Magnesium Implants: Prospects and Challenges
Abstract
:1. Introduction
2. Temporary Implants
3. Corrosion: The Major Drawback of Magnesium Implants
4. In-Vitro Corrosion of Magnesium Implants in Various Simulated Physiological Environments
4.1. Influence of Inorganic Ions Present in the In-Vitro Electrolytes
4.2. Influence of Organic Components Present in the In-Vitro Electrolytes
5. Protective Coatings to Improve the Corrosion Resistance of Magnesium Implants
5.1. Biodegradable Polymeric Coatings
5.2. Biodegradable Silane Coatings
5.3. Biodegradable Calcium Phosphate Coatings
5.4. Graphene-Derivative-Based Coatings
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Mushahary, D. Surface Functionalisation of Magnesium Alloys for Use as Bio-Implants; Institute for Frontier Materials, Deakin University: Geelong, Australia, 2014. [Google Scholar]
- Niinomi, M. Recent metallic materials for biomedical applications. Metall. Mater. Trans. A 2002, 33, 477. [Google Scholar] [CrossRef]
- Williams, D.F. Corrosion of Implant Materials. Annu. Rev. Mater. Sci. 1976, 6, 237–266. [Google Scholar] [CrossRef]
- Nielsen, K. Corrosion of metallic implants. Br. Corros. J. 1987, 22, 272–278. [Google Scholar] [CrossRef]
- Niinomi, M. Metallic biomaterials. J. Artif. Organs 2008, 11, 105. [Google Scholar] [CrossRef] [PubMed]
- Witte, F. The history of biodegradable magnesium implants: A review. Acta Biomater. 2011, 6, 1680–1692. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.Y.; Wicklund, B.H.; Gustilo, R.B.; Tsukayama, D.T. Titanium, chromium and cobalt ions modulate the release of bone-associated cytokines by human monocytes/macrophages in vitro. Biomaterials 1996, 17, 2233–2240. [Google Scholar] [CrossRef]
- Erne, P.; Schier, M.; Resink, T.J. The Road to Bioabsorbable Stents: Reaching Clinical Reality? CardioVasc. Int. Radiol. 2006, 29, 11–16. [Google Scholar] [CrossRef]
- Staiger, M.P.; Pietak, A.M.; Huadmai, J.; Dias, G. Magnesium and its alloys as orthopedic biomaterials: A review. Biomaterials 2006, 27, 1728–1734. [Google Scholar] [CrossRef] [PubMed]
- Zeng, R.; Dietzel, W.; Witte, F.; Hort, N.; Blawert, C. Progress and Challenge for Magnesium Alloys as Biomaterials. Adv. Eng. Mater. 2008, 10, B3–B14. [Google Scholar] [CrossRef]
- Zberg, B.; Uggowitzer, P.J.; Loffler, J.F. MgZnCa glasses without clinically observable hydrogen evolution for biodegradable implants. Nat. Mater. 2009, 8, 887–891. [Google Scholar] [CrossRef]
- Walker, J.; Shadanbaz, S.; Woodfield, T.B.F.; Staiger, M.P.; Dias, G.J. Magnesium biomaterials for orthopedic application: A review from a biological perspective. J. Biomed. Mater. Res. Part B Appl. Biomater. 2014, 102, 1316–1331. [Google Scholar] [CrossRef] [PubMed]
- Song, G.-L. Corrosion of Magnesium Alloys; Woodhead Publishing: Cambridge, UK, 2011. [Google Scholar]
- Böstman, O.M. Osteolytic changes accompanying degradation of absorbable fracture fixation implants. J. Bone Jt. Surg. 1991, 73, 679–682. [Google Scholar] [CrossRef]
- Cheung, H.-Y.; Lau, K.-T.; Lu, T.-P.; Hui, D. A critical review on polymer-based bio-engineered materials for scaffold development. Compos. Part B Eng. 2007, 38, 291–300. [Google Scholar] [CrossRef]
- Neves, N.M.; Kouyumdzhiev, A.; Reis, R.L. The morphology, mechanical properties and ageing behavior of porous injection molded starch-based blends for tissue engineering scaffolding. Mater. Sci. Eng. C 2005, 25, 195–200. [Google Scholar] [CrossRef] [Green Version]
