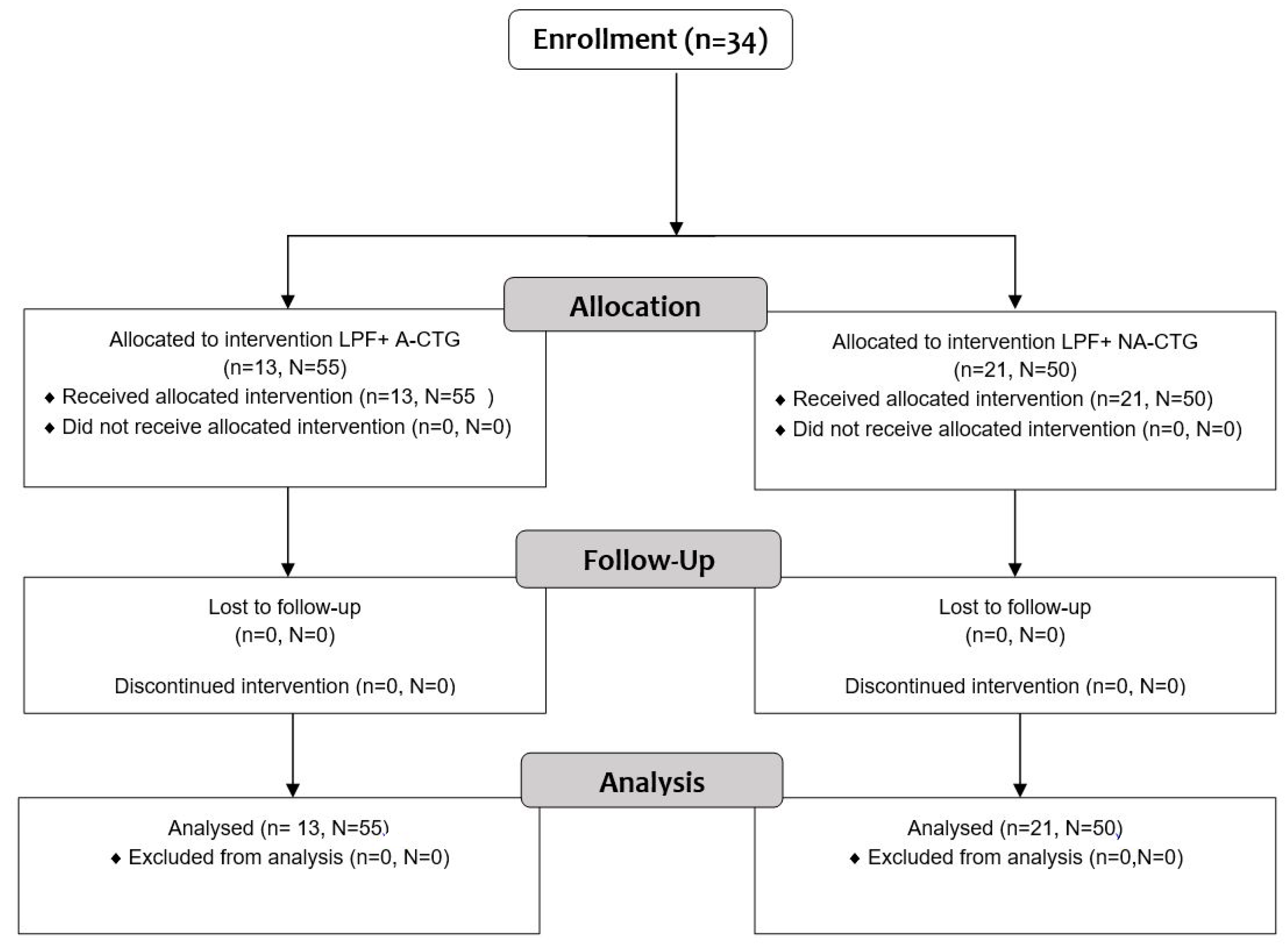
2. Materials and Methods
2.1. Study Population
2.2. Clinical Measurements
2.3. Surgical Procedures
2.4. Post-Surgical Management
2.5. Statistical Analysis
3. Results
3.1. Clinical Measurements for CAL and GRD
3.2. Clinical Measurements for GRW, PD and AG
3.3. Clinical Measurements for BGT1, BGT2, BGT3
3.4. Clinical Values for CRC and ARC
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Dominiak, M.; Gedrange, T. New perspectives in the diagnostic of gingival recession. Adv. Clin. Exp. Med. 2014, 23, 857–863. [Google Scholar] [CrossRef] [PubMed]
- Cairo, F. Periodontal plastic surgery of gingival recessions at single and multiple teeth. Periodontology 2000 2017, 75, 296–316. [Google Scholar] [CrossRef] [PubMed]
- Zucchelli, G.; Cesari, C.; Amore, C.; Montebugnoli, L.; De Sanctis, M. Laterally moved, coronally advanced flap: A modified surgical approach for isolated recession-type defects. J. Periodontol. 2004, 75, 1734–1741. [Google Scholar] [CrossRef] [PubMed]
- Grupe, H.E.; Warren, R.F., Jr. Repair of gingival defects by a sliding flap operation. J. Periodontol. 1956, 27, 92–95. [Google Scholar] [CrossRef]
- Caffesse, R.G.; Kon, S.; Castelli, W.A.; Nasjleti, C. Revascularization following the lateral sliding flap procedure. J. Periodontol. 1984, 55, 352–358. [Google Scholar] [CrossRef]
- Guinard, E.A.; Caffesse, R.G. Treatment of localized gingival recessions. Part 1. Lateral sliding flap. J. Periodontol. 1978, 49, 351–356. [Google Scholar] [CrossRef]
- Grupe, H.E. Modified Technique for the Sliding Flap Operation. J. Periodontol. 1966, 37, 491–495. [Google Scholar] [CrossRef]
- Staffileno, H. Management of gingival recession and root exposure problems associated with periodontal disease. Dent. Clin. N. Am. 1964, 8, 111–120. [Google Scholar] [CrossRef]
- Ruben, M.P.; Goldman, H.M.; Janson, W. Biological considerations in laterally repositioned pedicle flaps and free autogenous gingival grafts in periodontal therapy. In Periodontal Surgery—Biologic Basis and Technique; Stahl, S.S., Ed.; Charles, C. Thomas: Springfield, IL, USA, 1975; p. 235. [Google Scholar]
- Pfeifer, J.S.; Heller, R. Histologic evaluation of full and partial-tickness laterally repositioned flaps—A pilot study. J. Periodontol. 1971, 42, 331. [Google Scholar] [CrossRef]
- Cohen, D.; Ross, S. The double papillae repositioned flap in periodontal therapy. J. Periodontol. 1968, 39, 65–70. [Google Scholar] [CrossRef]
- Caffesse, R.G.; Espinel, M.C. Lateral sliding flap with a free gingival graft technique in the treatment of localized gingival recessions. Int. J. Periodontics Restor. Dent. 1981, 1, 23–29. [Google Scholar]
- Espinel, M.C.; Caffesse, R.G. Comparison of the results obtained with the laterally positioned pedicle sliding flap—Revised technique and the laterally sliding flap with a free gingival graft technique in the treatment of localized gingival recessions. Int. J. Periodontics Restor. Dent. 1981, 1, 31–38. [Google Scholar]
