The A, B and C’s of Silicone Breast Implants: Anaplastic Large Cell Lymphoma, Biofilm and Capsular Contracture
Abstract
:1. Introduction
2. Breast Implants
3. Capsular Contracture
4. Aetiopathogenesis of Capsular Contracture (CC)
5. Breast Implant Associated Anaplastic Large Cell Lymphoma
Author Contributions
Funding
Conflicts of Interest
References
- ASPS. ASPS Plastic Surgery Statistics Report. Available online: www.plasticsurgery.org (accessed on 30 June 2018).
- Cronin, T.D.; Gerow, F.J. Augmentation mammaplasty: A new “natural feel” prosthesis. In Proceedings of the Transactions of the Third International Congress of Plastic and Reconstructive Surgery, Washington, DC, USA, 13–18 October 1963; Excerpta Medica: Amsterdam, The Netherlands, 1964; pp. 41–49. [Google Scholar]
- Namnoum, J.D.; Largent, J.; Kaplan, H.M.; Oefelein, M.G.; Brown, M.H. Primary breast augmentation clinical trial outcomes stratified by surgical incision, anatomical placement and implant device type. J. Plast. Reconstr. Aesthet. Surg. 2013, 66, 1165–1172. [Google Scholar] [CrossRef] [PubMed]
- Headon, H.; Kasem, A.; Mokbel, K. Capsular contracture after breast augmentation: An update for clinical practice. Archiv. Plast. Surg. 2015, 42, 532–543. [Google Scholar] [CrossRef] [PubMed]
- O’Shaughnessy, K. Evolution and update on current devices for prosthetic breast reconstruction. Gland Surg. 2015, 4, 97–110. [Google Scholar] [PubMed]
- Henderson, P.W.; Nash, D.; Laskowski, M.; Grant, R.T. Objective Comparison of Commercially Available Breast Implant Devices. Aesthet. Plast. Surg. 2015, 39, 724–732. [Google Scholar] [CrossRef] [PubMed]
- Clubb, F.J.; Ciapper, D.L.; Deferrari, D.A.; Hu, S.; Stare, W.J., Jr.; Capik, P.P.; Armstrong, J.; McGEE, M.G.; Bilings, L.A.; Fuqua, J.M. Surface texturing and coating of biomaterial implants: Effects on tissue integration and fibrosis. ASAIO J. 1999, 45, 281–287. [Google Scholar] [CrossRef] [PubMed]
- Dalby, M.J.; Yarwood, S.J.; Riehle, M.O.; Johnstone, H.J.; Affrossman, S.; Curtis, A.S. Increasing fibroblast response to materials using nanotopography: Morphological and genetic measurements of cell response to 13-nm-high polymer demixed islands. Exp. Cell Res. 2002, 276, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Jones, P.; Mempin, M.; Hu, H.; Chowdhury, D.; Foley, M.; Cooter, R.; Adams, W.P., Jr.; Vickery, K.; Deva, A.K. The Functional Influence of Breast Implant Outer Shell Morphology on Bacterial Attachment and Growth. Plast. Reconstr. Surg. 2018, 142, 837–849. [Google Scholar] [CrossRef] [PubMed]