- Wong, P.-C.; Tsai, P.-H.; Li, T.-H.; Cheng, C.-K.; Jang, J.S.C.; Huang, J.C. Degradation behavior and mechanical strength of Mg-Zn-Ca bulk metallic glass composites with Ti particles as biodegradable materials. J. Alloys Compd. 2017, 699, 914–920. [Google Scholar] [CrossRef]
- Song, Y.W.; Shan, D.Y.; Han, E.H. Electrodeposition of hydroxyapatite coating on AZ91D magnesium alloy for biomaterial application. Mater. Lett. 2008, 62, 3276–3279. [Google Scholar] [CrossRef]
- Hänzi, A.C.; Gerber, I.; Schinhammer, M.; Löffler, J.F.; Uggowitzer, P.J. On the in vitro and in vivo degradation performance and biological response of new biodegradable Mg–Y–Zn alloys. Acta Biomater. 2010, 6, 1824–1833. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, J.J.M.D.; Hallab, N.J.P.; Skipor, A.K.M.S.; Urban, R.M.A.S. Metal Degradation Products: A Cause for Concern in Metal-Metal Bearings? Clin. Orthop. Relat. Res. 2003, 417, 139–147. [Google Scholar]
- Wolf, F.; Cittadini, A. Chemistry and Biochemistry of Magnesium. Mol. Asp. Med. 2003, 24, 3–9. [Google Scholar] [CrossRef]
- Harandi, S.E.; Banerjee, P.C.; Easton, C.D.; Singh Raman, R.K. Influence of bovine serum albumin in Hanks’ solution on the corrosion and stress corrosion cracking of a magnesium alloy. Mater. Sci. Eng. C 2017, 80, 335–345. [Google Scholar] [CrossRef]
- Grimm, M.J. Selection of Materials for Biomedical Applications. In Handbook of Materials Selection; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2007. [Google Scholar] [CrossRef]
- Witte, F.; Hort, N.; Vogt, C.; Cohen, S.; Kainer, K.U.; Willumeit, R.; Feyerabend, F. Degradable biomaterials based on magnesium corrosion. Curr. Opin. Solid State Mater. Sci. 2008, 12, 63–72. [Google Scholar] [CrossRef]
- Witte, F. Reprint of: The history of biodegradable magnesium implants: A review. Acta Biomater. 2015, 23, S28–S40. [Google Scholar] [CrossRef] [PubMed]
- Witte, F.; Fischer, J.; Nellesen, J.; Crostack, H.-A.; Kaese, V.; Pisch, A.; Beckmann, F.; Windhagen, H. In vitro and in vivo corrosion measurements of magnesium alloys. Biomaterials 2006, 27, 1013–1018. [Google Scholar] [CrossRef] [PubMed]
- McBRIDE, E.D. Absorbable metal in bone surgery: A further report on the use of magnesium alloys. J. Am. Med. Assoc. 1938, 111, 2464–2467. [Google Scholar] [CrossRef]
- Witte, F.; Kaese, V.; Haferkamp, H.; Switzer, E.; Meyer-Lindenberg, A.; Wirth, C.J.; Windhagen, H. In vivo corrosion of four magnesium alloys and the associated bone response. Biomaterials 2005, 26, 3557–3563. [Google Scholar] [CrossRef] [PubMed]
- Friedrich, H.E.; Mordike, B.L. Magnesium Technology; Springer: Berlin/Heidelberg, Germany, 2006. [Google Scholar] [CrossRef]
- Avedesian, M.M.; Baker, H. (Eds.) Magnesium and Magnesium Alloys, ASM Speciality Handbook; ASM International: Materials Park, OH, USA, 1999. [Google Scholar]
- Choudhary, L.; Singh Raman, R.K. Magnesium alloys as body implants: Fracture mechanism under dynamic and static loadings in a physiological environment. Acta Biomater. 2012, 8, 916–923. [Google Scholar] [CrossRef] [PubMed]
- Raman, R.K.S.; Choudhary, L. Cracking of magnesium-based biodegradable implant alloys under the combined action of stress and corrosive body fluid: A review. Emerg. Mater. Res. 2013, 2, 219–228. [Google Scholar] [CrossRef]