- Nelson, S.W. The subpedicle connective tissue graft. A bilaminar reconstructive procedure for the coverage of denuded root surfaces. J. Periodontol. 1987, 58, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Blanes, J.R.; Allen, E.P. The bilateral pedicle flap-tunnel technique: A New approach to cover connective tissue grafts. Int. J. Periodontics Restor. Dent. 1999, 19, 471–479. [Google Scholar]
- Harris, R. The connective tissue and partial thickness double pedicle graft: A predictable method of obtaining root coverage. J. Periodontol. 1992, 63, 477–486. [Google Scholar] [CrossRef] [PubMed]
- Santana, R.B.; Furtado, M.B.; Mattos, C.M.; de Mello Fonseca, E.; Dibart, S. Clinical evaluation of single-stage advanced versus rotated flaps in the treatment of gingival recessions. J. Periodontol. 2010, 81, 485–492. [Google Scholar] [CrossRef]
- Zucchelli, G.; De Sanctis, M. Modified two-stage procedures for the treatment of gingival recession. Eur. J. Esthet. Dent. 2013, 8, 24–42. [Google Scholar]
- Agarwal, C.; Purohit, P.; Sharma, S.K.; Sharma, A. Modified approach of double papillae laterally positioned flap technique using Alloderm® for root coverage. J. Clin. Diagn. Res. 2014, 8, 25–27. [Google Scholar] [CrossRef]
- Ahmedbeyli, C.; Ipci, S.D.; Cakar, G.; Yilmaz, S. Laterally positioned flap along with acellular dermal matrix graft in the management of maxillary localized recessions. Clin. Oral Investig. 2019, 23, 595–601. [Google Scholar] [CrossRef]
- Ricci, G.; Silvestri, M.; Tinti, C.; Rasperini, G. A clinical/statistical comparison between the subpedicle connective tissue graft method and the guided tissue regeneration technique in root coverage. Int. J. Periodontics Restor. Dent. 1996, 16, 538–545. [Google Scholar]
- Lee, C.T.; Chang, P.C.; Touchan, N.; Royzman, D. Root coverage with a modified laterally positioned flap combined with a subepithelial connective tissue graft in advanced recession. J. Periodontal. Implant. Sci. 2014, 44, 300–306. [Google Scholar] [CrossRef]
- Carnio, J.; Koutouzis, T. Palatal Augmentation Technique. A Predictable Method to Increase the Palatal Connective Tissue Donor Site: A Consecutive Case Series. Int. J. Periodontics Restor. Dent. 2015, 35, 707–713. [Google Scholar] [CrossRef] [PubMed]
- Bednarz, W.; Kobierzycki, C.; Dzięgiel, P.; Botzenhartd, U.; Gedrange, T.; Ziętek, M. Augmentation of the hard palate thin masticatory mucosa in the potential connective tissue donor sites using two collagen materials—Clinical and histological comparison. Ann. Anat. 2016, 208, 78–84. [Google Scholar] [CrossRef]
- Bednarz, W.; Majer, J.; Pakuszyńska-Błaszczyk, J.; Dominiak, M.; Gedrange, T.; Zielińska-Pałasz, A. Coronally Advanced Flap in the Treatment of Multiple Adjacent Gingival Recessions along with a Connective Tissue Graft Harvested from Augmented or Nonaugmented Palatal Mucous Membrane: A Two-Year Comparative Clinical Evaluation. Appl. Sci. 2021, 11, 1081. [Google Scholar] [CrossRef]
