Evidence of Autonomic Dysfunction in Patients with Relapsing-Remitting Multiple Sclerosis: Heart Rate Variability and Cardiovascular Parameters
Abstract
:1. Introduction
2. Experimental Section
2.1. Participants
2.2. Outcome Measures
2.3. Statistical Analysis
3. Results
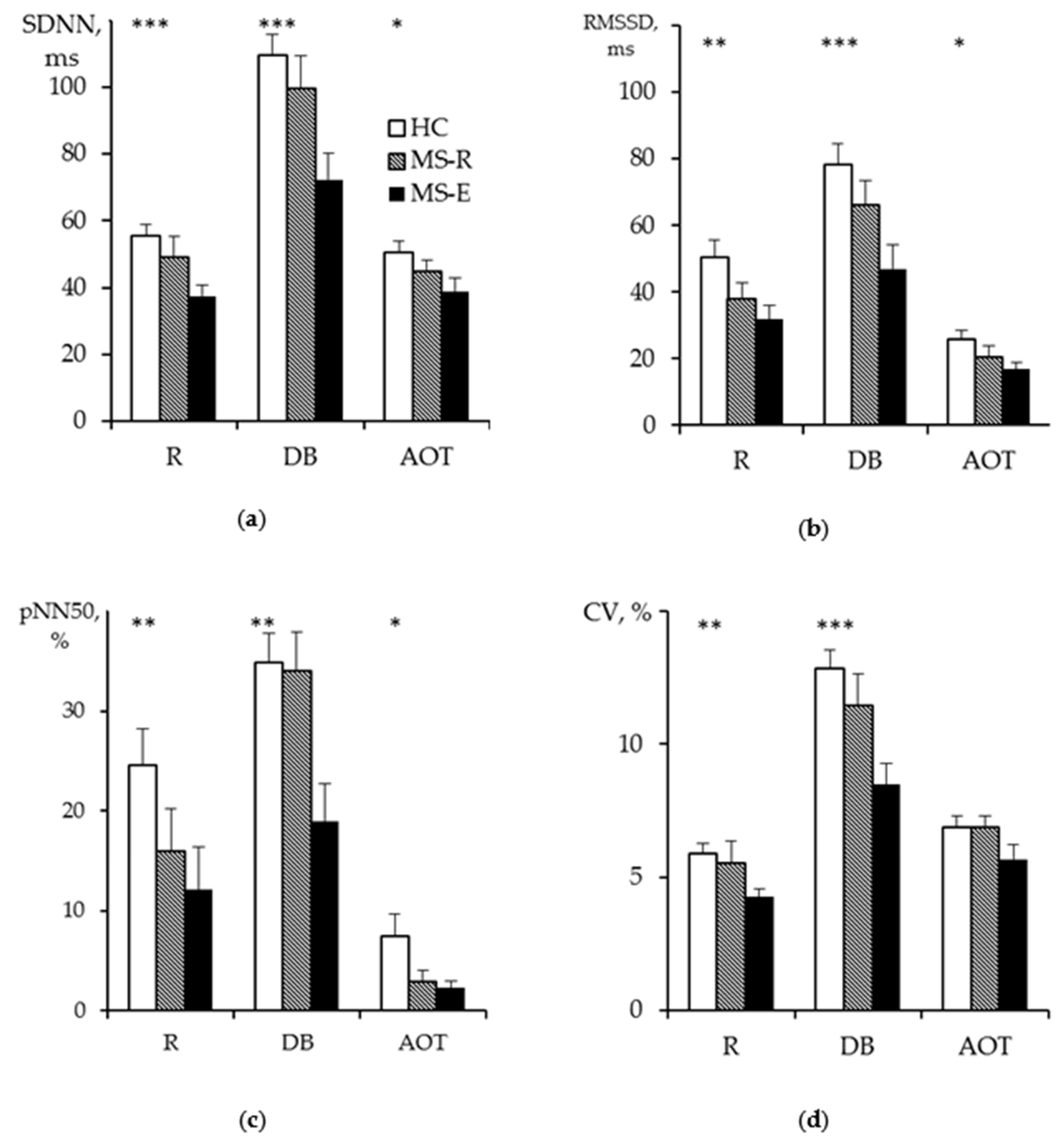
3.1. HRV Measurements at Rest
3.2. HRV Measurements at DB
3.3. HRV Measurements at AOT
3.4. HRV Measurements in MS of Different Activity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Crnošija, L.; Adamec, I.; Lovrić, M.; Junaković, A.; Skorić, M.K.; Lušić, I.; Habek, M. Autonomic dysfunction in clinically isolated syndrome suggestive of multiple sclerosis. Clin. Neurophysiol. 2016, 127, 864–869. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Findling, O.; Hauer, L.; Pezawas, T.; Rommer, P.S.; Struhal, W.; Sellner, J. Cardiac Autonomic Dysfunction in Multiple Sclerosis: A Systematic Review of Current Knowledge and Impact of Immunotherapies. J. Clin. Med. 2020, 9, 335. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Habek, M.; Crnošija, L.; Lovrić, M.; Junaković, A.; Skorić, M.K.; Adamec, I. Sympathetic cardiovascular and sudomotor functions are frequently affected in early multiple sclerosis. Clin. Auton. Res. 2016, 26, 385–393. [Google Scholar] [CrossRef] [PubMed]
- Pintér, A.; Cseh, D.; Sárközi, A.; Illigens, B.M.-W.; Siepmann, T. Autonomic Dysregulation in Multiple Sclerosis. Int. J. Mol. Sci. 2015, 16, 16920–16952. [Google Scholar] [CrossRef]
- Shmidt, T.E.; Yakhno, N.N. Multiple Sclerosis (Rassejannyj Skleroz); Medpress: Moscow, Russia, 2012; p. 272. (In Russian) [Google Scholar]
- Racosta, J.M.; Kimpinski, K.; Morrow, S.A.; Kremenchutzky, M. Autonomic dysfunction in multiple sclerosis. Auton. Neurosci. 2015, 193, 1–6. [Google Scholar] [CrossRef]
- Videira, G.; Castro, P.; Vieira, B.; Filipe, J.P.; Santos, R.; Azevedo, E.; Sá, M.J.; Abreu, P. Autonomic dysfunction in multiple sclerosis is better detected by heart rate variability and is not correlated with central autonomic network damage. J. Neurol. Sci. 2016, 367, 133–137. [Google Scholar] [CrossRef]
- Adamec, I.; Crnošija, L.; Junaković, A.; Skorić, M.K.; Habek, M. Progressive multiple sclerosis patients have a higher burden of autonomic dysfunction compared to relapsing remitting phenotype. Clin. Neurophysiol. 2018, 129, 1588–1594. [Google Scholar] [CrossRef] [Green Version]