- Ashley, F.L. Further studies on the natural-y breast prosthesis. Plast. Reconstr. Surg. 1972, 49, 414–419. [Google Scholar] [CrossRef] [PubMed]
- Sinclair, T.M.; Kerrigan, C.L.; Buntic, R. Biodegradation of the polyurethane foam covering of breast implants. Plast. Reconstr. Surg 1993, 92, 1003–1013; discussion 1014. [Google Scholar] [CrossRef] [PubMed]
- Chan, S.C.; Birdsell, D.C.; Gradeen, C.Y. Detection of toluenediamines in the urine of a patient with polyurethane-covered breast implants. Clin. Chem. 1991, 37, 756–758. [Google Scholar] [PubMed]
- Barr, S.; Bayat, A. Breast surgery review article: Breast implant surface development: Perspectives on development and manufacture. Aesthet. Surg. J. 2011, 31, 56–67. [Google Scholar] [CrossRef] [PubMed]
- Barone, F.E.; Perry, L.; Keller, T.; Maxwell, G.P. The biomechanical and histopathologic effects of surface texturing with silicone and polyurethane in tissue implantation and expansion. Plast. Reconstr. Surg. 1992, 90, 77–86. [Google Scholar] [CrossRef] [PubMed]
- Danino, A.M.; Basmacioglu, P.; Saito, S.; Rocher, F.; Blanchet-Bardon, C.; Revol, M.; Servant, J.-M. Comparison of the capsular response to the Biocell RTV and Mentor 1600 Siltex breast implant surface texturing: A scanning electron microscopic study. Plast. Reconstr. Surg. 2001, 108, 2047–2052. [Google Scholar] [CrossRef] [PubMed]
- Maxwell, G.P.; Hammond, D.C. Breast implants: Smooth versus textured. Adv. Plast. Reconstr. Surg. 1993, 9, 209–220. [Google Scholar]
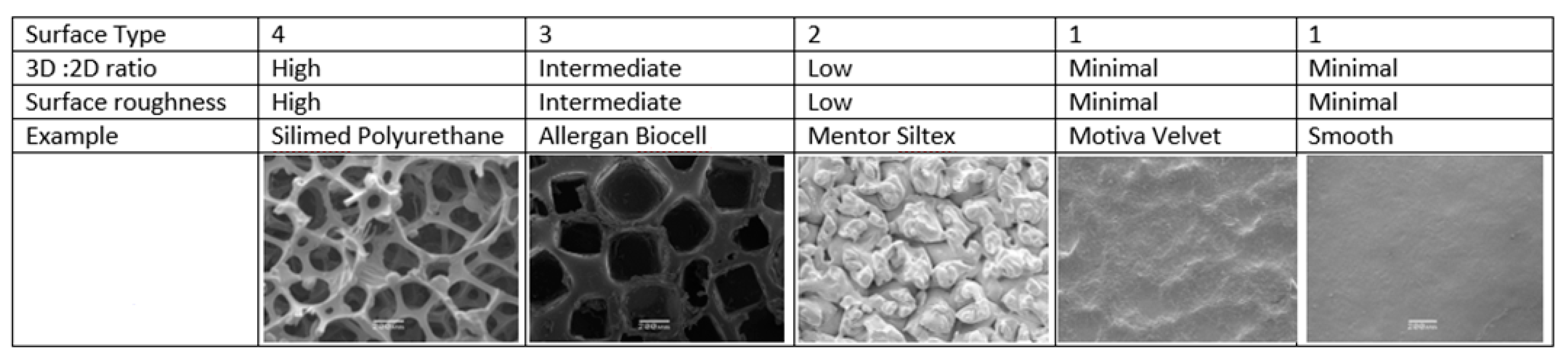
- Barr, S.; Hill, E.W.; Bayat, A. Functional biocompatibility testing of silicone breast implants and a novel classification system based on surface roughness. J. Mech. Behav. Biomed. Mater. 2017, 75, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Sforza, M.; Zaccheddu, R.; Alleruzzo, A.; Seno, A.; Mileto, D.; Paganelli, A.; Sulaiman, H.; Payne, M.; Maurovich-Horvat, L. Preliminary 3-Year Evaluation of Experience with SilkSurface and VelvetSurface Motiva Silicone Breast Implants: A Single-Center Experience with 5813 Consecutive Breast Augmentation Cases. Aesthet. Surg. J. 2018, 38, S62–S73. [Google Scholar] [CrossRef] [PubMed]
- Deva, A.K.; Adams, W.P.; Vickery, K. The role of bacterial biofilms in device-associated infection. Plast. Reconstr. Surg. 2013, 132, 1319–1328. [Google Scholar] [CrossRef] [PubMed]
- FDA. Breast Implant- Associated Anaplastic Large Cell Lymphoma (BIA-ALCL); FDA: Silver Spring, MD, USA, 2018.