- Yilmaz, E.; Ozcelik, O.; Comert, M.; Ozturan, S.; Seydaoglu, G.; Teughels, W.; Haytac, M.C. Laser-assisted laterally positioned flap operation: A randomized controlled clinical trial. Photomed. Laser Surg. 2014, 32, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Sculean, A.; Allen, E.P. The laterally closed tunnel for the treatment of deep isolated mandibular recessions: Surgical technique and a report of 24 cases. Int. J. Periodontics Restor. Dent. 2018, 38, 479–487. [Google Scholar] [CrossRef]
- Ucak, O.; Ozcan, M.; Seydaoglu, G.; Haytac, M.C. Microsurgical instruments in laterally moved, coronally advanced flap for Miller Class III isolated recession defects: A randomized controlled clinical trial. Int. J. Periodontics Restor. Dent. 2014, 37, 109–115. [Google Scholar] [CrossRef]
- Burkhardt, R.; Lang, N.P. Coverage of localized gingival recessions: Comparison of micro- and macrosugical techniques. J. Clin. Periodontol. 2005, 32, 287–293. [Google Scholar] [CrossRef]
- Pini Prato, G.P.; Baldi, C.; Nieri, M.; Franseschi, D.; Cortellinii, P.; Clauser, C.; Rotundo, R.; Muzzi, L. Coronally Advanced Flap: The post-surgical position of the gingival margin is an important factor for achieving complete root coverage. J. Periodontol. 2005, 76, 713–722. [Google Scholar] [CrossRef]
- Ozcelik, O.; Seydaoglu, G.; Haytac, C.M. An Explorative Study to Develop a Predictive Model Based on Avascular Exposed Root Surface Area for Root Coverage After a Laterally Positioned Flap. J. Periodontol. 2015, 86, 356–366. [Google Scholar] [CrossRef]
- Carnio, J. Modified apically repositioned flap technique: A surgical approach to enhance donor sites prior to employing a laterally positioned flap. Int. J. Periodontics Restor. Dent. 2014, 34, 423–429. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, R.C.; Joly, J.C.; De Lima, A.; Tatakis, D. Root coverage using the coronally positioned flap with or without a subepithelial connective tissue graft. J. Periodontol. 2004, 75, 413–419. [Google Scholar] [CrossRef] [PubMed]
- Bednarz, W.; Zielinska, A. Ultrasonic Biometer and its usage in an assessment of periodontal soft tissue thickness and comparison of its measurement accuracy with a bone sounding method. Dent. Med. Probl. 2011, 48, 481–489. [Google Scholar]
- Zucchelli, G.; Mele, M.; Stefanini, M.; Mazzotti, C.; Marzadori, M.; Montebugnoli, L.; de Sanctis, M. Patient morbidity and root coverage outcome after subepithelial connective tissue and de-epithelialized grafts: A randomized-controlled clinical trial. J. Clin. Periodontol. 2010, 37, 728–738. [Google Scholar] [CrossRef] [PubMed]