- Kaplan, T.B.; Berkowitz, A.L.; Samuels, M.A. Cardiovascular Dysfunction in Multiple Sclerosis. Neurology 2015, 20, 108–114. [Google Scholar] [CrossRef]
- Adamec, I.; Habek, M. Autonomic dysfunction in multiple sclerosis. Clin. Neurol. Neurosurg. 2013, 115, S73–S78. [Google Scholar] [CrossRef] [Green Version]
- Mahovic, D.; Lakusic, N. Progressive Impairment of Autonomic Control of Heart Rate in Patients with Multiple Sclerosis. Arch. Med. Res. 2007, 38, 322–325. [Google Scholar] [CrossRef]
- Studer, V.; Rocchi, C.; Motta, C.; Lauretti, B.; Perugini, J.; Brambilla, L.; Pareja-Gutierrez, L.; Camera, G.; Barbieri, F.R.; Marfia, G.A.; et al. Heart rate variability is differentially altered in multiple sclerosis: Implications for acute, worsening and progressive disability. Mult. Scler. J.-Exp. Transl. Clin. 2017, 3. [Google Scholar] [CrossRef] [PubMed]
- Tombul, T.; Anlar, O.; Tuncer, M.; Huseyinoglu, N.; Eryonucu, B. Impaired heart rate variability as a marker of cardiovascular autonomic dysfunction in multiple sclerosis. Acta Neurol. Belg. 2011, 111, 116–120. [Google Scholar] [PubMed]
- Flachenecker, P.; Reiners, K.; Krauser, M.; Wolf, A.; Toyka, K.V. Autonomic dysfunction in multiple sclerosis is related to disease activity and progression of disability. Mult. Scler. J. 2001, 7, 327–334. [Google Scholar] [CrossRef] [PubMed]
- Kodounis, A.; Stamboulis, E.; Constantinidis, T.S.; Liolios, A. Measurement of autonomic dysregulation in multiple sclerosis. Acta Neurol. Scand. 2005, 112, 403–408. [Google Scholar] [CrossRef]
- Gerasimova-Meigal, L.I.; Sirenev, I.M. Holod-inducirovannaja reaktivnost’ u pacientov s rassejannym sklerozom. [(Cold-induced reactivity in patients with multiple sclerosis.) (In Russian with English abstract.)]. Patol. Fiziol. Eksp. Ter. 2017, 61, 56–62. [Google Scholar] [CrossRef]
- Gafson, A.; Giovannoni, G.; Hawkes, C.H. The diagnostic criteria for multiple sclerosis: From Charcot to McDonald. Mult. Scler. Relat. Disord. 2012, 1, 9–14. [Google Scholar] [CrossRef]
- Kurtzke, J.F. Rating neurologic impairment in multiple sclerosis: An expanded disability status scale (EDSS). Neurology 1983, 33, 1444. [Google Scholar] [CrossRef] [Green Version]
- Kurtzke, J.F. On the origin of EDSS. Mult. Scler. Relat. Disord. 2015, 4, 95–103. [Google Scholar] [CrossRef]