- Hopper, I.; Parker, E.; Pelligrini, B.; Mulvany, C.; Pase, M.; Ahem, S.; Earnest, A.; McNeil, J. The Australian Breast Device Registry 2016 Report; Monash University: Melbourne, Australia, 2018. [Google Scholar]
- Bengtson, B.P.; Van Natta, B.W.; Murphy, D.K.; Slicton, A.; Maxwell, G.P.; Style 410 U.S. Core Clinical Study Group. Style 410 highly cohesive silicone breast implant core study results at 3 years. Plast. Reconstr. Surg. 2007, 120, 40S–48S. [Google Scholar] [CrossRef] [PubMed]
- Spear, S.L.; Murphy, D.K. Natrelle round silicone breast implants: Core study results at 10 years. Plast. Reconstr. Surg. 2014, 133, 1354–1361. [Google Scholar] [CrossRef] [PubMed]
- Adams, W.P., Jr.; Rios, J.L.; Smith, S.J. Enhancing patient outcomes in aesthetic and reconstructive breast surgery using triple antibiotic breast irrigation: Six-year prospective clinical study. Plast. Reconstr. Surg. 2006, 117, 30–36. [Google Scholar] [CrossRef] [PubMed]
- Pajkos, A.; Deva, A.K.; Vickery, K.; Cope, C.; Chang, L.; Cossart, Y.E. Detection of subclinical infection in significant breast implant capsules. Plast. Reconstr. Surg. 2003, 111, 1605–1611. [Google Scholar] [CrossRef] [PubMed]
- Ersek, R.A. Rate and incidence of capsular contracture: A comparison of smooth and textured silicone double-lumen breast prostheses. Plast. Reconstr. Surg. 1991, 87, 879–884. [Google Scholar] [CrossRef] [PubMed]
- Ersek, R.A.; Salisbury, A.V. Textured surface, nonsili- cone gel breast implants: Four years’ clinical outcome. Plast. Reconstr. Surg. 1997, 100, 1729–1739. [Google Scholar] [CrossRef] [PubMed]
- Handel, N.; Jensen, J.A.; Black, Q.; Waisman, J.R.; Silverstein, M.J. The fate of breast implants: A critical analysis of complications and outcomes. Plast. Reconstr. Surg. 1995, 96, 1521–1533. [Google Scholar] [CrossRef] [PubMed]
- Barnsley, G.P.; Sigurdson, L.J.; Barnsley, S.E. Textured surface breast implants in the prevention of capsular contracture among breast augmentation patients: A meta-analysis of randomized controlled trials. Plast. Reconstr. Surg. 2006, 117, 2182–2190. [Google Scholar] [CrossRef] [PubMed]
- Araco, A.; Caruso, R.; Araco, F.; Overton, J.; Gravante, G. Capsular contractures: A systematic review. Plast. Reconstr. Surg. 2009, 124, 1808–1819. [Google Scholar] [CrossRef] [PubMed]
- Spear, S.L.; Baker, J.L., Jr. Classification of capsular contracture after prosthetic breast reconstruction. Plast. Reconstr. Surg. 1995, 96, 1119–1123; discussion 1124. [Google Scholar] [CrossRef] [PubMed]
- Malata, C.M.; Varma, S.; Scott, M.; Liston, J.C.; Sharpe, D.T. Silicone breast implant rupture: Common/serious complication? Med. Prog. Technol. 1994, 20, 251–260. [Google Scholar] [PubMed]
- Maxwell, G.P.; Gabriel, A. The evolution of breast implants. Clin. Plast. Surg. 2009, 36, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Chang, L.; Caldwell, E.; Reading, G.; Wray, R.C., Jr. A comparison of conventional and low-bleed implants in augmentation mammaplasty. Plast. Reconstr. Surg. 1992, 89, 79–82. [Google Scholar] [CrossRef] [PubMed]