- Kannan, M.B.; Raman, R.K.S. In vitro degradation and mechanical integrity of calcium-containing magnesium alloys in modified-simulated body fluid. Biomaterials 2008, 29, 2306–2314. [Google Scholar] [CrossRef] [PubMed]
- Bobby Kannan, M.; Singh Raman, R.K.; Witte, F.; Blawert, C.; Dietzel, W. Influence of circumferential notch and fatigue crack on the mechanical integrity of biodegradable magnesium-based alloy in simulated body fluid. J. Biomed. Mater. Res. Part B Appl. Biomater. 2011, 96, 303–309. [Google Scholar] [CrossRef] [PubMed]
- Bobby Kannan, M.; Singh Raman, R.K. Evaluating the stress corrosion cracking susceptibility of Mg–Al–Zn alloy in modified-simulated body fluid for orthopaedic implant application. Scr. Mater. 2008, 59, 175–178. [Google Scholar] [CrossRef]
- Song, G. Control of biodegradation of biocompatable magnesium alloys. Corros. Sci. 2007, 49, 1696–1701. [Google Scholar] [CrossRef]
- Song, G.L.; Atren, A. Corrosion Mechanisms of Magnesium Alloys. Adv. Eng. Mater. 1999, 1, 11–33. [Google Scholar] [CrossRef]
- Zainal Abidin, N.I.; Atrens, A.D.; Martin, D.; Atrens, A. Corrosion of high purity Mg, Mg2Zn0.2Mn, ZE41 and AZ91 in Hank’s solution at 37 °C. Corros. Sci. 2011, 53, 3542–3556. [Google Scholar] [CrossRef]
- Ma, E.; Xu, J. The glass window of opportunities. Nat. Mater. 2009, 8, 855. [Google Scholar] [CrossRef]
- Atrens, A.; Liu, M.; Zainal Abidin, N.I. Corrosion mechanism applicable to biodegradable magnesium implants. Mater. Sci. Eng. B 2011, 176, 1609–1636. [Google Scholar] [CrossRef]
- Williams, D. New interest in magnesium. Med. Device Technol. 2006, 17, 9–10. [Google Scholar]
- Song, G.; Atrens, A.; John, D.S.; Wu, X.; Nairn, J. The anodic dissolution of magnesium in chloride and sulphate solutions. Corros. Sci. 1997, 39, 1981–2004. [Google Scholar] [CrossRef]
- Poinern, G.E.J.; Brundavanam, S.; Fawcett, D. Biomedical Magnesium Alloys: A Review of Material Properties, Surface Modifications and Potential as a Biodegradable Orthopaedic Implant. Am. J. Biomed. Eng. 2012, 2, 218–240. [Google Scholar] [CrossRef]
- Kraus, T.; Fischerauer, S.F.; Hänzi, A.C.; Uggowitzer, P.J.; Löffler, J.F.; Weinberg, A.M. Magnesium alloys for temporary implants in osteosynthesis: In vivo studies of their degradation and interaction with bone. Acta Biomater. 2012, 8, 1230–1238. [Google Scholar] [CrossRef] [PubMed]
- Kirkland, N.T.; Lespagnol, J.; Birbilis, N.; Staiger, M.P. A survey of bio-corrosion rates of magnesium alloys. Corros. Sci. 2010, 52, 287–291. [Google Scholar] [CrossRef]
- Xin, Y.; Liu, C.; Zhang, X.; Tang, G.; Tian, X.; Chu, P.K. Corrosion behavior of biomedical AZ91 magnesium alloy in simulated body fluids. J. Mater. Res. 2007, 22, 2004–2011. [Google Scholar] [CrossRef]
- Rettig, R.; Virtanen, S. Time-dependent electrochemical characterization of the corrosion of a magnesium rare-earth alloy in simulated body fluids. J. Biomed. Mater. Res. Part A 2008, 85, 167–175. [Google Scholar] [CrossRef] [PubMed]
- Xin, Y.; Hu, T.; Chu, P.K. In vitro studies of biomedical magnesium alloys in a simulated physiological environment: A review. Acta Biomater. 2011, 7, 1452–1459. [Google Scholar] [CrossRef] [PubMed]
- Abe, Y.; Kokubo, T.; Yamamuro, T. Apatite coating on ceramics, metals and polymers utilizing a biological process. J. Mater. Sci. Mater. Med. 1990, 1, 233–238. [Google Scholar] [CrossRef]