- Task Force of the European Society of Cardiology; The North American Society of Pacing and Electrophysiology. Heart rate variability: Standards of measurement, physiological interpretation and clinical use. Circulation 1996, 93, 1043–1065. [Google Scholar] [CrossRef] [Green Version]
- Shaffer, F.; Ginsberg, J.P. An Overview of Heart Rate Variability Metrics and Norms. Front. Public Health 2017, 5, 258. [Google Scholar] [CrossRef] [Green Version]
- Lebedeva, M.A.; Karganov, M.Y.; Kozlova, Y.A.; Gotovtceva, G.N.; Tumurov, D.A.; Gudkova, A.A.; Guekht, A.B. The role of autonomic dysfunction in pathogenesis of irritable bowel syndrome. Patol. Fiziol. Eksp. Ter. 2014, 58, 37–44. [Google Scholar]
- Huang, M.; Allen, D.R.; Keller, D.M.; Fadel, P.J.; Frohman, E.M.; Davis, S.L. Impaired carotid baroreflex control of arterial blood pressure in multiple sclerosis. J. Neurophysiol. 2016, 116, 81–87. [Google Scholar] [CrossRef] [Green Version]
- Sanya, E.; Tutaj, M.; Brown, C.M.; Goel, N.; Neundörfer, B.; Hilz, M.J. Abnormal heart rate and blood pressure responses to baroreflex stimulation in multiple sclerosis patients. Clin. Auton. Res. 2005, 15, 213–218. [Google Scholar] [CrossRef] [PubMed]
- Reynders, T.; Gidron, Y.; De Ville, J.; Bjerke, M.; Weets, I.; Van Remoortel, A.; Devolder, L.; D’Haeseleer, M.; De Keyser, J.; Nagels, G.; et al. Relation between Heart Rate Variability and Disease Course in Multiple Sclerosis. J. Clin. Med. 2019, 9, 3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rakhmatullin, A.R.; Bakhtiiarova, K.Z.; Magzhanov, R.V. Autonomic dysfunction in patients with multiple sclerosis. Zhurnal Nevrologii i Psikhiatrii Imeni SS Korsakova 2017, 117, 55. [Google Scholar] [CrossRef] [PubMed]
- Saari, A.; Tolonen, U.; Pääkkö, E.; Suominen, K.; Jauhiainen, J.; Sotaniemi, K.A.; Myllylä, V.V. Sudomotor dysfunction in patients with optic neuritis. Clin. Auton. Res. 2010, 20, 199–204. [Google Scholar] [CrossRef]


| System | Number of MS Patients |
|---|---|
| Pyramidal | 63% |
| Cerebellar | 59% |
| Brain stem | 44% |
| Sensory | 22% |
| Bowel and Bladder | 19% |
| Visual | 22% |
| Cerebral | 9% |
| Other | 6% |
| Parameter | MS:M (n = 17) | MS:W (n = 11) | HC:M (n = 15) | HC:W (n = 11) |
|---|---|---|---|---|
| Body Mass, kg | 75.7 ± 9.9 | 59.6 ± 17.4 | 77.8 ± 9.4 | 57.6 ± 4.4 |