- Cairo, F.; Cortellini, P.; Pilloni, A.; Nieri, M.; Cincinelli, S.; Amunni, F.; Pagavino, G.; Tonetti, M. Clinical efficacy of coronally advanced flap with or without connective tissue graft for the treatment of multiple adjacent gingival recessions in the aesthetic area: A randomized controlled clinical trial. J. Clin. Periodontol. 2016, 43, 849–856. [Google Scholar] [CrossRef]
- Clementini, M.; Discepoli, N.; Danesi, C.; de Sanctis, M. Biologically guided flap stability: The role of flap thickness including periosteum retention on the performance of the coronally advanced flap–A double-blind randomized clinical trial. J. Clin. Periodontol. 2018, 45, 1238–1246. [Google Scholar] [CrossRef]
- Pietruska, M.; Skurska, A.; Podlewski, Ł.; Milewski, R.; Pietruski, J. Clinical evaluation of Miller class I and II recessions treatment with the use of modified coronally advanced tunnel technique with either collagen matrix or subepithelial connective tissue graft: A randomized clinical study. J. Clin. Periodontol. 2019, 46, 86–95. [Google Scholar] [CrossRef]
- Barootchi, S.; Tavelli, L.; Di Gianfilippo, R.; Byun, H.-Y.; Oh, T.-J.; Barbato, L.; Cairo, F.; Wang, H.-L. Long term assessment of root coverage stability using connective tissue graft with or without an epithelial collar for gingival recession treatment. A 12-year follow-up from a randomized clinical trial. J. Clin. Periodontol. 2019, 46, 1124–1133. [Google Scholar] [CrossRef]
- Tavelli, L.; Barootchi, S.; Di Gianfilippo, R.; Modarressi, M.; Cairo, F.; Rasperini, G.; Wang, H.-L. Acellular dermal matrix and coronally advanced flap or tunnel technique in the treatment of multiple adjacent gingival recessions. A 12-year follow-up from a randomized clinical trial. J. Clin. Periodontol. 2019, 46, 937–948. [Google Scholar] [CrossRef]
- Leong, D.J.; Wang, H.L. A decision tree for soft tissue grafting. Int. J. Periodontics Restor. Dent. 2011, 31, 307–313. [Google Scholar]
- Hwang, D.; Wang, H.-L. Flap thickness as a predictor of root coverage: A systematic review. J. Periodontol. 2006, 77, 1625–1634. [Google Scholar] [CrossRef]
- Garces-McIntyre, T.; Carbonell, J.M.; Vallcorba, L.; Santos, A.; Valles, C.; Nart, J. Coronal advanced flap in combination with a connective tissue graft. Is the thickness of the flap a predictor for root coverage? A prospective clinical study. J. Clin. Periodontol. 2017, 44, 933–940. [Google Scholar] [CrossRef] [PubMed]
- Fan, Y.D.; Gong, Y.; Dong, J.C.; Shu, R. Clinical outcomes of modified lateral advanced flap combined with tunnel technique for the treatment of maxillary isolated soft tissue defect. J. Shanghai Jiaotong Univ. (Med. Sci.) 2020, 40, 139–144. [Google Scholar]
- Ioannou, A.L.; Kotsakis, G.A.; Kamintzi, G.I. Complete Coverage of a Class III (RT2) Gingival Recession with the Combination of a Free Subepithelial Connective Tissue Graft and a Laterally Positioned Flap. Clin. Adv. Periodontics 2016, 6, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Pilloni, A.; Dominici, F.; Rossi, R. Laterally moved, coronally advanced flap for the treatment of a single Stillman’s cleft. A 5-year follow-up. Eur. J. Esthet. Dent. 2013, 8, 390–396. [Google Scholar] [PubMed]