- Tanahashi, M.; Yao, T.; Kokubo, T.; Minoda, M.; Miyamoto, T.; Nakamura, T.; Yamamuro, T. Apatite Coating on Organic Polymers by a Biomimetic Process. J. Am. Ceram. Soc. 1994, 77, 2805–2808. [Google Scholar] [CrossRef]
- Oyane, A.; Minoda, M.; Miyamoto, T.; Nakanishi, K.; Masakazu, K.; Kokubo, T.; Nakamura, T. Apatite Formation on Ethylene-Vinyl Alcohol Copolymer Modified with Silane Coupling Agent and Calcium Silicate. Key Eng. Mater. 2000, 192–195, 713–716. [Google Scholar] [CrossRef]
- Krasner, P.; Person, P. Preserving Avulsed Teeth for Replantation. J. Am. Dent. Assoc. 1992, 123, 80–88. [Google Scholar] [CrossRef] [PubMed]
- Marques, P.A.A.P.; Magalhães, M.C.F.; Correia, R.N. Inorganic plasma with physiological CO2/HCO3− buffer. Biomaterials 2003, 24, 1541–1548. [Google Scholar] [CrossRef]
- Sigel, H.; Scheller, K.H.; Prijs, B. Metal ion/buffer interactions. Stability of alkali and alkaline earth ion complexes with triethanolamine (tea), 2-amino-2(hydroxymethyl)-1,3-propanediol (tris)and 2-[bis(2-hydroxyethyl)-amino] 2(hydroxymethyl)-1,3-propanediol (Bistris) in aqueous and mixed solvents. Inorg. Chim. Acta 1982, 66, 147–155. [Google Scholar]
- Marques, P.A.A.P.; Serro, A.P.; Saramago, B.J.; Fernandes, A.C.; Magalhães, M.C.F.; Correia, R.N. Mineralisation of two calcium phosphate ceramics in biological model fluids. J. Mater. Chem. 2003, 13, 1484–1490. [Google Scholar] [CrossRef]
- Harandi, S.E.; Singh Raman, R.K. Appropriate Mechanochemical Conditions for Corrosion-Fatigue Testing of Magnesium Alloys for Temporary Bioimplant Applications. JOM 2015, 67, 1137–1142. [Google Scholar] [CrossRef]
- Xin, Y.; Huo, K.; Tao, H.; Tang, G.; Chu, P.K. Influence of aggressive ions on the degradation behavior of biomedical magnesium alloy in physiological environment. Acta Biomater. 2008, 4, 2008–2015. [Google Scholar] [CrossRef] [PubMed]
- Song, G.; Atrens, A. Understanding Magnesium Corrosion—A Framework for Improved Alloy Performance. Adv. Eng. Mater. 2003, 5, 837–858. [Google Scholar]
- William, D.F.; William, R.L.; Ratner, B.D.; Hoffman, A.S.; Schoen, F.J.; Lemons, J.E. Biomaterials Science, 2nd ed.; Elsevier: San Diego, CA, USA, 2004. [Google Scholar]
- Yamamoto, A.; Hiromoto, S. Effect of inorganic salts, amino acids and proteins on the degradation of pure magnesium in vitro. Mater. Sci. Eng. C 2009, 29, 1559–1568. [Google Scholar] [CrossRef]
- Song, G.L.; Xu, Z. 5—Surface processing and alloying to improve the corrosion resistance of magnesium (Mg) alloys. In Corrosion Prevention of Magnesium Alloys; Song, G.-L., Ed.; Woodhead Publishing: Cambridge, UK, 2013; pp. 110–134. [Google Scholar]
- Chakraborty Banerjee, P.; Singh Raman, R.K.; Durandet, Y.; McAdam, G. Influence of Laser Processing Parameters on Microstructure and Corrosion Kinetics of Laser-Treated ZE41 Magnesium Alloy. Metall. Mater. Trans. A 2013, 44, 2346–2357. [Google Scholar] [CrossRef]
- Banerjee, P.C.; Raman, R.K.S.; Durandet, Y.; McAdam, G. Electrochemical investigation of the influence of laser surface melting on the microstructure and corrosion behaviour of ZE41 magnesium alloy—An EIS based study. Corros. Sci. 2011, 53, 1505–1514. [Google Scholar] [CrossRef]
- Chakraborty Banerjee, P.; Singh Raman, R.K. Electrochemical impedance spectroscopic investigation of the role of alkaline pre-treatment in corrosion resistance of a silane coating on magnesium alloy, ZE41. Electrochim. Acta 2011, 56, 3790–3798. [Google Scholar] [CrossRef]