| Height, m | 1.78 ± 0.04 | 1.68 ± 0.10 | 1.78 ± 0.07 | 1.60 ± 0.06 |
| BMI | 24.0 ± 3.1 | 21.2 ± 6.2 | 24.5 ± 3.3 | 22.9 ± 2.9 |
| Metabolic rate, kcal | 1816 ± 177 | 1361 ± 177 | 1817 ± 2 | 1328 ± 74.8 |
| Test | Parameter | HC | MS | Significance 1 |
|---|---|---|---|---|
| Rest | HR, per minute | 64 (61; 68) | 70 (62; 76) | p < 0.05 |
| R-R min, ms | 785 (700; 818) | 750 (669; 815) | n.s. | |
| R-R max, ms | 1103 (1046; 1173) | 1043 (906; 1105) | p < 0.05 | |
| RRNN, ms | 939 (880; 987) | 860 (794; 968) | p < 0.05 | |
| SDNN, ms | 51 (42; 67) | 39 (30; 49) | p < 0.01 | |
| RMSSD, ms | 43 (35; 60) | 29 (21; 47) | p < 0.01 | |
| pNN50, % | 22.7 (10.3; 35.4) | 5.6 (1.0;27.9) | p < 0.01 | |
| CV, % | 5.55 (4.38; 7.38) | 4.44 (3.67; 5.36) | p < 0.01 | |
| TP, ms2 | 2529 (1766; 4598) | 1551 (1047; 2527) | p < 0.01 | |
| VLF, ms2 | 832 (437; 1188) | 544 (377; 870) | n.s. | |
| LF, ms2 | 755 (419; 1713) | 577 (310; 702) | p < 0.05 | |
| HF, ms2 | 894 (446; 1587) | 407 (232; 998) | p < 0.05 | |
| LF/HF | 1.00 (0.43; 1.93) | 1.07 (0.55; 1.70) | n.s. | |
| % VLF | 32.9 (19.5; 41.3) | 37.7 (27.6; 52.1) | n.s. | |
| % LF | 32.2 (17.3; 43.5) | 27.9 (23.1; 36.8) | n.s. | |
| % HF | 33.6 (18.7; 45.6) | 25.9 (18.5; 41.3) | n.s. | |
| LF, n.u. | 49.95 (29.90; 65.60) | 51.65 (35.33; 62.88) | n.s. | |
| HF, n.u. | 50.05 (34.40; 70.10) | 48.35 (37.13; 64.68) | n.s. | |
| Cra | 1.38 (1.32; 1.63) | 1.32 (1.24; 1.38) | p < 0.05 | |
| DB | HR, per minute | 69 (64; 76) | 71 (65; 77) | n.s. |
| R-R min, ms | 670 (618; 738) | 688 (638; 768) | n.s. | |
| R-R max, ms | 1133 (1021; 1278) | 1055 (901; 1196) | p < 0.05 | |
| RRNN, ms | 853 (781; 934) | 852 (781; 918) | n.s. | |
| SDNN, ms | 107 (81; 133) | 78 (51; 114) | p < 0.01 | |
| RMSSD, ms | 72 (57; 100) | 48 (27; 73) | p < 0.01 | |
| pNN50, % | 34.6 (23.9; 46.1) | 25.8 (6.5; 40.4) | p < 0.05 | |
| CV, % | 12.70 (9.53; 16.33) | 9.34 (6.72; 12.33) | p < 0.01 | |
| Cra | 1.65 (1.47; 1.87) | 1.45 (1.32; 1.66) | p < 0.01 | |
| AOT | HR, per minute | 83 (79; 86) | 94 (84; 99) | p < 0.05 |
| R-R min, ms | 613 (579; 626) | 550 (518; 595) | p < 0.01 | |
| R-R max, ms | 855 (804; 955) | 803 (716; 865) | p < 0.05 | |
| RRNN, ms | 719 (685; 771) | 635 (608; 716) | p < 0.01 | |
| SDNN, ms | 47 (37; 63) | 42 (29; 51) | n.s. | |
| RMSSD, ms | 21 (17; 33) | 18 (12; 23) | p < 0.05 | |