- Bogetti, P.; Boltri, M.; Balocco, P.; Spagnoli, G. Augmentation mammaplasty with a new cohesive gel prosthesis. Aesthet. Plast. Surg. 2000, 24, 440–444. [Google Scholar] [CrossRef] [PubMed]
- Heden, P.; Jernbeck, J.; Hober, M. Breast augmentation with anatomical cohesive gel implants: The world’s largest current experience. Clin. Plast. Surg. 2001, 28, 531–552. [Google Scholar] [PubMed]
- Drever, J. Cohesive gel implants for breast augmentation. Aesthet. Surg. J. 2003, 23, 405–409. [Google Scholar] [CrossRef] [Green Version]
- Brown, M.H.; Shenker, R.; Silver, S.A. Cohesive silicone gel breast implants in aesthetic and reconstructive breast surgery. Plast. Reconstr. Surg. 2005, 116, 768–779. [Google Scholar] [CrossRef] [PubMed]
- Henriksen, T.F.; Fryzek, J.P.; Holmich, L.R.; McLaughlin, J.K.; Krag, C.; Karlsen, R.; Kjøller, K.; Olsen, J.H.; Friis, S. Reconstructive breast implantation after mastectomy for breast cancer: Clinical outcomes in a nationwide prospective cohort study. Arch. Surg. 2005, 140, 1152–1159. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.-H.; Samuel, M.; Tan, B.-K.; Song, C. Capsular contracture in subglandular breast augmentation with textured versus smooth breast implants: A systematic review. Plast. Reconstr. Surg. 2006, 118, 1224–1236. [Google Scholar] [CrossRef] [PubMed]
- Coleman, D.J.; Foo, I.T.; Sharpe, D.T. Textured or smooth implants for breast augmentation? A prospective controlled trial. Br. J. Plast. Surg. 1991, 44, 444–448. [Google Scholar] [CrossRef]
- Hakelius, L.; Ohlsen, L. Tendency to capsular contracture around smooth and textured gel-filled silicone mammary implants: A five-year follow-up. Plast. Reconstr. Surg. 1997, 100, 1566–1569. [Google Scholar] [CrossRef] [PubMed]
- Burkhardt, B.R.; Demas, C.P. The effect of Siltex texturing and povidone-iodine irrigation on capsular contracture around saline inflatable breast implants. Plast. Reconstr. Surg. 1994, 93, 123–128; discussion 129–130. [Google Scholar] [CrossRef] [PubMed]
- Burkhardt, B.R.; Eades, E. The effect of Biocell texturing and povidone-iodine irrigation on capsular contracture around saline-inflatable breast implants. Plast. Reconstr. Surg. 1995, 96, 1317–1325. [Google Scholar] [CrossRef] [PubMed]
- Asplund, O.; Gylbert, L.; Jurell, G.; Ward, C. Textured or smooth implants for submuscular breast augmentation: A controlled study. Plast. Reconstr. Surg. 1996, 97, 1200–1206. [Google Scholar] [CrossRef] [PubMed]
- Malata, C.M.; Feldberg, L.; Coleman, D.J.; Foo, I.T.; Sharpe, D.T. Textured or smooth implants for breast augmentation? Three year follow-up of a prospective randomised controlled trial. Br. J. Plast. Surg. 1997, 50, 99–105. [Google Scholar] [CrossRef]
- Poeppl, N.; Schreml, S.; Lichtenegger, F.; Lenich, A.; Eisenmann-Klein, M.; Prantl, L. Does the surface structure of implants have an impact on the formation of a capsular contracture? Aesthet. Plast. Surg. 2007, 31, 133–139. [Google Scholar] [CrossRef] [PubMed]