- Xie, Y.F.; Shu, R.; Qian, J.L.; Lin, Z.K.; Romanos, G.E. Esthetic management of mucogingival defects after excision of epulis using laterally positioned flaps. Cell Biochem. Biophys. 2015, 71, 1005–1010. [Google Scholar] [CrossRef]
- Chambrone, L.; Chambrone, L.A.; Tatakis, D.N.; Costa Hanemann, J.A.; Shibli, J.A.; Nevins, M. Wound Healing of the Laterally Positioned Flap: A Histomorphometric Assessment. Int. J. Periodontics Restor. Dent. 2015, 35, 785–792. [Google Scholar] [CrossRef]
- Zucchelli, G.; Marzadori, M.; Mele, M.; Stefanini, M.; Montebugnoli, L. Root coverage in molar teeth: A comparative controlled randomized clinical trial. J. Clin. Periodontol. 2012, 39, 1082–1088. [Google Scholar] [CrossRef]
- Chambrone, L.A.; Chambrone, L. Treatment of Miller Class I and II localized recession defects using laterally positioned flaps: A 24-month study. Am. J. Dent. 2009, 22, 339–344. [Google Scholar]







| Test Group (LPF + A − CTG) | Control Group (LPFF + NA − CTG) | Total | |
|---|---|---|---|
| Number enrolled patients | 13 (10 females, 3 males) | 21 (14 females, 7 males) | 34 24F 10M |
| Number surgical procedures | 23 | 24 | 47 |
| Number covered recessions | 55 | 50 | 105 |
| Number type of recession (Miller) | |||
| I | 23 | 29 | 52 |
| II | 32 | 21 | 53 |
| Number treated teeth per patient | |||
| Mean value ± SD | 4.23 ± 2.17 | 2.38 ± 1.60 | |
| Range | 2–10 | 1–6 | |
| Number localisation of recessions | |||
| Incisor | 18 | 27 | 45 |
| Canine | 16 | 11 | 27 |
| Premolar | 19 | 11 | 30 |
| Molar | 2 | 1 | 3 |
| Maxilla | 33 | 17 | 50 |
| Mandible | 22 | 33 | 55 |
| Mean Value in mm ± Standard Deviation | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Group/Time | CAL | PD | GRD | GRW | AG | BGT1 | BGT2 | BGT3 | |
| Test group (CAF + A − CTG) | Baseline | 4.64 ± 0.97 | 1.56 ± 0.55 | 3.05 ± 0.93 | 3.38 ± 0.78 | 0.93 ± 1.30 | 1.06 ± 0.24 | 1.04 ± 0.31 | 0.93 ± 0.23 |
| 6 months | 1.15 ± 0.78 *,** | 1.17 ± 0.45 * | 0.26 ± 0.47 * | 0.53 ± 0.94 * | 3.25 ± 1.12 *,** | 1.64 ± 0.24 *,** | 1.63 ± 0.22 *,** | 1.55 ± 0.22 *,** | |
| 12 months | 1.31 ± 0.92 *,** | 1.32 ± 0.44 * | 0.32 ± 0.62 *,** | 0.67 ± 1.14 * | 3.08 ± 1.14 *,** | 1.64 ± 0.23 *,** | 1.63 ± 0.21 *,** | 1.54 ± 0.21 *,** | |
| 24 months | 1.26 ± 0.87 *,** | 1.29 ± 0.45 * | 0.28 ± 0.55 *,** | 0.67 ± 1.14 * | 3.09 ± 1.10 *,** | 1.64 ± 0.23 *,** | 1.63 ± 0.24 *,** | 1.53 ± 0.24 *,** | |
| Control group (CAF + NA − CTG) | Baseline | 4.43 ± 1.36 | 1.36 ± 0.50 | 3.11 ± 1.10 | 3.11 ± 0.82 | 1.37 ± 1.37 | 1.05 ± 0.25 | 0.97 ± 0.28 | 0.95 ± 0.29 |
| 6 months | 1.66 ± 0.89 *,** | 1.21 ± 0.42 * | 0.49 ± 0.60 * | 1.05 ± 1.26 * | 2.28 ± 1.23 *,** | 1.37 ± 0.18 *,** | 1.31 ± 0.16 *,** | 1.35 ± 0.27 *,** | |