- Alabbasi, A.; Liyanaarachchi, S.; Kannan, M.B. Polylactic acid coating on a biodegradable magnesium alloy: An in vitro degradation study by electrochemical impedance spectroscopy. Thin Solid Films 2012, 520, 6841–6844. [Google Scholar] [CrossRef]
- Ostrowski, N.J.; Lee, B.; Roy, A.; Ramanathan, M.; Kumta, P.N. Biodegradable poly(lactide-co-glycolide) coatings on magnesium alloys for orthopedic applications. J. Mater. Sci. Mater. Med. 2013, 24, 85–96. [Google Scholar] [CrossRef]
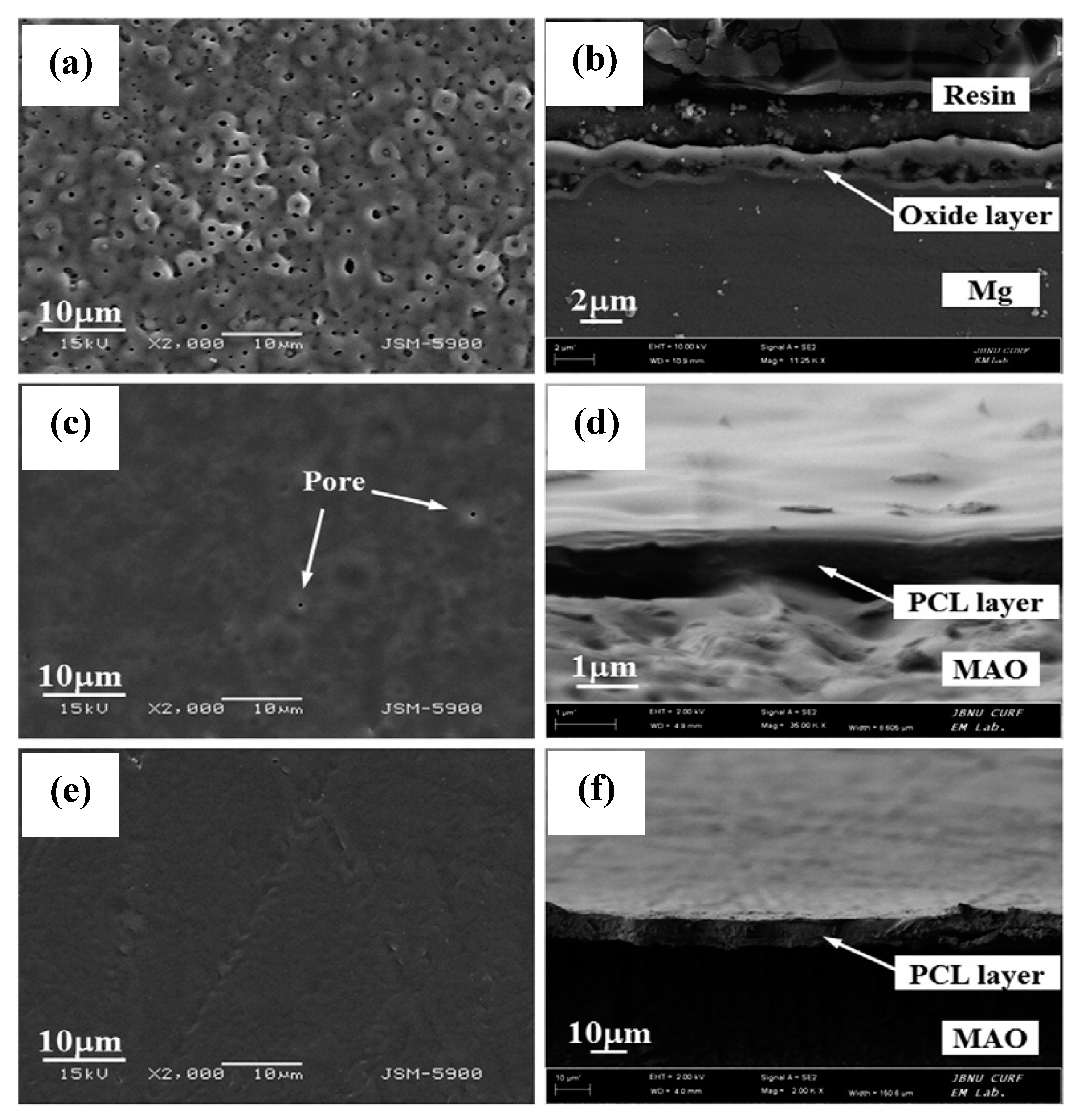
- Li, L.-H.; Sankara Narayanan, T.S.N.; Kim, Y.K.; Kong, Y.-M.; Park, I.S.; Bae, T.S.; Lee, M.H. Deposition of microarc oxidation–polycaprolactone duplex coating to improve the corrosion resistance of magnesium for biodegradable implants. Thin Solid Films 2014, 562, 561–567. [Google Scholar] [CrossRef]
- Shi, P.; Niu, B.; Shanshan, E.; Chen, Y.; Li, Q. Preparation and characterization of PLA coating and PLA/MAO composite coatings on AZ31 magnesium alloy for improvement of corrosion resistance. Surf. Coat. Technol. 2015, 262, 26–32. [Google Scholar] [CrossRef]
- Tian, P.; Xu, D.; Liu, X. Mussel-inspired functionalization of PEO/PCL composite coating on a biodegradable AZ31 magnesium alloy. Colloids Surf. B Biointerfaces 2016, 141, 327–337. [Google Scholar] [CrossRef]
- Hanas, T.; Sampath Kumar, T.S.; Perumal, G.; Doble, M. Tailoring degradation of AZ31 alloy by surface pre-treatment and electrospun PCL fibrous coating. Mater. Sci. Eng. C 2016, 65, 43–50. [Google Scholar] [CrossRef] [PubMed]
- Xi, Z.; Tan, C.; Xu, L.; Meng, Y.; Zhang, C.; Yang, N.; Li, Q. A novel functional HPPS/PCL/ZnO composite layer on AZ91 for anticorrosion. Mater. Lett. 2015, 148, 134–137. [Google Scholar] [CrossRef]
- Kim, J.; Mousa, H.M.; Park, C.H.; Kim, C.S. Enhanced corrosion resistance and biocompatibility of AZ31 Mg alloy using PCL/ZnO NPs via electrospinning. Appl. Surf. Sci. 2017, 396, 249–258. [Google Scholar] [CrossRef]
- Ravenscroft-Chang, M.S.; Stohlman, J.M.; Molnar, P.; Natarajan, A.; Canavan, H.E.; Teliska, M.; Stancescu, M.; Krauthamer, V.; Hickman, J.J. Altered calcium dynamics in cardiac cells grown on silane-modified surfaces. Biomaterials 2010, 31, 602–607. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jiang, G.; Evans, M.E.; Jones, I.A.; Rudd, C.D.; Scotchford, C.A.; Walker, G.S. Preparation of poly(ε-caprolactone)/continuous bioglass fibre composite using monomer transfer moulding for bone implant. Biomaterials 2005, 26, 2281–2288. [Google Scholar] [CrossRef] [PubMed]
- Müller, R.; Abke, J.; Schnell, E.; Macionczyk, F.; Gbureck, U.; Mehrl, R.; Ruszczak, Z.; Kujat, R.; Englert, C.; Nerlich, M.; et al. Surface engineering of stainless steel materials by covalent collagen immobilization to improve implant biocompatibility. Biomaterials 2005, 26, 6962–6972. [Google Scholar] [CrossRef] [PubMed]
- Ren, L.; Tsuru, K.; Hayakawa, S.; Osaka, A. Novel approach to fabricate porous gelatin–siloxane hybrids for bone tissue engineering. Biomaterials 2002, 23, 4765–4773. [Google Scholar] [CrossRef]
- Ren, L.; Tsuru, K.; Hayakawa, S.; Osaka, A. Synthesis and Characterization of Gelatin-Siloxane Hybrids Derived through Sol-Gel Procedure. J. Sol-Gel Sci. Technol. 2001, 21, 115–121. [Google Scholar] [CrossRef]
- Liu, X.; Yue, Z.; Romeo, T.; Weber, J.; Scheuermann, T.; Moulton, S.; Wallace, G. Biofunctionalized anti-corrosive silane coatings for magnesium alloys. Acta Biomater. 2013, 9, 8671–8677. [Google Scholar] [CrossRef] [Green Version]