- Stevens, W.G.; Nahabedian, M.Y.; Calobrace, M.B.; Harrington, J.L.; Capizzi, P.J.; Cohen, R.; d’Incelli, R.C.; Beckstrand, M. Risk factor analysis for capsular contracture: A 5-year Sientra study analysis using round, smooth, and textured implants for breast augmentation. Plast. Reconstr. Surg. 2013, 132, 1115–1123. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Zhou, L.; Pan, F.; Gao, Y.; Yuan, X.; Fan, D. Comparison of the postoperative incidence rate of capsular contracture among different breast implants: A cumulative meta-analysis. PLoS ONE 2015, 10, e0116071. [Google Scholar] [CrossRef] [PubMed]
- Burkhardt, B.R.; Fried, M.; Schnur, P.L.; Tofield, J.J. Capsules, infection, and intraluminal antibiotics. Plast. Reconstr. Surg. 1981, 68, 43–47. [Google Scholar] [CrossRef] [PubMed]
- Deva, A.K.; Chang, L.C. Bacterial biofilms: A cause for accelerated capsular contracture? Aesthet. Surg. J. 1999, 19, 130–133. [Google Scholar] [CrossRef]
- Rieger, U.; Mesina, J.; Kalbermatten, D.; Haug, M.; Frey, H.; Pico, R.; Frei, R.; Pierer, G.; Lüscher, N.; Trampuz, A. Bacterial biofilms and capsular contracture in patients with breast implants. Br. J. Surg. 2013, 100, 768–774. [Google Scholar] [CrossRef] [PubMed]
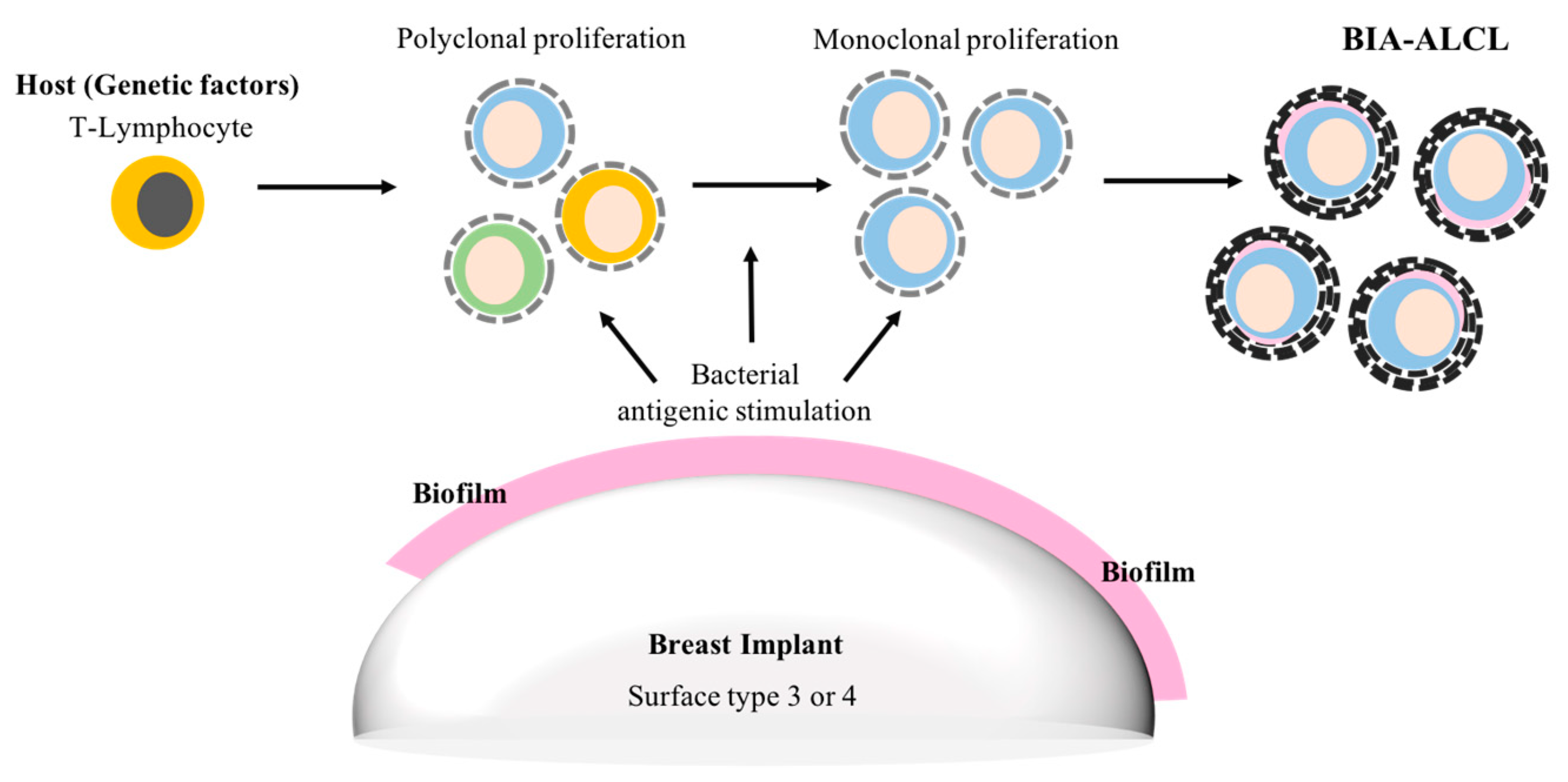
- Hu, H.; Jacombs, A.; Vickery, K.; Merten, S.L.; Pennington, D.G.; Deva, A.K. Chronic biofilm infection in breast implants is associated with an increased T-cell lymphocytic infiltrate: Implications for breast implant-associated lymphoma. Plast. Reconstr. Surg. 2015, 135, 319–329. [Google Scholar] [CrossRef] [PubMed]
- Fux, C.A.; Stoodley, P.; Hall-Stoodley, L.; Costerton, J.W. Bacterial biofilms: A diagnostic and therapeutic challenge. Expert Rev. Antiinfect. Ther. 2003, 1, 667–683. [Google Scholar] [CrossRef]
- Prantl, L.; Pöppl, N.; Horvat, N.; Heine, N.; Eisenmann-Klein, M. Serologic and histologic findings in patients with capsular contracture after breast augmentation with smooth silicone gel implants: Is serum hyaluronan a potential predictor? Aesthet. Plast. Surg. 2005, 29, 510–518. [Google Scholar] [CrossRef] [PubMed]
- Shah, Z.; Lehman, J.A., Jr.; Tan, J. Does Infection Play a Role in Breast Capsular Contracture? Plast. Reconstr. Surg. 1981, 68, 34–38. [Google Scholar] [CrossRef] [PubMed]
- Virden, C.P.; Dobke, M.K.; Stein, P.; Parsons, C.L.; Frank, D.H. Subclinical infection of the silicone breast implant surface as a possible cause of capsular contracture. Aesthet. Plast. Surg. 1992, 16, 173–179. [Google Scholar] [CrossRef]
- Netscher, D.T. Subclinical infection in breast capsules. Plast. Reconstr. Surg. 2004, 114, 818–820. [Google Scholar] [CrossRef] [PubMed]
- Del Pozo, J.L.; Tran, N.V.; Petty, P.M.; Johnson, C.H.; Walsh, M.F.; Bite, U.; Clay, R.P.; Mandrekar, J.N.; Piper, K.E.; Steckelberg, J.M. Pilot study of association of bacteria on breast implants with capsular contracture. J. Clin. Microbiol. 2009, 47, 1333–1337. [Google Scholar] [CrossRef] [PubMed]
- Marques, M.; Brown, S.A.; Cordeiro, N.D.; Rodrigues-Pereira, P.; Cobrado, M.L.; Morales-Helguera, A.; Queirós, L.; Luís, A.; Freitas, R.; Gonçalves-Rodrigues, A. Effects of coagulase-negative staphylococci and fibrin on breast capsule formation in a rabbit model. Aesthet. Surg. J. 2011, 31, 420–428. [Google Scholar] [CrossRef] [PubMed]