| 12 months | 1.84 ± 0.89 *,** | 1.24 ± 0.38 * | 0.63 ± 0.74 *,** | 1.17 ± 1.27 * | 2.38 ± 1.12 *,** | 1.36 ± 0.17 *,** | 1.31 ± 0.16 *,** | 1.35 ± 0.30 *,** | |
| 24 months | 1.67 ± 0.89 *,** | 1.27 ± 0.43 | 0.57 ± 0.67 *,** | 1.13 ± 1.27 * | 2.36 ± 1.20 *,** | 1.35 ± 0.18 *,** | 1.31 ± 0.16 *,** | 1.33 ± 0.29 *,** | |
| Percentage % ± Standard Deviation | |||||||
|---|---|---|---|---|---|---|---|
| Group/Time | ARC | %CAL | %BGT1 | %BGT2 | %BGT3 | CRC | |
| Test group (CAF + A − CTG) | 6 months | 92.0 ± 14.3 | 74.9 ± 16.1 ** | 60.3 ± 32.5 ** | 65.8 ± 36.2 ** | 78.0 ± 54.9 ** | 69.1 ** |
| 12 months | 90.6 ± 17.7 ** | 71.6 ± 18.6 ** | 60.5 ± 32.9 ** | 60.5 ± 32.9 ** | 76.4 ± 52.9 ** | 70.9 ** | |
| 24 months | 91.5 ± 16.4 ** | 72.6 ± 17.6 ** | 60.5 ± 33.4 ** | 64.4 ± 34.6 ** | 75.0 ± 54.3 ** | 70.9 ** | |
| Control group (CAF + NA − CTG) | 6 months | 85.7 ± 17.1 | 61.8 ± 15.9 ** | 31.4 ± 39.3 ** | 42.6 ± 30.7 ** | 48.1 ± 31.8 ** | 54.0 ** |
| 12 months | 81.7 ± 20.8 ** | 57.1 ± 17.8 ** | 30.2 ± 37.9 ** | 42.6 ± 30.7 ** | 47.6 ± 29.2 ** | 50.0 ** | |
| 24 months | 83.4 ± 19.0 ** | 61.5 ± 16.3 ** | 29.3 ± 36.9 ** | 42.6 ± 30.7 ** | 46.0 ± 30.0 ** | 52.0 ** | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bednarz, W.; Majer, J.; Pakuszyńska-Błaszczyk, J.; Dominiak, M.; Gedrange, T.; Zielińska-Pałasz, A. Laterally Positioned Flap Procedure with Augmented or Nonaugmented Palatal Connective Tissue Grafts in the Treatment of Multiple Adjacent Gingival Recessions: A Two-Year Follow-Up Study. Int. J. Environ. Res. Public Health 2022, 19, 12208. https://doi.org/10.3390/ijerph191912208
Bednarz W, Majer J, Pakuszyńska-Błaszczyk J, Dominiak M, Gedrange T, Zielińska-Pałasz A. Laterally Positioned Flap Procedure with Augmented or Nonaugmented Palatal Connective Tissue Grafts in the Treatment of Multiple Adjacent Gingival Recessions: A Two-Year Follow-Up Study. International Journal of Environmental Research and Public Health. 2022; 19(19):12208. https://doi.org/10.3390/ijerph191912208
Chicago/Turabian StyleBednarz, Wojciech, Jennifer Majer, Justyna Pakuszyńska-Błaszczyk, Marzena Dominiak, Tomasz Gedrange, and Agata Zielińska-Pałasz. 2022. "Laterally Positioned Flap Procedure with Augmented or Nonaugmented Palatal Connective Tissue Grafts in the Treatment of Multiple Adjacent Gingival Recessions: A Two-Year Follow-Up Study" International Journal of Environmental Research and Public Health 19, no. 19: 12208. https://doi.org/10.3390/ijerph191912208
APA StyleBednarz, W., Majer, J., Pakuszyńska-Błaszczyk, J., Dominiak, M., Gedrange, T., & Zielińska-Pałasz, A. (2022). Laterally Positioned Flap Procedure with Augmented or Nonaugmented Palatal Connective Tissue Grafts in the Treatment of Multiple Adjacent Gingival Recessions: A Two-Year Follow-Up Study. International Journal of Environmental Research and Public Health, 19(19), 12208. https://doi.org/10.3390/ijerph191912208