- Gaur, S.; Singh Raman, R.K.; Khanna, A.S. In vitro investigation of biodegradable polymeric coating for corrosion resistance of Mg-6Zn-Ca alloy in simulated body fluid. Mater. Sci. Eng. C 2014, 42, 91–101. [Google Scholar] [CrossRef] [PubMed]
- Gaur, S.; Nigam, S.; Khanna, A.S.; Raman, R.K.S. Silane-Coated Magnesium Implants with Improved In-Vitro Corrosion Resistance and Biocompatibility. J. Mater. Sci. Surf. Eng. 2016, 4, 415–424. [Google Scholar]
- Córdoba, L.C.; Montemor, M.F.; Coradin, T. Silane/TiO2 coating to control the corrosion rate of magnesium alloys in simulated body fluid. Corros. Sci. 2016, 104, 152–161. [Google Scholar] [CrossRef]
- Al-Saadi, S.; Banerjee, P.C.; Anisur, M.; Raman, R.S. Hexagonal Boron Nitride Impregnated Silane Composite Coating for Corrosion Resistance of Magnesium Alloys for Temporary Bioimplant Applications. Metals 2017, 7, 518. [Google Scholar] [CrossRef]
- Paital, S.R.; Dahotre, N.B. Calcium phosphate coatings for bio-implant applications: Materials, performance factors, and methodologies. Mater. Sci. Eng. R Rep. 2009, 66, 1–70. [Google Scholar] [CrossRef]
- Song, Y.; Zhang, S.; Li, J.; Zhao, C.; Zhang, X. Electrodeposition of Ca–P coatings on biodegradable Mg alloy: In vitro biomineralization behavior. Acta Biomater. 2010, 6, 1736–1742. [Google Scholar] [CrossRef] [PubMed]
- Liu, G.; Wang, J.; Bian, K.; Zhu, P. Preparation and characterization of nanostructured dibasic calcium phosphate coating on magnesium alloy wire. Mater. Lett. 2017, 209, 323–326. [Google Scholar] [CrossRef]
- Jafari, S.; Singh Raman, R.K. In-vitro biodegradation and corrosion-assisted cracking of a coated magnesium alloy in modified-simulated body fluid. Mater. Sci. Eng. C 2017, 78, 278–287. [Google Scholar] [CrossRef] [PubMed]
- Kannan, M.B. Enhancing the performance of calcium phosphate coating on a magnesium alloy for bioimplant applications. Mater. Lett. 2012, 76, 109–112. [Google Scholar] [CrossRef]
- Wang, H.X.; Guan, S.K.; Wang, X.; Ren, C.X.; Wang, L.G. In vitro degradation and mechanical integrity of Mg–Zn–Ca alloy coated with Ca-deficient hydroxyapatite by the pulse electrodeposition process. Acta Biomater. 2010, 6, 1743–1748. [Google Scholar] [CrossRef]
- Meng, E.C.; Guan, S.K.; Wang, H.X.; Wang, L.G.; Zhu, S.J.; Hu, J.H.; Ren, C.X.; Gao, J.H.; Feng, Y.S. Effect of electrodeposition modes on surface characteristics and corrosion properties of fluorine-doped hydroxyapatite coatings on Mg–Zn–Ca alloy. Appl. Surf. Sci. 2011, 257, 4811–4816. [Google Scholar] [CrossRef]
- Surmeneva, M.A.; Mukhametkaliyev, T.M.; Khakbaz, H.; Surmenev, R.A.; Bobby Kannan, M. Ultrathin film coating of hydroxyapatite (HA) on a magnesium–calcium alloy using RF magnetron sputtering for bioimplant applications. Mater. Lett. 2015, 152, 280–282. [Google Scholar] [CrossRef]
- Mukhametkaliyev, T.M.; Surmeneva, M.A.; Vladescu, A.; Cotrut, C.M.; Braic, M.; Dinu, M.; Vranceanu, M.D.; Pana, I.; Mueller, M.; Surmenev, R.A. A biodegradable AZ91 magnesium alloy coated with a thin nanostructured hydroxyapatite for improving the corrosion resistance. Mater. Sci. Eng. C 2017, 75, 95–103. [Google Scholar] [CrossRef]
- Ren, Y.; Zhou, H.; Nabiyouni, M.; Bhaduri, S.B. Rapid coating of AZ31 magnesium alloy with calcium deficient hydroxyapatite using microwave energy. Mater. Sci. Eng. C 2015, 49, 364–372. [Google Scholar] [CrossRef]