- Tamboto, H.; Vickery, K.; Deva, A.K. Subclinical (biofilm) infection causes capsular contracture in a porcine model following augmentation mammaplasty. Plast. Reconstr. Surg. 2010, 126, 835–842. [Google Scholar] [CrossRef] [PubMed]
- Darouiche, R.O.; Meade, R.; Mansouri, M.D.; Netscher, D.T. In vivo efficacy of antimicrobe-impregnated saline-filled silicone implants. Plast. Reconstr. Surg. 2002, 109, 1352–1357. [Google Scholar] [CrossRef] [PubMed]
- Jacombs, A.; Allan, J.; Hu, H.; Valente, P.M.; Wessels, W.L.F.; Deva, A.K.; Vickery, K. Prevention of Biofilm-Induced Capsular Contracture with Antibiotic-Impregnated Mesh in a Porcine Model. Aesthet. Surg. J. 2012, 32, 886–891. [Google Scholar] [CrossRef] [PubMed]
- Adams, W.P., Jr.; Conner, W.C.H.; Barton, F.E., Jr.; Rohrich, R.J. Optimizing breast-pocket irrigation: The post-Betadine era. Plast. Reconstr. Surg. 2001, 107, 1596–1601. [Google Scholar] [CrossRef] [PubMed]
- Blount, A.L.; Martin, M.D.; Lineberry, K.D.; Kettaneh, N.; Alfonso, D.R. Capsular contracture rate in a low-risk population after primary augmentation mammaplasty. Aesthet. Surg. J. 2013, 33, 516–521. [Google Scholar] [CrossRef] [PubMed]
- Giordano, S.; Peltoniemi, H.; Lilius, P.; Salmi, A. Povidone-iodine combined with antibiotic topical irrigation to reduce capsular contracture in cosmetic breast augmentation: A comparative study. Aesthet. Surg. J. 2013, 33, 675–680. [Google Scholar] [CrossRef] [PubMed]
- FDA. Anaplastic Large Cell Lymphoma (ALCL) in Women with Breast Implants: Preliminary FDA Findings and Analyses; Center for Devices and Radiological Health: Silver Spring, MD, USA, 2011.
- Stein, H.; Foss, H.-D.; Dürkop, H.; Marafioti, T.; Delsol, G.; Pulford, K.; Pileri, S.; Falini, B. CD30+ anaplastic large cell lymphoma: A review of its histopathologic, genetic, and clinical features. Blood 2000, 96, 3681–3695. [Google Scholar] [PubMed]
- Knight, R.; Loch-Wilkinson, A.-M.; Wessels, W.; Papadopoulos, T.; Magnusson, M.; Lofts, J.; Connell, T.; Hopper, I.; Beath, K.; Lade, S. Epidemiology and risk factors for Breast implant-associated anaplastic large cell lymphoma (BIA-ALCL) in Australia & New Zealand. Plast. Reconstr. Surg. 2016, 4, 94–95. [Google Scholar]
- Loch-Wilkinson, A.; Beath, K.J.; Knight, R.J.W.; Wessels, W.L.F.; Magnusson, M.; Papadopoulos, T.; Connell, T.; Lofts, J.; Locke, M.; Hopper, I.; et al. Breast Implant-Associated Anaplastic Large Cell Lymphoma in Australia and New Zealand: High-Surface-Area Textured Implants Are Associated with Increased Risk. Plast. Reconstr. Surg. 2017, 140, 645–654. [Google Scholar] [CrossRef] [PubMed]
- Doren, E.L.; Miranda, R.N.; Selber, J.C.; Garvey, P.B.; Liu, J.; Medeiros, L.J.; Butler, C.E.; Clemens, M.W. US Epidemiology of Breast Implant–Associated Anaplastic Large Cell Lymphoma. Plast. Reconstr. Surg. 2017, 139, 1042–1050. [Google Scholar] [CrossRef] [PubMed]
- TGA. Breast Implants and Anaplastic Large Cell Lymphoma. Update—Additional Confirmed Cases of Anaplastic Large Cell Lymphoma; TGA: Symonston, Australia, 2018.