| pNN50, % | 2.8 (0.8; 12.8) | 1.8 (0.1; 3.4) | p < 0.05 | |
| CV, % | 6.45 (5.44; 8.03) | 5.99 (4.53; 7.74) | n.s. | |
| TP, ms2 | 3188 (1907; 5013) | 2309 (1217; 3903) | n.s. | |
| VLF, ms2 | 1105 (717; 2046) | 989 (749; 1655) | n.s. | |
| LF, ms2 | 1131 (836; 2414) | 931 (409; 2074) | n.s. | |
| HF, ms2 | 313 (145; 656) | 178 (93; 289) | p < 0.05 | |
| LF/HF | 4.26 (2.69; 7.66) | 6.60 (3.81; 9.34) | n.s. | |
| % VLF | 36.1 (27.1;49.4) | 50.9 (38.4; 63.0) | p < 0.01 | |
| % LF | 47.8 (36.8; 64.4) | 41.3 (26.4; 55.1) | n.s. | |
| % HF | 9.7 (7.4; 15.3) | 6.3 (4.2; 9.9) | p < 0.01 | |
| LF, n.u. | 80.95 (72.88; 88.43) | 86.80 (79.20; 90.35) | n.s. | |
| HF, n.u. | 19.05 (11.58; 27.13) | 13.20 (9.68; 20.80) | n.s. | |
| Cra | 1.42 (1.32; 1.53) | 1.43 (1.26; 1.52) | n.s. | |
| K30:15 | 1.35 (1.23; 1.53) | 1.24 (1.19; 1.32) | p < 0.01 |
| Test | Parameter | HC | MS |
|---|---|---|---|
| Rest | SBP, mm Hg | 114 ± 9 | 112 ± 9 |
| DBP, mm Hg | 67 ± 7 | 68 ± 5 | |
| HR, per minute | 64 ± 9 | 69 ± 9 * | |
| AOT | SBP, mm Hg | 122 ± 13 | 118 ± 12 |
| DBP, mm Hg | 83 ± 10 | 80 ± 8 | |
| HR, per minute | 83 ± 9 | 92 ± 13 ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gerasimova-Meigal, L.; Sirenev, I.; Meigal, A. Evidence of Autonomic Dysfunction in Patients with Relapsing-Remitting Multiple Sclerosis: Heart Rate Variability and Cardiovascular Parameters. Pathophysiology 2021, 28, 10-19. https://doi.org/10.3390/pathophysiology28010002
Gerasimova-Meigal L, Sirenev I, Meigal A. Evidence of Autonomic Dysfunction in Patients with Relapsing-Remitting Multiple Sclerosis: Heart Rate Variability and Cardiovascular Parameters. Pathophysiology. 2021; 28(1):10-19. https://doi.org/10.3390/pathophysiology28010002
Chicago/Turabian StyleGerasimova-Meigal, Liudmila, Ilya Sirenev, and Alexander Meigal. 2021. "Evidence of Autonomic Dysfunction in Patients with Relapsing-Remitting Multiple Sclerosis: Heart Rate Variability and Cardiovascular Parameters" Pathophysiology 28, no. 1: 10-19. https://doi.org/10.3390/pathophysiology28010002
APA StyleGerasimova-Meigal, L., Sirenev, I., & Meigal, A. (2021). Evidence of Autonomic Dysfunction in Patients with Relapsing-Remitting Multiple Sclerosis: Heart Rate Variability and Cardiovascular Parameters. Pathophysiology, 28(1), 10-19. https://doi.org/10.3390/pathophysiology28010002