- Abdal-hay, A.; Amna, T.; Lim, J.K. Biocorrosion and osteoconductivity of PCL/nHAp composite porous film-based coating of magnesium alloy. Solid State Sci. 2013, 18, 131–140. [Google Scholar] [CrossRef]
- Abdal-hay, A.; Barakat, N.A.M.; Lim, J.K. Hydroxyapatite-doped poly(lactic acid) porous film coating for enhanced bioactivity and corrosion behavior of AZ31 Mg alloy for orthopedic applications. Ceram. Int. 2013, 39, 183–195. [Google Scholar] [CrossRef]
- Zomorodian, A.; Santos, C.; Carmezim, M.J.; Moura e Silva, T.; Fernandes, J.C.S.; Montemor, M.F. “In-vitro” corrosion behaviour of the magnesium alloy with Al and Zn (AZ31) protected with a biodegradable polycaprolactone coating loaded with hydroxyapatite and cephalexin. Electrochim. Acta 2015, 179, 431–440. [Google Scholar] [CrossRef]
- Kalbacova, M.; Broz, A.; Kong, J.; Kalbac, M. Graphene substrates promote adherence of human osteoblasts and mesenchymal stromal cells. Carbon 2010, 48, 4323–4329. [Google Scholar] [CrossRef]
- Lee, W.C.; Lim, C.H.Y.X.; Shi, H.; Tang, L.A.L.; Wang, Y.; Lim, C.T.; Loh, K.P. Origin of Enhanced Stem Cell Growth and Differentiation on Graphene and Graphene Oxide. ACS Nano 2011, 5, 7334–7341. [Google Scholar] [CrossRef]
- Nayak, T.R.; Andersen, H.; Makam, V.S.; Khaw, C.; Bae, S.; Xu, X.; Ee, P.-L.R.; Ahn, J.-H.; Hong, B.H.; Pastorin, G.; et al. Graphene for Controlled and Accelerated Osteogenic Differentiation of Human Mesenchymal Stem Cells. ACS Nano 2011, 5, 4670–4678. [Google Scholar] [CrossRef]
- Kim, S.; Ku, S.H.; Lim, S.Y.; Kim, J.H.; Park, C.B. Graphene–Biomineral Hybrid Materials. Adv. Mater. 2011, 23, 2009–2014. [Google Scholar] [CrossRef] [PubMed]
- Lahiri, D.; Dua, R.; Zhang, C.; de Socarraz-Novoa, I.; Bhat, A.; Ramaswamy, S.; Agarwal, A. Graphene Nanoplatelet-Induced Strengthening of UltraHigh Molecular Weight Polyethylene and Biocompatibility In vitro. ACS Appl. Mater. Interfaces 2012, 4, 2234–2241. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Liu, Q.; Jia, Z.; Xu, X.; Cheng, Y.; Zheng, Y.; Xi, T.; Wei, S. Graphene oxide/hydroxyapatite composite coatings fabricated by electrophoretic nanotechnology for biological applications. Carbon 2014, 67, 185–197. [Google Scholar] [CrossRef]
- Gao, F.; Xu, C.; Hu, H.; Wang, Q.; Gao, Y.; Chen, H.; Guo, Q.; Chen, D.; Eder, D. Biomimetic synthesis and characterization of hydroxyapatite/graphene oxide hybrid coating on Mg alloy with enhanced corrosion resistance. Mater. Lett. 2015, 138, 25–28. [Google Scholar] [CrossRef]
- Santos, C.; Piedade, C.; Uggowitzer, P.J.; Montemor, M.F.; Carmezim, M.J. Parallel nano-assembling of a multifunctional GO/HapNP coating on ultrahigh-purity magnesium for biodegradable implants. Appl. Surf. Sci. 2015, 345, 387–393. [Google Scholar] [CrossRef]












| Types of Implants | Materials Used |
|---|---|
| Metal | Titanium alloys, stainless steel, gold alloys, cobalt–Chromium alloys, platinum electrodes |
| Polymers | Poly(methyl-methacrilate), Polyethylenes, polypropelenes, polyamides, polyesters, hydrogels |
| Ceramics | Alumina, Zirconia, hydroxiapatite, porceins, phosphates, bioactive glass |
| Composites | Poly(methyl-methacrilate)-glass fibers, Bisphenol-A-glycidyl-methacrylate-quartz/silica fillers |
| Material | Immersion Time (days) | Compressive Modulus (MPa) | Compressive Strength (MPa) | Fracture Strain (%) |