- Bishara, M.R.; Ross, C.; Sur, M. Primary anaplastic large cell lymphoma of the breast arising in reconstruction mammoplasty capsule of saline filled breast implant after radical mastectomy for breast cancer: An unusual case presentation. Diagn. Pathol. 2009, 4, 11. [Google Scholar] [CrossRef] [PubMed]
- Thompson, P.A.; Lade, S.; Webster, H.; Ryan, G.; Prince, H.M. Effusion-associated anaplastic large cell lymphoma of the breast: Time for it to be defined as a distinct clinico-pathological entity. Haematologica 2010, 95, 1977–1979. [Google Scholar] [CrossRef] [PubMed]
- Rupani, A.; Frame, J.D.; Kamel, D. Lymphomas Associated with Breast Implants: A Review of the Literature. Aesthet. Surg. J. 2015, 35, 533–544. [Google Scholar] [CrossRef] [PubMed]
- Clemens, M.W.; Brody, G.S.; Mahabir, R.C.; Miranda, R.N. How to Diagnose and Treat Breast Implant-Associated Anaplastic Large Cell Lymphoma. Plast. Reconstr. Surg. 2018, 141, 586e–599e. [Google Scholar] [CrossRef] [PubMed]
- Roden, A.C.; Macon, W.R.; Keeney, G.L.; Myers, J.L.; Feldman, A.L.; Dogan, A. Seroma-associated primary anaplastic large-cell lymphoma adjacent to breast implants: An indolent T-cell lymphoproliferative disorder. Mod. Pathol. 2008, 21, 455–463. [Google Scholar] [CrossRef] [PubMed]
- Swerdlow, S.H. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues; WHO Classification of Tumours; WHO: Geneva, Switzerland, 2008; Volume 22008, p. 439. [Google Scholar]
- Jewell, M.; Spear, S.L.; Largent, J.; Oefelein, M.G.; Adams, W.P., Jr. Anaplastic large T-cell lymphoma and breast implants: A review of the literature. Plast. Reconstr. Surg. 2011, 128, 651–661. [Google Scholar] [CrossRef] [PubMed]
- Lechner, M.G.; Lade, S.; Liebertz, D.J.; Prince, H.M.; Brody, G.S.; Webster, H.R.; Epstein, A.L. Breast implant-associated, ALK-negative, T-cell, anaplastic, large-cell lymphoma: Establishment and characterization of a model cell line (TLBR-1) for this newly emerging clinical entity. Cancer 2011, 117, 1478–1489. [Google Scholar] [CrossRef] [PubMed]
- Kadin, M.E.; Deva, A.; Xu, H.; Morgan, J.; Khare, P.; MacLeod, R.A.; Van Natta, B.W.; Adams, W.P., Jr.; Brody, G.S.; Epstein, A.L. Biomarkers Provide Clues to Early Events in the Pathogenesis of Breast Implant-Associated Anaplastic Large Cell Lymphoma. Aesthet. Surg. J. 2016, 36, 773–781. [Google Scholar] [CrossRef] [PubMed]
- Lechner, M.G.; Megiel, C.; Church, C.H.; Angell, T.E.; Russell, S.M.; Sevell, R.B.; Jang, J.K.; Brody, G.S.; Epstein, A.L. Survival signals and targets for therapy in breast implant-associated ALK-anaplastic large cell lymphoma. Clin. Cancer Res. 2012, 18, 4549–4559. [Google Scholar] [CrossRef] [PubMed]
- Grivennikov, S.; Karin, M. Autocrine IL-6 signaling: A key event in tumorigenesis? Cancer Cell 2008, 13, 7–9. [Google Scholar] [CrossRef] [PubMed]
- Lam, L.T.; Wright, G.; Davis, R.E.; Lenz, G.; Farinha, P.; Dang, L.; Chan, J.W.; Rosenwald, A.; Gascoyne, R.D.; Staudt, L.M. Cooperative signaling through the signal transducer and activator of transcription 3 and nuclear factor-κB pathways in subtypes of diffuse large B-cell lymphoma. Blood 2008, 111, 3701–3713. [Google Scholar] [CrossRef] [PubMed]
- Scuto, A.; Kujawski, M.; Kowolik, C.; Krymskaya, L.; Wang, L.; Weiss, L.M.; DiGiusto, D.; Yu, H.; Forman, S.; Jove, R. STAT3 inhibition is a therapeutic strategy for ABC-like diffuse large B-cell lymphoma. Cancer Res. 2011, 71, 3182–3188. [Google Scholar] [CrossRef] [PubMed]
- Lechner, M.G.; Liebertz, D.J.; Epstein, A.L. Characterization of cytokine-induced myeloid-derived suppressor cells from normal human peripheral blood mononuclear cells. J. Immunol. 2010, 185, 2273–2284. [Google Scholar] [CrossRef] [PubMed]
- Stewart, T.J.; Smyth, M.J. Improving cancer immunotherapy by targeting tumor-induced immune suppression. Cancer Metastasis Rev. 2011, 30, 125–140. [Google Scholar] [CrossRef] [PubMed]
- Hu, H.; Johani, K.; Almatroudi, A.; Vickery, K.; Van Natta, B.; Kadin, M.E.; Brody, G.; Clemens, M.; Cheah, C.Y.; Lade, S.; et al. Bacterial Biofilm Infection Detected in Breast Implant-Associated Anaplastic Large-Cell Lymphoma. Plast. Reconstr. Surg. 2016, 137, 1659–1669. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.-Y.; Chen, C.; Gao, X.-Z.; Li, J.; Yue, J.; Ling, F.; Wang, X.-C.; Shao, S.-H. Distribution of Helicobacter pylori virulence markers in patients with gastroduodenal diseases in a region at high risk of gastric cancer. Microb. Pathog. 2013, 59–60, 13–18. [Google Scholar] [CrossRef] [PubMed]
- Matysiak-Budnik, T.; Fabiani, B.; Hennequin, C.; Thieblemont, C.; Malamut, G.; Cadiot, G.; Bouché, O.; Ruskoné-Fourmestraux, A. Gastrointestinal lymphomas: French Intergroup clinical practice recommendations for diagnosis, treatment and follow-up (SNFGE, FFCD, GERCOR, UNICANCER, SFCD, SFED, SFRO, SFH). Dig. Liver Dis. 2018, 50, 124–131. [Google Scholar] [CrossRef] [PubMed]
- Ferreri, A.J.M.; Govi, S.; Pasini, E.; Mappa, S.; Bertoni, F.; Zaja, F.; Montalbán, C.; Stelitano, C.; Cabrera, M.E.; Resti, A.G.; et al. Chlamydophila Psittaci eradication with doxycycline as first-line targeted therapy for ocular adnexae lymphoma: Final results of an international phase II trial. J. Clin. Oncol. 2012, 30, 2988–2994. [Google Scholar] [CrossRef] [PubMed]

© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mempin, M.; Hu, H.; Chowdhury, D.; Deva, A.; Vickery, K. The A, B and C’s of Silicone Breast Implants: Anaplastic Large Cell Lymphoma, Biofilm and Capsular Contracture. Materials 2018, 11, 2393. https://doi.org/10.3390/ma11122393
Mempin M, Hu H, Chowdhury D, Deva A, Vickery K. The A, B and C’s of Silicone Breast Implants: Anaplastic Large Cell Lymphoma, Biofilm and Capsular Contracture. Materials. 2018; 11(12):2393. https://doi.org/10.3390/ma11122393
Chicago/Turabian StyleMempin, Maria, Honghua Hu, Durdana Chowdhury, Anand Deva, and Karen Vickery. 2018. "The A, B and C’s of Silicone Breast Implants: Anaplastic Large Cell Lymphoma, Biofilm and Capsular Contracture" Materials 11, no. 12: 2393. https://doi.org/10.3390/ma11122393
APA StyleMempin, M., Hu, H., Chowdhury, D., Deva, A., & Vickery, K. (2018). The A, B and C’s of Silicone Breast Implants: Anaplastic Large Cell Lymphoma, Biofilm and Capsular Contracture. Materials, 11(12), 2393. https://doi.org/10.3390/ma11122393