| Poly-lactic acid | 0 | 200 ± 45 | 14 ± 5 | 30 ± 9 |
| Poly-lactic acid | 3 | 22 ± 3 | 5 ± 3 | 35 ± 8 |
| Poly-lactic acid | 14 | 39 ± 9 | 4 ± 2 | 32 ± 2 |
| Material | Immersion Time (days) | Compressive Modulus (MPa) | Fracture Strain (%) | |
| Poly-lactic acid | 0 | 200 ± 45 | 14 ± 5 | 30 ± 9 |
| Poly-lactic acid | 3 | 22 ± 3 | 5 ± 3 | 35 ± 8 |
| Poly-lactic acid | 14 | 39 ± 9 | 4 ± 2 | 32 ± 2 |
| Property | Natural Bone | Magnesium Alloys | Titanium Alloys | Cobalt–Chromium Alloys | Stainless Steels |
|---|---|---|---|---|---|
| Density (g/cm3) | 1.8–2.1 | 1.74–2.0 | 4.4–4.5 | 8.3–9.2 | 7.9–8.1 |
| Elastic modulus (GPa) | 3–20 | 41–45 | 110–117 | 230 | 189–205 |
| Yield strength (MPa) | 130–180 | 85–190 | 758–1117 | 450–1000 | 170–310 |
| Quantity of Ions and Organic Components | Blood Plasma | Hanks’ Solution | Ringer’s Solution | DMEM | PBS | Original SBF | c-SBF | r-SBF | i-SBF | m-SBF | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Na+ | (mmol L−1) | 142 | 142 | 130 | 1273 | 157 | 142 | 142 | 142 | 142 | 142 |
| K+ | (mmol L−1) | 5 | 5.9 | 4 | 5.3 | 4.1 | 5 | 5 | 5 | 5 | 5 |
| Ca+ | (mmol L−1) | 2.5 | 1.3 | 1.4 | 1.8 | _ | 2.5 | 2.5 | 2.5 | 1.6 | 2.5 |
| Mg2+ | (mmol L−1) | 1.5 | 0.8 | _ | 0.8 | _ | 1.5 | 1.5 | 1.5 | 1 | 1.5 |
| HCO3− | (mmol L−1) | 27 | 4.2 | _ | 44.1 | _ | 4.2 | 4.2 | 27 | 27 | 10 |
| Cl− | (mmol L−1) | 103 | 145 | 109 | 90.8 | 140 | 148.8 | 147.8 | 103 | 103 | 103 |
| HPO42− | (mmol L−1) | 1 | 0.8 | _ | 0.9 | 11.5 | 1 | 1 | 1 | 1 | 1 |
| SO42− | (mmol L−1) | 0.5 | 0.8 | _ | 0.8 | _ | 0 | 0.5 | 0.5 | 0.5 | 0.5 |
| Buffer | _ | _ | _ | _ | HEPES | _ | Tris | Tris | HEPES | HEPES | HEPES |
| Amino acids | (g L−1) | _ | _ | _ | 1.6 | _ | _ | _ | _ | _ | _ |
| Glucose | (g L−1) | 0.65–1.1 | 1 | _ | 4.5 | _ | _ | _ | _ | _ | _ |
| Albumin | (g L−1) | 30–55 | _ | _ | _ | _ | _ | _ | _ | _ | _ |
| α-globulins | (g L−1) | 5–10 | _ | _ | _ | _ | _ | _ | _ | _ | _ |
| β-globulins | (g L−1) | 6–12 | _ | _ | _ | _ | _ | _ | _ | _ | _ |
| γ-globulins | (g L−1) | 6.6–15 | _ | _ | _ | _ | _ | _ | _ | _ | _ |
| α1-lipoproteins | (g L−1) | 6–12 | _ | _ | _ | _ | _ | _ | _ | _ | _ |
| Fibronogen | (g L−1) | 1.7–4.3 | _ | _ | _ | _ | _ | _ | _ | _ | _ |
| cholesterol | (g L−1) | 1.2–2.5 | _ | _ | _ | _ | _ | _ | _ | _ | _ |
| Fatty acids | (g L−1) | 1.9–4.5 | _ | _ | _ | _ | _ | _ | _ | _ | _ |
| Lactate | (mmol L−1) | 0.5–2.2 | _ | _ | _ | _ | _ | _ | _ | _ | _ |
| Urea | (mmol L−1) | 3–7 | _ | _ | _ | _ | _ | _ | _ | _ | _ |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chakraborty Banerjee, P.; Al-Saadi, S.; Choudhary, L.; Harandi, S.E.; Singh, R. Magnesium Implants: Prospects and Challenges. Materials 2019, 12, 136. https://doi.org/10.3390/ma12010136
Chakraborty Banerjee P, Al-Saadi S, Choudhary L, Harandi SE, Singh R. Magnesium Implants: Prospects and Challenges. Materials. 2019; 12(1):136. https://doi.org/10.3390/ma12010136
Chicago/Turabian StyleChakraborty Banerjee, Parama, Saad Al-Saadi, Lokesh Choudhary, Shervin Eslami Harandi, and Raman Singh. 2019. "Magnesium Implants: Prospects and Challenges" Materials 12, no. 1: 136. https://doi.org/10.3390/ma12010136
APA StyleChakraborty Banerjee, P., Al-Saadi, S., Choudhary, L., Harandi, S. E., & Singh, R. (2019). Magnesium Implants: Prospects and Challenges. Materials, 12(1), 136. https://doi.org/10.3390/ma12010136







